Abstract
There is growing consensus in the family planning community around the need for novel measures of autonomy. Existing literature highlights the tension between efforts to pursue contraceptive targets and maximize uptake on the one hand, and efforts to promote quality, person-centeredness, and contraceptive autonomy on the other hand. Here, we pilot a novel measure of contraceptive autonomy, measuring it at two Health and Demographic Surveillance System sites in Burkina Faso. We conducted a population-based survey with 3,929 women of reproductive age, testing an array of new survey items within the three subdomains of informed choice, full choice, and free choice. In addition to providing tentative estimates of the prevalence of contraceptive autonomy and its subdomains in our sample of Burkinabè women, we critically examine which parts of the proposed methodology worked well, what challenges/limitations we encountered, and what next steps might be for refining, improving, and validating the indicator. We demonstrate that contraceptive autonomy can be measured at the population level but a number of complex measurement challenges remain. Rather than a final validated tool, we consider this a step on a long road toward a more person-centered measurement agenda for the global family planning community.
INTRODUCTION
Measuring Contraceptive Autonomy
Quality of care has long been of interest to the international family planning community, with Judith Bruce’s 1990 conceptual framework serving as the foundational text for researchers and family planning programmers. Bruce’s quality of care framework identified the key dimensions of technical and interpersonal quality that would guide the family planning field for decades to come. In recent years, major reproductive health funders (The David and Lucile Packard Foundation 2019), nongovernmental organizations (NGOs), (Tumlinson 2016), and multilateral agencies (UNFPA 2016) have called for a renewed focus on high-quality family planning services, both as part of a rights-based agenda as well as a means to promote contraceptive uptake (Hardee et al. 2014). This push toward high quality of care in family planning is echoed elsewhere in global health by bodies such as the Lancet Commission on High Quality Health Systems in the Sustainable Development Goal Era, which affirms the critical importance of quality more broadly throughout all areas of health care provision and research (Kruk et al. 2018). At the core of this work is the recognition that it is not sufficient for health services to be technically proficient. Rather, they must focus on the user experience and promote a patient-centered approach to care that is responsive to individual needs and desires.
This focus on responsiveness to user preferences is perhaps even more important in family planning than many other fields, due to the histories of Eugenics, neo-Malthusian population control, and sterilization abuse that have been enmeshed with family planning (Connelly 2008; Hartmann 1987; Rao 2004; Roberts 1997). The 1994 International Conference on Population and Development in Cairo shifted the family planning discourse away from overt population control, and has been lauded as the convening that ended the population control era (Langer 2006; Ashford 2014). Yet, despite this common framing, a focus on fertility reduction and increasing contraceptive uptake has remained at the core of most global family planning programs (Potts et al. 2011; Cleland, Ndugwa, and Zulu 2011; Ouedraogo et al. 2021; Cahill et al. 2018). One of the key ways in which the family planning community shows its abiding concern for fertility decline–a concern that has persisted even in a post-Cairo era–is through its measures, which have remained primarily focused on pregnancy intentions and contraceptive uptake (specifically of the most effective modern methods).
As many social scientists have noted, measurement is an important way through which a community formulates and communicates its priorities. Rather than technocratic assessments of objective truth, these scholars have described the process of quantification as a politicized form of knowledge production that “flies under the radar of social and political analysis as a form of power” (Merry 2016). As quantitative indicators are an essential tool for making sense of the complex world around us, understanding and interrogating their political and ideological orientation is equally imperative. The widespread adoption and promotion of specific indicators signal tacit agreement that these are the core constructs that matter to a given community.
As such, the ways that quantitative family planning metrics–primarily focused on contraceptive uptake–have been transformed into programmatic goals have had important implications on the design and implementation of contraceptive programs. Our previous work and that of others have shown how certain targets (such as increased rates of contraceptive uptake and continuation, increased use of the most effective methods, etc.) can reduce the quality of care and create perverse incentives for contraceptive coercion (Senderowicz et al. 2021; Senderowicz 2020; 2019; Towriss et al. 2019; Britton et al. 2021; Connelly 2008; Hendrixson 2018). In Tanzania, for example, the implementation of a postpartum intrauterine device (IUD) intervention led to biased contraceptive counseling, with providers emphasizing the benefits of the IUD and discouraging women from using other methods (Senderowicz et al. 2021; Senderowicz et al. 2022). In an anonymized sub-Saharan African country, qualitative data showed that women had a wide range of nonautonomous experiences with family planning providers pursuing uptake targets, ranging from false medical information to nonconsented provision of long-acting reversible contraceptives (LARCs) (Senderowicz and Kolenda 2022; Senderowicz 2019). A South African study found that postpartum women were given the injectable as a matter of routine and often without consent (Towriss et al. 2019; Towriss and Rucell 2019). In Kenya, Ethiopia, and Ghana, women have reported that providers refuse to remove LARC methods upon request (Britton et al. 2021; Yirgu et al. 2020; Callahan et al. 2020).
These studies add to the growing body of evidence highlighting the tension between efforts to pursue contraceptive targets and maximize the number of contraceptive users on the one hand, and efforts to promote the high quality of care, person-centeredness, and contraceptive autonomy on the other hand. These data from qualitative studies show serious lapses in quality of care and contraceptive autonomy as family planning programs pursue quantitative targets. This evidence puts into sharp relief both (1) how existing population-based measures create the wrong incentives for programs and providers, contributing to adverse contraceptive outcomes and coercion; and (2) how we lack quantitative measurement tools both to help us understand these adverse outcomes, and to create new incentives that promote contraceptive autonomy.
Researchers have made important strides in recent years in measuring the quality of care at the service provision level, with a spate of innovative research assessing the validity of standard approaches to quality measurement (Tumlinson et al. 2014), putting forward new frameworks and definitions (Holt, Dehlendorf, and Langer 2017), and testing new measurement scales (Holt et al. 2018). At the population level, however, there have been fewer attempts to develop novel person-centered family planning measurement approaches. The field of family planning currently relies on a suite of measurements that provide insight into the number of women using contraception, the types of contraception being used, and fertility patterns (including both total fertility as well as pregnancy intentions). But there is no widely used population-level indicator for family planning that measures the extent to which family planning programs are responsive to people’s needs and/or promote the ability to make autonomous decisions about family planning.
To begin to fill this gap, one of our team made the case for a novel indicator of contraceptive autonomy in a 2020 article in Studies of Family Planning (Senderowicz 2020). In that piece, Senderowicz argued that indicators of success for family planning should be person-centered and agnostic on questions of contraceptive uptake or fertility decline. In particular, that article argued that a new measure of contraceptive autonomy could help remove the structural measurement incentives for contraceptive coercion by reconceptualizing autonomous nonuse of contraception among women with no desire to use as a positive rather than negative outcome (Senderowicz 2020). That report concludes in part by asking readers to imagine what family planning would look like, instead of emerging from the population control movement, it had been created based entirely on reproductive well-being, postulating that concerns about contraceptive uptake would almost certainly be replaced by a more holistic focus on contraceptive autonomy and reproductive justice.
Beyond laying out the rationale for the new indicator, Senderowicz’s (2020) report also proposed a tentative methodology for calculating contraceptive autonomy. That article defines contraceptive autonomy as “the factors necessary for a person to decide for themself what they want in relation to contraception and then to realize that decision.” Then, borrowing from the work of Newman and Feldman-Jacobs, that paper breaks down the construct of contraceptive autonomy into the three subcomponents of informed choice, full choice, and free choice, and provides a framework for how to operationalize and measure these subcomponents via a population-based survey (Newman and Feldman-Jacobs 2015). To date, no empirical work has been published that operationalizes and tests the measure of contraceptive autonomy proposed in that article or attempts to apply the measurement approach to real data.
Testing this Approach in Burkina Faso
This paper applies the conceptual and methodological framework for contraceptive autonomy articulated in Senderowicz (2020) to a random sample of women of reproductive age from Burkina Faso, a country in the Sahel region of West Africa. West Africa is home to the second lowest contraceptive prevalence (25 percent) and second highest total fertility rate (5.3) globally, which has made the region a magnet for family planning investment in the past decade (Kaneda and Greenbaum 2019). Prior to 2011, there had been relatively little focus on the region from donors and NGOs seeking to promote family planning. And unlike South Asia, East Asia, or Latin America, the region had little history of large-scale population planning or other major government intervention, either pro- or antinatalist.
In 2011, the Regional Conference on Population, Development and Family Planning was held in Ouagadougou, Burkina Faso, bringing together international donors and the governments of nine francophone West African countries to create what has since been named the “Ouagadougou Partnership.” The main objective of the Partnership was to add 2,200,000 new family planning users to the region by 2020 (Population Reference Bureau 2011). The Ouagadougou Partnership (in collaboration with the global Family Planning 2020/2030 initiative) has galvanized governments, funders, and NGOs to make expanding family planning in francophone West Africa a priority (Population Reference Bureau 2011; Guttmacher Institute 2020).
As part of its commitment to the Ouagadougou Partnership, in 2013, the government of Burkina Faso issued a plan to “Relaunch Family Planning” in the country and set quantitative goals to help measure their progress in promoting contraception (Ministry of Health of Burkina Faso 2013). The overall national goal at that time was set to raise the modern contraceptive prevalence rate (mCPR) among married/in-union women from 15 percent in 2010 to 25 percent by 2015. This mCPR target was further divided by region, with some regions (considered regions with “strong potential”) given more ambitious targets than others (regions with “weak potential”). By 2017, a new document, now called a plan to “Accelerate Family Planning” was adopted by the Burkinabè government, with new targets for the year 2020 (Ministry of Health of Burkina Faso 2017). Overall, this plan aimed for an mCPR of 32 percent by 2020, and again, broke down that target by administrative region. The Acceleration Plan included the crude number of new contraceptive users needed to attain this goal (348,163 women), as well as a disaggregation of these figures by region and year. Additionally, the Acceleration plan included a breakdown of mCPR targets by method, with a strong focus on increasing the use of medium and long-acting methods: implants, IUDs, and injectables (Ministry of Health of Burkina Faso 2017).
Along with this recent influx of funding and programming for family planning has come a great deal of new research on contraception in Burkina Faso. Recent studies have concentrated in particular on contraceptive uptake in the postpartum period, joining a body of literature primarily focused on fertility patterns and contraceptive use dynamics (Rossier and Hellen 2014; Population Reference Bureau 2011; Potts et al. 2011; Pearson and Becker 2014; Speizer 2006; Morroni and Glasier 2020; Tran et al. 2019; Coulibaly et al. 2021). Some studies have explored the quality of contraceptive care in Burkina Faso as it relates to subsequent contraceptive use (Fruhauf et al. 2018), but less is known about dimensions of person-centeredness, respect for rights, and contraceptive autonomy in the country.
In this paper, we follow up on the proposed measurement of contraceptive autonomy, applying its methodology to a population-based sample of nearly 4,000 reproductive-aged women at two sites in Burkina Faso. We measure the contraceptive autonomy indicator for the first time. In addition to providing tentative estimates of the prevalence of contraceptive autonomy overall and its subdomains in our sample of Burkinabè women, we discuss which parts of the proposed methodology worked well, what challenges and limitations we encountered, and we propose next steps for refining, improving, and validating the measurement of contraceptive autonomy.
METHODS
Study Setting
Between April 2018 and July 2018, we carried out a cross-sectional, population-based survey on contraceptive autonomy within two research platforms in Burkina Faso: The Ouagadougou Health and Demographic Surveillance System (Ouaga HDSS) and the Nouna Health and Demographic Surveillance System (Nouna HDSS). These two research platforms are a part of the INDEPTH Network of global HDSSs that collect data from whole communities by defining a catchment area and performing repeated censuses of the population over time (Herbst et al. 2015). The research infrastructure and longitudinal background data that HDSSs provide make them conducive platforms for a range of population health research projects (Sankoh and Byass 2012).
The Ouagadougou HDSS was established in 2008 and is housed within the Institut Supérieur des Sciences de la Population, the advanced demographic research institute of Joseph KI-ZERBO University (then known as the University of Ouagadougou). The research site encompasses five neighborhoods of Burkina Faso’s capital city of Ouagadougou, including two formal neighborhoods (called zones loties, furnished with public services, such as electricity and running water) and three informal periurban neighborhoods (zones non-loties) that lack such services. These neighborhoods are not representative of the capital city as a whole, but do provide information on a wide swath of the city’s population, including both long-established urban families as well as recently arrived rural-to-urban migrants. The city of Ouagadougou is the historical center for the Moaga ethnic group, which is the largest ethnic group in Burkina Faso. While the majority of the Ouaga HDSS is Moaga, widespread internal migration means other ethnic groups are also represented. The Ouaga HDSS collects data on health, demographic, and vital events for approximately 80,000 individuals within their catchment area, with an average periodicity of 6–10 months (Rossier et al. 2012). In addition to these regular censuses, the Ouaga HDSS serves as a platform for a range of special health questionnaires and other studies. A full profile of the Ouaga HDSS can be found in Rossier et al. (2012).
The Nouna HDSS was established in 1992 as a part of the Centre de Recherche en Santé de Nouna, a research center affiliated with the Burkinabè Ministry of Health. The Nouna HDSS includes over 78,000 individuals and encompasses both the town of Nouna (a small administrative center which constitutes approximately 30 percent of the HDSS sampling frame), as well as 58 surrounding rural villages (comprising the remaining 70 percent of the HDSS’ population) (Sié et al. 2010). Located in the northwest of the country close to the border with Mali, the Nouna HDSS is home to members of a range of ethnic groups, including the Dafing, Bwaba, Fulani, and Dioula, among others. The average periodicity of the Nouna HDSS routine census is four months, with additional health and demographic studies conducted more sporadically. A full profile of the Nouna HDSS can be found in Sié et al. (2010). Taken together, the populations of the Nouna and Ouaga HDSSs are not nationally representative of Burkina Faso, but do provide a combined sampling frame with considerable diversity across axes of religion, ethnicity, language, urbanicity, education, and socioeconomic status.
Eligibility and Sampling
We aimed to have a total sample of 4,000 women of reproductive age. Eligibility criteria for inclusion were being a self-reported woman living within one of the two HDSS research platforms, being between15 and 49 years old (inclusive), and being willing and able to provide informed consent. In Nouna, an initial sample of 2,700 women was drawn from the census sampling frame, along with a list of 800 potential replacements. Of the initial sample of 2,700 women in Nouna, 17 refused to participate and 72 were not found. All 94 women were replaced from the contingency list, for a response rate of 96.7 percent in Nouna.
In Ouagadougou, we drew an initial sample of 1,300 women with 700 potential replacements for a total list of 2,000 initial respondents. Due to an error in the sampling process, this initial list included 811 women who were “visitors” to the HDSS catchment area rather than “residents.” These 811 women were thus ineligible for inclusion in the study. Among the 1,189 eligible residents from the initial sampling list, our interviewers were able to locate 879 of them (73.9 percent). In order to reach our intended sample size of 1,300 women, we then drew a second random sample of an additional 500 women from the same initial sampling frame. Of these 500 women, 421 were residents of the HDSS and thus were eligible for inclusion in the study. Our data interviewers were able to locate 415 (98.6 percent) of these women. All of the eligible respondents our interviewers encountered consented to participate. We thus have an overall response rate for the Ouagadougou survey across the two drawings of 80.4 percent. In order to account for the changes we made to the sampling approach, we created individual level-sampling weights based on inverse probability weighting. All analyses presented here use these weighted data.
Survey Tool
Given the novelty of the contraceptive autonomy construct and measurement framework, we employed a wide range of strategies to help inform the development of a novel survey tool. Priorities for our team included that the construct we measured and the survey items we used to measure it would be appropriate and relevant to both the larger family planning community as well as the local Burkinabè context. Measurement of contraceptive autonomy has little precedent in quantitative reproductive health research, so the bulk of survey items were created de novo. In order to create credible survey items with no gold standard and only weak frames of reference, we used an iterative, four-pronged approach to item development that included both emic and etic perceptions of contraceptive autonomy in Burkina Faso (Vijver 2010). These include: (1) an extensive literature review; (2) incorporating findings from an intensive phase of formative, qualitative research; (3) seeking input from other reproductive health experts; and (4) conducting cognitive interviews with the respondent debrief of novel items.
An initial review of the family planning and reproductive health literature in late 2016 revealed a growing body of research and a validated scale to measure reproductive autonomy as conceived of within the context of an intimate partnership (Upadhyay et al. 2014; Grace and Anderson 2016; McCauley et al. 2017). Though essential in its own right, this body of literature was not directly applicable to our conception of contraceptive autonomy which focuses much more on population policies, health systems, and other structural and institutional barriers/facilitators of contraceptive autonomy. We then expanded our search to the broader health literature. While the number of preexisting survey items on this topic we found even outside of reproductive health was small, we were able to find relevant research in two domains of health: inpatient mental health treatment (the MacArthur Admissions Experience Survey in particular), and research on research participation itself (including the Iowa Coercion Questionnaire) (Moser et al. 2004; Lidz 1998; Dugosh et al. 2010; Golay et al. 2017; Gardner et al. 1993). From these two subfields, we drew from psychometrically validated questions and scales, as well as benefited from the theoretical debates that went into their construction. We were then able to borrow and adapt some of these items for our own survey.
A substantial contribution to our survey development came from the analysis of our in-depth formative research, conducted in Burkina Faso during July–August of 2017. This research included 49 in-depth interviews and 17 focus-group discussions with women of reproductive age (15–49) of diverse religions, ethnic groups, marital status, and education levels. Careful analysis of these qualitative data gave us a better understanding not only of how Burkinabè women experience contraceptive autonomy, but of how they conceptualize the topic and the terminology they use to discuss it. Some of the items we were able to include in our survey thanks to insights from the formative work are: (1) Questions specific to the times that Burkinabè women said they were most likely to experience barriers to contraceptive autonomy, such as during the postpartum period; (2) Questions on discontinuation of provider-dependent methods; and (3) Questions on specific scare tactics and other facets of biased family planning counseling.
Once we had a draft of our questionnaire based on the results of our literature review and qualitative findings, we shared it for critique and input with a wide variety of reproductive health experts. Phone interviews as well as in-person consultations were conducted with experts from a wide range of backgrounds, including public health, demography, epidemiology, economics, sociology, and clinical medicine, and included researchers from a range of prominent reproductive health NGOs, universities, family planning program implementers, and donor organizations. They hailed from both the Global North and the Global South, and included several Burkinabè scholars. Feedback and constructive criticism on everything from question order and phrasing to substantive content was received and taken into account, and contributed greatly to the development of the questionnaire.
A revised version of the questionnaire that incorporated expert feedback was then translated into French, Mooré, and Dioula for cognitive interviews. We conducted 15 cognitive interviews with women of reproductive age in one of three study languages, focusing on issues of comprehension, recall, judgment, and response (DeMuro et al. 2012). Cognitive interviews were audio-recorded with respondent consent, and interviewers summarized relevant findings in a dedicated analytic table. We conducted working group meetings among collaborating researchers and data collectors to review the findings and agree on changes to the survey items. The survey was further piloted and amended during interviewer training.
The final survey includes a mix of conventional family planning questions (such as those the Demographic and Health Surveys [DHS] use to measure contraceptive use and unmet need) as well as novel questions that focus on respondents’ experiences with informed choice, full choice, and free choice. The survey consists of six total modules. The second module of the questionnaire includes a series of questions that are asked about each of the 14 methods that appear in the Burkina Faso 2010 DHS,1 with skip logic that depends on the woman’s status as a user/nonuser of that given method. The wording of the questions used to measure the contraceptive autonomy indicator are included in Appendix A.
Interviewer Training and Data Collection
Interviewer training took place over seven days and included didactic sessions on study goals, nonjudgmental interviewing techniques, and research ethics. A challenge of research in the Burkinabè context is that Mooré and Dioula are commonly spoken languages, but the vast majority of people do not read or write in these languages. As such, a formal, standardized written translation of the survey into those languages was not practicable. To address this challenge, we extended our data collector training to focus heavily on standardization, with data collectors and researchers deliberating over the optimal oral translation of all key concepts and phrases into these languages. Four days were spent exclusively on role-playing and practice interviews to promote standardization of language before interviewers began data collection. Training also included three pilot surveys per data collector that were reviewed for feedback and final adjustments before formal data collection began. Data were collected via household survey, during which interviewers visited women at their homes and administered the survey using Android-based tablets. Data collection took place between April and July of 2018. Forty-seven women were incorrectly administered the second module of the survey tool and were excluded from the analytic sample. Comparisons of the demographic characteristics of those 47 women to the remaining full sample showed no major differences between those excluded and those included.
Analytic Approach
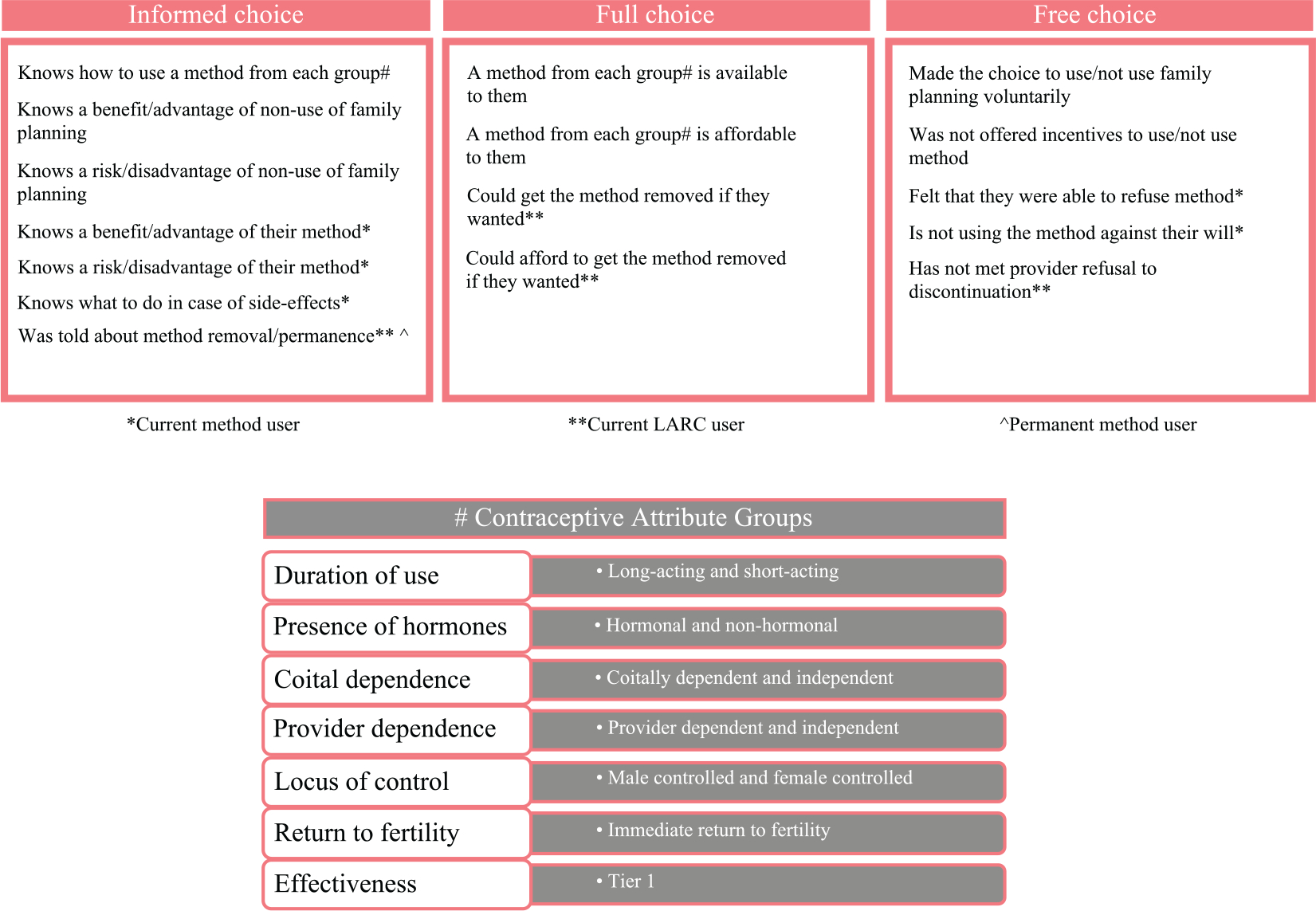
The outcome of interest for this analysis is contraceptive autonomy as described and elaborated in Senderowicz (2020). Contraceptive autonomy is comprised of three subdomains (informed choice, full choice, and free choice), shown in Figure 1. Informed choice is defined as a decision based on sufficient, unbiased information about a range of family planning options. Full choice is defined as a decision made with access to a sufficiently wide range of methods. Free choice is defined as a decision about whether or not to use contraception and what method to use is made voluntarily, without barriers or coercion. Each subdomain contains four to six specific items, with some of the items applying only to specific subpopulations of women (e.g., contraceptive users or users of LARCs). Informed choice captures whether women know how to use a wide range of methods, an advantage and disadvantage of family planning, an advantage and disadvantage of their current method, what to do in case of side effects, and if they were told about the method removal or permanence in the case of provider-dependence or method permanence, respectively. Full choice includes the availability and affordability of a wide mix of contraceptive methods and the availability and affordability of method removal, if applicable. The questions that make up full choice were determined based on the World Health Organization definition of access, which is “the perceptions and experiences of people as to their ease in reaching health services or health facilities in terms of location, time, and ease of approach” (World Health Organization 2021). Free choice requires voluntary family planning use or nonuse, no incentives offered to use or not use a method, the ability to refuse a method, and the ability to get a method removed without refusal. The total algorithm includes 16 items (Figure 2).
FIGURE 1. Components of contraceptive autonomy*.
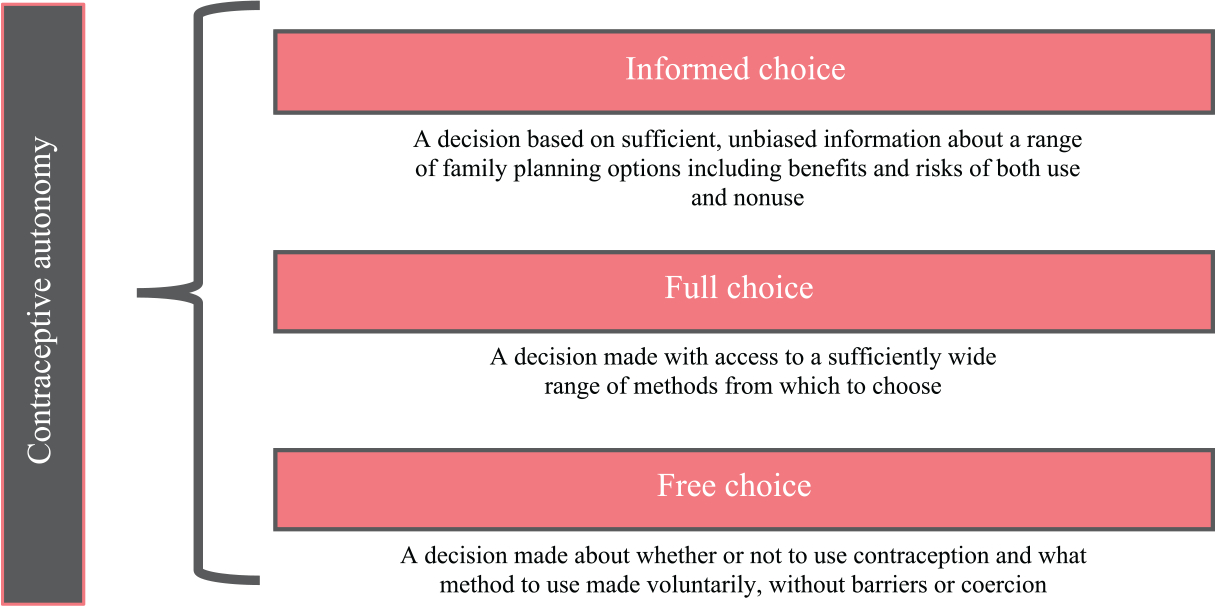
*From Senderowicz (2020). Adapted from Newman and Feldman-Jacobs (2015).
FIGURE 2. Algorithm for operationalizing contraceptive autonomy*.
We apply this algorithm to the data we collected at the Nouna and Ouaga HDSSs in Burkina Faso to pilot this indicator and highlight some key design choices that go into the calculation of this indicator. We discuss our analytic decisions, explaining where and how data issues limited us, as well as higher-level insights about the strengths and limitations of this approach to measurement. In particular, we show two different formulations of bringing together the 16 items into a single contraceptive autonomy score. The first of these is based on an “all or nothing” approach that stipulates that a person must meet all of the criteria relevant to her in order to be said to have contraceptive autonomy. This is based on the idea that autonomy is mutually constitutive, and that the absence of any single item or subdomain obviates the presence of autonomy altogether. This version of autonomy is calculated according to the following formula:
Where is the contraceptive autonomy score for the jth woman and is the answer (0 for no, 1 for yes) the jth women gave to item . The “all or nothing” contraceptive autonomy indicator can be interpreted as the proportion of women who have all subdomains of contraceptive autonomy.
The second formulation we call “shades of gray.” In contrast to the all or nothing approach, shades of gray allows a person’s autonomy score to be decremented for the autonomy components she does not have, but still retain credit for components of autonomy that are present. The “shades of gray” contraceptive autonomy approach can be interpreted as the average proportion of subdomains of contraceptive autonomy a population has. In this case, autonomy is calculated using the following formula:
where is the contraceptive autonomy score for the jth woman and is the answer (0 for no, 1 for yes) the jth women gave to item .
Regardless of the calculation approach, the contraceptive autonomy algorithm was conceived with the intent to be agnostic toward the goodness of contraceptive use, and as such, seeks symmetry in the inclusion of criteria on the advantages and disadvantages of both contraception and nonuse of contraception. However, in our initial analyses, knowledge of a benefit or advantage of nonuse of family planning was far lower than any of the other knowledge-related criteria, leading us to believe that there might have been some confusion about how to answer this question. As a result, we performed a sensitivity analysis, in which we calculate informed choice three times: once including the advantage of family planning nonuse in the algorithm, once removing the advantage of family planning nonuse in the algorithm, and lastly replacing the advantage and disadvantage of family planning nonuse with advantage and disadvantage of family planning in general. For the purposes of subsequent calculations, the informed choice score replacing advantages/disadvantages of family planning nonuse with advantages/disadvantages of family planning overall will be used, with the remaining approaches presented in Table S1.
We calculate descriptive statistics to show the underlying demographic makeup of our sample, the proportion of item-specific results by contraceptive user status, and the proportions of women meeting the criteria for the three subdomains of contraceptive autonomy. If a respondent is missing data for a given component of contraceptive autonomy, her other subdomains of contraceptive autonomy with full data were calculated and included, but the subdomain with missing data and overall contraceptive autonomy score were considered missing. Of note, data on the voluntariness of family planning use were missing for 329 participants, resulting in the missingness of the “free choice” subdomain and the overall contraceptive autonomy indicator. We, therefore, performed a sensitivity analysis to calculate bounds on the “free choice” subdomain and overall contraceptive autonomy, classifying all women with missing voluntariness of family planning use as alternately either voluntarily or not voluntarily using family planning (Tables S2a and b).
Key Variable Definitions and Classifications
Current family planning use can present measurement challenges, as coitally dependent methods (fertility-based awareness methods in particular) may be underreported by standard questions on current use (Fabic and Becker 2017; Dasgupta et al. 2017; Rossier, Senderowicz, and Soura 2013). For the purposes of this analysis, current contraceptive use was measured by prompting about the current use of each of the 14 methods included in the 2010 DHS, as well as use at the last sex. A woman was defined as a current method user if she said she was either a current user, or used the method at the last sex if the last sex took place within the past month (Fabic and Becker 2017).
Classifying contraceptive methods into the contraceptive attribute groups was based on Festin et al.’s (2016) classification scheme with two minor changes (Festin et al. 2016). First, due to some ambiguity around the term “medium-acting” and the fact that this term is not widely used, lactational amenorrhea and injectables were classified as short-acting methods for the purposes of this analysis. Second, we classify IUDs here as a nonhormonal method for this analysis, since copper IUDs were the only widely available form of IUD in Burkina Faso at the time of the survey.
Ethics Approval
This research was reviewed and approved by (1) the Institutional Review Board of the Office of Human Research Administration at the Harvard T.H. Chan School of Public Health in Boston, USA (#IRB17–0511); (2) Le Comité d’Ethique pour la recherche en santé du Ministère de la santé du Burkina Faso in Ouagadougou, Burkina Faso (#2017-5-067); and (3) Le Comité d’Ethique local du Centre de Recherche en Santé de Nouna, in Nouna Burkina Faso (#2017–01). Written informed consent was obtained for all adult participants. For minors, parental informed consent was obtained in addition to assent from the minor.
RESULTS
Our analytic sample includes 3,929 women of reproductive age. The sociodemographic characteristics of these women are shown in Table 1. The mean age of women in our sample was 28.5 years, with women in Ouagadougou being on average slightly older (29.6) than women in Nouna (28.0). Respondents had given birth to an average of 2.6 children (2.1 in Ouagadougou and 2.9 in Nouna). Most women were married (69.1 percent). In Ouagadougou, most women (90.8 percent) were from the Moaga ethnic group, whereas women from Nouna were more ethnically diverse, with 38.2 percent identifying as Dioula, 21.5 percent as Bobo, and 18.0 percent as Bissa. The majority of women in Ouagadougou (52.2 percent) reported at least some secondary education, whereas most women in Nouna (56.4 percent) reported no education. For the mode of transportation (often used as a proxy for household wealth in this context, Moran et al. 2006), the motorbike was the most common mode of transport in Ouagadougou (68.6 percent), while bicycle was the most common mode of transport in Nouna (69.8 percent). Approximately 31 percent of respondents were current users of contraception, with this proportion slightly higher in Ouagadougou (33.2 percent) than Nouna (29.6 percent).
TABLE 1.
Sociodemographic characteristics of respondents
| Ouagadougou n = 1,275 | Nouna n= 2,654 | Overall n = 3,929 | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | |
|
| ||||||
| Age | 29.6 | 0.28 | 28.0 | 0.18 | 28.5 | 0.15 |
| Parity | 2.1 | 0.06 | 2.9 | 0.05 | 2.6 | 0.04 |
|
| ||||||
| n | % | n | % | n | % | |
|
| ||||||
| Married | 846 | 66.3 | 1,868 | 70.4 | 2,714 | 69.1 |
| Ethnicity | ||||||
| Bobo | 8 | 0.6 | 571 | 21.5 | 578 | 14.7 |
| Dioula | 6 | 0.5 | 1,015 | 38.2 | 1,020 | 26.0 |
| Fulfuldé/Peul | 24 | 1.9 | 264 | 9.9 | 287 | 7.3 |
| Gourmantché | 2 | 0.1 | 34 | 1.3 | 35 | 0.9 |
| Gourounsi | 13 | 1.0 | 192 | 7.3 | 205 | 5.2 |
| Moaga | 1,158 | 90.8 | 9 | 0.3 | 1,618 | 29.7 |
| Touareg/Bella | 20 | 1.6 | 0 | 0.0 | 20 | 0.5 |
| Dagara | 16 | 1.3 | 0 | 0.0 | 17 | 0.4 |
| Bissa | 0 | 0.0 | 479 | 18.0 | 479 | 12.2 |
| Other | 30 | 2.4 | 89 | 4.8 | 119 | 3.0 |
| Education | ||||||
| None | 290 | 22.7 | 1,498 | 56.4 | 1,718 | 45.5 |
| At least some primary school | 320 | 25.1 | 646 | 24.3 | 965 | 24.6 |
| At least some secondary school | 666 | 52.2 | 510 | 19.2 | 1,176 | 29.9 |
| Primary mode of transport | ||||||
| Foot | 43 | 3.4 | 570 | 21.5 | 613 | 15.6 |
| Bicycle | 175 | 13.7 | 1,852 | 69.8 | 2,027 | 51.6 |
| Motorcycle | 874 | 68.6 | 216 | 8.1 | 1,090 | 27.7 |
| Car | 127 | 10.0 | 0 | 0.0 | 127 | 3.2 |
| Missing | 56 | 4.4 | 16 | 0.6 | 72 | 1.8 |
| Past contraceptive use | ||||||
| Ever user | 812 | 63.6 | 1,071 | 40.4 | 1,883 | 47.9 |
| Never user | 463 | 36.4 | 1,583 | 59.6 | 2,046 | 52.1 |
| Current contraceptive use a | ||||||
| Any method | 424 | 33.2 | 786 | 29.6 | 1,210 | 30.8 |
| Pill | 70 | 5.4 | 135 | 5.1 | 205 | 5.2 |
| Injectable | 58 | 4.6 | 113 | 4.3 | 171 | 4.4 |
| Implant | 103 | 8.1 | 178 | 6.7 | 281 | 7.2 |
| IUD | 19 | 1.5 | 36 | 1.4 | 55 | 1.4 |
| External condom | 109 | 8.5 | 202 | 7.6 | 311 | 7.9 |
| Calendar method | 80 | 6.3 | 145 | 5.5 | 225 | 5.7 |
| Withdrawal | 7 | 0.5 | 14 | 0.5 | 21 | 0.5 |
| Other | 8 | 0.6 | 16 | 0.6 | 24 | 0.6 |
Some women reported using more than one contraceptive method. All reported method use is included here.
We present results for the 16 individual items and the three subdomains of contraceptive autonomy in Table 2. These are shown for all women, as well as stratified by contraceptive use status and type of method (short-acting vs. long-acting). For informed choice, we present several approaches to measuring symmetry between information about the advantages and disadvantages of family planning. Overall, the proportion of all included women with informed choice was 12.1 percent. Levels of informed choice were lowest among users of short-acting methods (1.4–9.1 percent) and highest among contraceptive nonusers (4.5–28 percent). Only 38.8 percent of women knew how to use a method from each method attribute group. Few women (16.5 percent overall) knew an advantage of nonuse of family planning, ranging from 6.9 percent of LARC users to 19.0 percent of family planning nonusers, yet considerably more women (43 percent overall) knew a disadvantage of family planning nonuse. The proportion of women who knew an advantage of family planning was approximately double the proportion of women who could name a disadvantage of family planning (86.1 percent vs. 43.0 percent). Similarly, nearly double the proportion of contraceptive users could name an advantage of their current method than a disadvantage (83.1 percent vs. 47.7 percent). Less than half of contraceptive users (48.4 percent) knew what to do in case of side effects. Compared to users of short-acting methods, users of long-acting methods were less likely to know a disadvantage of their method (38.9 percent vs. 51.1 percent) but more likely to know what to do in case of side effects (76.0 percent vs. 37.7 percent). Among LARC users, 11.2 percent reported not being told about how to discontinue the method at the time that they acquired it.
TABLE 2.
Contraceptive autonomy: components and subdomains using the all or nothing approach
| All womena | Nonusers | Users (all methods) | Users (short-acting methods) | Users (long-acting methods) | |
|---|---|---|---|---|---|
|
| |||||
| n | 3,929 | 2,719 | 1,210 | 873 | 336 |
| Proportion of sample | 69.2 | 30.8 | 22.2 | 8.6 | |
| Informed choice (%) | |||||
| Knows how to use a method from each group | 38.8 | 35.8 | 45.5 | 39.2 | 62.1 |
| Knows an advantage of family planning | 86.1 | 81.7 | 95.9 | 95.2 | 97.8 |
| Knows a disadvantage of family planning | 43.0 | 41.0 | 47.4 | 49.1 | 42.8 |
| Knows an advantage of her method | · | · | 83.1 | 81.8 | 86.5 |
| Knows a disadvantage of her method | · | · | 47.7 | 51.1 | 38.9 |
| Knows what to do in case of side effects | · | · | 48.4 | 37.7 | 76.0 |
| Told about method removal/permanence | · | · | · | · | 88.8 |
| Overall informed choice | 12.1 | 14.7 | 6.0 | 4.9 | 9.0 |
| Full choice (%) | |||||
| Method from each group is available to her | 69.6 | 69.7 | 69.2 | 70.2 | 66.5 |
| Method from each group is affordable to her | 58.8 | 58.1 | 60.3 | 52.4 | 80.8 |
| Could get method removed if she wanted | · | · | · | · | 83.5 |
| Could afford to get method removed if she wanted | · | · | · | · | 84.0 |
| Overall full choice | 55.2 | 57.3 | 50.3 | 52.0 | 45.9 |
| Free choice (%) | |||||
| nb | 3,600 | 2,390 | 1,210 | 873 | 336 |
| Made the choice to use/not use voluntarily | 95.0 | 94.0 | 97.0 | 95.8 | 100 |
| Not offered incentives to use/not use method | 100 | 100 | 100 | 100 | 100 |
| Did not feel pressured to use method | · | · | 99.7 | 99.6 | 100 |
| Felt she could refuse method | · | · | 96.6 | 96.0 | 98.1 |
| Is not currently using method against her will | · | · | 98.1 | 98.1 | 98.1 |
| Has not been refused discontinuation | · | · | · | · | 97.1 |
| Overall free choice | 94.4 | 94.0 | 95.3 | 95.3 | 95.4 |
| Contraceptive autonomy (%) | |||||
| nb | 3,600 | 2,390 | 1,210 | 873 | 336 |
| 8.1 | 9.6 | 4.7 | 3.9 | 6.7 | |
The contraceptive autonomy indicator is designed such that some subdomains of informed, full, and free choice apply only to some women (i.e., contraceptive users or LARC users). In the “All women” column, data are only presented for subdomains that apply to all women. The overall informed, full, and free choice calculation for all women is calculated by applying the applicable subdomains to one womans contraceptive autonomy score, and presents the proportion of all women who have a given component of contraceptive autonomy or contraceptive autonomy overall.
Data were missing on voluntariness of family planning nonuse for 329 participants. Free choice and full contraceptive autonomy are calculated excluding these participants.
There was less variation in full choice by contraceptive use status compared to informed choice, with levels ranging between 45.9 percent (LARC users) and 57.3 percent (nonusers). Self-reported access to at least one method from each contraceptive attribute group was above 66 percent for all contraceptive use groups, while there was more variation in affordability, which ranged from 52.4 percent for short-acting method users to 80.8 percent for LARC users. 16.5 percent of LARC users reported that they would not be able to get their method removed if they wanted to and 16.0 percent of LARC users would not be able to afford method removal if they wanted to. Among all respondents, the proportion of women with full choice was 55.2 percent.
Levels of free choice were the highest of the three subdomains. 94.4 percent of women surveyed had free choice, with levels ranging from 94.0 percent among contraceptive nonusers to 95.4 percent among LARC users. Ninety-four percent of contraceptive nonusers said they made the choice to not use family planning voluntarily, whereas 95.8 percent of short-acting method users and 100 percent of LARC users said they made the choice to use family planning voluntarily. No women in our sample (0 percent) reported being offered incentives to use or not use family planning methods. A slightly higher proportion of LARC users (98.1 percent) felt they could refuse their method of contraception compared to short-acting method users (96.0 percent). Most family planning users (98.1 percent) were not using their method against their will, with no variation by method type. 2.9 percent of LARC users had previously been refused method discontinuation.
Results from our sensitivity analysis classifying all women with missing data on the voluntariness of family planning as either using/not using family planning voluntarily or using/not using family planning involuntarily found that missing data may have resulted in a slight overestimate of free choice (Tables S2a and b). When all women with missing data for voluntariness of family planning were classified as involuntarily using/not using family planning, 87.0 percent were voluntarily using/not using family planning, 86.5 percent had free choice, and 8 percent had contraceptive autonomy. When women with missingness were classified as voluntarily using family planning, 95.4 percent were voluntarily using/not using family planning and 95.9 percent had free choice, and 8.7 percent had contraceptive autonomy.
When we bring the contraceptive autonomy indicator together using the “all or nothing” approach, we find that 8.1 percent of women in our sample have full contraceptive autonomy, ranging from 9.6 percent of contraceptive nonusers to 3.9 percent of users of short-acting methods, as shown in Figure 3.
FIGURE 3. Contraceptive autonomy by contraceptive status, calculated using the all or nothing approach*.
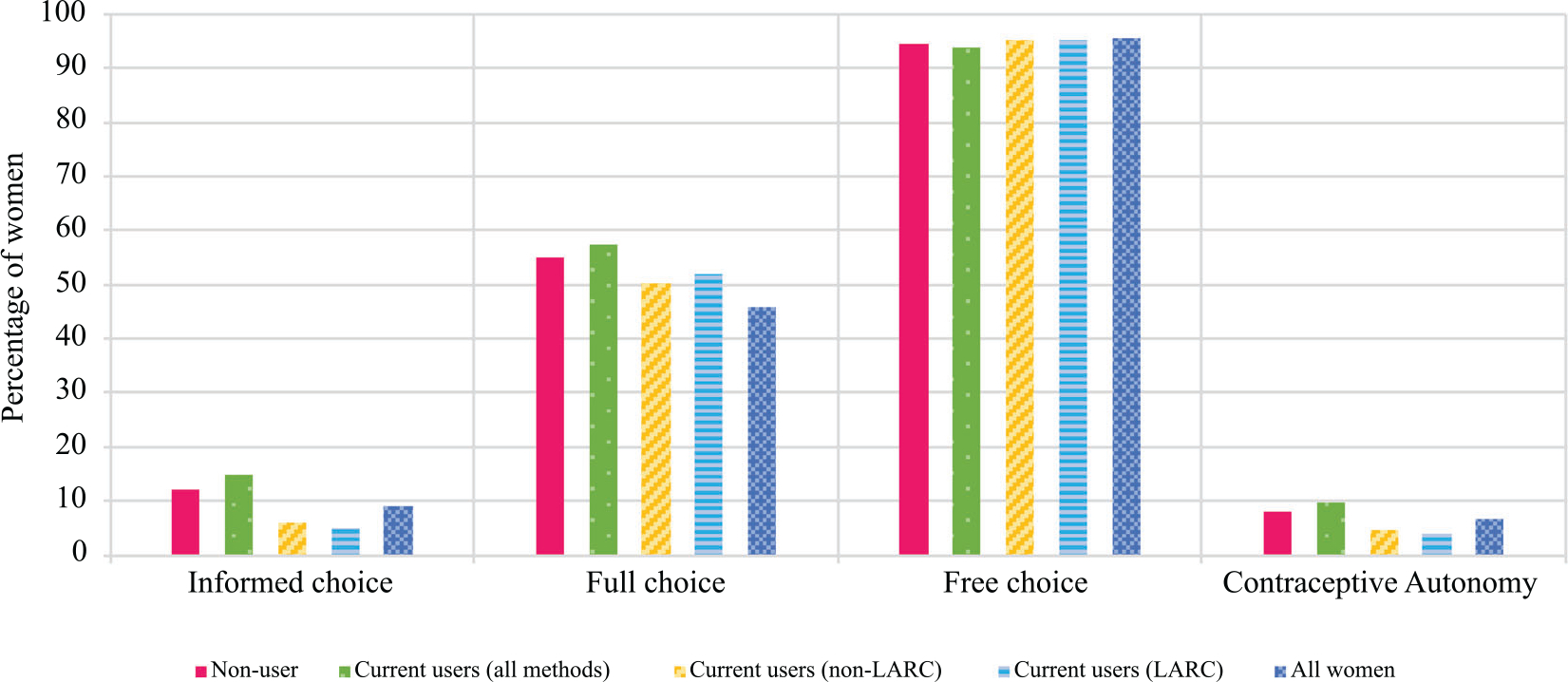
*The all or nothing approach to the contraceptive autonomy score can be interpreted as the proportion of women in a given contraceptive group (nonusers, current users, non-LARC users, LARC users, and all women) who have all components of contraceptive autonomy.
As an alternative to the “all or nothing approach,” we present the “shades of gray” approach to calculating contraceptive autonomy in Table 3 and Figure 4. Women had, on average, 57.6 percent of the components that make up informed choice, 65.1 percent of the components that make up full choice, and 97.4 percent of the components that make up free choice. Similar to the “all or nothing approach,” informed choice was the lowest subdomain and free choice was the highest subdomain. On average, LARC users had the most components of informed, full, and free choice compared to nonusers and short-acting method users. Overall, women in the study had 74 percent of the components that make up the entire contraceptive autonomy indicator, with LARC users on average having the highest percent of components (85.8 percent) and contraceptive nonusers having the lowest percent of components (71.7 percent).
TABLE 3.
Contraceptive autonomy:shades of gray approacha
| All women | Nonusers | Users (all methods) | Users (short-acting methods) | Users (long-acting methods) | |
|---|---|---|---|---|---|
|
| |||||
| Informed choice (%) | 57.6 | 55.2 | 63.1 | 59.1 | 73.7 |
| Full choice (%) | 65.1 | 63.9 | 67.7 | 61.3 | 84.2 |
| Free choice (%) | 97.4 | 97.0 | 98.2 | 97.9 | 98.9 |
| Contraceptive autonomy (%) | 74.0 | 71.7 | 78.4 | 75.6 | 85.8 |
The shades of gray approach of contraceptive autonomy allows partial credit for subdomains of contraceptive autonomy that individuals do have. A given subdomain of contraceptive autonomy (informed choice, full choice, and free choice) is calculated using the shades of gray approach by summing the components of that subdomain for an individual and dividing by the total number of components in that subdomain. Overall contraceptive autonomy is calculated using the shades of gray approach by summing the total number of components of all subdomains for an individual and dividing by the total number of components across all subdomains. The proportions presented here are averages across all women in our study, stratified by contraceptive use and method type.
FIGURE 4. Contraceptive autonomy by contraceptive status, calculated using the shades of gray approach*.
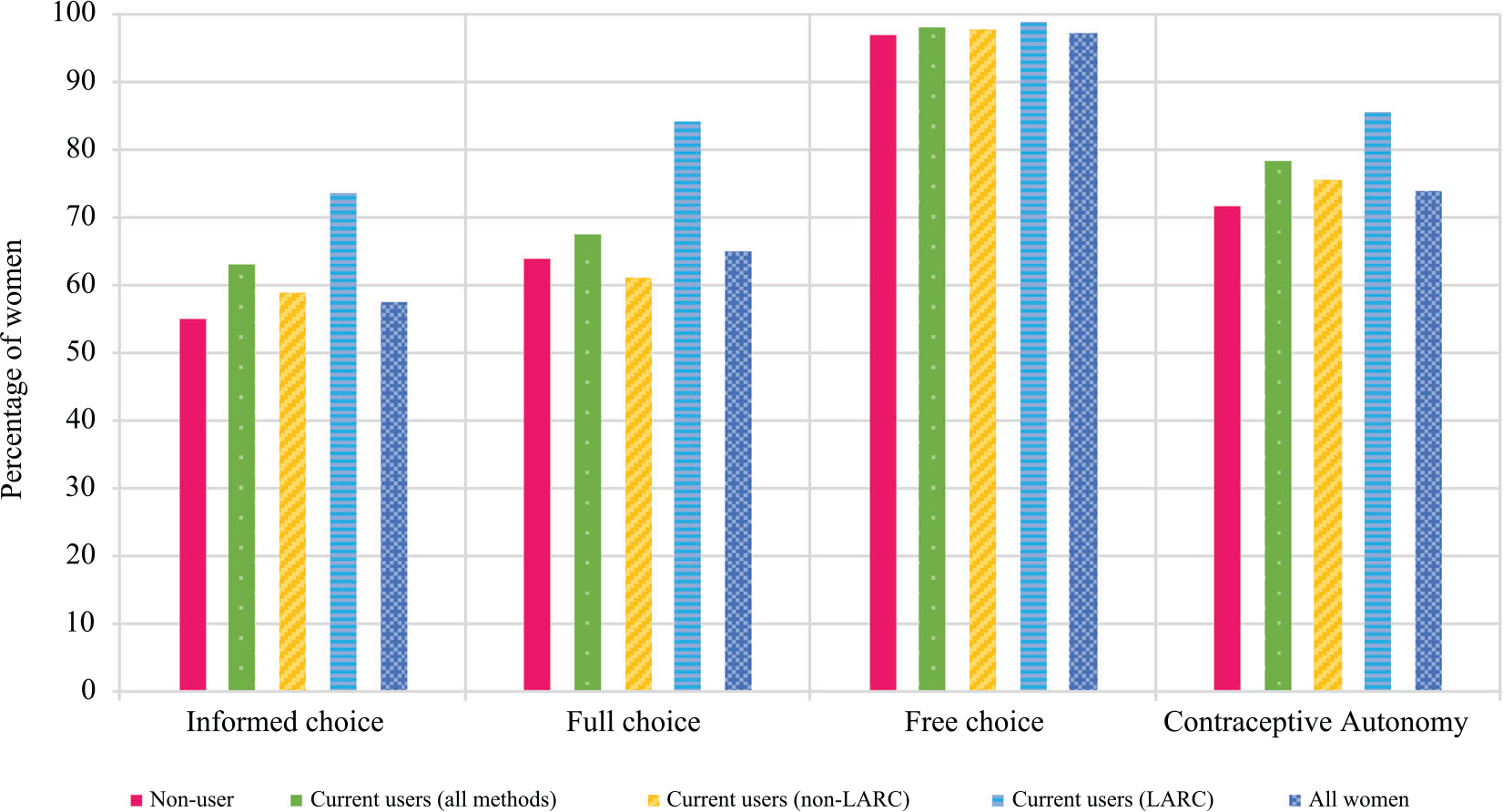
*The shades of gray approach to the contraceptive autonomy score can be interpreted as the average proportion of components of a given subdomain of contraceptive autonomy (informed choice, full choice, and free choice) or overall contraceptive autonomy that women in a contraceptive group (nonusers, current users, non-LARC users, LARC users, and all women) have in our sample.
When disaggregating the “all or nothing” approach by the site (Figure 5), we find that a higher proportion of women in Ouagadougou, the urban site, have contraceptive autonomy (12.6 percent) compared to women in Nouna, the rural site (5.9 percent). Compared to women in Nouna, more women in Ouagadougou have informed choice (16.7 percent vs. 9.8 percent) and free choice (95.7 percent vs. 93.7 percent). Interestingly, the proportion of women with full choice was higher in Nouna (58.1 percent) than Ouagadougou (51.9 percent). Low informed choice in Nouna was driven by fewer women being able to name a disadvantage of family planning use (35.4 percent vs. 58.8 percent in Ouagadougou). The proportion of women who could name an advantage at the two sites was similar (85.4 percent in Nouna and 87.3 percent in Ouagadougou), indicating that contraceptive counseling may be more asymmetrical in the rural setting, with providers emphasizing potential benefits of family planning and leaving out potential disadvantages.
FIGURE 5. Contraceptive autonomy by site using the all or nothing approach*.
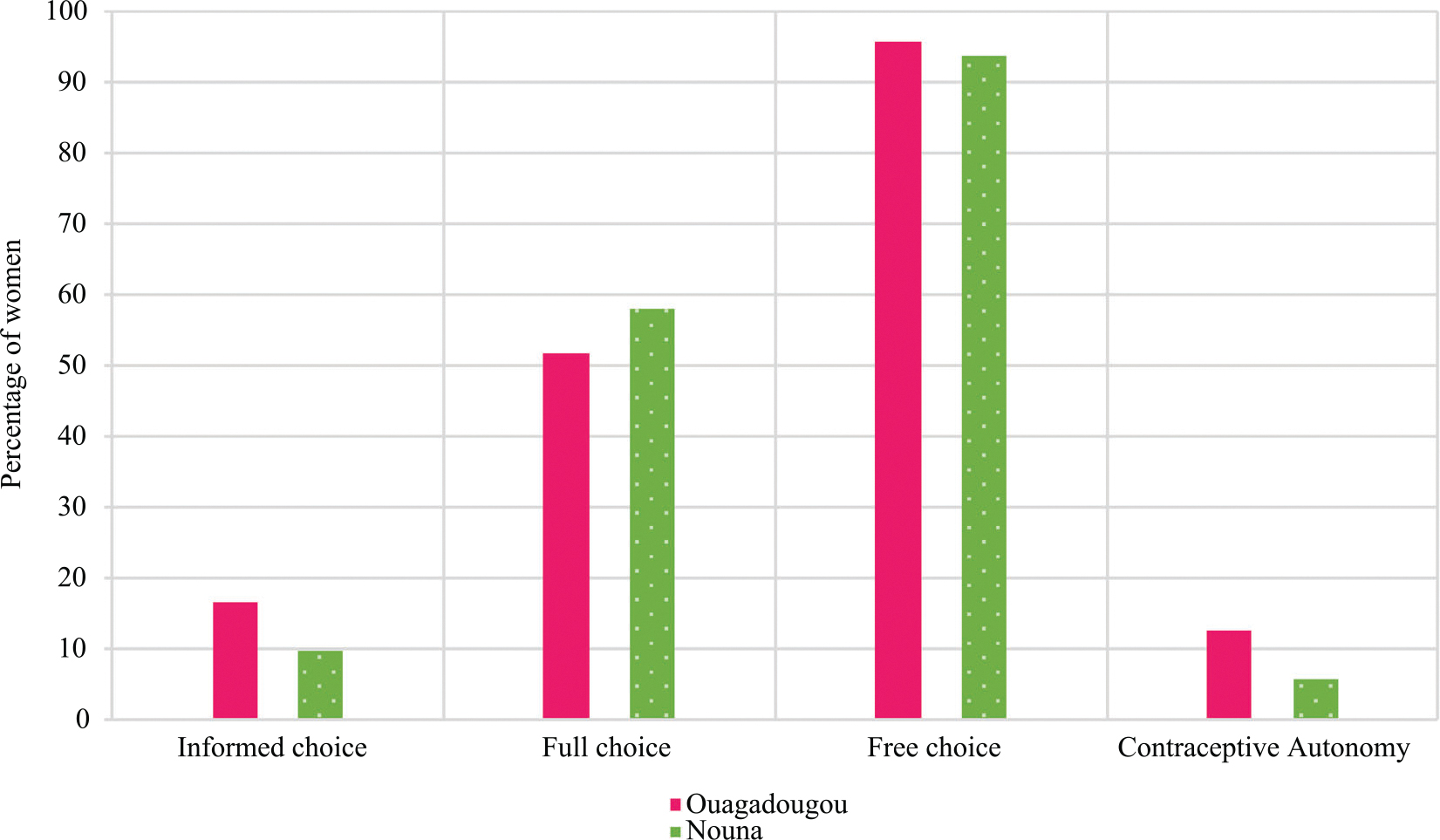
*The all or nothing approach to the contraceptive autonomy score can be interpreted as the proportion of women in a given contraceptive group (nonusers, current users, non-LARC users, LARC users, and all women) who have all components of contraceptive autonomy.
DISCUSSION
Measuring a novel indicator of contraceptive autonomy for the first time, we demonstrated that informed, full, and free choice can be captured at the population level. Within two Health and Demographic Surveillance Systems in Burkina Faso, we generated estimates of informed choice, full choice, and free choice, as well as overall contraceptive autonomy. The insights gained from these estimates allow us to assess some of the strengths and limitations of this measurement approach, exploring both the successes as well as areas where further refinement is needed.
Contraceptive Autonomy Estimates in the Ouagadougou and Nouna Health and Demographic Surveillance Systems
Overall proportions of contraceptive autonomy are low across all groups, but vary considerably based on the analytic approach used to calculate them. Overall, 8 percent of women in our sample had contraceptive autonomy using the “all or nothing” approach. Based on the “shades of gray” approach, on average, women had 74 percent of the subdomains that make up contraceptive autonomy. The low level of the “all or nothing” autonomy score seems particularly notable given that none of the criteria included in the autonomy indicator is aspirational.
The biggest contributor to reduced contraceptive autonomy among the women in our sample was the lack of informed choice, driven by a lack of information about how to use a method from each contraceptive attribute group, as well as a marked asymmetry between knowledge of the advantages and the disadvantages of family planning. We attempt to assess potential biases in contraceptive knowledge by examining patterns of imbalance among some of the complementary/symmetrical items (e.g., an item about knowing the benefits/advantages of the current method followed by an item on knowing the risks/disadvantages of the current method). This asymmetry was observed both among all women when asked about their knowledge of family planning generally, as well as among current contraceptive users when asked about their knowledge of a benefit and disadvantage of their current method. Among LARC users, in particular, over 86 percent said they could name an advantage of their method, while less than half that proportion (39 percent) said they could name a disadvantage.
The proportion of women who said they did not know an advantage of nonuse was so large that this criterion was dropped from the informed choice calculations for subsequent analyses, lest this single question drives too much of the overall contraceptive autonomy results on its own and obscure important variation elsewhere. Even without this item on the benefits of nonuse, there does appear to be a pattern of bias that emphasizes the positive aspects of contraception and deemphasizes the negative. These findings on low levels of informed choice are concordant with biased or directive approaches to family planning counseling, and are supported by much of the quality of care literature in family planning showing balanced counseling to be a widespread challenge (Machiyama and Cleland 2014; Wambui, Ek, and Alehagen 2009; Senderowicz 2015; Rossier and Hellen 2014; Holt et al. 2018). Previous qualitative research on family planning quality from Ouagadougou found that providers are sometimes reluctant to discuss side effects with their patients out of fear that doing so would cause psychosomatic manifestations of side effects and lead to contraceptive discontinuation (Senderowicz 2015).
Over two-thirds of women across contraceptive use statuses reported the availability of at least one method from each of the seven contraceptive attribute groups. Affordability of a broad contraceptive method mix appears to be a greater barrier among our respondents, with over 40 percent of all respondents reporting that they do not think that a method from each attribute group would be available to them. Though considerably more LARC users than short-acting method users reported financial access to a broad contraceptive method mix, LARC users showed the lowest levels of full choice overall, due to a substantial percentage of current LARC users who reported that they did not believe they would be able to get their method removed if they wanted to. These findings for full choice echo the results from the informed choice questions, showing an asymmetry between perceived ease of access to LARC insertion versus ease of LARC removal.
The level of free choice in this sample was the highest of the three subcomponents of contraceptive autonomy. Overall, 94 percent of women said that their current contraceptive status (either as a contraceptive user or nonuser) was a voluntary one, with this number lower among nonusers (94 percent) than users (97 percent). Understanding and measuring both upward and downward barriers to autonomy is essential to the contraceptive autonomy indicator, which seeks a broad understanding of threats to autonomy that can manifest either to keep a person from using a wanted method, or to impose an unwanted method on a woman who wishes not to use one, consistent with Senderowicz’s (2019) conception of autonomy as bidirectional. That 6 percent of nonusers say their choice not to use was made involuntarily suggests that Burkina Faso has made tremendous progress in recent years in expanding access to family planning service, although certainly barriers still remain.
The choice to include the offer of incentives as an item in the free choice domain was made not because there was any reason to suspect that incentives are used in Burkina Faso, but rather, because the longer-term goal of this indicator is to be piloted in other settings and eventually scaled-up for use internationally. Since there are many countries that do use incentives to drive family planning uptake, we decided to test this concept in Burkina Faso, but the results that no women were offered incentives are in line with expectations.
Our finding that 2.9 percent of LARC users have tried unsuccessfully to have their method removed is slightly lower than other estimates from Burkina Faso, which have found that 4.5 percent of women had tried and failed to remove their method in the last 12 months (PMA2020 2018). A total of 3 percent of contraceptive users lacked free choice in our sample, either because they felt they could not refuse their current method, were currently using their method against their will, or made the choice to use contraception involuntarily. This number may seem low, especially in comparison to the higher gaps in informed choice and full choice. However, any proportion greater than zero presents a cause for concern, given how anathema even a single violation of free choice is to the principles of voluntary family planning.
Levels of informed choice, full choice, and contraceptive autonomy overall are higher among nonusers of contraception compared to users. This may be influenced by the way the algorithm is constructed, which by definition applies more criteria to contraceptive users than to nonusers, and to LARC users than non-LARC users. But the fact that current nonusers have higher levels of free choice than users shows that this need not always be the case. We view the additional criteria that are applied to method users and LARC users not as holding these groups to a higher standard than nonusers, but rather, as adding relevant criteria as applicable. As such, we would not expect to always observe a simple mechanistic relationship in which nonusers have higher autonomy scores than their counterparts who use contraceptive methods in general or LARC methods in particular, and indeed, we do not find that to be the case here.
Levels of informed choice, full choice, and free choice are, as expected, lower using the “all or nothing” approach to calculation compared to the “shades of gray” approach, though much of this is due to differences in the definitions behind the two approaches. Among all respondents, the overall level of contraceptive autonomy using the shades of gray approach was 74 percent, compared to 8 percent using the all or nothing approach. We caution against the direct comparison of the two approaches given their varying interpretations; the “all or nothing” approach is the proportion of women with all subdomains of contraceptive autonomy, whereas the “shades of gray” approach is the proportion of subdomains of contraceptive autonomy women in our sample had on average. When proposing these two approaches to measurement, Senderowicz discussed some of the tradeoffs involved in the irrespective strategies, noting that “The ‘all or nothing’ approach is stricter in its adherence to the conceptual underpinnings of the indicator, and thus, perhaps a truer measurement of contraceptive autonomy than the shades of gray model.” However, this clarity comes at the cost of sensitivity to change, as the “all or nothing” approach may fail to reflect important but incomplete improvements in autonomy (Senderowicz 2020). This assumption has indeed been borne out in the results, which show that the all or nothing model provides a starker assessment of a family planning program’s overall successes and failures than the shades of gray model, while the latter will be more sensitive to small changes over time. That sensitivity to change, however, comes at the price of a sort of conceptual haziness and less interpretable result. Future work might consider a weighting scheme for the final survey items depending on their relative gravity(Senderowicz 2020).
Strengths of this study design include the four-pronged approach to new item development, rigorous item pretesting, and a large random sample of women of reproductive age taken from a well-established sampling frame. There are, however, several important limitations to our data collection. As with all survey-based research on reproductive health, visiting women in their homes to ask about sensitive topics, such as contraception, may result in social desirability bias. Because many of our questions for contraceptive users focused on the woman’s most recent experience with a provider, we may be missing many experiences of non-autonomy that happened prior to that visit. This approach also introduces the possibility of recall bias, as an implant user, for example, may be reporting an experience that happened more than four years ago. Since we introduce many new items, there remains the possibility that respondents are not interpreting our questions how we intended them, even after our cognitive interview testing. Because of the challenges with written local languages in this setting, the questionnaire may not have been translated the exact same way every time, and the same question may have been posed differently to different women despite our best attempts at standardization. Finally, these two HDSSs are not representative of the country of Burkina Faso and so generalizability outside of this study context is limited.
Appraising the Measurement Approach
In this first attempt at measuring the contraceptive autonomy indicator, we assessed informed choice, full choice and free choice among reproductive-aged women at two sites in Burkina Faso. We attempted to capture elements of contraceptive decision-making and quality of care that are commonly referenced in family planning research but often not directly measured at the population level. Our attempts to quantify contraceptive knowledge, access, and voluntariness were met with varying success. We believe, for example, that our measures of contraceptive access in the full choice subdomain, created by assessing the availability and affordability of methods broken into “contraceptive attribute groups,” represent a step forward in quantitatively capturing whether women can access an adequate mix of contraceptive methods. While many studies have previously attempted to quantify access, they are often limited by data that measure access to contraception only indirectly (Machiyama and Cleland 2014; Choi, Fabic, and Adetunji 2016; Senderowicz and Maloney 2022). Given that lack of access to contraceptives is a large driver of global family planning programs, a direct, population-level measure of access to a wide range of methods is very much needed. Additional research comparing population-level measures of perceived access and facility-level measures of access is an important next step.
In contrast to most of the commonly used indicators in family planning research, we made no assumptions about respondents’ desire or “need” for contraceptive use. Rather, we attempted to assess whether decisions to use or not use family planning were made autonomously, with enough information, access, and freedom to make a choice about their reproductive lives. Understanding women’s experiences with contraception from their own perspective by asking them directly about their interactions and desires and trusting their answers is a driving principle of contraceptive autonomy, and is necessary to promote reproductive justice. We note that the definition and measurement of contraceptive autonomy employed here do not include any normative assumptions about the desirability of sole or joint contraceptive decision-making. The measurement approach tested here seeks to assess whether or not the use/nonuse of a contraceptive method is voluntary and free from coercion, but has no items assessing whether those decisions are made individually or jointly (see Appendix A). A decision made jointly with a provider, partner, or other confident would not be decremented or penalized in any way by this measurement, as long as the respondent did not consider this decision to be an involuntary one.
In addition to noting these successes, we also encountered some thorny and unresolved measurement challenges in our attempt to measure contraceptive autonomy. For example, to build symmetry into our measurement of informed choice, we asked women about both advantages and disadvantages of contraceptive nonuse, with only 16.5 percent of women able to name an advantage. While this low proportion may be a reflection of asymmetry in family planning knowledge, it may also be an indication that the question itself was difficult to answer. Similarly, we are less confident in our measure of knowledge of various family planning methods. While we emphasize the importance of measuring knowledge about a wide swath of methods, asking women if they know how to use each method certainly does not capture all relevant dimensions of knowledge.
Another challenge to our measurement of informed choice is that we were unable to evaluate the content of contraceptive knowledge. While our algorithm directly assesses many components of the informed choice definition (such as knowledge of benefits, side effects, and risks of contraception), it does not directly measure others, like the completeness, accuracy, or unbiased nature of the information. A population-based survey tool is not a particularly apt methodological tool for capturing and scrutinizing the accuracy of the contraceptive knowledge of thousands of respondents. Yet, failing to do so may result in overestimates of informed choice and contraceptive autonomy as a whole, especially given evidence that women often receive incomplete, inaccurate, and biased contraceptive counseling (Senderowicz et al. 2021; Senderowicz 2019; Britton et al. 2021; Tumlinson, Okigbo, and Speizer 2015; Towriss et al. 2019; Manzer and Bell 2021; Yirgu et al. 2020; Sieverding et al. 2018). Improvement and reassessment of the informed choice questions would greatly benefit the overall measurement of contraceptive autonomy.
We also express uncertainty in our measures of free choice, and particularly in the survey items related to experiences of pressure to use family planning or other forms of nonautonomy. Previous research on free choice has found nonautonomous experiences to fall along a spectrum, with many forms of provider pressure to use/not use a contraceptive method taking very subtle forms (Senderowicz 2019). Other research has found that even overt instances of provider pressures and nonautonomy can be normalized within a society to the extent that respondents may not always consider them a problem (Senderowicz et al. 2022; Freedman and Kruk 2014). Though we capture some cases of nonautonomy among those without free choice, subtle experiences of pressure or involuntariness likely are not captured with our survey questions, especially given social desirability bias and the perhaps subjective interpretation of what it means for something to be “voluntary” or for someone to feel “pressured.” Measuring violations of free choice at the population-level is imperative to guide family planning policy and programming and so this remains an important area for considerable future formative research, item development, and measurement validation. Additional work is also needed to explore the provenance of the pressure women may feel, and perhaps refine question-wording to focus more specifically on interactions with providers, as a way to ensure that the indicator is driven primarily by things that the health center can control, rather than larger cultural forces and tendencies.
There is an important area of lingering tension for the measurement of contraceptive autonomy between a positivist approach to quantification (based on the pursuit and understanding of an objective and measurable third-party understanding of truth) and a more wholly person-centered approach (based on the respondent’s own understanding of their lived experiences). The approach we pilot here stands somewhere in between these two poles, seeking to find a happy medium between them. With the method of measuring contraceptive autonomy tested here, we as researchers are setting the bar for informed, full, and free choice, and then using these researcher-defined criteria to assess whether a respondent has contraceptive autonomy. We have, however, integrated a person-centered perspective in many regards, for example, relying on the respondent’s own perceptions and understandings of the availability and affordability of different contraceptive methods, rather than seeking to verify the presence and price of those contraceptive commodities at a nearby health facility. This approach has the benefit of giving priority to respondent’s own voices and understandings of their access to contraception. But this approach also has the limitation of reflecting back to us only this respondents’ understanding, rather than a third-party verification of access that may be more accurate or objective in a positivist sense. Meanwhile, a more wholly person-centered approach might simply involve asking a respondent whether they have contraceptive autonomy (and/or its subdomains), and trusting their perception of their knowledge, access, and freedom necessary for autonomous decision-making without imposing criteria that may not align with the respondents’ values. Future research exploring the extent to which people’s perception of their own informed, full, and free choices varies from our assigned values will provide further insights into the impact of these measurement decisions.
We also note here that contraceptive autonomy is but one small subset of the broader concept of reproductive autonomy, which we have defined elsewhere as “individuals’ ability to be fully empowered agents in their reproductive needs and decisions and to access reproductive health services without interference or coercion” (Senderowicz and Higgins 2020). Reproductive autonomy includes everything from abortion rights to birth justice to reproductive coercion stemming from intimate partners (Upadhyay et al. 2014; Grace and Anderson 2016; Luna and Luker 2013; Kimport 2021). Since no single measure can capture everything, the present measurement approach has been limited to contraceptive decision-making, with a specific focus on modifiable health system factors. Other work has focused on developing validated scales of reproductive autonomy within the intimate partnership and other contexts, and it would be of interest for future research to explore the relationships between these (and other) different domains of reproductive autonomy and their respective measurements (Upadhyay et al. 2014; Sudhinaraset et al. 2018; Rominski et al. 2014; Moreau et al. 2020).
The population-based survey methodology used by us here and by most major reproductive health surveys does not allow us to gain any insight into contraceptive service interactions from the providers’ perspectives. Future work collecting data from the provider perspective focusing on clinical insights as well as their experiences navigating various pressures and incentives within the health system would be valuable to our understanding of how to understand and measure contraceptive autonomy.
There are also methodological limitations to the type of composite indicator that we test here. Composite indicators aim to simplify complex phenomena into digestible metrics that are more easily interpretable by policymakers, program designers, and even other researchers. In condensing such complexity into a single nugget of information, what is gained in digestibility is often lost in nuance. Critics of composite indicators have argued that the threats to the validity of composite indicators are numerous, including a lack of transparency of what goes into the calculation of the metric, as well as challenges to appropriately combining individual measures into the larger composite (Barclay, Dixon-Woods, and Lyratzopoulos 2019; Greco et al. 2019). Acknowledging these and other pitfalls for composite indicators, careful consideration of how to bring together the contraceptive autonomy indicator is warranted, and any future attempts to add weights to items or make other changes to the methodology should be made as transparently as possible. Fortunately, because the indicator is comprised of 4–6 individual items per each of the three subdomains, in this case it remains feasible to present each domain or even each individual survey item separately, in addition to the composite metric, as we do here.
The next steps for the development and refinement of the contraceptive autonomy indicator also include psychometric methods for more formal measurement validity testing. Future development of the “shades of gray” approach should focus on the advantages and drawbacks of applying weights to the algorithm items according to their relative importance. In addition to testing the a priori algorithm for calculating contraceptive autonomy proposed in Senderowicz (2020), it will be helpful to use a range of multidimensional latent variable modeling techniques to test the dozens of novel survey items piloted in the Ouagadougou and Nouna Health and Demographic Surveillance Systems as part of the Contraceptive Autonomy Study. This might involve using tools, such as multidimensional item response theory, multiple indicator, multiple cause models, and other psychometric approaches that allow contraceptive autonomy to be modeled as a multidimensional, formative indicator (Fleuren et al. 2018; Irwing, Booth, and Hughes 2018; Linley et al. 2009). Modeling contraceptive autonomy as a formative multidimensional indicator is important, since the construct violates the assumption of unidimensionality on which many standard psychometric approaches rely. There may be many plausible situations, for example, in which a person may experience informed choice and full choice but not free choice, or be missing some portions of informed choice but not others. These multidimensional latent variable modeling approaches will help identify the questions that best assess the latent autonomy construct, as well as generate evidence of measurement validity. Once this evidence is generated in Burkina Faso, evidence for scale-up may be generated through additional qualitative and psychometric testing in other settings to enable evidence of cross-cultural equivalence and broader validity across a range of contexts (Frongillo et al. 2019; Coates et al. 2006).
CONCLUSION
This paper measures a novel indicator of contraceptive autonomy for the first time and highlights some of the challenges of this approach to measurement, some of the main decisions that have gone into the final calculation, and some of the key findings from this experience. This analysis represents the first attempt to quantify contraceptive autonomy at the population level, and provides useful insights into this measurement approach to inform future research. This attempt at measuring contraceptive autonomy provided some important preliminary data points on informed, full, and free choice in Burkina Faso, and also revealed many areas for improvement and avenues for future research. Overall, we found that limits to informed choice were the key drivers of lower contraceptive autonomy among these groups. Information about the benefits/advantages of contraception and access to method provision are consistently higher than information about the disadvantages/risks of contraception and access to method removal. This pattern is suggestive of a lack of complete and unbiased information about family planning, and highlights the importance of increased access to method removal, as a significant scale-up in implants and IUDs has been planned by the Burkinabè Ministry of Health (Ministry of Health of Burkina Faso 2017).
Rather than viewing the measurement approach assessed here as a final tool ready to be scaled up, we view this as an important step on a longer road toward a more rights-based and person-centered measurement agenda for the global family planning community. We caution that, even with considerable more development, some of the key elements of contraceptive autonomy may never be able to be measured well at the population level, since this survey approach necessarily limits our data to what our respondents know, and what they choose to share. This acknowledgment, however, should not be a deterrent to those seeking to address the vital need for new family planning indicators that measure people’s own desires and trust them to be the experts on their own lives. A radical shift in our measurement agenda away from fertility and contraceptive uptake to focusing on people’s access to a wanted method and respect for their contraceptive decisions is essential to move the global family planning field toward reproductive justice.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to gratefully acknowledge the feedback from Dr. Maggie McConnell, Dr. Jocelyn Viterna, and Dr. Joshua Salomon on earlier versions of this work. We would also like to thank the many reproductive health experts who shared freely of their time and knowledge to provide feedback on the development of our survey tool. We thank the research assistants and interviewers who worked tirelessly to collect the data for this analysis. And finally, we gratefully acknowledge the time and generosity the respondents who answered our survey questions.
FUNDING
This work was supported by the David and Lucile Packard Foundation under grant #2016-64774 and the Society of Family Planning Research Fund under grant #11-13.
LS’s contribution was supported by a Ruth L Kirschstein National Research Service Award (T32 HD049302) and a Population Research Infrastructure grant (P2C HD047873). BWB’s contribution was supported by a National Research Service Award (T32HD52468) and a Population Infrastructure grant (P2CHD050924). The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) awarded these grants. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NICHD. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
PERMISSION TO REPRODUCE MATERIALS FROM OTHER SOURCES
We have made new figures, but essentially replicate the figures Senderowicz previously published in this same journal. Please advise if any additional formalities are necessary.
These 14 methods are: oral contraceptive pills, injectable contraceptives, subdermal implants, intrauterine devices, external condoms, internal condoms, the rhythm/calendar method, emergency contraception, the lactational amenorrhea, the Standard Days Method, spermicide, withdrawal, the diaphragm, and female sterilization.
Contributor Information
Leigh Senderowicz, Department of Gender and Women’s Studies, University of Wisconsin-Madison, Madison, WI, USA.; Department of Obstetrics and Gynecology, University of Wisconsin-Madison, Madison, WI, USA. Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, MA, USA
Brooke W. Bullington, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA. Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Nathalie Sawadogo, Institut Supérieur des Sciences de la Population, Université Joseph Ki-ZERBO, Ouagadougou, Burkina Faso.
Katherine Tumlinson, Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.; Department of Maternal and Child Health, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Ana Langer, Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, MA, USA..
Abdramane Soura, Institut Supérieur des Sciences de la Population, Université Joseph Ki-ZERBO, Ouagadougou, Burkina Faso..
Pascal Zabré, Centre de Recherche en Santé de Nouna, Nouna, Burkina Faso..
Ali Sié, Centre de Recherche en Santé de Nouna, Nouna, Burkina Faso..
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are not openly available due to the terms of our ethics approval. Data may be made available by the corresponding author on a case-by-case basis upon reasonable request and ethical clearance.
REFERENCES
- Ashford Lori S. 2014. “What Was Cairo? The Promise and Reality of ICPD.” Population Reference Bureau Resource Library. [Google Scholar]
- Barclay Matthew, Dixon-Woods Mary, and Lyratzopoulos Georgios. 2019. “The Problem with Composite Indicators.” BMJ Quality & Safety 28(4): 338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton Laura E., Williams Caitlin R., Onyango Dickens, Wambua Debborah, and Tumlinson Katherine. 2021. “‘When It Comes to Time of Removal, Nothing Is Straightforward’: A Qualitative Study of Experiences with Barriers to Removal of Long-Acting Reversible Contraception in Western Kenya.” Contraception: X 3: 100063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill Niamh, Sonneveldt Emily, Stover John, Weinberger Michelle, Williamson Jessica, Wei Chuchu, Brown Win, and Alkema Leontine. 2018. “Modern Contraceptive Use, Unmet Need, and Demand Satisfied among Women of Reproductive Age Who Are Married or in a Union in the Focus Countries of the Family Planning 2020 Initiative: A Systematic Analysis Using the Family Planning Estimation Tool.” Lancet 391(10123): 870–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan Rebecca, Lebetkin Elena, Brennan Claire, Kuffour Emmanuel, Boateng Angela, Tagoe Samuel, Coolen Anne, Chen Mario, Aboagye Patrick, and Brunie Aurélie. 2020. “What Goes in Must Come Out: A Mixed-Method Study of Access to Contraceptive Implant Removal Services in Ghana.” Global Health: Science and Practice 8(2): 220–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Yoonjoung, Fabic Madeleine Short, and Adetunji Jacob. 2016. “Measuring Access to Family Planning: Conceptual Frameworks and DHS Data.” Studies in Family Planning 47(2): 145–161. [DOI] [PubMed] [Google Scholar]
- Cleland John, Ndugwa Robert, and Zulu Eliya. 2011. “Family Planning in Sub-Saharan Africa: Progress or Stagnation?” Bulletin of the World Health Organization 89(2): 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates Jennifer, Edward A Frongillo Beatrice Lorge Rogers, Webb Patrick, Wilde Parke E, and Houser Robert. 2006. “Commonalities in the Experience of Household Food Insecurity across Cultures: What Are Measures Missing?” Journal of Nutrition 136(5): 1438S–1448S. [DOI] [PubMed] [Google Scholar]
- Connelly Matthew James. 2008. Fatal Misconception: The Struggle to Control World Population. Belknap Press of Harvard University Press. [Google Scholar]
- Coulibaly Abou, Millogo Tieba, Baguiya Adama, Nguyen Toan Tran Blandine Thieba, Seuc Armando, Asa Cuzin-Kihl Sihem Landoulsi, Kiarie James, Yodi Rachel, Mashinda Désiré, and Kouanda Séni. 2021. “Time to Long-Acting Reversible Contraceptive Uptake Over Twelve Months Postpartum: Findings of the Yam Daabo Cluster Randomized-Controlled Trial in Burkina Faso and the Democratic Republic of the Congo.”Open Access Journal of Contraception 12: 73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta Aisha, Weinberger Michelle, Bellows Ben, and Brown Win. 2017. “New Users Are Confusing Our Counting: Reaching Consensus on How to Measure Additional Users of Family Planning.” Global Health: Science and Practice 5(1): 6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMuro Carla J, Lewis Sandra A, DiBenedetti Dana B, Price Mark A, and Fehnel Sheri E. 2012. “Successful Implementation of Cognitive Interviews in Special Populations.” Expert Review of Pharmacoeconomics & Outcomes Research 12(2): 181–187. [DOI] [PubMed] [Google Scholar]
- Dugosh Karen Leggett, Festinger David S, Croft Jason R, and Marlowe Douglas B. 2010. “Measuring Coercion to Participate in Research within a Doubly Vulnerable Population: Initial Development of the Coercion Assessment Scale.” Journal of Empirical Research on Human Research Ethics 5(1): 93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabic Madeleine Short, and Becker Stan. 2017. “Measuring Contraceptive Prevalence among Women Who Are at Risk of Pregnancy.” Contraception 96(3): 183–188. [DOI] [PubMed] [Google Scholar]
- Festin Mario Philip R, Kiarie James, Solo Julie, Spieler Jeffrey, Malarcher Shawn, Van Look Paul F A, and Temmerman Marleen. 2016. “Moving Towards the Goals of FP2020 - Classifying Contraceptives.” Contraception 94(4): 289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleuren Bram P. I., van Amelsvoort Ludovic G. P. M., Zijlstra Fred R. H., de Grip Andries, and Kant IJmert. 2018. “Handling the Reflective-Formative Measurement Conundrum: A Practical Illustration Based on Sustainable Employability.” Journal of Clinical Epidemiology 103(November): 71–81. [DOI] [PubMed] [Google Scholar]
- Freedman Lynn P., and Kruk Margaret E.. 2014. “Disrespect and Abuse of Women in Childbirth: Challenging the Global Quality and Accountability Agendas.” Lancet 384(9948): e42–e44. [DOI] [PubMed] [Google Scholar]
- Frongillo Edward A., Baranowski Tom, Subar Amy F., Tooze Janet A., and Kirkpatrick Sharon I.. 2019. “Establishing Validity and Cross-Context Equivalence of Measures and Indicators.” Journal of the Academy of Nutrition and Dietetics 119(11): 1817–1830. [DOI] [PubMed] [Google Scholar]
- Fruhauf Timothee, Zimmerman Linnea, Kibira Simon Peter Sebina, Makumbi Fredrick, Gichangi Peter, Shiferaw Solomon, Seme Assefa, Guiella Georges, and Tsui Amy. 2018. “Measuring Family Planning Quality and Its Link with Contraceptive Use in Public Facilities in Burkina Faso, Ethiopia, Kenya and Uganda.” Health Policy and Planning 33(7): 828–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner William, Hoge Steven K., Bennett Nancy, Roth Loren H., Lidz Charles W., Monahan John, and Mulvey Edward P.. 1993. “Two Scales for Measuring Patients’ Perceptions for Coercion During Mental Hospital Admission.” Behavioral Sciences & the Law 11(3): 307–321. [DOI] [PubMed] [Google Scholar]
- Golay Philippe, Semlali Imane, Beuchat Hélène, Pomini Valentino, Silva Benedetta, Loutrel Laurent, Thonney Jacques, Sylfa Fassasi Gallo Stéphane Morandi, and Bonsack Charles. 2017. “Perceived Coercion in Psychiatric Hospital Admission: Validation of the French-Language Version of the MacArthur Admission Experience Survey.” BMC Psychiatry 17(1): 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace Karen Trister, and Anderson Jocelyn C.. 2016. “Reproductive Coercion: A Systematic Review.” Trauma, Violence & Abuse 19(4): 471–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco Salvatore, Ishizaka Alessio, Tasiou Menelaos, and Torrisi Gianpiero. 2019. “On the Methodological Framework of Composite Indices: A Review of the Issues of Weighting, Aggregation, and Robustness.” Social Indicators Research 141(1): 61–94. [Google Scholar]
- Institute Guttmacher. 2020. “Investing in the Sexual and Reproductive Health of Adolescents in the Ouagadougou Partnership Countries.” https://www.guttmacher.org/fact-sheet/adding-it-up-investing-in-sexual-reproductive-health-adolescents-ouagadougou-partnership-countries
- Hardee Karen, Kumar Jan, Newman Karen, Bakamjian Lynn, Harris Shannon, Rodríguez Mariela, and Brown Win. 2014. “Voluntary, Human Rights-Based Family Planning: A Conceptual Framework.” Studies in Family Planning 45(1): 1–18. [DOI] [PubMed] [Google Scholar]
- Hartmann Betsy. 1987. Reproductive Rights and Wrongs: The Global Politics of Population Control and Contraceptive Choice. New York City: Harper and Row. [Google Scholar]
- Hendrixson Anne. 2018. “Population Control in the Troubled Present: The ‘120 by 20’ Target and Implant Access Program: Population Control in the Troubled Present.” Development and Change 50(3): 786–804. [Google Scholar]
- Herbst Kobus, Juvekar Sanjay, Bhattacharjee Tathagata, Bangha Martin, Patharia Nidhi, Tei Titus, Gilbert Brendan, and Sankoh Osman. 2015. “The INDEPTH Data Repository: An International Resource for Longitudinal Population and Health Data From Health and Demographic Surveillance Systems.” Journal of Empirical Research on Human Research Ethics 10(3): 324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt Kelsey, Dehlendorf Christine, and Langer Ana. 2017. “Defining Quality in Contraceptive Counseling to Improve Measurement of Individuals’ Experiences and Enable Service Delivery Improvement.” Contraception 96(3): 133–137. [DOI] [PubMed] [Google Scholar]
- Holt Kelsey, Zavala Icela, Quintero Ximena, Mendoza Doroteo, McCormick Marie C., Dehlendorf Christine, Lieberman Ellice, and Langer Ana. 2018. “Women’s Preferences for Contraceptive Counseling in Mexico: Results from a Focus Group Study.” Reproductive Health 15(1): 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwing Paul, Booth Tom, and Hughes David J.. 2018. The Wiley Handbook of Psychometric Testing: A Multidisciplinary Reference on Survey, Scale and Test Development. John Wiley & Sons. [Google Scholar]
- Kaneda Toshiko, and Greenbaum Charlotte. 2019. “Family Planning Data Sheet.” https://www.prb.org/wp-content/uploads/2019/03/fp-data-sheet-2019.pdf
- Kimport Katrina. 2021. No Real Choice: How Culture and Politics Matter for Reproductive Autonomy. Rutgers University Press. [Google Scholar]
- Kruk Margaret E, Anna D Gage, Arsenault Catherine, Jordan Keely, Leslie Hannah H, Roder-DeWan Sanam, Adeyi Olusoji, Barker Pierre, Daelmans Bernadette, Doubova Svetlana V,English Mike, García-Elorrio Ezequiel, Guanais Frederico, Gureje Oye, Hirschhorn Lisa R, Jiang Lixin, Kelley Edward, Lemango Ephrem Tekle, Liljestrand Jerker, Malata Address, Marchant Tanya, Matsoso Malebona Precious, Meara John G, Mohanan Manoj, Ndiaye Youssoupha, Norheim Ole F, Reddy K Srinath, Rowe Alexander K, Salomon Joshua A, Thapa Gagan, Twum-Danso Nana A Y, Pate Muhammad, 2018. “High-Quality Health Systems in the Sustainable Development Goals Era: Time for a Revolution.” Lancet Global Health 6(11): e1196–e1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer Ana. 2006. “Cairo after 12 Years: Successes, Setbacks, and Challenges.” Lancet 368(9547): 1552–1554. [DOI] [PubMed] [Google Scholar]
- Lidz Charles W. 1998. “Coercion in Psychiatric Care: What Have We Learned from Research?” Journal of the American Academy of Psychiatry and the Law 26(4): 631–637. [PubMed] [Google Scholar]
- Linley P Alex, Maltby John, Wood Alex M, Osborne Gabrielle, and Hurling Robert. 2009. “Measuring Happiness: The Higher Order Factor Structure of Subjective and Psychological Well-Being Measures.” Personality and Individual Differences 47(8): 878–884. [Google Scholar]
- Luna Zakiya, and Luker Kristin. 2013. “Reproductive Justice.” Annual Review of Law and Social Science 9: 327–352. [Google Scholar]
- Machiyama Kazuyo, and Cleland John. 2014. “Unmet Need for Family Planning in Ghana: The Shifting Contributions of Lack of Access and Attitudinal Resistance.” Studies in Family Planning 45(2): 203–226. [DOI] [PubMed] [Google Scholar]
- Manzer Jamie L, and Bell Ann V. 2021. “‘We’re a Little Biased’: Medicine and the Management of Bias through the Case of Contraception.” Journal of Health and Social Behavior 62(2): 120–135. [DOI] [PubMed] [Google Scholar]
- McCauley Heather L., Silverman Jay G., Jones Kelley A., Tancredi Daniel J., Decker Michele R., McCormick Marie C., Austin S. Bryn, Anderson Heather A., and Miller Elizabeth. 2017. “Psychometric Properties and Refinement of the Reproductive Coercion Scale.” Contraception 95(3): 292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry Sally Engle. 2016. The Seductions of Quantification: Measuring Human Rights, Gender Violence, and Sex Trafficking. Chicago, IL: University of Chicago Press. [Google Scholar]
- Ministry of Health of Burkina Faso. 2013. “Plan National de Relance de La Planification Familiale 2013–2015.” https://partenariatouaga.org/en/wp-content/uploads/2017/04/Plan-de-relance-PF_2013-2015_final-faso.pdf
- Ministry of Health of Burkina Faso. 2017. “Plan National de Relance de La Planification Familiale 2017–2020.” https://fp2030.org/sites/default/files/Burkina-Faso-CIP-2017_0.pdf
- Moran Allisyn C, Sangli Gabriel, Dineen Rebecca, Rawlins Barbara, Yaméogo Mathias, and Baya Banza. 2006. “Birth-Preparedness for Maternal Health: Findings from Koupéla District, Burkina Faso.” Journal of Health, Population, and Nutrition 24(4): 489. [PMC free article] [PubMed] [Google Scholar]
- Moreau Caroline, Karp Celia, Shannon N Wood Hadiza Galadanci, Kibira Simon Peter Sebina, Makumbi Fredrick, Omoluabi Elizabeth, Shiferaw Solomon, Seme Assefa, and Tsui Amy. 2020. “Reconceptualizing Women’s and Girls’ Empowerment: A Cross-Cultural Index for Measuring Progress Toward Improved Sexual and Reproductive Health.” International Perspectives on Sexual and Reproductive Health 46: 187–198. [DOI] [PubMed] [Google Scholar]
- Morroni Chelsea, and Glasier Anna. 2020. “Increasing the Use of Effective Postpartum Contraception: Urgent and Possible.” Lancet Global Health 8(3): e316–e317. [DOI] [PubMed] [Google Scholar]
- Moser David J., Arndt Stephan, Kanz Jason E., Benjamin Michelle L., Bayless John D., Reese Rebecca L., Paulsen Jane S., and Flaum Michael A.. 2004. “Coercion and Informed Consent in Research Involving Prisoners.” Comprehensive Psychiatry 45(1): 1–9. [DOI] [PubMed] [Google Scholar]
- Newman Karen, and Feldman-Jacobs Charlotte. 2015. “Family Planning and Human Rights: What’s the Connection and Why Is It so Important?” https://www.prb.org/wp-content/uploads/2021/02/08072015-family-planning-rights-brief.pdf
- Ouedraogo Leopold, Habonimana Desire, Nkurunziza Triphonie, Chilanga Asmani, Hayfa Elamin, Fatim Tall, Kidula Nancy, Conombo Ghislaine, Muriithi Assumpta, and Onyiah Pamela. 2021. “Towards Achieving the Family Planning Targets in the African Region: A Rapid Review of Task Sharing Policies.” Reproductive Health 18(1): 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson Erin, and Becker Stan. 2014. “Couples’ Unmet Need for Family Planning in Three West African Countries.” Studies in Family Planning 45(3): 339–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PMA2020. 2018. “Utilisation et Retrait de l’implant Au Burkina Faso.” https://www.pmadata.org/sites/default/files/data_product_results/PMA2020-Burkina-Faso-R5-Implants-memo-EN.pdf
- Population Reference Bureau. 2011. “Family Planning: Francophone West Africa on the Move—A Call to Action.” https://www.prb.org/wp-content/uploads/2021/02/10232012-ouagadougou-partnership_en.pdf
- Potts Malcolm, Gidi Virginia, Campbell Martha, and Zureick Sarah. 2011. “Niger: Too Little, Too Late.” International Perspectives on Sexual and Reproductive Health 37(2): 95–101. [DOI] [PubMed] [Google Scholar]
- Rao Mohan. 2004. From Population Control To Reproductive Health: Malthusian Arithmetic. New Dehli: SAGE Publications. [Google Scholar]
- Roberts Dorothy. 1997. Killing the Black Body: Race, Reproduction and the Meaning of Liberty. New York: Pantheon Books. [Google Scholar]
- Rominski Sarah D, Gupta Mira, Aborigo Raymond, Adongo Phillip, Engman Cyril, Hodgson Abraham, and Moyer Cheryl. 2014. “Female Autonomy and Reported Abortion-Seeking in Ghana, West Africa.” International Journal of Gynaecology and Obstetrics 126(3): 217–222. [DOI] [PubMed] [Google Scholar]
- Rossier Clémentine, and Hellen Jacqueline. 2014. “Traditional Birthspacing Practices and Uptake of Family Planning During the Postpartum Period in Ouagadougou: Qualitative Results.” International Perspectives on Sexual and Reproductive Health 40(2): 87–94. [DOI] [PubMed] [Google Scholar]
- Rossier Clémentine, Senderowicz Leigh, and Soura Abdramane. 2014. “Do Natural Methods Count? Underreporting of Natural Contraception in Urban Burkina Faso. Is Access Enough? Understanding and Addressing Unmet Need in Family Planning.” Studies in Family Planning 45: 171–182. [DOI] [PubMed] [Google Scholar]
- Rossier Clémentine, Soura Abdramane, Baya Banza, Compaoré Georges, Dabiré Bonayi, Santos Stéphanie Dos, Duthé Géraldine, Gnoumou Bilampoa, Kobiané Jean François, Kouanda Seni, Lankoandé Bruno, Legrand Thomas, Mbacke Cheikh, Millogo Roch, Mondain Nathalie, Montgomery Mark, Nikiema Aude, Ouili Idrissa, Pison Gilles, Randall Sara, Sangli Gabriel, Schoumaker Bruno, Zourkaleini Younoussi. 2012. “Profile: The Ouagadougou Health and Demographic Surveillance System.” International Journal of Epidemiology 41(3): 658–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankoh Osman, and Byass Peter. 2012. “The INDEPTH Network: Filling Vital Gaps in Global Epidemiology.” International Journal of Epidemiology 41(3): 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderowicz Leigh, Pearson Erin, Hackett Kristy, Huber-Krum Sarah, Francis Joel M, Ulenga Nzovu, and Bärnighausen Till. 2021. “‘I Haven’t Heard Much about Other Methods’: Quality of Care and Person-Centredness in a Programme to Promote the Postpartum Intrauterine Device in Tanzania.” BMJ Global Health 6: (e005775). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderowicz Leigh. 2015. “The Effects of Side-Effects: Issues with Modern Contraception in Urban Burkina Faso.” In Population Association of America Annual Meeting. San Diego, CA. [Google Scholar]
- Senderowicz Leigh. 2019. “‘I Was Obligated to Accept’: A Qualitative Exploration of Contraceptive Coercion.” Social Science & Medicine 239(March): 112531. [DOI] [PubMed] [Google Scholar]
- Senderowicz Leigh. 2020. “Contraceptive Autonomy: Conceptions and Measurement of a Novel Family Planning Indicator.” Studies in Family Planning 51(2): 161–176. [DOI] [PubMed] [Google Scholar]
- Senderowicz Leigh, and Higgins Jenny. 2020. “Reproductive Autonomy Is Nonnegotiable, Even in the Time of COVID-19.” Perspectives on Sexual and Reproductive Health 52(2): 81–85. [DOI] [PubMed] [Google Scholar]
- Senderowicz Leigh, and Kolenda Al. 2022. “‘She Told Me No, That You Cannot Change’: Understanding Provider Refusal to Remove Contraceptive Implants.” SSM - Qualitative Research in Health 2(December): 100154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderowicz Leigh, Kolenda Al, Eiseman Talia, and Suvarna Bhavana. 2022. “‘When They Force a Woman, It’s to Save Her Life’: Community Perceptions of Contraceptive Coercion.” In Population Association of America Annual Meeting. Atlanta, GA. [Google Scholar]
- Senderowicz Leigh, and Maloney Nicole. 2022. “Supply-Side Versus Demand-Side Unmet Need: Implications for Family Planning Programs.” Population and Development Review 48(3): 689–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderowicz Leigh, Pearson Erin, Hackett Kristy, Sarah Huber-Krum Joel M. Francis, Ulenga Nzovu, and Bärnighausen Till. 2021. “‘I Haven’t Heard Much about Other Methods’: Quality of Care and Person-Centeredness in a Program to Promote the Postpartum Intrauterine Device in Tanzania.” BMJ Global Health 6(4): 477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderowicz Leigh, Sokol Natasha, Pearson Erin, Francis Joel, Ulenga Nzovu, and Bärnighausen Till. 2022. “The Effect of a Postpartum Intrauterine Device Program on Choice of Contraceptive Method in Tanzania: A Secondary Analysis of a Cluster-Randomized Trial.” Health Policy and Planning. 38(1): 38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sié Ali, Louis Valérie R., Gbangou Adjima, Olaf Müller Louis Niamba, Stieglbauer Gabriele, Yé Maurice, Kouyaté Bocar, Sauerborn Rainer, and Becher Heiko. 2010. “The Health and Demographic Surveillance System (HDSS) in Nouna, Burkina Faso, 1993–2007.” Global Health Action 3(1): 5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieverding Maia, Schatzkin Eric, Shen Jennifer, and Liu Jenny. 2018. “Bias in Contraceptive Provision to Young Women Among Private Health Care Providers in South West Nigeria.” International Perspectives on Sexual and Reproductive Health 44(1): 19. [DOI] [PubMed] [Google Scholar]
- Speizer Ilene S. 2006. “Using Strength of Fertility Motivations to Identify Family Planning Program Strategies.” International Family Planning Perspectives 32(4): 185–191. [DOI] [PubMed] [Google Scholar]
- Sudhinaraset May, Afulani Patience A., Nadia Diamond-Smith Ginger Golub, and Srivastava Aradhana. 2018. “Development of a Person-Centered Family Planning Scale in India and Kenya.” Studies in Family Planning 49(3): 237–258. [DOI] [PubMed] [Google Scholar]
- David The and Foundation Lucile Packard. 2019. “Making Quality Matter.” https://www.packard.org/what-we-fund/population-reproductive-health/what-were-doing/making-quality-matter/
- Towriss Catriona A., Phillips Tamsin K., Brittain Kirsty, Zerbe Allison, Abrams Elaine J., and Myer Landon. 2019. “The Injection or the Injection? Restricted Contraceptive Choices among Women Living with HIV.” Sexual and Reproductive Health Matters 27(1): 215–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towriss Catriona A., and Rucell Jessica. 2019. “An Investigation into Contraceptive Choice in South Africa.” In 8th African Population Conference. Entebbe, Uganda. [Google Scholar]
- Tran Nguyen Toan, Seuc Armando, Coulibaly Abou, Landoulsi Sihem, Millogo Tieba, Sissoko Fatou, Yameogo Wambi Maurice E., Zan Souleyman, Cuzin-Kihl Asa, Kiarie James, Gaffield Mary Eluned, Thieba Blandine, and Kounda Séni. 2019. “Post-Partum Family Planning in Burkina Faso (Yam Daabo): A Two Group, Multi-Intervention, Single-Blinded, Cluster-Randomised Controlled Trial.” Lancet Global Health 7(8): e1109–e11017. [DOI] [PubMed] [Google Scholar]
- Tumlinson Katherine. 2016. “Measuring Quality of Care: A Review of Previously Used Methodologies and Indicators.” 2. Measuring and Monitoring Quality of Services and Quality of Care Project. https://www.popcouncil.org/uploads/pdfs/2016RH_MeasuringQOC_wp2.pdf [Google Scholar]
- Tumlinson Katherine, Okigbo Chinelo C., and Speizer Ilene S.. 2015. “Provider Barriers to Family Planning Access in Urban Kenya.” Contraception 92(2): 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumlinson Katherine, Speizer Ilene S., Curtis Siân L., and Pence Brian W.. 2014. “Accuracy of Standard Measures of Family Planning Service Quality: Findings from the Simulated Client Method.” Studies in Family Planning 45(4): 443–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNFPA. 2016. “Towards Equality in Access, Quality of Care and Accountability.” https://www.unfpa.org/publications/maternal-health-thematic-fund-annual-report-2016
- Upadhyay Ushma D., Dworkin Shari L., Weitz Tracy A., and Foster Diana Greene. 2014. “Development and Validation of a Reproductive Autonomy Scale.” Studies in Family Planning 45(1): 19–41. [DOI] [PubMed] [Google Scholar]
- Vijver Fons J. R. van de. 2010. “Emic–Etic Distinction.” In Encyclopedia of Cross-Cultural School Psychology, Clauss-Ehlers Caroline S. (ed.), 422–423. Boston, MA: Springer US. [Google Scholar]
- Wambui T, Ek A-C, and Alehagen S. 2009. “Perceptions of Family Planning among Low-Income Men in Western Kenya.” International Nursing Review 56(3): 340–345. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2021. WHO Guideline on Health Workforce Development, Attraction, Recruitment and Retention in Rural and Remote Areas. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Yirgu Robel, Wood Shannon N., Karp Celia, Tsui Amy, and Moreau Caroline. 2020. “‘You Better Use the Safer One… Leave This One’: The Role of Health Providers in Women’s Pursuit of Their Preferred Family Planning Methods.” BMC Women’s Health 20(170): e005775. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are not openly available due to the terms of our ethics approval. Data may be made available by the corresponding author on a case-by-case basis upon reasonable request and ethical clearance.


