Abstract
Background/aims
To assess surgical patterns in ophthalmology by subspecialty in the USA.
Methods
Ophthalmic surgeons were categorised as comprehensive/subspecialist based on billed procedures in the 2017–2018 Medicare Provider Utilization and Payment Data. Poisson regression models assessed factors associated with physicians performing surgeries in the core domain (eg, cataract extractions) and subspecialty domain. Models were adjusted for provider gender, time since graduation, geographical region, practice setting and hospital affiliation.
Results
There were 10 346 ophthalmic surgeons, 74.7% comprehensive and 25.3% subspecialists. Cataract extractions were performed by 6.0%, 9.9%, 21.0%, 88.1% and 95.3% of specialists in surgical retina, neuro-ophthalmology/paediatrics, oculoplastics, glaucoma and cornea, respectively. Retina specialists were more likely to perform cataract surgery if they were 20–30 or>30 years in practice (relative risk: 2.20 (95% CI: 1.17 to 4.12) and 3.74 (95% CI: 1.80 to 7.76), respectively) or in a non-metropolitan setting (3.78 (95% CI: 1.71 to 8.38)). Among oculoplastics specialists, male surgeons (2.71 (95% CI: 1.36 to 5.42)), those in practice 10–20 years or 20–30 years (1.93 (95% CI: 1.15 to 3.26) and 1.91 (95% CI: 1.11 to 3.27), respectively) and in non-metropolitan settings (3.07 (95% CI: 1.88 to 5.02)) were more likely to perform cataract surgery. Only 26 of the 2620 subspecialists performed surgeries in two or more subspecialty domains.
Conclusions
There is a trend towards surgical subspecialisation in ophthalmology in the USA whereby some surgeons focus their surgical practice on subspecialty procedures and rarely perform surgeries in the core domain.
INTRODUCTION
The field of ophthalmology is becoming increasingly subspecialised with more ophthalmology graduates pursuing subspecialty fellowship training than ever before. Estimates indicate that only 34% of ophthalmology graduates in 1996 pursued fellowship while that figure has risen to 45% by 2003 and 72% in 2018.1 2 Given the fast-paced evolution of knowledge and technology in ophthalmology, fellowship training may provide intense exposure to a subspecialty area and allow for the focused development of clinical and surgical skills.1 As more advanced surgeries fall under the purview of fellowship trained subspecialists, the procedures that define comprehensive ophthalmology have become more ambiguous.3 4 The changing landscape of a comprehensive ophthalmic practice impacts residency training. Ophthalmology residency was designed, by the Accreditation Council for Graduate Medical Education (ACGME), to provide an ‘adequate base for a comprehensive ophthalmic practice’.5 To best prepare graduates, residency training must therefore meet the demands of the modern comprehensive ophthalmic practice.
The purpose of this study was to evaluate the degree of subspecialisation among practicing ophthalmic surgeons and the factors associated with this subspecialisation. Using the 2017–2018 Medicare Provider Utilization and Payment Data, we compared the proportion of subspecialists who performed core domain ophthalmology surgeries, as required during ophthalmology residency, across various subspecialties. We hypothesised that providers in certain subspecialties (eg, cornea) would use core domain skills more than others (eg, surgical retina) and that external factors such as where the providers practiced (eg, in a rural setting) would influence the degree of subspecialisation as well. Understanding the scope of current practice patterns among ophthalmic surgeons can inform resident education as we design curricula to best prepare trainees for a contemporary ophthalmology practice.
MATERIALS AND METHODS
Data source
Our primary data source was the 2017–2018 Medicare Provider Utilization and Payment Data, specifically the Physician and Other Supplier Public Use File (PUF).6 The database includes claims submitted under the Medicare fee-for-service programme by all US physicians during this time period. The number of distinct services billed are identified by Healthcare Common Procedure Coding System (HCPCS) service code and linked to each physician identified by the National Provider Identifier. Statistics for individual HCPCS codes are included in the PUF only if the physician performed that service for at least 10 distinct patients. The subspecialty and comprehensive designation for each physician was calculated based on the HCPCS codes billed (online supplemental table 1). We augmented this PUF file with several auxiliary sources as previously described.7 In brief, we linked the PUF with the 2015 Physician Compare National Downloadable File which contains demographic information for Medicare physicians including the year of graduation from medical school.8 We linked the ZIP code of the provider’s practice from the PUF to Federal Information Processing Standard Publication county codes using the US Department of Housing and Urban Development mapping file.9 10 For ZIP codes that were matched to multiple county codes, the first county in the mapping file was used for subsequent analysis. County codes were then classified as metropolitan or non-metropolitan using the US Department of Agriculture county classification system.11 States were grouped into one of four major geographical regions using the US Census Bureau classification system.12
Categorising surgeons into subspecialist versus comprehensive
Subspecialists were identified on the basis of surgeries billed. Providers who billed for any subspecialty surgery were categorised as subspecialists. The list of subspecialty surgeries was created through an iterative process. We first compared the procedural categories and minimums from the ACGME against requirements for subspecialty fellowship training (including cornea, glaucoma, surgical retina, oculoplastics and neuro-ophthalmology/paediatrics) by the Association of University Professors of Ophthalmology, and American Society of Ophthalmic Plastic and Reconstructive Surgery.13 We then reviewed credentialing guidelines at academic institutions and expert consensus agreement (CXC, SA, FW, DS, NRM and PR) was reached to produce the final list of surgeries used to identify subspecialists (online supplemental table 1).
The procedural minimums from the ACGME were reviewed to create a list of core domain surgeries (online supplemental table 1). Surgeons who did not perform subspecialty surgery but billed for any surgery in the core domain including cataract extractions, conjunctival procedures, eyelid laceration repairs, chalazion excisions and ptosis repairs/blepharoplasties were categorised as comprehensive ophthalmologists.
To assess the performance of our subspecialist designation, we reviewed 50 randomly selected Medicare-billing physicians in each defined subspecialty category. We also reviewed 50 randomly selected physicians in the comprehensive category. Publicly available information including practice website, online physician biographies and American Academy of Ophthalmology membership data was used to determine if the ophthalmologist had completed formal fellowship training and the subspecialty of the fellowship.
Inclusion and exclusion criteria
Only ophthalmologists with MD or DO credentials who were more than 6 years from medical school graduation were included. We reasoned that most physicians have finished clinical training including fellowship and are in practice 6 years after medical school graduation.
Statistical analysis
The primary objective was to identify the proportion of physicians in each subspecialty who performed core domain as well as subspecialty surgeries. Physicians in each subspecialty were categorised by whether they performed only subspecialty surgery (surgical retina, cornea, glaucoma, oculoplastics, neuro-ophthalmology/paediatrics) or subspecialty combined with cataract surgery. Separate binary outcomes were constructed for each of the other core domain surgeries: conjunctival procedures, eyelid laceration repairs, chalazion excisions and ptosis repairs/blepharoplasties. We fit Poisson regression models adjusted for: gender, time since graduation (grouped by categories of 10 years), geographical region (Northeast, South, Midwest and West), rurality based on practice location (metropolitan or non-metropolitan) and practice category (whether the practice was affiliated with a hospital). Poisson regression models were chosen to estimate relative risk ratios directly since the outcome of performing core domain surgery in addition to subspecialty surgery was common (>10%) among certain subspecialties.14 The relative risk ratio reflects the probability of performing a core domain surgery with subspecialty surgery in one group compared with another. A similar analysis was performed among comprehensive ophthalmologists to assess factors that were associated with performing surgeries in each core domain. The fit of each model was evaluated with the goodness-of-fit χ2 test. Statistical significance was set at p<0.05. All analyses were performed using Python (Python Software Foundation. Python Language Reference, V.3.8.9) and Stata (StataCorp. 2019. Stata Statistical Software: Release 16).
RESULTS
There were 15 097 unique ophthalmologists with 10 346 providers performing sufficient ophthalmic surgeries to be in the database. The demographic characteristics of the providers are shown in table 1.
Table 1.
Baseline characteristics of providers who performed ophthalmic surgery in the 2017–2018 Medicare Provider Utilization and Payment Data
| Provider characteristics | All providers (N=10 346) | Retina (N=1224) | Oculoplastics (N=609) | Cornea (N=338) | Glaucoma (N=378) | Neuro/peds* (N=71) | Comprehensive (N=7726) | P value† |
|---|---|---|---|---|---|---|---|---|
| Years in practice | <0.001 | |||||||
| <10 years | 2912 (28.1%) | 473 (38.6%) | 193 (31.7%) | 129 (38.2%) | 125 (33.1%) | 19 (26.8%) | 1973 (25.5%) | |
| 10–20 years | 2831 (27.4%) | 345 (28.2%) | 180 (29.6%) | 85 (25.1%) | 108 (28.6%) | 19 (26.8%) | 2094 (27.1%) | |
| 20–30 years | 2931 (28.3%) | 316 (25.8%) | 158 (25.9%) | 81 (24.0%) | 107 (28.3%) | 25 (35.2%) | 2244 (29.0%) | |
| >30 years | 1672 (16.2%) | 90 (7.4%) | 78 (12.8%) | 43 (12.7%) | 38 (10.1%) | 8 (11.3%) | 1415 (18.3%) | |
| Gender | <0.001 | |||||||
| Female | 2147 (20.8%) | 108 (8.8%) | 124 (20.4%) | 51 (15.1%) | 84 (22.2%) | 18 (25.4%) | 1762 (22.8%) | |
| Male | 8199 (79.2%) | 1116 (91.2%) | 485 (79.6%) | 287 (84.9%) | 294 (77.8%) | 53 (74.6%) | 5964 (77.2%) | |
| Region | <0.001 | |||||||
| Northeast | 2192 (21.2%) | 185 (15.1%) | 103 (16.9%) | 52 (15.4%) | 63 (16.7%) | 9 (12.7%) | 1780 (23.0%) | |
| South | 3687 (35.6%) | 477 (39.0%) | 238 (39.1%) | 156 (46.2%) | 154 (40.7%) | 29 (40.8%) | 2633 (34.1%) | |
| Midwest | 2234 (21.6%) | 282 (23.0%) | 125 (20.5%) | 74 (21.9%) | 78 (20.6%) | 14 (19.7%) | 1661 (21.5%) | |
| West | 2233 (21.6%) | 280 (22.9%) | 143 (23.5%) | 56 (16.6%) | 83 (22.0%) | 19 (26.8%) | 1652 (21.4%) | |
| Rurality | <0.001 | |||||||
| Metro‡ | 9533 (92.1%) | 1186 (96.9%) | 580 (95.2%) | 329 (97.3%) | 362 (95.8%) | 71 (100.0%) | 7005 (90.7%) | |
| Non-metro | 813 (7.9%) | 38 (3.1%) | 29 (4.8%) | 9 (2.7%) | 16 (4.2%) | 0 (0.0%) | 721 (9.3%) | |
| Hospital affiliation | <0.001 | |||||||
| No | 4448 (43.0%) | 366 (29.9%) | 158 (25.9%) | 97 (28.7%) | 161 (42.6%) | 35 (49.3%) | 3631 (47.0%) | |
| Yes | 5898 (57.0%) | 858 (70.1%) | 451 (74.1%) | 241 (71.3%) | 217 (57.4%) | 36 (50.7%) | 4095 (53.0%) | |
| Core domain surgeries | ||||||||
| Cataract extractions | 8363 (80.8%) | 73 (6.0%) | 128 (21.0%) | 322 (95.3%) | 333 (88.1%) | 7 (9.9%) | 7500 (97.1%) | <0.001 |
| Conjunctival procedures | 568 (5.5%) | 56 (4.6%) | 102 (16.7%) | 93 (27.5%) | 85 (22.5%) | 1 (1.4%) | 231 (3.0%) | <0.001 |
| Eyelid laceration repairs | 315 (3.0%) | 0 (0.0%) | 282 (46.3%) | 0 (0.0%) | 1 (0.3%) | 0 (0.0%) | 32 (0.4%) | <0.001 |
| Chalazion excisions | 270 (2.6%) | 1 (0.1%) | 103 (16.9%) | 4 (1.2%) | 2 (0.5%) | 0 (0.0%) | 160 (2.1%) | <0.001 |
| Ptosis repairs/blepharoplasties | 1148 (11.1%) | 2 (0.2%) | 578 (94.9%) | 5 (1.5%) | 5 (1.3%) | 2 (2.8%) | 556 (7.2%) | <0.001 |
Neuro-ophthalmology/paediatrics.
Pearson’s χ2 test.
Metropolitan.
Our subspecialist designation showed good agreement with manual review of fellowship training. One hundred per cent of the selected physicians who performed retina specific surgery were surgical retina fellowship trained, 98% for cornea, 92% for glaucoma, 84% for oculoplastics and 98% for neuro-ophthalmology/paediatrics. Manual review of the randomly selected comprehensive ophthalmologists showed 28% were subspecialty fellowship trained (including cornea, anterior segment and glaucoma). This suggests that our subspecialty classification algorithm was very specific but less sensitive. Using this designation, 74.7% were categorised as comprehensive ophthalmologists, and 25.3% were categorised as subspecialists (cornea, glaucoma, neuro-ophthalmology/paediatrics, oculoplastics and retina).
A total of 8363 providers performed cataract surgery, most of whom were comprehensive ophthalmologists (89.7%) (figure 1). Among the subspecialists, 6.0% of retina specialists and 21.0% of oculoplastics specialists performed cataract surgery (table 1). Retina specialists were more likely to perform cataract surgery if they were further out from training, and practiced in a non-metropolitan county (table 2). Oculoplastics specialists were more likely to perform cataract surgery if they were men, had been in practice longer and worked in a non-metropolitan setting (table 2). Cataract surgery was performed by 95.3% of cornea specialists and 88.1% glaucoma specialists (table 1). No factors predicted performance of cataract surgeries among cornea and glaucoma specialists (table 2). Only 9.9% of neuro-ophthalmology/paediatrics specialists performed cataract surgery. All models constructed demonstrated good fit on χ2 tests.
Figure 1.
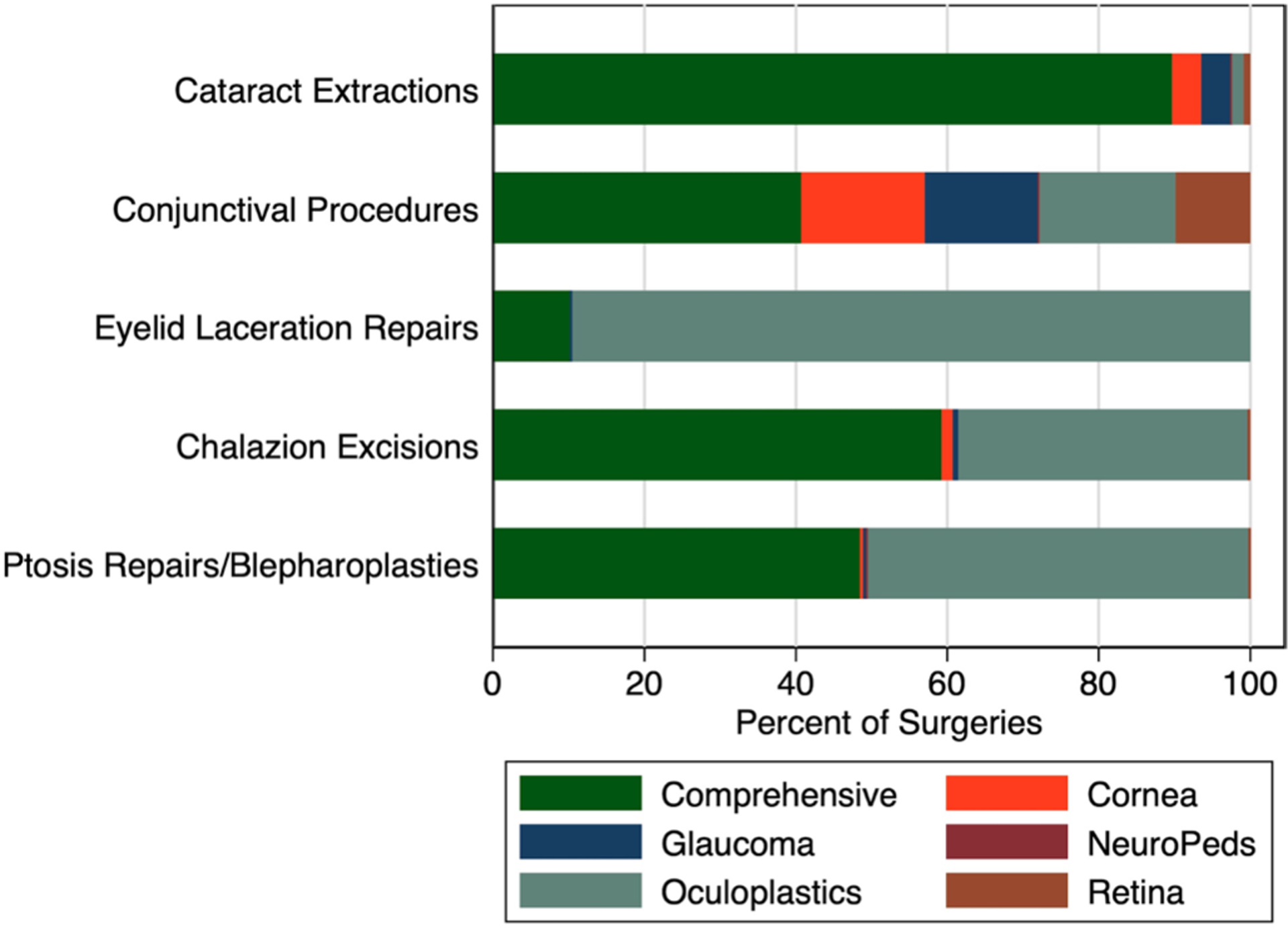
Primary specialty of the providers performing each core domain surgery.
Table 2.
Relative risk of performing cataract surgery as well as subspecialty surgery, stratified by provider primary subspecialty
| Retina (N=1224) | Oculoplastics (N=609) | Cornea (N=338) | Glaucoma (N=378) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | 95% CI | P value | Risk ratio | 95% CI | P value | Risk ratio | 95% CI | P value | Risk ratio | 95% CI | P value | |
| Years in practice | ||||||||||||
| <10 years | Reference | Reference | Reference | Reference | ||||||||
| 10–20 years | 1.51 | 0.78 to 2.92 | 0.22 | 1.93 | 1.15 to 3.26 | 0.01* | 0.99 | 0.75 to 1.31 | 0.94 | 1.02 | 0.78 to 1.33 | 0.91 |
| 20–30 years | 2.20 | 1.17 to 4.12 | 0.01* | 1.91 | 1.11 to 3.27 | 0.02* | 0.95 | 0.71 to 1.28 | 0.75 | 0.88 | 0.66 to 1.16 | 0.36 |
| >30 years | 3.74 | 1.80 to 7.76 | 0.00*** | 1.70 | 0.90 to 3.23 | 0.10 | 0.89 | 0.62 to 1.29 | 0.54 | 0.73 | 0.47 to 1.12 | 0.15 |
| Gender | ||||||||||||
| Female | Reference | Reference | Reference | Reference | ||||||||
| Male | 1.63 | 0.58 to 4.55 | 0.35 | 2.71 | 1.36 to 5.42 | 0.00** | 1.08 | 0.78 to 1.49 | 0.64 | 1.02 | 0.79 to 1.33 | 0.87 |
| Region | ||||||||||||
| Northwest | Reference | Reference | Reference | Reference | ||||||||
| South | 0.51 | 0.25 to 1.04 | 0.06 | 1.35 | 0.79 to 2.31 | 0.27 | 1.06 | 0.76 to 1.48 | 0.72 | 0.89 | 0.65 to 1.22 | 0.48 |
| Midwest | 0.90 | 0.44 to 1.83 | 0.77 | 1.14 | 0.61 to 2.11 | 0.68 | 1.04 | 0.71 to 1.51 | 0.86 | 0.96 | 0.68 to 1.36 | 0.82 |
| West | 1.08 | 0.54 to 2.16 | 0.82 | 1.17 | 0.65 to 2.10 | 0.60 | 1.06 | 0.71 to 1.57 | 0.78 | 0.94 | 0.66 to 1.33 | 0.72 |
| Rurality | ||||||||||||
| Metro* | Reference | Reference | Reference | Reference | Reference | |||||||
| Non-metro | 3.78 | 1.71 to 8.38 | 0.00** | 3.07 | 1.88 to 5.02 | 0.00*** | 1.07 | 0.55 to 2.09 | 0.84 | 1.08 | 0.64 to 1.83 | 0.76 |
| Hospital affiliation | ||||||||||||
| No | Reference | Reference | Reference | Reference | ||||||||
| Yes | 0.65 | 0.40 to 1.04 | 0.07 | 0.73 | 0.50 to 1.08 | 0.11 | 1.00 | 0.77 to 1.28 | 0.97 | 0.96 | 0.77 to 1.20 | 0.71 |
p<0.05,
p<0.01,
p<0.001.
Metropolitan.
A total of 568 providers performed pterygium repair or other conjunctival surgeries, most of whom were comprehensive ophthalmologists (40.7%) (figure 1, table 1). Retina surgeons in the South were more likely than those in the Northeast to perform conjunctival surgeries. No other major patterns predicted performance of conjunctival surgeries among the other subspecialists (online supplemental table 2). Among comprehensive ophthalmologists, male surgeons were more likely to perform conjunctival surgeries compared with females (online supplemental table 3).
Of the other core domain surgeries, a total of 315 providers performed eyelid laceration repairs, most eyelid laceration repairs were performed by oculoplastics specialists (89.5%), and some by comprehensive ophthalmologists (10.2%) (figure 1). No factors predicted which comprehensive ophthalmologists were more likely to perform eyelid laceration repairs (online supplemental table 3). A total of 270 providers performed chalazion excision, mostly by comprehensive ophthalmologists (59.3%) (figure 1). Among the comprehensive ophthalmologists, male surgeons and those located in the Midwest were more likely to perform chalazion excision (online supplemental table 3). A total of 1148 providers performed ptosis repairs and blepharoplasties, almost evenly split between oculoplastics specialists (50.4%) and comprehensive ophthalmologists (48.4%) (figure 1). Among the comprehensive ophthalmologists, surgeons located in the South, Midwest or West, and affiliated with a hospital were more likely to perform ptosis repairs and blepharoplasties (online supplemental table 3).
Only 26 of the 2620 subspecialists performed surgeries in two or more subspecialty domains and 13.8% of these specialists were in practice less than 10 years, 17.2% between 10–20 years, 44.8% between 20–30 years and 24% more than 30 years.
DISCUSSION
Using data from Medicare-billing providers, we find a trend towards surgical subspecialisation in ophthalmology whereby some surgeons focus their surgical practice on subspecialty procedures and rarely perform surgeries in the core domain. Although subspecialty surgeries are required for residency, most providers who perform these procedures do additional fellowship training, while providers who do not complete such fellowship training do not perform these procedures. There are some subspecialists (retina and neuro-ophthalmology/paediatrics) who rarely perform surgeries in the core domains taught during residency. Of the core domain surgeries, conjunctival procedures are performed most ubiquitously. Other core domain surgeries including eyelid laceration repairs, chalazion excisions, ptosis repairs/blepharoplasties, are predominantly performed by oculoplastics specialists and some comprehensive ophthalmologists. Overall, the degree of subspecialisation in surgical practice varies among the different ophthalmology subspecialties.
A limited number of subspecialty surgery is required for the procedural minimums of residency, but most providers who perform these procedures in practice undergo additional fellowship training. The choice of ophthalmology graduates to pursue fellowship training is multifactorial. It is influenced by financial issues, preferred practice setting, experiences during residency training, academic achievement, academic career aspirations, lifestyle choices, timing of career decisions and gender.1 The majority of graduates in the USA and other countries including Canada decide to pursue further fellowship training.1 15 Education during residency plays an important role in this process. Some studies suggest that graduates could be pursuing further subspecialty training because of inadequate training during residency and additional training in fellowship is needed to develop clinical and surgical skills related to the subspecialty.1 Indeed, this could be the case with the decision to pursue vitreoretinal surgery fellowship. Surveys of third-year residents indicate that few residents are comfortable performing vitreoretinal surgery after residency training.16 But with the ever-expanding number of surgical advances in vitreoretinal surgery and other subspecialties, it is difficult to train residents to master these procedures in the context of all the other demands of residency. Exposure to these procedures is still important during residency. It can help inform a graduate’s decision to pursue further training, help with patient preoperative counselling, improve quality of referrals, clarify communication among providers, improve outcomes of complex multispecialty cases and aid in arrangement of potential combined surgical cases.
Ophthalmology subspecialists perform surgeries of the core domain taught during residency to varying degrees. Cornea and glaucoma specialists use these skills the most. About 21% of oculoplastics specialists still perform intraocular surgeries, including cataract surgery or conjunctival procedures. Neuro-ophthalmology/paediatrics and retina specialists are the least likely to use skills in the core domain surgeries taught during residency. Assessing retina specialists, only 10% perform surgeries from core ophthalmology domains including cataract surgeries. Factors associated with this include being out in practice for a longer period of time, location in non-metropolitan areas and not practicing with groups affiliated with hospitals. This suggests that there could be external demands that influence practice patterns. It could be that retina specialists practicing in non-metropolitan areas do not have as easy access to anterior segment partners and thus have to perform their own cataract surgeries. Retina specialists affiliated with hospitals, representing large groups or academic centres, could have different referral patterns or perhaps have easier access to colleagues who could help perform combined cataract cases. The trend of retina surgeons who have been in practice for longer being more likely to perform their own cataract surgery compared with those who trained more recently gives further evidence to the increasing subspecialisation seen in more recent decades.
These data prompt consideration for restructuring residency education to ensure well-trained and well-prepared residents. As graduate medical education shifts to competence-based education and away from a largely time-based apprenticeship system, the subspecialisation seen in practicing ophthalmologists suggests that there could be flexibility within ophthalmology resident education for more individualised learning plans.17–19 Residents who have met procedural minimum requirements and who have achieved certain milestones could be given opportunities to tailor their education to their future practice. For example, graduates planning to pursue vitreoretinal surgery fellowship could be given more opportunities to begin their subspecialty training even during residency. Alternatively, for those planning to go into a comprehensive practice, more time could be spent to further skills in core domains. The integration of the internship year with ophthalmology residency could provide additional time and opportunities for individualised learning.
Surgeon specialisation also has implications for patient outcomes. Previous studies suggest that highly specialised cataract surgeons have lower complications rates including posterior capsule rupture, dropped lens fragments, retinal detachments and suspected endophthalmitis compared with diversified cataract surgeons who perform primarily non-cataract procedures (eg, corneal surgery, glaucoma surgery, retinal surgery, strabismus surgery and orbital surgery).20 It could be that more subspecialisation with a narrower focus on a few procedures allows surgeons to hone skills and techniques thus translating to improved patient outcomes. Although patient outcomes could not be evaluated as part of this study, future studies can assess whether these trends seen for increasing procedural subspecialisation also translate to improved patient outcomes.
There are several limitations of this study. This study is primarily concerned with surgical procedures and did not evaluate the other procedural minimums of residency including lasers and injections. There is no gold standard for how to identify fellowship training based on HCPCS codes billed. Our designation system was highly specific in identifying those who were fellowship trained but not sensitive. Because we were using HCPCS codes, we were only able to evaluate surgical retina specialists and not medical retina specialists. Since the database only includes HCPCS codes billed to at least 10 distinct patients, low-volume fellowship trained providers are more likely to be classified as comprehensive ophthalmologists than subspecialists. We thus are underestimating the proportion of providers with fellowship training. The results of our study are not generalisable as Medicare claims might not represent the entire scope of a physician’s practice, particularly among paediatric subspecialists.
This is one of the first studies to examine diversity of surgical practice patterns among ophthalmologists. Findings from our study suggest that certain procedures are highly subspecialised and are predominantly done by fellowship trained subspecialists, and the core domain surgeries are used by subspecialists to varying degrees depending on a number of external factors. These data suggest that there could be some flexibility to the existing residency curriculum to allow for individualised learning plans to best prepare graduates for their future intended practice.
Supplementary Material
Funding
This study was supported by an unrestricted departmental grant to the Wilmer Eye Institute from Research to Prevent Blindness (CC, FW, DS, NRM and PYR) and the Wilmer Biostatistics Core Grant P30EY01765 (JW).
Footnotes
Competing interests
None declared.
Ethics approval This study was reviewed by the Institutional Review Board at the Johns Hopkins University School of Medicine and determined to be exempt.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. See above.
REFERENCES
- 1.Gedde SJ, Budenz DL, Haft P, et al. Factors influencing career choices among graduating ophthalmology residents. Ophthalmology 2005;112:1247–54. [DOI] [PubMed] [Google Scholar]
- 2.Zafar S, Bressler NM, Golnik KC, et al. Fellowship match outcomes in the U.S. from 2010 to 2017: analysis of San Francisco match. Am J Ophthalmol 2020;218:261–7. [DOI] [PubMed] [Google Scholar]
- 3.Lee PP, Relles DA, Jackson CA. Subspecialty distributions of ophthalmologists in the workforce. Arch Ophthalmol 1998;116:917–20. [DOI] [PubMed] [Google Scholar]
- 4.Lee PP, Jackson CA, Relles DA. Estimating eye care workforce supply and requirements. Ophthalmology 1995;102:1964–72. [DOI] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. Acgme program requirements for graduate medical education in ophthalmology, 2007. Available: https://www.ghei.uci.edu/PDF/acgme-ophthalmology-requirements2007.pdf [Accessed21 Apr 2021].
- 6.Centers for Medicare & Medicaid Services. Physician and other supplier data cy 2018 | CMS. pdf,2012. Available: https://www.cms.gov/research-statistics-data-systems/medicare-provider-utilization-and-payment-data/medicare-provider-utilization-and-payment-data-physician-and-other-supplier/physician-and-other-supplier-data-cy-2018 [Accessed 1 Apr 2021].
- 7.Ahmad S, Ramulu P, Akpek E, et al. Gender-Specific trends in ophthalmologist Medicare collections. Am J Ophthalmol 2020;214:32–9. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services. National Downloadable file, 2003. Available: https://data.cms.gov/provider-data/dataset/mj5m-pzi6 [Accessed 1 Apr 2021].
- 9.Dim A, Wilson R. Crosswalking ZIP Codes to Census Geographies: Geoprocessing the U.S. Department of Housing & Urban Development’s ZIP Code Crosswalk Files. Cityscape: A Journal of Policy Development and Research 2020;22https://www.huduser.gov/portal/periodicals/cityscpe/vol22num1/ch12.pdf [Google Scholar]
- 10.United States Department of Housing and Urban Development. Hud USPS ZIP code Crosswalk files. Available: https://www.huduser.gov/portal/datasets/usps_crosswalk.html [Accessed 1 Apr 2021].
- 11.United States Department of Agriculture. Rural-Urban continuum codes,2012. Available: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/[Accessed1 Apr 2021].
- 12.United States Census Bureau. Geographic levels, 2009. Available: https://www.census.gov/programs-surveys/economic-census/guidance-geographies/levels.html [Accessed 1 Apr 2021].
- 13.Accreditation Council for Graduate Medical Education. Procedural categories and minimum numbers, 2003. Available: https://www.acgme.org/Portals/0/PFAssets/ProgramResources/OPH_CaseLogInfo.pdf?ver=2021-03-15-133325-270 [Accessed 20 Apr 2021].
- 14.McNutt L-A, Wu C, Xue X, et al. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 2003;157:940–3. [DOI] [PubMed] [Google Scholar]
- 15.Noble J, Schendel S, Daniel S, et al. Motivations and future trends: a survey of Canadian ophthalmology residents. Can J Ophthalmol 2007;42:821–5. [DOI] [PubMed] [Google Scholar]
- 16.Shah VA, Reddy AK, Bonham AJ, et al. Resident surgical practice patterns for vitreoretinal surgery in ophthalmic training programs in the United States. Ophthalmology 2009;116:783–9. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen VT, Losee JE. Time-versus competency-based residency training. Plast Reconstr Surg 2016;138:527–31. [DOI] [PubMed] [Google Scholar]
- 18.Accreditation Council for Graduate Medical Education. Ophthalmology milestones. Available: https://www.acgme.org/Portals/0/PDFs/Milestones/OphthalmologyMilestones.pdf?ver=2020-09-01-152146-910 [Accessed20 Apr 2021].
- 19.Accreditation Council for Graduate Medical Education. The milestone Guidebook. Available: https://www.acgme.org/Portals/0/MilestonesGuidebook.pdf?ver=2020-06-11-100958-330 [Accessed 20 Apr 2021].
- 20.Campbell RJ, El-Defrawy SR, Gill SS, et al. Surgical outcomes among focused versus diversified cataract surgeons. Ophthalmology 2021;128:827–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. See above.


