Abstract
Background:
While massive and irreparable rotator cuff tears (MIRCTs) have been abundantly studied, inconsistent definitions in the literature and theories about pain and dysfunction related to them can be difficult to navigate when considering an individual patient.
Purpose:
To review the current literature for definitions and critical concepts that drive decision-making for MIRCTs.
Study Design:
Narrative review.
Methods:
A search of the PubMed database was performed to conduct a comprehensive literature review on MIRCTs. A total of 97 studies were included.
Results:
Recent literature reflects added attention to clarifying the definitions of “massive, “irreparable,” and “pseudoparalysis.” In addition, numerous recent studies have added to the understanding of what generates pain and dysfunction from this condition and have reported on new techniques for addressing them.
Conclusion:
The current literature provides a nuanced set of definitions and conceptual foundations on MIRCTs. These can be used to better define these complex conditions in patients when comparing current surgical techniques to address MIRCTs, as well as when interpreting the results of new techniques. While the number of effective treatment options has increased, high-quality and comparative evidence on treatments for MIRCTs is lacking.
Keywords: rotator cuff tear, massive, irreparable, pseudoparalysis
Massive and irreparable rotator cuff tears (MIRCTs) present a challenging problem to shoulder surgeons; while they have been abundantly studied, the quantity and subjective quality of research can be difficult to navigate when considering an individual patient. These difficulties stem in large part from inconsistent definitions in the literature that make it difficult to understand and refine indications for the various techniques to treat these patients. Recent literature has added to our conceptual understanding of these tears and has attempted to build consensus on the terms to describe them. The purpose of this article was to review the current literature for definitions and critical concepts that drive decision-making for MIRCTs.
Study Design
A search of the PubMed database was performed to conduct a comprehensive literature review on MIRCTs using the search term “massive irreparable rotator cuff tear.” A total of 97 studies were included (see the References section).
Anatomy and Biomechanics
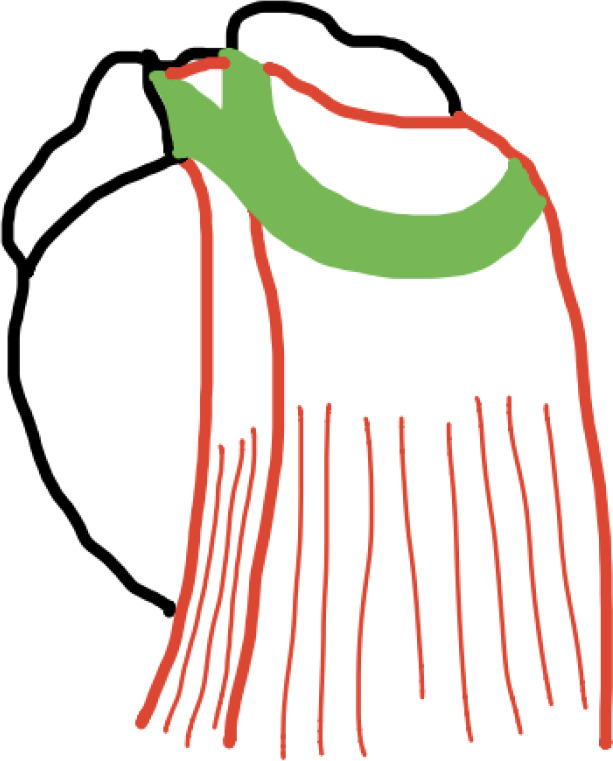
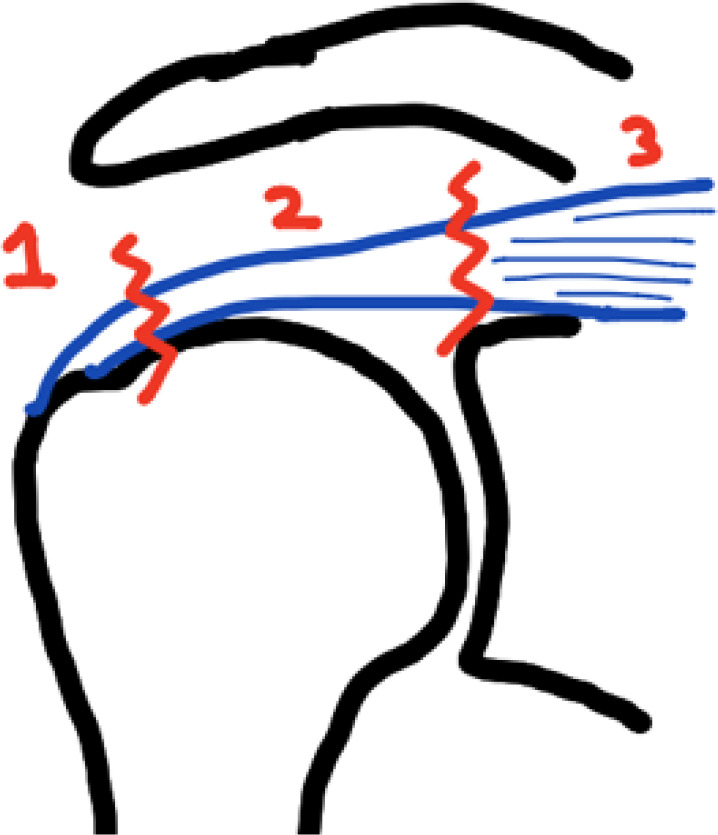
The 4 rotator cuff muscles work in concert to dynamically stabilize the humeral head on the shallow glenoid concavity that provides little osseous constraint compared with other joints, such as the hip. The balance of these muscle groups is best described as force couples. 10 The superior moment of the deltoid is balanced by the compressive action of the supraspinatus and slight inferiorly directed force vector of the inferior teres minor and subscapularis; this is referred to as the vertical or coronal force couple. Loss of vertical couple balance with a supraspinatus tear creates an unimpeded superiorly directed force on the humerus, resulting in proximal humeral migration noted on plain films. The internal rotation and anterior direct moment of the subscapularis are balanced by the infraspinatus and teres minor; this is referred to as the axial or horizontal force couple (Figure 1). Loss of horizontal couple balance results in the inability to maintain a centered humeral head or as the rotational function of the tendon involved. In short, massive rotator cuff tears (MRCTs) cause imbalance in the horizontal and vertical force couples, which makes it difficult to maintain a stable glenohumeral fulcrum for overhead motion.
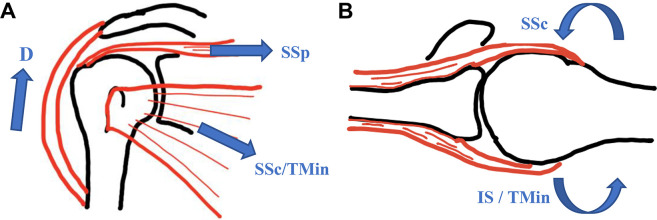
Figure 1.
Schematic of horizontal and vertical rotator cuff force couples. (A) The vertical force couple is described as the superiorly directed force of the deltoid (D) balanced by the compressive action of the supraspinatus (SSp) and inferiorly directed forces of the inferior subscapularis (SSc) and teres minor (TMin). (B) The horizontal force couple is described as the balance between the internally rotating force of the SSc and externally rotating forces of the infraspinatus (IS) and TMin.
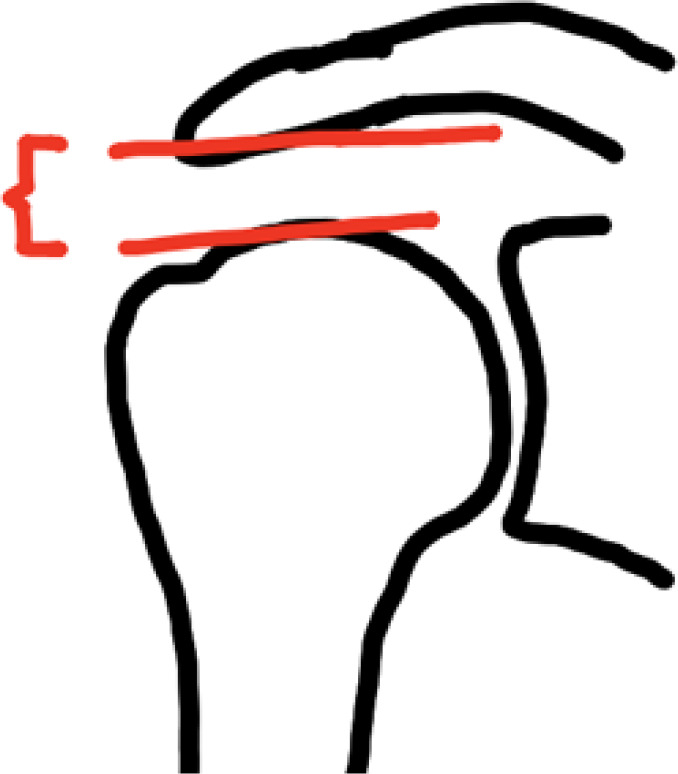
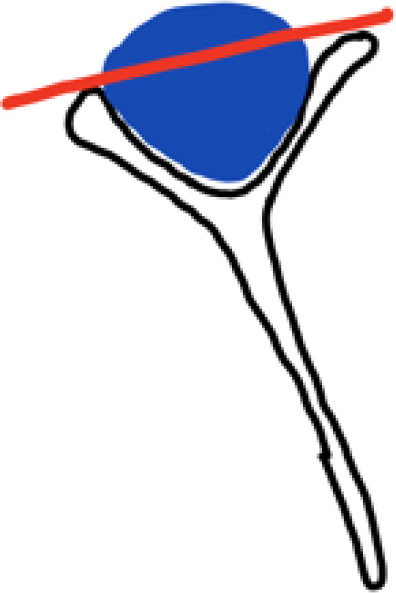
Force from the rotator cuff is transmitted primarily through the rotator cable, which is a semicircular thickening in the supraspinatus and infraspinatus tendon perpendicular to its fibers that attach anteriorly around the superior bicipital groove (Figure 2) and posteriorly at the inferior half of the infraspinatus. These 2 attachment points transmit tension from the muscle between, thus shielding tissue lateral to the cable between its attachment point (“rotator crescent”). This concept is commonly referred to as the “suspension bridge” model. 10 Tears in the crescent zone may not affect the horizontal force couple, while disruptions of the cable attachments may destabilize the shoulder. 12
Figure 2.
Schematic of the anterior rotator cable attachment. The anterior rotator cable attaches in 2 limbs around the superior portion of the bicipital groove. Tear patterns extending from the posterosuperior cuff to the superior portion of the subscapularis can be assumed to involve this attachment and may be associated with more profound loss of function.
The rotator interval is the space between the anterior edge of the supraspinatus and superior edge of the subscapularis. It contains the coracohumeral ligament and superior glenohumeral ligament. Release of these ligaments can be helpful in mobilizing the subscapularis and supraspinatus tendons. 67
The coracoacromial ligament (CAL) and acromion together form an arch on the superior aspect of the subacromial space. This arch can provide a fulcrum for glenohumeral motion in patients with proximal migration. 61 CAL incompetence or injury coupled with proximal migration can allow for anterosuperior escape of the humeral head past this arch, and over time this subluxation may become irreducible with associated inferior capsule contracture.
The causes of loss of function may be different than the pain generators. Proximal migration of the humeral head from the unopposed superior pull of the deltoid results in humeral head abutment against the acromion. The contour of the greater tuberosity and remnant cuff tissue can generate a painful crepitus and bursitis in this new subacromial articulation. In addition, the long head of the biceps tendon (LHBT) can generate pain. Biomechanical studies show that a posterosuperior tear involving the inferior infraspinatus leads to superior and anterosuperior glenohumeral translation, and loading of the biceps tendon in this situation centers the head 92 and prevents posterior subluxation with forward elevation. 76 Moreover, loss of the biceps pulley formed by the superior portion of the subscapularis in anterosuperior tears can allow LHBT subluxation. 32 Thus, biceps tendon pain may be understood as developing tendonitis because it is unstable or forced to play a supraphysiologic role in dynamic stability of the glenohumeral joint. Lastly, in simulated large cuff tear shoulder models, excessive force by the remaining cuff and deltoid is required to keep the joint stable during elevation 35 ; this supraphysiologic force may also generate tendonitis pain.
It has been suggested that retraction of a MRCT can create compression of the suprascapular nerve, which courses an average of 3 cm from the glenoid rim. 95 While some surgeons believe this contributes to developing atrophy, correlation studies between electromyography and magnetic resonance imaging (MRI) have shown that larger tears result in greater nerve dysfunction; however, there is no correlation with atrophy, 88 nor is the pattern of infiltration or atrophy consistent with muscle denervation. 30 Moreover, a recent prospective, randomized, double-blinded study of large and massive cuff tear repair with and without suprascapular neurolysis showed no difference in function scores at 1 year from surgery. 81
Definition of Terms
Massive Tears
The term “massive” has been defined based on multiple parameters, including
Number of torn tendons (≥2) 29
Total length of the tear, defined as the sum of medial-lateral and anterior-posterior lengths (≥5 cm) 16
Percentage of exposed humeral head 70
In 2020, a panel of experts used a Delphi method to define “massive” as retraction of the torn tendon in either the coronal or axial plane and/or at least 67% of the greater tuberosity exposed in the sagittal plane. 83 The Gerber definition of number of tendons involved is the most commonly used in the literature. 29
Irreparable Tears
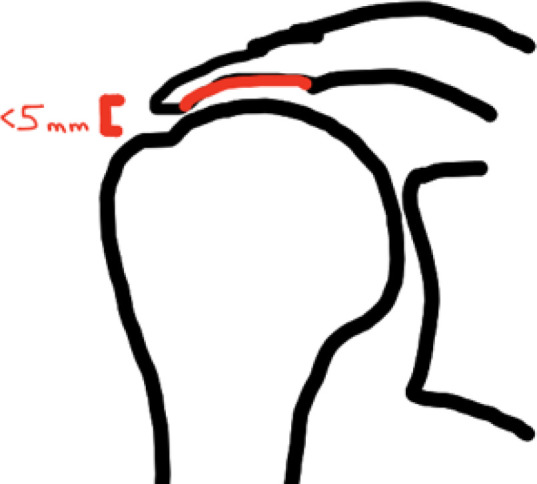
There are multiple perspectives on how a tear is defined as “irreparable.” On a fundamental level, a tendon is irreparable if the tendon stump cannot be advanced to the footprint or lateral to the articular margin (a medialized position) with a tension-free repair. The term “tension-free” is somewhat subjective but has been defined as being able to reach the native or medialized footprint in neutral rotation and abduction. No clinical study supports limiting how much abduction can be tolerated to accommodate repair, and postoperative abduction bracing does not appear to provide a benefit to structural or clinical outcomes. 73 High tension at the repair site is common because of the natural history of muscle fiber and tendon stump shortening, 56 as well as loss of tissue elasticity17,18 with long-standing tears. On a histologic level, the loss of elasticity is related to fatty infiltration, and scarring increases the passive tension of the musculotendinous unit. 30 Medialization of the repair more than 10 mm can result in large restrictions in motion, based on a cadaveric study. 96
An important caveat to deciding whether a tear cannot reach the intended repair point is that the surgeon should first use mobilization techniques to increase tendon excursion or the ability to reduce the tendon to the footprint. These include release of adhesions, interval slides, and capsule releases. Adhesions in MIRCTs are most often encountered in the undersurface of the acromion, posterior deltoid, and bursa. Excursion may also be improved by developing a plane between the capsule and labrum. 68 An interval slide is a technique in which a plane between 2 rotator cuff tendons is developed; it can be performed anteriorly through the rotator interval or posteriorly between the supraspinatus and infraspinatus. 47 An inferior capsule release improves medial-lateral tendon excursion by reducing the amount the tendon that must curve around the superior humeral head. A study of MRCT repair found that 88% of all tears could be repaired in a tension-free manner, and 62% required these techniques. 86 An equation to predict irreparability was recently developed by reviewing preoperative imaging of 758 full-thickness tears that underwent arthroscopic repair by an unspecified mobilization technique (Table 1). 42 Through the use of a cutoff value of 75%, the sensitivity and specificity for identifying irreparability were 66% and 97%, respectively, and the negative and positive predictive values were 95% and 75%, respectively. In other words, a value less than the cutoff of 75% is strongly predictive of a reparable tear, whereas a value >75% is moderately predictive of irreparability.
Table 1.
Predicting Repairability and Healing After Rotator Cuff Repair
| Predicting Irreparability (Kim et al 42 ) | Predicting Healing (Kwon et al 45 ) |
|---|---|
| 1.264 (CPP) + 0.084 (ML) – 0.472 (AHD) + 1.815 (TS) + 0.804 (SSFI) + 2.514 (TN) – 3.460 <75% is strongly predictive of repairability >75% is moderately predictive of irreparability |
≤4 points = 6% healing failure ≥5 points = 55% healing failure ≥10 points = 86% healing failure |
| Variables and Scoring | Variables and Scoring |
|
|
Tears can also be deemed irreparable if healing or functional improvement is so unreliable that attempted repair is inadvisable. These include the acromiohumeral interval, tendon stump length, high-grade fatty infiltration (≥2), age, osteoporosis, smoking, poorly controlled diabetes or hyperlipidemia, musculotendinous location, tendon delamination, and high critical shoulder angle.6,28,50 As with irreparability, recent multivariate analyses of large data sets have been used to create predictive models for retear (Table 1). 45 In a 2015 systematic review of arthroscopic repair of chronic massive cuff tears, the pooled retear rate was 79%. 37
Some may argue that repair is worthwhile despite a high retear risk because patients with structural failure can perform well clinically. This was well demonstrated by a 10-year follow-up study of 18 patients with known structural failure of a rotator cuff repair. Only 2 patients underwent reoperation (one at almost 9 years from surgery for new pain after a fall) despite progression of the Hamada grade. All others maintained pain relief and a mean American Shoulder and Elbow Surgeons score of 79. 75 Moreover, even repair with factors that portend a high risk of retear, such as grade 3 or 4 fatty infiltration, has been reported to significantly improve function scores.11,80 However, retear is associated with worse strength, 80 and laborers in particular have high rates of dissatisfaction with structural failure. 65 Given the significant added burden of the rehabilitation protocol for repair compared with nonrepair options such as debridement and reverse shoulder arthroplasty (RSA), certain patients may be unwilling to put themselves through a longer recovery for an unreliable result.
Pseudoparalysis
The term “pseudoparalysis” has been the topic of debate because of its implications on understanding clinical outcomes and indications for various techniques to treat MIRCTs. Classically, pseudoparalysis is a clinical finding that describes the inability to forward elevate the arm more than 90° with better passive motion and without another neurologic explanation for the issue (ie, C5 radiculopathy, axillary nerve injury, or plexopathy). 51
This classic definition can be problematic because of a group of patients who have limitations in elevation due to pain from subacromial space pain generators (ie, bursitis or abutment) rather than true muscle imbalance. This group of patients has been termed as having “painful loss of active elevation” (PLAE) and can be differentiated from those with true muscle weakness causing limited elevation, termed “isolated loss of active elevation,” with use of some pain-relieving measure. The most reported measure is intra-articular lidocaine. These authors also sought to describe horizontal muscle imbalance and defined 2 additional groups: “isolated loss of active external rotation” and “combined loss of active elevation and external rotation.” 7 A fifth “isolated loss of internal rotation” group exists, but this presentation is rare.
A 2017 systematic review on the definition of “pseudoparalysis” characterized the inconsistency of definitions across studies and attempted to differentiate pseudoparalysis from what they and others have termed “pseudoparesis.” 93 Pseudoparalysis was described as 0° active forward elevation (AFE), full passive forward elevation (PFE), the presence of anterosuperior escape, and no improvement with intra-articular lidocaine. By contrast, pseudoparesis was described as less than 90° AFE, full PFE, no anterosuperior escape, and improvement in elevation with intra-articular lidocaine. The vast majority of MIRCT literature has used this latter definition to describe pseudoparalysis and does not specify whether a pain-relieving measure was used at the time of examination.24,93
The presence of true pseudoparalysis is important to procedure selection, as pain-relieving operations would not be expected to restore muscle balance and improve function in these patients but may be successful in patients with PLAE. Moreover, revision rotator cuff repair has been reported to reverse pseudoparalysis in only 43% of cases when present 22 ; the poor reliability of revision repair may favor nonrepair procedures for patients with failed prior repairs and pseudoparalysis.
Critical Concepts
When possible and advisable, complete repair followed by partial repair is the best option. The definitions of “massive” and “irreparable” are critical in differentiating these tears from those that can be repaired because successful repairs result in long-term clinical benefit and milder complication profiles compared with nonrepair options. A recent study reporting 20-year outcomes of 53 patients with massive cuff tears who underwent open repair found a 10% revision rate and a mean total Constant score of 68 compared with 44 preoperatively; this score was maintained over the follow-up period. 18 Two studies similarly have found favorable function and pain relief, alongside less favorable strength and high rates of retear.20,85 Partial repair in 30 patients was recently compared with complete repair in 126 patients at a minimum 10-year follow-up; while forward flexion strength and progression of disease (ie, fatty infiltration, osteoarthritis, and size of tear) favored the complete repair group, University of California–Los Angeles scores were the same between the 2 groups. 39 Numerous other 5- and 10-year outcome studies have shown favorable results for complete and partial repair with low rates of reoperation.14,25,85,89 Of note, the percentage of humeral head coverage with repaired cuff tendon has positively correlated with functional scores.25,41 For a frame of reference, the 10-year revision rate of RSA has ranged from 12% to 43%,1,52,87 and dissatisfaction with RSA is more common for this indication (MIRCT without arthritis) than others.43,46,63 Moreover, the nature of revision procedures after RSA is generally more morbid than failed repair. Pain-relieving procedures such as debridement, biceps tenotomy, and subacromial balloon placement have been shown to not provide as much functional improvement as complete or partial repair even when postoperative structural healing was not examined.38,59,91
Which Patients or Tear Patterns Develop Pseudoparalysis?
This question has been explored through biomechanical and clinical approaches. Biomechanical studies identified disrupted MRCTs and associated disruptions in the cable attachments as causing an inability to maintain force couple balance.10,54 Without equilibrium, a fulcrum for shoulder motion cannot be obtained and pseudoparalysis ensues. 10 This theory has some clinical support from a retrospective study of 127 massive tears showing pseudoparalysis pseudoparalysis with intact cable insertions and 45% pseudoparalysis with both cables disrupted. 21
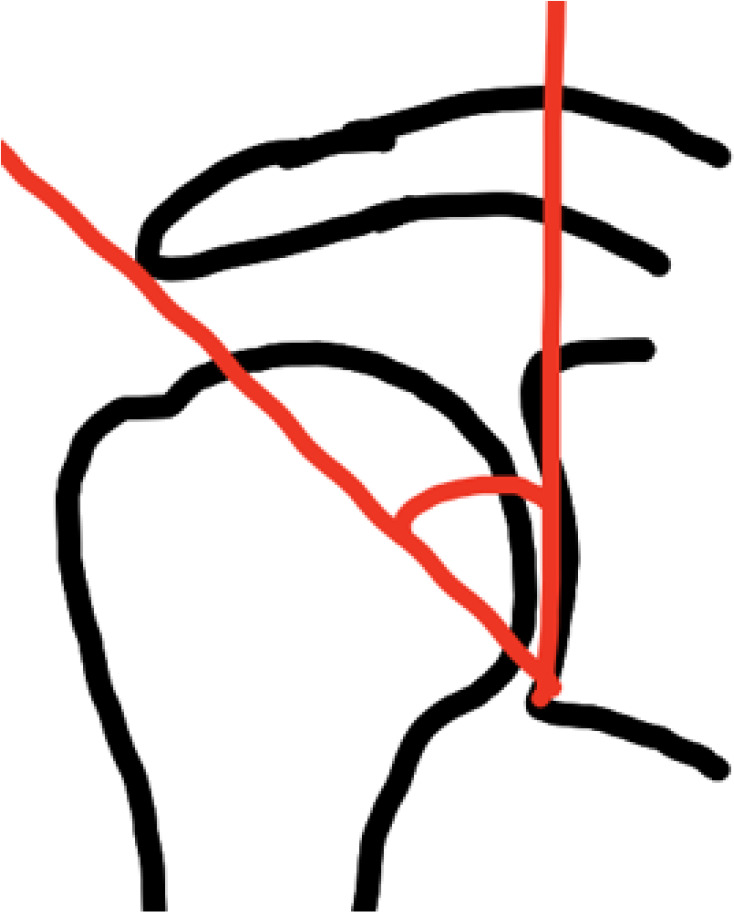
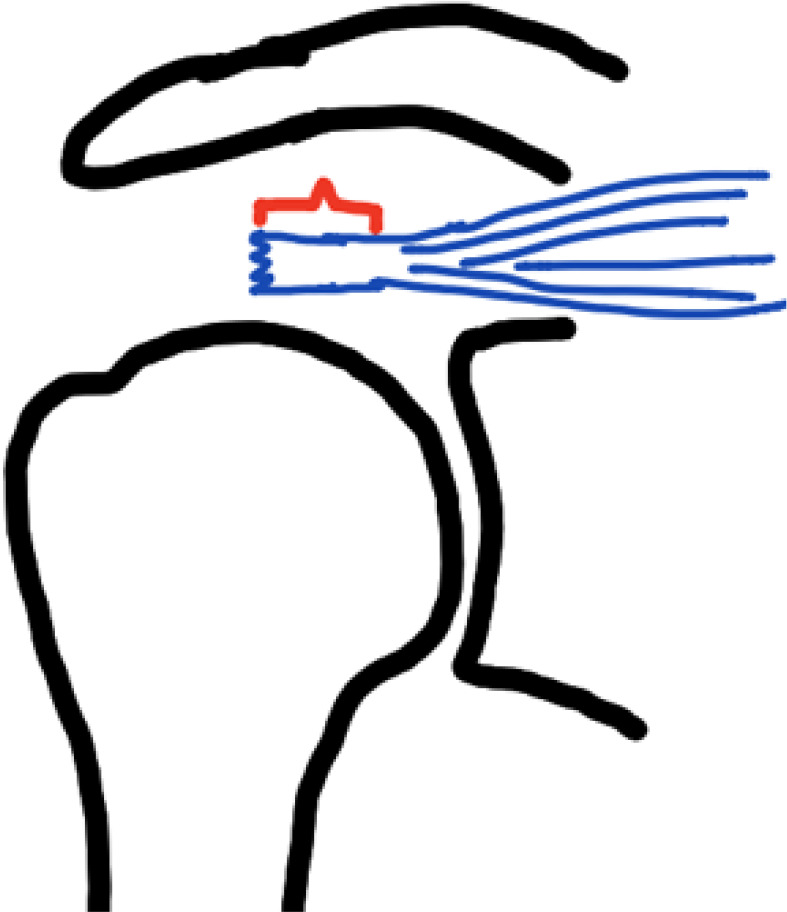
From a clinical standpoint, Collin et al 19 published a classification correlating massive tear patterns with pseudoparalysis (Figure 3). The higher rate of pseudoparalysis with type B and C patterns demonstrates the importance of entire subscapularis or 3-tendon involvement. This finding also supports the cable disruption theory, as involvement of the inferior subscapularis implies disruption completely through the upper subscapularis, where the anterior rotator cable attaches. In addition to understanding pseudoparalysis, this classification provides a useful tool for describing and studying specific tear patterns, which is not described in other methods of describing massive tears, such as number of tendons involved or humeral head area exposed.
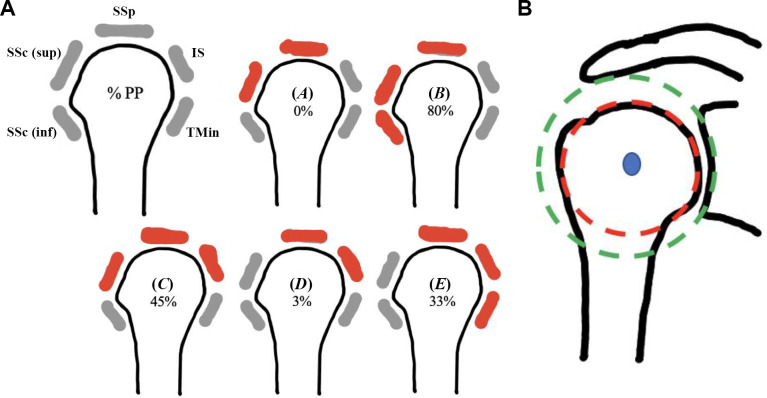
Figure 3.
Imaging findings that correlate with pseudoparalysis. (A) Collin et al 19 developed a classification for massive tear patterns (types A-E) based on the involvement of 5 portions of the rotator cuff: inferior subscapularis (SSc [inf]), superior subscapularis (SSc [sup]), supraspinatus (SSp), infraspinatus (IS), and teres minor (Tmin). These were correlated with the percentage of patients with pseudoparalysis (PP). Red and gray signify torn and intact portions of the cuff, respectively. (B) The Shoulder Abduction Moment index 9 is based on 2 circles. The green circle approximates the deltoid undersurface; it is drawn by being centered at the center of rotation and just touching the undersurface or sclerotic line of the acromion. The red circle approximates the rotator cuff moment arm; it is drawn centered on the humeral head and matching the articular surface.
Another important clinical finding that helps in understanding pseudoparalysis is the Shoulder Abduction Moment index. Described in 2018, 9 the authors found that a ratio of the moment arms of the rotator cuff and deltoid muscle (Figure 3B) less than 0.77 has a significantly higher risk for pseudoparalysis (odds ratio, 11). These findings suggest that the combination of a smaller humeral head—and therefore less intrinsic osseous stability and rotator cuff moment arm—and a long moment arm for the deltoid—a greater decentering force—predict pseudoparalysis in addition to the tear pattern and involvement of the rotator cable attachments.
Patient Evaluation
Presentation and Physical Examination
Patients with MIRCTs are evaluated with a spectrum of symptoms, including pain with overhead activity and weakness with elevation and/or rotation. History-taking should pay close attention to the duration of symptoms and weakness, and previous operations. In addition, attention should be paid to patients’ function goals and expectations, as well as factors that influence their ability to comply with recovery or rehabilitation programs.
The physical examination begins with a standard examination, including active motion, passive motion, and individual rotator cuff muscle strength (Table 2). As mentioned, a lidocaine injection can be used to differentiate true muscle imbalance from pain-limited active motion. A large external rotation lag sign, generally defined as greater than 40°, should be noted when present. The shoulder contour can be evaluated for muscle atrophy and anterosuperior escape. The skin can be examined for previous open or arthroscopic portal incisions. In the case of prior open cuff repairs, the deltoid can be palpated for dehiscence and muscle firing; spontaneous deltoid detachment has been reported even in MRCTs without prior surgery.17,62 The acromioclavicular joint and bicipital groove can be palpated to identify concomitant areas of pain.
Table 2.
Physical Examination Tests for Rotator Cuff Tears
| Test | Correlating Tendon |
|---|---|
| Belly press | Inferior subscapularis |
| Bear hug | Superior subscapularis |
| Abduction in scapular plane | Supraspinatus |
| External rotation with arm adducted | Infraspinatus |
| External rotation lag sign with arm adducted | Large infraspinatus and likely teres minor |
| External rotation with arm abducted (horn blower) | Teres minor |
Imaging
The most used imaging studies are routine radiography and noncontrasted MRI. As described above, the two can help predict the likelihood of being unable to reduce the tendon to the footprint and a high risk of retear. Table 3 shows common measurements and classifications from radiographs and MRI scans, along with their common uses in patients with MIRCTs. Each of these findings predicts a high likelihood of clinical and/or structural failure past specific cutoff values. Conversely, restoration of the acromiohumeral interval with surgery correlates with better function and pain.
Table 3.
Imaging Findings or Classifications Useful for Indicating Procedures to Treat MRCTs a
| Finding/Classification | Use/Correlations | |
|---|---|---|
| Radiograph | ||
| Acromiohumeral interval |
|
Indicator of vertical force couple imbalance. Stress examination can assess static versus dynamic superior migration. 40 |
| Critical shoulder angle |
|
Describes how vertical the moment arm of the deltoid is, and how much the shoulder relies on the cuff for initiation of overhead motion.28,60 |
| Hamada classification |
|
Describes radiographic progression, from muscle imbalance causing proximal migration, to bone remodeling of the acromion, and finally glenohumeral arthritis. 34 Joint-preserving procedures with generally inferior outcomes for Hamada ≥3. 27 |
| MRI | ||
| Patte |
|
Describes extent of tendon retraction. 74 |
| Tangent sign |
|
Describes extent of muscle atrophy.42,97 |
| Goutallier | 1 = normal muscle 2 = fatty streaks 3 = muscle > fat 4 = fat > muscle |
Describes extent of muscle fatty infiltration. 33 |
| Tendon stump length |
|
<15 mm correlates with 92% repair failure rate. 56 |
a MRCT, massive rotator cuff tear; MRI, magnetic resonance imaging.
Additional imaging findings to consider include the remaining greater tuberosity bone stock, the extent of prior acromioplasty, and whether there is concomitant acromioclavicular joint pathology. When planning RSA, computed tomography can be helpful in assessing glenoid deformity. In general, there is a limited role for ultrasonography, but it can be used as a low-cost method to assess postoperative healing.
Treatment Options
The number of treatment options for MIRCTs have increased considerably in the past decade (Figure 4), § and many follow a similar approach conceptually (Figure 5). While a complete discussion of these procedures is beyond the scope of this paper, a study group systematically reviewed published literature with the goal of comparing patient-reported outcomes, reoperation rates, and treatment response for the techniques. 44 While the meta-analysis drew some notable conclusions, the authors highlighted a need for higher-quality and comparative studies to guide treatment strategies for MIRCTs. This identified need will hopefully encourage high-quality studies from which evidence-based treatment algorithms can be developed. A small number of comparative studies have been published in recent years.2,4,55,71,91 Another issue with the current literature is that many of the less commonly performed techniques such as tendon transfers comes from a small set of institutions and authors, and thus their results may not be generalizable.
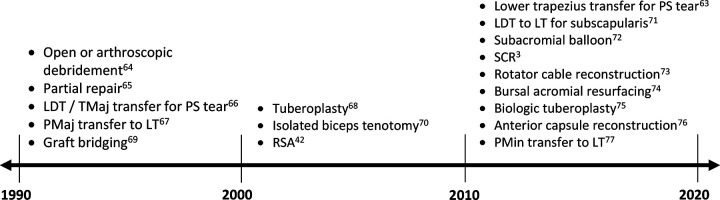
Figure 4.
Timeline showing the introduction of surgical techniques for massive rotator cuff tear. LDT, latissimus dorsi transfer; LT, lesser tuberosity; PMaj, pectoralis major; PMin, pectoralis minor; PS, posterosuperior; RSA, reverse shoulder arthroplasty; SCR, superior capsule reconstruction; TMaj, teres major.
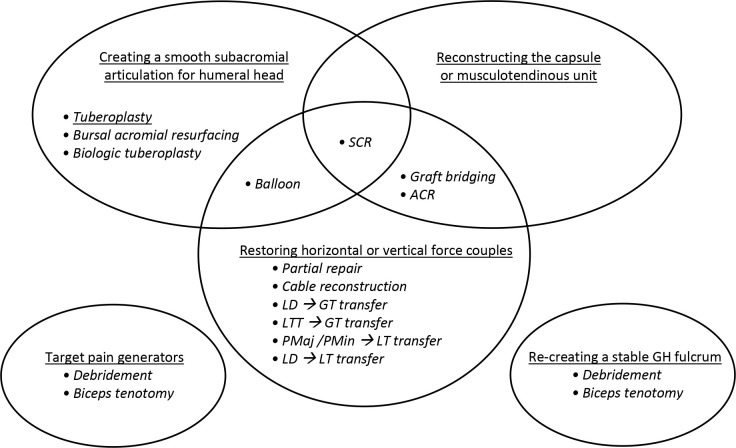
Figure 5.
Conceptual approach of current treatment options. ACR, anterior capsule reconstruction; GH, glenohumeral; GT, greater tuberosity; LD, latissimus dorsi; LT, lesser tuberosity; LTT, lower trapezius tendon; PMaj, pectoralis major; PMin, pectoralis minor; SCR, superior capsule reconstruction.
Table 4 shows outcome data from recent large patient series or systematic reviews on various techniques ∥ ; using these data for comparison is limited by varying levels of evidence, follow-up, inclusion criteria, and outcome measures. As better comparative literature emerges, an understanding of the principles of MRCTs discussed in this review allows the surgeon to identify tears that cannot or should not be repaired, and at least conceptually indicate patients for nonrepair procedures. Moreover, patient expectations, motivation, and activity or occupational demand remain a large part of procedure selection for MIRCTs.
Table 4.
Clinical Outcomes of Current Surgical Techniques a
| Technique | Follow-up, mo | Sample Size b | Mean age, y | △ASES/CS | △ Pain c | △AFE/ER, deg d | Complication Rate |
|---|---|---|---|---|---|---|---|
| Debridement, tenotomy, bursectomy, tuberoplasty 90 | 46 | 643 | 66 | 41/24 | 5 (7→2) | 36/4 | 7%, mostly RSA |
| Balloon 91 | 12 | 56 | 66 | —/18 | % taking pain meds: 73-4 | 32/— | 2% to RSA |
| RSA36,84 | >24 | 92 | >65 | 38/5.2 (SST) | –4.0 (mean, –1.6) | 79/25 | 12% major complication rate |
| Partial repair 49 | 16-41 | 348 | 64 | 29-44/21-34 | 2-5 | 20-52/1-23 | 3% |
| LTT for PS 15 | 40 | 48 | 56 | ▪ DASH: 34 ▪ SSV: 26% |
5 | 38/34 | — |
| oLDT for PS 66 | 46 (range, 24-126) | 258 | 59 | CS: 27 | CS pain: 7 (range, 0-15) | 35/10 | 7%; tendon rupture: 3.4% |
| aLDT for PS 53 | 34 (range, 18-72) | 258 | — | CS: 32 | 4.4 | 41/21 | ▪ Tendon rupture: 3% ▪ Hematoma: 2% |
| oLDT for AS 48 | 17 | 85 | 55 | CS: 35 | 4 | 44/— | ▪ Tendon rupture: 0%-20% ▪ Overall: 15% |
| PM for AS 48 | 67 | 184 | 59 | CS: 24 | 3.7 | 17/— | ▪ Tendon rupture: 7%-13% ▪ Overall: 15% |
| SCR 27 | — | 292 | 63 | 30-55/— | 2.5-5.9 | 28-56/9-15 | 12% |
| Bridge 3 | — | 357 | — | 34/— | 4/— | 41/13 | — |
a AFE, active forward elevation; aLDT, arthroscopic latissimus dorsi transfer; AS, anterosuperior cuff tear; ASES, American Shoulder and Elbow Surgeons score; CS, total Constant score; DASH, Disabilities of the Arm, Shoulder and Hand; ER, active external rotation; LTT, lower trapezius transfer; oLDT, open latissimus dorsi transfer; PM, pectoralis major; PS, posterosuperior cuff tear; RSA, reverse shoulder arthroplasty; SCR, superior capsule reconstruction; SST, Simple Shoulder Test; SSV, Subjective Shoulder Value; VAS, pain visual analog scale.
b Represents total number of patients included in systematic reviews, but the number of patients included for each outcome measure differed.
c Pain outcome listed as change in VAS pain unless otherwise stated.
d All changes in AFE and ER were positive (improvements).
Conclusion
Based on this review, the following definitions and critical concepts drive decision-making for MIRCTs:
Massive tears are most frequently defined as involving ≥2 tendons but may be better defined as retraction of the torn tendon with at least 67% of the greater tuberosity exposed in the sagittal plane.
Irreparability can refer to both the inability to reduce the tendon to the footprint despite mobilization techniques and a tear in which repair is associated with an unacceptably high rate of failure. Predictive models have been developed to quantify the likelihood of both scenarios accounting for multiple variables shown to affect tendon healing, although the clinical implications of structurally failed repair remain unclear.
Massive cuff tears result in unbalanced dynamic stabilization of the glenohumeral joint. They create an unstable fulcrum for overhead motion and loss of active rotation. Variations in osseous anatomy and tear patterns correlate with the patient’s ability to maintain overhead motion with massive cuff tears.
Pain generation is a parallel process likely related to excessive strain or wear on the biceps tendon, remaining cuff, deltoid, and subacromial space. These may be technically simpler targets for treating certain patients, as evidenced by the success of multiple palliative procedures.
Painful loss of elevation or pseudoparesis is defined as the inability to elevate the arm more than 90°, but with improvement after intra-articular lidocaine is given. Patients with this condition should be differentiated from those with true pseudoparalysis.
The use of consistent terminology will allow for better defining patient populations for comparative studies and interpreting outcomes of new techniques.
Footnotes
Final revision submitted October 21, 2022; accepted November 9, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.A.S. has received royalties from Medacta; education payments from Arthrex; consulting fees from Daiichi Sankyo, Flower Orthopedics, Medacta, RTI Surgical, and Smith & Nephew; nonconsulting fees from Daiichi Sankyo; and honoraria from Medacta. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Bacle G, Nové-Josserand L, Garaud P, Walch G. Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous study. J Bone Joint Surg Am. 2017;99(6):454–461. doi:10.2106/JBJS.16.00223 [DOI] [PubMed] [Google Scholar]
- 2.Baek CH, Lee DH, Kim JG. Latissimus dorsi transfer versus lower trapezius transfer for posterosuperior irreparable rotator cuff tears. J Shoulder Elbow Surg. 2022;31(9):1810–1822. doi:10.1016/j.jse.2022.02.020 [DOI] [PubMed] [Google Scholar]
- 3.Baek S, Shin MH, Kim TM, Im JM, Oh KS, Chung SW. Clinical outcomes of interposition graft versus superior capsular reconstruction in patients with irreparable rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(9):23259671211022241. doi:10.1177/23259671211022241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baverel LP, Bonnevialle N, Joudet T, et al. Short-term outcomes of arthroscopic partial repair vs. latissimus dorsi tendon transfer in patients with massive and partially repairable rotator cuff tears. J Shoulder Elbow Surg. 2021;30(2):282–289. doi:10.1016/j.jse.2020.06.002 [DOI] [PubMed] [Google Scholar]
- 5.Berthold DP, Ravenscroft M, Bell R, et al. Bursal acromial reconstruction (BAR) using an acellular dermal allograft for massive, irreparable posterosuperior rotator cuff tears: a dynamic biomechanical investigation. Arthroscopy. 2022;38(2):297–306. doi:10.1016/j.arthro.2021.07.021 [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Andreani O, Schramm M, Baba M, Barret H, Chelli M. The effect of tendon delamination on rotator cuff healing. Am J Sports Med. 2019;47(5):1074–1081. doi:10.1177/0363546519835491 [DOI] [PubMed] [Google Scholar]
- 7.Boileau P, Baba M, McClelland WB, Thélu CÉ, Trojani C, Bronsard N. Isolated loss of active external rotation: a distinct entity and results of L’Episcopo tendon transfer. J Shoulder Elbow Surg. 2018;27(3):499–509. doi:10.1016/j.jse.2017.07.008 [DOI] [PubMed] [Google Scholar]
- 8.Boileau P, Baqué F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89(4):747–757. doi:10.2106/JBJS.E.01097 [DOI] [PubMed] [Google Scholar]
- 9.Bouaicha S, Ernstbrunner L, Jud L, Meyer DC, Snedeker JG, Bachmann E. The lever arm ratio of the rotator cuff to deltoid muscle explains and predicts pseudoparalysis of the shoulder: the Shoulder Abduction Moment index. Bone Joint J. 2018;100 (12):1600–1608. doi:10.1302/0301-620X.100B12.BJJ-2018-0493.R1 [DOI] [PubMed] [Google Scholar]
- 10.Burkhart SS.Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992;284:144–152. [PubMed] [Google Scholar]
- 11.Burkhart SS, Barth JRH, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347–354. doi:10.1016/j.arthro.2006.12.012 [DOI] [PubMed] [Google Scholar]
- 12.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder’s “suspension bridge.” Arthroscopy. 1993;9(6):611–616. doi:10.1016/s0749-8063(05)80496-7 [DOI] [PubMed] [Google Scholar]
- 13.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10(4):363–370. doi:10.1016/s0749-8063(05)80186-0 [DOI] [PubMed] [Google Scholar]
- 14.Chen KH, Chiang ER, Wang HY, Ma HL. Arthroscopic partial repair of irreparable rotator cuff tears: factors related to greater degree of clinical improvement at 2 years of follow-up. Arthroscopy. 2017;33(11):1949–1955. doi:10.1016/j.arthro.2017.06.047 [DOI] [PubMed] [Google Scholar]
- 15.Clouette J, Leroux T, Shanmugaraj A, et al. The lower trapezius transfer: a systematic review of biomechanical data, techniques, and clinical outcomes. J Shoulder Elbow Surg. 2020;29(7):1505–1512. doi:10.1016/j.jse.2019.12.019 [DOI] [PubMed] [Google Scholar]
- 16.Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982;154(5):667–672. [PubMed] [Google Scholar]
- 17.Colak C, Bullen JA, Entezari V, Forney M, Ilaslan H. Magnetic resonance imaging of deltoid muscle/tendon tears: a descriptive study. Skeletal Radiol. 2021;50(10):1995–2003. doi:10.1007/s00256-021-03727-6 [DOI] [PubMed] [Google Scholar]
- 18.Collin P, Betz M, Herve A, et al. Clinical and structural outcome 20 years after repair of massive rotator cuff tears. J Shoulder Elbow Surg. 2020;29(3):521–526. doi:10.1016/j.jse.2019.07.031 [DOI] [PubMed] [Google Scholar]
- 19.Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg. 2014;23(8):1195–1202. doi:10.1016/j.jse.2013.11.019 [DOI] [PubMed] [Google Scholar]
- 20.Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy. 2012;28(7):909–915. doi:10.1016/j.arthro.2011.12.007 [DOI] [PubMed] [Google Scholar]
- 21.Denard PJ, Koo SS, Murena L, Burkhart SS. Pseudoparalysis: the importance of rotator cable integrity. Orthopedics. 2012;35(9):e1353–e1357. doi:10.3928/01477447-20120822-21 [DOI] [PubMed] [Google Scholar]
- 22.Denard PJ, Lädermann A, Jiwani AZ, Burkhart SS. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy. 2012;28(9):1214–1219. doi:10.1016/j.arthro.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 23.Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016;25(8):1346–1353. doi:10.1016/j.jse.2015.12.006 [DOI] [PubMed] [Google Scholar]
- 24.Fahey CJ, Delaney RA. Exploring expert variability in defining pseudoparalysis: an international survey. J Shoulder Elbow Surg. 2021;30(5):e237–e244. doi:10.1016/j.jse.2020.08.029 [DOI] [PubMed] [Google Scholar]
- 25.Farazdaghi A, Paschos NK, Kelly JD. Comparison between partial and full coverage repair in massive rotator cuff tears. A minimum five year follow-up. Orthop Traumatol Surg Res. 2021;107(4):102911. doi:10.1016/j.otsr.2021.102911 [DOI] [PubMed] [Google Scholar]
- 26.Fenlin JM, Chase JM, Rushton SA, Frieman BG. Tuberoplasty: creation of an acromiohumeral articulation—a treatment option for massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2002;11(2):136–142. doi:10.1067/mse.2002.121764 [DOI] [PubMed] [Google Scholar]
- 27.Gao I, Sochacki KR, Freehill MT, Sherman SL, Abrams GD. Superior capsular reconstruction: a systematic review of surgical techniques and clinical outcomes. Arthroscopy. 2021;37(2):720–746. doi:10.1016/j.arthro.2020.09.016 [DOI] [PubMed] [Google Scholar]
- 28.Garcia GH, Liu JN, Degen RM, et al. Higher critical shoulder angle increases the risk of retear after rotator cuff repair. J Shoulder Elbow Surg. 2017;26(2):241–245. doi:10.1016/j.jse.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 29.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi:10.2106/00004623-200004000-00006 [DOI] [PubMed] [Google Scholar]
- 30.Gerber C, Meyer DC, Flück M, et al. Muscle degeneration associated with rotator cuff tendon release and/or denervation in sheep. Am J Sports Med. 2017;45(3):651–658. doi:10.1177/0363546516677254 [DOI] [PubMed] [Google Scholar]
- 31.Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. A preliminary report. Clin Orthop Relat Res. 1988;232:51–61. [PubMed] [Google Scholar]
- 32.Godenèche A, Nové-Josserand L, Audebert S, et al. Relationship between subscapularis tears and injuries to the biceps pulley. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2114–2120. doi:10.1007/s00167-016-4374-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12(6):550–554. doi:10.1016/s1058-2746(03)00211-8 [DOI] [PubMed] [Google Scholar]
- 34.Hamada K, Fukuda H, Mikasa M, Kobayashi Y.Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;254:92–96. [PubMed] [Google Scholar]
- 35.Hansen ML, Otis JC, Johnson JS, Cordasco FA, Craig EV, Warren RF. Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am. 2008;90(2):316–325. doi:10.2106/JBJS.F.00880 [DOI] [PubMed] [Google Scholar]
- 36.Hartzler RU, Steen BM, Hussey MM, et al. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24(11):1698–1706. doi:10.1016/j.jse.2015.04.015 [DOI] [PubMed] [Google Scholar]
- 37.Henry P, Wasserstein D, Park S, et al. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review. Arthroscopy. 2015;31(12):2472–2480. doi:10.1016/j.arthro.2015.06.038 [DOI] [PubMed] [Google Scholar]
- 38.Holschen M, Brand F, Agneskirchner JD. Subacromial spacer implantation for massive rotator cuff tears: clinical outcome of arthroscopically treated patients. Obere Extrem. 2017;12(1):38–45. doi:10.1007/s11678-016-0386-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ishigaki N, Hata Y, Matsuba T, Hino M, Murakami N, Kobayashi H. Long-term results of partial repair for irreparable rotator cuff tear. JSES Int. 2021;5(4):642–648. doi:10.1016/j.jseint.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jeon YD, Yoon JY, Jeong HJ, et al. Significance of the acromiohumeral distance on stress radiography for predicting healing and function after arthroscopic repair of massive rotator cuff tears. J Shoulder Elbow Surg. 2021;30(8):e471–e481. doi:10.1016/j.jse.2020.10.029 [DOI] [PubMed] [Google Scholar]
- 41.Jung SW, Kim DH, Park TH, Park JY, Jeon JM. Humeral head coverage in arthroscopic partial repair of massive rotator cuff tears improves functional outcomes: an analysis of influential factors. J Shoulder Elbow Surg. 2022;31(11):2233–2241. doi:10.1016/j.jse.2022.03.030 [DOI] [PubMed] [Google Scholar]
- 42.Kim IB, Jung DW, Suh KT. Prediction of the irreparability of rotator cuff tears. Arthroscopy. 2018;34(7):2076–2084. doi:10.1016/j.arthro.2018.02.033 [DOI] [PubMed] [Google Scholar]
- 43.Kirsch JM, Patel M, Hill BW, McPartland C, Namdari S, Lazarus MD. Preoperative single assessment numeric evaluation score predicts poor outcomes after reverse shoulder arthroplasty for massive rotator cuff tears without arthritis. Orthopedics. 2022;45(4):215–220. doi:10.3928/01477447-20220225-07 [DOI] [PubMed] [Google Scholar]
- 44.Kovacevic D, Suriani RJ, Grawe BM, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg. 2020;29(12):2459–2475. doi:10.1016/j.jse.2020.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The rotator cuff healing index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019;47(1):173–180. doi:10.1177/0363546518810763 [DOI] [PubMed] [Google Scholar]
- 46.Liu B, Kim JU, Kim YK, Jeong HJ, Oh JH. Clinical outcome of reverse shoulder arthroplasty and rotator cuff repair in patients of massive rotator cuff tear without osteoarthritis: comparison using propensity score matching. J Shoulder Elbow Surg. 2022;31(10):2096–2105. doi:10.1016/j.jse.2022.02.040 [DOI] [PubMed] [Google Scholar]
- 47.Lo IKY, Burkhart SS. The interval slide in continuity: a method of mobilizing the anterosuperior rotator cuff without disrupting the tear margins. Arthroscopy. 2004;20(4):435–441. doi:10.1016/j.arthro.2004.01.016 [DOI] [PubMed] [Google Scholar]
- 48.Luo Z, Lin J, Sun Y, Zhu K, Wang C, Chen J. Outcome comparison of latissimus dorsi transfer and pectoralis major transfer for irreparable subscapularis tendon tear: a systematic review. Am J Sports Med. 2022;50(7):2032–2041. doi:10.1177/03635465211018216 [DOI] [PubMed] [Google Scholar]
- 49.Malahias MA, Kostretzis L, Chronopoulos E, Brilakis E, Avramidis G, Antonogiannakis E. Arthroscopic partial repair for massive rotator cuff tears: does it work? A systematic review. Sports Med Open. 2019;5(1):13. doi:10.1186/s40798-019-0186-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mall NA, Tanaka MJ, Choi LS, Paletta GA. Factors affecting rotator cuff healing. J Bone Joint Surg Am. 2014;96(9):778–788. doi:10.2106/JBJS.M.00583 [DOI] [PubMed] [Google Scholar]
- 51.Matsen FA III, Cordasco FA, Sperlling JW, Lippitt SB. Rockwood and Matsen’s The Shoulder. 6th ed. Elsevier; 2021. [Google Scholar]
- 52.Melis B, DeFranco M, Lädermann A, et al. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br. 2011;93(9):1240–1246. doi:10.1302/0301-620X.93B9.25926 [DOI] [PubMed] [Google Scholar]
- 53.Memon M, Kay J, Quick E, et al. Arthroscopic-assisted latissimus dorsi tendon transfer for massive rotator cuff tears: a systematic review. Orthop J Sports Med. 2018;6(6):2325967118777735. doi:10.1177/2325967118777735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mesiha MM, Derwin KA, Sibole SC, Erdemir A, McCarron JA. The biomechanical relevance of anterior rotator cuff cable tears in a cadaveric shoulder model. J Bone Joint Surg Am. 2013;95(20):1817–1824. doi:10.2106/JBJS.L.00784 [DOI] [PubMed] [Google Scholar]
- 55.Metcalfe A, Parsons H, Parsons N, et al. Subacromial balloon spacer for irreparable rotator cuff tears of the shoulder (START:REACTS): a group-sequential, double-blind, multicentre randomised controlled trial. Lancet. 2022;399(10339):1954–1963. doi:10.1016/S0140-6736(22)00652-3 [DOI] [PubMed] [Google Scholar]
- 56.Meyer DC, Wieser K, Farshad M, Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med. 2012;40(10):2242–2247. doi:10.1177/0363546512457587 [DOI] [PubMed] [Google Scholar]
- 57.Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40(10):2248–2255. doi:10.1177/0363546512456195 [DOI] [PubMed] [Google Scholar]
- 58.Mirzayan R, Bouz G. Biologic tuberoplasty with an acellular dermal allograft for massive rotator cuff tears. Arthrosc Tech. 2021;10(7):e1743–e1749. doi:10.1016/j.eats.2021.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Montgomery TJ, Yerger B, Savoie FH. Management of rotator cuff tears: a comparison of arthroscopic debridement and surgical repair. J Shoulder Elbow Surg. 1994;3(2):70–78. doi:10.1016/S1058-2746(09)80113-4 [DOI] [PubMed] [Google Scholar]
- 60.Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J. 2013;95(7):935–941. doi:10.1302/0301-620X.95B7.31028 [DOI] [PubMed] [Google Scholar]
- 61.Moorman CT, Deng XH, Warren RF, Torzilli PA, Wickiewicz TL. The coracoacromial ligament: is it the appendix of the shoulder? J Shoulder Elbow Surg. 1996;5(2):S9. doi:10.1016/S1058-2746(96)80097-8 [Google Scholar]
- 62.Morisawa K, Yamashita K, Asami A, Nishikawa H, Watanabe H. Spontaneous rupture of the deltoid muscle associated with massive tearing of the rotator cuff. J Shoulder Elbow Surg. 1997;6(6):556–558. doi:10.1016/s1058-2746(97)90089-6 [DOI] [PubMed] [Google Scholar]
- 63.Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92(15):2544–2556. doi:10.2106/JBJS.I.00912 [DOI] [PubMed] [Google Scholar]
- 64.Mun SW, Kim JY, Yi SH, Baek CH. Latissimus dorsi transfer for irreparable subscapularis tendon tears. J Shoulder Elbow Surg. 2018;27(6):1057–1064. doi:10.1016/j.jse.2017.11.022 [DOI] [PubMed] [Google Scholar]
- 65.Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD. Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am. 2014;96(2):99–105. doi:10.2106/JBJS.M.00551 [DOI] [PubMed] [Google Scholar]
- 66.Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94(10):891–898. doi:10.2106/JBJS.K.00841 [DOI] [PubMed] [Google Scholar]
- 67.Neer CS, Satterlee CC, Dalsey RM, Flatow EL. The anatomy and potential effects of contracture of the coracohumeral ligament. Clin Orthop Relat Res. 1992;280:182–185. [PubMed] [Google Scholar]
- 68.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg. 2009;18(5):808–818. doi:10.1016/j.jse.2009.03.013 [DOI] [PubMed] [Google Scholar]
- 69.Neviaser JS, Neviaser RJ, Neviaser TJ. The repair of chronic massive ruptures of the rotator cuff of the shoulder by use of a freeze-dried rotator cuff. J Bone Joint Surg Am. 1978;60(5):681–684. [PubMed] [Google Scholar]
- 70.Nobuhara K, Hata Y, Komai M. Surgical procedure and results of repair of massive tears of the rotator cuff. Clin Orthop Relat Res. 1994;304:54–59. [PubMed] [Google Scholar]
- 71.Ozturk BY, Ak S, Gultekin O, Baykus A, Kulduk A. Prospective, randomized evaluation of latissimus dorsi transfer and superior capsular reconstruction in massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2021;30(7):1561–1571. doi:10.1016/j.jse.2021.01.036 [DOI] [PubMed] [Google Scholar]
- 72.Paladini P, Campi F, Merolla G, Pellegrini A, Porcellini G. Pectoralis minor tendon transfer for irreparable anterosuperior cuff tears. J Shoulder Elbow Surg. 2013;22(6):e1–e5. doi:10.1016/j.jse.2012.12.030 [DOI] [PubMed] [Google Scholar]
- 73.Pandey V, Madi S, Maddukuri S, Acharya K, Karegowda LH, Willems WJ. Does application of abduction brace after arthroscopic rotator cuff repair improve blood flow around posterosuperior rotator cuff and repair site, affecting pain levels and clinical and structural outcomes? A pilot randomized controlled trial. JSES Int. 2020;4(4):848–859. doi:10.1016/j.jseint.2020.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 75.Paxton ES, Teefey SA, Dahiya N, Keener JD, Yamaguchi K, Galatz LM. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year follow-up. J Bone Joint Surg Am. 2013;95(7):627–632. doi:10.2106/JBJS.L.00255 [DOI] [PubMed] [Google Scholar]
- 76.Rauck RC, Jahandar A, Kontaxis A, et al. The role of the long head of the biceps tendon in posterior shoulder stabilization during forward flexion. J Shoulder Elbow Surg. 2022;31(6):1254–1260. doi:10.1016/j.jse.2021.12.026 [DOI] [PubMed] [Google Scholar]
- 77.Resch H, Povacz P, Ritter E, Matschi W. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J Bone Joint Surg Am. 2000;82(3):372–382. doi:10.2106/00004623-200003000-00008 [DOI] [PubMed] [Google Scholar]
- 78.Rockwood CA, Williams GR, Burkhead WZ. Débridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am. 1995;77(6):857–866. doi:10.2106/00004623-199506000-00006 [DOI] [PubMed] [Google Scholar]
- 79.Rogers JP, Kwapisz A, Tokish JM. Anterior capsule reconstruction for irreparable subscapularis tears. Arthrosc Tech. 2017;6(6):e2241–e2247. doi:10.1016/j.eats.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Russell RD, Knight JR, Mulligan E, Khazzam MS. Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am. 2014;96(4):265–271. doi:10.2106/JBJS.M.00265 [DOI] [PubMed] [Google Scholar]
- 81.Sachinis NP, Papagiannopoulos S, Sarris I, Papadopoulos P. Outcomes of arthroscopic nerve release in patients treated for large or massive rotator cuff tears and associated suprascapular neuropathy: a prospective, randomized, double-blinded clinical trial. Am J Sports Med. 2021;49(9):2301–2308. doi:10.1177/03635465211021834 [DOI] [PubMed] [Google Scholar]
- 82.Savarese E, Romeo R. New solution for massive, irreparable rotator cuff tears: the subacromial “biodegradable spacer.” Arthrosc Tech. 2012;1(1):e69–e74. doi:10.1016/j.eats.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schumaier A, Kovacevic D, Schmidt C, et al. Defining massive rotator cuff tears: a Delphi consensus study. J Shoulder Elbow Surg. 2020;29(4):674–680. doi:10.1016/j.jse.2019.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sellers TR, Abdelfattah A, Frankle MA. Massive rotator cuff tear: when to consider reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2018;11(1):131–140. doi:10.1007/s12178-018-9467-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shah NS, Suriel Peguero E, Umeda Y, Crawford ZT, Grawe BM. Long-term outcomes of massive rotator cuff tear repair: a systematic review. HSS J. 2022;18(1):130–137. doi:10.1177/15563316211008137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative radiographic risk factors for incomplete arthroscopic supraspinatus tendon repair in massive rotator cuff tears. Arthroscopy. 2018;34(4):1121–1127. doi:10.1016/j.arthro.2017.09.046 [DOI] [PubMed] [Google Scholar]
- 87.Sheth MM, Heldt BL, Spell JH, et al. Patient satisfaction and clinical outcomes of reverse shoulder arthroplasty: a minimum of 10 years’ follow-up. J Shoulder Elbow Surg. 2022;31(4):875–883. doi:10.1016/j.jse.2021.09.012 [DOI] [PubMed] [Google Scholar]
- 88.Shi LL, Boykin RE, Lin A, Warner JJP. Association of suprascapular neuropathy with rotator cuff tendon tears and fatty degeneration. J Shoulder Elbow Surg. 2014;23(3):339–346. doi:10.1016/j.jse.2013.06.011 [DOI] [PubMed] [Google Scholar]
- 89.Shon MS, Koh KH, Lim TK, Kim WJ, Kim KC, Yoo JC. Arthroscopic partial repair of irreparable rotator cuff tears: preoperative factors associated with outcome deterioration over 2 years. Am J Sports Med. 2015;43(8):1965–1975. doi:10.1177/0363546515585122 [DOI] [PubMed] [Google Scholar]
- 90.Soderlund M, Boren M, O’Reilly A, San Juan A, Mahylis JM. Arthroscopic debridement for management of massive, irreparable rotator cuff tears: a systematic review of outcomes. JSES Rev Rep Tech. 2022;2(1):1–7. doi:10.1016/j.xrrt.2021.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Srikumaran U, Roden C, Rogusky E, Lapner P, Abboud J, Verma N. Subacromial balloon spacer versus partial repair for massive rotator cuff tears: a prospective, randomized, multi-center trial. Orthop J Sports Med. 2021;9(7 suppl 4):2325967121S00244. doi:10.1177/2325967121S00244 [Google Scholar]
- 92.Su WR, Budoff JE, Luo ZP. The effect of posterosuperior rotator cuff tears and biceps loading on glenohumeral translation. Arthroscopy. 2010;26(5):578–586. doi:10.1016/j.arthro.2009.09.007 [DOI] [PubMed] [Google Scholar]
- 93.Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017;26(6):e177–e187. doi:10.1016/j.jse.2017.02.024 [DOI] [PubMed] [Google Scholar]
- 94.Veen EJD, Koorevaar CT, Diercks RL. Using the long head of biceps tendon autograft as an anatomical reconstruction of the rotator cable: an arthroscopic technique for patients with massive rotator cuff tears. Arthrosc Tech. 2018;7(7):e699–e703. doi:10.1016/j.eats.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Warner JP, Krushell RJ, Masquelet A, Gerber C. Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am. 1992;74(1):36–45. [PubMed] [Google Scholar]
- 96.Yamamoto N, Itoi E, Tuoheti Y, et al. Glenohumeral joint motion after medial shift of the attachment site of the supraspinatus tendon: a cadaveric study. J Shoulder Elbow Surg. 2007;16(3):373–378. doi:10.1016/j.jse.2006.06.016 [DOI] [PubMed] [Google Scholar]
- 97.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33(3):163–170. doi:10.1097/00004424-199803000-00006 [DOI] [PubMed] [Google Scholar]