Abstract
Background
With a dramatic increase in elderly population worldwide, the prevalence of degenerative spine disease is steadily rising. Even though the entire spinal column is affected the problem is more commonly seen in the lumbar, cervical spine and to some extent the thoracic spine. The treatment of symptomatic lumbar disc or stenosis is primarily conservative with analgesics, epidural steroids and physiotherapy. Surgery is advised only if conservative treatment is ineffective. Conventional open microscopic procedures even though are still a gold standard, have the disadvantages of excessive muscle damage and bone resection, epidural scarring along with prolonged hospital stay and increased need of postoperative analgesics. Minimal access spine surgeries minimize surgical access related injury by minimizing soft tissue and muscle damage and also bony resection thus preventing iatrogenic instability and unnecessary fusions. This leads to good functional preservation of the spine and enhances early postoperative recovery and early return to work. Full endoscopic spine surgeries are one of the more sophisticated and advanced form of MIS surgeries.
Purpose
Full endoscopy has definitive benefits over conventional microsurgical techniques. These include better and clear vision of the pathology due to presence of irrigation fluid channel, minimal soft tissue and bone trauma, better and relatively easy approach to deep seated pathologies like thoracic disc herniations and a possibility to avoid fusion surgeries. The purpose of this article is to describe these benefits, give an overview of the two main approaches - transforaminal and interlaminar, their indications, contraindications and their limitations. The article also describes about the challenges in overcoming the learning curve and its future prospectives.
Conclusion
Full endoscopic spine surgery is one of the fastest growing technique in the field of modern spine surgery. Better intraoperative visualization of the pathology, lesser incidence of complications, faster recovery time, less postoperative pain, better relief of symptoms and early return to activity are the main reasons behind this rapid growth. With better patient outcomes and reduced medical costs, the procedure is going to be more accepted, relevant and popular procedure in future.
Keywords: Full endoscopic spine surgery, Interlaminar, Transforaminal, PELD, Minimally invasive spine surgery disc prolapse, Spinal stenosis, Decompression, Discectomy, Unilateral laminotomy for bilateral decompression
1. Introduction
With a dramatic increase in elderly population worldwide, the prevalence of degenerative spine disease is steadily rising. Even though the entire spinal column is affected the problem is more commonly seen in the lumbar and cervical spine and to some extent the thoracic spine. The treatment of symptomatic lumbar disc or stenosis is primarily conservative with analgesics, epidural steroids and physiotherapy. Surgery is advised only if conservative treatment is ineffective. Conventional open microscopic procedures have the disadvantages of excessive muscle damage, bone resection and epidural scarring along with prolonged hospital stay and increased need of postoperative analgesics. The primary focus of modern spine surgery is to minimize surgical access related injury by minimizing soft tissue and muscle damage and to minimize bony resection thus preventing iatrogenic instability and unnecessary fusions. This leads to good functional preservation of the spine and enhances early postoperative recovery.
In an era of MIS surgeries where micro decompressions using tubular retractor systems are still a gold standard, endoscopic spine surgeries have started gathering attention and are becoming popular. Presently there are two popular endoscopic techniques. Full endoscopy and unilateral biportal endoscopy (UBE) technique. UBE surgery is a two-portal technique, one portal is for visualization using an arthroscope and another portal for passage of surgical instruments. UBE technique works by triangulation similar to knee joint arthroscopy and conventional open surgery instruments along with arthroscopic drill are used to perform the procedure. The focus of this article is to discuss about the Full endoscopic (Uniportal)technique which can be considered as a more sophisticated and advanced form of endoscopic surgeries. A full endoscope is actually a smart tube in which high definition optics, irrigation channel and a working channel for passage of surgical instruments, are all integrated together in one tube to offer trifold benefits of magnification, illumination and clear field of vision. The purpose is to improve the success rate while minimizing complications. In comparison to traditional open surgery, endoscopic spine surgery provides advantages such as less soft tissue trauma, reduced blood loss, decreased damage to the epidural blood supply and consequent epidural fibrosis, shorter hospital stays, shorter time to return to work.1, 2, 3, 4, 5
2. Benefits of full endoscopy
Full endoscopic surgeries have numerous advantages over conventional microscopic techniques.
As compared to the other techniques, the size of skin incision is the smallest (8–10 mm depending on the size on endoscope used), irrespective of the patients body structure and size,. There is no stripping of the muscles from the lamina and the spinous process. Most herniations are effectively removed without damaging any important structure in the transforaminal (TF) approach or only through a small slit made in the ligamentum flavum in interlaminar approach.
The real trump card is the presence normal saline irrigation which offers three advantages. It maintains a clear field of vision by washing all the debris and blood clots thus helping in minimizing intraoperative complications like dural tears. The fluid pressure has a hemostatic effect and lastly the continuous normal saline lavage reduces the chances of infection.6
Thirdly, compared to a microscope which offers a birds eye view, the surgeons eye is placed at the tip of the endoscope which is placed very close to the target pathology. This offers definitive advantage especially in difficult to access deep seated areas like the thoracic spine pathologies where approach related morbidity can be significant. Full endoscopy can prevent opening of the chest cavity to access thoracic disc herniations by either posterolateral transforaminal (over the rib) approach for lateral thoracic discs or a trans thoracic retropleural approach (under the rib approach) for a large central thoracic herniation. Both the approaches avoid opening of parietal pleura and prevent the need of a chest drain7,8
Lastly Full endoscopy provides the possibility to avoid unnecessary fusions9,10 eg: a large central disc herniation at upper lumbar level if approached by conventional interlaminar approach may need facet joint resection. Transforaminal approach where the endoscope passes under the facet joint will be able to remove the central herniation effectively without the need to retract the neural tissue (Fig. 1, Fig. 2, Fig. 3).
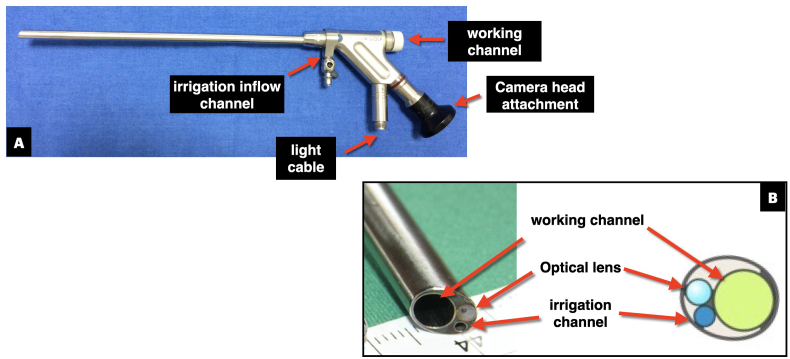
Fig. 1.
Full Endoscope Is a smart tube in which high definition optics, irrigation channel and working channel are all integrated together. Fig. 1A: demonstrates the parts of an endoscope Fig. 1B: shows cross section of the endoscope.
Fig. 2.
Endoscope causes least muscle and soft tissue trauma. Fig. 2A: MRI of a L5S1 left sided disc herniation treated with IL technique. Fig. 2B: disc fragments were removed successfully through a small cut of 2.5 mm wide and 10 mm long in the ligamentum flavum. Fig. 2C: postoperative MRI shows complete hernia removal. There is no damage to the posterior muscles or flavum. Fig. 2D: 8 mm skin incision closed with a single stitch Fig. 2E and F: show intraoperative microscopic and endoscopic vision in posterior cervical discectomy. The endoscopic vision is much superior without much bleeding Fig. 2G and H: show the difference of vision of a microscope and an endoscope. In an microscope, the surgeons eye is at a distance from the target pathology whereas the surgeons eye is at the tip of the endoscope which is very close to the pathology.
Fig. 3.
Case example: 43 year old male came with complaints of severe bilateral anterior thigh pain, tingling & difficulty in walking for 4 months. Patient had undergone open laminectomy L23, L34, 10 years ago. Transforaminal endoscopy from left side was performed under LA and conscious sedation Fig. 3A: MRI shows large central down migrated disc herniation with severe compression of thecal sac. Fig. 3B: Sagittal CT reconstruction shows two level laminectomy defect Fig. 3C: postoperative MRI shows complete hernia removal without any additional damage to the facet joint. Fig. 3D: Intraoperative endoscopic view shows the tail of the herniated fragment. Fig. 3E: Intraoperative endoscopic view after removal of the fragment with traversing root seen in the ventral epidural space above the annulus. In this case, if open revision surgery was performed, further damage to facet joint would have compromised the facet joint stability and requiring instrumented fusion surgery. Transforaminal endoscopy made it possible to remove the herniated fragment without further damage to the facet thus avoiding the need for fusion surgery.
3. Approach possibilities
Full endoscopy is a target oriented surgery in which the approach is planned carefully to reach the surgical target site.11
The basic purpose is to gain access to the pathology by the easiest route with minimal soft tissue and bone damage. Even though a variety of approaches have been reported to achieve this goal, the basic approaches are transforaminal (TF) and interlaminar (IL) (Fig. 4).
Fig. 4.
Illustration shows that endoscopy is a target specific surgery. Depending on the location of the herniation, the trajectory and angle of the endoscope is modified. Accordingly variations in the approaches can be seen. The two basic approaches are Transforaminal and Interlaminar. Fig. 4B: Clinical picture of Transforaminal approach Fig. 4C: Clinical picture of Interlaminar approach.
4. Transforaminal approach
It is the elder technique, first reported by Kambin in 1986 using an arthroscope.12 The approach utilises Kambin's triangle which is a safe working zone to access the spinal canal for removal of the herniated fragment. The two most popular variations of technique are Inside-out (I–O) technique of Anthony Yeung13, 14, 15 and Outside-in (O–I) technique popularised by Thomas Hoogland16,17. In the inside out technique the endoscope is first inserted in the posterior part of the disc space to remove the intradiscal fragments and then it is gradually levered up and shifted towards the posterior annulus to target the disc fragments in the ventral epidural space. Whereas in the Outside- In technique, the working channel is first placed on the posterolateral aspect of the facet joint and the undersurface of the SAP is cut with a trephine under fluoroscopy guidance to widen the size of the foramen. This procedure is called as foraminoplasty. It allows access to the ventral epidural space to remove any sequestrated or migrated fragments. If necessary, the surgeon may cut the annulus to enter the disc to remove any intradiscal fragments. Both the approaches have their own advantages and disadvantages. Inside-out approach, though more bloodless and less invasive may not always provide easy access to migrated herniations. On the other hand one should remember that it is not always necessary to undercut the facet to access simple non migrated herniations, which is a routine for the Outside- In approach. The third approach is half & half technique which is a variation of I–O technique.18 In this approach the target is the posterolateral annulus where the working channel is anchored and the endoscope visualises the epidural space, disc space and posterior annulus in between. Indications of transforaminal approach are foraminal and extraforaminal disc herniations in the lumbar spine, foraminal stenosis, paracentral non migrated or low migrated herniations and large central herniations in the upper lumbar spine (Fig. 5).
Fig. 5.
Illustration shows the popular variations in the technique of transforaminal approach. Fig. 5A: Inside out technique in which intradiscal fragments are first removed. The endoscope is then levered upwards to reach the epidural space Fig. 5B: Outside in technique in which the undersurface of the superior articular facet is removed first to reach the epidural herniated fragment. If necessary the annulus is cut to enter the disc space to remove intradiscal fragments Fig. 5C: Half & Half technique in which cannula is anchored at the posterior annulus to visualise both the posterior part of disc and epidural space at the same time.
4.1. Basic transforaminal technique for lumbar disc herniation
The procedure can be done under local, epidural or general anesthesia. Patient position is prone on bolsters. Two Lateral lines are drawn on lateral C-arm view. First line joins the tips of spinous process of adjoining vertebrae and is called the spinous process line. Second line which is more lateral joins the dorsum of the adjacent facet joints. It is called as the facet joint line. Depending on the location of disc herniation, size of foramen and facet, skin entry is usually taken between these two lines. Skin entry lateral to the facet joint line should be avoided as it can damage vital abdominal structures.The second line is the AP line drawn in the centre of disc space in an orthogonal AP C-arm view. The intersection of these two lines (AP line and any point between the two lateral lines is the skin entry point. If the surgery is done under local anesthesia along with conscious sedation (midazolam and fentanyl or other drug of choice) is given by the anesthetist. The skin and muscles are infiltrated with 2% lidocaine. 18 gauge endoscopy needle is inserted and advanced under AP and lateral fluoroscopy views. The needle position is approved if it lies at the centre of the disc parallel to the endplates and the tip positioned at the medial pedicle line in AP view and posterior vertebral line in the lateral view. At upper lumbar or thoracic levels it is safer to stop at mid or lateral pedicle line. Once the position of the needle is confirmed 5–7 ml of 1% lidocaine is instilled in the epidural space of Kambin's triangle. 8 mm skin incision is taken. Guide wire is then passed through the needle. Dilator is inserted over the guide wire. Working channel is then slided over the dilator and anchored in the disc space. Endoscope is passed through the working channel. Initially Triggerflex radio frequency probe is used to achieve hemostasis and delineate the anatomical structures. Intradiscal disc fragments are removed with a rongeur. Annular release is done by cutting the posterior part of annulus - PLL complex with a punch forceps. Herniated fragments are then removed. Endoscope is levered upwards to inspect the ventral epidural space and the traversing nerve root. Any free fragments visualised are removed under direct vision. Decompression of the nerve root is confirmed (Fig. 6).
Fig. 6.
Shows marking of two surface lines on the back of patient after prone position. Fig. 6A shows marking of the lateral line under lateral view of fluoroscopy. Green line is the tip of spinous process and red line is the level of dorsal aspect of facet joint. FIg 6B and C show the corresponding level in axial MRI and fluoroscopy view. The skin entry point should lie between these two lines and should more lateral to the red line as it can cause injury to the viscera Fig. 6D,E and F: show the marking of the AP line which is through the center of the disc and parallel to the endplates The intersection of AP and lateral lines is the point of skin incision.
4.2. Indications
The approach utilises the intervertebral foramen to access the spinal canal. Therefore larger the size of the foramen more easy it becomes to access the herniated fragment. The primary indications are foraminal/extraforaminal lumbar disc herniations and foraminal stenosis. It is also preferred for paracentral, central, low migrated herniations. It is a recommended approach for upper lumbar and thoracic spine pathologies. Even though experienced transforaminal surgeons are comfortable in tackling high grade migrated herniations or lateral recess stenosis, the surgery can be very challenging for the others and therefore not recommended. Contraindications are L5S1 herniation with a high iliac crest and central and lateral recess stenosis. Interlaminar approach is the preferred approach in both these conditions.
5. Interlaminar approach
Even though it was described almost two decades after the transforaminal approach, it is a more popular approach and should be credited for the rise in the popularity and acceptance of full endoscopic procedures worldwide. The approach was first reported by Ruetten19 & Gun Choi20 in 2006 for L5S1 disc herniations. Choi performed the surgery under LA in lateral position in which he passed serial dilators over needle & guide wire under fluoroscopy guidance to split the ligamentum flavum. Ruetten on the other hand cut the ligamentum flavum layer by layer under direct endoscopic visualization to enter the spinal canal. The latter technique because of its simplicity and safety has become more popular over the years. Ruetten published successful results for migrated disc herniations in 2007 21 With the advent of large working channel endoscopes, power drills and punches, then for lateral recess in 200922,23 and for central canal stenosis in 2015 by ULBD technique (unilateral approach for bilateral decompression)24
The versatility of the approach made it possible to treat cervical radiculopathy due to soft lateral discs or foraminal stenosis25,26 with promising results and also for thoracic spine27, 28, 29
5.1. Basic interlaminar technique for lumbar disc herniation
Procedure is similar to microdiscectomy procedure. Surgery is done under general or epidural anesthesia in prone position. In AP view of fluoroscopy the interlaminar space of the targeted level is identified. 8 mm incision is taken at the centre, just a few millimetres away from the midline, on the right or left side depending on the location of herniation. Dilator is inserted and advanced till it reaches the facet joint level. Once the position is confirmed on fluoroscopy, working channel is inserted and dilator is removed. Endoscope is inserted and exposure of the ligamentum flavum is done. If the interlaminar space is wide enough as usually seen at L5S1 level, there is no need for bone resection. A linear cut is made in the ligamentum flavum with a punch forceps starting close to the midline and extending laterally towards the facet joint. The flavum is cut layer by layer till the epidural space is opened and root is visualised. Lateral border of the root is confirmed. The tip of the working channel is used to retract the nerve, epidural vessels are coagulated and disc space is exposed and fragments are removed. If the interlaminar window is narrow or in case of migrated herniations, a high speed endoscopic drill is used to remove the bone and expose the fragment19
5.2. Indications
IL approach is more suitable for intracanal herniations in the lower lumbar spine.30 Migrated, calcified herniations or those associated with stenosis are ideal indications. Soft Lateral discs or foraminal stenosis in cervical spine causing cervical radiculopathy and posterior compression in thoracic spine due to hypertrophied or ossified flavum can also be successfully treated by this approach. At upper lumbar spine, IL approach is difficult especially for central discs because of narrow Interlaminar space and difficulty in retracting neural tissue. In such cases TF approach is preferred (Fig. 7).
Fig. 7.
Case example: 35 year old male was complaining of severe right leg pain and bilateral tingling & numbness since 3 months with no relief with conservative treatment. Interlaminar endoscopy was performed from right side under GA Fig. 7A: MRI shows large down migrated axillary disc herniation on right side with severe thecal sac compression Fig. 7B: postoperative MRI shows complete hernia removal without Fig. 7C–H: show intraoperative endoscopic views of various steps of the technique. Fig. 7C: exposed ligamentum flavum. Fig. 7D: Endoscopic punch is used to cut the flavum layer by layer to open up the epidural space. Fig. 7E: Once the epidural space is opened, flavum cut is extended laterally till facet joint. Fig. 7E: Large herniation protruding between the nerve root and dural sac. Fig. 7G: Herniated fragment being removed with a forceps. Fig. 7H: shows decompression of nerve root was achieved through a small slit in the ligamentum flavum.
6. How to choose an approach for a lumbar disc
The confusion of choice of approach is mainly for the lumbar disc herniations and not so much for other pathologies or cervical or thoracic regions.
To choose the right approach surgeon should consider the following two factors in the order of descending priority. Firstly choose an approach which is more easy, effective and less complicated with predictable and good success rate. For example in an L5S1 disc herniation with a high iliac crest, a conventional TF approach may not be possible whereas a trans-iliac TF approach will be more aggressive with higher chance of complications. An IL approach proves to be very easy in such cases especially since the interlaminar space is wide at L5S1 level. Second factor to be considered is that in some cases both the approaches may be equally effective, safe and easy. In such cases, choose an approach which is more minimally invasive amongst the two which is usually the transforaminal approach. For example, in a case of L45 non-migrated paracentral herniation, IL approach may need drilling of the medial part of the facet joint to reach the herniation lateral to the nerve root but if we use a TF approach in such case, the herniation can be removed effectively without the need of bone and ligamentum flavum resection. Hence TF approach should be considered as a first choice in such cases (Fig. 8).
Fig. 8.
Show comparison of the transforaminal & interlaminar approach. Transforaminal approach is more suitable and recommended at upper lumbar levels because the intervertebral foramen is wide and Interlaminar space is narrow. Similarly Interlaminar space is the widest at L45 & L5S1 levels making it is more suitable for the IL approach.
7. Discussion
The importance and acceptance of full endoscopic surgeries continues to grow. Even though the procedure was described in 1986, for next two decades, it was practiced only by a few surgeons, for a very limited number of indications. After 2006, there was a sudden and rapid rise in the popularity of the procedure. This can be attributed to two reasons. First is the technological advancements in the optics and introduction of mechanical instruments like power drill and Kerrison punches. Second reason is the introduction of interlaminar approach which has opened up the possibilities of treatment of complex degenerative disc and stenosis conditions in the lumbar, cervical and thoracic spine.
It is important for the surgeon to master Both TF and IL approaches to treat a wide range of spinal pathologies. Surgeon should try to develop equal proficiency with both the techniques and try not to restrict themselves to be only a transforaminal or an interlaminar surgeon, although they may prefer one of the approaches as their favourite approach. Proper handling of the instruments and good hand eye coordination takes time and practice. To make the learning curve easier, a beginner surgeon should start with TF approach as it is more easy to handle the long and delicate surgical instruments compared to IL approach. Even while practising the TF approach, surgeon should try to learn from other parallel techniques. For example, surgeons trained in inside out technique should learn to perform foraminoplasty to treat migrated herniations & foraminal stenosis, similarly outside in surgeons should to remember that it is not always necessary to undercut the facet joint for simple non-migrated herniations and implementing IO technique in their practice can make the procedure more easy and less invasive.
7.1. Anesthesia in endoscopic surgeries
Local anesthesia with conscious sedation is a good option in TF discectomy. Many surgeons recommend it due to advantages like intraoperative feedback from patients which prevents iatrogenic neural injury and avoiding complications of GA in elderly patients with severe medical morbidities. Other benefits are less hospital stay, early mobilization, early discharge from the hospital and reduced hospital cost31, 32, 33, 34. But an experienced surgeon will understand that the candidates for LA should be selected carefully with proper preoperative evaluation and counselling. LA may not be a good choice in patients with infective pathology, very anxious and noncooperative patient and in patients who need prolonged operative time as lying in prone position over bolsters may become very uncomfortable for the patient. Fang recommended epidural anesthesia for his foraminoplasty surgeries since his patients experienced discomfort with local anesthesia and expressed dissatisfaction35. For IL approach, the preferred anesthesia is either GA or EA. Although some authors perform IL surgeries under LA, most do not recommended it due to intraoperative discomfort. Chen prospectively compared the results of LA and GA for interlaminar approach at L5‐S1. The patients in the LA group usually felt discomfort in the low back and leg during intraoperative manipulation of the dural sac and nerve root36
7.2. Limitations
The main indication of full endoscopic surgeries are degenerative conditions in the lumbar, cervical and thoracic spine. Although there are numerous publications mentioning promising results in early infections37, 38, 39, its role in the management of intradural and metastatic tumors is very selective and limited (Fig. 9).40, 41, 42
Fig. 9.
Full endoscopic surgeries are more suitable and effective in focal pathologies (single or two level). It is not recommended in extensive or multilevel conditions because the duration of surgery is extremely prolonged and surgeon get tired making him prone to make complications. So the benefits of MIS surgeries are lost.
Full Endoscopy is more suitable for focal pathology than an extensive pathology because the excessive duration of surgery and the amount of surgeon effort needed, totally outweigh the benefits of MIS surgery. Benefit zone of full endoscopic surgeries is the maximum for one or two levels mainly discectomies, decompressions and fusions. As the surgical complexity of the procedure and the number of levels increase the incidence of complications and suboptimal results increase.43
7.3. Learning curve
There is an inherently long learning curve associated with all MIS procedures. The learning curve in endoscopy is comparatively more steep and difficult44 For a conventional open spine surgeon, TF technique is initially difficult to understand because of unfamiliar orientation of the anatomy, but once understood, it is easy to master. IL technique, on the other hand, is easy to understand due to its familiarity of approach but takes time to master because of difficulty in handling instruments making the learning curve steeper.44, 45, 46
. The major challenges in accepting and pursuing full endoscopic surgeries are unfamiliar surgical anatomy, absence of tactile sensation, restricted surgical field and technical difficulty of working through a narrow surgical corridor with limited visualization of anatomic landmarks11. Delicate surgical manipulations in constrained tubular working channel may be difficult to learn and master47 The learning curve is assessed on the basis of duration of the operation time, surgical outcome, conversion to open procedures and complication rates. Although complication rates between MIS and open surgeries are equivalent, Beginner MIS surgeons initially face a higher rate of complications that eventually normalises. Once mastered, these techniques can result in a significant reduction of complications.48 All complications, adverse events, and conversions to open techniques occurred within the initial 30 procedures11. Lack of proper training and improper case selection as per surgical experience are the two most important reasons for abandoning endoscopic spine surgery.44
Strategies to overcome the learning curve are proper understanding of the surgical anatomy, extensive training courses like cadaver workshops and fellowship training to become familiar with the technical steps and instruments and supervision by an experienced senior surgeon during the initial cases.49 Begin with simple cases. A gradual increase in surgical complexity along with careful patient selection, enables the surgeon to maintain the rate of complication within acceptable limits.50
Full endoscopic surgeries are now well-established procedures for decompression of single- or two-level pathologies, mostly degenerative but also infections. The indications of endoscopic spine surgery have shifted from simple discectomies, decompressions to lumbar interbody fusions. In recent years promising results are reported for grade one or two level lumbar and thoracic fusions. It won't be a surprise if full endoscopic surgery replaces microscope assisted procedures in future to become a gold standard. Further technological advancements not only in endoscopic instruments, but also in implants, navigation and robotics technology will help in expanding the surgical indications and make it possible to treat complex or even multilevel spinal problems, beyond degenerative disc diseases.
8. Conclusion
Full endoscopic spine surgery is one of the fastest growing technique in the field of modern spine surgery. Better intraoperative visualization of the pathology, lesser incidence of complications, faster recovery time, less postoperative pain, better relief of symptoms and early return to activity are the main reasons behind this rapid growth. With better patient outcomes and reduced medical costs, the procedure is going to be more accepted, relevant and popular procedure in future.
Funding/sponsorship
None.
Informed consent (patient/guardian), mandatory only for case reports/clinical images
None.
Institutional ethical committee approval (for all human studies)
None.
Authors contribution
Dr. Pramod V. Lokhande is responsible for Conceptualization; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Declaration of competing interest
None.
Acknowledgement
None.
References
- 1.Ruetten S., Komp M., Merk H., et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–939. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 2.Kim M.J., Lee S.H., Jung E.S., et al. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol. 2007;68:623–631. doi: 10.1016/j.surneu.2006.12.051. [DOI] [PubMed] [Google Scholar]
- 3.Komp M., Hahn P., Oezdemir S., et al. Bilateral spinal decompression of lumbar central stenosis with the full- endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18:61–70. [PubMed] [Google Scholar]
- 4.Ruetten S., Komp M., Merk H., et al. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009;10:476–485. doi: 10.3171/2008.7.17634. [DOI] [PubMed] [Google Scholar]
- 5.Lee D.Y., Shim C.S., Ahn Y., et al. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc. 2009;46:515–521. doi: 10.3340/jkns.2009.46.6.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahan M.A., Prasse T., Kim R.B., et al. Full-endoscopic spine surgery diminishes surgical site infections - a propensity score-matched analysis. Spine J. 2023 Jan 25;S1529–9430(23):18–19. doi: 10.1016/j.spinee.2023.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Ruetten S., Hahn P., Oezdemir S., Baraliakos X., Godolias G., Komp M. Decompression of the anterior thoracic spinal canal using a novel full-endoscopic uniportal transthoracic retropleural technique-an anatomical feasibility study in human cadavers. Clin Anat. 2018 Jul;31(5):716–723. doi: 10.1002/ca.23075. [DOI] [PubMed] [Google Scholar]
- 8.Ruetten S., Hahn P., Oezdemir S., et al. Full-endoscopic uniportal decompression in disc herniations and stenosis of the thoracic spine using the interlaminar, extraforaminal, or transthoracic retropleural approach. J Neurosurg Spine. 2018 Aug;29(2):157–168. doi: 10.3171/2017.12.SPINE171096. [DOI] [PubMed] [Google Scholar]
- 9.Hasan S., McGrath L.B., Sen R.D., Barber J.K., Hofstetter C.P. Comparison of full-endoscopic and minimally invasive decompression for lumbar spinal stenosis in the setting of degenerative scoliosis and spondylolisthesis. Neurosurg Focus. 2019 May 1;46(5):E16. doi: 10.3171/2019.2.FOCUS195. [DOI] [PubMed] [Google Scholar]
- 10.Kaneko T., Takano Y., Inanami H. One-year clinical outcome after full-endoscopic interlaminar lumbar discectomy for isthmic lumbar spondylolisthesis: two case reports. Medicine (Baltimore) 2021 Jun 25;100(25) doi: 10.1097/MD.0000000000026385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sclafani J.A., Kim C.W. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014 Jun;472(6):1711–1717. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kambin Parviz. Arthroscopic microdiscectomy of the lumbar spine. Clin Sports Med. 1993;12(1):143–150. [PubMed] [Google Scholar]
- 13.Yeung A.T. Minimally invasive disc surgery with the Yeung endoscopic spine system (YESS) Surg Technol Int. 1999;8:267–277. [PubMed] [Google Scholar]
- 14.Yeung A.T. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med. 2000 Sep;67(4):327–332. [PubMed] [Google Scholar]
- 15.Yeung A.T., Yeung C.A. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int. 2003;11:255–263. [PubMed] [Google Scholar]
- 16.Schubert M., Hoogland T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Operat Orthop Traumatol. 2005 Dec;17(6):641–661. doi: 10.1007/s00064-005-1156-9. [DOI] [PubMed] [Google Scholar]
- 17.Hoogland T., Schubert M., Miklitz B., Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006 Nov 15;31(24):E890–E897. doi: 10.1097/01.brs.0000245955.22358.3a. [DOI] [PubMed] [Google Scholar]
- 18.Lee S., Kim S.-K., Lee S.-H., et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431–437. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruetten S., Komp M., Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49:80–87. doi: 10.1055/s-2006-932172. [DOI] [PubMed] [Google Scholar]
- 20.Choi G., Lee S.H., Raiturker P.P., Lee S., Chae Y.S. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006 Feb;58(1 suppl l) doi: 10.1227/01.neu.0000192713.95921.4a. ONS59-68. [DOI] [PubMed] [Google Scholar]
- 21.Ruetten S., Komp M., Merk H., et al. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007;6:521–530. doi: 10.3171/spi.2007.6.6.2. [DOI] [PubMed] [Google Scholar]
- 22.Ruetten S., Komp M., Merk H., Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009 May;10(5):476–485. doi: 10.3171/2008.7.17634. [DOI] [PubMed] [Google Scholar]
- 23.Komp M., Hahn P., Merk H., et al. Bilateral operation of lumbar degenerative central spinal stenosis in full- endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. J Spinal Disord Tech. 2011;24:281–287. doi: 10.1097/BSD.0b013e3181f9f55e. [DOI] [PubMed] [Google Scholar]
- 24.Komp M., Hahn P., Oezdemir S., et al. Bilateral spinal decompression of lumbar central stenosis with the full- endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18:61–70. [PubMed] [Google Scholar]
- 25.Ruetten S., Komp M., Merk H., Godolias G. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg. 2007 Aug;50(4):219–226. doi: 10.1055/s-2007-985860. [DOI] [PubMed] [Google Scholar]
- 26.Ruetten S., Komp M., Merk H., Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008 Apr 20;33(9):940–948. doi: 10.1097/BRS.0b013e31816c8b67. [DOI] [PubMed] [Google Scholar]
- 27.Ruetten S., Hahn P., Oezdemir S., Baraliakos X., Godolias G., Komp M. Operation of soft or calcified thoracic disc herniations in the full-endoscopic uniportal extraforaminal technique. Pain Physician. 2018 Jul;21(4):E331–E340. [PubMed] [Google Scholar]
- 28.Ruetten S., Hahn P., Oezdemir S., et al. Full-endoscopic uniportal decompression in disc herniations and stenosis of the thoracic spine using the interlaminar, extraforaminal, or transthoracic retropleural approach. J Neurosurg Spine. 2018 Aug;29(2) doi: 10.3171/2017.12.SPINE171096. [DOI] [PubMed] [Google Scholar]
- 29.Fiani B., Siddiqi I., Reardon T., et al. Thoracic endoscopic spine surgery: a comprehensive review. Internet J Spine Surg. 2020 Oct;14(5):762–771. doi: 10.14444/7109. Epub 2020 Oct 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kotheeranurak V., Liawrungrueang W., Quillo-Olvera J., et al. Spine (Phila Pa; 1976. Full-endoscopic Lumbar Discectomy Approach Selection - A Systematic Review and Proposed Algorithm. 2023 Feb 6. [DOI] [PubMed] [Google Scholar]
- 31.Yeung A.T., Tsou P.M. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complication in 307 consecutive cases. Spine. 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 32.Yeung A., Gore S. Endoscopic foraminal decompression for failed back surgery syndrome under local anesthesia. Internet J Spine Surg. 2014;8 doi: 10.14444/1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sairyo K., Egawa H., Matsuura T. Transfo- raminal approach for percutaneous en- doscopic lumbar discectomy under local anesthesia. J Med Invest. 2014;61:217–225. doi: 10.2152/jmi.61.217. [DOI] [PubMed] [Google Scholar]
- 34.Ahn Y. Transforaminal percutaneous en- doscopic lumbar discectomy: technical tips to prevent complications. Expet Rev Med Dev. 2012;9:361–366. doi: 10.1586/erd.12.23. [DOI] [PubMed] [Google Scholar]
- 35.Fang G., Ding Z., Song Z. Comparison of the effects of epidural anesthesia and local anesthesia in lumbar transforaminal endoscopic surgery. Pain Physician. 2016 Sep-Oct;19(7):E1001–E1004. [PubMed] [Google Scholar]
- 36.Chen Z., Wang X., Cui X., Zhang G., Xu J., Lian X. Transforaminal versus interlaminar approach of full-endoscopic lumbar discectomy under local anesthesia for L5/S1 disc herniation: a randomized controlled trial. Pain Physician. 2022 Nov;25(8):E1191–E1198. [PubMed] [Google Scholar]
- 37.Lin G.X., Kim J.S., Sharma S., et al. Full endoscopic discectomy, debridement, and drainage for high-risk patients with spondylodiscitis. World Neurosurg. 2019 Jul;127:e202–e211. doi: 10.1016/j.wneu.2019.02.206. [DOI] [PubMed] [Google Scholar]
- 38.Choi E.J., Kim S.Y., Kim H.G., Shon H.S., Kim T.K., Kim K.H. Percutaneous endoscopic debridement and drainage with four different approach methods for the treatment of spinal infection. Pain Physician. 2017 Sep;20(6):E933–E940. [PubMed] [Google Scholar]
- 39.Lin I.H., Lin C.Y., Chang C.C., et al. Percutaneous endoscopic surgery alone to treat severe infectious spondylodiscitis in the thoracolumbar spine: a reparative mechanism of spontaneous spinal arthrodesis. Pain Physician. 2022 Mar;25(2):E299–E308. [PubMed] [Google Scholar]
- 40.Caballero-García J., Linares-Benavides Y.J., Leitão U.L.S., Aparicio-García C., López-Sánchez M. Minimally invasive removal of extra- and intradural spinal tumors using full endoscopic visualization. Global Spine J. 2022 Jan;12(1):121–129. doi: 10.1177/2192568220948806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Endo T., Tominaga T. Use of an endoscope for spinal intradural pathology. J Spine Surg. 2020 Jun;6(2):495–501. doi: 10.21037/jss.2020.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Şentürk S., Ünsal Ü.Ü. Percutaneous full-endoscopic removal of lumbar intradural extramedullary tumor via translaminar approach. World Neurosurg. 2019 May;125:146–149. doi: 10.1016/j.wneu.2019.01.206. [DOI] [PubMed] [Google Scholar]
- 43.Hasan S., Härtl R., Hofstetter C.P. The benefit zone of full-endoscopic spine surgery. J Spine Surg. 2019 Jun;5(Suppl 1):S41–S56. doi: 10.21037/jss.2019.04.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahn Y., Lee S., Son S., et al. Learning curve for interlaminar endoscopic lumbar discectomy: a systematic review. World Neurosurg. 2021;150:93–100. doi: 10.1016/j.wneu.2021.03.128. [DOI] [PubMed] [Google Scholar]
- 45.Sun B., Shi C., Xu Z., et al. Learning curve for percutaneous endoscopic lumbar diskectomy in bi-needle technique using cumulative summation test for learning curve. World Neurosurg. 2019;129:e586–e593. doi: 10.1016/j.wneu.2019.05.227. [DOI] [PubMed] [Google Scholar]
- 46.Hsu H.T., Chang S.J., Yang S.S., et al. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013;22:727–733. doi: 10.1007/s00586-012-2540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vaishnav A.S., Othman Y.A., Virk S.S., Gang C.H., Qureshi S.A. Current state of minimally invasive spine surgery. J Spine Surg. 2019 Jun;5(Suppl 1):S2–S10. doi: 10.21037/jss.2019.05.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Perez-Cruet M.J., Fessler R.G., Perin N.I. Review: complications of minimally invasive spinal surgery. Neurosurgery. 2002 Nov;51(5 Suppl):S26–S36. [PubMed] [Google Scholar]
- 49.Gadjradj P.S., Vreeling A., Depauw P.R., Schutte P.J., Harhangi B.S., PTED-Study Group Surgeons learning curve of transforaminal endoscopic discectomy for sciatica. Neurospine. 2022 Sep;19(3):594–602. doi: 10.14245/ns.2244342.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kimchi G., Orlev A., Hadanny A., Knoller N., Harel R. Minimally invasive spine surgery: the learning curve of a single surgeon. Global Spine J. 2020 Dec;10(8):1022–1026. doi: 10.1177/2192568219880872. [DOI] [PMC free article] [PubMed] [Google Scholar]