Abstract
Introduction:
Congenital diaphragmatic hernia (CDH) repair is an area of active research. Large defects requiring patches have a hernia recurrence rate of up to 50%. We designed a biodegradable polyurethane (PU)-based elastic patch that matches the mechanical properties of native diaphragm muscle. We compared the PU patch to a non-biodegradable Gore-Tex™ (polytetrafluoroethylene) patch.
Methods:
The biodegradable polyurethane was synthesized from polycaprolactone, hexadiisocyanate and putrescine, and then processed into fibrous PU patches by electrospinning. Rats underwent 4mm diaphragmatic hernia (DH) creation via laparotomy followed by immediate repair with Gore-Tex™ (n=6) or PU (n=6) patches. Six rats underwent sham laparotomy without DH creation/repair. Diaphragm function was evaluated by fluoroscopy at 1 and 4 weeks. At 4 weeks, animals underwent gross inspection for recurrence and histologic evaluation for inflammatory reaction.
Results:
There were no hernia recurrences in either cohort. Gore-Tex™ had limited diaphragm rise compared to sham at 4 weeks (1.3mm vs 2.9mm, p=0.003), but no difference was found between PU and sham (1.7mm vs 2.9mm, p=0.09). There were no differences between PU and Gore-Tex™ at any time point. Both patches formed an inflammatory capsule, with similar thicknesses between cohorts on the abdominal (Gore-Tex™ 0.07mm vs. PU 0.13mm, p=0.39) and thoracic (Gore-Tex™ 0.3 mm vs. PU 0.6 mm, p=0.09) sides.
Conclusion:
The biodegradable PU patch allowed for greater diaphragmatic excursion compared to Gore-Tex™. There were similar inflammatory responses to both patches. Further work is needed to evaluate long-term functional outcomes and further optimize the properties of the novel PU patch in vitro and in vivo.
Keywords: congenital diaphragmatic hernia, bioengineering, hernia repair, patch repair
INTRODUCTION
Primary repair of congenital diaphragmatic hernia (CDH) is not possible in up to 50% of cases [1,2], necessitating patch or muscular flap repair. Patch repair of CDH has been associated with a high hernia recurrence rate of up to 50% [3,4], and in some studies has been found to have a significantly higher recurrence rate than primary repair [5,6]. Additionally, a high rate of bowel obstructions due to adhesions has been seen with patch repair [3,7–9]. Materials used for patch repair have included polytetrafluoroethylene (PTFE), commonly known as Gore-Tex™, and biologic materials such as small intestinal submucosal tissues, marketed as Surgisis, however, the optimal material for patch repair of CDH remains unknown.
Factors contributing to recurrence following patch repair of CDH may include the inert nature of synthetic materials such as Gore-Tex™, inability to incorporate with native diaphragm tissue, and an inability to grow as the child grows [10]. Surgisis, on the other hand, may reabsorb quite early on after repair, ranging from 2–8 weeks [10,11], thus placing patients at risk of early recurrence. Tissue engineering may hold the key to the development of an ideal diaphragm replacement material, which matches the tensile strength of the muscle while promoting neovascularization of the patch to enable continued growth with the child [2,12].
Biodegradable elastomeric polyurethane has been studied for use in vascular and muscle tissue replacement due to its soft elastic nature, its high mechanical strength, and its ability to integrate with bioactive materials [13]. In this pilot study, we tested a biodegradable polyurethane (PU)-based elastic patch that matches the mechanical properties of native diaphragm muscle as a patch material for diaphragmatic hernia (DH) repair in a rodent model. We compared the PU patch to the commonly used and commercially available Gore-Tex™ patch and hypothesized that the patch would be durable, would allow for greater diaphragmatic excursion than Gore-Tex™ due to its elastic nature, and would result in less inflammatory response due to its biodegradable nature.
METHODS
Approval to perform this animal study was obtained from the Institutional Animal Care and Use Committee (IACUC Protocol #21833). All surgical procedures were done using sterile technique. Animal care was performed as specified by the Guide for the Care and Use of Laboratory Animals.
Electrospun PU Patch Synthesis
Synthesis of biodegradable PU was completed according to previous publication [14]. The biodegradable PU was synthesized from polycaprolactone (PCL, average number molecular weight Mn=2000, Sigma) and hexadiisocyanate (HDI, Sigma) with a chain extender of putrescine (Sigma) (PCL:HDI:Purescine molar ratio=1:2:1). PU was dissolved in 1,1,1,3,3,3-hexafluoro-2-propanol (Oakwood Products) to make the 8% w/v (weight/volume) PU solution. The PU solution was loaded into a syringe with a needle. The distance between the needle tip and the plate collector was 15 cm. The collection plate was located on an x-y motor that jogged in a square for even dispersal of PU fibers on the collector plate. The needle and plate were charged to +25 kV and −5kV, respectively. An infusion rate of PU solution was set as 1 mL/hr. Electrospinning process continued for 4 hours and then the sample was dried in a fume hood overnight.
PU and Gore-Tex™ Patch Characterization
Morphological analysis of PU and Gore-Tex™ (W.L. Gore & Associates, Inc) patches was carried out with a scanning electron microscope (SEM) (Hitachi S-4800 FE SEM) after sputter coated with silver/platinum in a Hummer VI Sputtering System. Fiber diameter (fiber #=120) was analyzed with ImageJ. A universal testing system (Test Resources) was used to perform tensile mechanical testing. PU and Gore-Tex™ patches were cut into strips (30 mm length × 5 mm width) (n = 12). A 5.6-pound (lb) load cell was used to measure cyclic loading behavior (30% strain for 10 cycles) for both PU and Gore-Tex™ patches. Failure testing used a 5.6 lb and 250 lb load cell for PU and Gore-Tex™ patches, respectively. A ramping rate of 10 mm/minute was used for both cyclic loading and failure tests. Tensile moduli were estimated by quantifying the slopes of the stress-strain curves at two strain ranges of 0–10% and 25–50%.
Surgical Model
The animal model used in this study was adult Sprague-Dawley rats, as rat models have been previously used to study CDH [12,15,16]. Three cohorts were utilized: DH creation and repair with Gore-Tex™ (n = 6); DH creation and repair with the novel PU patch (n = 6); and controls (n = 6). For the two DH cohorts, the rats were placed under general anesthesia via endotracheal intubation. The chest and abdomen were shaved and prepped with betadine. A midline laparotomy was made. The left hemidiaphragm was exposed. A 4-mm diaphragmatic defect was created using a 4-mm aortic punch in the central portion of the diaphragm. The defect was repaired immediately using a 6-mm circular patch of either Gore-Tex™ or the novel PU patch sutured to the surrounding diaphragm muscle with running prolene suture of sizes 5–0 to 7–0. Any residual pneumothorax was evacuated using a syringe and needle. The laparotomy incision was closed with running vicryl suture. The animals were awakened from anesthesia and recovered and returned to the vivarium housing. The control cohort underwent endotracheal intubation with general anesthesia, midline laparotomy, followed by no manipulation of the diaphragm, with closure of the laparotomy defect. The sham laparotomy was performed in the control animals to control for the effect of post-operative recovery from a midline laparotomy incision among cohorts, which may impact diaphragmatic movement due to post-operative pain. Animals were survived for 4 weeks and underwent functional testing as described below followed by euthanasia with post-mortem laparotomy and evaluation also described below.
With regards to the relative size of the chosen patches, it is relevant to note the average sizes of the rat diaphragm. The average anterior-posterior length of the diaphragms of the tested rats was 27.3 mm, while the average medial-lateral length of the diaphragms was 37.2 mm. Thus the 6 mm patch represents 22.0% of the anterior-posterior diaphragm and 16.1% of the medial-lateral diaphragm size in this animal model.
Functional Testing
Diaphragmatic excursion was evaluated by performing fluoroscopy of animals during spontaneous breathing. Animals were physically restrained without anesthesia. The fluoroscopic images were taken using a Inveon MM CT scanner. This was performed at 1 week and 4 weeks post-surgery. The fluoroscopic images were examined for frames that demonstrated the largest diaphragm excursion during inhalation and exhalation. In the frames with largest diaphragm excursion, the vertical displacement of the diaphragm was obtained by measuring the difference in the vertical position at the same point on the left diaphragm between inhalation and exhalation using ImageJ [17]. Functional testing was performed both at 1 and 4 weeks post-surgery to allow for full post-operative recovery, as pain in the early post-operative period may limit diaphragmatic excursion.
Post-Mortem Gross Analysis
At 4 weeks, animals were again placed under general anesthesia via nose cone and a midline laparotomy was performed. The left hemidiaphragm was inspected for recurrence (present or absent), and for adhesions between the liver and the diaphragm, graded at full adhesions, in which the liver was completely adherent to the patch; mild adhesions in which less than 50% of the patch was covered by liver, or no adhesions. The animals were then euthanized by exsanguination by aortic transection. Following euthanasia, the animals were perfused and the diaphragm was excised. Adhesions on the thoracic side of the diaphragm between the lung and the patch were graded in the same manner as previously described.
Histologic Evaluation
The diaphragms were stored in 10% buffered formalin. They were then dehydrated in 30% sucrose solution and cryopreserved in Optimal Cutting Temperature (OCT) compound. The diaphragms were serially sectioned into 9 μm sections and were stained with hematoxylin and eosin (H&) and coverslipped. The resulting H&E slides were digitally scanned at 10x magnification on the ImageXpress Pico Cell Imaging System (Molecular Devices, LLC) scanner The thickness of the inflammatory capsule that formed on both the abdominal and thoracic sides of the patch was measured.
Data Analysis
The following outcomes were compared between cohorts: distance of diaphragmatic excursion at 1 and 4 weeks; presence of recurrent DH at 4 weeks; degree of adhesions to the patch at 4 weeks; and thickness of the inflammatory capsule on the thoracic and abdominal sides at 4 weeks. Categorical data were compared by Fischer’s exact test. Continuous data are presented as median and interquartile range (IQR) and were compared using Kruskal Wallis test between all three cohorts or Mann Whitney U test between the two surgical cohorts. Results were considered statistically significant at p < 0.05. All data analysis was performed in Prism (GraphPad Software, Inc.).
RESULTS
Characterization of Gore-Tex™ and PU patches
Gore-Tex™ and PU patches are white in color and appear similar, but they exhibited different microstructures (Figure 1). Under SEM imaging, Gore-Tex™ patch contained solid fragments with fine fibers, while PU patch was composed of a vast nanofibrous network. Fiber diameters of PU patches were 638 ± 238nm. There were no notable large pores within the PU patches.
Figure 1:
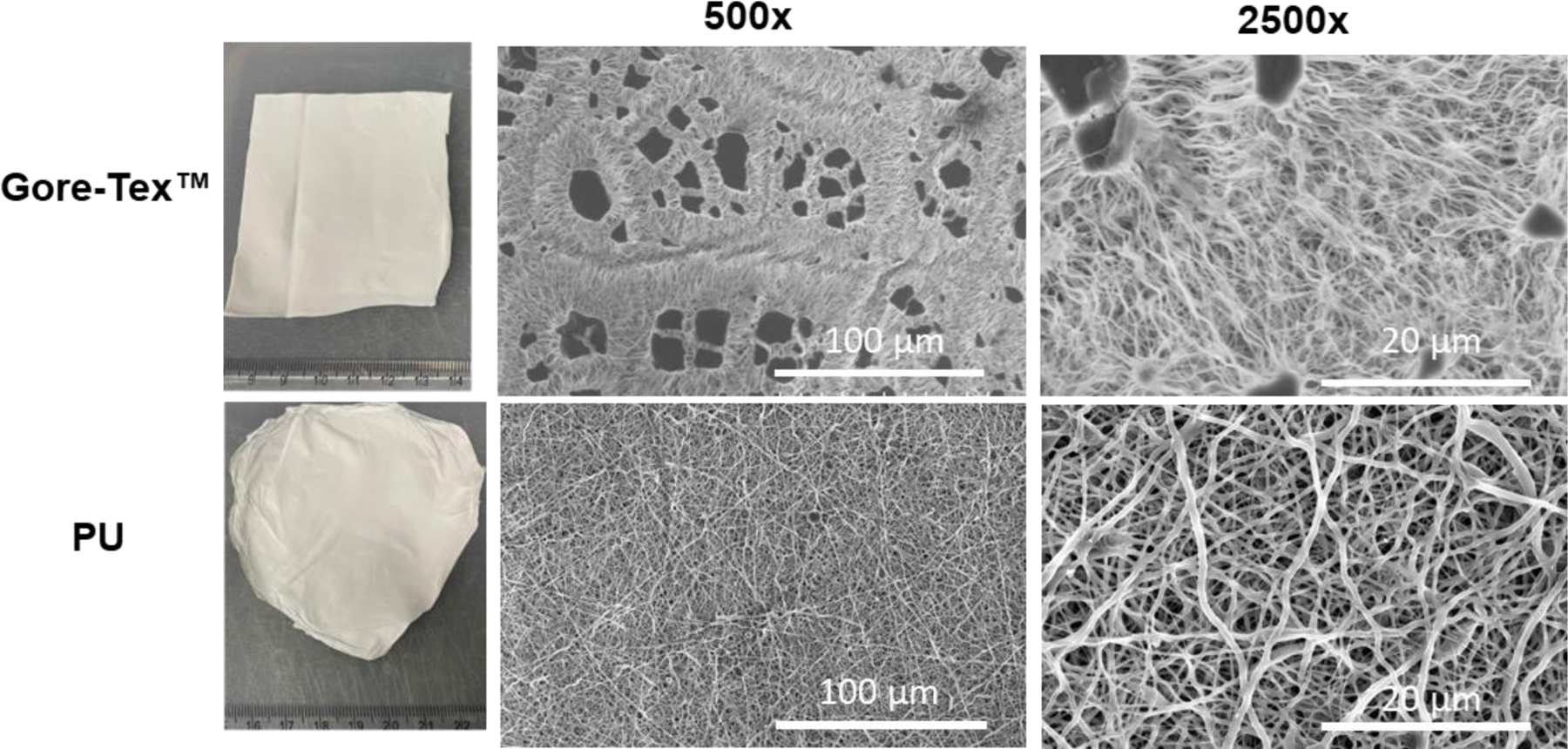
Macroscopic and SEM images of Gore-Tex™ and PU patches.
Gore-Tex™ and PU patches showed obvious differences in stress-strain behavior (Figure 2A). Gore-Tex™ had a failure stress of 10.8 ± 0.9 MPa, whereas the failure stress of PU patches was 2.1 ± 0.9 MPa. Initial tensile modulus (0–10% strain) for Gore-Tex™ and PU patches were 1.2 ± 0.3 MPa and 0.8 ± 0.3 MPa, respectively (p=0.067, Figure 2B). At 25–50% strain, the tensile modulus of the Gore-Tex™ patch (17.4 ± 1.3 MPa) was approximately 13 times more than that of PU patch (1.3 ± 0.4 MPa), indicating a significant difference (p<0.0001). Over the course of 10 cycles of cyclic loading, very notable differences in material responses occurred between Gore-Tex™ and PU patch. Gore-Tex™ appeared inelastic and underwent large plastic deformation after the first cycle (Figure 2C). Later cycles exhibited no readings of stress between 0–20% strain and exhibited resistance to loading in strain range larger than 21%. Cyclic stretching of PU patches showed repetitive loading and loading curves, reflecting the elastic nature of PU materials (Figure 2D).
Figure 2:

(A) Stress-Strain curves of Gore-Tex™ and PU patches. (B) Summary table of failure stress, failure strain, and moduli at different strain ranges. Cyclic stretching graphs of (C) Gore-Tex™ and (D) PU patches to 30% strain over 10 cycles.
Diaphragmatic Hernia Recurrence
There were no diaphragmatic hernia recurrences in either surgical cohort at 4 weeks on gross examination.
Diaphragmatic Excursion
At 1 week post DH creation and repair, there was no significant difference in diaphragmatic excursion between cohorts (compared to sham median 2.1 mm [IQR 1.5–2.8]: Gore-Tex™ median 1.2 mm [IQR 0.8–2.0], p = 0.05; PU median 2.0 mm [IQR 1.0–2.5], p = 0.52; Gore-Tex™ vs. PU, p = 0.19). At four weeks, Gore-Tex™ displayed limited diaphragmatic excursion compared to sham (Gore-Tex™ median 1.3 mm [IQR 0.7–1.6] vs. sham 2.9 mm [IQR 1.9–3.7], p = 0.003), but no difference was found between PU and sham (PU 1.7mm [IQR 1.0–2.8] vs. sham 2.9 mm [IQR 1.9–3.7], p = 0.09). PU and Gore-Tex™ had no significant difference at 4 weeks (PU 1.7 mm vs. Gore-Tex™ 1.3 mm, p = 0.20).
Adhesions
All animals in the Gore-Tex™ group had full adhesions between the liver and the patch and mild adhesions between the lung and the patch. All animals in the PU group had full adhesions between the liver and the patch and 5/6 had mild adhesions on the thoracic side while one animal had full adhesions between the lung and the patch. In the sham group one animal had mild adhesions to the liver and no other adhesions were seen in any animal.
Inflammatory Capsule
An inflammatory capsule formed surrounding both patch materials. There was no significant difference in the thickness of the inflammatory capsule on either the abdominal side (PU median 0.13 mm [IQR 0.06–0.62] vs. Gore-Tex™ 0.07mm [IQR 0.05–0.27], p = 0.39) or the thoracic side (PU 0.56 mm [IQR 0.41–0.92] vs. Gore-Tex™ 0.32 [IQR 0.22–0.51] mm, p = 0.09).
DISCUSSION
In this pilot study, we assessed the feasibility and effectiveness of a polyurethane-based biodegradable patch for the repair of diaphragmatic hernias. Our 4-week animal study demonstrated that the PU patch is durable during this period of time, allowing for greater diaphragmatic excursion than the commercially available Gore-Tex™ patch. We found that the diaphragmatic excursion of the PU patches at 4 weeks was comparable to the native diaphragm muscle and PU patches resulted in a similar degree of inflammatory capsule formation when compared to Gore-Tex™. These preliminary results are supportive of further optimization and evaluation of the PU based patch in animal studies of diaphragmatic hernia.
Hernia recurrence is a primary consideration in CDH repair. Larger defects are more likely to require patch repair, and defect size has been correlated with survival [1]. However, there is conflicting data on recurrence rates following patch CDH repair compared to primary repair in the literature. A systematic review of 20 studies found that patch repair was associated with a 2.83-times higher odds of recurrence than primary repair [6]. However, a single institution study out of Children’s Hospital of Philadelphia found very low recurrence rates following both patch (5.4%) and primary repair (4.0%), which the authors attributed not to patch material but to technical factors of patch repair, including fashioning the patch into a dome configuration [18]. Another single institution study also found an overall low rate of recurrence (10%), and on multivariable analysis, patch repair was not an independent predictor of recurrence [19]. With regards to the choice of patch material to reduce the risk of recurrence, several studies have found no significant difference between Gore-Tex™ and Surgisis [10,20], while an American Pediatric Surgical Association Outcomes and Evidence Based Practice Committee found that Gore-Tex™ was the most durable patch material, concluding that Level 4 evidence supported the use of oversized or dome-shaped Gore-Tex™ patches to reduce recurrence rates [8]. In this pilot study, we found that the short-term durability of the novel PU patch was confirmed at 4 weeks, with no defect recurrences identified. Further studies are needed on the long-term durability of the PU patch. CDH recurrences often are cited as occurring at a median time of 12 months post-repair, with 76% of recurrences happening before two years [5].
The optimal patch material is elastic and allows for appropriate diaphragmatic excursion during inspiration and expiration. A patch which is too stiff will not allow for adequate diaphragmatic motion, potentially resulting in respiratory compromise. The PU patch shows great elasticity and is less stiff than the Gore-Tex™ in the strain range of 25% to 50%. Those mechanical characteristics may result in diaphragmatic motion that is more physiological, allowing appropriate diaphragmatic excursion and improved respiratory function. As we know, decreased diaphragmatic excursion has been associated with prolonged hospitalizations, longer time on the ventilator, and higher rate of supplemental oxygen requirement at discharge [21]. We measured diaphragmatic excursion at 1 week and 4 weeks post repair. While there was no significant difference in diaphragmatic excursion at 1 week, at 4 weeks, Gore-Tex™ had limited excursion compared to sham, while diaphragms repaired with the novel PU patch had similar excursion compared to sham. Gore-Tex™ and PU were similar when compared to each other, thus indicating that the PU patch had similar motility compared to the commonly used Gore-Tex™ patch. Inherent to the function of the diaphragm and any replacement tissue is the tensile strength of the tissue. In autopsy studies of diaphragm composition, age-related changes have been identified, with increased extracellular matrix components in neonates and infants, while older children have higher tensile strength [22]. The mechanical behavior of the native diaphragm is thought to be determined by the native tissue tensile strength and the and the ability to modify its shape with changes in lung volume during respiration [23,24]. Diaphragmatic rupture, or in the case of CDH, re-herniation, may occur when the pressures the diaphragm is subjected to overcome the tissue tensile strength, especially of the muscular portion; thus, a diaphragmatic replacement with high tensile strength is desirable.
The biologic reaction to patch materials used in CDH repair may have downstream consequences. Gore-Tex™, an inert material which does not cause as robust an inflammatory response, has been found to have lower rates of subsequent adhesive bowel obstructions than biologic patch materials such as Surgisis [9]. However, a meta-analysis found no difference in bowel obstructions by type of patch material [10]. In our study, extensive adhesions were found between both Gore-Tex™ and PU patches to the liver on the abdominal side, with mild adhesions between both patches and the lung on the thoracic side. There were no adhesions to bowel identified. Additionally, the inflammatory capsule that formed in response to the patches were of similar thicknesses. Thus, the PU patch appears to invoke a similar inflammatory response to the Gore-Tex™ patches. What is unknown is the degree to which the PU patch integrates with the adjacent native diaphragm tissue. Further studies are planned to include histochemical analyses of the degree of ingrowth of native diaphragm muscle, connective tissue, and neovascularization, as these are critical components to designing a patch which can adapt and grow with the child. One potential advantage of the PU patch is the biodegradation rate can be altered, and by performing serial studies over a variety of timepoints, we hope to match the degradation rate to the rate of tissue ingrowth with the goal of complete replacement over time with native diaphragm.
Our mechanical testing of the PU patches in comparison to the Gore-Tex™ patches revealed key differences. Grossly, the PU patch appears as a non-woven nanofibrous network, while the Gore-Tex™ patch contains flakes and fibers. The nanofibrous scaffold has several potential advantages. In addition to structural integrity, homogeneity, and structural similarity to that of native collagenous matrix, they can be populated with cells such as myoblasts or mesenchymal stromal stem cells, which may aid in diaphragmatic regeneration [25,26]. Additionally, the modulus for Gore-Tex™ at higher strains was much higher than that of PU (13-times), indicating that the PU patch behaves more like soft connective tissue than the stiffer Gore-Tex™ patch. Cyclic loading-unloading testing showed that the Gore-Tex™ patches underwent large plastic deformation while the PU patch exhibited elastic behavior. This elastic behavior feature makes PU an attractive patch material for CDH, as the diaphragm is subject to cyclic large ranges of deformation over the course of an individual’s lifetime. Although the failure stress of Gore-Tex™ patch is much higher than the PU patch, the failure stress of PU at 2.1 ± 0.9 MPa makes PU patch comparable to other soft connective tissue such as heart valves, which primarily consist of collagen fibers, elastic fibers, and glycosaminoglycans [27], and which work under a demanding mechanical loading condition [27].
Limitations
This pilot study has several limitations. First, the small sample size in each cohort limits our ability to detect small differences between cohorts. The defect size is relatively small, and future animal studies are planned with larger diaphragmatic defects. The model is one of diaphragmatic defect in an adult animal and is surgically created, rather than a true model of congenital diaphragmatic hernia. This is due to the small size of fetal rats and the difficulty in performing diaphragmatic hernia repair on such a small scale in utero. Additionally, a surgical model was chosen to allow for identical defect creation with regards to size and location, to reduce confounding factors when comparing the repair modalities. Lastly, animals were survived for only 4 weeks to assess the short-term durability of this PU patch; however, most recurrences occur within the first 1–2 years following repair in human patients and longer-term survival studies are needed to evaluate long-term durability.
Future Directions
As one advantage of our PU system, many structural and mechanical features of the PU patch are modifiable, including fiber modulus, fiber density, fiber orientation/alignment, and fiber tortuosity, and future fine-tuning has the potential to fabricate patches more closely mimicking the features of native diaphragm tissue. Future studies will be required to evaluate the utility of the PU patch in the repair of larger diaphragmatic defects to more closely mimic the large CDH defects that require patch repair in human patients. We will also assess the evolution of the PU patch mechanical properties after implantation by performing biomechanical characterizations on the explants obtained at various post-repair time points. Additionally, longer-term outcomes will be evaluated as these repairs would ideally last the lifetime of the patient. Further histochemical analyses are planned to assess neovascularization into the patch and to evaluate for muscle fiber and collagen formation as the patch integrates with surrounding diaphragm muscle over time.
CONCLUSION
In this preliminary study, the PU patch was durable over a 4-week period and allowed for diaphragmatic excursion similar to control animals. There were similar inflammatory responses to both patches within 4-week implantation. Further work is needed to evaluate long-term functional outcomes and optimize the properties of the PU patch in vitro and in vivo.
Figure 3:

Fluoroscopic evaluation of diaphragmatic excursion at 1 week and 4 weeks after surgery. *denotes significance at p < 0.05.
Figure 4:

Histologic images of the PU and Gore-Tex™ patches showing the inflammatory capsule which formed on the abdominal and thoracic sides of the patches. The black bars indicate the measured inflammatory capsules.
Financial support:
This study was partially supported by the NIH grant 1R21HD107324-01 to Y.H. and A.W., the Shriners Hospitals for Children postdoctoral fellowship 84304-NCA-21 to C.Z, and Children’s Miracle Network funding to A.W. and D.F.
Footnotes
Disclosures: The authors have no conflicts of interest to declare.
Manuscript Category: Original article, Experimental Research
Previous Communication: This paper was presented as a Surgeon’s Den presentation at the Canadian Association of Paediatric Surgeons Annual Meeting in Victoria, British Columbia, Canada in September 2022.
Level of Evidence: Level II, prospective comparative study
REFERENCES
- [1].Lally KP, Lally PA, Lasky RE, Tibboel D, Jaksic T, Wilson JM, et al. Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics 2007;120. 10.1542/peds.2006-3040. [DOI] [PubMed] [Google Scholar]
- [2].Fauza DO. Tissue engineering in congenital diaphragmatic hernia. Semin Pediatr Surg 2014;23:135–40. 10.1053/j.sempedsurg.2014.04.004. [DOI] [PubMed] [Google Scholar]
- [3].Moss RL, Chen CM, Harrison MR. Prosthetic patch durability in congenital diaphragmatic hernia: A long-term follow-up study. J Pediatr Surg 2001;36:152–4. 10.1053/jpsu.2001.20037. [DOI] [PubMed] [Google Scholar]
- [4].Laituri CA, Garey CL, Valusek PA, Fike FB, Kaye AJ, Ostlie DJ, et al. Outcome of congenital diaphragmatic hernia repair depending on patch type. European Journal of Pediatric Surgery 2014;24:363–5. 10.1055/s-0030-1268456. [DOI] [PubMed] [Google Scholar]
- [5].Macchini F, Raffaeli G, Amodeo I, Ichino M, Encinas JL, Martinez L, et al. Recurrence of Congenital Diaphragmatic Hernia: Risk Factors, Management, and Future Perspectives. Front Pediatr 2022;10:1–6. 10.3389/fped.2022.823180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Heiwegen K, de Blaauw I, Botden SMBI. A systematic review and meta-analysis of surgical morbidity of primary versus patch repaired congenital diaphragmatic hernia patients. Sci Rep 2021;11:1–9. 10.1038/s41598-021-91908-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lund DP, Mitchell J, Kharasch V, Quigley S, Kuehn M, Wilson JM. Congenital diaphragmatic hernia: The hidden morbidity. J Pediatr Surg 1994;29:258–64. 10.1016/0022-3468(94)90329-8. [DOI] [PubMed] [Google Scholar]
- [8].Puligandla PS, Grabowski J, Austin M, Hedrick H, Renaud E, Arnold M, et al. Management of congenital diaphragmatic hernia: A systematic review from the APSA outcomes and evidence based practice committee. J Pediatr Surg 2015;50:1958–70. 10.1016/j.jpedsurg.2015.09.010. [DOI] [PubMed] [Google Scholar]
- [9].Peter SD st., Valusek PA, Tsao KJ, Holcomb GW, Ostlie DJ, Snyder CL. Abdominal Complications Related to Type of Repair for Congenital Diaphragmatic Hernia. Journal of Surgical Research 2007;140:234–6. 10.1016/j.jss.2007.03.018. [DOI] [PubMed] [Google Scholar]
- [10].Romao RLP, Nasr A, Chiu PPL, Langer JC. What is the best prosthetic material for patch repair of congenital diaphragmatic hernia? Comparison and meta-analysis of porcine small intestinal submucosa and polytetrafluoroethylene. J Pediatr Surg 2012;47:1496–500. 10.1016/j.jpedsurg.2012.01.009. [DOI] [PubMed] [Google Scholar]
- [11].Saxena AK. Surgical perspectives regarding application of biomaterials for the management of large congenital diaphragmatic hernia defects. Pediatr Surg Int 2018;34:475–89. 10.1007/s00383-018-4253-1. [DOI] [PubMed] [Google Scholar]
- [12].Liao GP, Choi Y, Vojnits K, Xue H, Aroom K, Meng F, et al. Tissue Engineering to Repair Diaphragmatic Defect in a Rat Model. Stem Cells Int 2017;2017. 10.1155/2017/1764523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Xu C, Hong Y. Rational design of biodegradable thermoplastic polyurethanes for tissue repair. Bioact Mater 2022;15:250–71. 10.1016/j.bioactmat.2021.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Punnakitikashem P, Truong D, Menon JU, Nguyen KT, Hong Y. Electrospun biodegradable elastic polyurethane scaffolds with dipyridamole release for small diameter vascular grafts. Acta Biomater 2014;10:4618–28. 10.1016/j.actbio.2014.07.031.Electrospun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].van Loenhout RB, Tibboel D, Post M, Keijzer R. Congenital diaphragmatic hernia: Comparison of animal models and relevance to the human situation. Neonatology 2009;96:137–49. 10.1159/000209850. [DOI] [PubMed] [Google Scholar]
- [16].Lally KP, Cheu HW, Vazquez WD. Prosthetic diaphragm reconstruction in the growing animal. J Pediatr Surg 1993;28:45–7. 10.1016/S0022-3468(05)80352-5. [DOI] [PubMed] [Google Scholar]
- [17].Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods 2012;9:671–5. 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tsai J, Sulkowski J, Adzick NS, Hedrick HL, Flake AW. Patch repair for congenital diaphragmatic hernia: Is it really a problem? J Pediatr Surg 2012;47:637–41. 10.1016/j.jpedsurg.2011.11.054. [DOI] [PubMed] [Google Scholar]
- [19].Fisher JC, Haley MJ, Ruiz-Elizalde A, Stolar CJH, Arkovitz MS. A multivariate model for predicting recurrence in congenital diaphragmatic hernia. J Pediatr Surg 2009;44:1173–80. 10.1016/j.jpedsurg.2009.02.043.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Grethel EJ, Cortes RA, Wagner AJ, Clifton MS, Lee H, Farmer DL, et al. Prosthetic patches for congenital diaphragmatic hernia repair: Surgisis vs Gore-Tex. J Pediatr Surg 2006;41:29–33. 10.1016/j.jpedsurg.2005.10.005. [DOI] [PubMed] [Google Scholar]
- [21].Ross JT, Liang NE, Phelps AS, Squillaro AI, Vu LT. A Novel Thoracic Ultrasound Measurement After Congenital Diaphragmatic Hernia Repair Identifies Decreased Diaphragmatic Excursion Associated With Adverse Respiratory and Surgical Outcomes. Front Pediatr 2021;9:1–7. 10.3389/fped.2021.707052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Steigman SA, Oh JT, Almendinger N, Javid P, Lavan D, Fauza D. Structural and biomechanical characteristics of the diaphragmatic tendon in infancy and childhood: An initial analysis. J Pediatr Surg 2010;45:1455–8. 10.1016/j.jpedsurg.2009.09.030. [DOI] [PubMed] [Google Scholar]
- [23].Pengelly LD, Alderson AM, Milic-Emili J. Mechanics of the diaphragm. J Appl Physiol 1971;30:797–805. 10.1152/jappl.1971.30.6.797. [DOI] [PubMed] [Google Scholar]
- [24].Kim MJ, Druz WS, Danon J, Machnach W, Sharp JT. Mechanics of the canine diaphragm. J Appl Physiol 1976;41:369–82. 10.1152/jappl.1976.41.3.369. [DOI] [PubMed] [Google Scholar]
- [25].Baker BM, Handorf AM, Ionescu LC, Li WJ, Mauck RL. New directions in nanofibrous scaffolds for soft tissue engineering and regeneration. Expert Rev Med Devices 2009;6:515–32. 10.1586/erd.09.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Zhao W, Ju YM, Christ G, Atala A, Yoo JJ, Lee SJ. Diaphragmatic muscle reconstruction with an aligned electrospun poly(ε-caprolactone)/collagen hybrid scaffold. Biomaterials 2013;34:8235–40. 10.1016/j.biomaterials.2013.07.057. [DOI] [PubMed] [Google Scholar]
- [27].Wang B, Sierad LN, Mercuri JJ, Simionescu A, Simionescu DT, Williams LN, et al. Structural and biomechanical characterizations of acellular porcine mitral valve scaffolds: anterior leaflets, posterior leaflets, and chordae tendineae. Engineered Regeneration 2022;3:374–86. 10.1016/j.engreg.2022.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


