Background:
Orbital fractures constitute a significant percentage of all midface injuries. Here, we present a contemporary evidence-based review of the major surgical approaches for orbital wall fractures and analyze the literature to compare all major surgical procedures and their complication rates.
Method:
A systematic review was conducted to compare surgical approaches (subciliary, transcaruncular, transconjunctival, subtarsal, and endoscopic) and postoperative complications in patients who underwent surgical fixation of orbital wall fractures. A database search in PubMed (PubMed Central, MEDLINE and Bookshelf) was performed for all articles containing the terms “orbital,” “wall,” “fracture,” and “surgery” with different combinations.
Results:
A total of 950 articles were obtained and 25 articles were included, representing an analysis of 1137 fractures. The most frequent surgical approach was the endoscopic (33.3%) followed by the external surgical approaches, specifically transconjunctival (32.8%), subciliary (13.5%), subtarsal (11.5%), and transcaruncular (8.9%). The transconjunctival approach had a statistically significantly higher rate of complications (36.19%), followed by the subciliary (21.4%), and endoscopic approach (20.2%, P < 0.0001). The subtarsal approach had a statistically significantly lower rate of complications (8.2%) followed by the transcaruncular approach (14.0%, P < 0.0001).
Conclusion:
The subtarsal and transcaruncular approaches were observed to have the lowest rates of complications, whereas the transconjunctival, subciliary, and endoscopic approaches were reported to have higher rates of complications.
Takeaways
Question: What are the risks and benefits of each surgical approach for orbital wall fractures, and which one offers the lowest complication rates?
Findings: We conducted a systematic review on postoperative complications and results of each surgical approach and found that subtarsal and transcaruncular approaches have a statistically significantly lower rate of complications.
Meaning: Choosing the correct approach for orbital wall fractures, it is imperative to understand the risks associated with each method. The subtarsal and transcaruncular approaches were observed to have the lowest rates of complications.
INTRODUCTION
Orbital fractures account for up to 40% of all midface trauma injuries.1 These fractures can be classified by those that only involve the orbital walls or those that extend to the orbital rim.2 Additionally, orbital fractures can either be isolated or part of more complex fractures, such as zygomaticomaxillary complex fractures, Le Fort II fractures (orbital floor fractures), and naso-orbital ethmoid fractures.3
The mechanism of orbital floor fractures has been modeled by the hydraulic theory and the buckling theory. The hydraulic theory postulates that forces transmitted to the globe are retropulsed hydraulically to the orbital wall, where they fracture the area of impact.4,5 Hydraulic forces are more likely to cause isolated orbital floor fractures than medial orbital wall fractures due to the underlying support that the trabecular ethmoid air cells give to the latter.6 However, when high-energy forces are applied to the globe, a combined orbital floor and medial orbital wall fractures can occur, as observed in cadaveric experimental studies.7 On the other hand, the buckling theory states that an injuring force, delivered directly along the orbital rim and surrounding structures, transmits along the orbital wall until a weak point is met.6,8,9
In general, the most common location of orbital fractures is the medial orbital wall (54.9%),10 specifically at the lamina papyracea of the ethmoid bone which is the thinnest region along the medial wall.6 Other fractures include combined medial orbital wall and nasal fractures (46%), combined naso-orbito-ethmoid fractures (26.8%), isolated inferior wall fractures (18.3%), zygomaticomaxillary complex fractures fractures (3%), and inferior orbital rim fractures (1%).10
Initial management should follow the Advance Trauma Life Support guidelines for maxillofacial injuries. A detailed history and physical exam are imperative with particular focus on visual disturbances, including blurred or double vision and loss of vision. A high suspicion for orbital fracture should be raised when physical exam reveals impact to extraocular movements, sensation changes, and/or orbital instability. A physical examination finding that should require immediate attention and treatment is a positive oculo-cardiac reflex. This presents as a triad of symptoms, including bradycardia, nausea, and syncope. Immediate attention is required to avoid fatal cardiac arrhythmia (1:3500).11
The gold standard for diagnostic confirmation is the orbital computed tomography. For orbital floor fractures, it is essential to visualize the inferior and medial rectus muscles, best seen in the coronal plane, which may suggest entrapment and diplopia. Medial orbital wall fractures have strong associations with enophthalmos (posterior malposition) as a result of the collapse of the lamina papyracea or entrapment of the medial rectus muscle. Red-flag computed tomography scan features that indicate immediate surgical correction include orbital apex fractures in the setting of worsening vision, damage to globe or optic nerve, periorbital emphysema, retrobulbar hematoma, and impinging bone fragment.3 In the pediatric population, the orbital floor can “spring back” into place causing entrapment which is also considered a surgical emergency.
Once surgical intervention is recommended, the type of surgical approach should be determined. There are four surgical approaches that can be performed for orbital fractures: the subciliary, the subtarsal, the transcaruncular/transconjunctival, and the endoscopic. Although there are multiple variations for the surgical approaches, the majority of the published articles about orbital fractures focus on surgical techniques, and just a few compared outcomes between surgical approaches.12 Furthermore, only one randomized control trial evaluated differences between open surgical approaches without including the endoscopic approach.13 The purpose of this practical review is to elucidate the risks and benefits of each surgical approach, and determine the one that offers lower complication rates.
METHODS
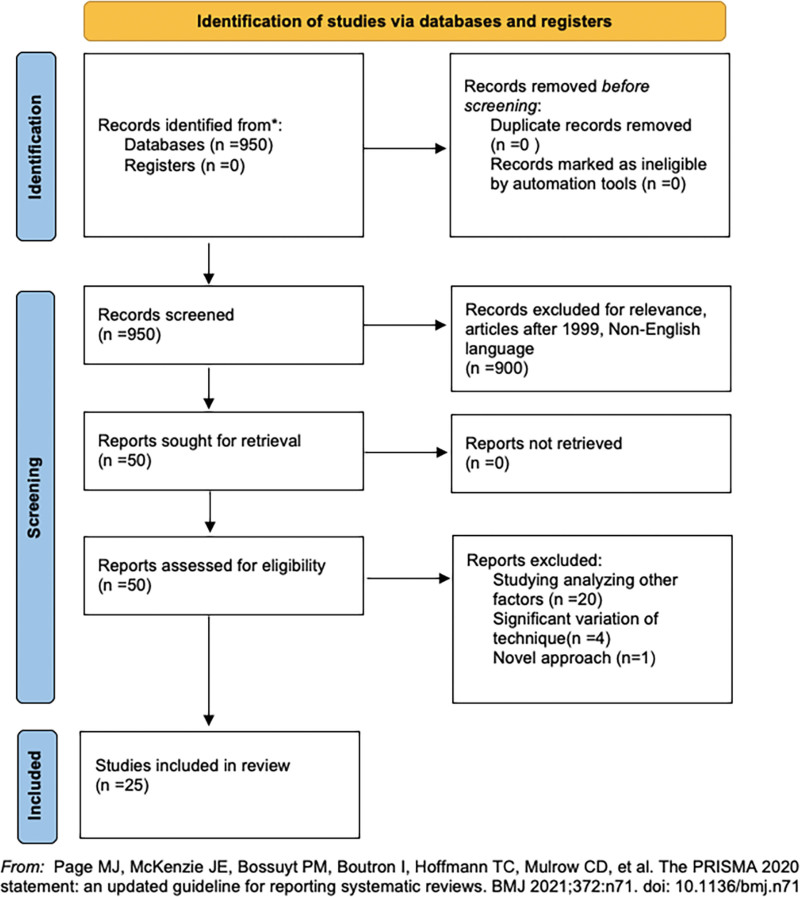
A systematic review was conducted to compare surgical approaches (subciliary, transcaruncular, transconjunctival, subtarsal, and endoscopic) and postoperative complications in patients who underwent orbital wall fractures. (See table, Supplemental Digital Content 1, which displays the detailed number of complications reported per study included in the review. http://links.lww.com/PRSGO/C535.) A database search was performed in June 2021 in PubMed (PubMed Central, MEDLINE and Bookshelf) for all articles containing the terms “orbital,” “wall,” “fracture,” and “surgery” with different combinations. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines were used for article identification and final selection. Two independent researchers (M.P. and J.J.) obtained preliminary data and selected final manuscripts following the inclusion and exclusion criteria. Inclusion criteria consisted of articles describing the surgical approach on patients who had orbital wall fractures after 1999. Studies older than 1999 were not considered in this review due to the evolution of surgical approaches since that time and because most of these studies did not separately report complications for each approach. Studies evaluating other factors such as types of implants or materials used, studies using novel approaches, nontraumatic surgical procedures, and non-English articles were also excluded.
Statistical Analysis
Total number of complications and noncomplications were summed by each of five surgical approaches. A five by two cross-tab was created with each row corresponding to specific surgical approach (endoscopic, subciliary, subtarsal, transcaruncular, and transconjunctival) and each column corresponding to whether complication occurred or not (yes/no). A chi-square test was used to evaluate whether there was a statistically significant relationship between surgical approaches and complication rate. This test was calculated using PROC FREQ with option of “chisq” using SAS version 9.4 (SAS Institute, Cary, N.C.; www.sas.com). The level of statistical significance was set at a P value less than 0.05.
SURGICAL APPROACHES
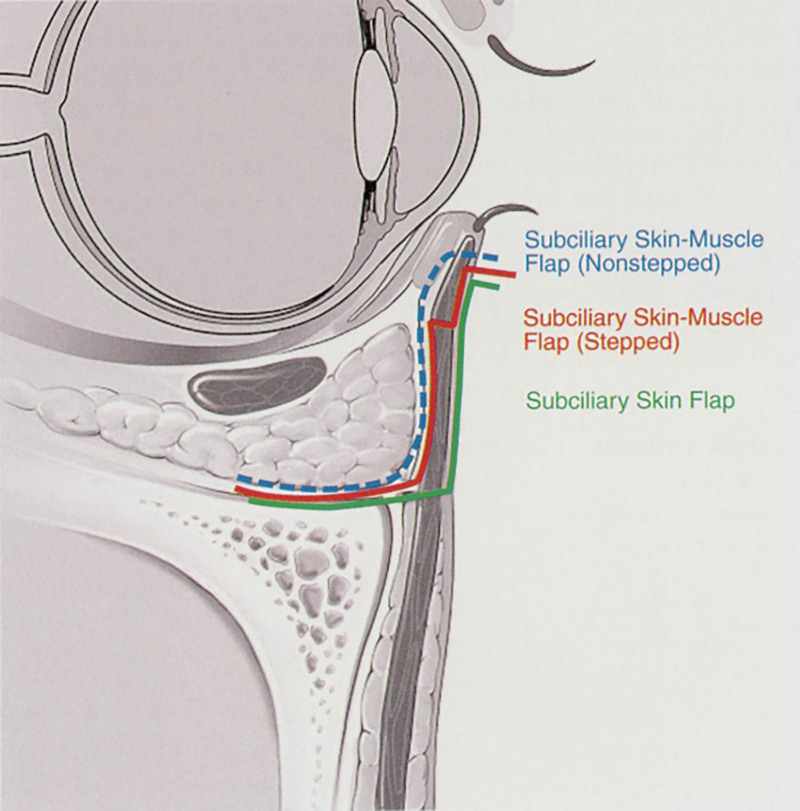
Subciliary
The subciliary approach was first introduced by Converse in 1944 to address orbital floor fractures.14 It is classically described as a cutaneous incision placed at the skin crease several millimeters below and parallel to the lash line (Fig. 1). The incision begins at the punctum medially and is continued laterally for 15 mm beyond the lateral canthus.15 The skin is dissected from the orbicularis to the level just beneath the tarsal plate before traversing the orbicularis muscle fibers down to the orbital septum (stepped or subciliary skin-muscle flap). This plane is then followed to the infraorbital rim. The periosteum is then incised, and access is gained to the fracture site. This stepwise fashion is completed so that there is no direct scarring of the eyelid, mitigating against scar inversion. There are two modifications: the subciliary skin flap, which divides the orbicularis fibers at the same level of the periosteal incision rather than subtarsally, and the nonstepped skin muscle flap, where the skin and orbicularis muscle are incised at the same time to the tarsal plate and the incision follows the preseptal plane to the infraorbital rim.15 The skin-muscle approach seems to have more favorable aesthetic outcomes with decreased skin necrosis than the skin-only approach, decreased ecchymosis, and lower incidence of ectropion. Nevertheless, the subciliary approach has been shown to have a higher incidence of denervation of the pretarsal orbicularis.15
Fig. 1.
Endoscopic approach. Reprinted with permission from Otolaryngol Head Neck Surg.140(6):849–854. © 2009 by Official Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation.
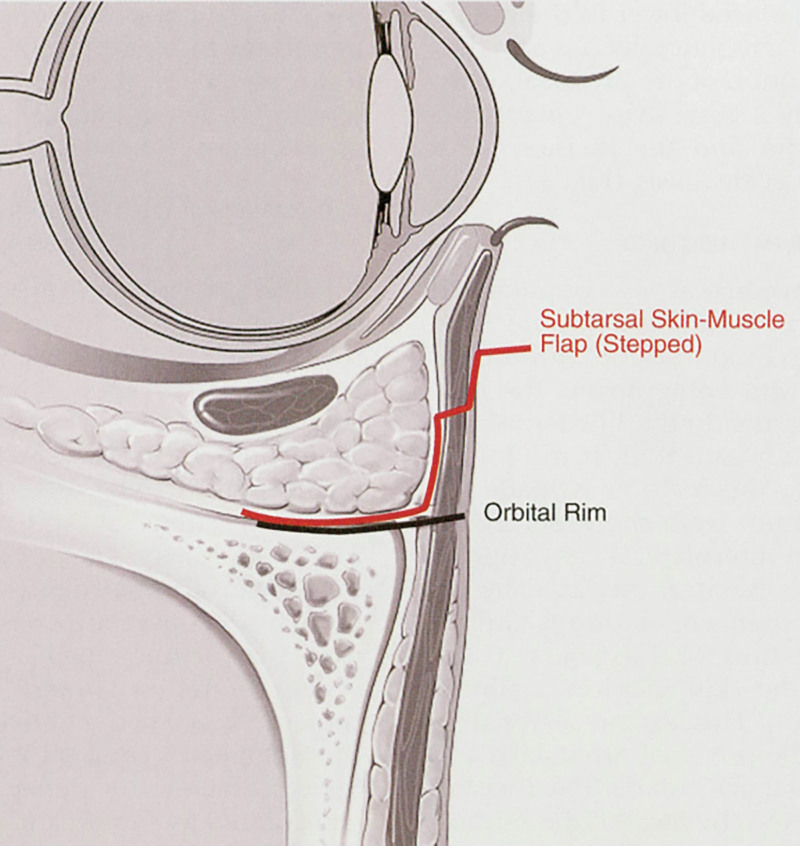
Subtarsal
The subtarsal approach was also created by Converse.14 The incision is made along the lower border of the tarsal plate in the subtarsal fold (Fig. 2). If there is edema, then the incision is made 5–7 mm from the lower eyelid margin following the inferolateral cant approximating the normal subtarsal crease. The orbicularis muscle is then encountered and divided in the direction of its fibers below the skin incision and carried to the level of the infraorbital rim in a preseptal plane. This prevents scar inversion and preserves all innervations to the pretarsal orbicularis and much of the preseptal orbicularis.15
Fig. 2.
Different subciliary approaches. Reprinted with permission from Plast Reconstr Surg. 2003;111(5):1708–1714.
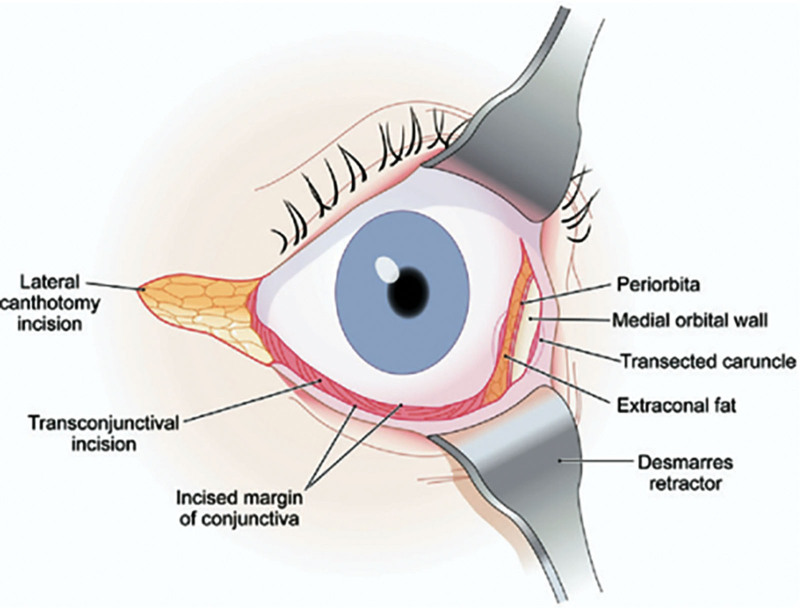
Transcaruncular/Transconjunctival
The transconjunctival approach can use two separate routes to access the infraorbital rim: retroseptal and preseptal (Figs. 3 and 4).16 The retroseptal route includes a transconjunctival incision with direct entry into the fat compartments of the lower eyelid and subsequently the infraorbital rim. The preseptal route makes an incision just below the tarsal border and enters toward the suborbicularis oculi/preseptal space above the fusion of the lower lid retractors and the orbital septum. The infraorbital rim is reached using the supraperiosteal plane.
Fig. 3.
Subtarsal approach. Reprinted with permission from Plast Reconstr Surg. 2003;111(5):1708–1714.
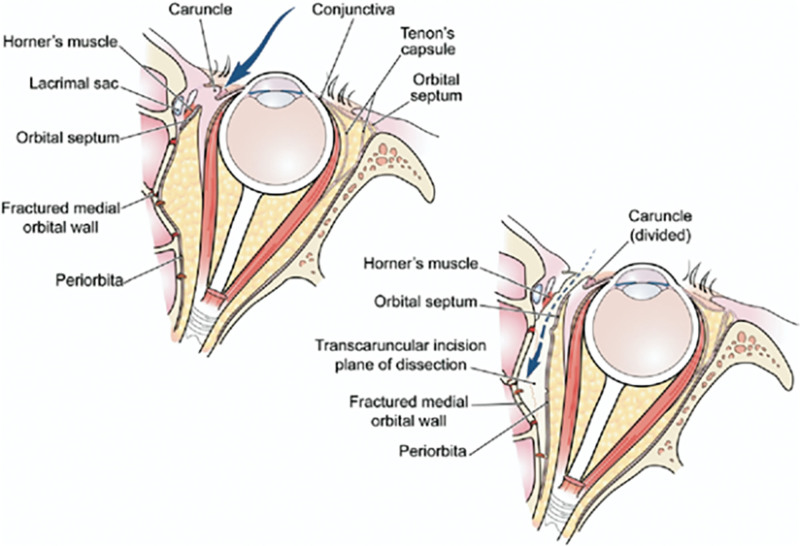
Fig. 4.
Transcaruncular, transconjuntival, and lateral canthotomy incisions. Reprinted with permission from Plast Reconstr Surg. 2007;65(11):2345–2349.
Similarly, the transconjunctival approach allows access to the medial orbital wall using a medial conjunctival incision posterior to the lacrimal draining system along the semilunar fold (Figs. 3 and 4).17 Incisions can either be precaruncular or transcaruncular. This dissection pathway is continued inside the periorbital soft tissue until the posterior lacrimal crest is reached. The lacrimal system is left intact and the periorbital is incised until the medial orbital wall is encountered.
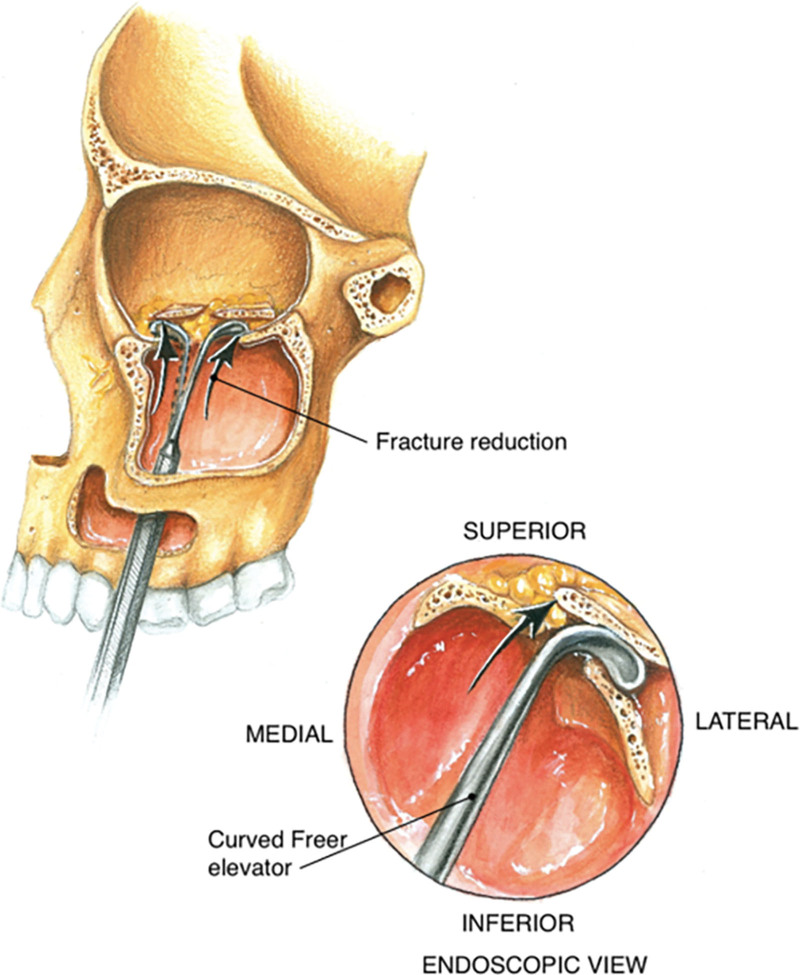
Endoscopic
Since its inception in the 1990s, the endoscopic method has evolved. Generally, endoscopic methods are carried out through a transnasal approach. Initial procedures performed a medial infundibulectomy, initially done via sickle knife (Fig. 5). The uncinate process is then removed with forceps via subluxation. The maxillary ostium is enlarged so that a 30-degree or 70-degree endoscope can be used to identify the orbital fracture. Ureteral balloon catheters can be used to elevate the fractured contents to their normal state.18 Initial procedures were done without rigid fixation, hence the use of the balloon. Modern endoscopic procedures are also conducted transnasally; however; there are other access sites (ie, transconjunctively).19 Largely, standard transnasal endoscope procedures are used, including 4-mm rigid nasal endoscopes (0 degree and 30 degrees). The orbital floor can be accessed via wide maxillary antrostomy, and an anterior ethmoidectomy is performed to assess the medial orbital wall in relation to the orbital floor. An isolated orbital floor fracture can then be created, which then causes herniation of orbital contents. Unstable bone fragments are removed, and a porous polyethylene plate (ie, MEDPOR; Stryker Corporation, Kalamazoo, Mich.) is inlayed along the defect.20 The use of a balloon inside the maxillary sinus for reduction of orbital fat is associated with more discomfort in comparison to nasal packing, which is now preferred. Complications that can arise from endoscopic approaches include discomfort, damage to surrounding structures, and increased infection (especially packing compared with balloon inflation). However, there are advantages including better visualization of the anatomy and aesthetic outcome.20 This method is generally used by otolaryngologists, and there are many studies accepting the validity of this method.
Fig. 5.
Axial views of transcaruncular approach (blue arrow) to the right medial orbital wall fracture and relationships. Reprinted with permission from Plast Reconstr Surg. 2007;65(11):2345–2349.
RESULTS
A total of 950 articles were retrieved from the search. After inclusion and exclusion criteria, a total of 25 manuscripts published between 1999 and 2020 were included in this review (Figure 6, Table 1). The number of patients in the studies ranged from four to 103, with a total of 1137 patients. Six studies evaluated the transcaruncular approach12,17,35,38,40,43; 12 studies, the endoscopic approach12,24,26,29,31,33,34,36,37,39,41,42; seven, the transconjunctival approach13,21,23,25,27,28,30; three, the subciliary approach13,21,30; and four, the subtarsal approach.13,22,30,32 The range of follow-up of the studies varied from 2 weeks to 63 months (Table 1).
Fig. 6.
Inclusion criteria.
Table 1.
Included Studies That Evaluated Different Types of Surgical Approach for Orbital Fractures
| Authors | Year | No. Patients | Number of Orbital Fractures | Surgical Approach | Complications | Follow-up |
|---|---|---|---|---|---|---|
| Bronstein et al21 | 2020 | 82 | 82 | Subciliary | Diplopia (n = 10), motor deficit (n = 2), ptosis (n = 1), entropion (n = 1), enophthalmos (n = 2), corneal injury (n = 6), proptosis (n = 3), ectropion (n = 2), lagophthalmos (n = 1), Keratoconjunctivitis Sicca (n = 3), vision disturbances (n = 1) | At least 6 mo |
| 102 | 102 | Transconjuntival | Diplopia (n = 11), motor deficit (n = 1), ptosis (n = 5), entropion (n = 4), enophthalmos (n = 7), infection (n = 4), corneal injury (n = 7), proptosis (n = 7), ectropion (n = 2), lagophthalmos (n = 1), Keratoconjunctivitis Sicca (n = 4), vision disturbances (n = 1) | At least 6 mo | ||
| Mahajan et al22 | 2020 | 30 | 30 | Subtarsal | Scar (n = 5), scleral show (n = 3) | At least 12 mo |
| Mohamed et al13 | 2020 | 15 | 15 | Subciliary | Ectropion (n = 3), scleral show (n = 4), epiphora (n = 2) | NS |
| 15 | 15 | Subtarsal | Scar (n = 2), ectropion (n = 1), scleral show (n = 1), epiphora (n = 1) | NS | ||
| 15 | 15 | Transconjuntival | Entropion (n = 3), ectropion (n = 1), scleral show (n = 2), epiphora (n = 3) | NS | ||
| Park et al23 | 2019 | 32 | 32 | Transconjuntival | Ptosis (n = 7) | 3 mo |
| Kühnel et al24 | 2017 | 17 | 17 | Endoscopic | Infection (n = 1), sensory injury (n = 1) | NS |
| Chou et al25 | 2017 | 19 | 19 | Transconjuntival | Diplopia (n = 1) | Median: 3.2 mo (range: 2 wk–6 mo) |
| Wu et al26 | 2013 | 93 | 93 | Endoscopic | Diplopia (n = 3), enophthalmos (n = 1), asymmetry (n = 1), intraorbital hemorrhage (n = 1) | Range: 6–15 mo |
| Novelli et al27 | 2011 | 53 | 56 | Transconjuntival | Entropion (n = 2), trichiasis (n = 2) | Mean: 22 mo (range: 2–48 mo) |
| Han et al12 | 2009 | 29 | 29 | Endoscopic | Enophthalmos (n = 4) | Mean: 70.8 mo (range: 11–163 mo) |
| 19 | 19 | Transcaruncular | Implant misplacement (n = 1), enophthalmos (n = 2) | Mean: 70.8 mo (range: 11–163 mo) | ||
| Kim et al28 | 2009 | 103 | 103 | Transconjuntival | Diplopia (n = 5), enophthalmos (n = 4), canthal dystopia (n = 1), hyperpigmentation (n = 4), lower eyelid skin dimpling (n = 2) | At least 6 mo |
| Hinohira et al29 | 2009 | 23 | 23 | Endoscopic | Enophthalmos (n = 1) | Mean: 12.9 mo |
| Ridgeway et al30 | 2009 | 74 | 74 | Subtarsal | Scar (n = 1), ectropion (n = 2), lid edema (n = 1) | NS |
| 56 | 56 | Subciliary | Scar (n = 2), ectropion (n = 7), lid edema (n = 5) | NS | ||
| 45 | 45 | Transconjuntival | Entropion (n = 2) | NS | ||
| Ducic and Verret31 | 2009 | 63 | 63 | Endoscopic | Poor reduction (n = 2) | NS |
| Baqain et al32 | 2008 | 12 | 12 | Subtarsal | Scar (n = 1), keratoconjunctivitis sicca (n = 1), scleral show (n = 1), lid edema (n = 1) | Mean ± SD: 37.25 ± 23.7 mo (range: 10–73 mo) |
| Jeon et al33 | 2007 | 40 | 40 | Endoscopic | Diplopia (n = 6), motor deficit (n = 1), enophthalmos (n = 4) | Range: 1.5–52 mo |
| Jin et al34 | 2007 | 48 | 48 | Endoscopic | Diplopia (n = 11), enophthalmos (n = 2), infection (n = 1) | Range: 3 mo–4 y |
| 48 | 48 | Transcaruncular | Diplopia(n = 20), implant misplacement (n = 1), enophthalmos (n = 4), scar (n = 1), intraorbital hemorrhage (n = 1), ectropion (n = 2) | Range: 3 mo–4 y | ||
| Kim et al35 | 2005 | 13 | 13 | Transcaruncular | Diplopia (n = 1), ocular motility (n = 3) | Range: 5–24 mo |
| Sanno et al36 | 2003 | 21 | 21 | Endoscopic | Diplopia (n = 4), mydriasis and blepharoptosis-superior orbital fissure syndrome (n = 1) | Mean: 341 days |
| Lee et al37 | 2002 | 16 | 16 | Endoscopic | Diplopia (n = 1) | Range: 13–25 mo |
| Graham et al38 | 2002 | 5 | 6 | Transcaruncular | None | Mean: 19.3 mo (range: 6–63 mo) |
| Chen et al39 | 2001 | 9 | 9 | Endoscopic | Diplopia (n = 1), enophthalmos (n = 1) | Mean: 10 mo |
| Shorr et al17 | 2000 | 10 | 10 | Transcaruncular | None | Mean: 23 mo (range: 2–62 mo). |
| Baumann and Ewers40 | 2000 | 5 | 5 | Transcaruncular | None | Mean: 12 mo |
| Jin et al41 | 2000 | 16 | 16 | Endoscopic | Diplopia (n = 1), enophthalmos (n = 2) | Mean: 7 mo |
| Chen et al42 | 1999 | 4 | 4 | Endoscopic | Enophthalmos (n = 1) | Mean: 11 mo (range: 8–16 mo) |
NS, not specified.
COMPARISON BETWEEN SURGICAL APPROACHES
The total number of orbital fractures included in the analysis was 1137 (Table 2). The most frequent surgical approach was the endoscopic (33.3%), followed by the external surgical approaches. The most frequent external surgical approaches included the transconjunctival (32.8%), the subciliary (13.5%), the subtarsal (11.5%), and the transcaruncular (8.9%). The incidence of complications regardless of surgical approach was 22.6%. The reported complications included diplopia, motor deficit, ptosis, entropion, ectropion, enophthalmos, corneal injury, proptosis, lagophthalmos, keratoconjuntivitis sicca, vision disturbances, scar, epiphora, scleral show, asymmetry, intraorbital hemorrhage, trichiasis, implant misplacement, canthal dystopia, hyperpigmentation, lower eyelid skin dimpling, lid edema, infection, and blepharoptosis. When complications were analyzed by surgical approach, the transconjunctival approach had a statistically significantly higher rate of complications (36.2%), followed by the subciliary (21.4%), and endoscopic approach (20.2%, P < 0.0001, Table 2). The subtarsal approach had the statistically significantly lowest rate of complications (8.2%) followed by the transcaruncular approach (14.0%, P < 0.0001, Table 2).
Table 2.
Comparison of Complications between Surgical Approaches for Orbital Wall Fractures*
| Approach | Complications (n = 257) | No. Complications (n = 880) | Total (N = 1137) |
|---|---|---|---|
| Endoscopic | 52 (20.2%) | 327 (37.2%) | 379 (33.3%) |
| Subciliary | 55 (21.4%) | 98 (11.1%) | 153 (13.5%) |
| Subtarsal | 21 (8.2%) | 110 (12.5%) | 131 (11.5%) |
| Transcaruncular | 36 (14.0%) | 65 (7.4%) | 101 (8.9%) |
| Transconjunctival | 93 (36.2%) | 280 (31.8%) | 373 (32.8%) |
P using chi-square test, with P < 0.0001 indicating a statistically significant relationship between any of five approaches and complication rate.
DISCUSSION
This practical review summarizes and highlights the initial evaluation and surgical approach of orbital fractures. Reporting the complications such as retrobulbar hemorrhage, infection, intraorbital hemorrhage/hematoma, and sensory injury, related with each surgical approach is important, as all these issues can potentially lead to blindness although there is a low probability of this happening.44 This study demonstrated that the subtarsal and transcaruncular approaches for orbital fractures have the lowest complication rates.
During the early days of transcutaneous orbital wall reconstruction, there were several concerns about scarring, especially now when compared with the conjunctival or endoscopic methods. Our findings align with Bähr’s 1992 study45 showing a significantly lower incidence of complications for the subtarsal approach (8.8%) compared with the subciliary (25%) and transcaruncular approaches (30.4%). In our current study, the incidence of complications for the subtarsal approach was 8.2% (Table 2). Out of the 131 patients who underwent a subtarsal approach, nine (6.9%) experienced scar; five (3.82%) had scleral show; three (2.29%), ectropion; two (1.53%), lid edema; one (0.76%), epiphora; and one (0.76%), keratoconjunctivitis sicca. Similarly to our study, Bähr et al45 also noted scar and scleral show as the most frequent complications for the subtarsal approach.
We have observed that scar was present more frequently in patients who had a subtarsal approach compared with those who underwent a subciliary approach. Heckler et al46 postulated that the etiology of the difference in scar formation is that the subtarsal incision has poorer muscle mobility and skin quality in comparison to the subciliary incision. Additionally, there is an increased risk for noticeable scar as the incision is further away from the lash line in comparison to a subciliary approach.12 Contrary to this, in 2021, Oztel et al47 found that out of a series of 67 patients who underwent subtarsal incision for orbital wall fractures, 61 had no visible scar. Although the conjunctival incision has no scar, the excellent outcomes proposed by Oztel et al47 demonstrate that scar formation may actually be limited, and that subtarsal incisions should be considered when reconstructing the orbital wall. Finally, when comparing surgical approaches, it is imperative to consider exposure and access for selecting the best approach. Both transcaruncular and subtarsal incisions allow for direct wide exposure of the orbital floor when compared with endoscopic and transconjunctival approach. When there is concomitant fracture to the lateral border of the orbit, a subtarsal incision can be extended with a lateral canthal extension.26
Finally, with the advent of endoscopic techniques, there has been a push to be minimally invasive for aesthetic outcomes with results similar to those of transcutaneous approaches. Han et al12 completed a comparison study of transcaruncular approach with endoscopic endonasal reduction. They ultimately concluded that the reduction rate in degree of enophthalmos, diplopia, and extraocular movement limitation between the two groups was insignificant (average reduction rate of endoscopic approach was 89.2% versus 90.7% for transcaruncular). However, they noticed that operation time, length of hospital stay, and cost were higher in the endoscopic approach.
As we improve our endoscopic technique, this may become the standard of care for orbital wall reconstruction; however, subtarsal or transcaruncular approaches are preferred at this time because they are low-complexity and low-cost procedures. Both procedures have minimally invasive incisions with a direct approach to the orbital floor and infraorbital rim.
LIMITATIONS
The main limitation of this systematic review is the heterogeneity of included studies which makes it difficult to compare types of complications between surgical approaches. In addition, the retrospective nature and different follow-up periods of the included articles may have influenced the rate of complications. This shows that there is a clear need for level 1 evidence comparing the surgical approaches discussed, with the inclusion of endoscopic techniques. High quality randomized controlled trials can help to reduce the confounding variables found in this study and definitively determine which approach has the fewest complications and best overall outcomes for orbital wall reconstructions. Moreover, selection bias may have occurred when trying to make the data uniform. Regardless of the limitations, we believe this review elucidates the best surgical approach that offers the lowest rate of complications for orbital wall reconstruction.
CONCLUSIONS
The subtarsal and transcaruncular approaches were observed to have the lowest rates of complications, whereas the transconjunctival, subciliary, and endoscopic approaches were reported to have higher rates of complications. Further research is needed to determine the best approach for patients with orbital wall fractures.
DISCLOSURE
Dr. Janis receives royalties from Thieme and Springer publishing. All the other authors have no financial interests to declare in relation to the content of this article.
Supplementary Material
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Ellis E, el-Attar A, Moos KF. An analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg. 1985;43:417–428. [DOI] [PubMed] [Google Scholar]
- 2.Hsu CK, Hsieh MW, Chang HC, et al. Anatomic factors predicting postoperative strabismus in orbital wall fracture repair. Sci Rep. 2019;9:14785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics. 2006;26:783–793. [DOI] [PubMed] [Google Scholar]
- 4.Converse JM, Smith B. Enophthalmos and diplopia in fractures of the orbital floor. Br J Plast Surg. 1957;9:265–274. [DOI] [PubMed] [Google Scholar]
- 5.Smith B, Regan WF. Blow-out fracture of the orbit; mechanism and correction of internal orbital fracture. Am J Ophthalmol. 1957;44:733–739. [DOI] [PubMed] [Google Scholar]
- 6.Choi M, Flores RL. Medial orbital wall fractures and the transcaruncular approach. J Craniofac Surg. 2012;23:696–701. [DOI] [PubMed] [Google Scholar]
- 7.Rhee JS, Kilde J, Yoganadan N, et al. Orbital blowout fractures: experimental evidence for the pure hydraulic theory. Arch Facial Plast Surg. 2002;4:98–101. [DOI] [PubMed] [Google Scholar]
- 8.Fujino T, Makino K. Entrapment mechanism and ocular injury in orbital blowout fracture. Plast Reconstr Surg. 1980;65:571–576. [DOI] [PubMed] [Google Scholar]
- 9.Waterhouse N, Lyne J, Urdang M, et al. An investigation into the mechanism of orbital blowout fractures. Br J Plast Surg. 1999;52:607–612. [DOI] [PubMed] [Google Scholar]
- 10.Burm JS, Chung CH, Oh SJ. Pure orbital blowout fracture: new concepts and importance of medial orbital blowout fracture. Plast Reconstr Surg. 1999;103:1839–1849. [DOI] [PubMed] [Google Scholar]
- 11.Sires BS, Stanley RB, Jr, Levine LM. Oculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repair. Arch Ophthalmol. 1998;116:955–956. PMID: 9682717. [PubMed] [Google Scholar]
- 12.Han K, Choi JH, Choi TH, et al. Comparison of endoscopic endonasal reduction and transcaruncular reduction for the treatment of medial orbital wall fractures. Ann Plast Surg. 2009;62:258–264. [DOI] [PubMed] [Google Scholar]
- 13.Mohamed FI, Reda HM, Khalifa GA. Anthropometric changes in the morphology of the lower eyelid after using three different approaches in patients with orbital fractures. J Craniomaxillofac Surg. 2020;48:985–993. [DOI] [PubMed] [Google Scholar]
- 14.Converse JM. Two plastic operations for repair of orbit following severe trauma and extensive comminuted fracture. Arch Ophthalmol. 1944;31:323–325. [Google Scholar]
- 15.Rohrich RJ, Janis JE, Adams WP, Jr. Subciliary versus subtarsal approaches to orbitozygomatic fractures. Plast Reconstr Surg. 2003;111:1708–1714. [DOI] [PubMed] [Google Scholar]
- 16.Edgin WA, Morgan-Marshall A, Fitzsimmons TD. Transcaruncular approach to medial orbital wall fractures. J Oral Maxillofac Surg. 2007;65:2345–2349. [DOI] [PubMed] [Google Scholar]
- 17.Shorr N, Baylis HI, Goldberg RA, et al. Transcaruncular approach to the medial orbit and orbital apex. Ophthalmology. 2000;107:1459–1463. [DOI] [PubMed] [Google Scholar]
- 18.Ikeda K, Suzuki H, Oshima T, et al. Endoscopic endonasal repair of orbital floor fracture. Arch Otolaryngol Head Neck Surg. 1999;125:59–63. [DOI] [PubMed] [Google Scholar]
- 19.Zhou G, Tu Y, Yu B, et al. Endoscopic repair of combined orbital floor and medial wall fractures involving the inferomedial strut. Eye (Lond). 2021;35:2763–2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Engle RD, Chaskes M, Wladis E, et al. Feasibility study for transnasal endoscopic repair of orbital floor fracture with alloplastic implant. Ann Otol Rhinol Laryngol. 2016;125:970–975. [DOI] [PubMed] [Google Scholar]
- 21.Bronstein JA, Bruce WJ, Bakhos F, et al. Surgical approach to orbital floor fractures: comparing complication rates between subciliary and subconjunctival approaches. Craniomaxillofac Trauma Reconstr. 2020;13:45–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahajan RK, Gupta K, Srinivasan K, et al. retrospective analysis of Subtarsal Incision in Maxillofacial Trauma. J Maxillofac Oral Surg. 2020;19:443–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park J, Kim S, Baek S. The characteristics of lower eyelid reverse ptosis after reconstruction of orbital floor wall fracture using transconjunctival approach. J Craniofac Surg. 2019;30:e649–e653. [DOI] [PubMed] [Google Scholar]
- 24.Kuhnel T, Jagle H, Hosemann W, et al. Orbital floor fracture repair: the endonasal approach. Rhinology. 2017;55:348–354. [DOI] [PubMed] [Google Scholar]
- 25.Chou C, Kuo Y-R, Chen C-C, et al. Medial orbital wall reconstruction with porous polyethylene by using a transconjunctival approach with a caruncular extension. Ann Plast Surg. 2017;78:S89–S94. [DOI] [PubMed] [Google Scholar]
- 26.Wu W, Jing W, Selva D, et al. Endoscopic transcaruncular repair of large medial orbital wall fractures near the orbital apex. Ophthalmology. 2013;120:404–409. [DOI] [PubMed] [Google Scholar]
- 27.Novelli G, Ferrari L, Sozzi D, et al. Transconjunctival approach in orbital traumatology: a review of 56 cases. J Craniomaxillofac Surg. 2011;39:266–270. [DOI] [PubMed] [Google Scholar]
- 28.Kim DW, Choi SR, Park SH, et al. Versatile use of extended transconjunctival approach for orbital reconstruction. Ann Plast Surg. 2009;62:374–380. [DOI] [PubMed] [Google Scholar]
- 29.Hinohira Y, Takahashi H, Komori M, et al. Endoscopic endonasal management of medial orbital blowout fractures. Facial Plast Surg. 2009;25:17–22. [DOI] [PubMed] [Google Scholar]
- 30.Ridgway EB, Chen C, Colakoglu S, et al. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg. 2009;124:1578–1586. [DOI] [PubMed] [Google Scholar]
- 31.Ducic Y, Verret DJ. Endoscopic transantral repair of orbital floor fractures. Otolaryngol Head Neck Surg. 2009;140:849–854. [DOI] [PubMed] [Google Scholar]
- 32.Baqain ZH, Malkawi Z, Hadidi A, et al. Subtarsal approach for orbital floor repair: a long-term follow-up of 12 cases in a Jordanian teaching hospital. J Oral Maxillofac Surg. 2008;66:45–50. [DOI] [PubMed] [Google Scholar]
- 33.Jeon SY, Kwon JH, Kim JP, et al. Endoscopic intranasal reduction of the orbit in isolated blowout fractures. Acta Oto-Laryngologica. 2007;127(Suppl 558):102–109. [DOI] [PubMed] [Google Scholar]
- 34.Jin HR, Yeon JY, Shin SO, et al. Endoscopic versus external repair of orbital blowout fractures. Otolaryngol Head Neck Surg. 2007;136:38–44. [DOI] [PubMed] [Google Scholar]
- 35.Kim S, Helen Lew M, Chung SH, et al. Repair of medial orbital wall fracture: transcaruncular approach. Orbit. 2005;24:1–9. [DOI] [PubMed] [Google Scholar]
- 36.Sanno T, Tahara S, Nomura T, et al. Endoscopic endonasal reduction for blowout fracture of the medial orbital wall. Plast Reconstr Surg. 2003;112:1228–1237. ; discussion 1238. [DOI] [PubMed] [Google Scholar]
- 37.Lee HM, Han SK, Chae SW, et al. Endoscopic endonasal reconstruction of blowout fractures of the medial orbital walls. Plast Reconstr Surg. 2002;109:872–876. [DOI] [PubMed] [Google Scholar]
- 38.Graham SM, Thomas RD, Carter KD, et al. The transcaruncular approach to the medial orbital wall. Laryngoscope. 2002;112:986–989. [DOI] [PubMed] [Google Scholar]
- 39.Chen CT, Chen YR. Endoscopically assisted repair of orbital floor fractures. Plast Reconstr Surg. 2001;108:2011–2018. ; discussion 2019. [DOI] [PubMed] [Google Scholar]
- 40.Arnulf B, Rolf E. Transcaruncular approach for reconstruction of medial orbital wall fracture. Int J Oral Maxillofac Surg. 2000;29:264–267. PMID: 11030396. [PubMed] [Google Scholar]
- 41.Jin HR, Shin SO, Choo MJ, et al. Endonasal endoscopic reduction of blowout fractures of the medial orbital wall. J Oral Maxillofac Surg. 2000;58:847–851. [DOI] [PubMed] [Google Scholar]
- 42.Chen CT, Chen YR, Tung TC, et al. Endoscopically assisted reconstruction of orbital medial wall fractures. Plast Reconstr Surg. 1999;103:714–20. . Quiz-721. [DOI] [PubMed] [Google Scholar]
- 43.Sung Joo Kim. and MDHLaS-HCaKHKaYJaSYL. Repair of medial orbital wall fracture: transcaruncular approach. Orbit. 2005;24:1–9. [DOI] [PubMed] [Google Scholar]
- 44.Jacobs SM, McInnis CP, Kapeles M, et al. Incidence, risk factors, and management of blindness after orbital surgery. Ophthalmology. 2018;125:1100–1108. [DOI] [PubMed] [Google Scholar]
- 45.Bähr W, Bagambisa FB, Schlegel G, et al. Comparison of transcutaneous incisions used for exposure of the infraorbital rim and orbital floor: a retrospective study. Plast Reconstr Surg. 1992;90:585–591. [DOI] [PubMed] [Google Scholar]
- 46.Heckler FR, Songcharoen S, Sultani FA. Subciliary incision and skin-muscle eyelid flap for orbital fractures. Ann Plast Surg. 1983;10:309–313. [DOI] [PubMed] [Google Scholar]
- 47.Oztel M, Goh R, Hsu E. Subtarsal versus transconjunctival approach: a long-term follow-up of esthetic outcomes and complications. J Oral Maxillofac Surg. 2021;79:1327.e1–1327.e6. [DOI] [PubMed] [Google Scholar]