Diabetes is a public health epidemic affecting ∼34 million Americans with type 2 diabetes (1). American Indians are nearly three times more likely to be diagnosed with type 2 diabetes than non-Hispanic Whites (2) and more than twice as likely to die of complications of type 2 diabetes (3).
Medications are often a necessary strategy for managing type 2 diabetes. Medication adherence is linked with better glycemic control, fewer hospitalizations, and decreased medical costs (4,5). Factors and sociodemographic variables that affect medication adherence have been explored extensively in the literature, including the cost of medications, skepticism about medications, regimen complexity, depression, age, and forgetfulness in both taking and refilling medications (5).
In a recent study, the medication adherence rate was found to be higher in Whites (76.9%) compared with Hispanics (68.5%), Blacks (69.4%), and Asians (74.3%), but American Indians were not included (6). Because of the high prevalence of type 2 diabetes in the American Indian population (2), it is important to improve our understanding of diabetes self-management strategies such as medication adherence, but we found no reviews of medication adherence among American Indians. The aim of our literature review was to fill this gap by describing medication adherence and associated facilitators, barriers, and sociodemographic variables in American Indians with type 2 diabetes.
Research Design and Methods
An integrated literature review on medication adherence in American Indians with type 2 diabetes was used to ensure inclusion of all research methodologies, as literature on this topic is limited (7). After consulting with a health science reference librarian, the databases selected to search for articles were PubMed and the Cumulative Index of Nursing and Allied Health Literature. We found 1,012 articles published between 1974 to 2021 by using the search terms (American Indian OR Native American OR Indians, North American OR Alaska Natives) AND (diabetes OR diabetes mellitus) AND (adherence OR compliance OR medication adherence OR medication barriers OR medication facilitators OR self-management OR barrier OR facilitator OR management).
We selected studies if they 1) were peer-reviewed studies, 2) included American Indian participants ≥18 years of age with type 2 diabetes, 3) discussed medication adherence in the results, 4) were conducted in the United States, and 5) were written in English. Studies were excluded if 1) all participants had type 1 diabetes, 2) participants had gestational diabetes, or 3) children or adolescents were included.
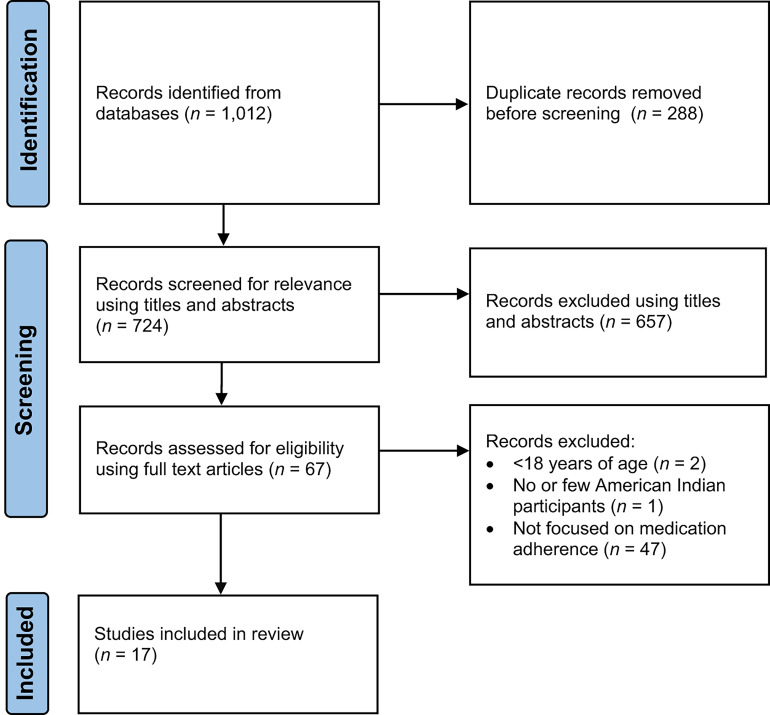
The systematic search was conducted using the Preferred Reporting Items for Systematic Review and Meta-Analysis (Figure 1) (8). A total of 1,012 articles were found, and 288 duplicates were then removed. The remaining 724 articles were screened using the title, with 657 irrelevant articles removed. Of the remaining 67 articles, an additional 50 were removed because they did not meet the inclusion or exclusion criteria. The remaining 17 articles were examined independently by two investigators using the Standard Quality Assessment Criteria for Evaluating Research Papers from a Variety of Fields (9). Disagreements were discussed to reach a consensus on final scores. The 17 articles met a minimum threshold of 55%, and none were eliminated from the review.
Figure 1.
Identification of studies.
Results
Study Characteristics
The characteristics of the 17 studies are presented in Table 1. Five studies used a qualitative design (10–14), five used a mixed-methods design (15–19), and seven used a quantitative methodology (20–26). American Indians made up the totality of participants in 10 studies (10–14,17–19,22,23), and seven studies included participants from other races or ethnicities (15,16,20,21,24–26). Nine studies focused on type 2 diabetes (10–12,15,18–21,23), whereas in seven studies, both type 1 diabetes and type 2 diabetes were included or diabetes type was not specified (13,16,17,22,24–26). One study focused on prediabetes, diabetes, and caregivers (14). Two studies included participants with either or both diabetes and hypertension, but did stratify results related to medication adherence by diagnosis (16,26).
Table 1.
Summary of Included Studies
| Article, Year | Design, Sample, Age, Setting, and Diabetes Type | Measure | Findings |
|---|---|---|---|
| Anderson, 2005 (16) | Design: mixed-methods study using community-based participatory research methods; sample: n = 86, 20% AI, 39% AA, 26% Asian, 10% Hispanic, 5% other; age range: ≥21 years; setting: urban; diabetes type: not specified | Interview with behavioral assessment survey | Most AI participants reported taking diabetes medication as prescribed. |
| Aronson et al., 2020 (19) | Design: mixed-methods study as part of community-based participatory research project (Maawaji’ idi-oog Mino-ayaawin); sample: n = 166, AI; age range: ≥18 years; setting: rural; diabetes type: type 2 diabetes | MMAS-4: low adherence 0–1 of 4, medium adherence 2–3 of 4, high adherence 4 of 4 | Average score on the MMAS-4 was 2.54 of 4; high medication adherence in 27.7%, and low medication adherence in 20.5%.; age and level of education linked with higher medication adherence; diabetes distress, depressive symptomology, and female gender linked with lower medication adherence |
| Bell et al., 2010 (20) | Design: cross-sectional study; sample: n = 696, 26% AI, 31.6% AA, 42.4% White; age range: ≥65 years; setting: rural; diabetes type: type 2 diabetes | SDSCA with medication adherence domain: number of days adherent to medication in past 7 days | 92.7% of all participants fully adherent (7 out of 7 days) with medication regimen; no correlation between depressive symptoms and adherence |
| Castro et al., 2009 (21) | Design: community case study; sample: n = 255, 88% urban AI/AN, 8% White, 5% AA, 5% other; age range: ≥18 years; setting: urban; diabetes type: type 2 diabetes | Intake form, lifestyle survey | Adherence: 74% reported most or all of the time, 7% seldom or sometimes, and 12% none of the time |
| Henderson, 2010 (11) | Design: ethnographic study; sample: n = 30, AI; age range: ≥55 years; setting: did not specify; diabetes type: type 2 diabetes | Structured and semi-structured interviews, including an adherence assessment | More participants adherent to medication than to diet; elders with strong cultural identity less likely to adhere to medication; social pressure against adherence to Western medicine identified; few participants believed insulin could increase severity of diabetes |
| Jacobs et al., 2014 (17) | Design: descriptive, correlational design, mixed-methods approach; sample: n = 40, AI; age range: ≥18 years; setting: rural; diabetes type: type 1 or type 2 diabetes | MMAS-4: lowest adherence 0 of 4, highest adherence 4 of 4 | Average medication adherence poor (0.90 of 4); many participants sometimes considered discontinuing medication; reported barriers included finances, pain from injections, treatment burden; reported facilitators included knowledge that medications are important and helpful and aid in improving blood glucose |
| Jones et al., 2020 (12) | Design: secondary analysis of qualitative descriptive data; sample: n = 28, AI; age range: >60 years; setting: rural; diabetes type: type 2 diabetes | Semi-structured interviews | Diabetes fatigue reported as a barrier; reported facilitators included partner who assists with care |
| Lautenschlager and Smith, 2006 (13) | Design: qualitative study; sample: n = 40, AI; age range: ≥18 years; setting: urban; diabetes type: not specified | Focus groups | Participants often nonadherent to prescribed medication; some used traditional medicine instead of or in combination with prescribed regimen; barriers included disbelief and pessimistic attitude toward diabetes diagnosis, cost, lack of health insurance, homelessness |
| Miller et al., 1987 (22) | Design: cross-sectional study; sample: n = 60, AI; age range: 25–70 years; setting: not specified; diabetes type: type 1 or type 2 diabetes | HBS: 5-point Likert scale with 1 = unlikely and 5 = likely | Medication adherence high for participants with controlled and uncontrolled diabetes; positive attitude toward taking medication in patients with uncontrolled diabetes |
| Newman et al., 2014 (14) | Design: qualitative study; sample: n = 84, AI; age range: ≥18 years; setting: rural; diabetes type: prediabetes, diabetes, or caregivers of family member with diabetes | Focus groups | Some participants reported hesitancy toward taking medication and wanted to reduce or quit taking medication; one noted reason was skepticism of medication; fear of starting insulin also reported |
| Ratner et al., 2017 (23) | Design: cross-sectional observational study as part of a community-based participatory research project (Maawaji’ idi-oog Mino-ayaawin); sample: n = 166, AI; age range: ≥18 years; setting: rural; diabetes type: type 2 diabetes | MMAS-4: 4 questions, 1 point each; higher scores = higher adherence, lower scores = lower adherence | Adherence to mediation linked to diabetes empowerment and patient-centered care; diabetes empowerment was a partial mediator for the relationship between medication adherence and patient-centered care; lower levels of adherence noted with younger participants and females |
| Scarton et al., 2019 (10) | Design: qualitative study; sample: n = 62, AI; age range: ≥18 years; setting: rural; diabetes type: type 2 diabetes | Focus groups | Barriers to medication adherence included feelings of laziness, adverse effects from medication, and forgetfulness |
| Schmittdiel et al., 2014 (24) | Design: observational cohort study; sample: n = 328,908, 1.8% AI/AN, 98.2% Non-Hispanic White; age range: ≥18 years; setting: urban; diabetes type: not specified | Pharmacy refill data: ≥80% = good adherence | AI/AN participants receiving care within a commercial integrated delivery system had lower adherence to oral medication than non-Hispanic Whites |
| Schoenberg et al., 2008 (15) | Design: mixed-methods study; sample: n = 80, 39% urban AI, 37% AA, 36% Mexican American, 24% rural White; age range: ≥55 years; setting: urban; diabetes type: type 2 diabetes | In-depth interviews, including SDSCA (number days adherent to medication in past 7 days) | Many reported taking medication 6 of 7 days; noted that adherence to medication may be influenced by self-efficacy and an understanding of the effectiveness of medications |
| Shiyanbola and Nelson, 2011 (25) | Design: cross-sectional study; sample: n = 16, 81.3% AI women, 18.7% other minority women; age range: not specified; setting: rural; diabetes type: both with 94% having type 2 diabetes | MMAS-4: nonadherent 4 of 4, adherent 0–1 of 4 | Most women (56.3%) not adherent to medications; correlation was identified between patients’ belief of individual control of diabetes and poor adherence; reason given was that patients did not feel medications controlled their diabetes |
| Wheat et al., 2020 (26) | Design: mirror-image study; sample: n = 33, 18.2% AI, 75.8% AA, 6.1% White; age range: ≥18 years; setting: not specified; diabetes type: not specified | Pharmacy refill data (PDC could not be calculated due to inconsistencies obtaining records); adherence barriers assessed using initial and follow-up interviews | Most frequently identified barriers to antidiabetic medications included forgetfulness, knowledge deficits, and side effects; additional barriers included cost and unavailability of refills; 63.9% of barriers to antidiabetic medications resolved with interventions by community health workers and pharmacists |
| Wilken and Nunn, 2017 (18) | Design: quasi-experimental study with mixed-methods approach; sample: n = 39, AI; age range: ≥21 years; setting: rural; diabetes type: type 2 diabetes | Talking Circles (culturally relevant forum) | Diabetes fatigue related to treatment burden noted as a barrier |
AI, American Indian; AN, Alaska Native; AA, African American; PDC, proportion of days covered.
Medication Adherence
Focus of Articles
In six of the 17 studies, medication adherence was a primary focus (17,19,23–26). In 11 of the articles, medication adherence was discussed within the context of self-management, but was not the primary focus (10–16,18,20–22).
Measures
Various methods were used to examine medication adherence (Table 1). Prescription claims data were used to assess adherence in one study, and good medication adherence was determined to be ≥80% on a scale from 0% (fully nonadherent) to 100% (fully adherent) (24).
Validated self-reported measures (5) assessing adherence were included in six studies (15,17,19,20,23,25). Four studies included the 4-item Morisky Medication Adherence Scale (MMAS-4) (17,19,23,25), which has dichotomous (yes/no) questions that are scored from 0 to 4. We suspect that the MMAS-4 data were likely shared in two of these four studies (i.e., data from the same participants in the same project used in two studies), but only one reported percentages of medication adherence (19,23). The Summary of Diabetes Self-Care Activities (SDSCA) measure was used during interviews in two studies to assess the number of days out of 7 days participants were adherent to their medication (15,20). One study included the Health Behavior Scale (HBS), a measurement tool not validated in participants with diabetes (22).
The remaining studies used several different methods to assess medication adherence and associated factors, including a behavioral assessment survey given as part of an interview (16), a diabetes self-management behavior intake form and lifestyle survey (21), and adherence assessment interviews (11). Interviews were used in two additional studies (12,26), and focus groups were used in three studies (10,13,14). A Talking Circle, a traditional forum in which individuals can discuss, provide, and receive support, was used to assess factors associated with adherence in one study (18).
Adherence
Overall adherence to medication was assessed in three of the four studies that used the MMAS-4. In one study, 27.7% of participants had high medication adherence (score of 4 of 4), and 20.5% had low adherence (0–1 of 4), and average adherence to diabetes medication was considered moderate (2.54 of 4) (19). Another study using the MMAS-4 found that average adherence to diabetes medication was low (0.90 of 4) (17). In the fourth study, 56.3% of females reported nonadherence to medication (>1 of 4) (25). In the first three studies, a higher score on the MMAS-4 indicated better adherence (17,19,23), whereas in the fourth, a score >1 indicated nonadherence (25). One study using the SDSCA measure found that 92.7% of participants reported being fully adherent to their medication regimen (20), and another study using the SDSCA measure found that most participants reported being adherent to medication on 6 of 7 days (15).
The only study using prescription claims data did not include medication adherence rates but found that American Indians were less adherent to oral diabetes medication than non-Hispanic Whites (24). Authors of another study planned to calculate the adherence rate using pharmacy records but were unable to consistently access pharmacy records (26).
Self-report forms and surveys used in two studies found that most participants took their medication as directed (16,21). Authors of the study using an intake form and lifestyle survey reported that 74% of participants took their medication as directed (21). In contrast, authors of a study using focus groups found that many participants did not adhere to their medication regimen, even when they recognized the benefits of the medication (13). In a study using interviews along with an adherence assessment (11) and another study using the HBS (22), investigators found that participants were more adherent to medication than to their dietary regimen. Also, medication adherence was lower in elders with strong ties to their Indigenous culture (11).
Adherence Barriers and Facilitators
Medication adherence barriers and facilitators were examined in 12 of the 17 studies (10–15,17,18,22,23,25,26) (Table 2). Three of these 12 studies included responses from participants from other racial and ethnic groups (15,25,26). The association between gender and medication adherence was examined in three studies, age and medication adherence was reported in two studies, and education and medication adherence was reported in one study (19,23,25) (Table 2). One of the three studies that looked at gender and adherence included responses from women participants from other minority groups (25). Financial barriers and diabetes fatigue related to treatment were the most common barriers noted (12,13,17,18,26), and knowledge that the medication was effective and assistance from care partners or community health workers were the most noted facilitators (12,15,17,26). Sociodemographic factors associated with lower adherence were female gender, younger age, and lower levels of education (19,23).
Table 2.
Medication Adherence Barriers, Facilitators, and Associated Sociodemographic Factors
| Barriers | Facilitators | Associated Sociodemographic Factors |
|---|---|---|
|
|
Discussion
The goal of this integrative review was to synthesize existing literature on medication adherence and associated facilitators, barriers, and sociodemographic variables in American Indians with type 2 diabetes. The 17 reviewed studies had a variety of methods and measures, and many included relatively small numbers of American Indians with type 2 diabetes. Findings indicate considerable variability in medication adherence and a number of facilitators and barriers. For the few studies considering sociodemographic variables, findings indicate that women, younger people, and individuals with lower education levels had lower medication adherence than their counterparts.
Measures
We found variability in the methods used to measure medication adherence across studies. Medication adherence was examined using prescription refill data in one study (24). Validated self-report measurements within this review included the MMAS-4 (17,19,23,25) and the SDSCA (15,20). Currently, there is no universal gold standard for measuring diabetes medication adherence (27,28). Self-report measures are commonly used because they are low-cost and easy to administer (29). In several studies with self-report measures, including the SDSCA, the HBS, surveys, and an intake form, the majority of participants reported taking their medication as directed most or all of the time (15,16,20–22). The preponderance of self-report measures in most of the reviewed studies may overestimate medication adherence as a result of biases such as recall bias and social desirability (29). In future studies of American Indians’ adherence with type 2 diabetes medications, we recommend using validated measures and incorporating two or more measures when possible (29).
Adherence
Overall, there was variability in findings regarding medication adherence among American Indians with type 2 diabetes. This variability may have been the result of the various approaches used to measure and report mediation adherence. Low adherence was reported in several studies (13,17,25), in addition to one study reporting lower adherence in American Indians compared with non-Hispanic Whites (24). These findings are consistent with previous studies noting racial and ethnic disparities in medication adherence in other underrepresented racial and ethnic groups (5,6,30,31). Because of the variability in findings, additional research is needed to examine adherence to diabetes medication using validated measures in American Indian communities.
Barriers
Many of the barriers found in our review such as knowledge deficits, forgetfulness, and financial issues are consistent with barriers to medication adherence in the general population (5,10,13,17,26,31). Consistent with our findings, prior literature noted that African American participants, a population also facing diabetes disparities, similarly reported concerns regarding adverse effects, as well as apprehension and frustration toward medications as barriers to adherence (32). In our review, participants from urban settings and medically underserved communities and those without access to medication and care provided by Indian Health Service benefits listed cost as a barrier (13,17,26). To fully understand the extent to which cost affects medication adherence, additional research is needed, specifically in reservation-dwelling American Indians who use tribal health care services, which provide medical care and prescriptions with no cost to patients.
Facilitators
Social support or involvement of community health workers, each noted in one included study as facilitators of medication adherence, have resulted in mixed findings in the literature (5,12,26,28,31,33–35). Diabetes empowerment and patient-centered care were both linked to medication adherence in our review (23). There is evidence from previous literature that diabetes empowerment, patient-centered care, and patient-centered medical homes may improve mediation adherence in patients with diabetes and other chronic diseases (36–38). Because of differences in values and beliefs regarding medications, culturally appropriate methodologies such as Talking Circles (18,21) should be considered when designing research studies to better understand facilitators and barriers in American Indians and other racial and ethnic minorities.
Sociodemographic Factors
Sociodemographic factors were also found to be associated with medication adherence. Although there is no consensus on the effects of sex or gender on medication adherence in the general population (31), some studies have shown that women have lower adherence than men, which is consistent with our findings (19,23,25,39). Shiyanbola and Nelson (25) explained that sociocultural factors such as having the role of caretaker within families may affect adherence to medication in some women with diabetes. Also, congruent with our findings (19,23), younger individuals aged 20–44 years have been found to be less adherent than individuals ≥45 years in the general population, and those with a high school education were less likely to be adherent than those with a college education (39). Future studies should further explore how sociodemographic variables affect medication adherence, specifically in American Indian populations.
Strengths and Limitations
Because of the limited published research in this area, this review included only 17 articles. The strengths of this integrative review were the inclusion of all articles that addressed medication adherence within American Indian communities and a rigorous approach to rating the quality of the selected articles. Notable limitations were that few studies measured medication adherence, making it difficult to reach conclusions regarding adherence to diabetes medication in the American Indian population. Recall bias can be an issue in studies with self-report measures, which were used in the majority of the reviewed studies. Other limitations include studies that did not report findings by race (15,20,21,25,26), studies that did not exclusively include participants with type 2 diabetes (13,14,16,17,24–26), and studies that included a small percentage of American Indians (16,24,26). In addition, measures not validated in participants with diabetes were used in some studies to assess adherence, and one study reported having inadequate power because of its small sample size (n <20) (25).
Clinical Implications
Diabetes empowerment, patient-centered care, and efforts to address barriers such as financial issues, diabetes fatigue, and knowledge deficits may be important strategies to improve medication adherence (11,13,15,17,23,26). Also, the use of community health workers in partnership with pharmacists to address barriers may be a useful strategy (26). Finally, there are many distinct Indigenous tribes in the United States, and culturally responsive practices need to be used while working alongside tribal communities.
Conclusion
Medication adherence in American Indians with type 2 diabetes was low in several studies, but the results were variable. More research is needed to understand medication adherence and associated factors in the American Indian population, specifically in reservation-dwelling American Indians. Future research using validated measures is also needed to better understand medication adherence and its associated factors in this population. It is imperative that researchers and health care providers practice cultural competence to address medication barriers and incorporate facilitators to improve diabetes medication adherence.
Article Information
Funding
This publication was made possible by a graduate fellowship award from the University of Florida (T.N.) and grants R01NR020386 and U54CA233444 from the National Institutes of Health (NIH) National Institute of Nursing Research (NINR), and National Cancer Institute (NCI). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NINR and NCI. The final peer-reviewed manuscript is subject to the NIH Public Access Policy.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
T.N. researched data and wrote the manuscript. D.J.W. conceptualized the literature review and reviewed/edited the manuscript. L.S. conceptualized the literature review, evaluated articles, and reviewed/edited the manuscript. T.N. is the guarantor of this work, and as such, had full access to the included articles and takes responsibility for the integrity and accuracy of this integrative review.
References
- 1. Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2020: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2020 [Google Scholar]
- 2. National Center for Health Statistics . National Health Interview Survey, 2018: public-use data file and documentation. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2018 [Google Scholar]
- 3. Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B. Deaths: final data for 2018. Natl Vital Stat Rep 2021;69:1–83 [PubMed] [Google Scholar]
- 4. Egede LE, Gebregziabher M, Echols C, Lynch CP. Longitudinal effects of medication nonadherence on glycemic control. Ann Pharmacother 2014;48:562–570 [DOI] [PubMed] [Google Scholar]
- 5. Capoccia K, Odegard PS, Letassy N. Medication adherence with diabetes medication: a systematic review of the literature. Diabetes Educ 2016;42:34–71 [DOI] [PubMed] [Google Scholar]
- 6. Xie Z, St Clair P, Goldman DP, Joyce G. Racial and ethnic disparities in medication adherence among privately insured patients in the United States. PLoS One 2019;14:e0212117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005;52:546–553 [DOI] [PubMed] [Google Scholar]
- 8. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021;18:e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kmet LM, Lee RC, Cook LS. Standard Quality Assessment Criteria for Evaluating Primary Research Papers From a Variety of Fields. Edmonton, Alberta, Alberta Heritage Foundation for Medical Research, 2004 [Google Scholar]
- 10. Scarton L, Velazquez I, O’Neal LJ, et al. Developing a culturally tailored multigenerational intervention to prevent and manage type 2 diabetes in American Indian families living in rural settings: findings from a focus group study. Res Nurs Health 2019;42:226–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Henderson LC. Divergent models of diabetes among American Indian elders. J Cross Cult Gerontol 2010;25:303–316 [DOI] [PubMed] [Google Scholar]
- 12. Jones J, Goins RT, Schure M, Winchester B, Bradley V. Putting self-management in the context of community-dwelling American Indians living with type 2 diabetes. Diabetes Educ 2020;46:108–117 [DOI] [PubMed] [Google Scholar]
- 13. Lautenschlager L, Smith C. Low-income American Indians’ perceptions of diabetes. J Nutr Educ Behav 2006;38:307–315 [DOI] [PubMed] [Google Scholar]
- 14. Newman S, Cheng T, Ghahate DM, et al. Assessing knowledge and attitudes of diabetes in Zuni Indians using a culture-centered approach. PLoS One 2014;9:e99614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schoenberg NE, Traywick LS, Jacobs-Lawson J, Kart CS. Diabetes self-care among a multiethnic sample of older adults. J Cross Cult Gerontol 2008;23:361–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anderson JB. Unraveling health disparities: examining the dimensions of hypertension and diabetes through community engagement. J Health Care Poor Underserved 2005;16(Suppl. A):91–117 [DOI] [PubMed] [Google Scholar]
- 17. Jacobs A, Kemppainen JK, Taylor JS, Hadsell C. Beliefs about diabetes and medication adherence among Lumbee Indians living in rural southeastern North Carolina. J Transcult Nurs 2014;25:167–175 [DOI] [PubMed] [Google Scholar]
- 18. Wilken M, Nunn M. Talking Circles to improve diabetes self-care management. Diabetes Educ 2017;43:388–395 [DOI] [PubMed] [Google Scholar]
- 19. Aronson BD, Sittner KJ, Walls ML. The mediating role of diabetes distress and depressive symptoms in type 2 diabetes medication adherence gender differences. Health Educ Behav 2020;47:474–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bell RA, Andrews JS, Arcury TA, Snively BM, Golden SL, Quandt SA. Depressive symptoms and diabetes self-management among rural older adults. Am J Health Behav 2010;34:36–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Castro S, O’Toole M, Brownson C, Plessel K, Schauben L. A diabetes self-management program designed for urban American Indians. Prev Chronic Dis 2009;6:A131. [PMC free article] [PubMed] [Google Scholar]
- 22. Miller P, Wikoff R, Keen O, Norton J. Health beliefs and regimen adherence of the American Indian diabetic. Am Indian Alsk Nativ Ment Health Res (1987) 1987;1:24–36 [PubMed] [Google Scholar]
- 23. Ratner NL, Davis EB, Lhotka LL, Wille SM, Walls ML. Patient-centered care, diabetes empowerment, and type 2 diabetes medication adherence among American Indian patients. Clin Diabetes 2017;35:281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schmittdiel JA, Steiner JF, Adams AS, et al. Diabetes care and outcomes for American Indians and Alaska natives in commercial integrated delivery systems: a SUrveillance, PREvention, and ManagEment of Diabetes Mellitus (SUPREME-DM) Study. BMJ Open Diabetes Res Care 2014;2:e000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shiyanbola OO, Nelson J. Illness perceptions, beliefs in medicine and medication non-adherence among South Dakota minority women with diabetes: a pilot study. S D Med 2011;64:365–368 [PubMed] [Google Scholar]
- 26. Wheat L, Roane TE, Connelly A, et al. Using a pharmacist-community health worker collaboration to address medication adherence barriers. J Am Pharm Assoc (2003) 2020;60:1009–1014 [DOI] [PubMed] [Google Scholar]
- 27. Chan SJ, Yeo HY. What are the instruments used to measure medication adherence in diabetes mellitus (DM) patients? A targeted literature review. Value Health 2018;21:S40 [Google Scholar]
- 28. Hu D, Juarez DT, Yeboah M, Castillo TP. Interventions to increase medication adherence in African-American and Latino populations: a literature review. Hawaii J Med Public Health 2014;73:11–18 [PMC free article] [PubMed] [Google Scholar]
- 29. Anghel LA, Farcas AM, Oprean RN. An overview of the common methods used to measure treatment adherence. Med Pharm Rep 2019;92:117–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Adams AS, Uratsu C, Dyer W, et al. Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA Intern Med 2013;173:54–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gast A, Mathes T. Medication adherence influencing factors: an (updated) overview of systematic reviews. Syst Rev 2019;8:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shiyanbola OO, Brown CM, Ward EC. “I did not want to take that medicine”: African-Americans’ reasons for diabetes medication nonadherence and perceived solutions for enhancing adherence. Patient Prefer Adherence 2018;12:409–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Newman PM, Franke MF, Arrieta J, et al. Community health workers improve disease control and medication adherence among patients with diabetes and/or hypertension in Chiapas, Mexico: an observational stepped-wedge study. BMJ Glob Health 2018;3:e000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Garcia ML, Castañeda SF, Allison MA, Elder JP, Talavera GA. Correlates of low-adherence to oral hypoglycemic medications among Hispanic/Latinos of Mexican heritage with type 2 diabetes in the United States. Diabetes Res Clin Pract 2019;155:107692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Huang J, Ding S, Xiong S, Liu Z. Medication adherence and associated factors in patients with type 2 diabetes: a structural equation model. Front Public Health 2021;9:730845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hernandez-Tejada MA, Campbell JA, Walker RJ, Smalls BL, Davis KS, Egede LE. Diabetes empowerment, medication adherence and self-care behaviors in adults with type 2 diabetes. Diabetes Technol Ther 2012;14:630–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schwartz DD, Stewart SD, Aikens JE, Bussell JK, Osborn CY, Safford MM. Seeing the person, not the illness: promoting diabetes medication adherence through patient-centered collaboration. Clin Diabetes 2017;35:35–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lauffenburger JC, Shrank WH, Bitton A, et al. Association between patient-centered medical homes and adherence to chronic disease medications: a cohort study. Ann Intern Med 2017;166:81–88 [DOI] [PubMed] [Google Scholar]
- 39. Kirkman MS, Rowan-Martin MT, Levin R, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care 2015;38:604–609 [DOI] [PMC free article] [PubMed] [Google Scholar]