Summary
Background
Inflammatory bowel disease (IBD) is associated with psychiatric diseases, but it is unclear to what degree patients with IBD are affected over their lifetime. We aimed to longitudinally investigate the risk of anxiety, depression, and bipolar disorder before and after IBD diagnosis to understand the full burden of these diseases in patients with IBD.
Methods
In this population based cohort study, we identified 22,103 patients diagnosed with IBD between January 1, 2003 and December 31, 2013 in the Danish National registers and 110,515 matched reference individuals from the general population. We calculated yearly prevalence of hospital contacts for anxiety, depression, and bipolar disorder and dispensed prescriptions for antidepressants from five years before to ten years after IBD diagnosis. We used logistic regression to calculate prevalence odds ratios (OR) for each outcome prior to IBD diagnosis, and Cox regression to calculate hazard ratios (HR) of new outcomes after IBD diagnosis.
Findings
During >150,000 person years follow-up, patients with IBD had higher risk of anxiety (OR 1.4; 95% confidence interval (CI) 1.2–1.7) and depression (OR 1.4; 95% CI 1.3–1.6) starting at least five years before and continuing until at least ten years after IBD diagnosis (HR 1.3; 95% CI 1.1–1.5 for anxiety and HR 1.5; 95% CI 1.4–1.7 for depression). The risk was particularly high around IBD diagnosis and in patients diagnosed with IBD after the age of 40 years. We found no association between IBD and bipolar disorder.
Interpretation
This population-based study suggests that anxiety and depression are clinically significant comorbidities of IBD both before and after IBD diagnosis, which warrant thorough evaluation and management, particularly around the time of IBD diagnosis.
Funding
The Danish National Research Foundation [DNRF148], the Lundbeck Foundation [R313-2019-857], and Aage og Johanne Louis-Hansens Fond [9688-3374 TJS].
Keywords: Inflammatory bowel disease, IBD, Gut-brain axis, Depression, Anxiety, Bipolar disorder
Research in context.
Evidence before this study
We searched MEDLINE and Embase from January 1st 1991 to July 26th 2022 with the search terms (inflammatory bowel disease OR ulcerative colitis OR crohn's disease OR IBD) AND (depression OR anxiety OR bipolar disorder), and we did a manual reference list search of identified studies. Previous research has shown that inflammatory bowel disease (IBD) is associated with anxiety and depression and has indicated that the relationship between the diseases is bidirectional, but there is a lack of population-based studies of the association over time. Bipolar disorder has not been well examined in IBD, but some previous studies have suggested an association.
Added value of this study
This study quantifies and illustrates the burden of psychiatric diseases over time in more than 22,000 patients with IBD and confirms a bidirectional pattern in the co-occurrence of IBD, anxiety and depression, but not bipolar disorder, with increased occurrence of anxiety and depression from five years before until at least ten years after IBD diagnosis. We detected a particularly high risk of anxiety and depression in the first year after IBD diagnosis, and a higher risk in those diagnosed with IBD after the age of 40.
Implications of all the available evidence
Our findings emphasise the need for concurrent management of anxiety and depression in the care for patients with IBD, with a particular focus around the time of diagnosis. Future research should focus on mechanisms linking the diseases and on improving the holistic treatment of patients with IBD.
Introduction
Inflammatory bowel disease (IBD)—with its two subtypes Crohn's disease (CD) and ulcerative colitis (UC)—is a chronic, immune-mediated disease of the gastro-intestinal tract. IBD can be diagnosed in all phases of life with a peak incidence in early adulthood.1 The disease course is unpredictable, and patients face periods with flares, medical therapy, and often surgery. Many patients are impacted by their IBD for a large portion of their life, which often leads to absence from work or education2,3 and reduced quality of life.4
Patients with IBD are more likely to experience anxiety, depression, and possibly bipolar disorder than the general population.5, 6, 7 A recent meta-analysis found a pooled prevalence of anxiety symptoms of 31.3% and a pooled prevalence of depression symptoms of 25.2% in patients with IBD,6 and a study found that patients with IBD had an increased risk of anxiety (HR 1.3, 95% CI 1.3–1.4) and of mood disorders (HR 1.4, 95% CI 1.4–1.5).5 Another study found an increased incidence rate ratio (IRR) of bipolar disorder in patients with IBD (IRR 1.82, 95% CI 1.44–2.30).8 The psychiatric comorbidities increases healthcare utilization and costs in patients with IBD,9,10 and anxiety and depression might exacerbate the disease course of IBD,11 while treatment of anxiety and depression has been linked to improvements in IBD symptoms along with enhanced quality of life.12 Research indicates that the relationship between IBD, anxiety, and depression is bidirectional,11 meaning that the risk of these diseases is higher both before and after IBD diagnosis. The hypothesized causes for this bidirectional relationship include shared diseases pathways, communication through the gut-brain axis, and shared genetic factors.12
While research into the connection between IBD and psychiatric diseases has increased, it remains unclear to which degree patients with IBD are impacted over their lifetime, and when the psychiatric comorbidities arise. Most previous studies have examined prevalence at a specific time point either before or after IBD diagnosis8,13,14 without considering the development longitudinally year by year both before and after IBD diagnosis.
We aimed to examine the burden of anxiety, depression, and bipolar disorder longitudinally leading up to and following IBD diagnosis. We will quantify the prevalence of these diseases in the five years before IBD diagnosis and estimate the incidence of these outcomes in the ten years after IBD diagnosis. Using hospital, outpatient clinic and prescription data, we characterize the longitudinal trajectories of both severe and more moderate expressions of psychiatric comorbidity over time in patients with IBD in the Danish population.
Methods
Study population
The source population was identified through the Danish Civil Registration System as all individuals over the age of 18 years with an address in Denmark in the period 01.01.2003–12.31.2013 and was linked to other national registers using the unique personal identification number issued to all persons at birth or upon immigration. The Danish Civil Registration System is complete with regards to follow-up on all individuals and contains daily updated data on vital status, immigration and emigration.15
Case definition
IBD cases were identified through the Danish National Patient Registry (NPR), which contains information on all inpatient hospital contacts since 1977 as well as on all outpatient, emergency department and psychiatric hospital contacts since 1995. Details about the NPR data quality and research potential is described by Schmidt and colleagues.16 We used ICD-8 (CD: 563.01, 563.02, 563.08, 563.09; UC: 563.19, 569.04) and ICD-10 codes (CD: K50; UC: K51). To limit inclusion of individuals with a misdiagnosis, cases had to have at least two hospital contacts (in- or outpatient) for IBD within a two-year period. This case definition has been shown to lead to a positive predictive value (PPV) of the IBD diagnosis of 95%.17 The two contacts had to be the first registrations for IBD for that patient, meaning, patients with an initial IBD contact who only later fulfilled the two-contact criteria were not included in order to increase the precision of time of diagnosis. The study period was 1998–2018. Both of the two IBD contacts had to be between January 1st 2003 and December 31st 2013 to allow for data on five years before and five to ten years after IBD diagnosis. The IBD patients had to have an address in a municipality in Denmark in the period between five years before first IBD contact and in the period between the two IBD contacts. IBD subtype was determined by ICD codes associated with the two contacts. If both CD and UC were registered, the IBD subtype was classified as CD. For each six-month interval of the inclusion period, all new IBD cases in the period were matched 1:5 on age, sex, municipality of residence, and calendar time (by year and semester) to individuals from the general population without IBD who were still living in Denmark at the end of the interval using frequency matching. We used the second of the two IBD contacts as time of matching. Each reference individual was assigned an index date, which was the first of the two IBD contacts of the corresponding IBD case.
Outcomes
Outcomes of psychiatric diseases were defined as at least one hospital contact for one of the psychiatric diseases obtained from the NPR and from the Danish Psychiatric Central Research Register, which contains information on psychiatric inpatient hospital contacts since 1970 and on psychiatric outpatient and emergency department contacts since 199518 (ICD-10 codes: depression: F32, F33; anxiety: F41; bipolar disorder: F31). The two registers were combined in 1995. These codes have not been systematically validated in scientific studies, but there is a data validation process at the Danish National Patient Register and at Centre for Psychiatric research, where electronic data from the registers and lists reported from individual departments are compared.16,18 Data on prescriptions for antidepressants and indications for those prescriptions were obtained from the Danish National Prescription Registry, which contains information on all dispensed prescriptions since 1994,19 using the ATC code N06A except for the subgroup N06AX12, and the outcome was defined as at least one dispensed prescription in a given year.
Statistical analysis
In order to have reliable data for the entire study period, we constricted the study to the years 1998–2018. We wanted to have ten years follow up time after IBD diagnosis for most individuals, and we chose to investigate the five years before IBD diagnosis so that we could reasonably assume that we included the time before the potential diagnostic delay, where the patients had developed IBD but had not yet been diagnosed.
We reported the annual prevalence of hospital contacts for anxiety depression, and bipolar disorder and dispensed prescriptions for antidepressants for the patients with IBD and the matched reference individuals. The annual prevalence of hospital contacts for a given was year was defined as the proportion of individuals with either a new contact starting that year or an ongoing contact continuing into that year. The annual prevalence of dispensed prescriptions for antidepressants was defined as the proportion with at least one dispensed prescription in that year.
We used logistic regression to analyse the prevalence odds ratio for anxiety, depression, bipolar disorder, and dispensed prescriptions for antidepressants five years before IBD diagnosis/index date in patients with IBD compared with reference individuals. We further analysed the prevalence odds ratio 0–2 years and 3–5 years before IBD diagnosis/index date, and we stratified analyses by IBD subtype, age at IBD diagnosis and sex.
We used Cox regression to analyse the risk of incident anxiety, depression, bipolar disorder, and dispensed prescriptions for antidepressants after IBD diagnosis/index date. This analysis was restricted to individuals with no contacts for anxiety, depression, or bipolar disorder or a dispensed prescription for antidepressants in the five years before IBD diagnosis/index date. The analysis was adjusted for age at diagnosis, sex, year of diagnosis, and municipality of residence since reference individuals were no longer matched after exclusion of individuals with a history of psychiatric disease or use of antidepressants. We further analysed the risk each year after IBD diagnosis, and we stratified analyses by IBD subtype, age at IBD diagnosis and sex.
All analyses were carried out using SAS 9.4 TS Level 1M7.
Ethical approval and informed consent
This study has approval from the Danish Data Protection Agency. In Denmark, ethical approval and informed consent is not required for register-based studies.
Role of the funding source
The funding sources had no role in study design; collection, analysis, and interpretation of data; writing of the report; and decision to submit the paper for publication. All authors had full access to the data in this study and accept responsibility for the decision to submit the manuscript for publication.
Results
From the source population of 5,341,271 individuals, we included 22,103 individuals with IBD (Supplementary Figure S1). The cohort consisted of 54.2% females and 45.8% males, 30.5% had CD, and 69.5% had UC. The mean age at IBD diagnosis was 45.9 years (Table 1). The 1:5 matched reference population contained 110,515 individuals.
Table 1.
Baseline characteristics of all patients diagnosed with IBD at age 18 or later in Denmark between 2003 and 2013 and matched reference individuals.
| IBD (n = 22,103) | Crohn's disease (n = 6738) | Ulcerative colitis (n = 15,365) | References (n = 110,515) | |
|---|---|---|---|---|
| Mean age at IBD diagnosis or index date | 45.9 years | 42.5 years | 47.3 years | 45.9 years |
| Age at diagnosis or index date | ||||
| 18–39 | 9394 (42.5%) | 3381 (50.2%) | 6013 (39.1%) | 46,970 (42.5%) |
| 40–59 | 6830 (30.9%) | 1916 (28.4%) | 4914 (32.0%) | 34,150 (30.9%) |
| 60+ | 5879 (26.6%) | 1441 (21.4%) | 4438 (28.9%) | 29,395 (26.6%) |
| Sex | ||||
| Female | 11,985 (54.2%) | 3873 (57.5%) | 8112 (52.8%) | 59,925 (54.2%) |
| Male | 10,118 (45.8%) | 2865 (42.5%) | 7253 (47.2%) | 50,590 (45.8%) |
| Year of IBD diagnosis or index date | ||||
| 2003–2006 | 7733 (35.0%) | 2254 (33.5%) | 5479 (35.7%) | 38,665 (35.0%) |
| 2007–2010 | 8283 (37.5%) | 2474 (36.7%) | 5809 (37.8%) | 41,415 (37.5%) |
| 2011–2013 | 6087 (27.5%) | 2010 (29.8%) | 4077 (26.5%) | 30,435 (27.5%) |
IBD, Inflammatory bowel disease.
In the Danish National Prescription Registry, 56% of prescriptions for antidepressants included indications. Of these, 78% were given for depression, 11% for anxiety, and 9% for the non-specific indication “psychiatric disease”. Less than 2% were given for pain, obsessive-compulsive disorder, and other rarer indications (Supplementary Table S5).
While 80%–90% of those with a hospital contact for depression received a prescription for antidepression, only 6%–11% of those with a prescription for antidepressants had a hospital contact for depression, indicating that antidepressants are prescribed for both severe and more moderate degrees of anxiety and depression, while only severe anxiety and depression is treated in the hospital sector (Supplementary Table S6).
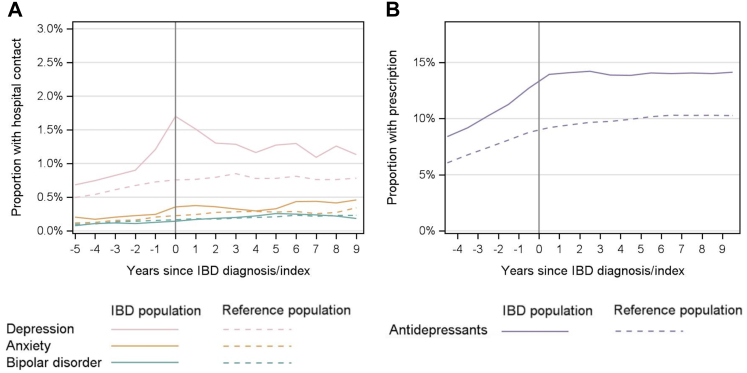
Yearly prevalence of anxiety, depression, and bipolar disorder before, around, and after IBD diagnosis
Fig. 1 shows the yearly percentage of patients with IBD and reference individuals that had a hospital contact for anxiety, depression, or bipolar disorder or a dispensed prescription for antidepressants in the 5 years before and 10 years after IBD diagnosis/index date. Depression was consistently more frequent in the patients with IBD with a peak prevalence in the year of diagnosis of 1.7% compared with 0.8% in the reference population. Anxiety was also more frequent in patients with IBD from five years before and through ten years after IBD diagnosis. Patients with IBD had prescriptions for antidepressants more frequently than the reference individuals consistently from 5 years before until at least ten years after IBD diagnosis, with a yearly prevalence ranging between 8.4% and 14.3% vs. 6.1%–10.3% in the reference group. The prevalence of bipolar disorder was similar in the IBD and reference populations (Supplementary Table S1 for numbers behind the figure).
Fig. 1.
Yearly prevalence of (A) hospital contacts for depression, anxiety, bipolar disorder, and (B) dispensed prescriptions for antidepressants in the five years before and ten years after IBD diagnosis in patients with IBD and matched individuals from the reference population. IBD, Inflammatory bowel disease.
Odds of anxiety, depression, and bipolar disorder in the five years before IBD diagnosis
During the five years before IBD diagnosis/index date, 161 of the 22,103 IBD patients (0.7%) and 572 of the 110,515 reference individuals (0.5%) had a hospital contact for anxiety, resulting in an OR of 1.4 (95% CI 1.2–1.7) for anxiety in patients with IBD compared with the reference population (Table 2). The odds were increased both 0–2 years (OR 1.3; 95% CI 1.0–1.7) before and 3–5 years (OR 1.5; 1.2–1.8) before IBD diagnosis. Similarly, five years prior to diagnosis, 559 IBD patients (2.5%) and 1984 reference individuals (1.8%) had a hospital contact for depression, resulting in an increased OR of 1.4 (95% CI 1.3–1.6) for depression prior to IBD diagnosis. We found no association between IBD and bipolar disorder in the five years before IBD diagnosis. When we examined anxiety and depression in a broader perspective, i.e., also including cases treated outside hospitals, 4215 (19.1%) of the patients with IBD had at least one dispensed prescription for antidepressants in the 5 years before IBD diagnosis, compared with 15,309 (13.9%) of the reference population (OR 1.5; 95% CI 1.4–1.5).
Table 2.
Frequency and odds of having a hospital contact for anxiety, depression, or bipolar disorders or having used antidepressants in the 0–5 years, 0–2 years and 3–5 years leading up to IBD diagnosis/index date.
| IBD |
Crohn's disease |
Ulcerative colitis |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Patients | References | OR (95% CI) | Patients | References | OR (95% CI) | Patients | References | OR (95% CI) | |
| Total | 22,103 | 110,515 | 6738 | 33,690 | 15,365 | 76,825 | |||
| Anxiety | |||||||||
| 0–5 years | 161 (0.7%) | 572 (0.5%) | 1.4 (1.2–1.7) | 44 (0.7%) | 195 (0.6%) | 1.1 (0.8–1.6) | 117 (0.8%) | 377 (0.5%) | 1.6 (1.3–1.9) |
| 0–2 years | 85 (0.4%) | 321 (0.3%) | 1.3 (1.0–1.7) | 26 (0.4%) | 108 (0.3%) | 1.2 (0.8–1.8) | 59 (0.4%) | 213 (0.3%) | 1.4 (1.0–1.9) |
| 3–5 years | 98 (0.4%) | 337 (0.3%) | 1.5 (1.2–1.8) | 28 (0.4%) | 114 (0.3%) | 1.2 (0.8–1.9) | 70 (0.5%) | 223 (0.3%) | 1.6 (1.2–2.1) |
| Depression | |||||||||
| 0–5 years | 559 (2.5%) | 1984 (1.8%) | 1.4 (1.3–1.6) | 191 (2.8%) | 595 (1.8%) | 1.6 (1.4–1.9) | 368 (2.4%) | 1388 (1.8%) | 1.3 (1.2–1.5) |
| 0–2 years | 368 (1.7%) | 1192 (1.1%) | 1.6 (1.4–1.7) | 128 (1.9%) | 365 (1.1%) | 1.8 (1.4–2.2) | 240 (1.6%) | 827 (1.1%) | 1.5 (1.3–1.7) |
| 3–5 years | 327 (1.5%) | 1219 (1.1%) | 1.3 (1.2–1.5) | 107 (1.6%) | 354 (1.1%) | 1.5 (1.2–1.9) | 220 (1.4%) | 865 (1.1%) | 1.3 (1.1–1.5) |
| Bipolar disorder | |||||||||
| 0–5 years | 46 (0.2%) | 268 (0.2%) | 0.9 (0.6–1.2) | 15 (0.2%) | 69 (0.2%) | 1.1 (0.6–1.9) | 31 (0.2%) | 199 (0.3%) | 0.8 (0.5–1.1) |
| 0–2 years | 34 (0.2%) | 203 (0.2%) | 0.8 (0.6–1.2) | 12 (0.2%) | 52 (0.2%) | 1.2 (0.6–2.2) | 22 (0.1%) | 151 (0.2%) | 0.7 (0.5–1.1) |
| 3–5 years | 34 (0.2%) | 199 (0.2%) | 0.9 (0.6–1.2) | 12 (0.2%) | 52 (0.2%) | 1.2 (0.6–2.2) | 22 (0.1%) | 147 (0.2%) | 0.7 (0.5–1.2) |
| Use of antidepressants | |||||||||
| 0–5 years | 4215 (19.1%) | 15,309 (13.9%) | 1.5 (1.4–1.5) | 1340 (19.9%) | 4535 (13.5%) | 1.6 (1.5–1.7) | 2875 (18.7%) | 10,774 (14.0%) | 1.4 (1.3–1.5) |
| 0–2 years | 3308 (15.0%) | 11,605 (10.5%) | 1.5 (1.4–1.6) | 1050 (15.6%) | 3462 (10.3%) | 1.6 (1.5–1.7) | 2258 (14.7%) | 8143 (10.6%) | 1.5 (1.4–1.5) |
| 3–5 years | 3012 (13.6%) | 11,167 (10.1%) | 1.4 (1.3–1.5) | 962 (14.3%) | 3267 (9.7%) | 1.6 (1.4–1.7) | 2050 (13.3%) | 7900 (10.3%) | 1.3 (1.3–1.4) |
IBD, Inflammatory bowel disease; OR, Odds ratio; CI, Confidence interval.
On analysis of UC and CD separately, the increased odds of anxiety were only statistically significant for patients with UC (OR 1.6; 95% CI 1.3–1.9), whereas the odds for depression and antidepressant use were increased in both patients with CD (OR 1.6; 95% CI 1.4–1.9 for depression and OR 1.6; 95% CI 1.5–1.7 for antidepressants) and UC (OR 1.3; 95% CI 1.2–1.5 for depression and OR 1.4; 95% CI 1.3–1.5 for antidepressants). There were no differences based on sex, but patients with IBD diagnosed in the youngest age group (18–39 years) had lower odds of both a hospital contact for depression and for having a dispensed prescription for antidepressants compared with the older-onset groups (40–59 years and 60+ years) (Supplementary Table S2).
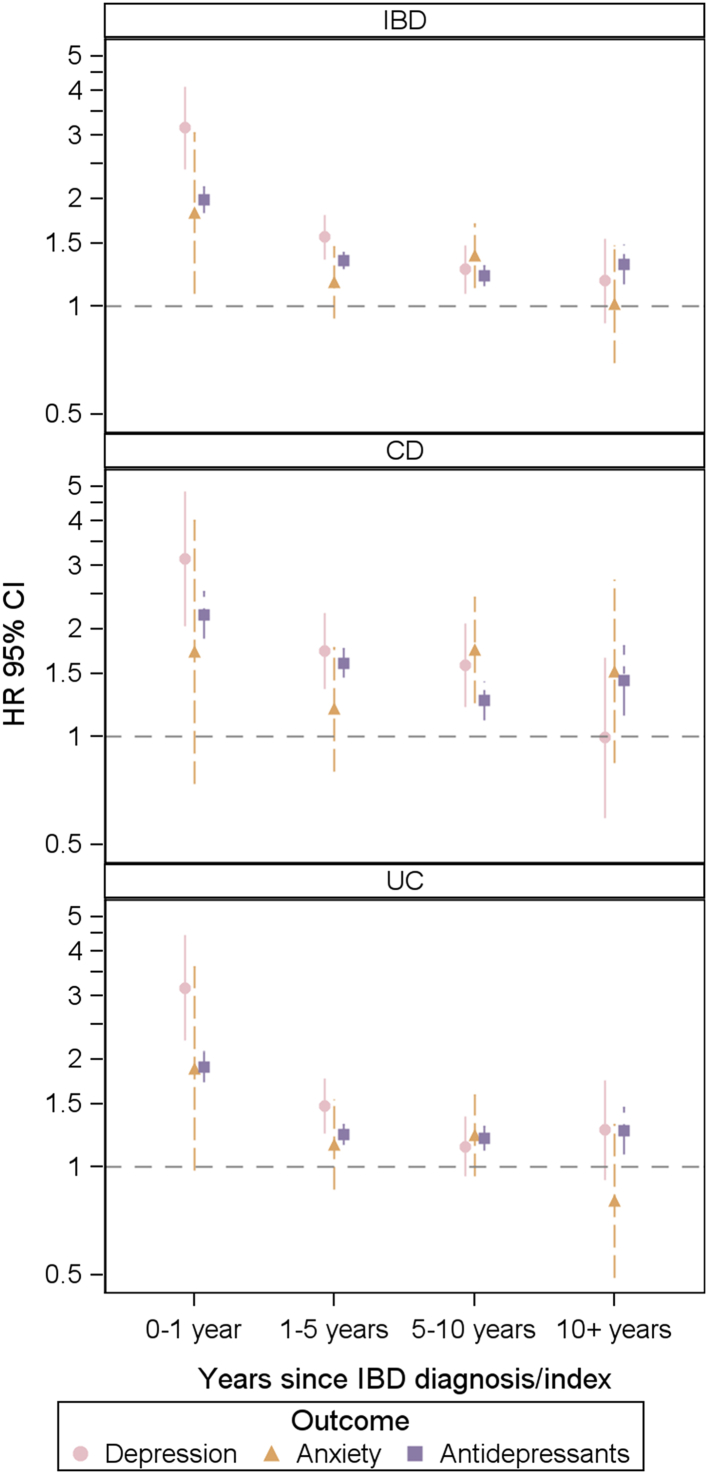
Risk of anxiety, depression, and bipolar disorder in the ten years after IBD diagnosis
To study the risk of psychiatric disease after IBD diagnosis, we included 17,817 patients with IBD and 94,884 reference individuals with no contacts for anxiety, depression, bipolar disorder, or use of antidepressants in the five years before IBD diagnosis/index date (Supplementary Table S3). The mean follow-up time for patients with IBD and references was 9.8 years for the outcome of anxiety, 9.7 years for depression, 9.8 years for bipolar disorder, and 8.9 years for use of antidepressants.
Cox-regression analyses showed that patients with IBD had an increased risk of hospital contacts for anxiety (HR 1.3 95% CI 1.1–1.5) and depression (HR 1.5; 95% CI 1.4–1.7), and an increased risk of having a dispensed prescription for antidepressants (HR 1.4; 95% CI 1.3–1.4) (Table 3) compared with reference individuals. The risk of depression (HR 3.2; 95% 2.4–4.1) and use of antidepressants (HR 2.0; 95% CI 1.8–2.2) was highest in the first year after IBD diagnosis, and the risk remained significantly increased for ten years after IBD diagnosis (Fig. 2). On subgroup-analysis, the risk of anxiety was statistically significantly increased for patients with CD (HR 1.5; 95% CI 1.2–1.9), but not for UC (HR 1.2; 95% CI 1.0–1.4). Patients with IBD did not overall have an increased risk of developing bipolar disorder after IBD diagnosis, but the risk was increased in patients with CD (HR 1.9; 1.2–3.1). Patients with IBD diagnosed between age 18 and 39 had a lower risk of depression (HR 1.2; 95% CI 1.0–1.4) or antidepressant use (HR 1.2; 95% CI 1.2–1.3) than those diagnosed after age 40. There were no differences in risk between females and males (Supplementary Table S4).
Table 3.
Frequency and risk of having anxiety, depression or bipolar disorders or receiving antidepressants in the ten years following IBD diagnosis or cohort entry in individuals who had not had psychiatric disorders or received antidepressants in the 5 years prior.
| IBD (n = 17,817) |
Crohn's disease (n = 5378) |
Ulcerative colitis (n = 12,439) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Events | Person-years | IR/1000 PY | HR (95% CI) | Events | Person-years | IR/1000 PY | HR (95% CI) | Events | Person-years | IR/1000 PY | HR (95% CI) | |
| Anxiety | ||||||||||||
| References | 1062 | 931,400 | 1.14 | 1 (ref) | 344 | 284,800 | 1.21 | 1 (ref) | 718 | 646,600 | 1.11 | 1 (ref) |
| IBD | 247 | 171,100 | 1.44 | 1.3 (1.1–1.5) | 93 | 51,100 | 1.82 | 1.5 (1.2–1.9) | 154 | 120,000 | 1.28 | 1.2 (1.0–1.4) |
| Depression | ||||||||||||
| References | 2119 | 925,100 | 2.29 | 1 (ref) | 672 | 282,800 | 2.38 | 1 (ref) | 1447 | 642,400 | 2.25 | 1 (ref) |
| IBD | 577 | 169,200 | 3.41 | 1.5 (1.4–1.7) | 202 | 50,400 | 4.01 | 1.7 (1.5–2.0) | 375 | 118,800 | 3.16 | 1.4 (1.3–1.6) |
| Bipolar disorder | ||||||||||||
| References | 198 | 934,500 | 0.21 | 1 (ref) | 64 | 285,900 | 0.22 | 1 (ref) | 134 | 648,600 | 0.21 | 1 (ref) |
| IBD | 46 | 171,100 | 0.27 | 1.2 (0.9–1.7) | 23 | 51,400 | 0.45 | 1.9 (1.2–3.1) | 23 | 120,500 | 0.19 | 0.9 (0.6–1.4) |
| Use of antidepressants | ||||||||||||
| References | 14,719 | 850,800 | 17.30 | 1 (ref) | 4412 | 260,200 | 16.95 | 1 (ref) | 10,307 | 590,500 | 17.45 | 1 (ref) |
| IBD | 3565 | 150,800 | 23.65 | 1.4 (1.3–1.4) | 1160 | 44,300 | 26.16 | 1.6 (1.5–1.7) | 2405 | 106,400 | 22.60 | 1.3 (1.3–1.4) |
IBD, Inflammatory bowel disease; IR, Incidence rate; PY, Person years; HR, Hazard ration; CI, Confidence interval.
Fig. 2.
Risk of a hospital contact for depression and anxiety, and risk of having a dispensed prescription for antidepressants in patients with IBD, CD, and UC compared with the reference population in the years after IBD diagnosis/index date. HR, Hazard Ratio; CI, Confidence interval; IBD, Inflammatory bowel disease; CD, Crohn's disease; UC, Ulcerative colitis. Symbols represent the estimate for each outcome and vertical lines represent the confidence interval. Bipolar disorder not represented because of too few cases.
Discussion
In this nationwide cohort study including more than 22,000 patients with IBD, we characterised the psychiatric comorbidity longitudinally year by year from before to around and after IBD diagnosis to further the understanding of the burden presented by these diseases over the lifetime of patients with IBD. We found that patients with IBD consistently have a higher occurrence of anxiety and depression starting at least five years before IBD diagnosis and continuing for at least ten years following IBD diagnosis compared with individuals from the general population. The pattern was present both for severe anxiety and depression as measured by hospital contacts and for a broader range of cases as measured by dispensed prescriptions for antidepressants. The increased risk of psychiatric disease and treatment hereof both pre- and postdiagnosis was observed in both UC and CD patients and in women and men.
Unlike most previous population-based studies on this topic,13,14,20, 21, 22 we examined the occurrence of psychiatric diseases in the same population over time both before and after IBD diagnosis. Our findings of an increased frequency of anxiety and depression as well as antidepressant use even 3–5 years before IBD diagnosis are in line with a 2019 study from Canada, where patients with IBD had increased incidence of depression five years before and of anxiety three years before IBD diagnosis.23 It is unlikely that this is merely due to diagnostic delay of IBD, which is usually less than a year in Denmark.24 It is possible that it could be due to subclinical inflammation present in the years before IBD development, or the diseases may share biological pathways that cause susceptibilities in individuals to both IBD, anxiety and depression. The increased levels of anxiety and depression and antidepressant use indicate that people are struggling even before getting an IBD diagnosis, and the stress could trigger onset of IBD, as has been previously suggested,25 though it remains to be robustly established how much perceived stress affects symptoms of IBD and bowel inflammation measured objectively.12,26
We also observed increased risk of new-onset anxiety and depression at least ten years after IBD diagnosis both for severe and for more moderate expressions of anxiety and depression. The risk was particularly high in the first year after diagnosis, which is in line with findings from a Swedish population-based study.5 The high diagnostic frequency of psychiatric comorbidity around the time of IBD-diagnosis indicates a particularly high strain from the bowel-symptoms and from dealing with being diagnosed with a chronic illness. It could also point to an early window of opportunity for managing the psychiatric comorbidities while potentially also improving the course of IBD, since psychiatric comorbidity has been suggested to increase risk of active IBD.11
Depression was more frequent than anxiety in both the IBD and the reference population. The connection between IBD and depression has been partly explained by several mechanisms, including impaired vagal nerve signalling, changes in brain morphology, nitric oxide overproduction in the brain, and circulating pro-inflammatory cytokines in the periphery and in the brain.12 However, it is important to note that anxiety is predominantly treated in general practice and specialist private practice, which means that it is much more frequent than what is reflected in data on hospital contacts.
The use of antidepressants in the Danish population rose during the study period and peeked around the year 2010, since when it slightly decreased,27 which we took into account in our study design by time-dependent matching. Throughout the study period, patients with IBD had a higher use of antidepressants than individuals from the general population, particularly around the time of and in the first years after IBD diagnosis. While antidepressants are used for multiple conditions such as stress, PTSD, and chronic pain, the vast majority of prescriptions are given for depression. In the Danish National Prescription Registry, 78% of prescriptions for antidepressants that contained indications were given for depression and 11% for anxiety. It is thus appropriate to view the increased use of antidepressants in the IBD population as a measure of a broader spectrum of anxiety and depression disease that is possibly more indicative of mental health struggles than hospital contacts alone, as the hospital contacts represent only patients with severe anxiety and depression.
In the stratified analyses, the youngest age group (18–39 years) had increased risk of a hospital contact for depression and of antidepressant use, but their risk was lower than that of the older age groups both before and after IBD diagnosis. The differences were statistically significant despite similar background frequencies of depression in the groups and despite higher background frequencies of antidepressant use in the older groups compared with the group aged 18–39. This could reflect a particular vulnerability in older patients with IBD as a result of a longer delay in diagnosis, which could lead to worse mental health, or it could be because of environmental factors that likely have a stronger influence on IBD development in the older relative to genetics that are probably more important for IBD development in the young.
Patients with CD and UC differed slightly in our analyses. Patients with CD had slightly higher increased risk of a hospital contact for depression and for having a prescription for antidepressants both in the years before and in the years following IBD diagnosis. This is in line with previous studies suggesting that patients with CD are more vulnerable to psychiatric comorbidity than patients with UC.14,20
We found no differences in relative risk between males and females, which is consistent with a 2019 study from South Korea.20 The rates of all outcomes were higher in both females with IBD and those from the background population, reflecting higher absolute rates of anxiety, depression, and bipolar disorder in females.
Bipolar disorder was not associated with IBD, except for patients with CD who had an increased risk of having a hospital contact for bipolar disorder in the years following IBD diagnosis. This could be an incidental finding, or it may be an effect of steroids given for CD that can lead to hypomania. The possible impact of steroid use on the association of IBD with anxiety, depression, and bipolar disorder merits further investigation, as steroids are well known to cause psychiatric adverse effects.28
A major strength of this work lies in the National Danish Registers, which contain complete information on all included individuals. We were able to include a large sample of patients with IBD that was unselected and represented all IBD patients in Denmark during the study period, and by using time-dependent matching, we were able to account for period effects. The cohort is thus representative for Denmark, and we believe that it is generalizable to other populations as well. We used well-validated criteria for identifying patients with IBD ensuring a high validity (PPV 95%).17 We ensured precision in time of diagnosis by restricting the population to individuals who lived in Denmark in the five years before IBD diagnosis and who had the two IBD contacts as their first registrations for IBD. While the patient registers contain information from in- and out-patient hospital contacts and thus capture those with severe psychiatric disease, the prescription register contains information on all those treated not only in hospital settings but also in General practice and specialist private practice. We used both hospital contacts for anxiety, depression, and bipolar disorder as well as dispensed prescriptions for antidepressants as outcomes, which allowed us to capture a large spectrum of outcome severity. Uniquely, we were able to follow the cohort longitudinally both back in time and year by year after IBD diagnosis, rather than focusing on just one timepoint either before or after IBD diagnosis. This enabled us to assess the longitudinal burden of psychiatric comorbidity in patients with IBD.
This study also carries potential limitations. While our national registers contain large amounts of information, we cannot obtain granular data on disease activity, which would have been useful to include in the analyses. Antidepressants are used for several indications, but as mentioned above, 89% of prescriptions were indicated for depression or anxiety, and less than 2% of prescriptions were for pain. Misclassification of outcomes cannot be completely ruled out, but as there is an ongoing data validation process in the Danish registers,16 this is likely a minor issue. Patients with IBD could be more frequently diagnosed with psychiatric diseases as an effect of more often being seen by a doctor resulting in surveillance bias. One way to try to account for surveillance bias is to adjust for number of hospital contacts. In this study, however, we compared the risk of psychiatric diseases in patients with IBD to that of individuals from the background population. Adjustment for hospital contacts would have resulted in a comparison between patients with IBD and patients with other chronic diseases. Still, surveillance bias is unlikely to be the only explanation for the continually increased risk of anxiety and depression in patients with IBD. The mean age of diagnosis for patients with IBD in this study was relatively high (45.9 years), in part because we excluded all those diagnosed before age 18, yet it matches another recent study which found that age of onset for UC has increased in Denmark.29 We did not adjust for other comorbidities, as our goal was to investigate the increased burden of the outcomes over time in patients with IBD compared with the general population. It would be interesting for future investigations to adjust for comorbidities, for instance using the Charlson comorbidity index, to attempt to deduct how much of the co-occurrence that can be directly attributed to IBD.
In conclusion, our nationwide population-based study with access to both pre- and post-diagnostic data from both hospitals, out-patient clinics, and pharmacies, showed a clinically significant burden of anxiety and depression in patients with IBD continually from at least five years before diagnosis to at least ten years following IBD diagnosis. The risk of depression was particularly high around the time of diagnosis and was highest in those diagnosed with IBD after the age of 40. These results demonstrate that patients with IBD are vulnerable to mental health struggles and could benefit from comprehensive care that include evaluation and management of psychiatric comorbidity, with special attention at the time of IBD diagnosis. Future research should focus on understanding the mechanisms underlying the co-occurrence of the diseases and on improving the detection and management of concurrent anxiety and depression.
Contributors
TB, GP, KA, and TJ conceived of and designed the study and collected and analysed the data. TB drafted the manuscript. TB, KA, GP, and TJ verified the data. All authors had access to and interpreted the data, revised the manuscript, and approved the final manuscript. All authors accept responsibility for the decision to submit the manuscript for publication.
Data sharing statement
Data for this study are drawn from the Danish national registers (https://sundhedsdatastyrelsen.dk) that cannot be made publicly available, as they are protected by the Danish Act on Processing of Personal Data. Access to the register data is achieved through application to and approval from the Danish Data Protection Agency and the Danish Health Data Authority.
Declaration of interests
TB: None. GP: None. KA: Board member, the Epidemiological Committee of the European Crohn's and Colitis Organization and the Danish Society for Pharmacoepidemiology. LK: LK is co-founder, consultant, and equity owner of Trellus Health. LK is a consultant to AbbVie, Pfizer, Takeda, and Eli Lilly. LK is on the Board of directors at the Rome Foundation. AA: AA has received payment or honoraria from Takeda and Pfizer. TJ: TJ has received support for the present manuscript from the Danish National Research Foundation, the Lundbeck Foundation, and the Aage og Johanne Louis-Hansen Fond. TJ is a member of the Board of the Danish medical society Selskab for Teoretisk og Anvendt Terapi.
Acknowledgements
This study was supported by the Danish National Research Foundation [grant number DNRF148], the Lundbeck Foundation [grant number R313-2019-857], and Aage og Johanne Louis-Hansens Fond [grant number 9688-3374 TJS].
Footnotes
Translation: for the Danish translation of the abstract see Supplementary Materials section.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.101986.
Appendix A. Supplementary data
References
- 1.Molodecky N.A., Soon I.N.G.S., Rabi D.M., et al. Increasing incidence and prevalence of the inflammatory bowel diseases. Gastroenterology. 2012;142:46–54. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Høivik M.L., Moum B., Solberg I.C., et al. Work disability in inflammatory bowel disease patients 10 years after disease onset: results from the IBSEN Study. Gut. 2013;62:368–375. doi: 10.1136/gutjnl-2012-302311. [DOI] [PubMed] [Google Scholar]
- 3.Dubinsky M.C., Dotan I., Rubin D.T., et al. Burden of comorbid anxiety and depression in patients with inflammatory bowel disease: a systematic literature review. Expert Rev Gastroenterol Hepatol. 2021;15:985–997. doi: 10.1080/17474124.2021.1911644. [DOI] [PubMed] [Google Scholar]
- 4.Williet N., Sarter H., Gower-Rousseau C., et al. Patient-reported outcomes in a French nationwide survey of inflammatory bowel disease patients. J Crohns Colitis. 2017;11:165–174. doi: 10.1093/ecco-jcc/jjw145. [DOI] [PubMed] [Google Scholar]
- 5.Ludvigsson J.F., Olén O., Larsson H., et al. Association between inflammatory bowel disease and psychiatric morbidity and suicide: a Swedish nationwide population-based cohort study with sibling comparison. J Crohns Colitis. 2021;15:1824–1836. doi: 10.1093/ecco-jcc/jjab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barberio B., Zamani M., Black C.J., Savarino E.V., Ford A.C. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359–370. doi: 10.1016/S2468-1253(21)00014-5. [DOI] [PubMed] [Google Scholar]
- 7.Eaton W.W., Pedersen M.G., Nielsen P.R., Mortensen P.B. Autoimmune diseases, bipolar disorder, and non-affective psychosis. Bipolar Disord. 2010;12:638–646. doi: 10.1111/j.1399-5618.2010.00853.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein C.N., Hitchon C.A., Walld R., et al. Increased burden of psychiatric disorders in inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:360–368. doi: 10.1093/ibd/izy235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong J.J., Sceats L., Dehghan M., et al. Depression and health care use in patients with inflammatory bowel disease. J Crohns Colitis. 2019;13:19–26. doi: 10.1093/ecco-jcc/jjy145. [DOI] [PubMed] [Google Scholar]
- 10.Irving P., Barrett K., Nijher M., de Lusignan S. Prevalence of depression and anxiety in people with inflammatory bowel disease and associated healthcare use: population-based cohort study. Evid Based Ment Health. 2021;24:102–109. doi: 10.1136/ebmental-2020-300223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fairbrass K.M., Lovatt J., Barberio B., Yuan Y., Gracie D.J., Ford A.C. Bidirectional brain–gut axis effects influence mood and prognosis in IBD: a systematic review and meta-analysis. Gut. 2022;71:1773–1780. doi: 10.1136/gutjnl-2021-325985. [DOI] [PubMed] [Google Scholar]
- 12.Bisgaard T.H., Allin K.H., Keefer L., Ananthakrishnan A.N., Jess T. Depression and anxiety in inflammatory bowel disease: epidemiology, mechanisms and treatment. Nat Rev Gastroenterol Hepatol. 2022;19:717–726. doi: 10.1038/s41575-022-00634-6. [DOI] [PubMed] [Google Scholar]
- 13.Blackwell J., Saxena S., Petersen I., et al. Depression in individuals who subsequently develop inflammatory bowel disease: a population–based nested case–control study. Gut. 2021;70:1642–1648. doi: 10.1136/gutjnl-2020-322308. [DOI] [PubMed] [Google Scholar]
- 14.Umar N., King D., Chandan J.S., et al. The association between IBD and mental ill health: a retrospective cohort study using data from UK primary care. Aliment Pharmacol Ther. 2022;56:814–822. doi: 10.1111/apt.17110. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt M., Pedersen L., Sørensen H.T. The Danish Civil registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt M., Schmidt S.A.J., Sandegaard J.L., Ehrenstein V., Pedersen L., Sørensen H.T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobsen H.A., Jess T., Larsen L. Validity of inflammatory bowel disease diagnoses in the Danish National Patient Registry: a population-based study from the North Denmark region. Clin Epidemiol. 2022;14:1099–1109. doi: 10.2147/CLEP.S378003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mors O.L.E., Perto G.P., Mortensen P.B.O. The Danish psychiatric central research register. Scand J Public Health. 2011;39:54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 19.Wallach Kildemoes H., Toft Sørensen H., Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39:38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 20.Choi K., Chun J., Han K., et al. Risk of anxiety and depression in patients with inflammatory bowel disease: a nationwide, population-based study. J Clin Med. 2019;8:654. doi: 10.3390/jcm8050654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frolkis A.D., Vallerand I.A., Shaheen A.A., et al. Depression increases the risk of inflammatory bowel disease, which may be mitigated by the use of antidepressants in the treatment of depression. Gut. 2019;68:1606–1612. doi: 10.1136/gutjnl-2018-317182. [DOI] [PubMed] [Google Scholar]
- 22.Ananthakrishnan A.N., Khalili H., Pan A., et al. Association between depressive symptoms and incidence of Crohn's disease and ulcerative colitis: results from the nurses' health study. Clin Gastroenterol Hepatol. 2013;11:57–62. doi: 10.1016/j.cgh.2012.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marrie R.A., Walld R., Bolton J.M., et al. Rising incidence of psychiatric disorders before diagnosis of immune-mediated inflammatory disease. Epidemiol Psychiatr Sci. 2019;28:333–342. doi: 10.1017/S2045796017000579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jess T., Riis L., Vind I., et al. Changes in clinical characteristics, course, and prognosis of inflammatory bowel disease during the last 5 decades: a population-based study from Copenhagen, Denmark. Inflamm Bowel Dis. 2007;13:481–489. doi: 10.1002/ibd.20036. [DOI] [PubMed] [Google Scholar]
- 25.Melinder C., Hiyoshi A., Fall K., Halfvarson J., Montgomery S. Stress resilience and the risk of inflammatory bowel disease: a cohort study of men living in Sweden. BMJ Open. 2017;7:1–8. doi: 10.1136/bmjopen-2016-014315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maunder R., Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Mol Med. 2008;8:247–252. doi: 10.2174/156652408784533832. [DOI] [PubMed] [Google Scholar]
- 27.https://medstat.dk
- 28.Warrington T.P., Bostwick J.M. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81:1361–1367. doi: 10.4065/81.10.1361. [DOI] [PubMed] [Google Scholar]
- 29.Agrawal M., Christensen H.S., Bøgsted M., Colombel J.F., Jess T., Allin K.H. The rising burden of inflammatory bowel disease in Denmark over two decades: a nationwide cohort study. Gastroenterology. 2022;163:1–8. doi: 10.1053/j.gastro.2022.07.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.