Abstract
Background
Sleep deprivation is a condition in which an individual does not get enough sleep, leading to a variety of negative effects on their physical and mental health. In the United States, sleep deprivation is a common problem, with many people not getting the recommended 7-9 hours of sleep per night. Excessive daytime sleepiness is also a common condition in the United States. It is characterized by a persistent feeling of fatigue or drowsiness during the day, despite getting enough sleep at night. The current study aims to document the frequency of sleepiness symptoms amongst the general US population.
Methods
A web-based survey was conducted to assess the frequency of daily anxiety symptoms amongst adults residing in the United States. Questions from the Epworth Sleepiness Scale were used to quantify the burden of daytime sleepiness. JMP 16.0 for Mac OS was used to perform statistical analyses. Our Institutional Review Board gave the study an exempt determination (#2022-569).
Results
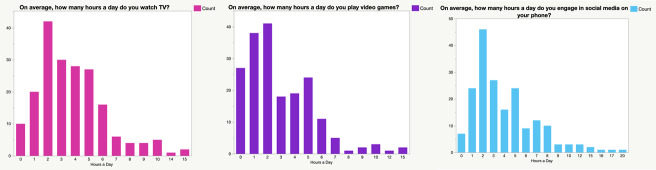
In total, 9% of people qualified as having lower normal daytime sleepiness, 34% qualified as having higher normal daytime sleepiness, 26% qualified as having mild excessive daytime sleepiness, 17% qualified as having moderate excessive daytime sleepiness, and 17% qualified as having severe excessive daytime sleepiness.
Limitations
The present findings are based on cross-sectional survey data.
Conclusion
Although sleep is one of the most crucial bodily activities, our study of young adults found that more than 60% had moderate to severe sleep deprivation/daytime sleepiness as reported on the Epworth Sleepiness scale.
Keywords: Epworth sleepiness scale, daytime sleepiness, sleep deprivation
Introduction
Sleep provides many benefits for both the physical and mental aspect of life, especially for young adults ages 16 through 24 as their brain is still evolving. Sleep is crucial for maintaining a healthy weight, lowering your risk for serious health problems, increasing one’s mood, performing better in school, and making good, cognizant, decisions.1 In young adults, it is very important that they get an adequate amount of sleep since what they learn in this stage of their lives will carry on with them throughout the rest of their careers. The CDC recommends that young adults sleep for between seven and eight hours to be at their peak performance throughout the day.2 However, many factors can hinder young adults from sleeping a sufficient amount. These factors include screen time use, whether they are in the workforce, what time of the day they work, and much more. While indulging in screen time, young adults are actually preventing the release of melatonin in their brains, causing them to not be able to fall asleep.3 This is why it is recommended that young adults shut off their screens at least 30 minutes before their planned bedtime. Employment status also has a major effect on one’s sleep patterns because those who work the early morning shifts or night shifts often have abnormal sleep patterns, which can result in developing excessive daytime sleepiness (EDS). The Sleep Foundation reports that 10% to 20% of Americans experience EDS, and describes EDS as your body telling you that you are not sleeping for an appropriate amount at night.4 The side effects of EDS can be falling asleep multiple times during the day, having a decreased performance in both school and work, having a hard time concentrating, and many more. EDS can also lead to other serious long-lasting illnesses, including depression, schizophrenia, anxiety, cancer, obesity, lupus, multiple sclerosis, Parkinson’s disease, and others.4
There are a multitude of ways to measure daytime sleepiness, one being the Epworth Sleepiness Scale (ESS). The ESS is a validated scale that consists of eight scenarios in which the patient is asked to rate their likelihood of falling asleep under those circumstances on a scale of zero, meaning no chance, to three, meaning a high chance. Once the test has been completed, the patient’s total score is added up and compared on a scale of zero to twenty-four. Where the patient’s score is, relative to the zero to twenty-four scale, determines whether the patient has Lower Normal Daytime Sleepiness, Higher Normal Daytime Sleepiness, Mild Excessive Daytime Sleepiness, Moderate Excessive Daytime Sleepiness, or Severe Excessive Daytime Sleepiness.5 In young adults, the concern is that they have extreme sleep deprivation due to their use of screens and video games, which leads to excessive daytime sleepiness. By conducting a survey on a population of 200 young adults, ages 16 through 24, our objective was to determine the extent of sleep deprivation in young adults, and how they range in the ESS for tiredness.
Methods
Recruitment and Data Collection
This survey polled 200 individuals on sleep quality and sleepiness throughout the day. The inclusion criteria required participants to be between the ages of 16 and 24 years and live in the United States. The survey was completed through an online research platform that uses organic sampling and random device engagement to approve valid responses. These built-in features ensure that each response represents a unique individual and prevents users from completing the survey multiple times using different devices. Over 700 million users are accessible through this research platform.
Statistical analyses
Statistical analyses were performed using JMP Pro 15 for Mac OS. Univariate distributions of age, gender, and region, were weighted. Logistic regression models were built to assess for predictors of sleep deprivation, with a p-value of <0.05 considered statistically significant.
The survey
The survey consisted of 15 questions. Questions 1 through 8 on the survey were the 8 ESS scenarios, and the respondents were given the four ESS test options as their choices. These 8 questions were preceded by “What are the chances of you falling asleep while…”. The next 6 questions were open-ended asking respondents how many hours are spent viewing a digital screen (television, smartphone, video games). The final question was multiple choice with one answer selection and asked participants if they are shift workers along with the timing of their shifts.
Ethical considerations
Our institutional HCA Centralized Algorithms for Research Rules on IRB Exemptions (CARRIE)/ IRB manager issued study exemption number 2022-569.
Results
In our cohort of 200 young adults ranging in age from 16 to 24, the median age was 22, and the interquartile range was 20 to 23. 55.5% were female and 44.5% were male. By race, the cohort was majority white (39%), followed by black (24%), Latino/Latina (19%), Asian (10%), multiracial (5%), and other (4%). While diverse, these values do not reflect the United States 2022 census which showed 75% of people being white and 13% being black. Sixty two percent of the cohort was single, 17% were living with a partner, and 10% were married. The majority (72%) of the survey respondents had 0 children, which was expected due to their younger age. Of those that did have children 14% reported one child, 6% reported two children, 2% had more, and 6% preferred not to disclose.
Of the working respondents, the majority of them had an income on the lower side of the spectrum. Over 50% of participants reported an income of between $0-$49,999, which was expected considering the demographics of our cohort. Due to the fact that we surveyed young adults, it is likely that they were employed in a minimum wage job, if they had a job at all, which means that they would receive a lower income. It is also possible that numerous of them did not have any job at all, taking into consideration that most of them are likely still studying.
The distribution of responses to the ESS is summarized in Table 1.
Table 1. Epworth Sleepiness Scale response distribution.
| ESS Test Questions | Would Never Fall Asleep | Slight Chance of Falling Asleep | Moderate Chance of Falling Asleep | High Chance of Falling Asleep |
|
15.5% | 44% | 24% | 16.5% |
|
10% | 30.5% | 36% | 23.5% |
|
21.5% | 23% | 29% | 26.5% |
|
22.5% | 31% | 27.5% | 19% |
|
4.5% | 18.5% | 32.5% | 44.5% |
|
65.5% | 21.5% | 9.5% | 3.5% |
|
36% | 33.5% | 22.5% | 8% |
|
65.5% | 19% | 9.5% | 6% |
ESS Scores can be interpreted as follows: A score between 0-5 corresponds to lower normal daytime sleepiness; a score between 6-10 indicates normal daytime sleepiness; a score between 11-12 mild indicates excessive daytime symptoms; a score between 13-15 correlates with moderate excessive daytime symptoms, and a score between 16-24 is associated with severe excessive daytime symptoms. The median score in our cohort was 10, with an interquartile range of 7 to 13. This means that most of the respondents had either higher normal daytime sleepiness, mild excessive daytime sleepiness, or moderate excessive daytime sleepiness. Only 9% of participants scored in the lower normal daytime sleepiness category, and 6% scored in the severe excessive daytime sleepiness category (figure 1).
Figure 1. Distribution of Epworth Sleepiness Scale scores.
The participants’ time they went to bed had a broad, 14-hour range, which was from 7 pm to 9 am. However, over 90% of respondents went to sleep between 10 pm and 3 am. Their wake-up time also ranged over a 14-hour time period, from 4 am to 6:30 pm, with most people waking up between 7 am to 10 am. Using the respondent’s bedtime and wake-up time, we calculated their total sleep time. The minimum amount of time slept was 5 hours, and the maximum was 16 hours. The median number of hours asleep was 9 hours, with an interquartile range from 8 to 10 hours.
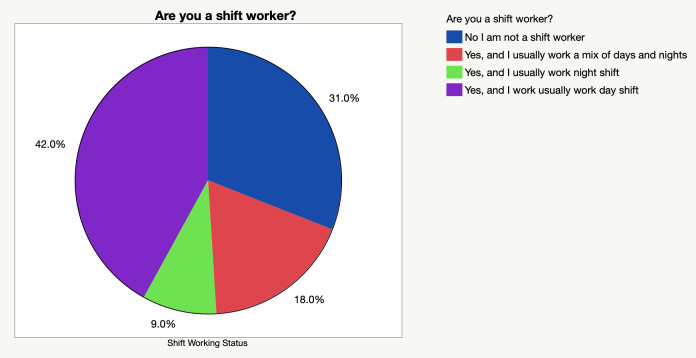
The next three questions asked about screen time. The number of hours participants spent watching TV varied greatly, spanning from 0 hours to 15 hours. Most people fell in the category of spending between 1-5 hours daily. When asked on average how many hours were spent playing video games, the majority (70%) spent between 0-4 hours, although the responses ranged from 0-15 hours. Similarly responses to number of hours spent on social media on their phone ranged from 0-20 hours, with the most frequent response reported as 2 hours (figure 2)
Figure 2. Number of hours per day spent on screen (TV, video games, social media on phone).
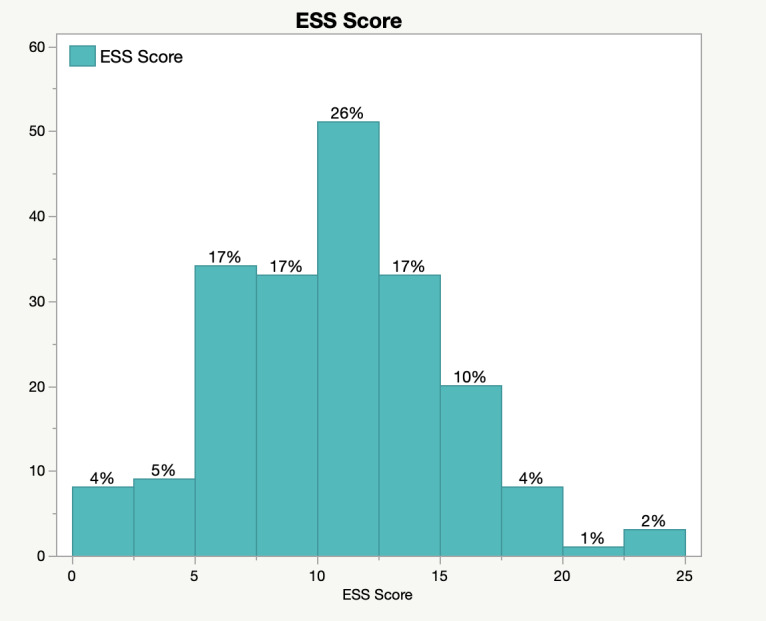
Interestingly 69% of respondents were shift workers (figure 3). 42% of participants said that they usually worked the day shift, 9% said they usually worked the night shift, and 18% said they worked a mixture. We found that whether someone worked the day or night shift greatly affected the times they woke up and went to bed, with those working the night shifts waking up very late and going to bed very early, and those working the day shifts waking up extremely early and going to bed very late. Shift working greatly affects people’s circadian rhythm. This disruption in their sleep cycle causes people to be confused, feeling awake when they should be asleep and feeling exhausted when they should be awake during the day, which can eventually lead the development of EDS. However, we found that the time that the participants used screens per day did not directly affect their ESS score, with some participants that slept the most also having screen time usage in the upper quartile.
Figure 3. Distribution of shift work schedules amongst respondents.
Factors that affect sleepiness using composite score
To better understand overall sleepiness in the cohort, a composite score was calculated by averaging respondents’ answers from 1 (never) to 4 (high chance of falling asleep) across the eight numeric questions that were administered. The composite score was modeled against a variety of demographic factors to quantify their relationship. Marital status (p = 0.544), gender (p = 0.630), race (p = 0.694), age (p = 0.756), and income (p = 0.883) were all statistically insignificant in predicting sleepiness in the sample population.
Participants were asked to disclose the timing of their work shifts, and this information was used to stratify composite scores. These findings are summarized in the table (Table 2), scores range from 1 (lowest) to 4 (highest), and 95% confidence intervals (CI) are 2 standard errors from the mean.
Table 2. Relationship between shift work timing and sleepiness composite score.
| Mean | Std. Error | 95% CI Lower | 95% CI Upper | |
|---|---|---|---|---|
| Day shift | 2.3169 | 0.0593 | 2.1983 | 2.4355 |
| Night shift | 2.6111 | 0.1282 | 2.3547 | 2.8675 |
| Mixture of day and night shift | 2.2639 | 0.0906 | 2.0827 | 2.4451 |
| Non-shift work | 2.2258 | 0.069 | 2.0878 | 2.3638 |
Discussion
Although adequate sleep time is commonly ignored, it is very crucial in the maintenance of a healthy life and overall lifestyle. The CDC accounts that in 2020, 29.7% of adults in the age range of 18 to 24 reported a short sleep duration.6 This can be detrimental to the progression of people’s careers, behavior, and overall health.
To summarize, out of our 200 respondents, 75% of them ranged from ages 20 to 23, their genders were almost an even split, with 55.5% being female and 44.5% being male, the majority were white, most were single, 72% had no children and 26.5% had an income less than $25,000 and 26.0% had an income between $25,000 and $49,999, with the rest of the respondents varying.
The Assistant Secretary for Planning and Evaluations (ASPE) says that the poverty line in 2022 is, when only one person is in the household, $13,590.7 If these respondents lived alone, many of them would fall under this line. According to the National Community Reinvestment Coalition (NCRC), 33.6% of people who qualify as under this poverty line report sleeping less than the adequate amount they should be getting each night.8 Those who fall below the poverty line are more likely to live in areas that make sleeping difficult. These factors could be noise, air, and light pollution, small living quarters, and working long and/or multiple shifts in order to acquire the necessary money they need to live.8 These long, sporadic shifts in one’s circadian rhythm, which is the sleep-wake cycle that everyone experiences that repeats every 48 hours, can greatly affect a person’s performance during their day-to-day life. Depending on the time of shift-workers shifts, they might be required to wake up to work when the circadian drive for alertness is very low, such as very early morning or very late night, and end up sleeping when it is very high, which is usually in the middle of the afternoon. This disrupts the rhythm of when their bodies think they should be awake and asleep, which can cause them to develop sleep disorders, such as EDS.9
The highest percentage of ESS scores was in the range of 10-13, which places these people between mild and moderate excessive daytime sleepiness. However, 46% of respondents reported sleeping for 8–10 hours, which is above what the CDC recommends. On average, these people went to sleep around 10 pm –3 am, and woke up between 7 am and 10 am. In total, 9% of people qualified as having lower normal daytime sleepiness, 34% qualified as having higher normal daytime sleepiness, 26% qualified as having mild excessive daytime sleepiness, 17% qualified as having moderate excessive daytime sleepiness, and 17% qualified as having severe excessive daytime sleepiness.
We found that the supplemental questions asked about screen time usage were not statistically significant, as we found that they were not predictors of having a higher ESS score. This was not expected, as many expect young adults to be getting a lack of sleep due to their normally excessive screen time. However, some of those who reported the most amount of screen usage were those who actually got some of the most amounts of sleep. Dissimilarly, the supplemental question about shift working was statistically significant. We found that those who reported normally working the night shift (9%), and those who worked a mix of the day and night shifts (18%) had a higher chance of dozing off in the daily activities asked in the ESS survey. Shift work, those who worked the night shifts in particular, was a predictor to have higher daytime sleepiness. However, those who reported normally working the day shift (42%) did not seem to suffer the same fate. Those who only usually worked the day shifts did not have a statistically higher chance of getting a higher ESS score.
There are some more questions that we could have asked to get a better understanding of young adults’ sleep. We could have asked if the respondents used some type of sleep aid in order to fall asleep, as that would have let us know if their sleep was partially medically induced, or all-natural. Another question that could have been beneficial is giving a free response box to what makes them choose the time they go to bed. This would let us know why they think they are going to bed at irregular times, whether it is because of homework, their screen usage, their job, an inability to fall asleep, or something else.
Conclusion
Although sleep is one of the most crucial bodily activities, our study of young adults found that more than 60% had moderate to severe sleep deprivation as reported on the Epworth Sleepiness scale. It is important that people get their age group’s recommended amount of sleep to be at their peak performance during their daily routine. Sleeping can help prevent the development of many diseases other than EDS as well, which is why it is influential for all aspects of one’s health.
Author agreement
All authors have seen and approved the final version of this manuscript. This research was approved by an institutional review board, has not been published and is not under consideration for publication elsewhere.
Declaration of Competing Interest
The authors declare no conflicts of interest
Acknowledgments
Acknowledgements
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Office of Disease Prevention and Health Promotion Get Enough Sleep. https://health.gov/myhealthfinder/healthy-living/mental-health-and-relationships/get-enough-sleep
- The National Institute for Occupational Safety and Health NIOSH Training for Nurses on Shift Work and Long Work Hours. http://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod2/08.html
- Cooper Joanna A. Screens and Your Sleep: The Impact of Nighttime Use. http://www.sutterhealth.org/health/sleep/screens-and-your-sleep-the-impact-of-nighttime-use
- Pacheco Danielle. Excessive Sleepiness. http://www.sleepfoundation.org/excessive-sleepiness
- Johns Murray. About the ESS. https://epworthsleepinessscale.com/about-the-ess/
- Sleep and Sleep Disorders. https://www.cdc.gov/sleep/data-and-statistics/adults.html
- Assistant Secretary for Planning and Evaluation U.S. Department of Health and Human Services Poverty Guidelines for 2022. https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines
- Orminski Emily. Sleep Is a Cyclical Inequity for Those in Poverty. https://ncrc.org/sleep-is-a-cyclical-inequity-for-those-in-poverty/
- Shift Work: Disrupted Circadian Rhythms and Sleep—Implications for Health and Well-being. James Stephen M., Honn Kimberly A., Gaddameedhi Shobhan, Van Dongen Hans P.A. Apr 27;2017 Current Sleep Medicine Reports. 3(2):104–112. doi: 10.1007/s40675-017-0071-6. doi: 10.1007/s40675-017-0071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]