Background:
Total knee arthroplasty (TKA) has long been considered the definitive treatment for knee osteoarthritis. Although tremendous improvements have been made in surgical techniques for conventional TKA, a substantial dissatisfaction rate among patients has persisted because of moderate-to-severe pain and stiffness following TKA. Robot-assisted TKA was developed as an alternative to conventional TKA with the goal of improving operative precision and producing better clinical outcomes with minimal postoperative complications. The aim of this study was to compare the radiographic outcomes, duration of surgery, and complication rate between robot-assisted TKA and conventional TKA.
Methods:
We conducted relevant literature searches of Medline, Scopus, ClinicalTrials.gov, and the Cochrane Library databases with use of specific keywords. The outcomes for continuous variables were pooled into mean differences, whereas the outcomes for dichotomous variables were pooled into odds ratios with 95% confidence intervals with use of random-effects models.
Results:
A total of 12 randomized clinical trials were included. Our pooled analysis revealed that robot-assisted TKA was associated with fewer outliers in the hip-knee-ankle (HKA) angle (p < 0.0001), femoral component (coronal) angle (p = 0.0006), femoral component (sagittal) angle (p = 0.009), tibial component (coronal) angle (p = 0.05), and tibial component (sagittal) angle (p = 0.01) when compared with conventional TKA. The postoperative HKA angle was also significantly more neutral in the robot-assisted TKA group (mean difference, −0.77°; p < 0.0001). However, the complication rate did not differ significantly between the 2 groups.
Conclusions:
Robot-assisted TKA may produce more accurate placement of the prosthetic component and better joint alignment accuracy than conventional TKA as shown by fewer outliers in several joint angles.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
Osteoarthritis (OA) is the most common type of arthritis encountered in daily clinical practice1. OA is caused by a degenerative process within the joint resulting from mechanical damage and inflammation in the cartilage and most commonly occurs in the knee1. The global prevalence of knee OA is estimated to be 16% among individuals aged ≥15 years and 22.9% among individuals aged ≥40 years2. Although knee OA does not directly result in death, the pain and limitations of daily activities that result from this disease can reduce quality of life3.
Management of knee OA generally involves symptomatic therapy with painkillers combined with physiotherapy or rehabilitation programs4,5. In situations in which knee OA does not respond to drug therapy or physiotherapy, as well as in advanced stages of knee OA, the main modality for reducing pain and restoring joint function is a surgical procedure such as total knee arthroplasty (TKA)5. Although TKA is the definitive treatment for knee OA, studies have demonstrated a substantial rate of patient dissatisfaction (approximately 20%) postoperatively6,7. Limited knee function and persistent moderate-to-severe pain and stiffness following TKA can contribute to patient dissatisfaction6,7. In addition, TKA has been associated with several complications, such as joint instability, that can arise postoperatively as a result of improper placement of the prosthetic components6,7. Therefore, to overcome these problems, new technologies continue to be developed. Robot-assisted TKA, for example, was developed with the aim of increasing the precision of prosthetic component placement and alignment in order to improve postoperative knee function and minimize postoperative pain and stiffness8. Unfortunately, randomized trials have had conflicting results regarding robot-assisted TKA. Song et al.9 reported that robot-assisted TKA was associated with better clinical outcomes (specifically, higher postoperative knee scores and greater range of motion) and better radiographic results (specifically, improved alignment accuracy and fewer outliers) compared with conventional TKA. In contrast, Liow et al.10 found no difference in functional outcomes between robot-assisted TKA and conventional TKA even though robot-assisted TKA was associated with a significant decrease in mechanical axis outliers. The purpose of the present systematic review and meta-analysis was to summarize the evidence from randomized clinical trials (RCTs) in order to compare the radiographic outcomes, duration of surgery, and complication rate between robot-assisted TKA and conventional TKA.
Materials and Methods
Eligibility Criteria
This review was written in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and the Cochrane Handbook guidelines11,12. A study was included if it met the following criteria, which are presented in the PICO (Population, Intervention, Control, and Outcomes) format. The population (P) was patients with knee OA who were candidates for surgical therapy in the form of TKA. The intervention (I) was TKA carried out with robot assistance (robot-assisted TKA). The control (C) was TKA procedures carried out manually, or conventionally (conventional TKA). The outcomes (O) were the duration of surgery, the rate of complications, and radiographic outcomes (as described below). In addition, all included studies were randomized trials.
Studies were excluded if they met ≥1 of the following criteria: (1) the population consisted of patients undergoing unicompartmental knee arthroplasty (UKA), (2) a comparison group was not utilized, (3) the study was not available in full-text format (i.e., it was available as an abstract only), and (4) the study was not an RCT.
Literature Search and Study Selection
A comprehensive search of 4 databases, Medline, Scopus, Cochrane Library, and ClinicalTrials.gov, for all literature in the English language published on or before January 5, 2023, was conducted independently by 2 authors. The following keywords were used to obtain relevant literature: “(robot OR robotic OR robot-assisted OR robot arm-assisted) AND (conventional OR manual OR non-robotic) AND (total knee arthroplasty OR TKA OR total knee replacement OR TKR) AND (clinical trials OR randomized trials OR RCT).” Two authors independently screened articles on the basis of the title and/or abstract and removed duplicates. For articles that passed the title and/or abstract screening, these 2 authors also performed a full-text assessment of study eligibility based on the inclusion criteria. All discrepancies were resolved through discussion. If there were ≥2 articles by the same author in which the same outcome was reported, the most recent article with the longest follow-up duration was included. However, if completely different outcomes were reported, then both articles were included for data analysis purposes.
Data Extraction and Quality Assessment
The data extraction process was carried out independently by 2 authors. Data were tabulated with use of Microsoft Excel 2019. The following data were extracted: author names, year of publication, study design, number of samples, baseline characteristics of study participants, robotic system utilized for robot-assisted TKA, robotic system manufacturer, prosthesis utilized for TKA, prosthesis manufacturer, and the outcome of interest in the form of radiographic outcomes, the duration of surgery, and the complication rate.
The outcomes of interest in this review were divided into 3 categories: duration of surgery, complication rate, and radiographic outcomes. Radiographic outcomes consisted of the hip-knee-ankle (HKA) angle, the femoral component (coronal) (FCC) angle, the femoral component (sagittal) (FCS) angle, the tibial component (coronal) (TCC) angle, the tibial component (sagittal) (TCS) angle, and the number of outliers (>±3°) for each angle. For the HKA angle outcome, we calculated the difference between the postoperative scores (i.e., at the latest follow-up) and preoperative scores. For outcomes related to the FCC angle, FCS angle, TCC angle, and TCS angle, we only calculated the postoperative values.
The same 2 authors also performed a risk of bias assessment of the included RCTs with use of the Risk of Bias 2 tool (RoB v2; The Cochrane Collaboration). This tool consists of a methodological assessment of 5 domains: (1) randomization process, (2) deviations from the intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported results. Studies were categorized as having “low risk,” “high risk,” or “some concerns” of bias.
Statistical Analysis
Mean differences and 95% confidence intervals (95% CIs) were computed with use of the inverse-variance formula to compare the continuous variable outcomes between the intervention group and the control group. Dichotomous variable outcomes were computed as odds ratios (ORs) and 95% CIs with use of the Mantel-Haenszel formula. The level of significance was set at p < 0.05. Random-effects models were chosen with the expectation that significant heterogeneity would result from differences between the studies regarding the characteristics of the study population, the duration of follow-up, and the robotic system or prosthesis that was utilized. The heterogeneity between studies was assessed with use of the I-squared (I2) statistic. I2 values of ≤25%, 26% to 50%, and >50% were categorized as low, moderate, and high heterogeneity, respectively. A combination of formulas from Luo et al.13 and Wan et al.14 was utilized to convert data expressed as the median and interquartile range or as the median, minimum, and maximum to the mean and the standard deviation (SD) for the purposes of the pooled analysis. A publication bias analysis was performed for each outcome of interest for which >10 studies were utilized. All statistical analyses were carried out with use of Review Manager 5.4 (The Cochrane Collaboration).
Results
Study Selection and Characteristics
A literature search of Scopus, Medline, Cochrane Library, and ClinicalTrials.gov yielded a total of 166 studies. One hundred and twenty-two articles were found to be duplicates on the basis of a review of their titles and abstracts and were excluded. The full-text version of the remaining 44 articles was assessed for eligibility; of these, 32 were excluded for the following reasons: 10 were not RCTs, 8 did not have data on the specified outcomes of interest, 8 were review articles, 3 included UKAs only, 2 did not have a control group, and 1 was not published in the English language. Ultimately, 12 RCTs15-26 with a total of 2,591 patients with knee OA were included in the final analysis (Fig. 1). Of these 12 RCTs, 10 were prospective and 2 were retrospective. Sample sizes of the included RCTs ranged from 33 to 1,348 patients. The study follow-up period ranged from 3 months to 13.5 years. Among the included trials, the most common robotic system was ROBODOC + ORTHODOC (pre-planning) from CUREXO and the most common prosthesis was the NextGen PS implant from Zimmer Biomet. Further details regarding the baseline characteristics of the included RCTs are shown in Table I.
Fig. 1.
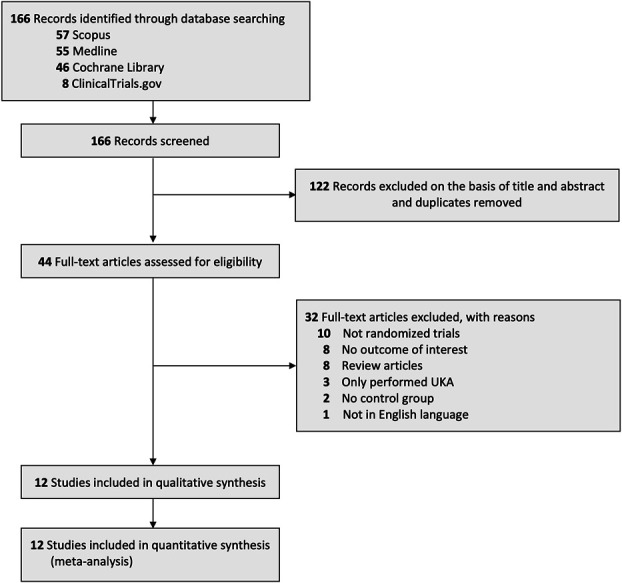
PRISMA diagram illustrating the process for selecting studies for inclusion in the present systematic review and meta-analysis.
TABLE I.
Characteristics of the Included Studies*
| Study | Study Design | Study Population | Mean Follow-up | Robotic System | Robotic System Manufacturer | Prosthesis | Prosthesis Manufacturer | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (no. of knees) | Age† (yr) | Male Sex (%) | BMI† (kg/m2) | |||||||
| Banger MS et al.15 (2020) | Prospective RCT | 70 | 69.7 ± 7.4 | 47.1% | 32.2 ± 12.1 | N/A | MAKO system | Stryker | Restoris MCK fixed-bearing onlay implant | Stryker |
| Blyth MJG et al.16 (2021) | Prospective RCT | 76 | 69.6 ± 7.3 | 50% | 32.5 ± 6.6 | 1 yr | MAKO system | Stryker | Restoris MCK fixed-bearing onlay implant | Stryker |
| Cho KJ et al.17 (2019) | Retrospective RCT | 390 | 67.8 ± 4.4 | 12% | N/A | 11 yr | ROBODOC + ORTHODOC (pre-planning) | CUREXO | NexGen CR & PS implants | Zimmer Biomet |
| Winnock de Grave P et al.18 (2022) | Retrospective RCT | 80 | 67.9 ± 9.6 | 36.2% | 30.1 ± 5.1 | 1 yr | MAKO system | Stryker | Triathlon TKA implant | Stryker |
| Kim YH et al.19 (2020) | Prospective RCT | 1,448 | 60.5 ± 7.5 | 20.4% | 28.5 ± 8.5 | 13.5 yr | ROBODOC + ORTHODOC (pre-planning) | Integrated Surgical Technology | Duracon posterior cruciate-substituting total knee prosthesis | Stryker |
| Liow MHL et al.20 (2017) | Prospective RCT | 60 | N/A | N/A | N/A | 2 yr | ROBODOC + ORTHODOC (pre-planning) | CUREXO | NexGen LPS-Flex PS implant | Zimmer Biomet |
| Li Z et al.21 (2022) | Prospective RCT | 150 | 68.5 ± 7 | 18.7% | 27.2 ± 3.3 | 3 mo | Legion system + HURWA TKA system | Smith & Nephew, BEIJING HURWA-ROBOT Technology | LEGION PS implant | Smith & Nephew |
| Song EK et al.22 (2013) | Prospective RCT | 100 | 65.4 ± 6.2 | 9% | 26.2 ± 3.3 | 5.4 yr | ROBODOC + ORTHODOC (pre-planning) | CUREXO | NexGen LPS-Flex PS implant | Zimmer Biomet |
| Thiengwittayaporn S et al.23 (2021) | Prospective RCT | 152 | 69 ± 7.7 | 13.8% | 27.8 ± 4.7 | N/A | NAVIO system | Smith & Nephew | LEGION PS implant | Smith & Nephew |
| Vaidya NV et al.24 (2022) | Prospective RCT | 60 | 61.1 ± 9.1 | 20% | 27.4 ± 4 | N/A | NAVIO system | Smith & Nephew | ANTHEM PS implant | Smith & Nephew |
| Xu J et al.25 (2022) | Prospective RCT | 72 | 63.9 ± 6.2 | 25% | 26.3 ± 3.4 | 3 mo | Surgical-assist system | YUANHUA-TKA | Fixed-platform & PCL sacrificing implant | Unique Knee |
| Xu Z et al.26 (2022) | Prospective RCT | 33 | 66.9 ± 3.5 | 18.2% | 25.5 ± 3 | 3 mo | Surgical-assist system | YUANHUA-TKA | Standard PS implant | Unique Knee |
BMI = body mass index, CR = cruciate-retaining, N/A = not available, PCL = posterior cruciate ligament, PS = posterior-stabilized, RCT = randomized clinical trial, TKA = total knee arthroplasty. †Data are presented as the mean and the standard deviation.
Assessment of Study Quality
With use of the RoB tool, we found that only 3 RCTs16,22,23 had a “low risk” of bias in all 5 assessment domains. Seven15,17,18,21,24-26 of the 12 RCTs were judged to have “some concerns” of bias for the following reasons: all 7 had “some concerns” of bias in the randomization process (because the allocation-concealment methods following the randomization process were not described and therefore we could not be sure that the allocations were concealed), and 4 studies15,17,18,24 also had “some concerns” of bias in the measurement of the outcome (because the studies did not provide enough information regarding whether the outcome measurement was performed in a blinded fashion). The remaining 2 RCTs19,20 were judged to have a “high risk” of bias. Of these 2 studies, 1 RCT19 did not have allocation concealment following randomization and there were no differences in the baseline characteristics of participants, which suggested that there could have been problems during randomization (i.e., “some concerns” of bias in the randomization process). Moreover, the outcome measurement was not blinded, which may have caused a biased assessment of the results (i.e., a “high risk” of bias in the outcome measurement). The other RCT20 did not have allocation concealment following randomization, nor did it provide data regarding the baseline characteristics of the participants (i.e., a “high risk” of bias in the randomization process). Additionally, the outcome measurement was not performed in a blinded fashion (i.e., a “high risk” of bias in the outcome measurement). A summary of the risk of bias assessment is presented in Table II.
TABLE II.
Risk of Bias Assessment of the Included Studies with Use of the RoB v2 Tool*
| Study | Randomization Process | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall |
|---|---|---|---|---|---|---|
| Banger MS et al.15 (2020) | ? | + | + | ? | + | ? |
| Blyth MJG et al.16 (2021) | + | + | + | + | + | + |
| Cho KJ et al.17 (2019) | ? | + | + | ? | + | ? |
| Winnock de Grave P et al.18 (2022) | ? | + | + | ? | + | ? |
| Kim YH et al.19 (2020) | ? | + | + | − | + | − |
| Liow MHL et al.20 (2017) | − | + | + | − | + | − |
| Li Z et al.21 (2022) | ? | + | + | + | + | ? |
| Song EK et al.22 (2013) | + | + | + | + | + | + |
| Thiengwittayaporn S et al.23 (2021) | + | + | + | + | + | + |
| Vaidya NV et al.24 (2022) | ? | + | + | ? | + | ? |
| Xu J et al.25 (2022) | ? | + | + | + | + | ? |
| Xu Z et al.26 (2022) | ? | + | + | + | + | ? |
Low risk of bias is represented with “+”; some concerns of bias, with “?”; and high risk of bias, with “−”.
Duration of Surgery
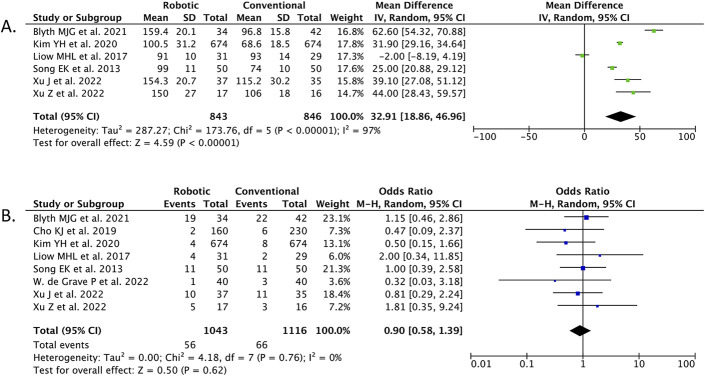
Our pooled analysis of 6 RCTs (n = 1,689) demonstrated that robot-assisted TKA was associated with a longer duration of surgery than conventional TKA (mean difference, 32.91 minutes [95% CI, 18.86 to 46.96]; p < 0.00001; I2 = 97%) (Fig. 2-A).
Fig. 2.
Forest plots demonstrating the comparison between robot-assisted TKA and conventional TKA in terms of the duration of surgery (Fig. 2-A) and the rate of complications (Fig. 2-B). M-H = Mantel-Haenszel, IV = inverse variance, df = degrees of freedom.
Complication Rate
Our meta-analysis of 8 RCTs (n = 2,159) showed that the complication rate did not differ significantly between the robot-assisted TKA and conventional TKA groups (OR, 0.90 [95% CI, 0.58 to 1.39]; p = 0.62; I2 = 0%) (Fig. 2-B).
Radiographic Outcomes
HKA Angle
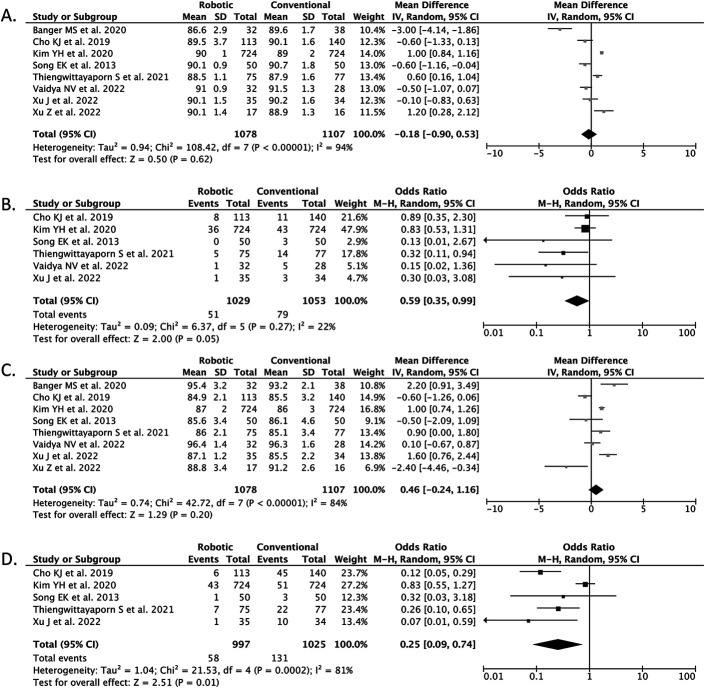
Our meta-analysis of 9 RCTs (n = 2,335) showed that the postoperative HKA angle was significantly more neutral in the robot-assisted TKA group than in the conventional TKA group (mean difference, −0.77° [95% CI, −1.11 to −0.43]; p < 0.0001; I2 = 60%) (Fig. 3-A).
Fig. 3.
Forest plots demonstrating the comparison between robot-assisted TKA and conventional TKA in terms of HKA angle (Fig. 3-A), HKA angle outliers (Fig. 3-B), FCC angle (Fig. 3-C), FCC angle outliers (Fig. 3-D), FCS angle (Fig. 3-E), and FCS angle outliers (Fig. 3-F). M-H = Mantel-Haenszel, IV = inverse variance, df = degrees of freedom.
HKA Angle Outliers
Our meta-analysis of 8 RCTs (n = 2,258) showed that robot-assisted TKA was associated with significantly fewer HKA angle outliers when compared with conventional TKA (OR, 0.36 [95% CI, 0.22 to 0.58]; p < 0.0001; I2 = 37%) (Fig. 3-B).
FCC Angle
Our meta-analysis of 8 RCTs (n = 2,185) showed that the mean postoperative FCC angle did not differ significantly between the robot-assisted TKA and conventional TKA groups (mean difference, 0.33° [95% CI, −0.29 to 0.95]; p = 0.29; I2 = 90%) (Fig. 3-C).
FCC Angle Outliers
Our meta-analysis of 6 RCTs (n = 2,082) showed that robot-assisted TKA was associated with significantly fewer FCC angle outliers when compared with conventional TKA (OR, 0.50 [95% CI, 0.34 to 0.75]; p = 0.0006; I2 = 0%) (Fig. 3-D).
FCS Angle
Our meta-analysis of 8 RCTs (n = 2,185) showed that the mean postoperative FCS angle did not differ significantly between robot-assisted TKA and conventional TKA (mean difference, −0.75° [95% CI, −1.90 to 0.40]; p = 0.20; I2 = 98%) (Fig. 3-E).
FCS Angle Outliers
Our meta-analysis of 5 RCTs (n = 2,022) showed that robot-assisted TKA was associated with significantly fewer FCS angle outliers when compared with conventional TKA (OR, 0.24 [95% CI, 0.08 to 0.69]; p = 0.009; I2 = 79%) (Fig. 3-F).
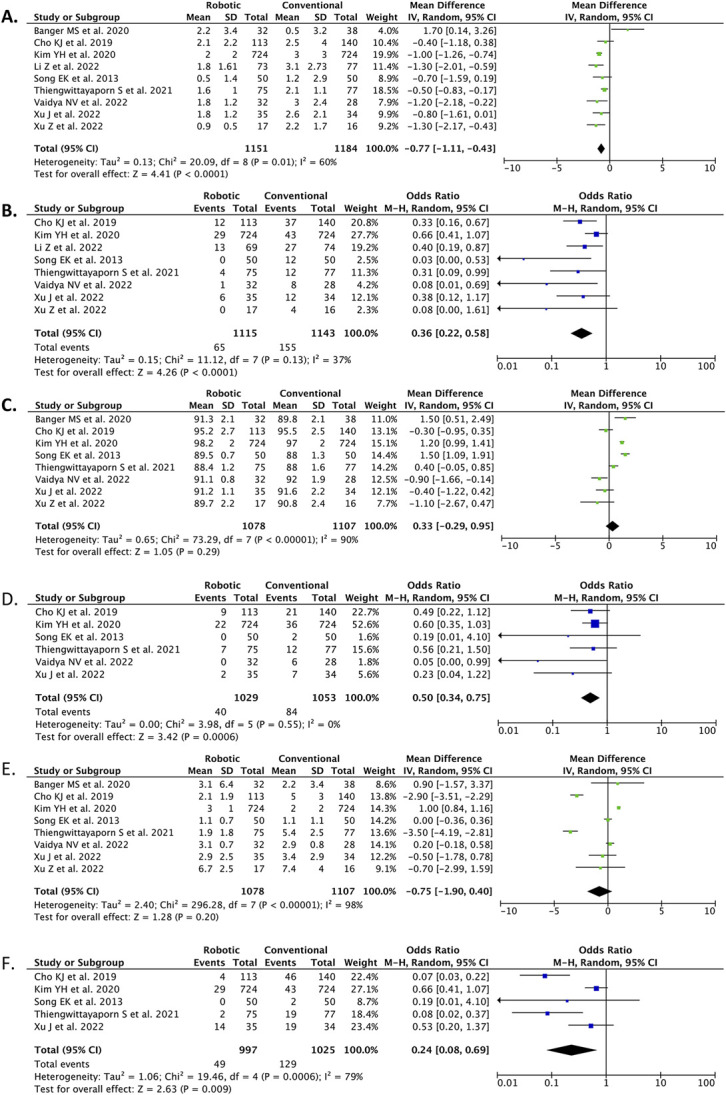
TCC Angle
Our meta-analysis of 8 RCTs (n = 2,185) showed that the mean postoperative TCC angle did not differ significantly between robot-assisted TKA and conventional TKA (mean difference, −0.18° [95% CI, −0.90 to 0.53]; p = 0.62; I2 = 94%) (Fig. 4-A).
Fig. 4.
Forest plots demonstrating the comparison between robot-assisted TKA and conventional TKA in terms of TCC angle (Fig. 4-A), TCC angle outliers (Fig. 4-B), TCS angle (Fig. 4-C), and TCS angle outliers (Fig. 4-D). M-H = Mantel-Haenszel, IV = inverse variance, df = degrees of freedom.
TCC Angle Outliers
Our meta-analysis of 6 RCTs (n = 2,082) showed that robot-assisted TKA was associated with significantly fewer TCC angle outliers when compared with conventional TKA (OR, 0.59 [95% CI, 0.35 to 0.99]; p = 0.05; I2 = 22%) (Fig. 4-B).
TCS Angle
Our meta-analysis of 8 RCTs (n = 2,185) showed that the mean postoperative TCS angle did not differ significantly between robot-assisted TKA and conventional TKA (mean difference, 0.46° [95% CI, −0.24 to 1.16]; p = 0.20; I2 = 84%) (Fig. 4-C).
TCS Angle Outliers
Our meta-analysis of 5 RCTs (n = 2,022) showed that robot-assisted TKA was associated with significantly fewer TCS angle outliers when compared with conventional TKA (OR, 0.25 [95% CI, 0.09 to 0.74]; p = 0.01; I2 = 81%) (Fig. 4-D).
Publication Bias
The number of studies for each outcome of interest in this review was <10. Because funnel plots and statistical tests to detect publication bias are less reliable for sample sizes of <1027,28, a publication bias analysis was not performed in this study.
Discussion
The results of our meta-analysis showed that robot-assisted TKA was associated with a longer duration of surgery than conventional TKA. Furthermore, the rate of complications did not differ significantly between the 2 intervention groups.
However, robot-assisted TKA had an advantage over conventional TKA in terms of increased accuracy and precision as indicated by a more neutral postoperative HKA angle and by fewer outliers in the FCC, FCS, TCC, and TCS angles.
Although robot-assisted TKA had better radiographic outcomes than conventional TKA, it was not superior to conventional TKA with regard to the duration of surgery or the rate of complications. Nonetheless, robot-assisted TKA still has the potential to provide considerable clinical benefit. Hence, additional studies with a longer duration of follow-up are needed to elucidate the benefit and efficacy of robot-assisted TKA.
The results of our meta-analysis are comparable to those of a previous meta-analysis on a similar topic by Onggo et al., who concluded that robot-assisted TKA is capable of achieving better alignment in several axes as demonstrated by the smaller number of outliers associated with robot-assisted TKA. However, there are several substantial differences between our study and that of Onggo et al.29.
Onggo et al.29 included a total of 18 studies in their final analysis, consisting of 6 RCTs, 4 prospective cohort studies, 5 retrospective cohort studies, 2 case-control studies, and 1 economic analysis. Combining the results from different study designs into a meta-analysis is not recommended because it has the potential to generate misleading results30,31. Nonrandomized studies, such as cohort, case-control, or case-series studies, are very likely to be affected by various biases, such as selection bias and information bias, which can diminish the validity of the results obtained30-32. In addition, the results of nonrandomized studies are influenced by several confounding factors that may not have been addressed in the study30-32. In contrast, RCTs are minimally biased because (1) the process of recruiting participants is carried out randomly and in a concealed manner, (2) it is possible to provide therapy in a blinded manner, and (3) the assessment of outcomes is also carried out independently and in a blinded manner so that the results obtained are more valid and reliable33,34. RCTs also address as many existing confounders as possible so that there are usually no significant differences in baseline characteristics33,34. In our meta-analysis, we included only 12 RCTs in the final analysis so that the results that we obtained would be more valid and reliable.
One concern that may be raised is that robot-assisted TKA is just a proxy for computer-navigated TKA. Recent technological advances have led to the development of computer-navigated and robot-assisted techniques for TKA surgery35. Computer-navigated TKA involves the use of a device with an interface that allows anatomical data to be entered; the device then gives feedback to the surgeon regarding implant alignment and overall knee alignment but cannot be programmed to perform a task35. Computer-navigated TKA is most often utilized as an image-free modality35. The anatomical landmarks of the patient are collected intraoperatively and used to create a reference frame, according to which the knee and cutting jig can be positioned35.
Robotic systems generally provide feedback similar to that of computer navigation but can be programmed to assist in the execution of certain surgical tasks36. An intraoperative robotic device helps the surgeon to execute the preoperative patient-specific plan with a high level of accuracy36. The action of the sawblade is limited to the preoperative surgical plan for femoral and tibial resection, thereby limiting the risk of iatrogenic periarticular soft-tissue injury and bone trauma37.
Several studies have demonstrated the advantages of robot-assisted TKA over computer-navigated TKA. The precision and accuracy of robotic technology has been shown to allow better alignment and positioning of implant components, which reduces the likelihood of complications such as implant loosening, wear and tear, and the need for revision surgery36,37. Buchlak et al.38 found that robot-assisted TKA was associated with a shorter operative duration, a higher likelihood of achieving the target alignment, and a shorter length of stay than computer-navigated TKA. A critical analysis review showed that robot-assisted TKA provided more accurate and precise implant positioning, potentially leading to better long-term outcomes39. Similarly, another review concluded that robot-assisted TKA was superior to computer-navigated TKA in terms of the accuracy and precision of implant placement, with a significantly lower rate of outliers40. Some robot-assisted TKA systems are designed to prevent deviations from the surgical plan by incorporating haptic feedback41. Moreover, 1 study demonstrated that robotic systems reduced the learning curve of certain orthopaedic procedures without increasing risk to patients42.
However, the high cost of robotic systems is a considerable concern for health-care practitioners and systems. Although robotic systems may offer advantages such as improved accuracy and potentially better clinical outcomes, they also come at a higher cost43,44. However, studies have shown that robot-assisted TKA may be more cost-effective than conventional TKA when the number of annual cases is >9443,44. Robot-assisted TKA also has been associated with lower 90-day episode-of-care costs than conventional TKA45.
Ultimately, although robot-assisted TKA has had promising results, additional long-term follow-up studies are needed to fully assess the benefits and cost-effectiveness of robot-assisted TKA versus conventional TKA.
Our study had some limitations. Notable heterogeneities were identified in some of the outcomes of interest in our study, which could have been caused by differences in the baseline characteristics of study participants and differences in the robotic system or the prosthesis that was utilized in each RCT. The total number of participants in most of the RCTs was also relatively small (∼100 patients), so we cannot be certain that the same results can also be obtained in a larger patient population. Finally, data regarding the total cost of robot-assisted TKA were lacking in the included studies and thus we were unable to analyze cost. The high cost of robot-assisted TKA is still a major concern related to the use of this method for the treatment of knee OA.
Our systematic review and meta-analysis suggested that robot-assisted TKA may result in better accuracy and joint alignment when compared with conventional TKA as demonstrated by fewer outliers in each joint angle that was measured. However, the complication rate was similar between the 2 intervention groups.
Footnotes
Investigation performed at Siloam Hospitals Lippo Village, Tangerang, Indonesia
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A518).
Contributor Information
Albert Riantho, Email: albertriantho@yahoo.com.
Kevin Fidiasrianto, Email: kev_fid@yahoo.com.
Elson Elson, Email: elsonn@outlook.com.
Irvan Irvan, Email: irvan.md@outlook.com.
Handy Haryono, Email: handyharyono@yahoo.com.
Jeremy Nathan Prasetio, Email: Ronald.A.Navarro@kp.org.
References
- 1.Quicke JG, Conaghan PG, Corp N, Peat G. Osteoarthritis year in review 2021: epidemiology & therapy. Osteoarthritis Cartilage. 2022 Feb;30(2):196-206. [DOI] [PubMed] [Google Scholar]
- 2.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020 Nov 26;29-30:100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, Hawker GA, Henrotin Y, Hunter DJ, Kawaguchi H, Kwoh K, Lohmander S, Rannou F, Roos EM, Underwood M. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014 Mar;22(3):363-88. [DOI] [PubMed] [Google Scholar]
- 5.Katz JN, Arant KR, Loeser RF. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021 Feb 9;325(6):568-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakano N, Shoman H, Olavarria F, Matsumoto T, Kuroda R, Khanduja V. Why are patients dissatisfied following a total knee replacement? A systematic review. Int Orthop. 2020 Oct;44(10):1971-2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J Arthroplasty. 2017 Dec;32(12):3854-60. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqi A, Horan T, Molloy RM, Bloomfield MR, Patel PD, Piuzzi NS. A clinical review of robotic navigation in total knee arthroplasty: historical systems to modern design. EFORT Open Rev. 2021 Apr 1;6(4):252-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2011 Jul;19(7):1069-76. [DOI] [PubMed] [Google Scholar]
- 10.Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014 Dec;29(12):2373-7. [DOI] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011. Accessed 2023 April 4. www.handbook.cochrane.org [Google Scholar]
- 13.Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018 Jun;27(6):1785-805. [DOI] [PubMed] [Google Scholar]
- 14.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014 Dec 19;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banger MS, Johnston WD, Razii N, Doonan J, Rowe PJ, Jones BG, MacLean AD, Blyth MJG. Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: a prospective randomized controlled trial. Bone Joint J. 2020 Nov;102-B(11):1511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blyth MJG, Banger MS, Doonan J, Jones BG, MacLean AD, Rowe PJ. Early outcomes after robotic arm-assisted bi-unicompartmental knee arthroplasty compared with total knee arthroplasty: a prospective, randomized controlled trial. Bone Joint J. 2021 Oct;103-B(10):1561-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho KJ, Seon JK, Jang WY, Park CG, Song EK. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop. 2019 Jun;43(6):1345-54. [DOI] [PubMed] [Google Scholar]
- 18.Winnock de Grave P, Kellens J, Tampere T, Vermue H, Luyckx T, Claeys K. Clinical outcomes in TKA are enhanced by both robotic assistance and patient specific alignment: a comparative trial in 120 patients. Arch Orthop Trauma Surg. 2022 Oct 3. [DOI] [PubMed] [Google Scholar]
- 19.Kim YH, Yoon SH, Park JW. Does Robotic-assisted TKA Result in Better Outcome Scores or Long-Term Survivorship Than Conventional TKA? A Randomized, Controlled Trial. Clin Orthop Relat Res. 2020 Feb;478(2):266-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017 Sep;25(9):2942-51. [DOI] [PubMed] [Google Scholar]
- 21.Li Z, Chen X, Wang X, Zhang B, Wang W, Fan Y, Yan J, Zhang X, Zhao Y, Lin Y, Liu J, Lin J. HURWA robotic-assisted total knee arthroplasty improves component positioning and alignment - A prospective randomized and multicenter study. J Orthop Translat. 2022 Feb 16;33:31-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013 Jan;471(1):118-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiengwittayaporn S, Uthaitas P, Senwiruch C, Hongku N, Tunyasuwanakul R. Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. Int Orthop. 2021 Nov;45(11):2851-8. [DOI] [PubMed] [Google Scholar]
- 24.Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P. Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2022 Feb;30(2):621-6. [DOI] [PubMed] [Google Scholar]
- 25.Xu J, Li L, Fu J, Xu C, Ni M, Chai W, Hao L, Zhang G, Chen J. Early Clinical and Radiographic Outcomes of Robot-Assisted Versus Conventional Manual Total Knee Arthroplasty: A Randomized Controlled Study. Orthop Surg. 2022 Sep;14(9):1972-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu Z, Li H, Liu Z, Li J, Zhang J, Wang M, Zhang Y. Robot-assisted surgery in total knee arthroplasty: trauma maker or trauma savior? A prospective, randomized cohort study. Burns Trauma. 2022 Sep 16;10:tkac034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thornton A, Lee P. Publication bias in meta-analysis: its causes and consequences. J Clin Epidemiol. 2000 Feb;53(2):207-16. [DOI] [PubMed] [Google Scholar]
- 28.Terrin N, Schmid CH, Lau J, Olkin I. Adjusting for publication bias in the presence of heterogeneity. Stat Med. 2003 Jul 15;22(13):2113-26. [DOI] [PubMed] [Google Scholar]
- 29.Onggo JR, Onggo JD, De Steiger R, Hau R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg. 2020 Oct;140(10):1533-49. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3. 2022. Accessed 2023 April 4. www.training.cochrane.org/handbook [Google Scholar]
- 31.Mueller M, D’Addario M, Egger M, Cevallos M, Dekkers O, Mugglin C, Scott P. Methods to systematically review and meta-analyse observational studies: a systematic scoping review of recommendations. BMC Med Res Methodol. 2018 May 21;18(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Delgado-Rodríguez M, Llorca J. Bias. J Epidemiol Community Health. 2004 Aug;58(8):635-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hariton E, Locascio JJ. Randomised controlled trials - the gold standard for effectiveness research: Study design: randomised controlled trials. BJOG. 2018 Dec;125(13):1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaptchuk TJ. The double-blind, randomized, placebo-controlled trial: gold standard or golden calf? J Clin Epidemiol. 2001 Jun;54(6):541-9. [DOI] [PubMed] [Google Scholar]
- 35.Figueroa PD, Fritsch B, Oussedik S. New and evolving technologies for knee arthroplasty-computer navigation and robotics: state of the art. J Clin Orthop Trauma. 2019 Mar-Apr;10(2):283-7. [Google Scholar]
- 36.Kayani B, Haddad FS. Robotic total knee arthroplasty: clinical outcomes and directions for future research. Bone Joint Res. 2019 Nov 2;8(10):438-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khlopas A, Chughtai M, Hampp EL, Scholl LY, Prieto M, Chang TC, Abbasi A, Bhowmik-Stoker M, Otto J, Jacofsky DJ, Mont MA. Robotic-arm assisted total knee arthroplasty demonstrated soft tissue protection. Surg Technol Int. 2017 Jul 25;30:441-6. [PubMed] [Google Scholar]
- 38.Buchlak QD, Clair J, Esmaili N, Barmare A, Chandrasekaran S. Clinical outcomes associated with robotic and computer-navigated total knee arthroplasty: a machine learning-augmented systematic review. Eur J Orthop Surg Traumatol. 2022 Jul;32(5):915-31. [DOI] [PubMed] [Google Scholar]
- 39.Mancino F, Jones CW, Benazzo F, Singlitico A, Giuliani A, De Martino I. Where are We Now and What are We Hoping to Achieve with Robotic Total Knee Arthroplasty? A Critical Analysis of the Current Knowledge and Future Perspectives. Orthop Res Rev. 2022 Oct 17;14:339-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mullaji AB, Khalifa AA. Is it prime time for robotic-assisted TKAs? A systematic review of current studies. J Orthop. 2022 Aug 8;34:31-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty. 2016 Oct;31(10):2353-63. [DOI] [PubMed] [Google Scholar]
- 42.Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. 2018 Aug;100-B(8):1033-42. [DOI] [PubMed] [Google Scholar]
- 43.Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective: a markov decision analysis. Bone Joint J. 2019 Sep;101-B(9):1063-70. [DOI] [PubMed] [Google Scholar]
- 44.Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can Robot-Assisted Unicompartmental Knee Arthroplasty Be Cost-Effective? A Markov Decision Analysis. J Arthroplasty. 2016 Apr;31(4):759-65. [DOI] [PubMed] [Google Scholar]
- 45.Pierce J, Needham K, Adams C, Coppolecchia A, Lavernia C. Robotic arm-assisted knee surgery: an economic analysis. Am J Manag Care. 2020 Jul 1;26(7):e205-10. [DOI] [PubMed] [Google Scholar]