Obesity is associated with enhanced breast cancer mortality, yet the mechanisms underlying this relationship remain poorly understood. McDowell et al. provide insight into the role of obesity on myeloid-driven cancer metastasis by identifying how monocyte development is skewed to promote prometastatic neutrophil effector functions.
Abstract
Obesity is characterized by chronic systemic inflammation and enhances cancer metastasis and mortality. Obesity promotes breast cancer metastasis to lung in a neutrophil-dependent manner; however, the upstream regulatory mechanisms of this process remain unknown. Here, we show that obesity-induced monocytes underlie neutrophil activation and breast cancer lung metastasis. Using mass cytometry, obesity favors the expansion of myeloid lineages while restricting lymphoid cells within the peripheral blood. RNA sequencing and flow cytometry revealed that obesity-associated monocytes resemble professional antigen-presenting cells due to a shift in their development and exhibit enhanced MHCII expression and CXCL2 production. Monocyte induction of the CXCL2–CXCR2 axis underlies neutrophil activation and release of neutrophil extracellular traps to promote metastasis, and enhancement of this signaling axis is observed in lung metastases from obese cancer patients. Our findings provide mechanistic insight into the relationship between obesity and cancer by broadening our understanding of the interactive role that myeloid cells play in this process.
Introduction
The link between obesity and cancer is well-established, with many types of cancer showing increased mortality rates in obese individuals. During weight gain, adipocytes undergo hyperplasia and hypertrophy, leading to the recruitment and activation of innate immune cells to establish a proinflammatory adipose tissue microenvironment (ATME) that is dominated by a substantial myeloid compartment (Brestoff and Artis, 2015; Jaitin et al., 2019). The metabolic and inflammatory demands of the obese ATME cause chronic systemic changes, such as altered levels of adipokines, proinflammatory cytokines, free fatty acids, and systemic markers of oxidative stress. These changes contribute to the development of metabolic syndrome, chronic leukocytosis, and impaired immune function, and disrupt tissue homeostasis across many organs. As such, ATME inflammation and its associated systemic effects are thought to contribute to the link between obesity and cancer progression, where metastasis is also sensitive to systemic regulatory factors (Olson et al., 2017; Quail and Dannenberg, 2019).
Obesity is associated with enhanced breast cancer (BC) mortality (Calle et al., 2003; Petrelli et al., 2021), particularly in postmenopausal women. BC mortality is largely driven by metastasis, and in obese individuals, metastasis to lung and liver are most affected (Osman and Hennessy, 2015). Preclinical studies examining lung metastasis have shown that obesity changes the myeloid landscape to be more permissive to dissemination. This is driven by adipose tissue–derived factors, such as IL5 and GM-CSF, which stimulate the expansion of monocytes and neutrophils within the periphery (Quail et al., 2017). As neutrophils are cleared into tissues, such as lung, they exhibit heightened effector functions including increased ROS production and neutrophil extracellular trap (NET) formation, which cause a breakdown in vascular barrier integrity to enable metastatic transmigration (McDowell et al., 2021). The ability of obesity to stimulate monocytosis systemically is well-established (Nagareddy et al., 2014), although the functional role of monocytes in obesity-associated cancer is less clear. Both of these myeloid populations are highly plastic and can adopt various activation states in response to microenvironmental cues (Ballesteros et al., 2020). Pathological conditions can also enrich for myeloid cells of specific developmental states, including those that are unique to cancer (Evrard et al., 2018; Zilionis et al., 2019). However, little is known about how myeloid developmental states shift in response to obesity to facilitate these processes and how they affect overall immune function both within innate and adaptive compartments.
Here, we investigate how obesity alters the systemic immune landscape to shape the acquisition of myeloid identities that underlie BC metastasis. Using high-parameter immune profiling, we demonstrate that obesity biases immune lineages toward myeloid populations at the expense of the lymphoid compartment. Within the myeloid pool, obesity enriches for Ly6Chi monocytes with a professional antigen-presenting cell (pAPC)-like phenotype, which support the maturation and effector function of neutrophils to promote metastatic progression. Our findings refine prior work linking obesity with neutrophilia and monocytosis (McDowell et al., 2021; Nagareddy et al., 2014) and define how these systemic processes are developmentally connected in the context of cancer metastasis.
Results
Obesity causes systemic immunological changes and a myeloid bias
To investigate the effects of obesity on systemic immunological responses, we first explored changes in peripheral immune cell populations in lean and obese mice. Based on our previous work (McDowell et al., 2021), we used a genetically induced obesity (GIO) model in which female B6.Cg-Lepob/J (ob/ob) mice fed a normal diet display hyperphagia due to a leptin deficiency and rapidly gain weight compared with control WT C57BL6 mice (Zhang et al., 1994; Fig. S1 A). We performed mass cytometry time-of-flight (CyTOF) on blood from WT and ob/ob mice using a panel of 33 antibodies to define functionally distinct states within major myeloid and lymphoid immune lineages (Fig. S1 B and Table S1). Supervised clustering analysis was performed using the uniform manifold approximation and projection (UMAP) algorithm (Becht et al., 2018) to separate all samples into a two-dimensional plot based on their expression of the 33 markers (Fig. 1, A and B). We identified distinct myeloid and lymphoid populations through canonical cell surface markers, including neutrophils, Ly6C− and Ly6Chi monocytes, dendritic cells (DCs), natural killer cells, B cells, and various subsets of T cells (regulatory, helper, and cytotoxic; Fig. 1 B). Through this approach, lymphoid cells were the most abundant peripheral immune compartment in WT samples, while myeloid cells were most abundant in ob/ob samples (Fig. 1 C and Fig. S1 C). This pattern was consistent with the enrichment in neutrophil-to-lymphocyte ratios observed in obese humans (Suarez-Cuenca et al., 2019), which was also evident in our dataset (Fig. S1D). Notably, B cells had the highest frequency in WT samples, while neutrophils had the highest frequency in ob/ob samples (Fig. 1C), consistent with our previous work (McDowell et al., 2021). Monocytes (both Ly6C− and Ly6Chi) were also enriched in ob/ob samples compared with WT samples, while CD4+ and CD8+ T cell frequencies were reduced (Fig. 1 C). These data are consistent with findings that obesity is associated with enhanced myelopoiesis and monocytosis (Nagareddy et al., 2014) and myeloid-mediated suppression of the lymphoid compartment (Clements et al., 2018; Xia et al., 2011).
Figure S1.
Obesity reduces the proportion of lymphoid populations. (A) Bar graph depicting the average weight of the leptin-deficient model of GIO. WT, n = 9 mice; ob/ob, n = 8 mice; mean ± SEM; Student’s t test. (B) Gating strategy for CyTOF cell-type identification in WT and ob/ob blood. (C) Pie chart of lymphoid and myeloid MC distribution from CyTOF. WT, n = 4 mice; ob/ob, n = 4 mice. (D) Neutrophil-to-lymphocyte ratio from CyTOF. WT, n = 4 mice; ob/ob, n = 4 mice; mean ± SEM. Student’s t test. (E) Pie chart of lymphoid MC distribution from CyTOF. WT, n = 4 mice; ob/ob, n = 4 mice. (F) UMAP plot of unsupervised PhenoGraph analysis of the CD45+ CD3+ T cell compartment from CyTOF. WT, n = 4 mice; ob/ob, n = 4 mice. (G) Heatmap of marker expression (x axis) across TMCs (y axis) from F. Normalization by z-score. Coloured bars along y axis correspond to cell types in legend. (H) Quantification of four CD4+ TMCs as a percentage of total T cells. WT, n = 4 mice; ob/ob, n = 4 mice; mean ± SEM; Student’s t test. (I and J) Flow cytometric analysis of the proportion of PD-1+ cells (I, left), TNFα+ cells (I, right), or FOXP3+ cells (J) out of total CD4+ T cells in LF and HF lung. HF, n = 10 mice; LF, n = 10 mice; mean ± SEM; Student’s t test. (K) Gating strategy for cell-type identification of neutrophil and monocytes. (L) Flow cytometric analysis of CD45+ CD11b− lymphoid cells (left) and CD45+ CD11b+ myeloid cells (right) as a percentage of live cells in WT and ob/ob blood samples. WT, n = 10 mice; ob/ob, n = 10 mice; mean ± SEM; Student’s t test. (M) Bar graph depicting average weight of the DIO model. n = 9 mice per group; mean ± SEM; Student’s t test. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001.
Figure 1.
Obesity causes systemic immunological changes and a myeloid bias. (A) UMAP of mass cytometric analyses of CD45+ cells in WT or ob/ob blood, including (left) density plot and (right) contour plot (WT, n = 4 mice; ob/ob, n = 4 mice). (B) Designation of cell types from mass cytometry data in A. (C) Quantification of cell types identified in B between WT and ob/ob mice. (D) UMAP of unsupervised PhenoGraph analysis of mass cytometry data in A. (E) Heatmap of marker expression (x axis) across immune MCs (y axis) from D. Normalization by z-score. Colored bars along y axis correspond to cell types in the legend. (F) Pie chart of myeloid MC distribution between WT and ob/ob mice, based on analysis in E. (G and H) Flow cytometric analysis of neutrophils (left) and monocytes (right) as a percentage of live cells in WT and ob/ob blood (G) or lung (H). WT, n = 10 mice; ob/ob, n = 10 mice; mean ± SEM; Student’s t test. (I) Flow cytometric analysis of neutrophils (left) and monocytes (right) as a percentage of live cells in LF and HF lung. LF, n = 9 mice; HF, n = 10 mice; mean ± SEM; Student’s t test. (J) Immunofluorescence quantification of CCR2+ cells as a percentage of total DAPI+ cells in LF and HF lung samples. LF, n = 4 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. (K) Representative immunofluorescence image for quantification shown in J. Scale bar = 100 μm. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
To expand these observations, we performed unsupervised clustering analysis via the PhenoGraph algorithm (Levine et al., 2015), which distributed our high-dimensional data into 36 unique metaclusters (MC; Fig. 1, D and E). Consistent with our analysis of major populations (Fig. 1 C), obesity was associated with an enrichment in myeloid-related MC (Fig. 1 F) and a decrease in lymphoid-related MC (Fig. S1 E). Among the lymphoid pool, the overall frequencies of T cell clusters MC17 and MC22 were significantly decreased by obesity (Fig. S1 E), which expressed high CTLA-4, PD-1, and CD86 along with low Ki67 (Fig. 1 E), suggestive of exhaustion. To explore this relationship in more detail, we gated on total CD3+ cells and reclustered cells into 24 states (termed TMC; Fig. S1, F and G). Of all TMC affected by obesity, the majority were from the CD4+ T cell compartment and all were decreased as a percentage of total T cells (TMC5, 9, 11, and 12; Fig. S1 H). Within the CD4+ T cell pool, flow cytometry revealed a significant increase in the proportion of cells with elevated PD-1 expression and reduced production of the proinflammatory cytokine TNFα upon ex vivo stimulation (Fig. S1 I), as well as an increase in the proportion of FOXP3+ T regulatory (Treg) cells (Fig. S1 J). Together these data painted an overall picture of weakened adaptive immune responses, particularly in the CD4+ compartment, whereby multiple T cell subsets are reduced in frequency and those that remain appear functionally impaired.
Within the myeloid compartment, many MCs were overrepresented in ob/ob compared with WT samples, including MC1 and 4 (Ly6Chi monocytes) and MC2, 5, 6, and 9 (Ly6G+ neutrophils; Fig. 1, E and F). Given previous findings that obesity-associated BC metastasis to the lungs is driven by CD11b+Gr1+ cells (Clements et al., 2018; Quail et al., 2017), yet the inability of Gr1 to effectively discern between Ly6C and Ly6G expression, we focused our attention on myeloid clusters to further resolve Ly6C+ and Ly6G+ populations using flow cytometry for canonical markers (Fig. S1 K). We confirmed that peripheral immune populations shift from lymphoid to myeloid during obesity (Fig. S1 L), validating our CyTOF findings (Fig. S1 C). Moreover, ob/ob mice exhibited elevated proportions of Ly6G+Ly6Clo neutrophils and Ly6G−Ly6Chi monocytes in blood and lungs compared with WT mice (Fig. 1, G and H). These findings refine previous observations that CD11b+Gr1+ cells are elevated in blood and lungs in response to obesity, where they mediate BC metastatic progression (Quail et al., 2017). We confirmed these results using a diet-induced obesity (DIO) model in which female WT C57BL6 mice were enrolled on a low-fat (LF) or high-fat (HF) diet for 15 wk (Fig. S1 M). This model shares similar myeloid aberrances observed in ob/ob mice in the context of BC (McDowell et al., 2021; Quail et al., 2017). Reflecting our findings in ob/ob mice, HF lungs displayed elevated numbers of both Ly6G+Ly6Clo neutrophils and Ly6G−Ly6Chi monocytes compared with LF lungs (Fig. 1 I). To confirm the inflammatory status of these monocytes (Geissmann et al., 2003), we performed immunofluorescence staining for CCR2 within lung tissues and observed increased CCR2+ cells in HF versus LF mice (Fig. 1, J and K). Taken together, these data confirm our CyTOF findings that obesity increases neutrophil and monocyte populations in mice, including inflammatory monocyte states.
Obesity alters monocyte identities
To further interrogate obesity-associated myeloid identities in greater detail, we gated on total CD45+ CD11b+ cells and reclustered cells into 28 states (termed MMC; Fig. 2 A). We observed drastic differences in MMC frequencies between WT and ob/ob samples (Fig. 2 B), the vast majority of which were Ly6G+ and/or Ly6C+ (Fig. S2 A), indicative of neutrophil and monocyte identities. Of these, six MMCs highly expressed Ly6C (Fig. 2 C) and all were significantly enriched during obesity (MMC11, 12, 17, 18, 20, and 26; Fig. 2 D), consistent with our flow cytometry and immunofluorescence analyses that inflammatory monocytes are enriched in obese hosts (Fig. 1, G–K). Across these Ly6Chi MMCs, we observed differences in the expression of various phenotypic markers, including Ki67, which was prominent in MMC18, 20, and 26, indicative of a proliferative state (Fig. 2 E). In addition, we found shifts in MHCII and the costimulatory markers CD40 and CD86. Of note, MMC11 was the top upregulated MMC during obesity and uniquely expressed CD11c and MHCII together (Fig. 2, D and E; and Fig. S2, B and C), markers more typically expressed by pAPCs. These data suggest that monocytes may exhibit functionally distinct states during obesity with enrichment for those with an pAPC-like identity, consistent with our findings of altered CD4+ T cell populations (Fig. S1, H and I). Moreover, within the total pool of Ly6Chi monocytes, the frequency of cells expressing the coregulatory molecules CD80 and CD86 was increased (Fig. S2 D), aligning with our finding of increased Tregs with obesity (which express the binding partner, CTLA-4; Fig S1 J).
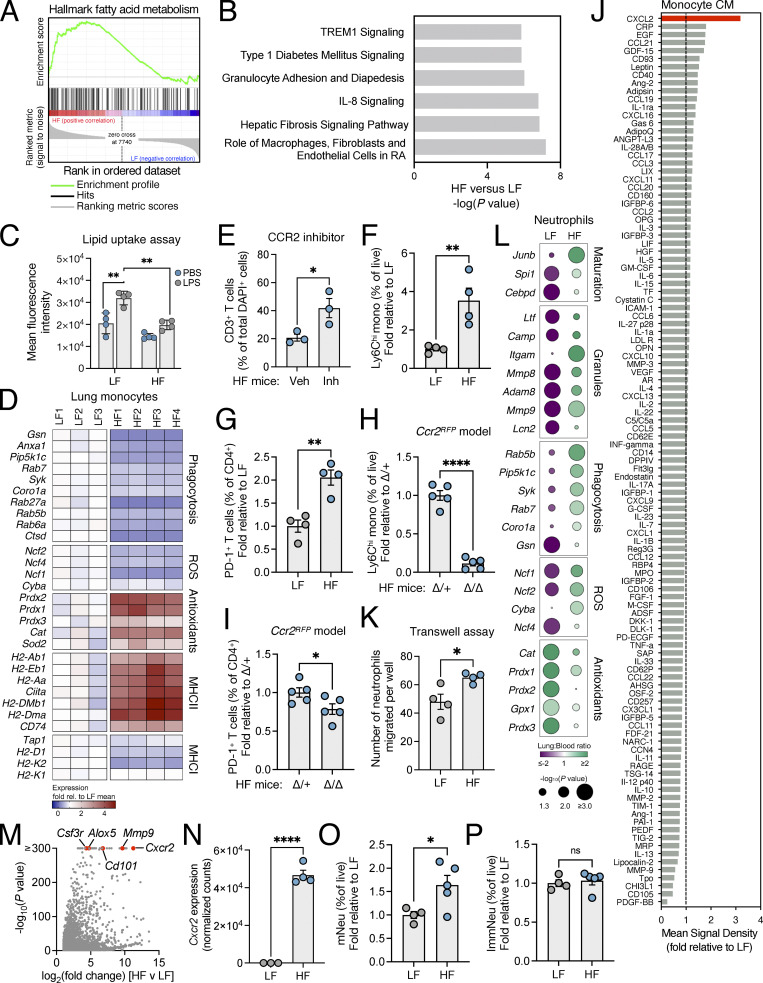
Figure 2.
Obesity alters monocyte identities. (A) UMAP plot of unsupervised phenograph analysis of CD45+ CD11b+ myeloid cells from mass cytometry on WT or ob/ob blood (WT, n = 4 mice; ob/ob, n = 4 mice). (B) MMC distribution between WT and ob/ob blood samples based on analysis in A. (C) Heatmap of marker expression (x axis) across MMC (y axis) from A. Normalization by z-score. Colored bars on y axis correspond to cell types in the legend. (D) CyTOF analysis of Ly6Chi MMCs in WT and ob/ob blood as a percentage of total myeloid cells. WT, n = 4 mice; ob/ob, n = 4 mice; mean ± SEM; Student’s t test. (E) Heatmap of expression of specific immune markers (x axis) across Ly6Chi MMCs (y axis) from D. (F and G) RNA-seq normalized counts for Irf8 and Klf4 (F) or Cebpe and Gfi1 (G) in LF and HF blood and lung monocytes. LF blood, n = 4 mice; LF lung, n = 3 mice; HF blood, n = 4 mice; HF lung, n = 4 mice; mean ± SEM; one-way ANOVA and Holm-Šídák test for the indicated comparisons. (H) Volcano plot showing DEGs from RNA-seq of lung monocytes from HF versus LF mice. LF, n = 3 mice; HF, n = 4 mice. (I) Flow cytometric analysis of the frequency of MDP or M-mono in BM, blood, or lungs from HF versus LF mice. Each data point represents one replicate mouse; mean ± SEM; Student’s t test. (J) Flow cytometric analysis of MDP as a percentage of live cells in HF versus LF spleen. LF, n = 5 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. (K) Flow cytometric analysis of Ly6Chi monocytes derived from MDPs (left) or GMPs (right) upon treatment with serum from WT or ob/ob mice, graphed as fold change relative to WT. WT, n = 6 mice; ob/ob, n = 6 mice; mean ± SEM; Student’s t test. (L) Flow cytometric analysis of CD45.1+ monocytes derived from adoptively transferred MDPs in the lungs of CD45.2+ HF versus LF mice, graphed as fold change relative to LF. LF, n = 8 mice; HF, n = 9 mice; mean ± SEM; Student’s t test. (M) Flow cytometric analysis of MHCII+ cells as a percentage of total Ly6Chi monocytes, derived in vitro from GMP cultures treated with recombinant M- or GM-CSF. M-CSF, n = 3 mice; GM-CSF, n = 3 mice; mean ± SEM; Student’s t test. (N) Flow cytometric analysis of MHCII+ cells as a percentage of total Ly6Chi monocytes in the blood following antibiotic (ABX) treatment in HF mice. Control, n = 10 mice; ABX, n = 10 mice; mean ± SEM; Student’s t test. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure S2.
Monocyte phenotypes are regulated by obesity. (A) UMAP contour plot of mass cytometric analyses of CD45+ CD11b+ myeloid cells from CyTOF, depicting Ly6G (top) and Ly6C (bottom) expression across all samples. WT, n = 4 mice; ob/ob, n = 4 mice. (B) UMAP plot from CyTOF highlighting myeloid MC 11. (C) Line graph showing the relative expression (transformed) of all CyTOF makers in MMC11 (pink) compared with other MMC (gray). (D) CyTOF analysis of the proportion of PD-L1+ cells, CD80+ cells, CD86+ cells, or CD40+ cells as a percentage of total Ly6Chi monocytes. WT, n = 4 mice; ob/ob, n = 4 mice; mean ± SEM; Student’s t test; *, P < 0.05. (E) Schematic of monocyte developmental trajectories from GMP or MDP, including proposed hypothesis of obesity-induced hematopoietic skewing of depicted populations (green “+” symbols). Created with BioRender.com. (F) Principal component analysis of RNA-seq on monocytes isolated from blood (left: LF, n = 4 mice; HF, n = 4 mice) or lung (right: LF, n = 3 mice; HF, n = 4 mice).
Given the effect of obesity on monocyte states, we investigated whether obesity shifts the developmental trajectory of monocytes during trafficking. Previous studies have shown that Ly6Chi monocytes are ontogenically diverse and can be derived from either granulocyte–monocyte progenitors (GMPs) or monocyte–DC progenitors (MDPs), whereby GMPs yield neutrophil-like Ly6Chi monocytes (G-mono) while MDPs yield DC-like Ly6Chi monocytes (M-mono; Yanez et al., 2017; Yanez et al., 2015). During inflammatory conditions, neutrophils can selectively expand from GMPs at the expense of G-monos (Kwok et al., 2020). Given that obesity stimulates neutrophil expansion (McDowell et al., 2021; Quail et al., 2017) and promotes pAPC-like monocyte identities, we hypothesized that obesity may enhance monocyte development from MDP-lineages (Fig. S2 E). To address this, we performed RNA sequencing (RNA-seq) on fluorescence-activated cell sorting (FACS)–purified CD45+ CD11b+ Ly6G− Ly6Chi monocytes from the blood and lungs of LF and HF mice (Fig. S2 F). Gene expression analysis revealed that HF monocytes maintained expression of the monocyte and DC transcription factors (TFs) Irf8 and Klf4 as they trafficked from blood to lungs, while LF lung monocytes downregulated these TFs (Fig. 2 F) and instead expressed high levels of the neutrophil TFs Gfi1 and Cepbe (Fig. 2 G). Analysis of lung monocytes revealed 9,764 differentially expressed genes (DEGs; P < 0.05) between HF versus LF conditions; of these, LF lung monocytes exhibited enrichment in neutrophil-like genes (e.g., Mmp9, Csf3r, Cd101) while HF lung monocytes had enriched expression of DC-like genes (e.g., H2-DMa, H2-aa, Ciita; Fig. 2 H), consistent with our observation of upregulated MHCII expression by CyTOF. These data support the possibility that obesity promotes monocytosis along an MDP-derived maturation trajectory.
We next performed flow cytometry on bone marrow (BM), spleen, and blood from LF and HF mice, using an antibody panel to distinguish GMPs, MDPs, G-mono, M-monos, and relevant intermediary precursors (granulocyte progenitors and monocyte progenitors [MP/cMoPs]; Fig. S3, A and B; Yanez et al., 2017; Yanez et al., 2015). Within the BM of HF mice, we observed a decrease in MDPs, MP/cMoPs, and M-monos, coinciding with a concurrent enrichment in mature M-monos in the blood (despite steady levels of G-mono), and a resultant enrichment within lungs (Fig. 2 I and Fig. S3 C). Since the spleen acts as a reservoir for M-mono progenitor cells (Yanez et al., 2017), we profiled the spleen for precursor populations. We observed enrichment for MDPs and MP/cMoPs but not G-mono progenitors, within the spleen of HF versus LF mice (Fig. 2 J and Fig. S3 D). Moreover, splenic Ly6Chi monocytes from HF mice were smaller and less granular than those from LF mice (Fig. S3 E), consistent with an M-mono phenotype (Yanez et al., 2017). Together, these data hinted that LF and HF monocytes may be developmentally distinct, with obesity enriching for those resembling M-mono.
Figure S3.
Obesity promotes an M-mono–like monocyte state. (A) Gating strategy for GMPs, MDPs, G-mono, M-mono, and intermediary precursors. (B) Absolute number of GMP and MDP per leg in WT C57BL6 mice. n = 6 mice per group; mean ± SEM; Student’s t test. (C) Flow cytometric analysis of MP/cMoPs and G-mono of total live cells in HF versus LF BM (n = 5 mice/group) or blood (n = 7–9 mice). Graphs depict mean ± SEM; Student’s t test. (D) Flow cytometric analysis of MP/cMoPs, GMP, granulocyte progenitors (all n = 5/group), and Ly6Chi monocytes (n = 10/group) of total live cells in HF versus LF spleen. Graphs depict mean ± SEM; Student’s t test. (E) Representative flow cytometry histogram plot depicting monocytes from LF and HF spleen. (F) Competitive expansion of congenic CD45.1/CD45.2 GMP and MDP, mixed 1:1, and treated with serum from LF or HF mice for 5 d. Left, mean ± SEM for all samples; right, mean ± SEM for MDP- or GMP-derived monocytes with statistics displayed. (G) Flow cytometric quantification of M-mono following adoptive transfer of CD45.2+ MDP from LF or HF donors into CD45.1+ WT (normal diet) recipients. LF, n = 6 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. (H and I) Flow cytometric quantification of G-mono (H) and MHCII+ G-mono (I) following adoptive transfer of CD45.1+ GMP from WT (normal diet) donors into CD45.2+ LF or HF recipients. LF, n = 3 mice; HF, n = 3 mice; mean ± SEM; Student’s t test. (J) Pie chart of mean relative bacterial abundance at the phylum level, based on 16S rRNA-seq of fecal samples from LF and HF mice. (K) Flow cytometric analysis of Ly6Chi monocytes in HF mice treated with antibiotics (ABX) versus control, graphed as a percentage of total leukocytes in the blood. For both groups, n = 10 mice; mean ± SEM; Student’s t test. (L) Diffusion UMAP of BM-derived CD11b+Ly6C+ cells from LF (top) and HF (bottom) mice. Arrows depict RNA velocity fields based on scRNA-seq data. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001.
To test this hypothesis, we isolated MDPs or GMPs from WT mice and treated them in vitro with serum from lean or obese mice. Serum from obese mice stimulated the expansion of Ly6Chi monocytes from MDPs but not GMPs (Fig. 2 K), supporting the notion that obesity promotes the accumulation of M-mono. As an orthogonal approach, we cocultured congenic CD45.1+ or CD45.2+ MDP and GMP at a 1:1 ratio and treated cultures with serum from lean or obese mice to assess competitive expansion, and found a preference for M-mono enrichment at the expense of G-mono (Fig. S3 F). To confirm these findings in vivo, we used a fate-mapping model to track the maturation and trafficking of MDP in mice. CD45.1+ WT MDPs were adoptively transferred into CD45.2+ LF or HF recipient mice. We found a greater number of CD45.1+ Ly6Chi M-mono in the lungs of HF mice compared with LF mice (Fig. 2 L). This effect was not reversible when MDPs from HF donors were transferred into lean (normal diet) recipients (Fig. S3 G), indicating that obesity educates MDPs to promote their expansion. These data support the role of obesity on MDP-lineage enrichment within the lungs, which could reflect a change in their trafficking, proliferation, or both.
We next tested whether the increase in monocytes was specific to MDP-lineages (that is, M-mono) or if they could be derived from other progenitor populations and mimic M-mono–like features (e.g., MHCII expression). CD45.1+ WT GMPs were adoptively transferred into CD45.2+ LF or HF recipient mice. Surprisingly, although not statistically significant, we found a clear trend toward higher CD45.1+ Ly6Chi G-mono in the lungs of HF mice (Fig. S3 H), including those expressing MHCII (Fig. S3 I). We wondered if G-mono were capable of expressing MHCII in the setting of obesity, a feature more commonly ascribed to M-mono under steady-state conditions (Yanez et al., 2017). GM-CSF has been shown to induce DC-like maturation from M-mono, including MHCII expression (Yanez et al., 2017). Given that GM-CSF is chronically upregulated during obesity (Quail et al., 2017), we tested whether GM-CSF was also sufficient to induce MHCII expression in G-mono after prolonged exposure. When we treated GMPs in vitro with recombinant GM-CSF for 7 d, we found higher MHCII expression on Ly6Chi monocytes compared with M-CSF controls (Fig. 2 M). As an alternative explanation, we explored the possibility that dysbiosis associated with obesity may have immunological consequences on monocyte expansion. As expected, 16S rRNAseq on fecal samples from LF and HF mice revealed major differences in bacterial composition, particularly within the Firmicutes phylum (Fig. S3 J). Importantly, treatment of HF mice with antibiotics was sufficient to reduce the proportion of Ly6Chi monocytes that expressed MHCII (Fig. 2 N), despite an overall increase in the frequency of total Ly6Chi monocytes (Fig. S3 K). Together, these data suggest that obesity supports the expansion of “M-mono–like” cells, and this occurs in part from MDP-lineage expansion, but it is also possible that after prolonged exposure to obesity-related factors, low levels of MHCII can be induced on G-mono to mimic M-mono–like features. Given the complexity of obesity as a systemic condition, this effect is likely to be multifactorial and the data presented here are not conclusive; GM-CSF and the microbiome represent two of many possibilities.
To further explore the origins of M-mono–like cells, we performed single-cell RNA-seq (scRNA-seq) on CD45+ CD11b+ Ly6C+ cells from the BM of HF versus LF mice and performed UMAP dimensionality reduction followed by RNA Velocity analysis (La Manno et al., 2018) to assess cell state transitions. Across LF and HF conditions, we found 13 clusters (CL) of cells, which were assessed on the basis of canonical monocyte markers. The top three genes defining CL3 were Cd74, H2-Aa, and H2-Ab1, with additional genes related to M-mono signatures (Yanez et al., 2017), including Cebpb, Tspan13, and Hpgd. Under LF conditions, CL3 appeared to arise exclusively from CL2 (enriched in DC-like genes, e.g., Irf7, Cx3cr1), whereas, under HF conditions, there were additional contributions from CL1 (enriched in neutrophil-like genes, e.g., Cebpd, Junb; Fig. S3 L). Therefore, these data align with our adoptive transfer experiments, where cell resembling GMP lineages may contribute to putative M-mono–like states in the context of obesity.
Obesity-induced monocytes promote neutrophil maturation via CXCL2
We next explored monocyte identity within the lung microenvironment, given the established link with metastasis (McDowell et al., 2021; Quail et al., 2017). We confirmed that higher frequencies of M-mono–like cells persist within the lungs from obese mice via immunofluorescence co-staining for Ly6C and MHCII (Fig. S4 A), mirroring our analysis in the periphery. Gene set enrichment analysis (GSEA) of RNA-seq data from lung monocytes identified “fatty acid metabolism” as the top enriched gene set in HF versus LF mice (Fig. 3 A), crucial for DC development (Rehman et al., 2013). Similarly, Ingenuity Pathway Analysis (IPA) revealed that “TREM1 signaling” was among the top enriched pathways under obese conditions (Fig. 3 B), concomitant with a significant increase in Trem2 expression (7.7-fold increase; Fig. S4 B). Triggering receptors expressed on myeloid cells (TREMs) are transmembrane receptors that recognize endogenous lipids and have been implicated in lipid uptake in ATME macrophages, which accumulate with weight gain from peripheral inflammatory monocytes (Gong et al., 2020; Jaitin et al., 2019). RNA-seq on circulating monocytes from humans similarly revealed that “TREM1 signaling” was among the top enriched pathways in obese (body mass index [BMI] > 35) compared with lean (BMI = 18.5–25) donors (Fig. S4 C). At the functional level, we confirmed that monocytes derived from obese mice exhibited altered lipid uptake following LPS stimulation ex vivo compared with monocytes derived from lean mice (Fig. 3 C), potentially reflecting differences in innate immune responses. Together these data support the notion that the M-mono–like phenotype is maintained within the lungs of obese hosts and may coincide with a shift in lipid metabolism. We suspect this may stem from the increased availability of free fatty acids resulting from lipolysis during obesity and insulin resistance (Boden, 2008).
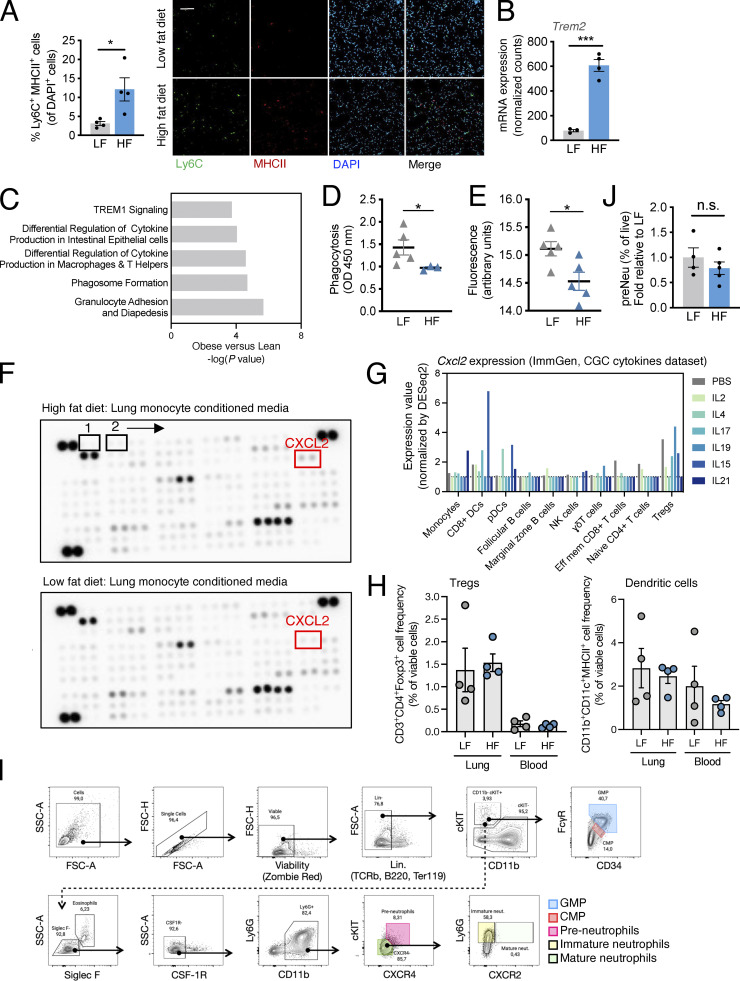
Figure S4.
Obesity is associated with altered monocyte effector functions. (A) Immunofluorescence quantification and representative images of Ly6C+ MHCII+ cells as a percentage of total DAPI+ cells in LF and HF lungs. For both groups, n = 4 mice; mean ± SEM; Student’s t test. Scale bar = 100 μm. (B) Trem2 normalized counts from lung monocyte RNA-seq. LF, n = 3 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (C) RNA-seq IPA of blood monocytes from obese (BMI > 35; n = 10 donors) versus lean (BMI < 25; n = 10 donors) human donors. (D) Phagocytosis of enzyme-labeled E. coli particles by LF and HF lung monocytes. LF, n = 5 mice; HF, n = 3 mice; mean ± SEM; Student’s t test. (E) ROS production by LF and HF lung monocytes. LF, n = 5 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. (F) Cytokine array corresponding to Fig. 3 J and Table S2. (G) Cxcl2 gene expression across splenic immune populations in response cytokines, obtained from the Skyline CGC cytokine database, ImmGen (http://rstats.immgen.org/Skyline_CGC/skyline.html). (H) Flow cytometric analysis of Tregs (left) and DCs (right) in HF and LF lung and blood samples from mice with established metastases. For all groups, n = 4 mice; mean ± SEM. (I) Gating strategy for flow cytometric assessment of neutrophil maturation. (J) Flow cytometric analysis of pre-neutrophils (preNeu) of total live cells in HF versus LF lungs. LF, n = 4 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. *, P < 0.05; ***, P < 0.001.
Figure 3.
Obesity-induced monocytes promote neutrophil maturation. (A) GSEA showing that hallmark fatty acid metabolism is the top enriched pathway from HF versus LF lung monocyte RNA-seq (normalized enrichment score = 1.76; false discovery rate q value = 0.144). (B) RNA-seq IPA of lung monocytes from HF versus LF mice. (C) Palmitate uptake in monocytes from HF or LF mice following LPS or PBS stimulation shown as BODIPY mean fluorescent intensity. For all groups, n = 4 mice; mean ± SEM; one-way ANOVA and Holm-Šídák test for multiple comparisons. (D) RNA-seq gene expression changes between lung monocytes from HF versus LF mice. All displayed changes are at least P < 0.05. LF, n = 3 mice; HF, n = 4 mice. (E) Immunofluorescence analysis of lung CD3+ T cells as a percentage of total DAPI+ cells, following CCR2 inhibition in HF mice. Veh, n = 3 mice; Inh, n = 3 mice; mean ± SEM; Student’s t test. (F) Flow cytometric analysis of liver metastasis, showing Ly6Chi monocyte frequency in HF versus LF mice. LF, n = 4 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (G) Flow cytometric analysis of liver metastasis, showing the proportion of CD4+ T cells that are PD-1+ in HF versus LF mice. LF, n = 4 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (H) Flow cytometric analysis of liver metastasis in HF mice (Ccr2RFP model), showing Ly6Chi monocyte frequency in Δ/Δ versus Δ/+ mice. Δ/+, n = 5 mice; Δ/Δ, n = 5 mice; mean ± SEM; Student’s t test. (I) Flow cytometric analysis of liver metastasis in HF mice (Ccr2RFP model) showing the proportion of CD4+ T cells that are PD-1+ in Δ/Δ versus Δ/+ mice. Δ/+, n = 5 mice; Δ/Δ, n = 5 mice; mean ± SEM; Student’s t test. (J) Cytokine array quantification performed on mCM from HF versus LF mice. Data represent HF values, displayed as fold relative to LF (set to 1). The top upregulated protein, CXCL2, is highlighted in red. (K) Transwell chemotaxis assay of neutrophils (upper chamber) toward lung monocytes from HF or LF mice (lower chamber). LF, n = 4 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (L) Bubble plot of RNA-seq gene expression changes in LF or HF neutrophils, as they move from blood (LF, n = 4; HF, n = 4) to lung (LF, n = 3; HF, n = 4). Bubble color represents the ratio of expression between lung:blood (purple, downregulated; green, upregulated) and bubble size represents P value. (M) Volcano plot showing DEGs from RNA-seq of lung neutrophils isolated from HF versus LF mice. LF, n = 3 mice; HF, n = 4 mice. (N) Cxcr2 normalized counts from lung neutrophil RNA-seq. LF, n = 3 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (O) Flow cytometric analysis of HF versus LF lung, showing mature neutrophil (mNeu) frequency. LF, n = 4 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. (P) Flow cytometric analysis of HF versus LF lung, showing immature neutrophil (ImmNeu) frequency. LF, n = 4 mice; HF, n = 5 mice; mean ± SEM; Student’s t test. *, P < 0.05; **, P < 0.01; ****, P < 0.0001.
Given our finding of altered response to LPS stimulation ex vivo, we next examined additional effector functions in monocytes from lean and obese mice. Through gene expression analysis, we found a significant downregulation of genes related to phagocytosis and ROS biosynthesis in lung monocytes from HF versus LF mice and an upregulation in those related to antioxidants (Fig. 3 D). Supporting these findings, coculture of monocytes with labeled Escherichia coli particles functionally confirmed reduced phagocytosis by HF versus LF lung monocytes (Fig. S4 D). In parallel, we observed impaired in vitro ROS production of HF versus LF lung monocytes via real-time detection of ROS with a fluorescence-based probe (Fig. S4 E). On the other hand, genes related to MHCII were enriched in HF versus LF lung monocytes, with no concurrent enrichment in MHCI-related genes (Fig. 3 D), consistent with the similarities between M-mono and pAPCs (Yanez et al., 2017). Moreover, targeting monocytes via CCR2 in vivo significantly increased T cells within the lungs of HF mice by flow cytometry (Fig. 3 E). A similar effect was observed in a liver metastasis model, where obesity caused an increase in Ly6Chi monocytes and PD1+ CD4+ T cells (Fig. 3, F and G), which was reversed via genetic deletion of Ccr2 (Fig. 3, H and I). Together these data highlight that obesity compromises several monocyte effector functions while promoting the acquisition of pAPC-like features, which can influence CD4+ T cell function after chronic exposure, reminiscent of exhaustion.
We next explored cytokine production by monocytes. We performed a cytokine array targeting 111 soluble proteins in lung monocyte conditioned media (mCM) to identify factors differentially released by monocytes in obese and lean hosts (Fig. S4 F and Table S2). Of all secreted factors, we observed that the CXCR2 ligand, CXCL2 (a murine homolog of CXCL8/IL8 and an important regulator of neutrophil biology and trafficking [Martin et al., 2003]), was the top upregulated protein in mCM from HF versus LF mice (Fig. 3 J). Besides monocytes, DCs and Tregs are also sources of CXCL2; however, we found no significant changes in the frequency of these populations in either the blood or lungs of HF compared with LF mice (Fig. S4, G and H), whereas monocytes displayed both elevated CXCL2 (Fig. 3 J) and elevated cellular frequency (Fig. 1, G–I). Recapitulating these findings, IPA analysis highlighted an enrichment for pathways involved in IL8 signaling and/or granulocyte adhesion and diapedesis in monocytes from obese versus lean mice and humans (Fig. 3 B and Fig. S4 C). Consistently, using an in vitro Transwell assay, monocytes isolated from obese mice stimulated neutrophil chemotaxis more than those from lean mice (Fig. 3 K). These data raise the question of whether lung monocytes regulate neutrophils in the context of obesity through the CXCL2–CXCR2 signaling axis.
Neutrophil maturation coincides with the acquisition of effector function and the expression of CXCR2 (Quail et al., 2022). Therefore, we explored monocyte regulation of neutrophil maturation under obese conditions, where monocyte-derived CXCL2 is high. Mirroring our analysis in monocytes, we first compared gene expression changes by RNA-seq in FACS-purified CD45+ CD11b+ Ly6G+ Ly6Clo neutrophils as they are cleared from the blood into the lungs. TFs typically expressed by mature neutrophils (mNeu), including Cebpd, Spi1/PU.1, and Junb, were enriched as cells trafficked from blood to lung under obese conditions (Fig. 3 L; Evrard et al., 2018; Khoyratty et al., 2021). Consistently, we observed an enrichment in genes related to tertiary granules as neutrophils cleared from the blood into the lung in HF versus LF mice, which are specific to mNeu states (Evrard et al., 2018), along with genes related to phagocytosis and ROS biosynthesis (Fig. 3 L). In contrast, these genes were downregulated during neutrophil clearance in LF animals (Fig. 3 L), potentially reflecting their disarming under steady-state conditions (Adrover et al., 2020). Notably, Cxcr2 was the top upregulated gene that was expressed 2,415-fold higher in neutrophils from HF mice compared with LF mice (P < 1 × 10−300; Fig. 3, M and N), coinciding with an increase in several other canonical maturation markers (e.g., Csf3r, Cd101). To confirm these findings, we performed flow cytometry using antibodies specific for neutrophil developmental states (Fig. S4 I; Evrard et al., 2018). As expected, we observed an increase in CXCR2hi mNeu within lungs of HF mice compared with LF mice (Fig. 3 O), with no significant differences in frequencies of CXCR2lo/− immNeu or preNeu (Fig. 3 P and Fig. S4 J), reflecting the pattern of monocyte CXCL2 production (Fig. 3 J). These data suggest that obesity enriches for mature neutrophil states with elevated effector features.
Monocytes promote NET formation and metastasis under obese conditions
A key feature of neutrophil effector function is the ability to deploy NETs. We have previously shown that NET formation by neutrophils underlies obesity-associated BC metastasis by weakening the vascular barrier in the lung to facilitate metastatic extravasation (McDowell et al., 2021). Moreover, the accumulation of these neutrophils has been mechanistically linked to monocytes (Quail et al., 2017). Thus, we hypothesized that monocytes function to stimulate neutrophil recruitment and NET formation during obesity-associated metastasis through the CXCL2–CXCR2 signaling axis. We first confirmed that in the context of BC extravasation (McDowell et al., 2021), obesity led to an increase in Ly6G− Ly6Chi monocytes, Ly6Chi MHCII+ monocytes, and Ly6G+ Ly6Clo neutrophils within the lungs relative to lean controls (Fig. 4, A–C; and Fig. S5 A), along with a decrease in the frequency of T cells (Fig. S5 B), echoing findings in non-tumor bearing hosts (Fig. 1 I). Moreover, in established metastases, the proportion of mature CXCR2hi neutrophils (but not CXCR2lo/− neutrophils) was significantly enriched in HF lungs compared with LF lungs (Fig. 4 D). Consistently, in the spontaneous MMTV-PyMT model, obesity led to an increase in metastasis, neutrophils, and NET formation within the lungs via histological analysis (Fig. S5 C), aligning with our previous work (McDowell et al., 2021).
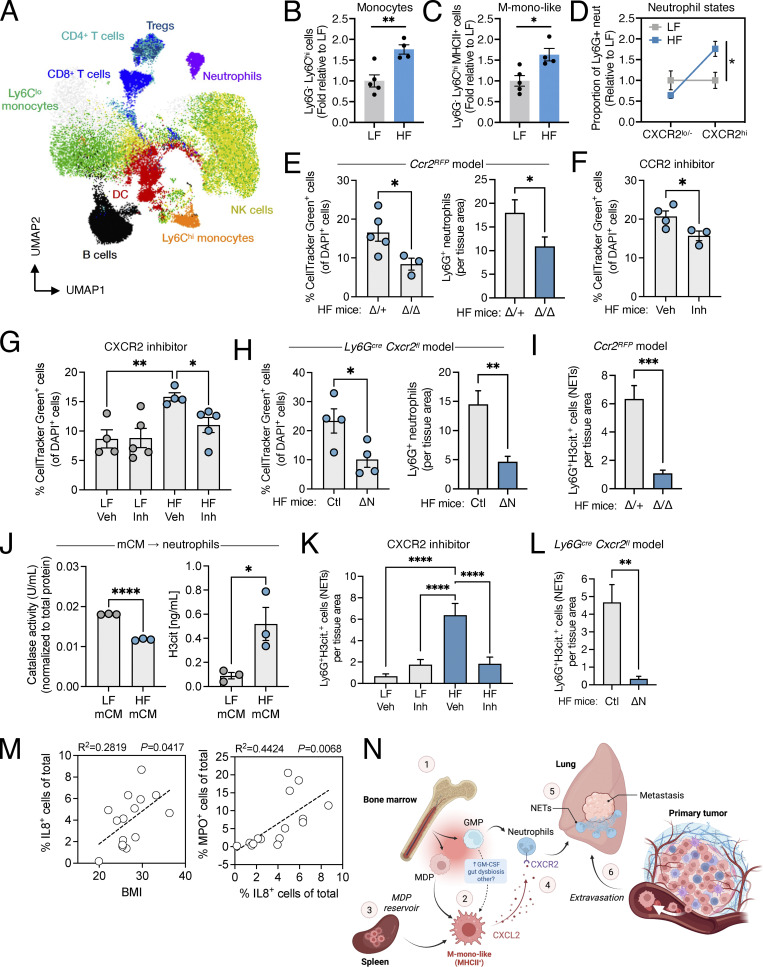
Figure 4.
Monocytes promote NET formation and metastasis under obese conditions. (A) UMAP from spectral flow cytometry of lung immune cells in mice with established metastases (∼7 wk, metastasis-bearing). (B) Flow cytometric analysis of Ly6Chi monocytes in HF versus LF lung samples with early metastasis (48 h extravasation assay). LF, n = 5 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (C) Flow cytometric analysis of Ly6Chi MHCII+ M-mono in HF versus LF lung samples (48 h). LF, n = 5 mice; HF, n = 4 mice; mean ± SEM; Student’s t test. (D) Flow cytometric analysis of CXCR2lo/− or CXCR2hi neutrophils as a proportion of total neutrophils in established lung metastases from HF versus LF mice. LF, n = 4 mice; HF, n = 3 mice; mean ± SEM; Student’s t test. (E) Left: Flow cytometric analysis of extravasated CellTracker+ Py230 BC cells in HF mice (Ccr2RFP model), graphed as a percentage of total DAPI+ cells. Δ/+, n = 5 mice; Δ/Δ, n = 3 mice; mean ± SEM; Student’s t test. Right: Immunofluorescence quantification of Ly6G+ neutrophils normalized to tissue area. For both groups, n = 3 mice with four ROIs/mouse; mean ± SEM; Student’s t test. (F) Flow cytometric analysis of extravasated CellTracker+ Py230 BC cells in lungs of HF mice, treated with a CCR2 inhibitor (Inh) versus vehicle (Veh), graphed as a percentage of total DAPI+ cells. Veh, n = 4 mice; Inh, n = 3 mice; mean ± SEM; Student’s t test. (G) Flow cytometric analysis of extravasated CellTracker+ Py230 BC cells in lungs of LF or HF mice, treated with a CXCR2 inhibitor (Inh) versus vehicle (Veh), graphed as a percentage of total DAPI+ cells. LF/HF Veh, n = 4 mice; LF/HF Inh, n = 5 mice; mean ± SEM; one-way ANOVA and Holm-Šídák test for the indicated comparisons. (H) Left: Flow cytometric analysis of extravasated CellTracker+ Py230 BC cells in HF mice (Ly6Gcre Cxcr2fl model), graphed as a percentage of total DAPI+ cells. Ctl, n = 4 mice; ΔN, n = 4 mice; mean ± SEM; Student’s t test. Right: Immunofluorescence quantification of Ly6G+ neutrophils normalized to tissue area. For both groups, n = 3 mice with four ROIs/mouse; mean ± SEM; Student’s t test. (I) Immunofluorescence quantification of NETosing neutrophils (Ly6G+H3cit+ double positive cells) in HF mice (Ccr2RFP model), normalized to tissue area. For both groups, n = 3 mice with four ROIs/mouse; mean ± SEM; Student’s t test. (J) Left: Neutrophil catalase activity following treatment with (mCM from LF or HF mice. Right: NET formation measured by H3cit ELISA, following treatment with lung mCM from LF or HF mice. For both graphs, LF, n = 3 mice; HF, n = 3 mice; mean ± SEM. Student’s t test. (K) Immunofluorescence quantification of NETosing neutrophils in LF or HF mice, treated with a CXCR2 inhibitor (Inh) versus vehicle (Veh), normalized to tissue area. For all groups, n = 3 mice with four ROIs/mouse; mean ± SEM; one-way ANOVA and Holm-Šídák test for multiple comparisons. (L) Immunofluorescence quantification of NETosing neutrophils in HF mice (Ly6Gcre Cxcr2fl model), normalized to tissue area. For both groups, n = 3 mice with four ROIs/mouse; mean ± SEM; Student’s t test. (M) Pearson’s correlation of IL8+ cells versus BMI (left) or MPO+ cells versus IL8+ cells (right). n = 14 patients with lung metastasis. (N) Working model for the effects of obesity on monocytes. Briefly, obesity promotes M-mono–like monocyte states from MDP (1), with potential contributions from GMP-derived G-mono, which can upregulate MHCII in response to obesity-related systemic factors (2). In parallel, the spleen acts as a reservoir for MDP in obese hosts (3). Obesity-associated M-mono–like cells produce elevated CXCL2, which signals to CXCR2+ mature neutrophils to support their trafficking and effector status (4). The CXCL2–CXCR2 axis underlies NET formation in the lungs (5) in association with enhanced metastasis under obese conditions (6). Created with BioRender.com. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001.
Figure S5.
Monocytes underlie neutrophil states during obesity. (A) Flow cytometric analysis of neutrophils as a percentage of live cells in HF versus LF lung samples with early metastasis (48 h extravasation assay). LF, n = 10 mice; HF, n = 10 mice; mean ± SEM; Student’s t test. (B) Flow cytometric analysis of CD8+ and CD4+ as a percentage of CD45+ cells in WT and ob/ob lung samples with early metastasis (48 h). WT, n = 4 mice; ob/ob, n = 4 mice; mean ± SEM; Student’s t test. (C) Histology analysis in LF and HF lung tissues showing (left) PyMT metastatic lesions per lung area (LF, n = 7 mice and 18 lung sections; HF, n = 9 mice and 31 lung sections; median ± IQR; Mann-Whitney test); (middle) MPO+ neutrophils (LF, n = 5 mice; HF, n = 5 mice; mean ± SEM; Student’s t test); and (right) MPO+H3cit+ NET-forming neutrophils (LF, n = 5 mice; HF, n = 5 mice; median ± IQR; Mann-Whitney test). (D) Representative flow cytometry plots of CCR2 and RFP in blood samples from the Ccr2RFP model. (E) Immunofluorescence quantification of CCR2+ monocytes as a percentage of total DAPI+ cells in lungs from HF mice treated with a CCR2 inhibitor (Inh) or vehicle (Veh). Veh, n = 3 mice; Inh, n = 4 mice; mean ± SEM; Student’s t test. (F) Immunofluorescence quantification and representative images of GFP+ E0771 cells as percentage of total DAPI+ cells in lungs from HF mice treated with a CXCR2 inhibitor (Inh) or vehicle (Veh). Veh, n = 6 mice; Inh, n = 4 mice; mean ± SEM; Student’s t test. Scale bar = 100 μm. (G) Immunofluorescence quantification of lung CD3+ T cells in HF mice (Ly6Gcre Cxcr2fl model), graphed as a percentage of total DAPI+ cells. Ctl, n = 4 mice; ΔN, n = 4 mice; mean ± SEM; Student’s t test. (H) Immunofluorescence quantification and representative images of NETosing neutrophils (MPO+ H3Cit+ double-positive cells) as a percentage of total DAPI+ cells in HF and LF lungs. LF, n = 4 mice; HF, n = 3 mice; mean ± SEM; Student’s t test. Scale bar = 100 μm. (I–K) Representative immunofluorescence images of lung from the Ccr2RFP model (I), CXCR2 inhibition (J) or the Ly6Gcre Cxcr2fl model (K). Scale bars = 10 μm. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
To test the effects of monocyte depletion in obese mice, we employed genetic targeting of Ccr2 (Ccr2RFP model) or a CCR2 inhibitor (RS-504393; Fig. S5, D and E), which resulted in reduced neutrophil accumulation and experimental metastasis compared to monocyte-proficient controls (Fig. 4, E and F). To complement this approach by disrupting putative signaling between monocytes and neutrophils, we targeted CXCR2 using an inhibitor (AZD-5069) or via neutrophil-specific deletion of Cxcr2 (Ly6Gcre Cxcr2flox model, or Cxcr2ΔN). Using two BC cell lines (Py230 or E0771), inhibition of CXCR2 resulted in reduced experimental lung metastasis in obese mice (Fig. 4 G and Fig. S5 F), and this was recapitulated in Cxcr2ΔN mice (Fig. 4 H). As expected, deletion of Cxcr2 in neutrophils also reduced their accumulation in the lungs of obese mice (Fig. 4 H), consistent with the shift in lung metastasis. These data support our hypothesis that the CXCL2–CXCR2 axis of communication between monocytes and neutrophils may underlie obesity-associated BC metastatic progression to lung, although monocyte-specific deletion of Cxcl2 remains to be explored. Of note, targeting CCR2 (Fig. 3 E), but not CXCR2 (Fig. S5 G), was sufficient to increase lung T cell numbers in obese hosts, suggesting that the mechanism by which monocytes regulate T cells is unrelated to their effect on neutrophils.
CXCL2 has been shown to not only mediate neutrophil chemotaxis, but is also sufficient to stimulate NET formation (Alfaro et al., 2016; Nie et al., 2019; Teijeira et al., 2020). Indeed, we have previously shown that neutrophil oxidative burst and NETs underlie obesity-associated BC metastasis to lung (McDowell et al., 2021), and we similarly confirmed here an elevation in NETs in the lungs of obese mice compared with lean mice via immunofluorescent co-staining for MPO and H3cit (Fig. S5 H); however, it is unknown how NETs are stimulated in this context. Therefore, we questioned whether monocytes acted upstream of NET formation given their propensity to release CXCL2 in obese hosts. First, we confirmed that monocyte depletion via genetic targeting of Ccr2 was sufficient to reduce MPO+ H3cit+ cells in the lungs of obese mice (Fig. 4 I and Fig. S5 I). To determine if this effect was mediated by soluble factors supplied by the monocytes, we treated neutrophils in vitro with mCM from HF versus LF mice and confirmed a significant reduction in catalase activity and an increase in H3cit (Fig. 4 J; McDowell et al., 2021; Metzler et al., 2011). To test whether these observations could be phenocopied by targeting the CXCR2 signaling axis, we quantified NETs in lung tissues from lean and obese mice treated with AZD-5069 and confirmed a significant reduction in MPO+ H3cit+ cells with CXCR2 blockade (Fig. 4 K and Fig. S5 J). This effect was specific to obesity, as there was no effect of CXCR2 inhibition on NET formation in lean mice, where CXCL2 levels are lower in this model (Fig. 4 K). Similarly, NETs were reduced in the lungs from HF Cxcr2ΔN mice compared with HF controls (Fig. 4 L and Fig. S5 K). Finally, immunofluorescence staining of lung metastases from patients revealed a positive correlation between IL8+ cells and BMI, and between IL8+ cells and MPO+ cells (Fig. 4 M), consistent with our previous finding that BMI correlates with NETs and chlorotyrosine levels in these same patient samples (McDowell et al., 2021). These data underscore the important role of monocytes in pathologic neutrophil activation during obesity to promote BC metastasis.
Discussion
Here, we have shown that obesity biases immune populations toward myeloid lineages to enhance metastatic progression (Fig. 4 N). Using a combination of CyTOF and RNA-seq to characterize the diversity of myeloid developmental and functional identities, we discovered that obesity promotes mNeu expansion and enrichment of M-mono–like cells, leading to a global shift in myeloid states during trafficking. Mechanistically, we found that M-mono–like cells underlie obesity-associated neutrophil activation and NET formation, which is regulated by monocyte CXCL2 production and neutrophil expression of CXCR2. Importantly, targeting monocytes or the CXCL2–CXCR2 signaling axis is sufficient to rescue obesity-mediated BC metastasis. These findings have implications for myeloid-targeted immunotherapy development for obese cancer patients (and for those who are metabolically obese with a normal body weight) and shed light on epidemiological studies linking obesity with accelerated BC mortality.
Previous work outside of the cancer setting has shown that myelopoiesis and monocytosis are enhanced in preclinical mouse models of obesity to give rise to greater frequencies of Ly6G+ neutrophils and Ly6Chi inflammatory monocytes (Nagareddy et al., 2014). Similar observations have been made in humans, where obesity is associated with higher frequencies of proinflammatory classical monocytes in blood (Friedrich et al., 2019). It has been proposed that this systemic expansion results from chronically inflamed white adipose tissue, which signals to the BM to promote maturation and recruitment of monocytic lineages (Jaitin et al., 2019; Nagareddy et al., 2014). However, a remaining knowledge gap is the relative contribution of GMP versus MDP developmental trajectories to the total monocyte pool during obesity (Geissmann et al., 2003; Yanez et al., 2017) and how this influences their functional role within the metastatic niche. Here, we have discovered that obesity enriches for MDPs and M-mono–like monocyte states, arising both from an increase in MDP-derived lineages and from GMP-lineages that adopt M-mono–like features like MHCII. Given the systemic complexity of obesity in multiple organ systems, we suspect that the induction of MHCII on monocytes is likely to be multifactorial. Here, we propose two of many possibilities, including GM-CSF enrichment and/or gut dysbiosis; however, the data presented are not conclusive, and future functional experiments are needed to confirm a regulatory role. Of particular interest was our finding that obesity primes MDPs to sustain enhanced differentiation and trafficking, even after transfer into lean hosts. Although not formally tested, this raises the possibility that obesity may “train” the monocyte progenitor pool to have long-lasting consequences on innate immune responses, as has been shown following exposure to a Western diet in preclinical models (Christ et al., 2018).
We observed that myeloid enrichment in response to obesity occurred at the expense of lymphoid populations. Thus, obesity may be associated with a shift in HSC fate during hematopoiesis. Supporting this notion, previous work has shown that high adiposity shifts hematopoietic production from lymphoid to myeloid populations in preclinical mouse models of obesity to reduce B cells in BM and blood (Chan et al., 2012). Similar reports have been observed in humans whereby adipose tissue–derived adiponectin impairs B cell development (Yokota et al., 2003). During obesity, ectopic adipocytes also accumulate in the BM (Bredella et al., 2011), which perturbs the hematopoietic stem cell niche. Indeed, the accumulation of BM adipocytes has been shown to impair hematopoietic function (Ambrosi et al., 2017) and counter hematopoietic restoration after chemotherapy (Zhu et al., 2013). However, it is unclear how obesity regulates the developmental states of these skewed hematopoietic populations and the functional consequences that occur as a result. Our findings highlight diversity in lymphoid subsets within the peripheral circulation; notably, CD4+ T cells are both reduced in number and exhibit features reminiscent of exhaustion. It is conceivable that this shift in the balance between myeloid:lymphoid populations may underlie immunological dysfunction associated with obesity beyond cancer, for example, a heightened susceptibility to infections (Falagas and Kompoti, 2006; Mertz et al., 2013; Sudhakar et al., 2022).
We observed that monocytes are an important source of neutrophil chemokines during obesity, including CXCR2 ligands. CXCR2 is a critical regulator of neutrophil maturation and effector function (Adrover et al., 2019; Evrard et al., 2018), and we consistently see that obesity enhances mNeu expansion and NET formation within lungs. These findings align with our previous observations that NETs underlie obesity-associated BC metastasis (McDowell et al., 2021) and suggest that CXCR2 signaling may be the cause. Corroborating these observations, preclinical mouse models have shown that CXCR2 signaling in neutrophils promotes metastatic progression, which can be reduced by targeting the CXCR2 axis (Nie et al., 2019; Steele et al., 2016). Our findings extend these observations in the context of obesity and demonstrate the involvement of additional cell types within the microenvironment (monocytes) that supply CXCR2 ligands to mediate NETs and metastasis. Other studies have shown that tumor cells are major producers of CXCR2 ligands, and in turn, CXCR2-induced NETs can shield tumor cells from T cell–mediated cytotoxicity (Teijeira et al., 2020). Consistently, targeting CXCR2 signaling can improve T cell function and immunotherapy efficacy in standard (lean) mouse models of cancer (Steele et al., 2016; Sun et al., 2019). However, in obesity models, we found that targeting CXCR2 had no effect on T cell numbers while targeting CCR2 did. Although the exact mechanisms governing myeloid–T cell communication in our model are not fully resolved, our findings suggest that monocytes may play a role independent of their effect on the CXCR2 signaling axis.
Although epidemiological studies have highlighted a strong link between obesity and cancer progression, mechanisms underlying these clinical observations are incomplete. This study provides mechanistic insight into how obesity enhances the metastatic process through monocyte-secreted factors that regulate pathologic, chronic neutrophil activation. Given that neutrophil depletion is not safe for cancer patients due to the risk of sepsis, our study highlights new putative myeloid-targeted immunotherapeutic approaches that can potentially be leveraged in obese patients that display myeloid aberrancies. As obesity is increasing worldwide, our study provides translational insights for a rapidly expanding population of cancer patients.
Materials and methods
Cell lines, pharmacological, and biological reagents
Py230 cells were purchased from ATCC and maintained in Ham’s F-12K (Kaighn’s basal medium) supplemented with 5% FBS, 1% penicillin and streptomycin (P/S), and 0.1% MITO+ growth factor. E0771 cells were purchased from CH3 BioSystems, engineered to express pHIV-Luc-ZsGreen (Addgene), and maintained in RPMI supplemented with 10% FBS and 1% P/S. MC38 cells were purchased from Kerafast and maintained in DMEM supplemented with 10% FBS, 1% P/S, and non-essential amino acids (Gibco). Targeting of CXCR2 in vivo was performed using the drug AZD-5069 (SelleckChem) at a dose of 100 mg kg−1 body weight, administered by oral gavage twice daily beginning 1 wk before tumor cell injections, and continued until trial endpoint (vehicle, 5 mg/ml hydroxypropylmethyl cellulose + 0.1% Tween 80 in PBS; Norman, 2013). Targeting CCR2 in vivo was performed using the drug RS-504393 (MedChemExpress) at a dose of 2 mg kg−1 body weight, administered by oral gavage once daily beginning 1 wk before tumor cell injections, and continued until trial endpoint (vehicle, 90% corn oil + 10% saline vol/vol).
Animal models
Mice were maintained in specific pathogen–free conditions. Animal protocols were reviewed and given approval by McGill University Animal Care Committee. All animal protocols conformed to standards by the Canadian Council on Animal Care.
DIO model
As previously described (Quail et al., 2017), 5-wk-old female C57BL6 mice (Jackson Laboratory) were enrolled on HF (60% fat, 20% protein, and 20% carbohydrate; Research Diets D12492I) or LF (0% fat, 20% protein, and 70% carbohydrate; Research Diets D12450BI) irradiated isocaloric diet for 15 wk beginning at 5 wk of age. DIO mice were used when they were at 20 wk of age (average weight, 41.1 versus 21.6 g in LF controls).
GIO model
As previously described (Quail et al., 2017), female C57BL6 WT or ob/ob age-matched mice (Jackson Laboratory) were maintained on a standard rodent chow diet. Ob/ob mice quickly gain weight from hyperphagia because of a deficiency in leptin. GIO mice were used when they were at 10 wk of age (average weight, 46.6 versus 18.9 g in WT controls).
Genetic targeting of Ccr2
Ccr2RFP knock-in mice were a kind gift from Dr. Judith Mandl (McGill University, Canada). In homozygous mice, the sequence for RFP replaces the coding sequence of the Ccr2 gene, which removes gene function (Saederup et al., 2010). In this model, RFP is largely expressed in inflammatory monocytes, with some expression in T cells and natural killer cells. Heterozygous mice were used as a control.
Neutrophil-specific deletion of Cxcr2
Ly6g-cre mice were a kind gift from Dr. Matthias Gunzer (University Hospital Essen, Germany) based on prior published work (Hasenberg et al., 2015). The Ly6g locus was engineered to express cre-recombinase, allowing for neutrophil-specific gene targeting. Ly6g-cre mice were crossed to Cxcr2-flox mice to target Cxcr2 in mature neutrophils (Cxcr2ΔN). Cxcr2fl/fl mice crossed with WT Ly6g were used as a control.
Spontaneous MMTV-PyMT model
MMTV-PyMT mice in a C57BL6 background were purchased from the Jackson Laboratory. Tumor latency is longer in the C57BL6 background compared to the more common FVB/n background, allowing for sufficient time for weight gain in response to experimental diets (Davie et al., 2007). Mice were euthanized when they reached 20 wk of age (or when symptomatic).
Serum isolation from mice
Submandibular bleeds were performed using a Goldenrod lancet directly into Eppendorf tubes. Blood was allowed to clot at room temperature (RT) for 20 min and then samples were centrifuged at 2,000 rpm, at 4°C for 20 min. The resulting supernatant was transferred to a clean polypropylene tube.
In vivo experimental metastasis assays
Experimental lung metastasis assays were performed as previously optimized (McDowell et al., 2021). For analysis of extravasation into the lungs (48 h after injection), Py230 or E0771 BC cells were labeled with green fluorescent CellTracker (Vybrant CFDA SE Cell Tracer Kit, Invitrogen; 1:1,500 dilution in 1× PBS) and 1 × 106 BC cells were injected into the tail vein. For analysis of established lung metastases, 1 × 106 unlabeled Py230 BC cells diluted in 1× PBS were injected into the tail vein. Mice were individually euthanized upon the development of symptoms resulting from overt lung metastasis (e.g., labored breathing), which was confirmed by MRI. For analysis of established liver metastases (2–3 wk after injection), 5 × 105 unlabeled MC38 colorectal cancer cells diluted in 1× PBS were injected intrasplenically. At endpoint, lung or liver tissues were fixed in 4% paraformaldehyde (PFA) at 4°C for 24 h and then moved to 30% sucrose at 4°C for at least 24 h. Note that lungs were perfused through the trachea with 4% PFA (Santa Cruz) prior to collection. Tissues were embedded and frozen in Optimal Cut Temperature compound (Tissue-Tek, Sakura) and cryosectioned for immunostaining and fluorescence analysis. Fluorescence was visualized using an Axio Scan.Z1 (Zeiss), and HALO Image Analysis Software (Perkin Elmer) was used for quantification.
Human tissue microarray (TMA)
The McGill University Health Centre Research Ethics Board, no. 2009–5354 approved the protocol for human sample biobanking. Human samples were collected with patients giving their informed consent. P.O. Fiset (pathologist) and J.D. Spicer (thoracic surgeon) provided formalin-fixed paraffin-embedded lung metastasis samples. Cores within tumor centers were selected by K.D. Lach and M.S.M. Issac (pathology) to make the human TMA. Patients’ BMI ranged from 19.9 to 36.3. Immunofluorescent staining on human TMA and subsequent analysis were performed as described below.
Immunofluorescent staining of tissues
As previously described (McDowell et al., 2021), 10-μm sections were left to thaw and dehydrate at RT. Sections were rehydrated in 1× PBS and subsequently blocked with Dako blocking reagent (Agilent) for 1 h at RT. Dako antibody diluent was used to dilute primary antibodies (Table S1). Antibodies were incubated in Dako antibody diluent overnight at 4°C. The next day, tissues were washed in 1× PBS three times and then incubated with AlexaFluor secondary antibodies (1:500; Invitrogen) for 1 h at RT and washed in 1× PBS three times. The counterstain used was DAPI. For quantification and analysis, an Axio Scan.Z1 (Zeiss) and HALO (Perkin Elmer) were used.
Flow cytometry
Lungs and spleen were isolated from animals, mechanically dissociated, and filtered using a 40-μm mesh. BM (femurs and tibiae) was isolated, flushed with 1× PBS, and filtered using a 40-μm mesh. Blood was isolated via submandibular bleeding as described above. All tissues were lysed with 1× RBC lysis buffer (BD Biosciences) as per the manufacturer’s instructions. Cells were rinsed with 1× FACS buffer and incubated with antibodies for 1 h (Table S1). A BD LSRFortessa or Cytek Aurora was used for performing flow cytometry, and OneComp eBeads (eBioscience) were used for compensation controls. Dead cells and debris were excluded from analyses using forward scatter and side scatter, and live/dead stain (Invitrogen) or DAPI. All gating strategies are provided in the supplementary figures. FlowJo v.10.7.1 was used for analysis. FlowJo plugins UMAP, Phenograph, and Cluster Explorer were used for analysis. Graphs are displayed as a percentage of total cells or as indicated. For BM analysis of progenitor populations, absolute numbers of cells per leg are also provided in Fig. S3 B as a reference.
Isolation of primary neutrophils and monocytes and preparation of conditioned media
Primary neutrophils or monocytes were isolated under sterile conditions and filtered using a 40-μm mesh. Primary neutrophils were isolated using a Neutrophil Isolation Kit (Millipore), an OctoMACs Separator column (Millipore), and MS columns (Millipore). Primary monocytes were isolated using a Monocyte Isolation Kit (Millipore), an OctoMACs Separator column (Millipore), and LS columns (Millipore). Neutrophils or monocytes were seeded into low-attachment plates in serum-free DMEM media with 1% P/S at 50,000 cells per mm2 at 37°C and 5% CO2 and used for downstream assays (e.g., conditioned medium was collected over a period of 20 h).
In vitro functional assays
Functional assays were performed on primary FACS-purified monocytes from the lungs of LF or HF mice. Phagocytosis was quantified using a Phagocytosis assay kit (Cell Bio Labs). ROS biosynthesis was quantified using a ROS-ID detection kit (Enzo Life Sciences). Catalase activity was quantified using a Catalase Colorimetric Activity Kit (Arbor Assays). NET formation was quantified using a citrullinated histone-H3 (H3cit, clone 11D3) ELISA (Cayman Chemical). Transwell chemotaxis assays were performed as previously described (McDowell et al., 2021) with lean or obese lung monocytes in the lower chamber and neutrophils from WT in the upper chamber.
Ex vivo stimulation of T cells
Peripheral blood was collected from LF and HF mice. RBCs were lysed using BD Pharm Lyse lysing solution for 2 × 15 min at RT. Cells were stimulated for 3 h at 37°C in 25 ng/ml PMA (Stemcell Technologies), 1 μg/ml ionomycin (Stemcell Technologies), and brefeldin A (BioLegend), or in brefeldin A alone as an unstimulated control, before undergoing antibody staining for flow cytometry (Table S1).
Lipid uptake assay
Cells were isolated from the BM of LF or HF mice and duplicates were pooled. Monocytes were isolated using the EasySep Monocyte Isolation kit (Stemcell Technologies). Monocyte purity and viability were assessed via flow cytometry using an anti-CD11b antibody (Table S1) and a fixable viability dye (eFluor 780; eBioscience). Cells were seeded into a 96-well plate in duplicate and treated with 100 ng/ml of LPS (Salmonella minnesota; InvivoGen) for 6 h at 37°C, 5% CO2. Cells were resuspended in 100 μl of serum-free RPMI containing glucose, L-glutamine, and 1 μM BODIPY FL C16-Palmitate (Invitrogen) and incubated for 1 h at 37°C, 5% CO2. Cells were then stained with 7-AAD viability dye, and BODIPY dye uptake was visualized using flow cytometry.
Adoptive transfer of BM progenitors
Adoptive transfer of GMPs or MDPs was performed as previously described (Yanez et al., 2017; Yanez and Goodridge, 2018). Briefly, mouse BM progenitors were isolated from femurs and tibias by a combination of magnetic and fluorescence sorting. Lin− cells were obtained using a MACS lineage cell depletion kit (containing antibodies against CD5, CD11b, Gr-1, 7-4, and Ter-119) and an OctoMACS Separator column (Miltenyi). Lin− cells were stained with the appropriate antibody cocktail (Table S1) and progenitor populations (GMPs or MDPs) were isolated with a FACS Aria III cell sorter (BD Biosciences) according to the gating strategy in Fig. S3 A. WT CD45.1+ GMPs or MDPs were adoptively transferred (25,000–50,000 cells/mouse in 100 ml PBS) into LF or HF CD45.2+ recipient mice via tail vein (day 0). Alternatively, WT CD45.2+ LF or HF MDPs were adoptively transferred into CD45.1+ recipients on a normal diet. In both cases, mice were sacrificed after 3 d; blood, lungs, and spleens were harvested, and single-cell suspensions were prepared. RBCs were lysed with ammonium chloride (BD Bioscience Pharm Lyse), and CD45.1+ immune cells were analyzed by flow cytometry as described above (BD LSRFortessa).
Mouse XL cytokine array
Monocyte CM was isolated from LF or HF mice as described above, and 111 soluble proteins were quantified via a Mouse XL Cytokine Array Kit (R&D Systems). See Table S2 for a complete list of targets. To visualize proteins, a Chemi Reagent Mix (R&D Systems) and an Amersham Imager 600 (GE Healthcare Life Sciences) were used. Densiometric analyses were performed using Amersham Imager 600 Analysis Software.
Bulk RNA-seq and analysis
FACS of mouse samples
Mice were anesthetized with avertin. Blood was first collected and then cardiac perfusion with PBS was performed prior to the collection of lung tissue in order to flush blood leukocytes from tissues. The following procedures were used to prepare blood and lung samples for FACS.
Blood processing (mouse)
Fresh whole-blood samples were collected from mice into EDTA-coated tubes by submandibular bleeding. RBCs were lysed directly (Pharm Lyse, BD Biosciences), cells were counted, incubated with mouse Fc block (1 h; BD Biosciences; 1:100/106 cells), incubated with conjugated antibodies (1 h), and stained with DAPI for dead cell exclusion (10 min). Mouse antibodies and dilutions were used as follows: CD45-APC (30-F11, 1:100; BD Pharmingen), CD11b-PE-Cy7 (M1/70, 1:1,000; BioLegend), Ly6C-APC-Cy7 (HK1.4, 1:500; BioLegend), and Ly6G-PE (1A8, 1:200; BD Pharmingen). Cell surface markers included DAPI− CD45+ CD11b+ Ly6Chi Ly6G− to define monocytes and DAPI− CD45+ CD11b+ Ly6G+ Ly6Clo to define neutrophils. In some cases, OneComp eBeads (eBioscience) were used for compensation.
Lung processing (mouse)
Lung tissues were mechanically dissociated and filtered through a 40-μm mesh to generate a single cell suspension, and RBCs were lysed (Pharm Lyse; BD Biosciences). Cells were counted, incubated with mouse Fc block (1 h; BD Biosciences; 1:100/106 cells), incubated with conjugated antibodies (1 h), and then stained with DAPI for dead cell exclusion (10 min). Mouse antibodies and dilutions were used as follows: CD45-APC (30-F11, 1:100; BD Pharmingen), CD11b-PE-Cy7 (M1/70, 1:1,000; BioLegend), Ly6C-APC-Cy7 (HK1.4, 1:500; BioLegend), and Ly6G-PE (1A8, 1:200; BD Pharmingen). Cell surface markers included DAPI− CD45+ CD11b+ Ly6Chi Ly6G− to define monocytes and DAPI− CD45+ CD11b+ Ly6G+ Ly6Clo to define neutrophils. For all antibodies, OneComp eBeads (eBioscience) were used for compensation. Note that lung neutrophil RNA-seq data were obtained from our previous work (McDowell et al., 2021).
FACS of human blood samples
The Rockefeller University Institutional Review Board approved the protocol JWA-921 for human blood collection from healthy lean (BMI = 18.5–25; average = 21.4) and obese (BMI >3 5; average = 39.6) postmenopausal women (n = 9 per group) matched by age (average = 60 yr). All donors gave their informed consent. At least 15 ml of blood was collected into heparin-coated tubes. 5 ml of blood was centrifuged at 8,000 rpm for 10 min to collect the upper layer (plasma), which was frozen and stored at −80°C. The remaining blood was subjected to direct RBC lysis (Pharm Lyse; BD Biosciences), rinsed with FACS buffer (2% BSA in PBS), and repeated until the sample was clear. Following isolation, cells were counted, incubated with human Fc block (30 min; BD Biosciences; 1:100/106 cells), incubated with conjugated antibodies (30 min), and then stained with DAPI for dead cell exclusion (10 min). Human antibodies and dilutions were used as follows: CD45-BV605 (HI-30, 1:100; BioLegend), CD11b-BUV395 (M1/70, 1:500; BD Horizon), CD66b-PE-Cy7 (G10F5, 1:100; BioLegend), CD16-A700 (3G8, 1:500; BioLegend), and CD14-A488 (HCD14, 1:100; BioLegend). OneComp eBeads (eBioscience) were used for compensation. Cell surface markers were used to sort different cell populations for sequencing; classical monocytes were defined as CD45+ CD11b+ CD66b− CD16− CD14+.
Bulk RNA-seq
RNA-seq was performed on FACS-purified mouse monocytes (DAPI− CD45+ CD11b+ Ly6Chi Ly6G−) and neutrophils (DAPI− CD45+ CD11b+ Ly6G+ Ly6Clo) from DIO and GIO models, and on FACS-purified human circulating classical monocytes (CD45+ CD11b+ CD66b− CD16− CD14+) from lean and obese donors (as described above). As done previously (McDowell et al., 2021), GENEWIZ performed RNA isolation, RNA-seq, and quality control, and bioinformatics was done in-house. Briefly, TRIzol LS (Invitrogen) was used for RNA isolation, and integrity was assessed via Agilent Bioanalyzer 2100. A SMART-Seq library preparation kit was utilized and 2 × 100 base-pair sequencing was performed on an Illumina HISeq 2000.
QC and extraction of DEGs (mouse)
To collect quality control metrics of the raw reads, Fastp (v.0.20.0) was utilized. RNA sequences were aligned and sorted by coordinates to the National Center for Biotechnology Information (NCBI) mouse genome build 38 (GRCh38.p12) v.96 of gene annotations using the STAR aligner (STAR_2.6.1b). The removal of alignment duplicates was performed via Sambamba (v.0.7.0). To quantify genes, featureCounts (v.2.0.0) was used. DESeq2 (v.1.24.0) was utilized to normalize gene counts and to find DEGs. HGNC symbols were extracted and added to DESeq2 results data frame via biomaRt (v.2.40.0) using the “mmusculus_gene_ensembl” dataset and the Ensembl Release 96 (April 2019).
QC and extraction of DEGs (human)
To collect quality control metrics of the raw reads, Fastp (v.0.19.4) was utilized. RNA sequences were aligned and sorted by coordinates to the NCBI human genome build 38 (GRCh38.p12) version 94 of gene annotations using the STAR aligner (STAR_2.6.1b). The removal of alignment duplicates was performed via Sambamba (v.0.6.8). To quantify genes, featureCounts (v.1.6.3) was used. DESeq2 (v.1.20.0) was utilized to normalize gene counts and to find DEGs. HGNC symbols were extracted and added to DESeq2 results data frame via biomaRt (v.2.38.0) using the “hsapiens_gene_ensembl” dataset, and the “Ensembl Release 94 (October 2018)” mart.
Pathway analysis
For mouse pathway analysis, IPA software v.01-13 (Qiagen) was used for pathway enrichment assessment in murine lung monocytes. The top 1,000 DEGs (P < 0.000001 ± threefold change) were selected and “Core Analysis” was selected with all default parameters. RNA-seq normalized read counts were converted to .gmt format and analyzed via GSEA software v.4.1.0 (Broad Institute). All analyses were performed using default settings. Gene set database, “h.all. v6.2.symbols.gmt”. Chip platform, “Mouse Gene Symbol Remapping Human Orthologs MSigDB.v7.2.chip.” All analyses were performed in RStudio v.3.6.1. For human pathway analysis, IPA software v.01-13 (Qiagen) was also used. The top 792 DEGs (P < 0.05 ± 0.5 fold change) were selected and “Core Analysis” was used with all default parameters.
scRNA-seq
CD45+CD11b+Ly6G−Ly6Chi monocytes were isolated from BM of LF or HF mice via FACS and diluted to a concentration of 1,000 cells/μl in PBS + 0.2% BSA. scRNA-seq libraries were generated according to the Chromium Next GEM Single Cell 5′ kit (10x Genomics) instructions. The generated single-cell libraires were submitted to McGill Genome for sequencing on a NovaSeq6000 S4 v1.5, PE100 (Illumina) flow cell at >250 million reads per sample. Raw feature counts from Cell Ranger were aggregated using Seurat (v.4.3.0) in R (v.4.1.0). UMAPs were generated using Seurat (v.4.3.0). Immune clusters were identified using SingleR (v.1.6.1). All cells not identified as monocytes were removed. RNA velocity was conducted using scVelo (v.0.2.5) in Python (v.3.10.2).
16S rRNA-seq and antibiotic experiments
Fecal pellets were collected from LF or HF mice, DNA was extracted, and 16S rRNA-seq was performed through the McGill Genome Centre. The MicrobiomeAnalyst tool was used as previously described (Chong et al., 2020). Data integrity analysis was performed in which amplicon sequence variants with zero values across all samples and those that appeared in only one sample were excluded. Data were normalized by rarefraction (Weiss et al., 2017) prior to bacterial abundance profiling. To assess the role of the microbiome on the regulation of monocytes, mice were enrolled on an HF diet at 5 wk of age and treated with antibiotics after 13 wk. Antibiotics were administered via drinking water (1 mg/ml ampicillin, 5 mg/ml streptomycin, and 1 mg/ml colistin) and replenished every 3 d. After 1 wk, flow cytometry was performed on blood collected via submandibular puncture.
Mass cytometry (CyTOF) experiments and analysis
Sample preparation
Blood from 10-wk-old female WT and ob/ob GIO mice was collected by submandibular bleeding as described above. Blood was treated with 1× RBC lysis buffer (BD Biosciences) for 15 min at RT and then quenched with 1× HBSS. Samples were centrifuged at 300 g for 5 min at RT and then resuspended in 10 ml of 35% Percoll and spun at 360 g for 15 min at 20°C to enrich for leukocytes. The supernatant was removed, and cells were resuspended in 1× PBS and counted.
Sample staining with antibodies
1 × 106 cells were centrifuged to remove PBS and resuspended in 100 μl of cisplatin to stain for viability for 5 min at RT. The reaction was quenched with Maxpar cell staining buffer and the cells were resuspended in 100 μl of Fc block solution for 10 min at RT. Samples were centrifuged and 50 μl of blocking buffer was removed. 50 μl of metal isotope–labeled antibody cocktail was then added to samples (Fig. S1 B). Samples were gently mixed and incubated for 15 min at RT. Samples were gently vortexed and then incubated for an additional 15 min at RT. Following incubation, cells were washed with 2 ml Maxpar Cell Staining Buffer and centrifuged at 300 ×g for 5 min and supernatant was aspirated. This was repeated two more times. Samples were vortexed to thoroughly disrupt the pellet and 200 μl of nuclear antigen staining buffer working solution was added to each tube, followed by a gentle vortex. Samples were incubated for 30 min at RT. Cells were washed with 2 ml of Nuclear Antigen Staining Perm (1×) and centrifuged at 600–800 ×g, and the supernatant was discarded. This wash step was repeated for a total of two washes. Cells were resuspended in 100 μl of FOXP3 antibody solution, gently vortexed, and incubated for 30 min at RT. Cells were washed 2× with 2 ml Maxpar cell staining buffer and then vortexed to disrupt the cell pellet.
Fixation
Fresh 1.6% PFA solution from 16% formaldehyde stock ampule was prepared. One part of stock formaldehyde was diluted with nine parts Maxpar PBS. 1 ml of the 1.6% PFA solution was added to each tube and gently vortexed to mix well. Tubes were incubated for 10 min at RT. Cells were centrifuged at 800 ×g for 5 min. Samples were carefully aspirated to remove supernatant.
Sample staining with intercalator
1 ml of intercalation solution was prepared for each sample by adding Cell-ID Intercalator-Ir into Maxpar Fix and Perm Buffer for a final concentration of 125 nM. 1 ml of the cell intercalation solution was added to each tube, gently vortexed, and incubated for 1 h at RT.
Sample preparation for acquisition
Samples were centrifuged in intercalation solution at 800 ×g for 5 min, then washed with 2 ml of Maxpar Cell Staining Buffer, centrifuged at 800 ×g for 5 min, and the supernatant was removed. Cells were resuspended in 1 ml of Maxpar Cell Acquisition Solution. Cells were counted and then samples were centrifuged at 800 ×g for 5 min and acquired with the Helios CyTOF mass cytometer (Fluidigm).
CyTOF analysis
All .fcs files were analyzed with v.10.8.0 FlowJo (Flowjo, LLC) using a standard clean-up protocol on all WT and ob/ob samples (n = 4 mice per group), as previously described (Olsen et al., 2019). Samples were downsampled, concatenated, and analyzed with the Phenograph plugin using standard settings. Manual gating was also performed on all CD45+ cells to define major immune lineages according to canonical cell surface markers (Fig. S1 B). The Cluster Explorer plugin was used to generate signal-intensity heatmaps and 3D colorized UMAPs.
Statistics and reproducibility
GraphPad Prism Pro v.8 was used for data analysis and all data are presented as mean ± SEM unless indicated otherwise. P < 0.05 was considered statistically significant for all analyses. For quantitative data, the statistical test utilized is indicated in figure legends. First, normal distribution was examined via the Shapiro–Wilk normality test. Parametric data were analyzed via unpaired Student’s t test (two groups) or ordinary one-way analysis of variance (ANOVA; >2 groups), and Holm-Šídák’s multiple comparisons test for select pairwise comparisons, as indicated in figure legends. Data determined to be nonparametric were analyzed via Mann–Whitney test (two groups) or Kruskal–Wallis test (>2 groups), and Dunn’s multiple comparisons for select pairwise comparisons as indicated. All tests performed were two-tailed. Pearson’s correlation was utilized for patient TMA analysis.
Online supplemental material
Fig. S1 shows unsupervised CyTOF analyses of T lymphocyte MCs in the blood in the ob/ob obesity model. This figure also presents CyTOF and flow cytometry gating strategies for cell-type identification. Fig. S2 shows CyTOF immunophenotyping of blood monocytes in the ob/ob model, as well as a principal component analysis of RNA-seq performed on blood and lung monocytes in LF and HF mice. Fig. S3 presents a flow cytometry and scRNA-seq characterization of MDPs, G-mono, M-mono, and intermediary precursors in various tissues in LF and HF mice. Fig. S4 presents a characterization of monocyte effector functions in LF and HF mice. Fig. S5 shows the distribution and functions of neutrophils during obesity in various models. Table S1 contains a list of all antibodies used for flow cytometry, CyTOF, and immunofluorescence. Table S2 presents a legend showing protein targets of the cytokine array performed in Fig. S4 F.
Supplementary Material
lists all antibodies used for flow cytometry, CyTOF, and immunofluorescence.
presents a legend showing protein targets of the cytokine array performed in.
Acknowledgments
We thank the Goodman Cancer Institute and Life Sciences Complex at McGill University for core facility support, including the Single Cell and Imaging Mass Cytometry Platform (Yuhong Wei), Histology (Plinio Queiroz Da Cruz), the Comparative Medicine and Animal Resource Centre, the Flow Cytometry facility (Julien Leconte, Camille Stegen), and the McGill Genome Centre (Ken Dewar).
The authors acknowledge funding from the Susan G. Komen Foundation (D.F. Quail), La Vie en Rose (D.F. Quail), Canada Foundation for Innovation (D.F. Quail, L.A. Walsh), Canadian Institutes of Health Research (D.F. Quail, L.A. Walsh), the Terry Fox Research Institute (D.F. Quail), and the Breast Cancer Research Foundation (A.J. Dannenberg). D.F. Quail holds a Tier II Canada Research Chair in Tumour Microenvironment research. L.A. Walsh holds a Rosalind Goodman Chair in Lung Cancer Research. S.A.C. McDowell acknowledges support from the Rosalind Goodman Commemorative Scholarship Charlotte, Michael D’Avirro Scholarship, Leo Karassik Fellowship Foundation, and Canadian Institutes of Health Research Canada Graduate Scholarship. S. Milette acknowledges support from the Canadian Institutes of Health Research Doctoral Fellowship program.
Author contributions: S.A.C. McDowell and D.F. Quail designed and led the study and wrote the original version of the manuscript; S. Milette and D.F. Quail wrote the revised version. S.A.C. McDowell, S. Milette, S. Doré, M.W. Yu, M. Sorin, and D.F. Quail interpreted the data. S.A.C. McDowell, S. Milette, S. Doré, M.W. Yu, M. Sorin, L. Wilson, L. Desharnais, A. Cristea, O. Varol, V. Breton, A. Arabzadeh, S. Petrecca, A. Bhagrath, J.N. Mandl, L.A. Walsh, and D.F. Quail performed in vivo experiments. S.A.C. McDowell, S. Milette, M.W. Yu, L. Wilson, L. Desharnais, A. Cristea, O. Varol, V. Breton, H. Loucif, and J.H. Fritz performed in vitro assays and/or immunostaining. S. Milette, S. Doré, M. Sorin, A. Atallah, A. Swaby, B. Fiset, and L.A. Walsh provided analysis support for RNA-seq, CyTOF, scRNA-seq, and/or 16S rRNA-seq analysis. A.J. Dannenberg, P.R. Holt, and D.F. Quail generated bulk RNA-seq data. K.D. Lach, M.S.M. Issac, R.F. Rayes, P.O. Fiset, and J.D. Spicer provided human lung metastasis samples, built the patient TMA, and provided pathology/clinical insight. All authors provided essential insight throughout the study and reviewed and approved the manuscript.
Data availability
Data are available upon reasonable request. All sequencing data have been deposited at the NCBI BioProject resource (PRJNA954438) with the exception of bulk RNA-seq data from mouse LF/HF lung neutrophils, which were previously published (McDowell et al., 2021) and can be accessed at the Gene Expression Omnibus (GSE165442).
References
- Adrover, J.M., Aroca-Crevillén A., Crainiciuc G., Ostos F., Rojas-Vega Y., Rubio-Ponce A., Cilloniz C., Bonzón-Kulichenko E., Calvo E., Rico D., et al. 2020. Programmed “disarming” of the neutrophil proteome reduces the magnitude of inflammation. Nat. Immunol. 21:135–144. 10.1038/s41590-019-0571-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adrover, J.M., Del Fresno C., Crainiciuc G., Cuartero M.I., Casanova-Acebes M., Weiss L.A., Huerga-Encabo H., Silvestre-Roig C., Rossaint J., Cossío I., et al. 2019. A neutrophil timer coordinates immune defense and vascular protection. Immunity. 50:390–402.e10. 10.1016/j.immuni.2019.01.002 [DOI] [PubMed] [Google Scholar]
- Alfaro, C., Teijeira A., Oñate C., Pérez G., Sanmamed M.F., Andueza M.P., Alignani D., Labiano S., Azpilikueta A., Rodriguez-Paulete A., et al. 2016. Tumor-produced interleukin-8 attracts human myeloid-derived suppressor cells and elicits extrusion of neutrophil extracellular traps (NETs). Clin. Cancer Res. 22:3924–3936. 10.1158/1078-0432.CCR-15-2463 [DOI] [PubMed] [Google Scholar]
- Ambrosi, T.H., Scialdone A., Graja A., Gohlke S., Jank A.M., Bocian C., Woelk L., Fan H., Logan D.W., Schürmann A., et al. 2017. Adipocyte accumulation in the bone marrow during obesity and aging impairs stem cell-based hematopoietic and bone regeneration. Cell Stem Cell. 20:771–784.e6. 10.1016/j.stem.2017.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballesteros, I., Rubio-Ponce A., Genua M., Lusito E., Kwok I., Fernández-Calvo G., Khoyratty T.E., van Grinsven E., González-Hernández S., Nicolás-Ávila J.A., et al. 2020. Co-Option of neutrophil fates by tissue environments. Cell. 183:1282–1297.e18. 10.1016/j.cell.2020.10.003 [DOI] [PubMed] [Google Scholar]
- Becht, E., McInnes L., Healy J., Dutertre C.A., Kwok I.W.H., Ng L.G., Ginhoux F., and Newell E.W.. 2018. Dimensionality reduction for visualizing single-cell data using UMAP. Nat. Biotechnol. 10.1038/nbt.4314 [DOI] [PubMed] [Google Scholar]
- Boden, G. 2008. Obesity and free fatty acids. Endocrinol Metab. Clin. N. Am. 37:635–646. 10.1016/j.ecl.2008.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredella, M.A., Torriani M., Ghomi R.H., Thomas B.J., Brick D.J., Gerweck A.V., Rosen C.J., Klibanski A., and Miller K.K.. 2011. Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity. 19:49–53. 10.1038/oby.2010.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brestoff, J.R., and Artis D.. 2015. Immune regulation of metabolic homeostasis in health and disease. Cell. 161:146–160. 10.1016/j.cell.2015.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calle, E.E., Rodriguez C., Walker-Thurmond K., and Thun M.J.. 2003. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med. 348:1625–1638. 10.1056/NEJMoa021423 [DOI] [PubMed] [Google Scholar]
- Chan, M.E., Adler B.J., Green D.E., and Rubin C.T.. 2012. Bone structure and B-cell populations, crippled by obesity, are partially rescued by brief daily exposure to low-magnitude mechanical signals. FASEB J. 26:4855–4863. 10.1096/fj.12-209841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong, J., Liu P., Zhou G., and Xia J.. 2020. Using MicrobiomeAnalyst for comprehensive statistical, functional, and meta-analysis of microbiome data. Nat. Protoc. 15:799–821. 10.1038/s41596-019-0264-1 [DOI] [PubMed] [Google Scholar]
- Christ, A., Günther P., Lauterbach M.A.R., Duewell P., Biswas D., Pelka K., Scholz C.J., Oosting M., Haendler K., Baßler K., et al. 2018. Western diet triggers NLRP3-dependent innate immune reprogramming. Cell. 172:162–175.e14. 10.1016/j.cell.2017.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements, V.K., Long T., Long R., Figley C., Smith D.M.C., and Ostrand-Rosenberg S.. 2018. Frontline Science: High fat diet and leptin promote tumor progression by inducing myeloid-derived suppressor cells. J. Leukoc. Biol. 103:395–407. 10.1002/JLB.4HI0517-210R [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davie, S.A., Maglione J.E., Manner C.K., Young D., Cardiff R.D., MacLeod C.L., and Ellies L.G.. 2007. Effects of FVB/NJ and C57Bl/6J strain backgrounds on mammary tumor phenotype in inducible nitric oxide synthase deficient mice. Transgenic Res. 16:193–201. 10.1007/s11248-006-9056-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evrard, M., Kwok I.W.H., Chong S.Z., Teng K.W.W., Becht E., Chen J., Sieow J.L., Penny H.L., Ching G.C., Devi S., et al. 2018. Developmental analysis of bone marrow neutrophils reveals populations specialized in expansion, trafficking, and effector functions. Immunity. 48:364–379.e8. 10.1016/j.immuni.2018.02.002 [DOI] [PubMed] [Google Scholar]
- Falagas, M.E., and Kompoti M.. 2006. Obesity and infection. Lancet Infect. Dis. 6:438–446. 10.1016/S1473-3099(06)70523-0 [DOI] [PubMed] [Google Scholar]
- Friedrich, K., Sommer M., Strobel S., Thrum S., Blüher M., Wagner U., and Rossol M.. 2019. Perturbation of the monocyte compartment in human obesity. Front. Immunol. 10:1874. 10.3389/fimmu.2019.01874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geissmann, F., Jung S., and Littman D.R.. 2003. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity. 19:71–82. 10.1016/S1074-7613(03)00174-2 [DOI] [PubMed] [Google Scholar]
- Gong, T., Liu L., Jiang W., and Zhou R.. 2020. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Nat. Rev. Immunol. 20:95–112. 10.1038/s41577-019-0215-7 [DOI] [PubMed] [Google Scholar]
- Hasenberg, A., Hasenberg M., Männ L., Neumann F., Borkenstein L., Stecher M., Kraus A., Engel D.R., Klingberg A., Seddigh P., et al. 2015. Catchup: A mouse model for imaging-based tracking and modulation of neutrophil granulocytes. Nat. Methods. 12:445–452. 10.1038/nmeth.3322 [DOI] [PubMed] [Google Scholar]
- Jaitin, D.A., Adlung L., Thaiss C.A., Weiner A., Li B., Descamps H., Lundgren P., Bleriot C., Liu Z., Deczkowska A., et al. 2019. Lipid-associated macrophages control metabolic homeostasis in a trem2-dependent manner. Cell. 178:686–698.e14. 10.1016/j.cell.2019.05.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoyratty, T.E., Ai Z., Ballesteros I., Eames H.L., Mathie S., Martín-Salamanca S., Wang L., Hemmings A., Willemsen N., von Werz V., et al. 2021. Distinct transcription factor networks control neutrophil-driven inflammation. Nat. Immunol. 22:1093–1106. 10.1038/s41590-021-00968-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok, I., Becht E., Xia Y., Ng M., Teh Y.C., Tan L., Evrard M., Li J.L.Y., Tran H.T.N., Tan Y., et al. 2020. Combinatorial single-cell analyses of granulocyte-monocyte progenitor heterogeneity reveals an early uni-potent neutrophil progenitor. Immunity. 53:303–318.e5. 10.1016/j.immuni.2020.06.005 [DOI] [PubMed] [Google Scholar]
- La Manno, G., Soldatov R., Zeisel A., Braun E., Hochgerner H., Petukhov V., Lidschreiber K., Kastriti M.E., Lönnerberg P., Furlan A., et al. 2018. RNA velocity of single cells. Nature. 560:494–498. 10.1038/s41586-018-0414-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine, J.H., Simonds E.F., Bendall S.C., Davis K.L., Amir A.D., Tadmor M.D., Litvin O., Fienberg H.G., Jager A., Zunder E.R., et al. 2015. Data-driven phenotypic dissection of AML reveals progenitor-like cells that correlate with prognosis. Cell. 162:184–197. 10.1016/j.cell.2015.05.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, C., Burdon P.C., Bridger G., Gutierrez-Ramos J.C., Williams T.J., and Rankin S.M.. 2003. Chemokines acting via CXCR2 and CXCR4 control the release of neutrophils from the bone marrow and their return following senescence. Immunity. 19:583–593. 10.1016/S1074-7613(03)00263-2 [DOI] [PubMed] [Google Scholar]
- McDowell, S.A.C., Luo R.B.E., Arabzadeh A., Doré S., Bennett N.C., Breton V., Karimi E., Rezanejad M., Yang R.R., Lach K.D., et al. 2021. Neutrophil oxidative stress mediates obesity-associated vascular dysfunction and metastatic transmigration. Nat. Cancer. 2:545–562. 10.1038/s43018-021-00194-9 [DOI] [PubMed] [Google Scholar]
- Mertz, D., Kim T.H., Johnstone J., Lam P.P., Science M., Kuster S.P., Fadel S.A., Tran D., Fernandez E., Bhatnagar N., and Loeb M.. 2013. Populations at risk for severe or complicated influenza illness: Systematic review and meta-analysis. BMJ. 347:f5061. 10.1136/bmj.f5061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler, K.D., Fuchs T.A., Nauseef W.M., Reumaux D., Roesler J., Schulze I., Wahn V., Papayannopoulos V., and Zychlinsky A.. 2011. Myeloperoxidase is required for neutrophil extracellular trap formation: Implications for innate immunity. Blood. 117:953–959. 10.1182/blood-2010-06-290171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagareddy, P.R., Kraakman M., Masters S.L., Stirzaker R.A., Gorman D.J., Grant R.W., Dragoljevic D., Hong E.S., Abdel-Latif A., Smyth S.S., et al. 2014. Adipose tissue macrophages promote myelopoiesis and monocytosis in obesity. Cell Metabol. 19:821–835. 10.1016/j.cmet.2014.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie, M., Yang L., Bi X., Wang Y., Sun P., Yang H., Liu P., Li Z., Xia Y., and Jiang W.. 2019. Neutrophil extracellular traps induced by IL8 promote diffuse large B-cell lymphoma progression via the TLR9 signaling. Clin. Cancer Res. 25:1867–1879. 10.1158/1078-0432.CCR-18-1226 [DOI] [PubMed] [Google Scholar]
- Norman, P. 2013. Evidence on the identity of the CXCR2 antagonist AZD-5069. Expert Opin. Ther. Pat. 23:113–117. 10.1517/13543776.2012.725724 [DOI] [PubMed] [Google Scholar]
- Olsen, L.R., Leipold M.D., Pedersen C.B., and Maecker H.T.. 2019. The anatomy of single cell mass cytometry data. Cytometry A. 95:156–172. 10.1002/cyto.a.23621 [DOI] [PubMed] [Google Scholar]
- Olson, O.C., Quail D.F., and Joyce J.A.. 2017. Obesity and the tumor microenvironment. Science. 358:1130–1131. 10.1126/science.aao5801 [DOI] [PubMed] [Google Scholar]
- Osman, M.A., and Hennessy B.T.. 2015. Obesity correlation with metastases development and response to first-line metastatic chemotherapy in breast cancer. Clin. Med. Insights Oncol. 9:105–112. 10.4137/CMO.S32812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrelli, F., Cortellini A., Indini A., Tomasello G., Ghidini M., Nigro O., Salati M., Dottorini L., Iaculli A., Varricchio A., et al. 2021. Association of obesity with survival outcomes in patients with cancer: A systematic review and meta-analysis. JAMA Netw. Open. 4:e213520. 10.1001/jamanetworkopen.2021.3520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quail, D.F., Amulic B., Aziz M., Barnes B.J., Eruslanov E., Fridlender Z.G., Goodridge H.S., Granot Z., Hidalgo A., Huttenlocher A., et al. 2022. Neutrophil phenotypes and functions in cancer: A consensus statement. J. Exp. Med. 219:e20220011. 10.1084/jem.20220011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quail, D.F., and Dannenberg A.J.. 2019. The obese adipose tissue microenvironment in cancer development and progression. Nat. Rev. Endocrinol. 15:139–154. 10.1038/s41574-018-0126-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quail, D.F., Olson O.C., Bhardwaj P., Walsh L.A., Akkari L., Quick M.L., Chen I.C., Wendel N., Ben-Chetrit N., Walker J., et al. 2017. Obesity alters the lung myeloid cell landscape to enhance breast cancer metastasis through IL5 and GM-CSF. Nat. Cell Biol. 19:974–987. 10.1038/ncb3578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehman, A., Hemmert K.C., Ochi A., Jamal M., Henning J.R., Barilla R., Quesada J.P., Zambirinis C.P., Tang K., Ego-Osuala M., et al. 2013. Role of fatty-acid synthesis in dendritic cell generation and function. J. Immunol. 190:4640–4649. 10.4049/jimmunol.1202312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saederup, N., Cardona A.E., Croft K., Mizutani M., Cotleur A.C., Tsou C.L., Ransohoff R.M., and Charo I.F.. 2010. Selective chemokine receptor usage by central nervous system myeloid cells in CCR2-red fluorescent protein knock-in mice. PLoS One. 5:e13693. 10.1371/journal.pone.0013693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele, C.W., Karim S.A., Leach J.D.G., Bailey P., Upstill-Goddard R., Rishi L., Foth M., Bryson S., McDaid K., Wilson Z., et al. 2016. CXCR2 inhibition profoundly suppresses metastases and augments immunotherapy in pancreatic ductal adenocarcinoma. Cancer Cell. 29:832–845. 10.1016/j.ccell.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suárez-Cuenca, J.A., Ruíz-Hernández A.S., Mendoza-Castañeda A.A., Domínguez-Pérez G.A., Hernández-Patricio A., Vera-Gómez E., De la Peña-Sosa G., Banderas-Lares D.Z., Montoya-Ramírez J., Blas-Azotla R., et al. 2019. Neutrophil-to-lymphocyte ratio and its relation with pro-inflammatory mediators, visceral adiposity and carotid intima-media thickness in population with obesity. Eur. J. Clin. Invest. 49:e13085. 10.1111/eci.13085 [DOI] [PubMed] [Google Scholar]
- Sudhakar, M., Winfred S.B., Meiyazhagan G., and Venkatachalam D.P.. 2022. Mechanisms contributing to adverse outcomes of COVID-19 in obesity. Mol. Cell. Biochem. 477:1155–1193. 10.1007/s11010-022-04356-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, L., Clavijo P.E., Robbins Y., Patel P., Friedman J., Greene S., Das R., Silvin C., Van Waes C., Horn L.A., et al. 2019. Inhibiting myeloid-derived suppressor cell trafficking enhances T cell immunotherapy. JCI Insight. 4:e126853. 10.1172/jci.insight.126853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teijeira, Á., Garasa S., Gato M., Alfaro C., Migueliz I., Cirella A., de Andrea C., Ochoa M.C., Otano I., Etxeberria I., et al. 2020. CXCR1 and CXCR2 chemokine receptor agonists produced by tumors induce neutrophil extracellular traps that interfere with immune cytotoxicity. Immunity. 52:856–871.e8. 10.1016/j.immuni.2020.03.001 [DOI] [PubMed] [Google Scholar]
- Weiss, S., Xu Z.Z., Peddada S., Amir A., Bittinger K., Gonzalez A., Lozupone C., Zaneveld J.R., Vázquez-Baeza Y., Birmingham A., et al. 2017. Normalization and microbial differential abundance strategies depend upon data characteristics. Microbiome. 5:27. 10.1186/s40168-017-0237-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia, S., Sha H., Yang L., Ji Y., Ostrand-Rosenberg S., and Qi L.. 2011. Gr-1+ CD11b+ myeloid-derived suppressor cells suppress inflammation and promote insulin sensitivity in obesity. J. Biol. Chem. 286:23591–23599. 10.1074/jbc.M111.237123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yáñez, A., Coetzee S.G., Olsson A., Muench D.E., Berman B.P., Hazelett D.J., Salomonis N., Grimes H.L., and Goodridge H.S.. 2017. Granulocyte-monocyte progenitors and monocyte-dendritic cell progenitors independently produce functionally distinct monocytes. Immunity. 47:890–902.e4. 10.1016/j.immuni.2017.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yáñez, A., and Goodridge H.S.. 2018. Identification and isolation of oligopotent and lineage-committed myeloid progenitors from mouse bone marrow. J. Vis. Exp. 58061. 10.3791/58061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yáñez, A., Ng M.Y., Hassanzadeh-Kiabi N., and Goodridge H.S.. 2015. IRF8 acts in lineage-committed rather than oligopotent progenitors to control neutrophil vs monocyte production. Blood. 125:1452–1459. 10.1182/blood-2014-09-600833 [DOI] [PubMed] [Google Scholar]
- Yokota, T., Meka C.S., Kouro T., Medina K.L., Igarashi H., Takahashi M., Oritani K., Funahashi T., Tomiyama Y., Matsuzawa Y., and Kincade P.W.. 2003. Adiponectin, a fat cell product, influences the earliest lymphocyte precursors in bone marrow cultures by activation of the cyclooxygenase-prostaglandin pathway in stromal cells. J. Immunol. 171:5091–5099. 10.4049/jimmunol.171.10.5091 [DOI] [PubMed] [Google Scholar]
- Zhang, Y., Proenca R., Maffei M., Barone M., Leopold L., and Friedman J.M.. 1994. Positional cloning of the mouse obese gene and its human homologue. Nature. 372:425–432. 10.1038/372425a0 [DOI] [PubMed] [Google Scholar]
- Zhu, R.J., Wu M.Q., Li Z.J., Zhang Y., and Liu K.Y.. 2013. Hematopoietic recovery following chemotherapy is improved by BADGE-induced inhibition of adipogenesis. Int. J. Hematol. 97:58–72. 10.1007/s12185-012-1233-4 [DOI] [PubMed] [Google Scholar]
- Zilionis, R., Engblom C., Pfirschke C., Savova V., Zemmour D., Saatcioglu H.D., Krishnan I., Maroni G., Meyerovitz C.V., Kerwin C.M., et al. 2019. Single-cell transcriptomics of human and mouse lung cancers reveals conserved myeloid populations across individuals and species. Immunity. 50:1317–1334.e10. 10.1016/j.immuni.2019.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
lists all antibodies used for flow cytometry, CyTOF, and immunofluorescence.
presents a legend showing protein targets of the cytokine array performed in.
Data Availability Statement
Data are available upon reasonable request. All sequencing data have been deposited at the NCBI BioProject resource (PRJNA954438) with the exception of bulk RNA-seq data from mouse LF/HF lung neutrophils, which were previously published (McDowell et al., 2021) and can be accessed at the Gene Expression Omnibus (GSE165442).