Summary
An inability to proliferate at high temperatures typically gives viruses an attenuated phenotype. Here, we present a protocol to obtain and isolate temperature-sensitive (TS) SARS-CoV-2 strains via 5-fluorouracile-induced mutagenesis. We describe steps for the induction of mutations in the wild-type virus and selection of TS clones. We then show how to identify the mutations associated with the TS phenotype, following forward and reverse genetics strategies.
For complete details on the use and execution of this protocol, please refer to Yoshida et al. (2022).1
Subject areas: Microbiology, Molecular Biology
Graphical abstract

Highlights
-
•
Generation of a SARS-CoV-2 random mutation library by 5-fluorouracil
-
•
Isolation of viral clones and screening of TS phenotypes
-
•
Confirmation of temperature sensitivity by reverse genetics system
Publisher’s note: Undertaking any experimental protocol requires adherence to local institutional guidelines for laboratory safety and ethics.
An inability to proliferate at high temperatures typically gives viruses an attenuated phenotype. Here, we present a protocol to obtain and isolate temperature-sensitive (TS) SARS-CoV-2 strains via 5-fluorouracile-induced mutagenesis. We describe steps for the induction of mutations in the wild-type virus and selection of TS clones. We then show how to identify the mutations associated with the TS phenotype, following forward and reverse genetics strategies.
Before you begin
TS viruses show lower proliferation at high temperatures, and can thus be very helpful in the study of, for example, the function of the viral proteins. In addition, they have historically been used in the development of live vaccines since they generally tend to show an attenuated phenotype.2,3 We recently reported the potential use of SARS-CoV-2 TS strains for vaccine-related purposes.1 In the present paper, we focus on the process itself to generate them, and to characterize them, regardless of any specific application.
Institutional permissions
Since SARS-CoV-2 is classified as a Biosafety Level Class 3 (BSL3) virus,4 all experiments using it must be performed under the stipulated biosafety conditions. The cloning of genome fragments and reconstruction of mutant viruses are considered genetic modification experiments. Therefore, to perform them, it is necessary to obtain the approval of the committee responsible for genetic modification experiments in the corresponding country, abiding by the “Law Concerning the Conservation and Sustainable Use of Biological Diversity through Regulations on the Use of Living Modified Organisms” (in Japan) or its equivalent in the corresponding country.
Establishment of BHK-hACE2 cells
For the reconstruction of SARS-CoV-2 at low temperatures, we generated a cell line stably expressing the human ACE2 (hACE2) gene. We chose to use BHK cells due to their high transfection efficiency, and good viability at low temperatures (See related section, problem 5, and limitations).
-
1.Cloning hACE2 gene from 293T cells.
-
a.Culture 293T cells and BHK cells with optimal culture media (See materials and equipment).
-
b.Extract total RNA from 293T cells using TriReagent (Molecular Research Center, Cat# TR118), according to the manufacturer’s protocol.
-
c.Synthesize cDNA using SuperScript III First-Strand Synthesis System for RT-PCR with the oligo dT primer (Invitrogen, Cat# 18080051).
-
i.Mix 100 ng RNA from step 1-b with the reagents, following the table below.Note: Prepare the RNA/primer mixture with the following the table below.RNA/primer mixture
Reagent Amount 50 μM oligo(dT)20 1 μL 10 mM dNTP mix 1 μL RNA (100 ng) n μL DEPC-treated water Up to 10 μL -
ii.Incubate the mixture of RNA and primers at 65°C for 5 min.
-
iii.Chill on ice for more than 1 min.Note: Prepare cDNA synthesis master mix, following the table below.cDNA Synthesis master mix
Reagent Amount 10× RT buffer 2 μL 25 mM MgCl2 4 μL 0.1 M DTT 2 μL RNaseOUT™ (40 U/μL) 1 μL SuperScript™ III RT (200 U/μL) 1 μL -
iv.Add 10 μL of cDNA synthesis master mix to the RNA/primer mixture from step iii.
-
v.Incubate at 50°C for 50 min.
-
vi.Incubate at 85°C for 5 min.
-
vii.Chill on ice.
-
viii.Add 1 μL RNase H and incubate at 37°C for 20 min.
-
ix.Chill on ice.
-
i.
-
d.Amplify hACE2 cDNA using KOD One PCR Master Mix (TOYOBO, Cat#KMM-201) with the specific primers listed in the key resource table.Note: Prepare the PCR reaction master mix following the table below.PCR reaction mix
Reagent Volume KOD one master mix 25 μL Forward Primer 10 μM 1.5 μL Reverse Primer 10 μM 1.5 μL cDNA 1 μL Ultra-pure water 21 μL PCR conditionTemperature Time 98°C 10 s 68°C 30 s 35 cycles -
e.Digest the obtained fragments, and the PiggyBac cDNA Cloning and Expression Vector (System Biosciences, PB514B-2) with Xba I (NEB, Cat#R0145) and Not I (NEB, Cat#R0189) for 1 h at 37°C in 1× rCutSmart Buffer (NEB, Cat#B6004).
-
f.Ligate the two fragments using the DNA Ligation kit ver.2.1 (TAKARA Bio, Cat#6022). Mix 100 ng of the digested vector fragment and 33 ng digested insert fragments with ligation mix (Final volume: 20 μL).
-
g.Incubate at 16°C for 40 min.
-
h.Use 10 μL of the ligation reaction from step 1-g to transform JM109 competent cells (SMOBIO, Cat#CC0202) and follow typical molecular biology techniques to amplify and purify the constructed expression vector, using any commercially available kits.
-
a.
-
2.Transfection of the hACE2-coding PiggyBac vector together with the transposase expression vector (System Biosciences, PB200A-1) into BHK cells, using Polyethylenimine “Max” (PEI “Max”, Polysciences, Inc., Cat#24765).
-
a.Seed BHK cells (3 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before transfection and incubate at 37°C, 5% CO2 for 12–18 h.
-
b.Add 0.5 μg hACE2-coding PiggyBac vector and 0.2 μg transposase expression vector to 50 μL Opti-MEM (Gibco, Cat#31985062).
-
c.Add 6.3 μL of 1 mg/mL (9 times the amount of DNA) PEI “Max” solution to 50 μL Opti-MEM.
-
d.Mix the solutions from steps 2-b and 2-c, by gentle pipetting.
-
e.Incubate at room temperature for 15 min.
-
f.Add drop-wise to BHK cells and swirl to disperse.
-
g.Incubate at 37°C, 5% CO2 for 12–18 h.
-
h.Change the culture medium to the complete one, optimal for BHK cells, to reduce cell death by PEI “Max”.
-
i.Incubate at 37°C, 5% CO2, until cells become confluent.
-
a.
-
3.Selection of hACE2-positive cells with puromycin.
-
a.To determine the concentration of puromycin for the selection step, culture non-transfected-BHK cells in culture medium containing different concentrations of puromycin (Gibco, Cat#A1113803).Note: The concentration of puromycin should be optimized to obtain one concentration at which non-transfected cells die. In our case, it was 3 μg/mL.
-
b.Passage the potentially hACE2-transfected BHK cells from step 2-i.
-
c.Add the optimal concentration of puromycin (determined in step 3-a above) to potentially hACE2-transfected BHK cells, at each passage.
-
d.At each cell passage, verify the expression of mRuby, the fluorescent reporter protein originally encoded in the PiggyBac vector, indicative of successfully transfected cells.
-
e.After 2 weeks of selection, mRuby-positive cells should become dominant, so you can move on to the next step.
-
a.
-
4.Confirmation of the expression of hACE2 by western blotting.
-
a.Lyse a fraction of the established BHK-hACE2 cells and of the control non-transfected BHK cells (∼5 × 106 cells) with 2 mL of RIPA buffer (Thermo Scientific, Cat#89900) containing a proteinase inhibitor cocktail (Thermo Scientific, Cat#78430).
-
b.Mix 25 μL of the cell lysate with an equal volume of EzApply, containing dithiothreitol (ATTO, Cat#AE-1430) and boil at 95°C for 5 min.
-
c.Apply 5–20 μL/well of each sample to an e-PAGEL HR gel (ATTO, Cat#EHR-R1020L) to run an electrophoresis at 200 V for 60 min, using EzRun buffer (ATTO, Cat#AE-1410).
-
d.Blot samples to a 0.2 μm polyvinylidene fluoride (PVDF) membrane (Bio-Rad Laboratories, Inc., Cat#1704156) at 25 V for 7 min.
-
e.Wash the membrane with tris-buffer saline including 0.05% tween-20 (TBS-T).
-
f.Block the membrane with PVDF Blocking Reagent (TOYOBO, Cat#NYPBR01) at room temperature for 1 h.
-
g.Wash the membrane with TBS-T three times for 5 min each.
-
h.Soak the membrane in Can Get Signal Solution 1 (TOYOBO, Cat#NKB-201) with diluted anti-hACE2 antibody (1/1000) (Abcam, Cat#ab15348) or anti-β-actin antibody (1/1000) (Abcam, Cat#ab8226), and then incubate at room temperature for 1 h.
-
i.Wash the membrane with TBS-T, three times for 5 min each.
-
j.Soak the membrane in Can Get Signal Solution 2 (TOYOBO, Cat#NKB-301) with diluted anti-Rabbit antibody (1/5000) (Abcam, Cat#ab6721) or anti-Mouse IgG H&L antibody (1/5000) (Abcam, Cat#ab205719), and then incubate at room temperature for 1 h.
-
k.Wash the membrane with TBS-T three times for 5 min each.
-
l.Prepare the detection reagent by mixing an equal volume of solution A and solution B, included in the ECL Prime Western Blotting Detection Reagents (cytiva, Cat#RPN2232).
-
m.Take a picture using an available imager (we used ImageQuant LAS-500 system (cytiva)). See expected outcomes 1.
-
a.
Note: In the current protocol, we used a transposon-coding vector for hACE2 gene cloning, but other methods such as the use of retrovirus vectors, may also be used for the establishment of stable hACE2-expressing cells.
Preparation of agarose gel for the plaque isolation described in step 6 of the step-by-step method details
-
5.
Make a 2% (w/v) agarose solution by dissolving SeaPlaque Agarose (Lonza, #50100) with ultra-pure water or phosphate-buffered saline (PBS).
-
6.
Autoclave the solution at 121°C for 20 min.
-
7.
Make 25 mL-aliquots of the agarose solution into 50 mL-tubes before it solidifies, for storage.
-
8.
The agarose solution can be stored at 4°C until use for up to 1 month.
-
9.
Prior to use, remelt the agarose gel by heating at 80°C in an incubator or microwave oven.
-
10.
Once the agarose has melted, cool to 40°C and add an equal volume (25 mL) of Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 4% (v/v) fetal bovine serum (FBS) pre-warmed to 40°C (final concentration of agarose: 1% (w/v), FBS: 2% (v/v)).
-
11.
Keep the solution warm to prevent solidification by incubating at more than 40°C.
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| Anti-ACE2 antibody | Abcam | Cat# ab15348 |
| Goat Anti-Rabbit IgG H&L (HRP) | Abcam | Cat# ab6721 |
| Anti-beta actin antibody [mAbcam 8226] | Abcam | Cat# ab8226 |
| Anti-Mouse IgG H&L antibody | Abcam | Cat# ab205719 |
| Bacterial and virus strains | ||
| SARS-CoV-2: pre-alpha type, D614G, B-1 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603286 |
| SARS-CoV-2: gamma variant, TY7-501 strain | National Institute of Infectious Diseases | GISAID ID : EPI_ISL_833366 |
| SARS-CoV-2: delta variant, BK325 strain | Research Foundation for Microbial Diseases of Osaka University | N/A |
| SARS-CoV-2: omicron variant, TY38-873 strain | National Institute of Infectious Diseases | GISAID ID : EPI_ISL_7418017 |
| JM109 competent cells | SMOBIO | Cat# CC0202 |
| Chemicals, peptides, and recombinant proteins | ||
| 5-Fluorouracil | FUJIFILM Wako | Cat# 068-01401 |
| KOD One PCR Master Mix -Blue- | TOYOBO | Cat# KMM-201 |
| PrimeSTAR GXL DNA polymerase | TaKaRa Bio | Cat# R050A |
| Lipofectamin LTX Reagent with PLUS™ Reagent | Invitrogen | Cat# 15338100 |
| SeaPlaque Agarose | LONZA | Cat# 50100 |
| TriReagent | Molecular Research Center | Cat# TR118 |
| Dulbecco’s modified Eagle’s Medium (DMEM) | Sigma-Aldrich | Cat# D6429 |
| Minimum Essential Medium Eagle (MEM) | Sigma-Aldrich | Cat# M4655 |
| Dulbecco's phosphate-buffered saline (D-PBS) | Nacalai Tesque | Cat# 14249 |
| Fetal bovine serum (FBS) | Sigma-Aldrich | Cat# F7524 |
| Penicillin (100 U/mL), and streptomycin (0.1 mg/mL) (PS) | Gibco | Cat# 1154887 |
| Puromycin | Gibco | Cat# A1113803 |
| G418 Sulfate, Geneticin | Gibco | Cat# 10131027 |
| Opti-MEM | Gibco | Cat# 31985062 |
| XbaI | NEB | Cat# R0145 |
| NotI | NEB | Cat# R0189 |
| rCutSmart Buffer | NEB | Cat# B6004 |
| Polyethylenimine "Max" (PEI “Max”) | Polysciences, Inc. | Cat# 24765 |
| Canget signal solution I | TOYOBO | Cat# NKB-201 |
| Canget signal solution II | TOYOBO | Cat# NKB-301 |
| ECL Prime Western Blotting Detection Reagents | Cytiva | Cat# RPN2232 |
| RIPA buffer | Thermo Scientific | Cat# 89900 |
| proteinase inhibitor cocktail | Thermo Scientific | Cat# 78430 |
| Plus Protein Dual Color Standards | BIO-RAD | Cat#1610374 |
| EzApply | ATTO | Cat# AE-1430 |
| EzRun buffer | ATTO | Cat#AE-1410 |
| Trans-Blot Turbo Mini 0.2 μm PVDF Transfer Packs | Bio-Rad Laboratories, Inc. | Cat# 1704156 |
| 10×TBS | Bio-Rad Laboratories, Inc. | Cat# 1706435 |
| Tween-20 (polyoxyethylene sorbitan monolaurate) | Nacalai Tesque | Cat# 35624-15 |
| PVDF blocking reagent | TOYOBO | Cat# NYPBR01 |
| e-PAGEL HR gel | ATTO | Cat#EHR-R1020L |
| Critical commercial assays | ||
| QIAamp viral RNA mini kit | QIAGEN | Cat# 52904 |
| SuperScript™ III First-Strand Synthesis System for RT-PCR | Invitrogen | Cat# 18080051 |
| DNA Ligation Kit Ver.2.1 | TaKaRa Bio | Cat# 6022 |
| GenNext RamDA-seq Single Cell Kit | TOYOBO | Cat# RMD-101 |
| Nextera XT DNA Library Prep Kit | Illumina | Cat# FC-131-1096 |
| Nextera XT Index Kit v2 | Illumina | Cat# FC-131 |
| Deposited data | ||
| Viral genome sequence of B-1 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603286 |
| Viral genome sequence of A50-18 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603287 |
| Viral genome sequence of H50-11 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603288 |
| Viral genome sequence of L50-33 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603289 |
| Viral genome sequence of L50-40 strain | Hirotaka Ebina, Osaka University1 | NCBI: LC603290 |
| Experimental models: Cell lines | ||
| Green monkey: Vero cells | ATCC | Cat# CCL-81; RRID: CVCL_0059 |
| Green monkey: Vero cells with constitutive expression of TMPRSS II, VeroE6-TMPRSS II cells | Japanese Collection of Research Bioresources Cell Bank | Cat# JCRB1819; RRID: CVCL_YQ49 |
| Syrian hamster: BHK-21(C-13) cells | Japanese Collection of Research Bioresources Cell Bank | Cat# JCRB9020; RRID: CVCL_1915 |
| Syrian hamster: BHK-21(C-13) cells with constitutive expression of hACE2, BHK-hACE2 cells | This paper | N/A |
| Human 293T cells LX-293 | ATCC | CRL-3216 |
| Oligonucleotides | ||
| hACE2-cloning-Fw (AAATCTAGACGA TGTCAAGCTCTTCCTGGCTCCT) |
Hirotaka Ebina, Osaka University1 | N/A |
| hACE2-cloning-Rv (TTTGCGGCC GCTAAAAGGAGGTCTGAACATC ATCAGTGTTTTG) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-F1-Fw (CTATATAAGCAG AGCTCGTTTAGTGAACCGT attaaaggtttataccttcccaggtaac) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F1-Rv (cagattcaacttgcat ggcattgttagtagccttatttaaggctcctgc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F2-Fw (gcaggagccttaaataa ggctactaacaatgccatgcaagttgaatctg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F2-Rv (ggtaggattttccacta cttcttcagagactggttttagatcttcgcaggc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F3-Fw (gcctgcgaagatctaaaa ccagtctctgaagaagtagtggaaaatcctacc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F3-Rv (ggtgcacagcgcagcttct tcaaaagtactaaagg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F4-Fw (caccactaattcaaccta ttggtgctttggacatatcagcatctatagta gctggtgg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F4-Rv (gtttaaaaacgattg tgcatcagctgactg |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F5-Fw (cacagtctgtaccgtctgcgg tatgtggaaaggttatggctgtagttgtgatc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F5-Rv (gcggtgtgtacatagcct cataaaactcaggttcccaataccttgaagtg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F6-Fw (cacttcaaggtattggga acctgagttttatgaggctatgtacacaccgc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F6-Rv (catacaaactgccaccatca caaccaggcaagttaaggttagatagcactctag) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F7-Fw (ctagagtgctatctaacctt aacttgcctggttgtgatggtggcagtttgtatg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F7-Rv (ctagagactagtggcaataa aacaagaaaaacaaacattgttcgtttagttgttaac) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F8-Fw (gttaacaactaaacgaacaa tgtttgtttttcttgttttattgccactagtctctag) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F8-Rv (gcagcaggatccacaagaa caacagcccttgagacaactacagcaactgg) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F9-Fw (ccagttgctgtagttgtctca agggctgttgttcttgtggatcctgctgc) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F9-Rv (caatctccattggttgctcttcatc) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F10-Fw (gatgaagagcaaccaatggagattg) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-F10-Rv (GGAGATGCCATG CCGACCCtttttttttttttttttttttttttgtca ttctcctaag) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-Linker-Fw (cttaggagaatgacaaa aaaaaaaaa aaaaaaaaaaaaaGGGTCGG CATGGCATCTCC) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-Linker-Rv (gttacctgggaaggta taaacctttaatACGGTTCACTAAACGA GCTCTGCTTATATAG) |
Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-TS-F6-Rv (catacaaactgccacta tcacaaccaggcaagttaaggttagatagcactctag) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-TS-F7-Fw (ctagagtgctatctaaccttaa cttgcctggttgtgatagtggcagtttgtatg) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-4052T-Fw (tatattgacattaatggca attttcatccagattctgcca) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-4052T-Rv (ttgccattaatgtcaatataa agtaacaagttttctgtga) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-18782T-Fw (tgattgatgttcaacaatgg gtttttacaggtaacctaca) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-18782T-Rv (ccattgttgaacatcaat cataaacggattatagacgtaa) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-19285A-Fw (aaccttaacttgcctggttg tgatagtggcagtttgtatg) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-19285A-Rv (caaccaggcaagttaaggt tagatagcactctagtgtcaa) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-19550T-Fw (tctcgatgcttataacatga tgatctcagttggctttagc) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-19550T-Rv (tcatgttataagcatcgagata caatctgtactcattagc) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-20857A-Fw (ctgtaccctataatatga gaattatacattttggtgctggttct) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-20857A-Rv (tctcatattatagggtacagc taatgttaatgtgtttaaa) |
Hirotaka Ebina, Osaka University1 | N/A |
| CoV-2-G2-Fw (cggcagtgaggacaatcagacaactac) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-G2-Rv (ggcttagcataattagctatagtatcccaagggac) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-G6-Fw (tgtagatgatatcgtaaaaacagatggtacac) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-G6-Rv (aacgtgttatacacgtagcagactttagtggtac) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-G7-Fw (aaaggttcaacacatggttgttaaagctgc) | Yoshiharu Matsuura, Osaka University5 | N/A |
| CoV-2-G7-Rv (cgtacactttgtttctgagagagggtc) | Yoshiharu Matsuura, Osaka University5 | N/A |
| covid-dp-4655-4683r (ggcactttgagagatctcatataccgagc) | Yoshiharu Matsuura, Osaka University5 | N/A |
| covid-dp-18160-18186f (gttgacatacctggcatacctaaggac) | Yoshiharu Matsuura, Osaka University5 | N/A |
| covid-dp-19712-19738r (caacaccatcaacttttgtgtaaacag) | Yoshiharu Matsuura, Osaka University5 | N/A |
| covid-dp-20470-20496f (gcgcaaacaggttcatctaagtgtgtg) | Yoshiharu Matsuura, Osaka University5 | N/A |
| Recombinant DNA | ||
| PiggyBac cDNA Cloning and Expression Vector | System Biosciences | PB514B-2 |
| transposase expression vector | System Biosciences | PB200A-1 |
| Software and algorithms | ||
| CLC Genomics Workbench 21 | QIAGEN | N/A |
| Other | ||
| ImageQuant LAS-500 system | Cytiva | N/A |
| MiSeq platform | Illumina | N/A |
Materials and equipment
Medium for the maintenance of Vero, VeroE6-TMPRSS2, and 293T cells
| Reagent | Final concentration | Amount |
|---|---|---|
| Dulbecco’s Modified Eagle’s Medium (DMEM) | N/A | 445 mL |
| Heat-inactivated fetal bovine serum (FBS) | 10% (v/v) | 50 mL |
| Penicillin-Streptomycin (10,000 U/mL) | Penicillin (100 U/mL) Streptomycin (100 μg/mL) |
5 mL |
| G418 Sulfate, Geneticin | 1 mg/mL | N/A |
| Total | N/A | 500 mL |
Notes: Culture medium may be stored at 4°C, up to one month. G418 should be included in medium only for maintenance of VeroE6-TMPRSS2 cells.
Medium for the maintenance of BHK and BHK-hACE2 cells
| Reagent | Final concentration | Amount |
|---|---|---|
| Minimum Essential Medium Eagle (MEM) | N/A | 445 mL |
| Heat-inactivated fetal bovine serum (FBS) | 10% (v/v) | 50 mL |
| Penicillin-Streptomycin (10,000 U/mL) | Penicillin (100 U/mL) Streptomycin (100 μg/mL) |
5 mL |
| Puromycin | 3 μg/mL ∗ | N/A |
| Total | N/A | 500 mL |
Notes: Culture medium may be stored at 4°C, up to one month. Puromycin should be included in medium only for maintenance of BHK-hACE2 cells. The concentration must be optimized to one at which non-transduced cells die.
Step-by-step method details
Induction of mutations in the wild type virus
Timing: 1 week
The aim of this step is to generate a virus library containing mutated viruses.
-
1.
Seed Vero cells (5 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before viral infection and incubate at 37°C, 5% CO2 for 12–18 h.
-
2.Induce mutations.
-
a.Viral infection.
-
i.Remove the medium.
-
ii.Infect the cells by adding a small amount of medium (200–500 μL) containing the virus with an infectious titer of about 1 × 106 wild type viruses (Multiplicity of infection (MOI) is 1.0.
-
iii.Incubate at 37°C, 5% CO2 for 1 h to allow the virus to adsorb.
-
i.
-
b.Mutation induction.
-
i.Remove the supernatant.Note: Remove viral supernatant with a micropipette, not with an aspirator, to avoid producing aerosols. Disinfect infectious wastewater by adding a 500–1000 ppm sodium hypochlorite solution. Autoclave all instruments suspected to be virus-contaminated.
-
ii.Add 2 mL of fresh pre-warmed DMEM containing 10% (v/v) FBS and 400 μg/mL 5-FU (FUJIFILM Wako, Cat#068-01401) to induce mutations.
-
iii.Incubate at 32°C, 5% CO2 for 24–36 h to permit temperature sensitive virus to proliferate.
-
iv.Collect the supernatant.
-
v.Centrifuge and collect the supernatant containing mutated viruses.Note: The concentration of 5-FU should be optimized depending on the sensitivity of the cells and viruses. The growth rate of 5-FU-treated viruses should be lower than that of non-treated ones. A previous study showed that a concentration of 350–450 μg/mL of 5-FU was enough to in inhibit murine hepatitis virus amplification by 90%.6 We used 400 μg/mL. For other viruses, we recommend evaluating viral amplification under several 5-FU concentrations conditions that do not significantly affect the host cells.
-
i.
-
a.
-
3.
Seed Vero cells (5 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before viral infection, and incubate at 37°C, 5% CO2 for 12–18 h.
-
4.Amplification of the mutated viruses at a lower temperature.
-
a.Infect the pre-seeded Vero cells by adding 50 μL of the mutated viruses obtained in step 2-b-v.
-
b.Incubate at 32°C, 5% CO2 for 3–4 days, until cytopathic effect (CPE) is observed using an optical microscope.Note: Virus passaging should be performed when CPE is observed.
-
c.Collect the supernatant.
-
d.Centrifuge and collect the supernatant. This virus solution will be used for TS clones’ selection.
- e.
-
a.
Selection of TS clones
Timing: 2 weeks
The aim of this step is to isolate a large number of single virus clones and to screen for the TS phenotype.
-
5.
Seed Vero cells (5 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before viral infection and incubate at 37°C, 5% CO2 for 12–18 h.
-
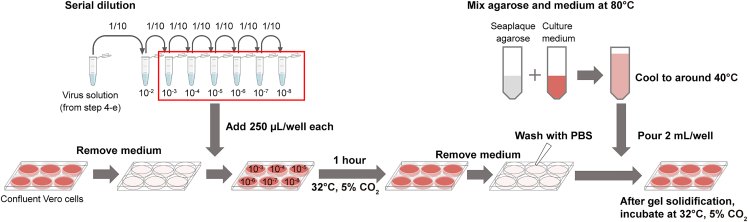
6.Plaque formation (See Figure 1).
-
a.Make 10-fold serial dilutions of the mutated virus solution obtained in step 4 (10−3–10−8).
-
b.Remove the medium from the cultured Vero cells of step 5.
-
c.Add enough volume of the diluted virus solutions (250–500 μL) to the cells, to prevent them from drying during adsorption.
-
d.Incubate at 32°C, 5% CO2 for 1 h to allow the virus to adsorb.Note: In the procedure for plaque formation, to prevent cells from drying out during virus adsorption, rock plates occasionally.
-
e.Remove the virus solution.
-
f.Wash the cells once with PBS.
-
g.Pour 2 mL of fresh medium containing 1% (w/v) SeaPlaque agarose onto the cells and wait until it solidifies. Viral spread is inhibited by SeaPlaque agarose, which allows infection to progress only from infected cells to neighboring cells, resulting in the formation of plaques.Note: Agar solutions should be kept at approximately 40°C to prevent solidification and not to kill the cells.
-
h.Incubate at 32°C, 5% CO2 for 4–5 days until plaques are clearly visible.
-
a.
-
7.
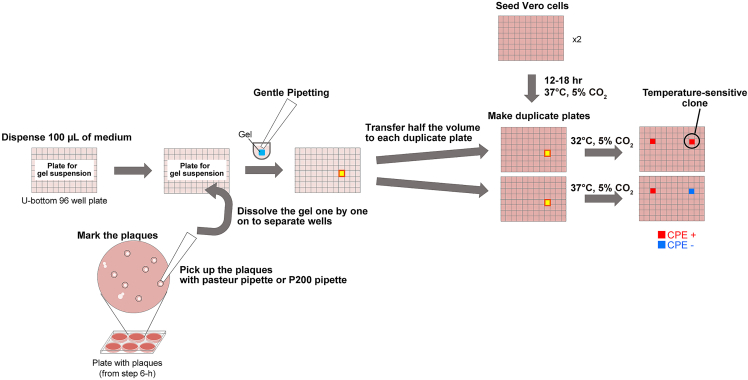
Seed Vero cells (2.5 × 105 cells/mL, 100 μL/well) in 96-well plates 1 day before plaque picking, and incubate at 37°C, 5% CO2 for 12–18 h. Make sure to prepare double number of plates (See Figure 2).
-
8.Plaque picking (See Figures 2 and 3).
-
a.Dispense 100 μL of Vero cell-optimal medium into each well of new 96-well plates (U bottom).
-
b.Identify and mark the plaques from the underside of the plate (Figure 3).
-
c.Pick up the plaques with a Pasteur pipette or pipette tip.Note: For the isolation of single virus clones, care should be taken not to pick overlapping plaques. Therefore, it is preferable to make multiple dilutions of the virus solution to form 10–20 plaques in one well.
-
d.Suspend the pieces of gel by adding them one by one onto separate wells containing medium (in the 96-well plates prepared in step 8-a).
-
a.
-
9.Checking temperature sensitivity (related to problem 1, Figure 2, expected outcomes 2).
-
a.Add 50 μL of the content of each well from step 8-d to the Vero cells on the two 96-well plates prepared in step 7, following the same layout so as to obtain duplicate plates (Figure 2, expected outcomes 2).
-
b.Incubate one of the duplicate plates at 32°C, and other plate at 37°C, 5% CO2 for at least 5 days to reduce the possibility of false positives.
-
c.Check each individual well for the presence of CPE.Note: If the virus shows a temperature-sensitive phenotype, it will be CPE-positive at 32°C and CPE-negative at 37°C (expected outcomes 2).
-
d.Collect the temperature-sensitive viruses from the CPE-positive wells of the plates incubated at 32°C.
-
e.Store at −80°C.
-
a.
-
10.
(Additional) To isolate single clones of temperature-sensitive viruses, repeat steps 5–9, two or three times.
Note: Performing step 10 is recommended to minimize contamination and ensure viral clonality.
Figure 1.
Schematic figure of steps 5 to 6
Figure 2.
Schematic figure of steps 7 to 9
Figure 3.
Plaque-picking procedure
Identification of TS-responsible substitutions
Timing: 4–6 weeks
The aim of this step is to identify the mutations responsible for the TS phenotype by obtaining revertants and checking their genomic sequences.
-
11.
Extract RNA from the 140 μL of the viruses obtained in steps 9-d to 10 using TriReagent (Molecular Research Center, Cat# TR118) or a QIAamp viral RNA mini kit (Qiagen, Cat# 52904), without carrier RNA, according to the manufacturers’ protocols.
-
12.
Determine the entire sequences of each viral clone via next generation sequencing, after preparing the samples with any appropriate commercially available kits.
Note: For next generation sequencing, we requested the NGS core facility of the Genome Information Research Center at the Research Institute for Microbial Diseases of Osaka University for the processing and sequencing of the SARS-CoV-2 viruses. Synthesis of cDNA was performed using GenNext RamDA-seq Single Cell Kit (TOYOBO, Cat#RMD-101). Illumina library construction was performed using Nextera XT DNA Library Prep Kit (Illumina, Cat#FC-131-1096) and Nextera XT Index Kit v2 (Illumina, Cat#FC-131). Sequencing was performed on the MiSeq platform (Illumina) with 150 bp paired-end mode. The obtained reads were analyzed using CLC Genomics Workbench 21.
-
13.
Compare full genome sequence with parental strain and identify mutations.
-
14.
Seed Vero cells (2.5 × 105 cells/mL, 100 μL/well) in 96-well plates (at least 2 plates for each temperature to be tested in step 16), 1 day before virus infection, and incubate at 37°C, 5% CO2 for 12–18 h.
-
15.
Add the virus obtained in steps 9-d to 10, to all wells at a MOI = 1.0–10.0.
-
16.
Incubate at non-permissive temperatures (in this case 37, 38 or 39°C) for 2–5 days.
Note: We recommend to try this step at 37, 38, and 39°C. Because the temperature sensitivity of the virus strains might vary, there is a possibility that revertants emerge only at higher temperatures (38°C–39°C) (See problem 4).
-
17.
Collect cell culture aliquots from CPE-positive wells which may include revertants (See problems 3 and 4, limitations).
-
18.
Extract RNA from the samples obtained in step 17 using TriReagent (Molecular Research Center, Cat# TR118) or a QIAamp viral RNA mini kit (Qiagen, Cat# 52904), according to the manufacturers’ protocols.
-
19.
Synthesize cDNA using the SuperScript™ III First-Strand Synthesis System for RT-PCR (Invitrogen, Cat# 18080051) with random primers, according to the manufacturer’s protocol.
-
20.
Amplify the genomic regions surrounding each mutation of interest via PCR using specific primers (See key resources table).
-
21.
Determine the sequence of the PCR products through Sanger sequencing and compare them to those of the corresponding parental TS strains.
Note: The primers we used are listed in the Key Resources Table. Sanger sequencing was requested to Azenta Co., Ltd. (Japan).
Note: If mutations are found to have changed back to the wild type, these could be the responsible mutations. However, viruses may not be typical revertants whose mutations change back to the wild type sequence. For example, the reversions may involve amino acids with similar polarity in the positions initially affected or in their interacting counterparts within the 3D structure of the protein. See problems 3 and 4.
Note: The sample size to obtain revertants depends on the characteristics of each TS strain, the conditions of the experiments, such as MOI and culture temperature (pressure). In our study, when culturing at 37°C and MOI = 1.0, the frequency of revertant-containing wells was 15.2% (35/230) and 0.9% (2/230) for the highest and lowest strains, respectively. Therefore, you need to try to analyze a considerable number of wells.
Reconstruction of temperature-sensitive virus by reverse genetics
Timing: 2.5 weeks
The aim of this step is to confirm whether the mutations observed in the revertants were TS-responsible mutations, and to construct recombinant strains following reverse genetics methods (e.g., circular polymerase extension reaction (CPER)5 or bacterial artificial chromosome (BAC) system8). We utilized CPER with few modifications, as described below (See Figure 4).
CRITICAL: Torii et al. transfected the CPER products to tetracycline-inducible ACE2- and TMPRSS-expressing IFNAR1-deficient HEK293 (HEK293-3P6C33) cells.5 However, in our study, viral reconstruction was not successful at 32°C with these cells. Alternatively, to obtain TS-recombinant viruses, we used BHK-hACE2 cells because they can replicate with high transfection efficacy even at low temperatures (See also problem 5, limitations).
-
22.
Seed BHK-hACE2 cells (1 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before transfection and incubate at 37°C, 5% CO2 for 12–18 h.
Note: Establishment of the BHK-hACE2 cell line is described in the “before you begin” section.
-
23.
Assemble SARS-CoV-2 gene fragments by CPER using PrimeSTAR GXL DNA polymerase (Takara Bio, Cat# R050A), according to Torii et al., 2021.5 Mix the fragments with the polymerase and perform the reaction following the information on the table below.
CPER reaction mix
| Reagent | Volume |
|---|---|
| F1+2 | 0.1 pmol |
| F3 | 0.1 pmol |
| F4 | 0.1 pmol |
| F5 | 0.1 pmol |
| F6 | 0.1 pmol |
| F7 | 0.1 pmol |
| F8 | 0.1 pmol |
| F9 | 0.1 pmol |
| F10-12 | 0.1 pmol |
| PrimeStar GXL | 2 μL |
| 5×GXL buffer | 10 μL |
| dNTPs | 4 μL |
| Ultra-pure water | Up to 50 μL |
Thermal cycler condition
| Temperature | Time | |
|---|---|---|
| 98°C | 2 min | |
| 98°C | 10 s | 20 cycles |
| 55°C | 15 s | |
| 68°C | 25 min | |
| 68°C | 25 min |
-
24.
Use 25 μL of the 50 μL assembled circular-DNA reaction mix from step 23, without prior purification, to transfect BHK-hACE2 cells, using Lipofectamine LTX Reagent with PLUS™ Reagent (Invitrogen, Cat# 15338100) according to the manufacture’s protocol.
-
25.
Incubate at 32°C, 5% CO2, for 7 days.
-
26.
Make sure to seed VeroE6-TMPRSS2 cells (5 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before virus recovery, and incubate at 37°C, 5% CO2 for 12–18 h.
-
27.
Collect the supernatants.
-
28.
To confirm the proper reconstruction of SARS-CoV-2 by CPE, use 2 mL of these supernatants to infect VeroE6-TMPRSS2 cells and incubate at 32°C, 5% CO2, for up to 7 days.
Note: Since there may be less virus in the supernatant after transfection, VeroE6-TMPRSS2, which is more sensitive to SARS-CoV-2, is useful for the initial virus amplification. Then, reconstructed viruses can be passaged in Vero cells to be used in various assay.
-
29.
If the recombinant virus strains were successfully reconstructed, CPE will be observed (expected outcomes 3).
-
30.
Make sure to seed Vero cells (5 × 105 cells/mL, 2 mL/well) in 6-well plates, 1 day before virus infection, and incubate at 37°C, 5% CO2 for 12–18 h.
-
31.
Collect supernatants and transfer 10–50 μL to the newly prepared Vero cells to amplify the recombinant viruses.
-
32.
Incubate at 32°C for 3–4 days, until CPE was observed.
-
33.
Collect the supernatants containing the recombinant viruses.
-
34.
Evaluate growth kinetics of recombinant viruses at 32°C–39°C, to confirm their temperature sensitivity (expected outcomes 41).
Figure 4.
Schematic figure of steps 22 to 31
Expected outcomes
Expected outcome 1
The expression of hACE2 in BHK-hACE2 cells, constructed in the “before you begin” section, was confirmed by Western blotting shown in step 4 of the same section. BHK and BHK-hACE2 cells were lysed with RIPA buffer and total cell lysates were used to run an SDS-PAGE and then analyzed by Western blotting. Beta-actin was used as an internal control for protein loading. hACE2 protein was not observed in the parental BHK cells using 20 μL cell lysate, but it was detected in BHK-hACE2 cells using 5 μL of lysate (Figure 5). Therefore, BHK cells stably expressing hACE2 were successfully constructed, and used for reconstruction of SARS-CoV-2.
Figure 5.
(Expected outcomes 1): hACE2 expression of established BHK-hACE2 cell line
M: Precision Plus Protein Dual Color Standards (BIO-RAD, Cat#1610374).
Expected outcome 2
In order to screen the wells containing TS strains, CPE was assessed after incubation at lower and higher temperatures, as described in step 9 (see also the scheme related to Figure 2). The plaque-containing pieces of gel were suspended with medium in individual wells. Then, the medium was divided into two 96-well plates containing confluent Vero cells, for culture at 32°C and 37°C. The cells were fixed with 10% formalin and stained with crystal violet after incubating for 4–5 days (Figure 6). The assessment of CPE was determined by cell detachment. The wells where CPE was observed at 32°C but not at 37°C (framed in red squares in the figure) are expected to contain TS strains.
Figure 6.
(Expected outcomes 2): First screening of the temperature-sensitive mutants
Vero cells were infected with the viruses at 32°C and 37°C in duplicate. Non-temperature-sensitive viruses induce cytopathic effects at both 32°C and 37°C, while temperature-sensitive mutants do at 32°C but not at 37°C (Red boxes). d.p.i.: Days-post infection.
Expected outcomes 3 and 4
In step 29, to amplify viruses and confirm whether CPER was successful or not, we added the supernatant of transfected-BHK- hACE2 cells to VeroE6 cells and checked for CPE development. As shown in Figure 7 (expected outcomes 3), typical CPE was observed when viruses were properly reconstructed, or cells survived when viral reconstruction failed. In step 34, evaluation of the growth kinetics of these recombinant viruses at several temperatures was performed. Recombinant viruses which have predicted-TS mutations were added to pre-seeded Vero cells at MOI = 0.01 and incubated at 32, 37, or 39°C. As shown in Figure 8 (expected outcomes 4), these recombinant viruses showed a wide spectrum of temperature-sensitive phenotypes. These results suggested that the mutations they have are responsible for the temperature sensitivity. See also figure 2B of our previous report.1
Figure 7.
(Expected outcomes 3): Cytopathic effects of a CPER-reconstructed virus in VeroE6-TMPRSS2 cells
Scale bar: 100 μm.
Figure 8.
(Expected outcomes 4): Growth kinetics of recombinant TS viruses1
Limitations
You need multiple CO2 incubators in a BSL3 facility for the isolation of temperature-sensitive SARS-CoV-2, which is classified as a class 3 virus. If you apply this protocol to another kind of virus, you need a cell culture system to amplify the virus in vitro that can result in visible CPE to facilitate evaluation. Also, if you want to obtain recombinant TS viruses, you need a cell line which is able to proliferate at 32°C and is able to be infected by the virus.
Troubleshooting
Problem 1
Inability to obtain any TS viruses when you add 5-FU (related to step 2).
Potential solution
-
•
The concentration of 5-FU and the duration of treatment should be optimized. Viral growth in drug-treated infected cells should preferably be slower than in non-treated cells. We obtained TS mutant strains by adding 400 μg/mL of 5-FU. In one previous study, TS mutants of a mouse hepatitis virus were obtained by adding 150 μg/mL of 5-FU, a concentration shown to inhibit 99% of the viral amplification.7 Another previous study used 350–450 μg/mL of 5-FU, a concentration shown to inhibit 90% of the viral proliferation.6
- •
Problem 2
The TS phenotype is lost while you passage the TS mutants (related to all steps).
Potential solution
-
•
Non-TS viruses may become dominant in the viral pool if cloning was not complete. Also, virulent reversion may occur if culture temperatures were to be a pressure. Repeat plaque isolation steps to pick up TS viruses and passage them at the lowest temperature that cells can proliferate.
Problem 3
Unsuccessful attempts to obtain typical revertants, whose mutations change back to the wild type sequence, when you incubate the TS mutants at high temperatures (related to step 17).
Potential solution
-
•
Multiple mutations may be involved in the TS phenotype. You may find other TS-responsible mutations.
-
•
Additional mutations which increase viral proliferation may occur in genomic regions distant from each of the original TS-associated mutations, leading to CPE development. Therefore, in order to generate typical revertants, we recommend making several attempts.
Problem 4
If their temperature sensitivity is not clearly evident, non-reverted viruses may proliferate and cause CPE even at 37°C (false-positive). In this case, they cannot be distinguished from real revertants by CPE observation (related to steps 17 to 21).
Potential solution
-
•
Raise the incubation temperature. For H50-11, a SARS-CoV-2 TS strain we isolated, proliferation was slow at 37°C,1 but the number of false-positives decreased when we tested at 38°C.
Problem 5
Failure to recover CPER-reconstructed TS viruses (related to step 29). This may be due to the PCR reaction, the transfection procedure, or the viral culture conditions, such as cell strain and incubation temperature.
Potential solution
-
•
Optimize the CPER protocol according to Torii et al., 2021.5
-
•
Lower culture temperature for efficient recovery of TS strains.
-
•
Change the cell strain. Cells for viral recovery should be able to replicate and show high transfection efficacy at the target temperatures.
-
•
Change the transfection reagent. However, polyethylenimine is not recommended because of its relatively high cytotoxicity.
-
•
To efficiently collect the viruses, freeze-thaw of the culture plates could be performed once. Viral particles in the cells can also be collected because this procedure breaks the cell membrane.
Resource availability
Lead contact
Further information and requests for resources and reagents should be directed to and will be fulfilled by the lead contact, Hirotaka Ebina (hebina@biken.osaka-u.ac.jp).
Materials availability
BHK-hACE2 cells generated in this study are held in-house and are available under reasonable request.
Acknowledgments
We appreciate the assistance from Mitsuyo Kosaka and Manae Morishima (BIKEN). The authors thank Shiho Torii, Chikako Ono, and Yoshiharu Matsuura for their CPER technical support. Also, we would like to thank the NGS Core Facility of the Genome Information Research Center at the Research Institute for Microbial Diseases of Osaka University for their support with next-generation sequencing analyses. This work was supported by The Research Foundation for Microbial Diseases of Osaka University (BIKEN) and the Japan Agency for Medical Research and Development (AMED) under Grant Number JP20pc0101047.
Author contributions
H.E., S.O., and A.Y. established the majority of the experimental procedures. M.M. established the BHK-hACE2 cell line. A.Y., S.O., and P.M. wrote the original manuscript and H.E. revised it.
Declaration of interests
S.O., A.Y., P.M., M.M., and H.E. are employed by BIKEN. We report that S.O., A.Y., and H.E. are named on a patent that describes the use of the TS mutants as vaccine candidates, currently being filed by BIKEN. H.E. holds a managerial position at BIKEN.
Data and code availability
The data from this report are available from the lead contact upon request. The viral genome sequences of the TS mutants isolated in this study have been deposited at the National Center for Biotechnology Information (Accession numbers for B-1, A50-18, H50-11, L50-33, and L50-40 are GenBank: LC603286, LC603287, LC603288, LC603289, and LC603290, respectively). This study did not require any code.
References
- 1.Yoshida A., Okamura S., Torii S., Komatsu S., Miyazato P., Sasaki H., Ueno S., Suzuki H., Kamitani W., Ono C., et al. Versatile live-attenuated SARS-CoV-2 vaccine platform applicable to variants induces protective immunity. iScience. 2022;25:105412. doi: 10.1016/j.isci.2022.105412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Komase K., Nakayama T., Iijima M., Miki K., Kawanishi R., Uejima H. The phosphoprotein of attenuated measles AIK-C vaccine strain contributes to its temperature-sensitive phenotype. Vaccine. 2006;24:826–834. doi: 10.1016/j.vaccine.2005.06.036. [DOI] [PubMed] [Google Scholar]
- 3.Hilimire T.A., Nogales A., Chiem K., Ortego J., Martinez-Sobrido L. Increasing the safety profile of the master donor live attenuated influenza vaccine. Pathogens. 2020;9:86. doi: 10.3390/pathogens9020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Laboratory Biosafety Guidance Related to Coronavirus Disease (COVID-19): Interim Guidance (who.Int) 2021. https://www.who.int/publications/i/item/WHO-WPE-GIH-2021.1
- 5.Torii S., Ono C., Suzuki R., Morioka Y., Anzai I., Fauzyah Y., Maeda Y., Kamitani W., Fukuhara T., Matsuura Y. Establishment of a reverse genetics system for SARS-CoV-2 using circular polymerase extension reaction. Cell Rep. 2021;35:109014. doi: 10.1016/j.celrep.2021.109014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaad M.C., Stohlman S.A., Egbert J., Lum K., Fu K., Wei T., Jr., Baric R.S. Genetics of mouse hepatitis virus transcription: identification of cistrons which may function in positive and negative strand RNA synthesis. Virology. 1990;177:634–645. doi: 10.1016/0042-6822(90)90529-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haspel M.V., Lampert P.W., Oldstone M.B. Temperature-sensitive mutants of mouse hepatitis virus produce a high incidence of demyelination. Proc. Natl. Acad. Sci. USA. 1978;75:4033–4036. doi: 10.1073/pnas.75.8.4033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye C., Chiem K., Park J.-G., Oladunni F., Platt R.N., Anderson T., Almazan F., de la Torre J.C., Martinez-Sobrido L. Rescue of SARS-CoV-2 from a single bacterial artificial chromosome. mBio. 2020;11 doi: 10.1128/mBio.02168-20. e02168-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data from this report are available from the lead contact upon request. The viral genome sequences of the TS mutants isolated in this study have been deposited at the National Center for Biotechnology Information (Accession numbers for B-1, A50-18, H50-11, L50-33, and L50-40 are GenBank: LC603286, LC603287, LC603288, LC603289, and LC603290, respectively). This study did not require any code.