Abstract
Background
In Gabon, children under 5 years of age and pregnant women are the populations who are most at risk of malaria. Despite the presence of accessible health facilities, the community-based management of childhood fever remains a very common practice in Gabon, which may have serious consequences on child health. As such, the objective of this descriptive cross-sectional survey is to assess the mothers’ perception and knowledge of malaria and its severity.
Methods
Different households were selected using the simple random sampling method.
Results
A total of 146 mothers from different households were interviewed in the city of Franceville, in southern Gabon. Among the households interviewed, 75.3% had a low monthly income (below the minimum monthly income of $272.73). Among the respondents, 98.6% of mothers had heard of malaria and 55.5% had heard of severe malaria. Regarding preventive measures, 83.6% of mothers used an insecticide-treated net as a means of protection. Self-medication was practiced by 68.5% of women (100/146).
Discussion
The use of health facilities was motivated by better care, the decision of the head of the family, but above all by the severity of the disease. Women identified fever as the main symptom of malaria, which could be beneficial for a quicker and more efficient management of the disease in children. Malaria educational campaigns should also increase awareness of severe forms of malaria and its manifestations. This study shows that Gabonese mothers react quickly when their children have fever. However, several external factors lead them to practice self-medication as a first resort. In this survey population, the practice of self-medication did not depend on social status, marital status, level of education, on the young age or inexperience of mothers (p > 0.05).
Conclusions
The data revealed that mothers may underestimate severe malaria and delay medical care by self-medicating, which can have detrimental effects for children and hinder the regression of the disease.
Keywords: Malaria knowledge, Malaria perception, Malaria practices, Maternal perception, Community-based management
Background
To date, malaria remains the most prevalent vector-borne parasitic disease in the world and a major public health problem in sub-Saharan Africa. Among the 241 million malaria cases and 627,000 deaths worldwide in 2020, sub-Saharan Africa accounted for more than 96% of cases [1]. Malaria is both a disease of poverty and a cause of poverty [2]. Delayed urbanization, poor quality of life, underfunded and poorly managed health services with long consultation times, all make malaria eradication difficult. Despite the high intensity of malaria infection in the African region, the use of control measures is still often insufficient in developing countries. Furthermore, people only consult health services when their practice of self-medication has failed despite the availability of early diagnosis and treatment for malaria in health facilities [3–5].
According to the World Health Organization (WHO), the majority of these reported cases in sub-Saharan Africa are children under 5 years of age which account for 67% of cases [1]. Moreover, in the Central African region, malaria is one of the main causes of morbidity and mortality for vulnerable groups such as pregnant women and young children [6–8]. In children, malaria can cause several organ malfunctions, which can lead to complicated forms of the disease. Severe anaemia is one of the main manifestations of severe malaria in children aged under five, followed by cerebral malaria and respiratory distress [9–11].
In Gabon, a central African country, malaria transmission is stable and intense throughout the year. According to the National Malaria Control Programme (NMCP), Gabon has recorded nearly 799,000 cases of malaria with over 500 deaths. Yet, in 2010, the country had 50% coverage of insecticide-treated nets (ITNs) and 99% coverage of artemisinin-based combination therapy (ACT). However, in recent years, the absence of the NMCP in the field and, therefore, the absence of awareness campaigns, education on malaria epidemiology and the distribution or sale of ITNs are becoming increasingly rarer each year [12].
The city of Franceville, located in southeastern Gabon, is the capital of the Haut-Ogooué province and the third largest city in the country. This city has a high population but mostly with a low economic status. Franceville is an urban area but additional urbanization efforts are needed as anarchic constructions favor the presence of mosquito breeding grounds and, therefore, their proliferation. The prevalence rate of malaria in Franceville is approximately 20% and the most frequently encountered plasmodial species is Plasmodium falciparum.
Despite the accessibility of health facilities, the community-based management of childhood fever remains a very common practice in Gabon and leads to a delay in proper care by health facilities. The objective of this study was to evaluate the level of knowledge of the various symptoms of childhood malaria among mothers, as well as their attitudes and care practices.
Methods
Type of study and location
This study is a descriptive cross-sectional survey. It was conducted in six districts (Ongouégné, Sable, Alélé, Ombelé, Ongali, Yéné) of the city of Franceville, in southeastern Gabon. The study was conducted during the month of June 2021. The different households were selected by the simple random sampling method. The city of Franceville is an administrative city whose neighborhoods are mostly under-integrated. According to the latest population census, dating from 2013, the city of Franceville had 129,694 inhabitants [13].
Data collection
Mothers from each selected household were included in the study after obtaining their informed consent. A survey with closed-ended questions was administered through an interview. The structured interviews were conducted by a team of two examiners. The information collected from the mothers in each household included socio-demographic data; knowledge, attitudes, and practices about malaria and its different forms; use of preventive or control means for malaria; possession of ITNs; practice of self-medication and type of medication used. The survey of mothers was conducted in French for those who spoke French and in the vernacular language of the region (Teke-Obamba) for those who did not speak French well.
Data analysis
The different answers of all interviewed mothers were recorded in Excel 2013 spreadsheets. Statistical analyses were performed with Epi-info version 3.3.2 (2005, CDC, Atlanta, USA) and RStudio version software (version 1.1.419). Categorical variables were described by proportions. These proportions were compared using the Chi2 test. For all analyses, the significance level was set at α = 5%.
Ethical clearance and approval was obtained from the National Research Ethics Committee in Gabon (No. 001/PR/SG/CNER/2018). Informed written consents were obtained from all levels of local government prior to data collection, and verbal consents were obtained from participants during data collection. Respondents were given the right to refuse or participate in the study and to withdraw from the study at any time. Privacy and confidentiality were maintained throughout the study.
Results
Socio-demographic characteristics of mothers
A total of 146 mothers from different households were interviewed in the city of Franceville. All of the households visited were from under-integrated neighbourhoods (100%). The Ongouégné neighbourhood had the highest proportion of mothers interviewed (30.3%), followed by the Alélé neighbourhood (29.4%). The majority of the study population had a middle school education (55.5%), followed by primary (Table 1) education (34.2%). Approximately 75.3% of the households surveyed had a low monthly income (below the minimum monthly income of about 272 dollars). The majority of mothers were unemployed (54.8%), and 15.7% were students. The study population was predominantly composed of young mothers, as 54.8% of women were aged 18 to 30 years.
Table 1.
Socio-demographic characteristics of the mothers in the study
| characteristics | Modality | Numbers | % |
|---|---|---|---|
| Age group (in years) of mothers | [18–30] | 80 | 54.8 |
| [31–40] | 47 | 32.2 | |
| [41–50] | 13 | 8.9 | |
| > 50 | 6 | 4.1 | |
| Marital status | Married | 19 | 13 |
| Cohabitation | 59 | 40.4 | |
| Single | 67 | 45.9 | |
| Divorced | 1 | 0.7 | |
| Level of education | Primary school | 50 | 34.2 |
| Middle school | 81 | 55.5 | |
| High school | 15 | 10.3 | |
| Mother’s occupation | Health Officer | 7 | 4.8 |
| Security officer | 1 | 0.7 | |
| Merchant | 16 | 10,9 | |
| Student | 23 | 15.7 | |
| University student | 6 | 4.1 | |
| Surface technician | 3 | 2.1 | |
| Teacher | 6 | 4.1 | |
| Mecanist | 1 | 0.7 | |
| Secretary | 1 | 0.7 | |
| Drugstore saleswoman | 2 | 1.4 | |
| Unemployed | 80 | 54.8 | |
| Economic/household level | Low | 110 | 75.3 |
| Mean | 11 | 7.5 | |
| High | 25 | 17.2 | |
| Number of people per household | [1–3] | 33 | 22.6 |
| [4–6] | 66 | 45.2 | |
| [7–10] | 36 | 24.7 | |
| > 10 | 11 | 7.5 | |
| Place of residence | Ongouégné | 44 | 30.3 |
| Sable | 17 | 11.6 | |
| Alélé | 43 | 29.4 | |
| Ombelé | 13 | 8.9 | |
| Ongali | 15 | 10.3 | |
| Yéné | 14 | 9.5 |
Description of the mothers’ knowledge of malaria
The analysis of the mothers’ knowledge showed that 98.6% had at least heard of malaria and 55.5% of them knew about severe malaria. Among the 146 mothers, 93.2% cited mosquito as the vector of malaria and 83.6% of them used ITNs as a means of protection. Other information is shown in Table 2.
Table 2.
Mothers’ knowledge of malaria in Franceville, Gabon
| Questions | Participant Responses | Number | % |
|---|---|---|---|
| Knowledge of malaria | Yes | 144 | 98.6 |
| No | 2 | 1.4 | |
| Symptoms in children | Fever | 125 | 85.6 |
| Vomiting | 71 | 48.6 | |
| Chills | 44 | 30.1 | |
| Diarrhea | 22 | 15.1 | |
| Température > 37.5 °C | 81 | 55.5 | |
| Other* | 106 | 72.6 | |
| Knowledge of severe malaria | Yes | 81 | 55.5 |
| No | 65 | 44.5 | |
| Signs of severe malaria | Neuromalaria | 34 | 23.3 |
| Convulsions | 67 | 45.9 | |
| Severe anemia | 50 | 34.2 | |
| Respiratory distress | 24 | 16.4 | |
| Prostration | 27 | 18.5 | |
| Other** | 20 | 13.7 | |
| Sources of information | Television | 11 | 7.5 |
| Radio | 4 | 2.8 | |
| Hospital | 45 | 30.8 | |
| Awareness campaign | 13 | 8.9 | |
| Community relay | 73 | 50 | |
| Vectors | Mosquitoes | 136 | 93.2 |
| Does not know | 9 | 6.2 | |
| Other | 1 | 0.7 | |
| Preventives measures | ITNs | 122 | 83.6 |
| IDP | 41 | 28.1 | |
| Other*** | 94 | 64.4 | |
| Factors favoring the development of mosquitoes | Unsanitary conditions | 100 | 68.5 |
| Poverty | 7 | 4.8 | |
| Stagnant water | 94 | 64.4 |
*(e.g., headache, stomach ache, fatigue, cough); **(altered consciousness, hypoglycemia, fatigue, diarrhea); ***(fan, hard house, drinking alcohol). ITNs: insecticide-treated bed nets, IDP: intra-domiciliary pulverization
Assessment of the mothers’ attitudes and practices
The results show that 68.5% (100/146) of mothers chose to self-medicate when their child had malaria and only 24.7% (36/146) of women went to a health centre as is proper. The use of health facilities was motivated by better (Table 3) care, the decision of the head of the family and, to a lesser extent, the severity of the disease. During the onset of fever in children, the practice of self-medication consisted of buying medicines in pharmacies and administering mainly Artefan (41.1%, 60/137), followed by Coartem (37.0%, 54/137). All the information is recorded in Fig. 1.
Table 3.
Determinants of the mothers’ self-medication practices
| Determinants | Modality | Number | % | P |
|---|---|---|---|---|
| Age group of mothers (in years) | [18–30] | 52 | 52 | 0.21 |
| [31–40] | 34 | 34 | ||
| [41–50] | 8 | 8 | ||
| > 50 | 4 | 4 | ||
| Level of education | Primary school | 37 | 37 | 0.2 |
| Middle school | 56 | 56 | ||
| Higher school | 7 | 7 | ||
| Marital status | Maried | 14 | 14 | 0.19 |
| Cohabiting | 41 | 41 | ||
| Single | 45 | 45 | ||
| Household standard of living | Low | 78 | 78 | 0.19 |
| Mean | 7 | 7 | ||
| High | 15 | 15 |
Fig. 1.
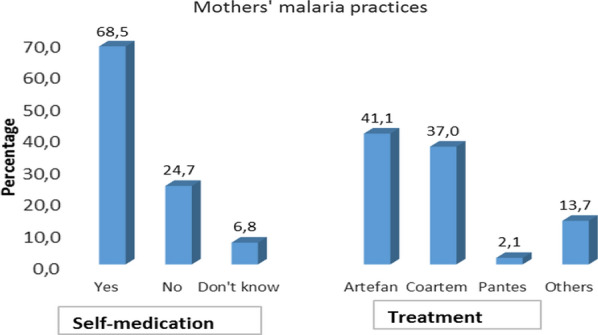
Malaria pratices of mothers in Franceville, Gabon
Comparison of self-medication by socio-demographic data
The analysis of these data showed that the practice of self-medication was not related to age, level of education, marital status and standard of living of the mother’s household in relation to the occurrence of malaria in children (p > 0.05).
Discussion
This study highlights the unfavorable socio-economic conditions to which the majority of mothers (75.3%) are subjected in their households in Franceville. Given that malaria is a disease which affects impoverished areas [14], the study was conducted to focus on sub-integrated neighbourhoods of Franceville to conduct this study.
All of the mothers who participated in the study had attended school (100%) and 98.6% of them had knowledge of the epidemiology of malaria and its mode of transmission (93.2%). The proportion of women with a knowledge of the mode of transmission was higher than that in other studies, 17.3% and 63% in Ethiopia [15, 16]. In this study population, 93.2% of women had good knowledge of the malaria vector, and 85.6% named fever as the main symptom of malaria. Other studies showed that mothers in Togo and Senegal also identify fever as the main symptom of malaria, with proportions of 72% and 81%, respectively [17, 18]. Knowledge of fever as the main symptom of malaria among mothers is beneficial for a rapid and effective management of the disease in children. However, the findings suggest that educational campaigns should also insist on the manifestations of severe forms of malaria. In fact, only 55.5% of the population surveyed in our study had knowledge of severe malaria and its different clinical signs.
The main sources of information for the surveyed population were community relays (50.0%), followed by health agents (30.8%) and malaria awareness campaigns (8.9%). These results are partially similar to those of Seck et al. in Senegal [18], where the dominant source of information were community health workers (62.9%).
These findings show that mothers react quickly to fever in their children. However, several external factors lead them to self-medicate as a first resort. This practice has also been widely reported in other studies focused on mothers with febrile children, such as in Tunisia with a frequency of 88.2%. In a study conducted in Gabon, 24.1% of mothers practiced self-medication [19–21]. This practice of self-medication could be a major problem by leading to the emergence of strains resistant to the different anti-malarial drugs. In this study population, the practice of self-medication did not depend on social status, marital status, level of education, on the young age or inexperience of mothers. This result could be explained by the fact that mothers are very responsive when their child has a fever, and even better, they always have antipyretics in reserve at home to bring down the child’s temperature in case of fever.
Conclusion
This descriptive cross-sectional study was conducted to support education campaigns and health measures to control malaria in Franceville, Gabon. The data revealed that mothers may underestimate severe malaria and delay medical care by self-medicating, which can have detrimental effects for children and hinder the regression of the disease. These results show that there is a need for the Ministry of Health through the NMCP to increase awareness campaigns on severe malaria in Gabon so that the population can improve their knowledge of the disease and seek medical care.
Acknowledgements
We thank the mothers of the city of Franceville for their hospitality. To the entire team of the UNEEREP unit of CIRMF. As well as, the members of the DEBIM/SP-MT-ML/SM team.
Abbreviations
- WHO
World Health Organization
- ITNs
Insecticide-Treated bed Net
- ACT
Artemisinin-based Combination Therapy
Author contributions
JBLD, EI, SMN and EBN designed the study and coordinated its execution. JBLW, SSO and APO collected conducted the survey from the mothers. JBLW, CNMM and FM analyzed the data. JBLW wrote the first draft of the article; JBLD, SLOL, and EBN made corrections. JBLD, JBLD and EBN provided guidance for data collection on clinical and confirmed malaria cases. All authors read and approved the final manuscript.
Funding
This work was done without funding.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and Consent to Participate
Ethical clearance and approval was obtained from the National Research Ethics Committee in Gabon (No. 001/PR/SG/CNER/2018). Informed written consents were obtained from all levels of local government prior to data collection, and verbal consents were obtained from participants during data collection. Respondents were given the right to refuse or participate in the study and to withdraw from the study at any time. The study as well as to withdraw at any time from the interview. Privacy and confidentiality were maintained throughout the study.
Consent for publication
Not applicable.
Competing interests
None of the authors have any financial or personal conflicts of interest related to this study. The corresponding author has full access to all study data and has final responsibility for the decision to submit this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . World malaria report 2021. Geneva: World Health Organization; 2021. [Google Scholar]
- 2.WHO . World malaria report 2007. Geneva: World Health Organization; 2007. [Google Scholar]
- 3.Théra MA, D’Alessandro U, Ouedraogo A, Packou J, Souleymane OA, Fané M, et al. Child malaria treatment practices among mothers in the district of Yanfolila, Sikasso region, Mali. Trop Med Int Health. 2000;5:876–81. doi: 10.1046/j.1365-3156.2000.00652.x. [DOI] [PubMed] [Google Scholar]
- 4.Fawole O, Onadeko M. Knowledge and home management of malaria fever by mothers and care givers of under five children. West Afr J Med. 2001;20:152–7. [PubMed] [Google Scholar]
- 5.Nyamongo I. Health care switching behaviour of malaria patients in a kenyan rural community. Soc Sci Med. 2002;54:377–86. doi: 10.1016/S0277-9536(01)00036-3. [DOI] [PubMed] [Google Scholar]
- 6.Bouyou-Akotet MK, Offouga CL, Mawili-Mboumba DP, Essola L, Madoungou B, Kombila M. Falciparum malaria as an emerging cause of fever in adults living in Gabon, Central Africa. Biomed Res Int. 2014;2014:351281. doi: 10.1155/2014/351281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dzeing-Ella A, Nze Obiang PC, Tchoua R, Planche T, Mboza B, Mbounja M, et al. Severe falciparum malaria in gabonese children: clinical and laboratory features. Malar J. 2005;4:1. doi: 10.1186/1475-2875-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richard-Lenoble D, Kombila M, Chandenier J, Gay F, Billiault X, Nguiri C. Le paludisme au Gabon. II: evaluation des prévalences parasitaires qualitatives et quantitatives sur l’ensemble du pays en milieu scolaire et préscolaires. Bull Soc Path Exot. 1987;80:532–42. [PubMed] [Google Scholar]
- 9.Kunuanunua TS, Nsibu CN, Bodi JM, Tshibola TK, Makusi Bura M, Magoga K, et al. Severe malaria in children: a descriptive report from Kinshasa, the Democratic Republic of Congo. J Trop Pediatr. 2015;61:272–8. doi: 10.1093/tropej/fmv029. [DOI] [PubMed] [Google Scholar]
- 10.Maitland K, Marsh K. Pathophysiology of severe malaria in children. Acta Trop. 2004;90:131–40. doi: 10.1016/j.actatropica.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Sumbele IUN, Kimbi HK, Ndamukong-Nyanga JL, Nweboh M, Anchang-Kimbi JK, Lum E, et al. Malarial anaemia and anaemia severity in apparently healthy primary school children in urban and rural settings in the Mount Cameroon area: cross sectional survey. PLoS ONE. 2015;10:e0123549. doi: 10.1371/journal.pone.0123549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO . World malaria report 2013. Geneva: World Health Organization; 2014. [Google Scholar]
- 13.DGDLS. Recensement general de la population et des logements de 2013 du Gabon. https://gabon.unfpa.org/sites/default/files/pub-pdf/Resultats%20Globaux%20RGPL%281%29.pdf. 2015:97.
- 14.WHO . World malaria report: 2012. Geneva: World Health Organization; 2012. [Google Scholar]
- 15.Deressa W, Ali A, Hailemariam D. Malaria-related health-seeking behaviour and challenges for care providers in rural Ethiopia: implications for control. J Biosoc Sci. 2008;40:115–35. doi: 10.1017/S0021932007002374. [DOI] [PubMed] [Google Scholar]
- 16.Yeneneh H, Gyorkos TW, Joseph L, Pickering J, Tedla S. Antimalarial drug utilization by women in Ethiopia: a knowledge-attitudes-practice study. Bull World Health Organ. 1993;71:763. [PMC free article] [PubMed] [Google Scholar]
- 17.Déti EK, Flénon J, Zohoun T, Maurice-Tison S, Salamon R, Atakouma YD. Prise en charge à domicile du paludisme chez l’enfant: propositions d’actions à partir des résultats d’une enquête CAP menée auprès des mères d’enfants de moins de 5 ans à Notsé (Togo) Santé. 2008;18:155–61. doi: 10.1684/san.2008.0109. [DOI] [PubMed] [Google Scholar]
- 18.Seck I, Fall I, Faye A, Ba O, Tal-Dia A. Malaria knowledge, attitudes and practices among women living in the rural area of Poponguine, Senegal. Med Trop (Mars) 2008;68:629–33. [PubMed] [Google Scholar]
- 19.Escourrou B, Bouville B, Bismuth M, Durrieu G, Oustric S. Automédication des enfants par les parents un vrai risque. Rev Prat. 2010;60:27–34. [PubMed] [Google Scholar]
- 20.Houéto D, d’Hoore W, Ouendo EM, Hounsa A, Deccache A. Fièvre chez l’enfant en zone d’endémie palustre au Bénin: analyse qualitative des facteurs associés au recours aux soins. Sante publique. 2007;19:363–72. doi: 10.3917/spub.075.0363. [DOI] [PubMed] [Google Scholar]
- 21.Mawili-Mboumba DP, Bouyou-Akotet MK, Kombila M. Usage des antipaludiques en automédication pour le traitement de la fièvre chez les enfants au Gabon. Sante. 2012;21:127–31. doi: 10.1684/san.2011.0267. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.


