Abstract
In elderly women, a lack of regular physical exercise may result in faster decreases in general health and functional performance. Although high-intensity interval training (HIIT) and moderate-intensity continuous training (MICT) have been effectively applied in young and clinical groups, there is no evidence to support their use in elderly women to achieve health benefits. Thus, the major goal of this study was to investigate how HIIT affected health-related outcomes in elderly women. Twenty-four inactive elderly women agreed to participate in the 16-week HIIT and MICT intervention. Body composition, insulin resistance, blood lipids, functional capacity, cardiorespiratory fitness, and quality of life were all measured before and after the intervention. The number of differences between groups was determined using Cohen’s effect sizes, and the pre-post intra-group changes were compared using paired t-tests. Using 2 × 2 ANOVA, the time × group interaction effects between HIIT and MICT were evaluated. Body fat percentage, sagittal abdominal diameter, waist circumference, and hip circumference all were improved significantly in the 2 groups. HIIT substantially improved fasting plasma glucose and cardiorespiratory fitness as compared to the MICT. HIIT improved the lipid profile and functional ability more significantly compared to the MICT group. These findings show that HIIT is a useful exercise for improving elderly women’s physical health.
Keywords: HIIT, physical, health, obese, elderly
What do we already know about this topic?
HIIT substantially improved fasting plasma glucose and cardiorespiratory fitness compared to MICT. HIIT improved lipid profile and functional ability more significantly compared to the MICT group
How does your research contribute to the field?
The major goal of this study was to investigate how HIIT affected health-related outcomes in elderly persons
What are your research’s implications toward theory, practice, or policy?
Our research implications toward practice
Introduction
Obesity is one of major health issues in several nations, and the hazards connected with obesity are becoming more widespread among women. Obesity is a growing public health issue that is rising morbidity and mortality rate. World Health Organization (WHO) statistics suggest that around 650 million persons worldwide are obese, with 15% of women and 11% of men being obese. 1 The general population’s nutritional position, particularly that of women, is linked to the direct implications of obesity on women’s health. This syndrome permits women to acquire disorders that are health risks.2,3 In the Southeast Asian area, the prevalence of obesity in elderly women was 31%. 4
According to the Indonesian Ministry of Health, the prevalence of obesity in Indonesia among those over the age of 18 was 21.83% in 2018, up from 14.53% in 2013 5 and healthy lifestyle practices are the reasons why it is important to apply to obese people to reduce the risk of premature death and increase mortality from noncommunicable diseases. 6 Obesity, as measured by a rise in BMI, increases the risk of stroke and heart disease, as well as other chronic diseases such as hypertension, dyslipidemia, cardiovascular disease, and type 2 diabetes. 7
Obesity (BMI > 25) 8 was also used to assess abdominal fat accumulation, which was linked to a major health risk factor. Waist circumference estimations of >80 cm (women) and >90 cm (men) are a popular approach for measuring the quantity of visceral adipose tissue. 9 Many rules exist for estimating waist circumference, which is defined as the measurement (in cm) of waist circumference, although it is also dependent on other recommendations. 10 Obesity is associated with several problems, one of which is a national public health concern, particularly in Indonesia. Obesity has been linked to coronary artery disease, type 2 diabetes, and hypertension, with further evidence linking obesity to metabolic syndrome, gout, fatty liver, asthma, and cancer, according to current treatment guidelines. 11
Nowadays, obesity is becoming increasingly widespread among elderly people as a result of the risks linked with it. It is becoming a pandemic in developing nations, which is why establishing effective lifestyle methods and practices to manage this condition and the risk of mortality is critical.12-14 The elderly nowadays consume too many calories and live sedentary lifestyles, leading to obesity and related health problems. Metabolic syndrome is more common in the elderly, and it mainly affects women.12,14-23
Exercise can prevent and cure obesity-related disorders such as metabolic syndrome, type 2 diabetes, and cardiovascular disease. Low cardiorespiratory fitness and type 2 diabetes are connected with higher mortality in those who exercise less and have a metabolic syndrome diagnosis. 24 Exercise has a higher and more direct influence on obesity risk variables. 25 Popular exercise recommendations for women advocate exercising for at least 30 min per day, or 5 days per week at a moderate to high intensity, for the best effect on health. 26 The increase of regular exercise has been reported to improve cardiorespiratory fitness and lower the incidence of obesity and associated muscular diseases in obese women. 25 Therefore, regular and moderate exercise is strongly associated with fitness and health physiology, as well as illness prevention and health promotion. 27
High-intensity interval training (HIIT) is described as high-intensity aerobic exercise (85%-95% maximum heart rate) conducted for brief periods of time (30 s-4 min), alternated with low to moderate intensity recovery intervals (50%-70% maximum heart rate). 28 HIIT has traditionally been utilized by top athletes, but it is gaining favor in clinically inactive groups, with most research concentrating on the effects of HIIT in those with coronary artery disease, congestive heart failure, metabolic syndrome, and type 2 diabetes.21,23,28-47 HIIT has excellent benefits, including considerable increases in VO2max and insulin sensitivity. Although the advantages of HIIT have been thoroughly researched, the majority of this study has concentrated on the young and clinical populations. 43
For a long time, the benefits of HIIT exercise and diet have been researched as essential variables in the prevention and treatment of numerous illnesses. Although HIIT exercise and nutrition have distinct impacts, it has recently been shown that HIIT exercise and food also interact. When the 2 are combined, a greater benefit is obtained. 48 The impact of HIIT and its related advantages on body composition, metabolic blood measurements (blood lipids and insulin resistance), cardiorespiratory fitness (VO2max), and quality of life in obese elderly have never been explored. More study is needed to investigate whether HIIT, as compared to other forms of exercise, is an acceptable and tolerated form of exercise in obese women aged 50 to 60 years who were previously sedentary. As a result, the ultimate goal of this study was to study how the high intensity interval training (HIIT) versus moderate intensity continuous training (MICT) program affected health-related outcomes in obese women aged 50 to 60 years who previously ran sedentary life style in Indonesia.
Materials and Methods
The study used a cross-sectional pilot study design. Participants were assigned at random to either an HIIT or a MICT. Before and after a 16-week supervised intervention, all outcome variables were evaluated. Participation in this study was entirely voluntary, and participants were made aware that they might opt out at any moment. Prior to the first day of testing, participants signed an informed consent form. Each participant was clearly told the testing processes and workout activities, and they were encouraged to ask questions. A competent biokineticist who was trained in cardiopulmonary resuscitation (CPR) and basic life support oversaw all testing procedures and exercise sessions. Participants were advised that they could cease cycle ergometer testing or exercise sessions at any time and were shown how to utilize the emergency stop on the cycle ergometer
Participants
A cross-sectional pilot study was conducted in this study, there were 24 volunteers fulfilling the inclusion and exclusion criteria. Furthermore, the inclusion criteria used were 50 to 60 years old, residing in Indonesia; BMI between 25 and 29.9 kg/m2; maximum exercise twice a week for 45 min. In addition, the exclusion criteria include having diabetes, hypertension, or heart disease; having an injury such as a fracture, sprain, surgery, or a condition requiring immobilization; or being seen by an attending emergency physician. 8 These 24 participants were then initially randomly allocated to an HIIT or MICT group. Participants gave their verbal and written agreement in accordance with the Declaration of Helsinki, and all procedures were carried out as described. The ethics committee at Khon Kaen University gave the study their blessing (Decision number: HE622224).
Laboratory Visits
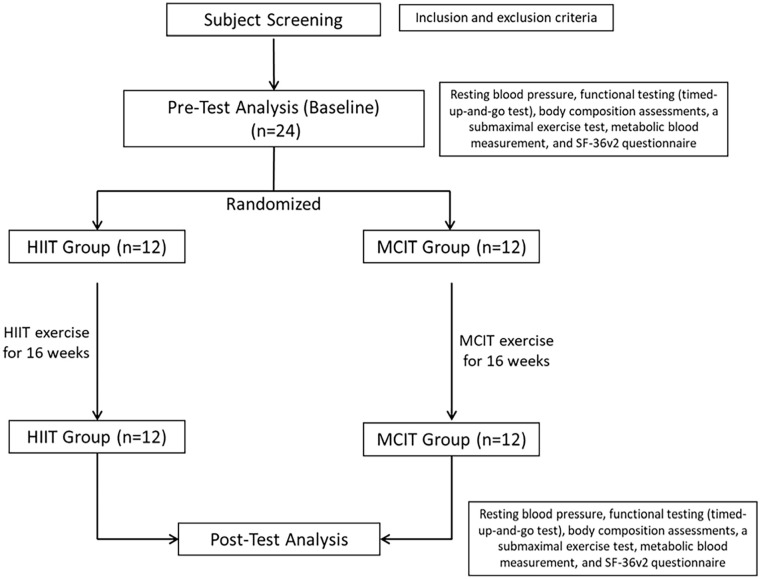
During the research, the participants were visited by the research team for several times on different days. The detail of the visit is shown by the Figure 1.
Figure 1.
Flowchart diagram of the research.
Visit day 1: Pre-participation screening
The initial visit to the laboratory involved screening tests to assess if the participants were qualified to participate. Co-morbidities were identified using cholesterol and glucose testing, anthropometry (body mass index, waist and hip circumference, and cardiovascular measurements (resting blood pressure and resting ECG).
Visit day 2: Baseline testing
Participants who passed the pre-participation screening returned to the laboratory for baseline (pre) testing on a subsequent day. Participants were instructed to clear their bladders immediately before testing and to avoid activity and diuretics such as coffee or alcohol for at least 8 h before the tests. Participants were also asked to refrain from smoking for 4 h prior to the measurements. Prior to participating in baseline testing, written informed permission was obtained.
Resting blood pressure, functional testing (timed-up-and-go test), body composition assessments (stature, body mass, waist and hip circumferences, sagittal abdominal diameter, and percentage body fat), a submaximal exercise test (Bruce protocol), and metabolic blood measurement were all part of the baseline testing (lipogram and insulin resistance). Participants were also asked to fill out the SF-36v2 questionnaire (quality of life).
At the end of this session, individuals were randomly assigned to either the HIIT and MICT groups. A statistician who was not engaged in the study generated random numbers for each group using www.randomizer.org. In sealed envelopes, an impartial participant distributes team assignments. Participants were requested to keep their existing lifestyle and not change their level of physical activity or food while taking part in the study.
Visit day 3-50: Exercise sessions
All HIIT and MICT exercise sessions were overseen by certified biokineticists. All personnel who supervised the sessions were directed to monitor the participants’ heart rates, as well as the cycle ergometer speed and inclination, and to verify that the individuals always exercised at the appropriate pre-determined intensity. For a total of 16 weeks, both exercise groups conducted 3 exercise sessions each week. In the Universitas PGRI Semarang Lab, all sessions were conducted on a cycle ergometer. After each interval during the HIIT training and every 10 min during the MICT session, a rating of perceived effort (0-10) was recorded.
Visit day 51: Post-testing
Post-testing was carried out between 24 and 48 h of the last exercise session. All procedures carried out during baseline testing were carried out again. When the appointment for the final assessments was arranged, the participants were reminded of the pre-test requirements.
Exercise Intervention
The intervention lasted 16 weeks and was conducted under supervision at physiology laboratory Universitas Negeri Yogyakarta. HIIT training sessions are carried out on a bicycle ergometer with an emergency stop. Participants are taught what to do and how to utilize the emergency button. Each subject did four 4-minute intervals at 90% to 95% of their anticipated age HRmax. For active recovery, participants cycled slowly on the ergometer for 3 min at 50% to 70% of their estimated HRmax after each 4-minute period. The workout was preceded by a 5-min warm-up at 70% of their projected age HRmax, followed by a 5-min cool-down. Heart rate was continually monitored and recorded around the clock (Garmin, Schaffhausen, Switzerland). Each training session is monitored by a skilled biokinetician, who adjusts the bicycle speed ergometer to attain the ideal heart rate range. The HIIT session lasts 38 min in total.
Participants in the MICT group cycled continuously for 47 min at a moderate effort set at 70% to 75% of their age predicted HRmax. This workout has the same time and intensity as the previous HIIT sessions. 49 Throughout the session, the heart rate was measured (Garmin, Schaffhausen, Switzerland). Participants were told to change their training tempo to keep their heart rate within the target range. The formula for age-max cardiac prediction was (220 age) × percent intensity (90%-95% for HIIT and 70%-75% for MICT). During the HIIT session, RPEs were recorded at the end of each interval, and every 10 min during the MICT session. To complete the intervention, all individuals who were eligible for the research made a total of 51 visits.
Research Instruments
All measures were obtained between 07.00 and 9.00 am following an overnight fast, both before and after the intervention. For each test, the same equipment was utilized. Measurements were taken by research assistants in accordance with a predetermined technique.
Blood pressure measurement
Blood pressure (mmHg) measurement using Omron M4-I Intellisense Blood Pressure (Kyoto Headquarters, Japan). For 30 min before the measurement, participants were not allowed to eat, consume alcohol, smoke, exercise, or bathe. Allow at least 15 min to rest before collecting measurements. Measurements should be avoided during times of stress since stress boosts blood pressure. Measurements should be performed in a peaceful location. Remove any restrictive garments from the sleeves. Place your feet flat on the floor and sit on a chair. Place your hands on the table so that the cuff is at the level of your heart. The cuff’s bottom should be roughly 1 to 2 cm above the elbow. Keep calm and avoid talking throughout the measurement. A team of doctors takes blood pressure and pulse readings.
Resting electrocardiogram (ECG)
During the pre-participation examination, a resting ECG was performed. To assess if there were any underlying cardiovascular irregularities, a 12-lead ECG (ELI 250, Milwaukee, USA) was employed. The individual was advised to lie anatomically supine on a plinth. Prior to applying the electrodes, the skin was prepped by removing any unwanted hair and cleaning the region with alcohol swabs to guarantee adherence. Six electrodes were put on the chest (V1-V6) and 4 were inserted on the limbs (RA, LA, F, N).
Measurement of body composition and anthropometry
Participants were measured height barefoot and only during the pre-test since they seldom altered and were measured up to 0.1 cm closest to the stadiometer (DS-103, DongSahn Jenix, Seoul, Korea). Participants were instructed to wear minimum clothes, remove jewelry, and not move or speak during body composition measurements (weight (kg), percent fat (percent)) using the Karada Scan HBF 375 (Omron Healthcare, Kyoto, Japan). The formula for calculating BMI/Body Mass Index is weight/kg divided by height/m, which is given as a square (kg/m2). The waist circumference is measured in millimeters using a tape measure linked to an iliac crest tape measure (cm).
Measurement of metabolic blood size
Total cholesterol and glucose testing were done during pre-participation screening. A competent biokineticist collected a drop of blood from the ring finger of the non-dominant hand using a disposable finger prick and a cholesterol or glucose strip (Roche Diagnostics) put into a portable instrument (Accutrend (R) plus, 2007, Roche Diagnostics). On the same day that participants completed baseline and post-testing, they were given a Pathcare Centre form (Stellenbosch). The subject was told to visit Pathcare Centre (Stellenbosch) within the following 24 to 48 h to undergo a lipogram and insulin resistance blood test. The participants were told to fast for 8 h before the test and to have it done first thing in the morning. The lipogram revealed total cholesterol, LDL-C, HDL-C, and TG levels. The insulin resistance test was performed on the same day as the lipogram and yielded data that included fasting plasma insulin and fasting plasma glucose levels. The formula: fasting insulin concentration (U/mL) × fasting glucose concentration (mmol/L)/22.5 was used to calculate insulin sensitivity (HOMA-IR technique). 50
Cardiorespiratory fitness
For the cycling test, the Astrand maximal cycle test protocol was used. The Cosmed metabolic system (Cosmed Quark b2 2000, Italy) and software were used to gather the metabolic data, which computed and recorded the exercise intensity as well as selected cardiorespiratory parameters during the test. The gas analyzer was equipped with a telemetric heart rate monitor (POLAR®, Polar Electro Oy, Finland), which recorded heart rate in beats per minute (bpm).
The gas analyzers were calibrated using ambient gas and known gas concentrations of 16% oxygen, 4% carbon dioxide, and a balance of nitrogen, according to the manufacturer’s instructions (Cosmed Quark b2 2000, Italy). A 3 l syringe was used to calibrate the turbine flow meter. All calibration was completed the morning before testing began. THR=((HR max-HR rest) × percent intensity) + HR rest was the Karvonen formula used to compute the participant’s goal heart rate (THR) set at 75% of their maximum.
Prior to the start of the exam, all participants were shown how to use the emergency stop button and advised that they could stop the test at any time. A safety strap was also used to secure participants to the cycle ergometer. The test began with a 10 degree gradient and a speed of 2.7 km/h. Every 3 min, the slope and pace were raised progressively until the goal heart rate was attained. After that, participants cooled down for 5 min at 2.7 km/h (no gradient). At the end of each step, the heart rate and rating of perceived effort (RPE) were recorded. RPE is a useful measure for determining a participant’s exercise tolerance. 51 Borg created the RPE scale to rate an individual’s whole-body sensations during exercise. Borg’s category-ratio scale of 0 to 10 (modified Borg scale) was employed, and it provided an early warning of imminent weariness. 51 During the test, no speech was permitted unless it was to convey extreme discomfort or weariness.
When the participants met their goal heart rate or when one of the termination criteria for halting an exercise test was apparent, the test was discontinued. 51 Among these were: The onset of angina or angina-like symptoms; a decline in systolic blood pressure more than 10 mmHg from baseline despite increasing activity intensity; significant increase in systolic blood pressure beyond 250 mmHg or diastolic blood pressure above 115 mmHg; shortness of breath, wheezing, leg cramps, or claudication that is unusual; signs of inadequate perfusion: dizziness, disorientation, ataxia, pallor, cyanosis, nausea, or cold and clammy skin; failure of heart rate to rise with increased exercise intensity; changes in cardiac rhythm; participant begs to pause; physical or verbal symptoms of extreme exhaustion; the testing equipment had failed.
Each participant’s estimated VO2max score was determined before and after the intervention. For women, the equation was VO2max (ml/kg/min) =4.38(T)−3.9, 52 while for males, it was 14.8 – (1.379 × T) + (0.451 × T2) – (0.012 × T3). 53 “T” represents the entire time of the exam in minutes and fractions of a minute.
Functional assessment
The Timed-Up-and-Go (TUG) test was originally used to assess frailty in the elderly. 54 However, it is currently routinely used to measure functional capacity in numerous demographic categories (elderly, obese, respiratory and cardiac illness). 55 This test is simple to conduct and evaluates a person’s mobility by requiring both static and dynamic balance.
Participants were instructed to wear comfortable workout shoes before the test. Participants were told to sit in a chair with back support but no arm rests. On the order “Go,” the participant rose from the chair, walked 3 m ahead, turned around a cone, and returned to the chair. The timer began when the instruction was issued and ended when the participant’s buttocks were put on the chair. Participants were instructed to do the instruction as quickly as possible without running. Each participant completed 3 trials, with the best time recorded in seconds to 2 decimal places.
Self-administered questionnaire
The short form health survey version 2 (SF-36v2) is a 36-question multipurpose health survey. This survey has shown beneficial in both general and particular groups, and it is simple to conduct. 56 This questionnaire collects data on an individual’s subjective mental and physical quality of life. The SF-36v2 measures 8 concepts: function (restricted physical activity such as climbing objects, lifting objects, sifting, and walking distance); role-physical (restricted function or daily responsibilities caused by physical health problems); body pain (severity of pain and how it interferes with daily functioning); general health (physical health status); vitality (controls energy and fatigue); social function (quality and quantity of social interaction); role-emotional (limitations in job activities other than those induced by physical health issues); Mental well-being (dimensions of anxiety, depression, behavioral or emotional loss and well-being).
Each question yields a score, which when combined together yields a total score for each section (0-100). The lower the score, the greater the individual’s incapacity. There are also scores for the psychometric-based summary of physical components (PCS) and summary of mental components (MCS). Each participant’s quality of life was assessed using the standardized form of the SF-36v2 health survey. Before and after the intervention, questionnaires were distributed.
Statistical Analysis
The data was statistically analyzed using Microsoft Office (Office 365, USA), STATISTICA 14.0 (Statsoft®, 2020, USA). Participants’ descriptive data were provided as means and standard deviations (SD). The paired t-test was used to assess mean differences between the HIIT and MICT groups. The effects of time × group interaction were investigated using 2 × 2 ANOVA. For all analyzes, the level of significance was fixed at P < .05. Cohen’s effect sizes were used to determine if there were any statistically significant differences between the 2 groups. The impact sizes were classified as follows: trivial practically significant effect 0.20, small practically significant effect 0.20, moderate practically significant effect 0.50, big practically significant effect 0.80, and very large practically significant effect 1.20. Cronbach’s alpha was used to measure the reliability of the SF-36 version 2, and the questionnaire was judged trustworthy if Cronbach’s alpha was better than .70.
Results
The Characteristics of the Elderly Participants
The study involved 24 elderly participants (24 women). The subjects were all healthy elderly individuals with an average age of 53.95 years (Table 1). According to ASEAN standard, the participants had a mean BMI of 26.65 ± 4.2 kg/m2, putting them in the obese category. However, it has been proposed that elderly persons only have an elevated cardiovascular disease risk if their BMI exceeds 30 kg/m2, 57 implying that elderly were still considered healthy. Despite the fact that the participants’ body fat percentage (38.167%) would place them at an elevated health risk for their age. 51 Because these people had previously been sedentary, both men and women had an initial projected VO2max of 20.6 ± 19.5 ml/kg/min, which is regarded as extremely low for both men and women. 51
Table 1.
The Participants’ Baseline Physical and Physiological Parameters.
| Variables | HIIT | MICT |
|---|---|---|
| N | 12 | 12 |
| Age (years) | 54.3 ± 5.1 | 53.6 ± 6.1 |
| Height (cm) | 164.6 ± 7.2 | 163.5 ± 7.9 |
| Body mass(kg) | 72.1 ± 13.8 | 74.1 ± 14.3 |
| BMI (kg/m2) | 26.6 ± 4.2 | 26.7 ± 4.1 |
| Body fat (%) | 37.3 ± 6.6 | 36.7 ± 6.9 |
Prior to the trial, all participants were verified that they were not actively participating in any form of structured exercise program and were free of any orthopedic injury. Twenty-nine of the 38 people that were assessed before to participation were authorized to enroll, and 24 completed the 16-week trial. Some participants reported some muscle soreness following the initial sessions, however no participant sought a break during the workout sessions. Two people dropped out of the study. One of these people got damaged her hip in a separate incident, and another had a preexisting injury that she did not disclose before to the research. The exercise sessions were well tolerated by the other individuals, who reported no side effects.
The Effect of HIIT and MICT on Body Composition
Both the HIIT and MICT groups exhibited a marginally significant reduction in body mass (ES = 0.08 and 0.16, respectively), however the latter group experienced a statistically significant drop (1.3 kg; P = .001). Following the HIIT and MICT intervention, both groups had statistically significant decreases in percent body fat (HIIT 1.7% vs MICT 1.2%), sagittal abdominal diameter (HIIT 1 cm vs MICT 0.5 cm), waist circumference (HIIT 4.2 cm vs MICT 3.3 cm), and hip circumference (HIIT 4.6 cm vs MICT 1.9 cm) (P < .05) (Table 2).
Table 2.
Change in Body Composition.
| Variables | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| Body mass (kg) | 72.1 ± 13.8 | 70.8 ± 13.2 a | 74.1 ± 14.3 | 73.4 ± 14.2 * a |
| Body fat (%) | 37.3 ± 6.6 | 35.6 ± 6.8 * b | 36.7 ± 6.9 | 35.5 ± 6.9 * b |
| Sagittal abdominal diameter (cm) | 20.3 ± 2.9 | 19.3 ± 2.7 * c | 20.3 ± 4.3 | 19.8 ±4.2 * c |
| Waist circumference (cm) | 82.4 ± 11.3 | 78.2 ± 9.8 * b | 85.2 ± 12.6 | 81.9 ± 11.8 * b |
| Hip circumference (cm) | 101.7 ± 9.2 | 97.1 ± 11.5 * c | 101.5 ± 9.9 | 99.6 ± 7.8 * b |
Trivial practically significant effect within groups (ES ≤ 0.20).
Small practically significant effect within groups (ES ≥ 0.20).
Moderate practically significant effect within groups (ES ≥ 0.50).
Statistically significant difference between pre and post (P < .05).
The Effect of HIIT and MICT on Metabolic Blood Measures
In the HIIT (0.4 mIU/L) and MICT groups (0.2 mIU/L), respectively, there was a tiny (ES = 0.37) and trivial (ES = 0.08) practically meaningful drop in fasting insulin; however, these reductions were not statistically significant (P > .05) (Table 3).
Table 3.
Change in Insulin Resistance Measures.
| Variables | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| Insulin fasting (mIU/L) | 6.7 ± 3.3 | 6.3 ± 3.1 b | 6.8 ± 3.5 | 6.6 ± 4.2 a |
| P-glucose fasting (mmol/l) | 6.6 ± 2.1 | 6.0 ± 2.2 * b | 6.1 ± 0.8 | 5.8 ± 0.6 a |
| Glucose: insulin ration | 1.2 ± 0.5 | 1.3 ± 0.4 b | 1.1 ± 0.5 | 1.3 ± 0.9 b |
| Insulin sensitivity (HOMA-IR) | 1.4 ± 1.1 | 1.2 ± 1.1 b | 1.6 ± 1.1 | 1.5 ± 1.3 a |
Trivial practically significant effect within group (ES ≤ 0.20).
Small practically significant effect within groups (ES ≥ 0.20).
Statistically significant difference between pre and post (P < .05).
Only the HIIT intervention resulted in substantially decreased fasting plasma glucose (HIIT 0.6 mmol/l vs MICT 0.2 mmol/l). The glucose: insulin ratio increased by 0.1 and 0.2 in the HIIT and MICT groups, respectively (P > .05; ES = 0.23 and 0.33, respectively), and there was a small but statistically significant change in insulin sensitivity (HOMA-IR) in the HIIT group, compared to a trivial but statistically significant change in the MICT group (P > .05; HIIT ES = 0.22 vs MICT ES = 0.09).
Table 4 shows blood lipid levels before and after the 16-week intervention for both the HIIT and MICT groups. Following the intervention, total cholesterol was lower in the HIIT group (0.4 mmol/l; P > .05; ES = 0.28), while it increased in the MICT group (0.2 mmol/l; P > .05; ES = − 0.12). Similarly, the MICT group had an increase in LDL-C (0.2 mmol/l; P > .05; ES = −0.13) while the HIIT group had a reduction (0.3 mmol/l; P > .05; ES = 0.22). In either group, there was no statistically or practically significant change in HDL-C (P > .05; ES 0.20). The HIIT group had a trivial practically significant change in TG compared to the MICT group, which had a small practically significant change in TG (HIIT 0.2 mmol/l; ES = 0.17vs MICT 0.1 mmol/l; ES = 0.27) and a trivial practically significant change in the cholesterol:HDL ratio (HIIT 0.2 mmol vs MICT 0.0 mmol/l; ES 0.2, in both cases).
Table 4.
Change in Blood Lipids.
| Variables | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| Total-cholesterol (mmol/l) | 6.8 ± 1.2 | 6.4 ± 1.1 b | 6.7 ± 0.8 | 6.9 ± 1.1 a |
| LDL-C(mmol/l) | 4.8 ± 1.1 | 4.5 ± 1.0 b | 4.4 ± 0.6 | 4.560.9 a |
| HDL-C (mmol/l) | 1.8 ± 0.5 | 1.8 ± 0.4 a | 1.8 ± 0.5 | 1.8 ± 0.5 a |
| Triglycerides (mmol/l) | 1.3 ± 0.8 | 1.1 ± 0.6 a | 1.3 ± 0.8 | 1.2 ± 0.7 b |
| Cholesterol : HDL ratio | 4.7 ± 1.0 | 4.5 ± 1.0 a | 4.6 ± 1.1 | 4.6 ± 1.1 a |
Trivial practically significant effect within groups (ES ≤ 0.20).
Small practically significant effect within groups (ES ≥ 0.20).
The Effect of HIIT and MICT on Functional Capacity
Table 5 depicts functional ability before and after the 16-week intervention as determined by the timed-up-and-go test (TUG). Following the intervention, there were statistically significant decreases in TUG test time in both the HIIT and MICT groups (HIIT 0.2 s vs MICT 0.1 s; p 0.05; ES = 0.41 and 0.28, respectively).
Table 5.
Change in Functional Capacity.
| Variables | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| TUG (s) | 6.5 ± 0.9 | 6.3 ± 0.8 * a | 6.6 ± 0.9 | 6.5 ± 0.9 * a |
Small practically significant effect within groups (ES ≥ 0.20).
Statistically significant difference between pre and post (P < .05).
The Effect of HIIT and MICT on Cardiorespiratory Fitness
The results for cardiorespiratory fitness as represented by the Bruce protocol termination time and projected VO2max before and after the 16-week intervention are shown in Table 6. Following the intervention, the HIIT group showed a statistically significant and substantial practically meaningful improvement in termination time (109 s; P = .003; ES = 0.87). In comparison, the MICT group showed just a tiny statistically significant improvement (21 s; P > .05; ES = 0.22). Similarly, the HIIT intervention resulted in a statistically and practically enhanced predicted VO2max (7.8 ml/kg/min; P = .01; ES = 0.85), compared to a marginally and practically significant change in the MICT group (2.8 ml/kg/min; P > .05; ES = 0.19).
Table 6.
Change in Cardiorespiratory Fitness.
| Variables | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| Termination time (s) | 267.5 ± 121.2 | 376.5 ± 94.2 * c | 269 ± 154.2 | 290 ± 79.8 b |
| Predicted VO2max (ml/kg/min) | 19.7 ± 11.1 | 27.5 ± 6.8 * c | 21.6 ± 11.4 | 24.4 ± 7.6 a |
Trivial practically significant effect within groups (ES ≤ 0.20).
Small practically significant effect within groups (ES ≥ 0.20).
Large practically significant effect within groups (ES ≥ 0.80).
Statistically significant difference between pre and post (P < .05).
The Effect of HIIT and MICT on Quality of Life
In this demographic group, the SF 36 version 2 was determined to be trustworthy (Cronbach’s = .85, .03). Table 7 depicts pre and post quality of life measurements among the groups following the 16-week intervention. Physical functioning (HIIT 1.2 vs MICT 0.6), body pain (HIIT −1.6 vs MICT 3.8), general health (HIIT: 2.1 vs MICT 3) and the physical component summary showed no statistically significant differences in either group (HIIT -1 vs MICT 0.9). Only the MICT group improved statistically significantly (P < .05) in role/physical (3.9), vitality/energy (3.9), social functioning (7.2), and mental health (5.4), whereas the HIIT group improved statistically significantly (P < .05) in role/emotional (3.9). Furthermore, both groups improved statistically significantly in the mental component summary (HIIT 4.8 vs MICT 3.8; P < .05).
Table 7.
Change in Quality of Life Score.
| Subscales of SF-36v2 | Pre HIIT | Post HIIT | Pre MICT | Post MICT |
|---|---|---|---|---|
| Physical functioning | 53.3 ± 3.8 | 54.5 ± 1.1 | 52.2 ± 5.5 | 52.8 ± 4.6 |
| Role/physical | 52.3 ± 5.5 | 55.6 ± 4.2 | 53.3 ± 2.6 | 57.2 ± 1.3* |
| Bodily pain | 54.3 ± 7.1 | 52.7 ± 8.2 | 52.6 ± 4.1 | 56.4 ± 7.2* |
| General health | 55.2 ± 6.5 | 57.3 ± 4.6 | 53.2 ± 6.6 | 56.2 ± 6.7 |
| Vitality/energy | 57.7 ± 2.2 | 58.7 ± 5.6 | 52.7 ± 6.1 | 56.6 ± 6.3* |
| Social functioning | 53.6 ± 6.7 | 57.2 ± 2.7 | 50.4 ± 7.6 | 57.6 ± 6.5* |
| Role/emotional | 52.4 ± 7.5 | 57.4 ± 6.9* | 53.6 ± 3.3 | 55.6 ± 3.7 |
| Mental health | 57.2 ± 6.3 | 59.7 ± 5.2 | 51.3 ± 7.5 | 56.7 ± 6.5* |
| Physical component summary | 56.2 ± 4.3 | 55.2 ± 5.6 | 53.7 ± 5.7 | 54.6 ± 7.5 |
| Mental component summary | 54.4 ± 5.4 | 59.2 ± 6.4* | 52.3 ± 9.2 | 56.1 ± 6.1* |
Statistically significant difference between pre and post (P < .05).
The impact magnitude of the differences between the HIIT and MICT groups is shown in Table 8. Furthermore, there was a moderately significant difference in body pain between the 2 groups (ES = 0.75), indicating that physical pain improved more with MICT than with HIIT. For all of the SF-36v2 subscales, there were no statistically significant interaction effects (P > .05).
Table 8.
Effect Sizes of Quality of Life.
| Subscales of SF-36v2 | HIIT vs MICT |
|---|---|
| Physical functioning | 0.17 a |
| Role/physical | −0.44 b |
| Bodily pain | −0.75 c |
| General health | −0.54 b |
| Vitality/energy | −0.50 b |
| Social functioning | −0.40 b |
| Role/emotional | −0.36 b |
| Mental health | −0.40 b |
| Physical component summary | −0.46 b |
| Mental component summary | −0.47 b |
Trivial practically significant effect between groups (ES ≤ 0.20).
Small practically significant effect between groups (ES ≥ 0.20).
Moderate practically significant effect between groups (ES ≥ 0.50).
Discussion
HIIT has been shown in several trials to enhance health-related outcomes such as aerobic capacity, insulin sensitivity, body composition, and HDL-C.49,58-61 However, there is insufficient information on the impact of HIIT on these health-related outcomes in elderly. The goal of this study was to investigate how a high intensity interval training (HIIT) program affected several health-related outcomes in elderly women.
Regular aerobic exercise training has been shown to lower body mass by increasing the quantity of calories spent. 62 HIIT programs performed 3 to 4 times per week for 8 to 16 weeks in healthy men and women, metabolic syndrome patients, and overweight and obese elderly, on the other hand, have shown inconsistencies in their findings regarding body composition, specifically body mass.33,38,60,63-65 Keating et al 63 and Wallman et al 64 discovered no significant body mass decrease with either HIIT or overweight people. This lack of improvement might be due to a gradual increase in the length of HIITsessions over a 12-week period, with individuals only maximizing calorie expenditure in week 5 (HIIT: 20-24 min vs MICT: 36-45 min). 63 Furthermore, the exercise intervention could not have been long enough (8 weeks). 64 Trapp et al 38 discovered a substantial decrease in body mass after 15 weeks of HIIT. Although no statistically significant change in calorie expenditure treatments was discovered, HIIT resulted in higher calorie expenditure over time.
Furthermore, Schjerve et al 60 and Tjonna et al 49 discovered a substantial reduction in body mass in the HIIT group with a 12 to 16 week intervention in obese individuals and patients with metabolic syndrome. This similar drop may be due to the isocaloric nature of HIIT, as predicted. However, despite the fact that the 2 protocols were isocaloric, the body mass of the HIIT participants was not significantly reduced, whereas the MICT group obtained a considerable body mass reduction of 1.3 kg.This lack of significant change in body mass in the HIIT group may be attributed to an increase in muscle mass. 66 As Mitranun et al 67 reported a significant increase in quadriceps and hamstrings muscle strength with 12 weeks of cycle ergometer based HIIT in type 2 diabetic patients. Although a measurement of muscle mass and strength was not included in this study, the HIIT and MICT participants had similar reductions in body fat percentage and abdominal diameter following the intervention. This suggests that leg muscle mass was increased due to the nature of cycle ergometer incline during the HIIT program, therefore compensating for the lack of change in body mass.
Despite the fact that there was little change in body mass and no controlled dietary intervention, this study indicated that frequent participation in HIIT can considerably ameliorate abdominal obesity. This is critical since excess body fat accumulation, particularly in the abdominal area, has been identified as an independent risk factor for insulin resistance, cardiovascular disease, and mortality. HIIT is therefore thought to improve body fat percentage and abdominal obesity, however a corresponding effect on body mass is not always obvious. It might be argued that the primary goal of elderly fitness training should not be weight loss, but rather visceral adiposity reduction, which would result in a lower risk of cardiovascular and metabolic disorders. 68
It has been proposed that those with higher levels of insulin resistance have a stronger metabolic response to exercise. 69 Despite the fact that the MICT group had higher insulin levels at baseline than the HIIT group, the latter group showed a bigger drop in fasting insulin, resulting in a lower death rate. Although the findings with HIIT were not significant, it is hypothesized that HIIT may improve insulin signaling and insulin action in muscle, resulting in lower intracellular buildup of TG and higher fatty acid oxidation.23,49 This shows that HIIT has the potential to enhance insulin metabolism in healthy individuals to a higher extent, lowering the risk of developing T2DM. This data also implies that the effect of exercise on insulin activity in muscle is reliant on the intensity of the exercise, as the individuals in both groups did the same amount of labor.
The time it took participants to complete their blood tests following post-testing might potentially have an impact on the study’s findings. Although participants were told they had 24 h to complete these assessments, this was not always the case. Exercise has a diminishing effect on insulin sensitivity over time, and insulin sensitivity increases for just 24 to 48 h after the previous session of exercise. 70 Although the gains in insulin sensitivity were not statistically significant, individuals in the HIIT group improved their insulin sensitivity more significantly than the MICT group. Thus, HIIT may be able to improve insulin action in elderly to a larger extent than MICT, implying HIIT as an alternate type of exercise to improve metabolic health in elderly at risk for insulin resistance.
Elevated cholesterol levels, particularly LDL-C, are a major risk factor for cardiovascular disease, and lowering LDL-C should be the primary goal for elderlypersons diagnosed with dyslipidaemia. 51 In the current study, neither HIIT nor MICT resulted in a significant reduction in total cholesterol or LDL-C. This is consistent with earlier study that used comparable isocaloric HIIT and MICT programs for 8 to 12 weeks in young women, CAD patients, overweight elderly, and HF patients.23,34,64,71 Furthermore, 8 to 12 weeks of HIIT conducted by young and middle-aged men with no similar isocaloric control procedure did not result in substantial changes in total cholesterol and LDL-C.72,73
Participants in both groups had high total cholesterol and LDL-C levels at the start of the trial, putting them at a greater risk of cardiovascular and metabolic illness. 51 Despite no significant decreases in either group, HIIT resulted in a more practically meaningful reduction in total cholesterol and LDL-C, whereas individuals in the MICT group had higher levels at the conclusion of the intervention period. This is in contrast to recent research, which found that continuous aerobic exercise resulted in higher improvements in these variables than an isocaloric HIIT program in overweight and obese individuals and HF patients.59,60,74
Improving and maintaining functional capacity is critical to avoiding physical deterioration as we age. 45 Both HIIT and the MICT group improved their functional capacity significantly in the current study, as determined by the timed-up-and-go test (TUG). This is significant because it shows that elderly persons participating in HIIT may enhance and maintain their physical function and mobility as they age. This allows individuals to maintain their independence by improving their capacity to undertake daily activities.
This study’s findings are consistent with those of Adamson et al 45 and Nilsson et al, 37 who found that 8 weeks of HIIT improved functional capacity as determined by the 6 min walk test, TUG, sit to stand test, and 50 m load walk test in middle-aged people and HF patients. Furthermore, Koufaki et al 75 and Freyssin et al 40 found that 8 to 24 weeks of HIIT improved functional capacity in HF patients as determined by the 6-min walk test, sit-to-stand test, and gait speed analyzes. Both trials contained HIIT routines, however they were not isocaloric.
Improving cardiorespiratory fitness is an important element of living a healthy lifestyle since poor fitness levels are associated with an increased risk of early mortality from any cause, including cardiovascular disease. 51 Cardiorespiratory fitness, as determined by the Bruce protocol in this study, was considerably enhanced with HIIT compared to MICT. The HIIT group outperformed the MICT group in terms of projected VO2max. These findings are comparable to similar isocaloric HIIT programs,34,49,60 which found a 35%, 33%, and 46% increase in VO2max with HIIT in obese elderly, HF, and metabolic syndrome patients, respectively.
The current study demonstrates that training intensity, not volume, is the most important factor in enhancing cardiorespiratory fitness, which is the core training premise of HIIT. More research is needed to determine whether elderly can achieve these superior improvements in a shorter time span, as previous evidence suggests that increases in cardiorespiratory fitness with HIIT occur in only 50% to 60% of the time required for the same gain with continuous aerobic exercise in middle-aged elderly. 63
Both HIIT and MICT improved various areas of quality of life significantly. The HIIT group participants reported substantial improvements in role-emotional and mental component summary. This correlates to improved emotional wellbeing in the workplace, as well as improved mental health and emotional well-being overall. Participants in the MICT group, on the other hand, reported substantial improvements in role-physicality, vitality and energy, social functioning, mental health, and mental component summary. This leads to an improvement in the physical elements of the workplace, an increase in energy levels and weariness, an improvement in the quality and quantity of social connections, and an overall improvement in mental health and emotional well-being. This shows that the MICT group improved more SF-36v2 subscales than the HIIT group, contributing to an improved overall quality of life. Surprisingly, the MICT group reported a somewhat significant reduction in physical pain following the intervention, but the HIIT group reported a deterioration in bodily pain.
The findings of the present study are in contrast with previous research which found that HIIT improved quality of life more than MICT61,76 in heart disease patients. This improvement may be attributed to participants finding more intensive physical training to be more rewarding. 61 The opposite was true for the present study and this difference may be attributed to the age of the participants and the potential for recovery. The lack of significant improvement in quality of life may be due to an increased incidence of bodily pain or muscle soreness as a result of HIIT. As recovery between sessions was only one full day, the incidence of bodily pain experienced by the HIIT group may have reduced overall physicality as indicated by the physical component summary, thereby contributing to a reduced quality of life, despite an improvement in the mental component summary. Recent evidence suggests that elderly are able to significantly improve aerobic capacity, physical function and glucose control by completing 2 sessions of HIIT per week compared to 3. 45 This would allow elderly sufficient recovery time while still attaining the associated health benefits of HIIT.
The current study’s findings contradict prior studies that revealed HIIT enhanced quality of life in heart disease patients.61,76 This improvement might be attributable to individuals finding more intense physical exercise more enjoyable. 61 The contrary was true in the current investigation, which might be attributable to the subjects’ age and the possibility of recovery. The absence of substantial improvement in quality of life might be attributed to an increase in body pain or muscular stiffness as a result of HIIT. Because recuperation between sessions was just one full day, the HIIT group’s incidence of body discomfort may have lowered overall physicality, as shown by the physical component summary, resulting to a lower quality of life despite an improvement in the mental component summary. Recent data reveals that people can considerably increase their aerobic capacity, physical function, and glycemic management by doing 2 HIIT sessions per week instead of 3. 45 This would give people enough time to recuperate while still reaping the health advantages of HIIT.
Previous studies discovered that HIIT is safe, efficient, and low-risk for healthy elderly persons. This conclusion was reinforced by 4 studies that demonstrated no negative effects after 8 to 16 weeks of HIIT in HF and CAD patients.40,61,71,77 Rognmo et al 77 studied the safety of HIIT in 4846 individuals with coronary artery disease. The results showed that there is a minimal probability of a cardiovascular event occurring during HIIT, with just 2 non-fatal cardiac events occurring during HIIT. 77 Healthcare specialists have previously judged HIIT contentious for the treatment of high-risk patients.41,78 However, no negative effects have been documented in comparison to huge improvements, therefore HIIT can be recommended for a wide variety of particular groups, including elderly. However, prior study participants were deemed stable, therefore HIIT may not be suited for some illness groups. In conclusion, when participants are properly screened and enough contact with the patient’s doctor is maintained, HIIT can be a safe exercise alternative for high-risk people and elderly.
Limitations
First of all, the sample size was insufficient because a larger population is required to boost the reliability of the findings. Second, the use of the Bruce protocol in this study was constrained and might have underestimated the subject’s level of cardiorespiratory fitness. Several of the test subjects were unaccustomed to the test’s first slope of 10 degrees because it does not simulate daily walking. Due to the rapid increase in heart rate brought on by the steep hill, people reached their target heart rates earlier than intended. Given that no adverse effects associated to any cardiac events were observed and the HIIT exercise sessions were done at a close to maximal intensity, a more realistic assessment of cardiorespiratory fitness should have been employed. Even a maximal exercise test should have been used.
Although it was requested that participants keep their existing way of life, level of physical activity, and food while taking part in the study, this was not monitored, and the degree to which they followed these instructions was not assessed. The inability to regulate how long after post-testing subjects waited to have blood collected for measurements of insulin resistance and the blood lipid profile was another drawback of this study. The metabolic blood measurements may have been impacted by the delay, even though they were supposed to see Pathcare 24 h after post-testing. Finally, the lack of a measurement of leg muscular strength or mass may have contributed to the HIIT group’s inability to experience a change in body mass.
Conclusions
In conclusion, 16 weeks of HIIT resulted in positive health-related outcomes in elderly. Elderly who participated in an HIIT program had similar or higher changes in body composition, insulin resistance measurements, cardiorespiratory fitness, and functional ability. These advantages advocate HIIT as an alternative training regimen for elderly. In addition, future research should focus on developing an ideal workout program for elderly that combines HIIT with other types of training.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ashira Hiruntrakul  https://orcid.org/0000-0003-1292-1897
https://orcid.org/0000-0003-1292-1897
Ethics: The Ethics Committee for Human Research at Universitas PGRI Semarang (HE30/2020) authorized this study proposal
References
- 1.World Health Organization. Media centre Obesity and overweight. Accessed March 1, 2019. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2.Humphries CKS, Roger LH.Current Diagnosis and Treatment Emergency Medicine, 6th ed.McGaraw Hill; 2011. [Google Scholar]
- 3.Jialal I, Vikram N.Nutrition therapy for diabetes: Implications for decreasing cardiovascular complications. J Diabetes Complications. 2017;31(10):1477-1480. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Media centre Obesity and overweight. Accessed March 1, 2019. https://www.who.int/health-topics/obesity#tab=tab_1
- 5.Kementerian Kesehatan Republik Indonesia. Potret sehat indonesia dari riskesdas 2018. Accessed March 1, 2019. https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-indonesia-2019.pdf
- 6.Polyzos SA, Margioris AN.Sarcopenic obesity. Hormones. 2018;17(3):321-331. [DOI] [PubMed] [Google Scholar]
- 7.Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. New Engl J Med. 2011;364(14):1315-1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Accessed March 1, 2019. https://apps.who.int/iris/handle/10665/206936
- 9.World Health Organization. Global recommendations on physical activity for health. Accessed March 1, 2019. http://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng.pdf?sequence=1 [PubMed]
- 10.Janssen I, Leblanc AG.Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7(40):1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rainer R, Katriina KH, Jari A, et al. Update on current care guidelines: physical activity and exercise training for adults in sickness and in health. Duodecim. 2011;127(2):150-151. [PubMed] [Google Scholar]
- 12.Carroll S, Dudfield M.What is the relationship between exercise and metabolic abnormalities? A review of the metabolic syndrome. Sports Med. 2004;34(6):371-418. [DOI] [PubMed] [Google Scholar]
- 13.Warburton DE, Nicol CW, Bredin SS.Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Church T.Exercise in obesity, metabolic syndrome, and diabetes. Prog Cardiovasc Dis. 2011;53(6):412-418. [DOI] [PubMed] [Google Scholar]
- 15.Kassi E, Pervanidou P, Kaltsas G, Chrousos G.Metabolic syndrome: definitions and controversies. BMC Med. 2011;9(1):48-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thyfault JP, Rector RS, Noland RC.Metabolic inflexibility in skeletal muscle: a prelude to the cardiometabolic syndrome? J Cardiometab Syndr. 2006;1(3):184-189. [DOI] [PubMed] [Google Scholar]
- 17.Desai M, Jellyman JK, Han G, Beall M, Lane RH, Ross MG.Maternal obesity and high-fat diet program offspring metabolic syndrome. Am J Obstet Gynecol. 2014;211(3):237.e1-237.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abate N.Obesity and cardiovascular disease: Pathogenetic role of the metabolic syndrome and therapeutic implications. J Diabetes Complications. 2000;14(3):154-174. [DOI] [PubMed] [Google Scholar]
- 19.Gill JM, Celis-Morales CA, Ghouri N.Physical activity, ethnicity and cardio-metabolic health: does one size fit all? Atherosclerosis. 2014;232(2):319-333. [DOI] [PubMed] [Google Scholar]
- 20.Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome-a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabetic Med. 2006;23(5):469-480. [DOI] [PubMed] [Google Scholar]
- 21.Metcalfe RS, Babraj JA, Fawkner SG, Vollaard NB.Towards the minimal amount of exercise for improving metabolic health: beneficial effects of reduced-exertion high-intensity interval training. Eur J Appl Physiol. 2012;112(7):2767-2775. [DOI] [PubMed] [Google Scholar]
- 22.Oda E, Kawai R.Comparison among body mass index (BMI), waist circumference (WC), and percent body fat (%BF) as anthropometric markers for the clustering of metabolic risk factors in Japanese. Intern Med. 2010;49(15):1477-1482. [DOI] [PubMed] [Google Scholar]
- 23.Ciolac EG, Bocchi EA, Bortolotto LA, Carvalho VO, Greve JM, Guimarães GV. Effects of high-intensity aerobic interval training vs. Moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension. Hypertens Res. 2010;33(8):836-843. [DOI] [PubMed] [Google Scholar]
- 24.Greenway FL, Pekarovics S. Anthropometry of local fat reduction. In: Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease, edited by R.P. Victor, 1989-2005. Springer; 2012. [Google Scholar]
- 25.Landry BW, Driscoll SW.Physical activity in children and adolescents. PM R. 2012;4(11):826-832. [DOI] [PubMed] [Google Scholar]
- 26.Ferguson B. ACSM’s guidelines for exercise testing and prescription 9th ed. 2014. J Can Chiropr Assoc. 2014;58(3):328. [Google Scholar]
- 27.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-1359. [DOI] [PubMed] [Google Scholar]
- 28.Kessler HS, Sisson SB, Short KR.The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42(6):489-509. [DOI] [PubMed] [Google Scholar]
- 29.Gaesser GA, Angadi SS.High-intensity interval training for health and fitness: can less be more? J Appl Physiol. 2011;111(6):1540-1541. [DOI] [PubMed] [Google Scholar]
- 30.Herrera Covarrubias CI, De León LG, Candia Luján R, Ortiz Rodríguez B, Carrasco Legleu CE.HIIT in a treadmill for people with overweight or obesity: a systematic review. TECNOCIENCIA Chihuahua. 2021;15(1):52-61. [Google Scholar]
- 31.de Matos MA, Garcia BCC, Vieira DV, et al. High-intensity interval training reduces monocyte activation in obese adults. Brain Behav Immun. 2019;80:818-824. [DOI] [PubMed] [Google Scholar]
- 32.Meyer P, Gayda M, Juneau M, Nigam A.High-intensity aerobic interval exercise in chronic heart failure. Curr Heart Fail Rep. 2013;10(2):130-138. [DOI] [PubMed] [Google Scholar]
- 33.Helgerud J, Høydal K, Wang E, et al. Aerobic high-intensity intervals improve V˙O2max more than moderate training. Med Sci Sports Exerc. 2007;39(4):665-671. [DOI] [PubMed] [Google Scholar]
- 34.Wisløff U, Ellingsen, Kemi OJ.High-intensity interval training to maximize cardiac benefits of exercise training? Exerc Sport Sci Rev. 2009;37(3):139-146. [DOI] [PubMed] [Google Scholar]
- 35.Heydari M, Freund J, Boutcher SH.The effect of high-intensity intermittent exercise on body composition of overweight young males. J Obes. 2012;6:480467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Devlin JT, Horton ES.Effects of prior high-intensity exercise on glucose metabolism in normal and insulin-resistant men. Diabetes. 1985;34(10):973-979. [DOI] [PubMed] [Google Scholar]
- 37.Nilsson BB, Westheim A, Risberg MA.Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. Am J Cardiol. 2008;102(10):1361-1365. [DOI] [PubMed] [Google Scholar]
- 38.Trapp EG, Chisholm DJ, Freund J, Boutcher SH.The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes. 2008;32(4):684-691. [DOI] [PubMed] [Google Scholar]
- 39.Talanian JL, Galloway SD, Heigenhauser GJ, Bonen A, Spriet LL.Two weeks of high-intensity aerobic interval training increases the capacity for fat oxidation during exercise in women. J Appl Physiol. 2007;102(4):1439-1447. [DOI] [PubMed] [Google Scholar]
- 40.Freyssin C, Verkindt C, Prieur F, Benaich P, Maunier S, Blanc P.Cardiac rehabilitation in chronic heart failure: Effect of an 8-week, high-intensity interval training versus continuous training. Arch Phys Med Rehabil. 2012;93(8):1359-1364. [DOI] [PubMed] [Google Scholar]
- 41.Weston KS, Wisløff U, Coombes JS.High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227-1234. [DOI] [PubMed] [Google Scholar]
- 42.Little JP, Gillen JB, Percival ME, et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol. 2011;111(6):1554-1560. [DOI] [PubMed] [Google Scholar]
- 43.Wewege M, van den Berg R, Ward RE, Keech A. The effects of high-intensity interval training vs. Moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes Rev. 2017;18(6):635-646. [DOI] [PubMed] [Google Scholar]
- 44.Liu J, Zhu L, Su Y.Comparative effectiveness of high-intensity interval training and moderate-intensity continuous training for cardiometabolic risk factors and cardiorespiratory fitness in childhood obesity: A meta-analysis of randomized controlled trials. Front Physiol. 2020;11:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adamson S, Lorimer R, Cobley JN, Lloyd R, Babraj J.High intensity training improves health and physical function in middle aged adults. Biology. 2014;3(2):333-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Racil G, Ben Ounis O, Hammouda O, et al. Effects of high vs. Moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. 2013;113(10):2531-2540. [DOI] [PubMed] [Google Scholar]
- 47.Fisher G, Brown AW, Bohan Brown MM, et al. High intensity interval- vs moderate intensity- training for improving cardiometabolic health in overweight or obese males: a randomized controlled trial. PLoS One. 2015;10(10):e0138853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tarasov K, Ekroos K, Suoniemi M, et al. Molecular lipids identify cardiovascular risk and are efficiently lowered by simvastatin and PCSK9 deficiency. J Clin Endocrinol Metab. 2014;99(1):45-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tjønna AE, Lee SJ, Rognmo, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation. 2008;118(4):346-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C.Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics. 2005;115(4):e500-e503. [DOI] [PubMed] [Google Scholar]
- 51.Pescatello LS. American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription 9th ed.J Can Chiropr Assoc. 2014;58(3):328. [DOI] [PubMed] [Google Scholar]
- 52.Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A.Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J. 1982;103(3):363-373. [DOI] [PubMed] [Google Scholar]
- 53.Foster C, Jackson AS, Pollock ML, et al. Generalized equations for predicting functional capacity from treadmill performance. Am Heart J. 1984;107(6):1229-1234. [DOI] [PubMed] [Google Scholar]
- 54.Richardson S.The timed “up & go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148. [DOI] [PubMed] [Google Scholar]
- 55.Shumway-Cook A, Brauer S, Woollacott M.Predicting the probability for falls in community-dwelling adults using the timed up and go test. Phys Ther. 2000;80(9):896-903. [PubMed] [Google Scholar]
- 56.Davenport TE, Stevens SR, Baroni K, Mark Van Ness J, Snell CR.Reliability and validity of Short Form 36 version 2 to measure health perceptions in a sub-group of individuals with fatigue. Disabil Rehabil. 2011;33(25-26):2596-2604. [DOI] [PubMed] [Google Scholar]
- 57.Tsigos C, Bitzur R, Kleinman Y, et al. Targets for body fat, blood pressure, lipids, and glucose-lowering interventions in healthy older people. Diabetes Care. 2013;36(Supplement_2):S292-S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Whyte LJ, Ferguson C, Wilson J, Scott RA, Gill JMR. Effects of single bout of very high-intensity exercise on metabolic health biomarkers in overweight/obese sedentary men. Metabolism. 2013;62(2):212-219. [DOI] [PubMed] [Google Scholar]
- 59.Moreira MM, Souza HP, Schwingel PA, Sá CK, Zoppi CC.Effects of aerobic and anaerobic exercise on cardiac risk variables in overweight adults. Arq Bras Cardiol. 2008;91(4):200-219. [DOI] [PubMed] [Google Scholar]
- 60.Schjerve IE, Tyldum GA, Tjønna AE, et al. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin Sci. 2008;115(9):283-293. [DOI] [PubMed] [Google Scholar]
- 61.Wisløff U, Støylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation. 2007;115(24):3086-2094. [DOI] [PubMed] [Google Scholar]
- 62.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS.The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Keating SE, Machan EA, O’Connor HT, et al. Continuous exercise but not high intensity interval training improves fat distribution in overweight adults. J Obes. 2014;2014:834865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wallman K, Plant LA, Rakimov B, Maiorana AJ.The effects of two modes of exercise on aerobic fitness and fat mass in an overweight population. Res Sports Med. 2009;17(3):156-170. [DOI] [PubMed] [Google Scholar]
- 65.Tjønna AE, Stølen TO, Bye A, et al. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clin Sci. 2009;116(4):317-326. [DOI] [PubMed] [Google Scholar]
- 66.Boudou P, Sobngwi E, Mauvais-Jarvis F, Vexiau P, Gautier JF.Absence of exercise-induced variations in adiponectin levels despite decreased abdominal adiposity and improved insulin sensitivity in type 2 diabetic men. Eur J Endocrinol. 2003;149(5):421-424. [DOI] [PubMed] [Google Scholar]
- 67.Mitranun W, Deerochanawong C, Tanaka H, Suksom D.Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand J Med Sci Sports. 2014;24(2):e69-e76. [DOI] [PubMed] [Google Scholar]
- 68.Darmon P.Intentional weight loss in older adults: useful or wasting disease generating strategy? Curr Opin Clin Nutr Metab Care. 2013;16(3):284-289. [DOI] [PubMed] [Google Scholar]
- 69.Gremeaux V, Drigny J, Nigam A, et al. Long-term lifestyle intervention with optimized high-intensity interval training improves body composition, cardiometabolic risk, and exercise parameters in patients with abdominal obesity. Am J Phys Med Rehabil. 2012;91(11):941-950. [DOI] [PubMed] [Google Scholar]
- 70.Rynders CA, Weltman A.High-intensity exercise training for the prevention of type 2 diabetes mellitus. Phys Sportsmed. 2014;42(1):7-14. [DOI] [PubMed] [Google Scholar]
- 71.Moholdt TT, Amundsen BH, Rustad LA, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: A randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;158(6):1031-1037. [DOI] [PubMed] [Google Scholar]
- 72.Nybo L, Sundstrup E, Jakobsen MD, et al. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc. 2010;42(10):1951-1958. [DOI] [PubMed] [Google Scholar]
- 73.Musa DI, Adeniran SA, Dikko AU, Sayers SP.The effect of a high-intensity interval training program on high-density lipoprotein cholesterol in young men. J Strength Cond Res. 2009;23(2):587-592. [DOI] [PubMed] [Google Scholar]
- 74.Iellamo F, Manzi V, Caminiti G, et al. Matched dose interval and continuous exercise training induce similar cardiorespiratory and metabolic adaptations in patients with heart failure. Int J Cardiol. 2013;167(6):2561-2565. [DOI] [PubMed] [Google Scholar]
- 75.Koufaki P, Mercer TH, George KP, Nolan J.Low-volume high-intensity interval training vs continuous aerobic cycling in patients with chronic heart failure: a pragmatic randomised clinical trial of feasibility and effectiveness. J Rehabil Med. 2014;46(4):348-356. [DOI] [PubMed] [Google Scholar]
- 76.Molmen-Hansen HE, Stolen T, Tjonna AE, et al. Aerobic interval training reduces blood pressure and improves myocardial function in hypertensive patients. Eur J Prev Cardiol. 2012;19(2):151-160. [DOI] [PubMed] [Google Scholar]
- 77.Rognmo Ø, Moholdt T, Bakken H, et al. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126(12):1436-1440. [DOI] [PubMed] [Google Scholar]
- 78.Gripp F, Nava RC, Cassilhas RC, et al. HIIT is superior than MICT on cardiometabolic health during training and detraining. Eur J Appl Physiol. 2021;121(1):159-172. [DOI] [PubMed] [Google Scholar]