Abstract
The usage of video calls for social connection generally increased during the COVID-19 pandemic. It remains unclear, how individuals with dementia (IWD), many of who already experienced isolation in their care settings, use and perceive video calls, what barriers and benefits exist, and how the COVID-19 pandemic impacted their use of video calls. An online survey was conducted to healthy older adults (OA) and people surrounding IWD as proxies. Both OA and IWD showed increased use of video calls after COVID-19 and the severity of dementia was not correlated with the video call usage among IWD during this period. Both groups perceived significant benefits in using video calls. However, IWD exhibited more difficulties and barriers to using them compared to OA. Given the perceived benefits of video calls to the quality of life in both populations, education and support by family, caregivers, or healthcare professionals are necessary for them.
Keywords: video calls, COVID-19, dementia, social communication, aging
Introduction
Social communication is an essential component throughout the lifespan. It provides us with one of the most powerful means of building relationships and connecting with others in our communities. Further, it strengthens social networks and support systems that can be crucial for positive health outcomes1-3 and plays a central role in maintaining psychological well-being, with interlocutors exchanging and affirming their opinions, beliefs, and values.
Face-to-face communication has been one of the most frequently occurring modalities of social communication. In March 2020, the frequency and quality of face-to-face communication were adversely impacted by social and physical distancing practices resulting from the COVID-19 pandemic. The distancing practices and related restrictions during the pandemic made it exceptionally difficult for vulnerable populations to maintain their social relationships, given the decreased in-person encounters between people. 4 The decreased face-to-face communication opportunities led to detrimental consequences. For example, physical distancing and isolation caused increased mental and psychological distress in many populations, including older adults with and without clinical conditions.5-8
Among the clinical populations significantly challenged by the pandemic, individuals with dementia (IWD) were one of the most negatively and disproportionately impacted groups. For instance, evidence suggests that the COVID-19 pandemic exacerbated neuropsychological and psychiatric problems in people with ADRD (Alzheimer’s disease and related dementias),6,9 which may be resulted from fewer opportunities for social engagement and interactions. While social communication is essential to social connection and support throughout the lifespan of all human beings, IWD already experience breakdowns in social communication over the course of their disease progression, primarily due to their significant cognitive neuropsychological declines.10-14 In addition to the already existing challenges in communication, the COVID-19 pandemic made social communication in this population excruciatingly challenging and scarce, especially for those in long-term care facilities. 15
This has been a serious problem, as active social engagement is critical to protect against the progression of ADRD. The current literature suggests that engagement in social and mental activities promotes cognitive and neural reserve and even reduces the risk of developing dementia.16-19 Engagement and social interactions are also significantly associated with increased quality of life, better mood, and happiness in people with ADRD.20-22 Decreased activity and participation, social isolation, and therefore decreased quality of life (see a recent review in Masterson-Algar et al., 2022) 23 caused by the COVID-19 pandemic have been devastating for individuals with ADRD and their families. 24
During this pandemic, video calls have been recommended as an alternative to in-person communications and visits to avoid the negative consequences of social isolation while maintaining the distance required to reduce the spread of COVID-19. In fact, one survey study 25 showed that the use of technology-mediated communication, especially video calls, increased to meet the need for social support and being connected with one another; the use of technology-mediated communication with close friends and family is significantly associated with subjective wellbeing. Connecting through video calls to family and friends who are physically distant may be especially beneficial for individuals with ADRD, who often experience isolation in their care settings. 26 Video calls may stimulate social and cognitive aspects of communication 27 and increase their quality of life by providing social support (see also Shapira et al., 2021). 28 Further, the need for video calls has become unprecedently urgent, as the advancement of technology and the forced social and physical distancing due to the pandemic accelerated the utilization of telepractice in many healthcare fields.
Despite increased demand for video calls and telepractice, differences between in-person communication and computer-mediated communication may present challenges to using these technologies, especially for those with cognitive impairment. For example, interlocutors may experience delays in information transmission and weaker non-verbal backchannel feedback between them during technology-assisted communications. As a result, interlocutors speak louder and smile more 29 and produce longer and more disrupted interactions 30 during computer-mediated communication than in face-to-face communication. Further, Lyons et al. (2012) 31 demonstrated that there is a potential for increased cognitive load when individuals are less familiar with the software and technology being used. This finding is consistent with the recent survey result that demonstrated a significant negative relationship between age and the use of video calls. Older adults who tend to be less familiar with technology are less likely to use video calls compared to younger adults who are more exposed to recent technological development. 25 Similarly, technology usage for communication is highly correlated with age, socioeconomic status (e.g., educational level), and physical capacity and disability status in the older population; younger, more educated older adults are more likely to use technology to communicate and have more access to the internet. 32 Not surprisingly, older adults with vision or/and memory impairment reported decreased use of technology compared to those without vision/memory impairments.
Given the fairly recent development of technology and its widespread usage by the public, little is known about how this video call is used, especially in the older population who may not be familiar with it. Research is needed to understand whether there has been an increased frequency of video calls by older adults, and if so, whether the video calls provide this population with any benefits (i.e., users’ perceptions and satisfactions). Further, it is unclear whether a clinical population, such as IWD, is able to make use of video calls in their daily lives. Understanding their usage and perception of video calls and investigating potential barriers and subjective benefits to the use of video calls may contribute to development of educational strategies and facilitation of social communication in IWD who need more positive social connection. In addition, the effects of the COVID-19 pandemic on how IWD communicated using video calls remain unclear. The COVID-19 pandemic facilitated the use of video calls in healthy older adults, 33 but with their associated cognitive declines, IWD might show different patterns of usage or encounter greater challenges compared to healthy older adults. Therefore, we investigated the usage of video calls in IWD and typical older adults to understand whether these populations are capable of making video calls and, if so, how the COVID-19 pandemic affected their video call usage, (e.g., how much and frequently they use(d) video calls before and after the pandemic). We also sought to understand how much these populations enjoy video calls and what barriers may exist to using them. We investigated these questions by conducting an online survey among healthy older adults and individuals surrounding IWD, including caregivers, family, and close friends, who participated as proxies to report information about the use of video calls in IWD.
Methods
Participants
The survey Paek et al., was completed by 153 older adults (OA) (age mean 72.90; standard deviation (SD) 5.71; 53 males, 99 females, 1 preferred not to answer) and 70 adults as proxies for IWD (age mean 50.83; SD 14.8; 16 males, 54 females). The inclusionary criteria for healthy older adults were: a) between 65-99 years old; b) English speakers with no history of psychiatric/neurological disorders; and c) able to see and hear well enough to live independently. Healthy older adults voluntarily completed the survey without monetary compensation for their time. The inclusionary criteria for caregivers as proxies were: a) a close friend, family member, or caregiver of an individual with mild or moderate dementia; b) able to communicate with the individual with mild or moderate dementia in any way at least once a week; c) between 18-99 years old; and d) English speakers with no history of psychiatric/neurological disorders. Caregivers as proxies voluntarily completed the survey and received a $10 Amazon e-gift card for their participation. Most of the proxies for IWD were adult children (N = 50, 71.43%), adult grandchildren (N = 7, 10.00%), friends (N = 5, 7.14%), or spouse/partners (N = 3, 4.29%) of IWD or others (N = 5, 7.14%), such as siblings or formal caregivers. Proxies reported that IWD started to show dementia symptoms on average 4.77 years previously (SD = 4.03) and were diagnosed on average 3.15 years previously (SD = 3.20). Their diagnosis varied, including Alzheimer’s dementia, primary progressive aphasia, Lewy body dementia, Parkinson’s disease dementia, and vascular dementia, among others (See Appendix Table A1).
The demographic information of the participants is shown in Table 1. There were significant differences in age (t (101.18) = −5.61, P < .001) and education level (t (221) = 5.30, P < .001) between IWD and OA, reflecting the demographic characteristics of dementia 34 as older adults with less education or/and who are older are significantly more likely to develop dementia. Note that proxies for IWD reported demographic information for the IWD as well as information about themselves (Table 1).
Table 1.
Demographic Information (Mean and Standard Deviation or Response Count (n) and its Percentage (%)) for Each Group.
| Proxies | IWD | OA | |
|---|---|---|---|
| Age | 50.81 (14.69) | 78.94 (8.15) | 72.90 (5.71) |
| Gender | |||
| Male | 16 | 32 | 53 |
| Female | 54 | 38 | 99 (1 preferred not to answer) |
| Education | 16.23 (1.82) | 13.74 (3.25) | 16.09 (2.88) |
| Race | |||
| White | 65 (92.86%) | 64 (91.43%) | 144 (94.12%) |
| Black or African American | 0 (0%) | 1 (1.43%) | 2 (1.31%) |
| Asian or Pacific Islander | 3 (4.29%) | 3 (4.29%) | 3 (1.96%) |
| Native American | 0 (0%) | 0 (0%) | 2 (1.31%) |
| Mixed race | 1 (1.43%) | 0 (0%) | 0 (.0%) |
| Others | 0 (0%) | 1 (1.43%) | 1 (.65%) |
| Prefer not to answer | 0 (0%) | 0 (0%) | 1 (.65%) |
| Ethnicity | |||
| Hispanic or Latino | 1 (1.43%) | 1 (1.43%) | 3 (1.96%) |
| Non-Hispanic | 67 (95.71%) | 67 (95.71%) | 145 (94.77%) |
| Prefer not to answer or skipped | 2 (2.86%) | 2 (2.86%) | 5 (3.27%) |
| Marital Status | |||
| Married/Partnered | 55 (78.57%) | 36 (51.43%) | 107 (69.93%) |
| Single/Widowed | 10 (14.29%) | 27 (38.57%) | 33 (21.57%) |
| Divorced/Separated | 4 (5.71%) | 6 (8.57%) | 13 (8.50)% |
| Prefer not to answer | 1 (1.43%) | 1 (1.43%) | 0 (0%) |
| Living Status | |||
| Living alone; totally independent | - | 1 (1.43%) | 35.10% |
| Living alone but some assistance needed | - | 11 (15.71%) | 1.32% |
| Living with family | - | 30 (42.86%) | 41.72% |
| Assisted living or senior living facility | - | 17 (24.29%) | 3.31% |
| Nursing home or healthy care center | - | 11 (15.71%) | 0% |
| Others | - | 0 (0%) | 18.54% |
Note. All question responses were optional. IWD = Individuals with dementia; OA = Older adults.
Materials and Procedure
Survey Development
Two versions of an online survey were developed – one for caregivers surrounding IWD as proxies and one for OA – to investigate the use of video calls in IWD and OA before and after the COVID-19 pandemic. We have a broad definition of video calls that can be used to connect with their friends or family in their daily lives but excluded work-related calls or teletherapy. It could refer to a wide range of communication including using a smartphone, mobile/tablet device (e.g., iPad), webcam, etc., and using platforms such as Skype, Zoom, Google Meet, etc. The questions were created to understand 1) the usage of video calls, 2) the perceived satisfaction with video calls, 3) their confidence and competence in using video calls, 4) the quality of life affected by the use of video calls, and 5) needs and barriers to use video calls. All the responses about their video call usage could be based on the participants’ recall, and we did not ask them to have a more objective record (e.g., looking at the usage time in their device) before they answered the questions.
The procedures for the survey development were the following: initial development, expert and stakeholder review, revision, and pilot testing. We initially developed two versions of the survey, including separate surveys for OA and IWD. The draft surveys were sent to IWD and speech-language pathologists who have worked with IWD to obtain their feedback. In this review stage, all respondents with dementia relied on their proxies to complete the survey. Thus, the survey for IWD was modified for administration to proxies surrounding IWD instead of IWD themselves. We added to this survey the demographic questions about proxies and their relationship with IWD. Finally, we piloted the revised version of the surveys before distributing them to the community.
Data Collection
The survey was administered via the online survey platform Qualtrics (Provo, UT), and distributed to community members in the states of Iowa and Tennessee via email and flyers. The survey was open between February 15, 2021 and March 31, 2021. The survey study was approved by the Institutional Review Boards (IRBs) at the University of Tennessee Health Science Center (UTHSC) and the University of Iowa. The two versions of the surveys and raw data files are available through the first author’s OSF repository for the project (https://osf.io/x3vef/).
The study invitation and the survey link were distributed to elderly daycare centers, skilled nursing facilities, local support groups, and local community email lists, as well as by word-of-mouth. When potential respondents opened the survey link, captcha verification was completed first to block bots and then they were provided with information about the study. They indicated their consent to participate in the survey upon clicking to proceed to the next page. They first completed screening questions about the inclusionary criteria and if they were eligible, moved on to the survey questions. If they were not eligible, the survey automatically closed. The survey for older adults was composed of a total of 15 main questions with multiple choice options and open text boxes, including nine questions about the participant’s demographic information. There were branching questions that participants may have been asked depending on their response to the main question.
The survey for proxies consisted of 52 main questions. Compared to the OA survey, there were additional questions about (1) demographic information of the proxy, (2) the diagnosis and severity of disease in the IWD, 3) measuring the severity of the IWD’s conditions using the Dementia Severity Rating Scale (DSRS 35 ; and 4) the IWD’s experience of receiving speech-language therapy and if they have received therapy, their progress in the speech-language pathologist’s video call training practice. The questions about speech-language therapy in the survey instrument originated from a different research question that is beyond the goal of this research. The results that pertain to them will not be discussed further. All questions in the survey except for the screening questions were optional. The survey for OA took approximately 8 minutes and the survey for proxies took an average of 20 minutes to complete.
Data Analysis
In the main analysis, we used repeated measures ANOVA to test whether the two groups differed in the frequency of video call usage before and after the COVID-19 pandemic. Differences in call duration between the two groups were assessed using a linear regression model. Ordinal measures for video call frequency and duration were all treated as continuous for the analysis.36,37 In the IWD group, Spearman’s correlation analyses were also conducted to understand the relationships between the severity of dementia and the use of video calls before and after the COVID-19 pandemic. In all models reported, age and education level were included as covariates due to the significant differences between groups.
Using linear models with covariates for age and education, we also compared the groups in terms of their perceptions of video calls. Perceptions included levels of comfort, need in life for video calls, and the impact of video calls on their quality of life. In line with the analysis of video call frequency, ordinal measures for video call perceptions were also treated as continuous. Further, logistic regression models were used to test whether there was a difference between OA and IWD in preference for video calls or difficulty using them. Finally, we reported descriptive statistics to analyze the questions to understand their difficulties or challenges to use video calls.
Results
The Usage of Video Calls Before and After the COVID-19 Pandemic
Our primary analysis examined and compared the usage of video calls in OA and IWD before and after the COVID-19 pandemic. 1 Table 2 presents the respondents’ reported frequency of video call usage. Both OA and caregivers as proxies reported the increased use of video calls after the pandemic relative to before the pandemic. A repeated measures ANOVA was used to test whether reported increases in the use of video calls differed between the two groups before and after the pandemic (Appendix Table A2). Age and education were added as covariates since the participants in the OA group were significantly younger and more educated than the IWD group. The model revealed a significant interaction between group and time (F (1, 219) = 5.91, p = .02). OA used video calls significantly more than IWD before the COVID-19 pandemic (F (1, 219) = 16.37, P < .001), whereas the difference between groups becomes not statistically significant after the pandemic (F (1, 219) = 2.41, P = .12). The results suggest that both OA (F (1, 219) = 35.07, P < .001) and IWD (F (1, 219) = 47.10, P < .001) groups used video calls more after COVID-19 compared to before COVID-19, and the mean difference between groups after COVID-19 was reduced.
Table 2.
The Frequency of Video Call Use in OA and IWD (Reported by Proxies).
| IWD | OA | |
|---|---|---|
| Frequency before COVID-19 | ||
| More than five times per week | 1 (1.43%) | 5 (3.27%) |
| Three to four times per week | 1 (1.43%) | 7 (4.58%) |
| Once or twice per week | 3 (4.29%) | 22 (14.38%) |
| A few times per month | 4 (5.71%) | 34 (22.22%) |
| A few times per year | 22 (31.43%) | 42 (27.45%) |
| Not at all | 39 (55.71%) | 43 (28.10%) |
| Frequency after COVID-19 | ||
| More than five times per week | 4 (5.71%) | 10 (6.54%) |
| Three to four times per week | 4 (5.71%) | 14 (9.15%) |
| Once or twice per week | 10 (14.29%) | 38 (24.84%) |
| A few times per month | 16 (22.86%) | 37 (24.18%) |
| A few times per year | 18 (25.71%) | 32 (20.92%) |
| Not at all | 18 (25.71%) | 22 (14.38%) |
Note. IWD = Individuals with dementia; OA = Older adults.
The Usage of Video Calls and the Severity of Dementia
Within the IWD group, we examined the relationship between the severity of dementia as measured by DSRS 35 ; Appendix Table A1) and the use of video calls. The responses to the DSRS questions were summed across all questions to define each individual’s severity of dementia. The average severity was 22.0 (SD = 11.39), ranging from 3 to 51 (out of 54). The IWD participants in the study represented a wide range of dementia severity, from mild to severe. We conducted Spearman’s correlation analyses to examine the relationship between dementia severity and video call usage. Before COVID-19, as the severity of dementia increased, the use of video calls significantly decreased (r s = −.27, P = .02). Surprisingly, after COVID-19, the severity was no longer correlated with the video call usage, suggesting that all IWD tended to use more video calls after COVID-19, regardless of the severity of their dementia (r s = −.09, P = .48).
Perceptions Towards and Barriers to the Use of Video Calls
We asked the subset of respondents who indicated they have used video calls about their usage and preference for video calls (Table 3). After controlling for education and age in a linear regression model (R2 = .11, F (3, 218) = 8.62, P < .001), OA reported on average longer video call duration than IWD (B = .36, P = .02) (Appendix Table A3). Further, over fifty percent (51.54%) of the OA group and 62.79% of the IWD group reported that they preferred video calls over phone calls. However, a logistic regression model (Appendix Table A4) that adjusted for age and education revealed no significant difference between OA and IWD in preference for video calls over phone calls (OR = .58, P = .17)). Education was significantly associated with preference for video calls (OR = 1.12, P = .04).
Table 3.
Perception About Video Calls in IWD (Reported by Proxies) and OA.
| IWD | OA | |
|---|---|---|
| [Among the subset of respondents who indicated they have used video calls] | ||
| Average duration of a video call | ||
| Less than 5 minutes | 2 (4.65%) | 9 (6.87%) |
| 5-10 minutes | 12 (27.91%) | 31 (23.66%) |
| 10-30 minutes | 22 (51.16%) | 34 (25.95%) |
| 30 minutes to 1 hour | 6 (13.95%) | 38 (29.01%) |
| Longer than 1 hour | 1 (2.33%) | 19 (14.50%) |
| Preference of video calls over phone calls | ||
| Agree | 27 (62.79%) | 67 (51.54%) |
| Disagree | 16 (37.21%) | 63 (48.46%) |
| N/A (missing) | 1 (.76%) | |
| Experiencing difficulties in keeping in touch with family using video calls | ||
| Agree | 19 (44.19%) | 26 (19.85%) |
| Disagree | 24 (55.81%) | 105 (80.15%) |
| [All respondents] | ||
| I (or IWD) am comfortable with making video calls | ||
| Strongly Agree | 5 (7.14%) | 58 (37.91%) |
| Agree | 11 (15.71%) | 47 (30.72%) |
| Neutral | 6 (8.57%) | 21 (13.73%) |
| Disagree | 14 (20.00%) | 12 (7.84%) |
| Strongly Disagree | 33 (47.14%) | 5 (3.27%) |
| I (or caregiver) do not know | 1 (1.43%) | 10 (6.54%) |
| I (or IWD) enjoy video calls | ||
| Strongly Agree | 23 (32.86%) | 50 (32.68%) |
| Agree | 18 (25.71%) | 54 (35.29%) |
| Neutral | 5 (7.14%) | 28 (18.30%) |
| Disagree | 12 (17.14%) | 11 (7.19%) |
| Strongly Disagree | 10 (14.29%) | 1 (.65%) |
| I (or caregiver) do not know | 2 (2.86%) | 9 (5.88%) |
| Video calls improve the quality of my life | ||
| Strongly Agree | 18 (25.71%) | 46 (30.07%) |
| Agree | 14 (20.00%) | 52 (33.99%) |
| Neutral | 12 (17.14%) | 32 (20.92%) |
| Disagree | 7 (10.00%) | 11 (7.19%) |
| Strongly Disagree | 10 (14.29%) | 3 (1.96%) |
| I (or caregiver) do not know | 8 (11.43%) | 9 (5.88%) |
| I (or IWD) need video calls in my daily life | ||
| Strongly Agree | 11 (15.71%) | 12 (7.84%) |
| Agree | 14 (20.00%) | 26 (16.99%) |
| Neutral | 14 (20.00%) | 46 (30.07%) |
| Disagree | 16 (22.86%) | 39 (24.49%) |
| Strongly Disagree | 12 (17.14%) | 25 (16.34%) |
| I (or caregiver) do not know | 2 (2.86%) | 5 (3.27%) |
| IWD need training to use video calls | ||
| Strongly Agree | 21 (30.00%) | - |
| Agree | 9 (12.86%) | - |
| Neutral | 9 (12.86%) | - |
| Disagree | 4 (5.71%) | - |
| Strongly Disagree | 4 (5.71%) | - |
| Training/Learning is impossible | 22 (31.43%) | - |
| IWD requires assistance when making video calls | ||
| Strongly Agree | 41 (58.57%) | - |
| Agree | 13 (18.57%) | - |
| Neutral | 6 (8.57%) | - |
| Disagree | 4 (5.71%) | - |
| Strongly Disagree | 2 (2.86%) | - |
| I do not know | 3 (4.29%) | - |
| IWD can make video calls independently | ||
| Strongly Agree | 3 (4.29%) | - |
| Agree | 4 (5.71%) | - |
| Neutral | 2 (2.86%) | - |
| Disagree | 22 (31.43%) | - |
| Strongly Disagree | 36 (51.43%) | - |
| I do not know | 2 (2.86%) | - |
| Video calls with IWD provide significant benefits to me | ||
| Strongly Agree | 17 (24.29%) | - |
| Agree | 23 (32.86%) | - |
| Neutral | 12 (17.14%) | - |
| Disagree | 4 (5.71%) | - |
| Strongly Disagree | 5 (5.71%) | - |
| I do not know | 10 (14.29%) | - |
| Video calls of IWD with other people provide significant benefits to IWD | ||
| Strongly Agree | 18 (25.71%) | - |
| Agree | 29 (41.43%) | - |
| Neutral | 6 (8.57%) | - |
| Disagree | 3 (4.29%) | - |
| Strongly Disagree | 4 (5.71%) | - |
| I do not know | 10 (14.29%) | - |
Note. IWD = Individuals with dementia; OA = Older adults.
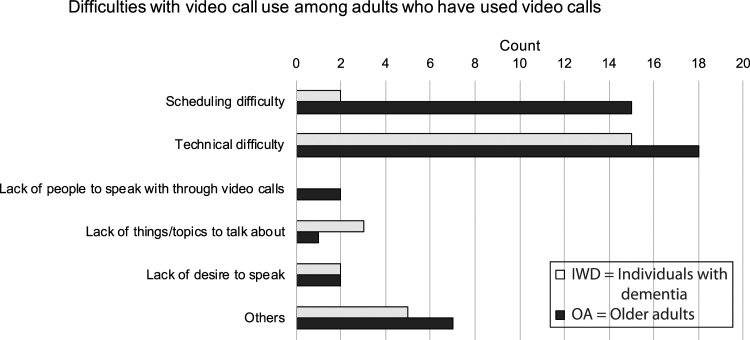
A second logistic regression model (Table A4) also showed IWD had 3.57 greater odds (P = .004) of experiencing difficulties in keeping in touch with family using video calls (44.19%) than OA (19.85%) after controlling for age and education. The most frequent difficulties were related to technical issues for both OA and IWD (Figure 1). Among OA, scheduling difficulties were the second most frequent difficulties experienced, whereas caregivers as proxies reported other challenges for IWD such as availability of caregivers to help or potential mental stress (e.g., getting more confused and distracted while using video calls than phone calls).
Figure 1.
Reported difficulties with video call use that the adults who have used video calls may encounter.
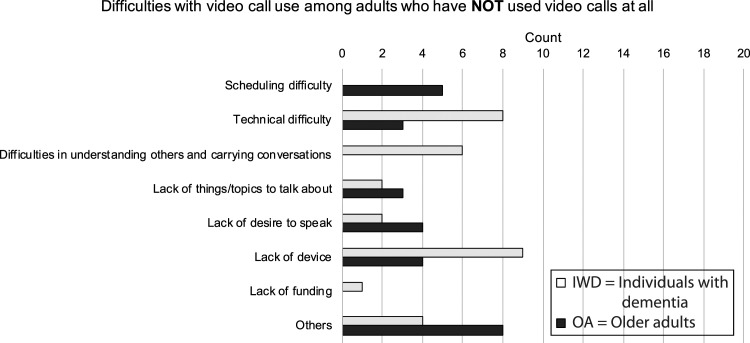
We separately analyzed the difficulties that adults who had not used video calls at all encountered (Figure 2). Different patterns were observed between the groups who had and the groups who had not used video calls previously. Among adults who had not used video calls before, the difficulties were more equally distributed across all options, although technical difficulties and lack of appropriate devices were the leading challenges. Other reasons included a lack of interest in using video calls or considering that video was not necessary.
Figure 2.
Reported difficulties with video call use that the adults who have not used video calls may encounter.
Simple linear regression compared perceptions towards video calls among IWD and OA, regardless of their past video call usage, controlling for age and education (Appendix Table A5). The model for video call comfort revealed that cognitive status (i.e., OA vs IWD) significantly predicted comfort in making video calls (B = 1.55, P < .001), with OA being more comfortable than IWD. A separate linear model evaluated beliefs that video calls improve quality of life, perceived need for video calls in daily life, and enjoyment of video calls, respectively (Appendix Table A5). After controlling for age and education, cognitive status was not a significant predictor of improved quality of life (B = .40, P = .09), perceived need for video calls in daily life (B = −.15, P = .47), and video call enjoyment (B = .41, P = .07). This finding suggests that although IWD may feel less comfortable to use video calls than OA, both groups equally recognize the need of video calls and enjoy using them regardless of their cognitive status, consistent with previous findings. 38
Although proxies also acknowledged the benefits of video calls to IWD (67.14%), only 10% of proxies reported that IWD could make video calls independently and 83% of them reported that IWD could not make video calls independently (Table 3). Further, they reported that most IWD required assistance when making video calls (77.14%) and needed training to use video calls (42.86%), but 31.43% of the proxies thought that training and learning were not possible for IWD. 52.86% of proxies provided training to IWD on how to use video calls and 60.00% of them reported that they provided cues or assistance to help IWD make video calls. Cues included demonstrations (23.89%), verbal instructions (30.09%), written instructions (9.73%), helping by directly manipulating devices and apps (23.01%), simulation/role-playing (7.08%), and others (6.19%). Proxies reported that helping directly or providing demonstrations helped IWDs the most.
Discussion
Communication is a means of meeting basic human needs for social connection and support. Due to the physical and social distancing practices and relevant restrictions during the COVID-19 pandemic, many people suffered from social isolation and consequently experienced detrimental psychological, physical, and mental effects, particularly those in vulnerable populations. Use of technology that can connect people virtually, such as video calls, rose during this pandemic and gained popularity as a way to overcome and compensate for the social isolation across individuals and households. The current survey suggests that there was indeed an increase in the use of video calls in cognitively healthy older adults after the pandemic began (see also Brown & Greenfield, 2020.) 25 This finding is consistent with reports that older adults listed social connection with loved ones via social media or video calls as a source of joy and comfort during the COVID-19 pandemic. 39
More importantly, this increase was not only observed in a cognitively healthy population, but also in people with a variety of dementias. Despite the neurodegenerative disease and varying severity of dementia, our survey findings indicated that IWDs increased use of video calls to speak with their friends and families after the pandemic began. Survey questions about video call usage instructed the respondents to exclude their video call usage for work, telemedicine, or teletherapy when responding, so the increase we describe in the current study is solely related to the need for social connection and communication.
Also, we found that there was no significant relationship between the severity of dementia and video call use after the COVID-19 pandemic. One possible explanation is that video call usage has increased for all levels of dementia severity. This can provide a piece of counterintuitive evidence, as people with advanced dementia are often considered to be incapable and apathetic and may not be given opportunities to connect socially, especially using technology.
Another important finding is that although the proxies for IWD reported that they prefer video calls over phone calls and benefitted as significantly from the use of video calls (e.g., improved quality of life) as did cognitively healthy older adults, there remained a substantial barrier to their use of video calls, which calls for attention. As increased social activity and participation can delay disease progression, it is important that people with dementia are given proper training and opportunities to participate in video calls and technology-mediated social communication, in addition to in-person communication and connections. More importantly, our survey results suggest that there are still nihilistic attitudes towards what people with dementia can do, as approximately one-third of proxies who are family, close friends, or caregivers reported that people with dementia could never learn or be trained to use video calls. As there is a myriad of evidence that learning and neuroplasticity still occur at least during the mild stages of dementia (e.g., Paek et al., 2021) 40 and that implicit learning approaches are appropriate for mild to moderate stages of dementia, 41 more education and support may be needed for both IWD and their caregivers to raise awareness about how to capitalize on remaining skills in people with dementia. For example, as our respondents reported, inclusion of step-by-step written instructions that are syntactically and semantically simple for people with dementia to understand may be an appropriate element of the training. This may be either combined with implicit memory approaches or allowed to stand alone as a means to support the use of video calls by the dementia population. As individuals with mild to moderate dementia are capable of learning technologies regardless of severity 42 and the importance of video calls is constantly increasing in society, it is important that healthcare professionals and care partners provide education and training directly or indirectly to clients with or without dementia and their family, caregivers, friends, and relevant stakeholders.
One thing to note is that all responses in the IWD group were reported by their proxies of IWD. This was inevitable due to their cognitive decline and difficulty administering the survey independently, which was observed during the pilot study. IWD often have difficulty correctly recalling their usage of video calls or making judgments on their perception of video calls. We decided to have the proxies complete the survey for the IWD to collect more accurate responses after piloting, but this might cause qualitatively limited data sets to directly compare between OA and IWD (i.e., self-reports from older adults vs proxy reports for individuals with dementia). Although all proxies were in close contact with IWD in their daily lives, their responses may reflect the proxy’s perspective rather than IWD’s opinion, especially regarding the questions about the perception of video calls. The current study undertook the first step in understanding the current video call usage in older adults with and without dementia in specific geographic regions and warrants further investigation by expanding the IWD group with different stages of dementia and dementia types across diverse regions and incorporating their self-reports assisted with the proxy’s support.
Limitations and Future Directions
The current study includes a few limitations. First, our sample size is relatively small and the racial and ethnic distribution is homogeneous. Most of our respondents were white and non-Hispanic. Future research will need to include more diverse populations, as there have been disparities in social, psychological, and medical findings across different races and ethnicities in the field of aging and dementia research. 43 It may also be necessary to break down the group of dementias as a function of diagnosis and dementia stage to investigate whether individuals with different types and severity of dementia exhibit different patterns of video call usage. It may be the case that people with severe visual impairments (i.e., posterior cortical atrophy due to Alzheimer’s disease) may not benefit from video calls any more than they do from phone calls. Further, the current study investigated the usage of video calls only with friends or family and thus excluded work-related calls or teletherapy. According to the recent increased demand of teletherapy, a comprehensive understanding of video call usage in older population requires an investigation including all types of video calls and telecommunication. Lastly, all responses from both groups were based on the participants’ recollection, not necessarily based on an objective measure (e.g., device/app usage time in their device). The reports about their video call usage before and after the pandemic heavily relied on their memory and this might be skewed and influence their responses.
In conclusion, we explored the usage of video calls in older adults with and without dementia possibly affected by the COVID-19 pandemic, and their perception of video call usage. The current results demonstrated that older adults become to use video calls more often after the pandemic, regardless of their cognitive status (OA vs IWD), and in the IWD group, their dementia severity is not correlated with the use of video calls after the pandemic. Both cognitively healthy adults and IWD acknowledged the potential benefits of using video calls in their daily lives, but IWD may encounter more barriers than OA, such as difficulty to make video calls independently. This finding suggests that there is an urgent need to develop training programs or strategies to help them use video calls more independently to facilitate social connections even in the era of social distancing.
In future studies, we will investigate healthcare providers working with individuals with dementia and older populations to understand the current clinical practice and recommendations related to the use, training, and education regarding video calls in older adults with and without dementia. Further, a direct link will need to be established between video call usage, the quality of social connection, and subsequent psychological and mental consequences (e.g., depression) in older populations to serve them better. 44 Our findings will offer significant insights into strategies to facilitate and promote social communication in older adults with and without dementia in this era of social distancing that will likely long outlast the COVID-19 pandemic.45,46
Appendix A.
Table A1.
The Diagnosis of Individuals with Dementia and the Results of DSRS (Dementia Severity Rating Scale).
| Response Count | Response Percentage, % | |
|---|---|---|
| Diagnosis a | ||
| Alzheimer’s dementia | 36 | 47.37 |
| Lewy Body dementia | 6 | 7.89 |
| Vascular dementia | 7 | 9.21 |
| Parkinson’s disease dementia | 9 | 11.84 |
| Primary progressive aphasia | 1 | 1.32 |
| Frontotemporal dementia | 2 | 2.63 |
| Others | 15 | 19.74 |
| Memory b | ||
| Normal memory | 0 | 0 |
| Occasionally forgets things that they were told recently. Does not cause many problems | 7 | 10.00 |
| Mild consistent forgetfulness. Remembers recent events but often forgets parts | 12 | 17.14 |
| Moderate memory loss. Worse for recent events. May not remember something you just told them. Causes problems with everyday activities | 18 | 25.71 |
| Substantial memory loss. Quickly forgets recent or newly-learned things. Can only remember things that they have known for a long time | 19 | 27.14 |
| Does not remember basic facts like the day of the week, when last meal was eaten or what the next meal will be | 12 | 17.14 |
| Does not remember even the most basic things | 2 | 2.86 |
| Speech and Language b | ||
| Normal ability to talk and to understand others | 8 | 11.43 |
| Sometimes cannot find a word, but able to carry on conversations | 23 | 32.86 |
| Often forgets words. May use the wrong word in its place. Some trouble expressing thoughts and giving answers | 19 | 27.14 |
| Usually answers questions using sentences but rarely starts a conversation remember something you just told them. Causes problems with everyday activities | 6 | 8.57 |
| Answers questions, but responses are often hard to understand or don’t make sense. Usually able to follow simple instructions | 9 | 12.86 |
| Speech often does not make sense. Can not answer questions or follow instructions | 4 | 5.71 |
| Does not respond most of the time | 0 | 0 |
| Recognition of family members b | ||
| Normal - recognizes people and generally knows who they are | 29 | 41.43 |
| Usually recognizes grandchildren, cousins or relatives who are not seen frequently but may not recall how they are related | 15 | 21.43 |
| Usually does not recognize family members who are not seen frequently. Is often confused about how family members such as grandchildren, nieces, or nephews are related to them | 9 | 12.86 |
| Sometimes does not recognize close family members or others who they see frequently. May not recognize their children, brothers, or sisters who are not seen on a regular basis | 10 | 14.29 |
| Frequently does not recognize spouse or caregiver | 6 | 8.57 |
| No recognition or awareness of the presence of others | 0 | 0 |
| Orientation to time b | ||
| Normal awareness of time of day and day of week | 13 | 18.57 |
| Some confusion about what time it is or what day of the week, but not severe enough to interfere with everyday activities | 32 | 45.71 |
| Frequently confused about time of day | 13 | 18.57 |
| Almost always confused about the time of day | 5 | 7.14 |
| Seems completely unaware of time | 6 | 8.57 |
| Orientation to place b | ||
| Normal awareness of where they are even in new places | 15 | 21.43 |
| Sometimes disoriented in new places | 22 | 31.43 |
| Frequently disoriented in new places | 14 | 20.00 |
| Usually disoriented, even in familiar places. May forget that they are already at home | 16 | 22.86 |
| Almost always confused about place | 3 | 4.29 |
| Ability to make decisions b | ||
| Normal - as able to make decisions as before | 5 | 7.14 |
| Only some difficulty making decisions that arise in day-to-day life | 11 | 15.71 |
| Moderate difficulty. Gets confused when things get complicated or plans change | 24 | 34.29 |
| Rarely makes any important decisions. Gets confused easily | 23 | 32.86 |
| Not able to understand what is happening most of the time | 7 | 10.00 |
| Social and Community activity b | ||
| Normal-acts the same with people as before | 3 | 4.29 |
| Only mild problems that are not really important, but clearly acts differently from previous years | 9 | 12.86 |
| Can still take part in community activities without help. May appear normal to people who don’t know them | 26 | 37.14 |
| Often has trouble dealing with people outside the home without help from caregiver. Usually can participate in quiet home activities with friends. The problem is clear to anyone who sees them | 25 | 35.71 |
| No longer takes part in any real way in activities at home involving other people. Can only deal with the primary caregiver | 6 | 8.57 |
| Little or no response even to primary caregiver | 1 | 1.43 |
| Home activities and Responsibilities b | ||
| Normal. No decline in ability to do things around the house | 3 | 4.29 |
| Some problems with home activities. May have more trouble with money management (paying bills) and fixing things. Can still go to a store, cook or clean. Still watches TV or reads a newspaper with interest and understanding | 20 | 28.57 |
| Makes mistakes with easy tasks like going to a store, cooking or cleaning. Losing interest in the newspaper, TV or radio. Often can’t follow a long conversation on a single topic | 25 | 35.71 |
| Not able to shop, cook or clean without a lot of help. Does not understand the newspaper or the TV. Cannot follow a conversation | 4 | 5.71 |
| No longer does any home-based activities | 18 | 25.71 |
| Personal care-Cleanliness b | ||
| Normal. Takes care of self as well as they used to | 17 | 24.29 |
| Sometimes forgets to wash, shave, comb hair, or may dress in wrong type of clothes. Not as neat as they used to be | 27 | 38.57 |
| Requires help with dressing, washing and personal grooming | 13 | 18.57 |
| Totally dependent on help for personal care | 13 | 18.57 |
| Eating b | ||
| Normal, does not need help in eating food that is served to them | 32 | 45.71 |
| May need help cutting food or have trouble with some foods, but basically able to eat by themselves | 22 | 31.43 |
| Generally able to feed themselves but may require some help. May lose interest during the meal | 15 | 21.43 |
| Needs to be fed. May have trouble swallowing | 1 | 1.43 |
| Control of urination and bowels b | ||
| Normal - does not have problems controlling urination or bowels except for physical problems | 29 | 41.43 |
| Rarely fails to control urination (generally less than one accident per month) | 11 | 15.71 |
| Occasional failure to control urination (about once a week or less) | 12 | 17.14 |
| Frequently fails to control urination (more than once a week) | 7 | 10.00 |
| Generally fails to control urination and frequently can not control bowels | 10 | 14.29 |
| Ability to get from place to place b | ||
| Normal, able to get around on their own. (May have physical problems that require a cane or walker) | 9 | 12.86 |
| Sometimes gets confused when driving or taking public transportation, especially in new places. Able to walk places alone | 9 | 12.86 |
| Cannot drive or take public transportation alone, even in familiar places. Can walk alone outside for short distances. Might get lost if walking too far from home | 22 | 31.43 |
| Cannot be left outside alone. Can get around the house without getting lost or confused | 14 | 20.00 |
| Gets confused and needs help finding their way around the house | 3 | 4.29 |
| Almost always in a bed or chair. May be able to walk a few steps with help, but lacks sense of direction | 11 | 15.71 |
| Always in bed. Unable to sit or stand | 1 | 1.43 |
Note that all question responses were optional.
aMultiple-choice question, select all that apply.
bMultiple-choice question, one answer only.
Table A2.
A Repeated Measures of ANOVA Results for Video Call Usage Before and After the Pandemic (Time: Before vs After the Pandemic; Cognitive Status: OA vs IWD).
| Predictor | F | P | Partial η2 |
|---|---|---|---|
| Within-subject effects | |||
| Time | .001 | .98 | 0 |
| Time*Cognitive Status | 5.91 | .02 | .03 |
| Time*Education | 4.52 | .04 | .02 |
| Time*Age | .008 | .93 | 0 |
| Error | |||
| Between-subject effects | |||
| Cognitive Status | 9.17 | .003 | .04 |
| Education | 1.35 | .25 | .01 |
| Age | .14 | .71 | .001 |
| Error | |||
| Group Contrasts | |||
| Before COVID | 16.37 | <.001 | .07 |
| After COVID | 2.41 | .12 | .01 |
| Time Contrasts | |||
| OA | 35.07 | <.001 | .14 |
| IWD | 47.10 | <.001 | .18 |
Note. IWD = Individuals with dementia; OA = Older adults.
Table A3.
Coefficients and Confidence Interval for Call Length Linear Models.
| B (SE) | 95% CI [LL, UL] | |
|---|---|---|
| Cognitive Status | .36 (.15) | [.06, .66] |
| Age | .004 (.01) | [-.02, .03] |
| Education | .09 (.02) | [.04, .13] |
| R 2 | .11 | |
Table A4.
Coefficients and Confidence Interval for Preference and Difficulty Logistic Regression Models.
| Model 1: Preference | Model 2: Difficulty | |||||
|---|---|---|---|---|---|---|
| B (SE) | OR | 95% CI (OR) [LL, UL] | B (SE) | OR | 95% CI (OR) [LL, UL] | |
| Cognitive Status | .58 (.42) | 1.78 | [.79, 4.02] | 1.27 (.44)** | 3.57 | [1.50, 8.49] |
| Age | .03 (.02) | 1.03 | [.98, 1.08] | −.02 (.03) | .99 | [.94, 1.04] |
| Education | .11 (.05)* | 1.12 | [1.01, 1.24] | .001 (.06) | 1.00 | [.89, 1.13] |
| Likelihood Ratio Test | χ2 (3) = 7.50, P = .06 | χ2 (3) = 9.67, P = .02 | ||||
**P < .01.
*P < .05.
Table A5.
Coefficients and Confidence Interval for Perceptions of Video Calls Linear Models.
| Model 1: Comfort | Model 2: Quality of Life | Model 3: Need | Model 4: Enjoy | |||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | 95% CI [LL, UL] | B (SE) | 95% CI [LL, UL] | B (SE) | 95% CI [LL, UL] | B (SE) | 95% CI [LL, UL] | |
| Cognitive Status | 1.55 (.22)*** | [1.12, 1.98] | .40 (.24) | [-.07, .86] | −.15 (.21) | [-.56, .26] | .41 (.22) | [-.03, .85] |
| Age | −.02 (.01) | [-.05, .01] | −.004 (.01) | [-.03, .02] | .02 (.01) | [-.01, .04] | −.002 (.01) | [-.03, .02] |
| Education | .07 (.03)* | [.01, .13] | .05 (.03) | [-.01, .10] | .03 (.03) | [-.02, .09] | .04 (.03) | [-.02, .09] |
| R 2 | .37 | .06 | .02 | .05 | ||||
***P < .001.
*P < .05.
Note
We asked the proxies about the use of video calls from two aspects: 1) their own use of video calls with IWD and 2) their observation about how their loved one with dementia used video calls with their family and friends. Responses for both aspects showed a similar pattern – increased frequency of using video calls after COVID-19 compared to the frequency before COVID-19. Here, we focused on reporting the latter aspect to make a comparison with healthy older adults, although we acknowledge that the direct experience of OA and indirect experience reported by proxies might be qualitatively different. We further discuss this point in the discussion.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health/National Institute on Aging Grant R03AG072236 to Eun Jin Paek and Si On Yoon.
ORCID iD
Eun Jin Paek, PhD https://orcid.org/0000-0002-3826-8243
References
- 1.Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676-684. [DOI] [PubMed] [Google Scholar]
- 2.Gunnar MR. Social buffering of stress in development: A career perspective. Perspect Psychol Sci. 2017;12(3):355-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCowan B, Beisner BA, Bliss-Moreau E, Vandeleest JJ, Jin J, Hannibal D, et al. Connections matter: Social networks and lifespan health in primate translational models. Front Psychol. 2016;7(433):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heid AR, Cartwright F, Wilson-Genderson M, Pruchno R. Challenges experienced by older people during the initial months of the COVID-19 pandemic. Gerontologist. 2021, 61;48-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sibley CG, Greaves LM, Satherley N, Wilson MS, Overall NC, Lee CHJ, et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am Psychol. 2020;75:618-630. [DOI] [PubMed] [Google Scholar]
- 6.Wei G, Diehl-Schmid J, Matias-Guiu JA, Pijnenburg Y, Landin-Romero R, Bogaardt H, et al. The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: An international multicentre study. Sci Rep. 2022;12(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zacher H, Rudolph CW. Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am Psychol. 2021;76(1):50-62. [DOI] [PubMed] [Google Scholar]
- 8.Krendl AC, Perry BL. The impact of sheltering in place during the Covid-19 pandemic on older adults’ social and mental well-being. J Gerontol B Psychol Sci Soc Sci. 2021;76:e53-e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toniolo S, Scarioni M, Di Lorenzo F, . Dementia and COVID-19, a bidirectional liaison: Risk factors, biomarkers, and optimal health care. J Alzheimers Dis. 2021;82(3):883-898. [DOI] [PubMed] [Google Scholar]
- 10.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the national institute on aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moreau N, Rauzy S, Viallet F, Champagne-Lavau M. Theory of mind in Alzheimer disease: Evidence of authentic impairment during social interaction. Neuropsychology. 2016;30(3):312-321. [DOI] [PubMed] [Google Scholar]
- 12.Feyereisen P, Berrewaerts J, Hupet M. Pragmatic skills in the early stages of Alzheimer’s disease: An analysis by means of a referential communication task. Int J Lang Commun Disord. 2007;42(1):1-17. [DOI] [PubMed] [Google Scholar]
- 13.Hugo J, Ganguli M. Dementia and cognitive impairment: Epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014;30:421-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weintraub S, Wicklund AH, Salmon DP. The neuropsychological profile of Alzheimer disease. Cold Spring Harb Perspect Med. 2012;2(1):a006171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hado E, Feinberg LF. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J. Aging Soc Policy. 2020;32(4-5):410-415. doi: 10.1080/08959420.2020.1765684 [DOI] [PubMed] [Google Scholar]
- 16.Alzheimer’s Association . Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2021;17(3):1-104. [DOI] [PubMed] [Google Scholar]
- 17.Di Marco LY, Marzo A, Muñoz-Ruiz M, Ikram MA, Kivipelto M, Ruefenacht D, et al. Modifiable lifestyle factors in dementia: A systematic review of longitudinal observational cohort studies. J Alzheimers Dis. 2014;42(1):119-135. [DOI] [PubMed] [Google Scholar]
- 18.Evans IEM, Martyr A, Collins R, Brayne C, Clare L. Social isolation and cognitive function in later life: A systematic review and meta-analysis. J Alzheimers Dis. 2019;70(s1):S119-S144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yates LA, Ziser S, Spector A, Orrell M. Cognitive leisure activities and future risk of cognitive impairment and dementia: Systematic review and meta-analysis. Int Psychogeriatr. 2016;28(11):1791-1806. [DOI] [PubMed] [Google Scholar]
- 20.Ballard C, Corbett A, Orrell M, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial. PLoS Med. 2018;15(2):e1002500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beerens HC, Zwakhalen SMG, Verbeek H, et al. The relation between mood, activity, and interaction in long-term dementia care. Aging Ment Health. 2018;22(1):26-32. [DOI] [PubMed] [Google Scholar]
- 22.Vigliotti AA, Chinchilli VM, George DR. Evaluating the benefits of the timeslips creative storytelling program for persons with varying degrees of dementia severity. Am J Alzheimers Dis Other Demen. 2019;34(3):163-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masterson-Algar P, Allen MC, Hyde M, Keating N, Windle G. Exploring the impact of Covid-19 on the care and quality of life of people with dementia and their carers: A scoping review,. Dementia. 2022;21:648-676. [Google Scholar]
- 24.Boutoleau-Bretonniere C, Pouclet-Courtemanche H, Gillet A, et al. The effects of confinement on neuropsychiatric symptoms in Alzheimer’s disease during the COVID-19 crisis. J Alzheimers Dis. 2020;76:41-47. 10.3233/JAD-200604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown G, Greenfield PM. Staying connected during stay-at-home: Communication with family and friends and its association with well-being. Hum Behav Emerg Technol. 2021;3(1):147-156. [Google Scholar]
- 26.Curelaru A, Marzolf SJ, Provost JCKG, Zeon HHH. Social isolation in dementia: The Effects of COVID-19. J Nurse Pract. 2021;17(8):950-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooper C, Mansour H, Carter C, et al. Social connectedness and dementia prevention: Pilot of the APPLE-Tree video-call intervention during the Covid-19 pandemic. Dementia. 2021;20(8):2779-2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shapira S, Yeshua-Katz D, Cohn-Schwartz E, Aharonson-Daniel L, Sarid O, Clarfield AM. A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interv. 2021;24:100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Croes E., Antheunis M. L., Schouten A. P., Krahmer E. J.. Social attraction in video-mediated communication: The role of nonverbal affiliative behavior. Journal of social and personal relationships 2019;36(4):1210-1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Malley C, Langton S, Anderson A, Doherty-Sneddon G, Bruce V. Comparison of face-to-face and video-mediated interaction. Interact Comput. 1996;8:177-192. [Google Scholar]
- 31.Lyons A, Reysen S, Pierce L. Video lecture format, student technological efficacy, and social presence in online courses. Comput Hum Behav. 2012;28:181-186. [Google Scholar]
- 32.Gell NM, Rosenberg DE, Demiris G, LaCroix AZ, Patel KV. Patterns of technology use among older adults with and without disabilities. Gerontologist. 2015;55:412-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman VA, Hu M, Kasper JD. Changes in older adults’ social contact during the COVID-19 pandemic. J Gerontol B Psychol Sci Soc Sci. 2022;77:e160-e166. doi: 10.1093/geronb/gbab166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chi W, Graf E, Hughes L, Hastie J, Khatutsky G, Shuman S, et al. Community-Dwelling Older Adults with Dementia and Their Caregivers: Key Indicators from the National Health and Aging Trends Study. Washington, DC: U.S. Department of Health and Human Services; 2019. https://aspe.hhs.gov/basic-report/community-dwelling-older-adults-dementia-and-their-caregivers-key-indicators-national-health-and-aging-trends-study [Google Scholar]
- 35.Clark CM, Ewbank DC. Performance of the dementia severity rating scale: A caregiver questionnaire for rating severity in Alzheimer disease. Alzheimer Dis Assoc Disord. 1996;10:31-39. [PubMed] [Google Scholar]
- 36.Mircioiu C, Atkinson J. A comparison of parametric and non-parametric methods applied to a likert scale. Pharmacy. 2017;5(2):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norman G. Likert scales, levels of measurement and the “laws” of statistics. Adv Health Sci Educ Theory Pract. 2010;15(5):625-632. [DOI] [PubMed] [Google Scholar]
- 38.Boman IL, Lundberg S, Starkhammar S, Nygard L. Exploring the usability of a videophone mock-up for persons with dementia and their significant others. BMC Geriatr. 2014;14:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whitehead BR, Torossian E. Older adults’ experience of the COVID-19 pandemic: A mixed-methods analysis of stresses and joys. Gerontologist. 2021;61:36-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paek EJ, Murray LL, Newman SD. Effects of concurrent action and object naming treatment on naming skills and functional brain activation patterns in primary progressive aphasia: An fMRI study with a case-series design. Brain Lang. 2021;218:104950. [DOI] [PubMed] [Google Scholar]
- 41.Murray LL, Paek EJ. Behavioral/nonpharmacological approaches to addressing cognitive-linguistic symptoms in individuals with dementia. Perspect ASHA Spec Interest Groups. 2016;1(15):12-25. [Google Scholar]
- 42.Kerkhof YJF, Bergsma A, Mangiaracina F, Planting CHM, Graff MJL, Dröes RM. Are people with mild dementia able to (re)learn how to use technology? A literature review. Int Psychogeriatr. 2021;34:113-128. [DOI] [PubMed] [Google Scholar]
- 43.Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimers Dement. 2016;12(3):216-224. doi: 10.1016/j.jalz.2015.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hajek A, König HH. Social isolation and loneliness of older adults in times of the COVID-19 pandemic: Can use of online social media sites and video chats assist in mitigating social isolation and loneliness? Gerontology. 2021;67(1):121-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J Med Internet Res. 2020;22:e19434. doi: 10.2196/19434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization . Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. URL. https://www.who.int/publications-detail/WHO-2019-nCoV-MentalHealth-2020.1