Abstract
Purpose
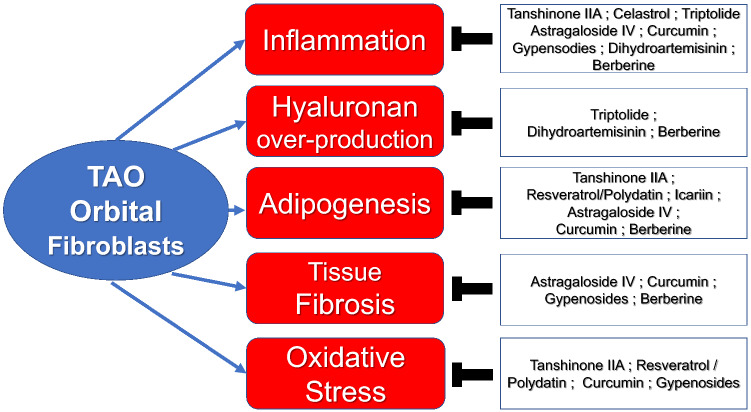
Orbital fibroblasts (OF) are considered the central target cells in the pathogenesis of thyroid-associated orbitopathy (TAO), which comprises orbital inflammation, orbital tissue edema, adipogenesis, fibrosis, oxidative stress and autophagy. Certain active ingredients of traditional Chinese medicine (TCM) demonstrated inhibition of TAO-OF in pre-clinical studies and they could be translated into novel therapeutic strategies.
Methods
The pertinent and current literature of pre-clinical studies on TAO investigating the effects of active ingredients of TCM was reviewed using the NCBI PubMed database.
Results
Eleven TCM compounds demonstrated inhibition of TAO-OF in-vitro and three of them (polydatin, curcumin, and gypenosides) resulted in improvement in TAO mouse models. Tanshinone IIA reduced inflammation, oxidative stress and adipogenesis. Both resveratrol and its precursor polydatin displayed anti-oxidative and anti-adipogenic properties. Celastrol inhibited inflammation and triptolide prevented TAO-OF activation, while icariin inhibited autophagy and adipogenesis. Astragaloside IV reduced inflammation via suppressing autophagy and inhibited fat accumulation as well as collagen deposition. Curcumin displayed multiple actions, including anti-inflammatory, anti-oxidative, anti-adipogenic, anti-fibrotic and anti-angiogenic effects via multiple signaling pathways. Gypenosides reduced inflammation, oxidative stress, tissue fibrosis, as well as oxidative stress mediated autophagy and apoptosis. Dihydroartemisinin inhibited OF proliferation, inflammation, hyaluronan (HA) production, and fibrosis. Berberine attenuated inflammation, HA production, adipogenesis, and fibrosis.
Conclusions
Clinical trials of different phases with adequate power and sound methodology will be warranted to evaluate the appropriate dosage, safety and efficacy of these compounds in the management of TAO.
Keywords: Traditional Chinese medicine, thyroid-associated orbitopathy; Orbital fibroblasts; Autophagy; Inflammation; Oxidative stress
Introduction
Thyroid-associated orbitopathy (TAO), also termed Graves’ orbitopathy, is an orbital inflammatory disorder related to autoimmune thyroid disease and is the most common extrathyroidal manifestation of Graves’ disease (GD) [1–5]. The classical features of TAO include soft tissue inflammation, upper eyelid retraction, diplopia, proptosis, as well as rare but sight-threatening complications due to dysthyroid optic neuropathy or corneal breakdown [6, 7]. Owing to significant disfigurement and disability, TAO compromises patients’ psychological well-being and incurs a huge socioeconomic burden [8–12]. Over the past two decades, important pharmacological advances in the management of TAO remarkably improved patients’ outcomes and quality of life. However, the current treatment options have limitations in terms of response rates, potential toxicities, geographical availability, and affordability, therefore the search for novel treatment strategies is warranted and ongoing [5, 13–17]. Importantly, various active ingredients of traditional Chinese medicine (TCM) demonstrated potential therapeutic benefits in in-vitro and animal studies of TAO. In this review, we provide a brief overview of the pathogenesis of TAO and summarize how these TCM compounds may provide novel therapeutics insights in TAO.
Pathophysiology of TAO
The exact pathogenesis of TAO remains unclear, although most researchers have considered TAO an orbital inflammatory disorder related to autoimmune thyroid disease [15, 18–20]. The pathological hallmarks of TAO include orbital inflammatory infiltration, over-production of hydrophilic glycosaminoglycans, de novo adipogenesis, and tissue fibrosis. In the presence of genetic, autoimmune and environmental factors, autoimmune T cells, B cells, and OF are activated by unbalanced immune tolerance, resulting in a series of inflammatory responses, including cellular and humoral immunity [21, 22]. The overproduction of hydrophilic glycosaminoglycans, especially hyaluronan (HA), leads to orbital tissue edema, which, together with de novo adipogenesis, causes orbital tissue expansion [6, 18, 23, 24]. These pathological processes explain most of the clinical manifestations of TAO.
Orbital fibroblasts (OF) are considered the central cells in the pathogenesis of TAO [6, 15, 18, 19, 23, 24]. OF-mediated interaction with immune cells via the production of different cytokines and chemokines is the primary mechanism for maintaining orbital inflammation in TAO [24, 25], and most pathological processes and clinical features of TAO involve OF. Thyrotropin receptor (TSH-R) acts as the principal autoantigen in GD and TAO. TSH-R autoantibody (TSH-R-Ab) is the specific biomarker and major pathogenic autoantibody in these disorders, and its titer was positively correlated with the activity and severity of TAO [26–32]. Upon stimulation by TSH-R-Ab, TSH-R/insulin growth factor-1 receptor (IGF-1R) crosstalk signaling pathway represents the most important mechanism of OF activation, including overproduction of HA [18, 19], differentiation into adipocytes [23, 24], and differentiation into myofibroblasts induced by transforming growth factor (TGF)-β, interleukin (IL)-17A and IL-23A resulting in tissue remodeling and fibrosis [18, 19]. In addition, the activation of OF also produces cytokines and chemokines (e.g. IL-6, IL-8, IL-16, and monocyte chemoattractant protein-1 [MCP-1]), and perpetuates orbital inflammation [33].
Oxidative stress, defined as an imbalance between the production and elimination of reactive oxygen species (ROS), plays a major role in TAO [18, 34–36]. Oxygen radicals induced the proliferation of OF and the expression of 72-kDa heat shock protein, leading to the production of ROS and oxidative stress [18, 34, 35]. In contrast to healthy controls, various substances involved in oxidative stress, including superoxide dismutase, superoxide anions, malondialdehyde, hydrogen peroxide, and glutathione reductase, were significantly increased in the OF of patients with TAO (TAO-OF) [34]. Cigarette smoking, which is the most important environmental risk factor of TAO, enhanced the in-vitro ROS synthesis and suppressed the antioxidant machinery [7, 18]. Selenium, an antioxidant, reduced the proliferation of OF and the production of glycosaminoglycans and hyaluronan, and benefited patients with mild TAO [37, 38]. In addition, several other antioxidants, including beta-carotene, N‑acetyl cysteine, vitamin C, and melatonin, demonstrated therapeutic efficacy in in-vitro studies of TAO-OF [37, 39].
Autophagy, a natural and destructive mechanism that allows orderly degradation and recycling of unnecessary cellular components, has also been implicated in the pathogenesis of TAO recently [40]. Autophagy plays an adaptive role in cell survival, development, differentiation and intracellular homeostasis [41]. Autophagy is recognized as a ‘self-cannibalizing’ process that is active during stress (e.g. starvation, chemotherapy, infection, aging, and hypoxia) to protect organisms from various irritants and to regenerate materials and energy. However, autophagy can also lead to a form of programmed cell death distinct from apoptosis [41]. In the immune system, autophagy regulates antigen uptake and presentation, pathogen removal, immune cell survival, and cytokine-dependent inflammation [42]. Insufficient and excessive autophagic activities have been implicated in several autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), Crohn’s disease, and multiple sclerosis [43]. A study showed that autophagy, induced by the pro-inflammatory cytokine IL-1β, was upregulated in TAO orbital tissues and blocking autophagy inhibited adipogenic differentiation [40]. Therefore, inhibiting autophagy may become a therapeutic target in TAO.
In summary, OF are mainly involved in orbital inflammation, orbital tissue expansion, adipogenesis, fibrosis, oxidative stress and autophagy in TAO. Inhibiting TAO-OF by interrupting one or more of the above pathological processes represents a major direction in developing novel therapeutic strategies.
Potential therapeutic effects of TCM active ingredients in TAO
Eleven active ingredients of traditional Chinese medicine demonstrated potential therapeutic benefits in in-vitro experiments using OF, and three of them (polydatin, curcumin, and gypenosides) showed favorable effects in TAO mouse models. They are reviewed in this session and the mechanisms of action of these compounds in relation to the pathophysiology of TAO is summarized in Fig. 1.
Fig. 1.
Active ingredients in traditional Chinese medicine: mechanisms of action shown in pre-clinical TAO studies
Tanshinone IIA
Tanshinone IIA, a lipophilic diterpene, is the most abundant active ingredient extracted from the Chinese herb Salvia miltiorrhiza bunge (Danshen) and it has been widely used to treat ischemic heart disease and cerebrovascular disease in the Chinese community for many centuries, owing to its proposed anti-inflammatory and anti-oxidative properties [44].
Tanshinone IIA demonstrated anti-inflammatory, anti-oxidative and anti-adipogenic effects on TAO-OF in an in-vitro study [45]. Tanshinone IIA inhibited IL-1β-induced expression of pro-inflammatory cytokines (IL-6, IL-8, and MCP-1), reduced cigarette smoke extract or H2O2-induced generation of ROS, and upregulated the expression of the anti-oxidative enzyme heme oxygenase-1 (HO-1) through activating extracellular signal-regulated kinase (ERK) signaling pathway. The expression of adipogenesis-related factors (peroxisome proliferator-activated receptor gamma, PPARγ; CCAAT-enhancer-binding protein alpha, C/EBPα) was downregulated. These results were consistent with findings from recent non-OF in-vitro studies, which confirmed the anti-inflammatory, anti-oxidative, as well as antifibrotic properties of tanshinone IIA [44, 46, 47].
Resveratrol
Resveratrol, a well-known polyphenol phytoalexin, is extracted from the roots of the Chinese herb Polygonum cuspidatum (Huzhang) and multitudinous fruits (e.g. grapes, and berries). It has been extensively utilized and prescribed in TCM practice [48, 49]. Resveratrol demonstrated immunomodulatory effects in-vitro via various signaling pathways (e.g. arachidonic acid, nuclear factor kappa B [NF-κb], mitogen-activated protein kinase (MAPK) and anti-oxidant defense pathways [50]). Multiple studies employing animal models of inflammatory bowel disease showed that resveratrol exerted anti-inflammatory action via targeting various molecular targets and signaling pathways (e.g. NF-κb, Sirtuin-1 [SIRT1], mammalian target of rapamycin [mTOR], hypoxia-inducible factor-1α [HIF-1α], microRNA [miRNAs], nuclear factor erythroid 2-related factor 2 [NRF2], tumor necrosis factor-alpha [TNFα], and autophagy) [51]. In two double-blind placebo-controlled randomized clinical trials, supplementation with resveratrol improved clinical disease activity and quality of life in patients with ulcerative colitis, via reducing inflammation and oxidative stress [52, 53].
Treatment with resveratrol attenuated oxidative stress and suppressed adipogenesis in TAO-OF [54]. Resveratrol inhibited ROS production stimulated by cigarette smoke extract and H2O2. It reduced levels of HO-1, copper/zinc-superoxide dismutase [SOD], catalase and thioredoxin, but increased the level of manganese-SOD, reflecting regulation in the expression of anti-oxidative defenses. Resveratrol counteracted rosiglitazone (PPARγ agonist) induced adipogenesis, as evidenced by a decreased number of adipocytes and the accumulation of intracellular lipid droplets. Furthermore, alterations in the levels of transcriptional regulators suggested that resveratrol modulated ERK, JNK and NF-κB signaling pathways.
Polydatin
Polydatin, a glycoside and natural precursor of resveratrol, similarly displayed anti-oxidative and anti-adipogenic properties in both in-vitro and in-vivo models [55]. It inhibited H2O2-induced ROS production by cultured non-TAO-OFs in a dose-dependent manner, while silencing NRF2 decreased the anti-oxidative effect of polydatin. In a TAO mouse model, treatment with polydatin reduced ROS production. The attenuation in orbital oxidative stress was associated with a lower level of Keap1, as well as a higher level of nuclear located NRF2 and antioxidant genes (e.g. NAD(P)H dehydrogenase, quinone 1 [NQO1]), suggesting that polydatin mediated anti-oxidative effect via stimulating Keap1/NRF2/ARE pathway. Polydatin also inhibited adipose tissue expansion and lipid droplet accumulation in retrobulbar fat of TAO mice, reflecting suppression of adipogenesis.
Celastrol
Celastrol, a natural triterpene, is isolated from the root extracts of Tripterygium wilfordii and Tripterygium regelii, both from the Celastraceae family. It suppressed inflammatory responses in experimental models of various autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease, SLE, psoriasis and type 1 diabetes [56]. The potential mechanisms of celastrol-mediated anti-inflammatory and anti-oxidative effects include preventing the production and expression of pro-inflammatory cytokines, promoting the heat-shock response, inhibiting the generation of inducible nitric oxide synthase and lipid peroxidation, as well as restoring the level of autophagy [57].
In an in-vitro study [58], celastrol significantly reduced IL-1β-induced expression of pro-inflammatory molecules (IL‑6, IL‑8, prostaglandin E2, cyclooxygenase-2 [COX-2], intercellular adhesion molecule‑1 [ICAM-1]) in TAO-OF. The anti-inflammatory action of celastrol was mediated through inhibition of the NF-κB signaling pathway, as evidenced by suppression of IL-1β induced phosphorylation of IκBα (an inhibitor of NF-κB). This is consistent with the observation that celastrol attenuated inflammation in experimental models of osteoarthritis and rheumatoid arthritis by inhibiting the NF-κB signaling pathway [57, 59].
Triptolide
Triptolide, a diterpene triepoxide, is another pharmacologically active component of Tripterygium wilfordii Hook F from the Celastraceae family. It has been used as a remedy for various inflammatory and autoimmune disorders, including lupus nephritis, rheumatoid arthritis, inflammatory bowel disease, and asthma [60]. In an in-vitro study, triptolide effectively inhibited interferon-γ induced activation of TAO-OF, as evidenced by reduced expression of human leukocyte antigen (HLA)-DR, ICAM-1, and CD40, as well as suppression of cellular proliferation and HA synthesis [61].
Icariin
Icariin, a flavonoid isolated from several species of plants in the genus Epimedium, has several pharmacological properties, such as immunomodulatory, anti-inflammatory, anti-oxidative and lipid-lowering effects [62, 63]. Adipogenesis and autophagy were considered two important mechanisms in TAO [18, 24, 40]. Adipogenesis involves the process of autophagy, which is regulated by two factors, mTOR and 5' adenosine monophosphate-activated protein kinase (AMPK, a serine-threonine kinase that functions as a metabolic sensor and activates autophagy in response to low energy levels) [64]. Icariin attenuated cardiomyocyte hypertrophy induced by isoproterenol in mice, by suppressing apoptosis and promoting autophagic flux. Isoproterenol promoted phosphorylation of AMPK (p-AMPK) and inhibited phosphorylation of mTOR (p-mTOR), while icariin reversed these effects, suggesting that the cardioprotective effect was mediated through AMPK/mTOR signaling pathway [62].
The effects of Icariin were evaluated in both in-vitro study and in-vivo TAO mouse model [64]. Icariin inhibited the differentiation of preadipocytes into adipocytes through the suppression of autophagy, which was a key process essential for adipogenesis. Similarly, it suppressed adipogenesis in orbital tissues in terms of PPARγ expression and lipid droplet accumulation, while it partially reversed the enhanced autophagy observed in TAO mice. The inhibition of adipogenesis by icariin, which decreased p-AMPK and increased p-mTOR levels in both in-vitro and in-vivo studies, was probably mediated by the suppression of autophagy through AMPK/mTOR signaling pathway. Furthermore, Pingmu decoction (composed of a mixture of herbs including Epimedium Brevicornu Maxim) reduced viability/proliferation of TAO-preadipocytes and induced apoptosis of TAO-adipocytes, by activating programmed cell death via Fas/Fas ligand signaling pathway [65, 66].
Astragaloside IV
The Chinese herbs Radix Astragali Mongolici (Huangqi), the dried root of leguminous plants Mongolia, is widely prescribed to treat cardiovascular disorders, hepatitis, kidney disease, and skin diseases in China [67, 68]. Astragaloside IV, a tetracyclic triterpenoid saponin, has been identified as one of the bioactive ingredients in Huangqi [67]. It has been reported to possess anti-oxidative, cardioprotective, anti-inflammatory, antimicrobial, antifibrotic, anti-diabetic, and immunoregulatory properties [69]. Astragaloside IV was effective in inhibiting pro-inflammatory macrophages and promoting the pro-resolving macrophages to ameliorate experimental inflammatory bowel disease via the regulation of the STAT signaling pathway [69]. Astragaloside IV improved oxidative stress-mediated endothelial dysfunction relevant to cardiovascular diseases through several mechanisms: preventing the uncoupling of endothelial nitric oxide synthase (eNOS), increasing eNOS and nitric oxide (NO), and enhancing several activating enzymes to activate the antioxidant system [70].
Astragaloside IV demonstrated an anti-inflammatory effect, which was mediated by suppression of autophagy, in both in-vitro and in vivo models of TAO [71]. It inhibited IL-1β-induced expression of pro-inflammatory cytokines (IL-6, IL-8, TNF-α, and MCP-1) in non-TAO-OF. Rapamycin (an autophagy activator) significantly enhanced, but autophagy inhibitors or silencing autophagy-related proteins attenuated inflammation of non-TAO-OF, suggesting that autophagy was involved in IL-1β mediated inflammatory response. Pre-treatment with astragaloside IV strongly inhibited IL-1β induced autophagy and prevented rapamycin from enhancing IL-1β mediated inflammation. In the TAO mouse model, astragaloside IV administration resulted in lower serum levels of thyroid hormones, TSH-R-Ab and pro-inflammatory cytokines. The orbital tissues of astragaloside IV-treated TAO mice also displayed significant improvement, as evidenced by a reduction in fat accumulation, collagen deposition, macrophage infiltration, as well as autophagic activity.
Curcumin
Curcumin is an active ingredient extracted from Curcuma longa, a traditional Chinese medicinal herb with a long history of use as a treatment for inflammatory conditions in China and Southeast Asia [72]. Curcumin has strong anti-oxidative and anti-inflammatory activities and was tested in more than 100 clinical trials in various chronic diseases, including inflammatory bowel disease, rheumatoid arthritis and psoriasis [72].
The effects of curcumin on TAO-OF were evaluated in two separate in-vitro studies. Curcumin inhibited the production of proinflammatory cytokines induced by IL-1β (IL-6, IL-8, MCP-1, ICAM-1). Upon induction of adipogenic differentiation, curcumin significantly reduced intracellular lipid droplet accumulation and levels of adipogenic transcription factors (PPARγ, C/EBPα, and C/EBPβ), reflecting suppression of adipogenesis. H2O2 or cigarette smoke extract stimulated ROS production was also attenuated by pretreatment with curcumin. Curcumin inhibited phosphorylation of multiple signaling molecules (ERK, JNK, NF-κB, p65), and stimulated nuclear translocation of β-catenin during adipogenesis which probably resulted in increased expression of downstream anti-adipogenic genes [73].
In another study curcumin demonstrated anti-fibrotic and anti-angiogenic properties [74], Transforming growth factor beta 1 (TGFβ1) induced expression of myofibroblast differentiation markers (connective tissue growth factor, CTGF; alpha-smooth muscle actin, α-SMA) and phosphorylation of SMAD2/3 (major signal transducers for receptors of TGFβ superfamily) were suppressed by curcumin, therefore curcumin inhibited TGFβ1 induced myofibroblast differentiation of TAO-OF. The conditioned medium from curcumin-treated TAO-OF reduced the TGFβ1-induced migratory ability and tube-forming capacity of endothelial cell lines in-vitro, hence curcumin inhibited the TGFβ1 mediated pro-angiogenic effect on TAO-OF.
Gypenosides
Gypenosides are saponins and represent the most pharmacologically active component of Gynostemma pentaphyllum. Their biological actions include: regulating the activation of immune cells and the expression of cytokines [75]; decreasing inflammatory response in inflammatory bowel disease by inhibiting NF-κB and signal transducer and activator of transcription 3 (STAT3) signal pathways [76]; and inhibiting differentiation of hepatic progenitor cells into myofibroblasts and hence hepatic fibrosis by inhibiting the expression of TGF-β1, TGF-β1 receptor 1 and SMAD2/3 [77, 78].
Gypenosides displayed anti-inflammatory, anti-fibrotic and anti-oxidative effects in two separate in-vitro studies employing TAO-OF [75, 79]. Pretreatment with gypenosides significantly attenuated IL-1β-induced expression of pro-inflammatory cytokines (IL-6, IL-8, TNFα, CCL2) by TAO-OF, via reducing activation of Toll-like receptors 4 (TLR4)/NF-κB signaling pathway. TGFβ1 induced upregulation of fibrotic markers (hyaluronic acid, α-SMA, collagen type 1, fibronectin) in TAO-OF was prevented by gypenosides, through inhibiting SMAD2/4 signaling pathway [75].
In another study [79], gypenosides decreased oxidative stress via NRF2/ERK/HO-1 signaling pathway, as well as inhibited autophagy and apoptosis in TAO-OF treated with H2O2. They enhanced H2O2-stimulated malondialdehyde production but attenuated H2O2-induced SOD expression, suggesting regulation in the level of oxidative stress in TAO-OF. Gypenosides further promoted H2O2-induced expression NRF2/ERK/HO-1 proteins, while they inhibited H2O2-induced autophagy, as evidenced by reduced expression of autophagy activation-related proteins and reduced number of autophagosomes/autophagolysosomes. The anti-apoptotic effect was suggested by reducing the expression of apoptosis-related mRNA (caspase 3, BAX) and apoptosis rate of TAO-OF treated with H2O2. In addition, through in silico methods (including gene ontology analysis, protein–protein interaction network construction, and molecular docking), gypenosides might play an anti-inflammatory and anti-oxidative role in TAO via STAT1/3 signaling pathways [80]. Nonetheless, the therapeutic potential of gypenosides needs to be verified by further in-vitro and in-vivo studies.
Dihydroartemisinin
Dihydroartemisinin is a derivative of artemisinin, a sesquiterpene lactone extracted from the Chinese herb Artemisia annua L. It is widely used in the treatment of fever and malaria [81]. Many in vivo experiments in disease-relevant animal models demonstrated the therapeutic efficacy of artemisinin-type drugs against rheumatic diseases, inflammatory bowel disease, and other inflammatory and autoimmune diseases [82, 83]. Apart from their antimalarial efficacy, artemisinin compounds demonstrated remarkable antifibrotic properties in multiple preclinical disease models [81]. For instance, dihydroartemisinin inhibited pulmonary inflammation/fibrosis and arthritis in animal models by suppressing JAK2/STAT3 signaling pathway [84, 85]. In an SLE mouse model, dihydroartemisinin ameliorated disease manifestation by inhibiting the senescence of myeloid-derived suppressor cells via activating NRF2/HO-1 signaling pathway [86]. Furthermore, dihydroartemisinin was shown to attenuate lipopolysaccharide-induced acute kidney injury via the inhibition of inflammatory mediators and oxidative stress [87].
Dihydroartemisinin demonstrated potent anti-inflammatory and antifibrotic effects on TAO-OF [88]. It reduced HA production and mRNA expression of pro-inflammatory cytokines, chemokines (IL-6, IL-8, CXCL-1, MCP-1, ICAM-1), as well as HA synthases, suggesting inhibition of IL-1β induced inflammation. Dihydroartemisinin inhibited proliferation, migration capacity and wound-healing ability of TAO-OF. Dihydroartemisinin significantly downregulated TGFβ1-induced expression of fibrosis markers (e.g. α-SMA, CTGF) at both mRNA and protein levels. As dihydroartemisinin decreased TGFβ1-induced phosphorylation of ERK1/2 and STAT3, its anti-fibrotic action was likely mediated via suppression of ERK and STAT3 signaling pathways.
Berberine
Berberine, an isoquinoline alkaloid extracted from the Chinese herb Coptidis rhizoma (Huanglian), demonstrated multiple biological functions, including anti-inflammatory and anti-bacterial effects, alleviation of liver fibrosis, inhibition of carcinogenesis, cardiometabolic protection, as well as neuroprotection [89–92].
Berberine exerted inhibition on TAO-OF in an in-vitro experiment by suppressing inflammation, HA production, fibrosis, adipogenesis [93]. It attenuated IL-1β-induced expression of pro-inflammatory mediators (IL-6, PTX-3, and COX-2) via inactivating NF-κB signaling pathway. Berberine also inhibited TGFβ1 induced HA production and mRNA expression of HA synthases. Various fibrotic markers were downregulated at both mRNA and protein levels. A reduction of intracellular fat accumulation and various adipogenic markers at both mRNA and protein level was evident when TAO-OF undergoing adipogenic differentiation were treated with berberine. The suppression of adipogenesis was mediated through inhibiting AMPK and PPARγ signaling pathways.
Hydroxypropyl-berberrubine, an analog of berberine metabolite, significantly decreased cholesterol level by upregulating low-density lipoprotein receptor (LDL-R) and downregulating proprotein convertase subtilisin/kexin type 9 (PCSK9) in-vitro. Hypercholesterolemia itself was associated with increased risk and disease activity, as well as decreased response to intravenous glucocorticoid in TAO [94–96]. Statin, a class of well-established cholesterol-lowering agents, inhibited TAO-OF in-vitro [97–99], and atorvastatin was recently shown in a randomized controlled trial to enhance the clinical efficacy of intravenous glucocorticoid therapy in patients with active moderate-to-severe TAO [100]. Therefore, berberine may be beneficial in the management of TAO. Furthermore, the efficacy of berberine in Graves’ hyperthyroidism was also evaluated in a small non-randomized clinical trial [101]. Compared with methimazole monotherapy, the addition of berberine was associated with higher chance of normalizing TSH level and lower TSH-R-Ab levels at 6 months. Combination treatment also significantly modified the composition of gut microbiota, with an increased abundance of beneficial bacteria Lactococcus lactis and a reduced abundance of pathogenic bacteria Enterobacter hormaechei and Chryseobacterium indologenes. The potential beneficial effects of berberine on Graves’ hyperthyroidism and TAO will need to be further evaluated in larger clinical trials.
Potential roles of TCM in Graves’ hyperthyroidism
Given the potential therapeutic effects of various TCM compounds on TAO and the shared pathogenesis between GD and TAO, TCM compounds could also be beneficial in the clinical management of Graves’ hyperthyroidism. Compared with antithyroid drug (ATD) monotherapy, ATD/TCM herbal combination more effectively reduced goiter size and relieved hypermetabolic symptoms in small clinical trials. Combined treatment may also offer both control of hyperthyroidism and desensitization in the setting of ATD allergy [102]. Acupuncture, an important TCM technique, is probably the most popular alternative therapy practiced in western countries, and its anti-inflammatory and immunomodulatory properties may also have potential therapeutic roles in TAO [103].
Conclusions
Various active ingredients in TCM demonstrated inhibition of TAO-OF in-vitro and improved TAO in mouse models in-vivo. The growing interaction between conventional western medicine and TCM will help identify the effective molecules in herbal medicine with therapeutic implications and define precisely their role in clinical management [103]. Clinical trials of different phases with adequate power and sound methodology will be warranted to evaluate the appropriate dosage, safety and efficacy of these compounds in the management of TAO.
Funding
Open Access funding enabled and organized by Projekt DEAL. None.
Declarations
Conflict of interest
All authors stated that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals.
Informed consent
No informed consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Y. P. Hai and A. C. H. Lee shared co-first authorship and contributed equally to the preparation of the manuscript.
Contributor Information
Y. P. Hai, Email: haiyuanping2018@163.com
A. C. H. Lee, Email: qcalanov@gmail.com
K. Chen, Email: kainch@sina.com
G. J. Kahaly, Email: george.kahaly@unimedizin-mainz.de
References
- 1.Bartalena L, Fatourechi V. Extrathyroidal manifestations of Graves' disease: a 2014 update. J Endocrinol Invest. 2014;37(8):691–700. doi: 10.1007/s40618-014-0097-2. [DOI] [PubMed] [Google Scholar]
- 2.Ippolito S, Cusini C, Lasalvia P, Gianfagna F, Veronesi G, Gallo D, Masiello E, Premoli P, Sabatino J, Mercuriali A, Lai A, Piantanida E, Tanda ML, Bartalena L. Change in newly diagnosed Graves' disease phenotype between the twentieth and the twenty-first centuries: meta-analysis and meta-regression. J Endocrinol Invest. 2021;44(8):1707–1718. doi: 10.1007/s40618-020-01479-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piantanida E, Tanda ML, Lai A, Sassi L, Bartalena L. Prevalence and natural history of Graves' orbitopathy in the XXI century. J Endocrinol Invest. 2013;36(6):444–449. doi: 10.3275/8937. [DOI] [PubMed] [Google Scholar]
- 4.Kahaly GJ, Bartalena L, Hegedus L, Leenhardt L, Poppe K, Pearce SH. 2018 European thyroid association guideline for the management of graves' hyperthyroidism. Eur Thyroid J. 2018;7(4):167–186. doi: 10.1159/000490384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartalena L, Kahaly GJ, Baldeschi L, Dayan CM, Eckstein A, Marcocci C, Marino M, Vaidya B, Wiersinga WM, Dagger E. The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves' orbitopathy. Eur J Endocrinol. 2021;185(4):G43–G67. doi: 10.1530/EJE-21-0479. [DOI] [PubMed] [Google Scholar]
- 6.Bartalena L, Tanda ML. Current concepts regarding Graves' orbitopathy. J Intern Med. 2022;292(5):692–716. doi: 10.1111/joim.13524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartalena L, Piantanida E, Gallo D, Lai A, Tanda ML. Epidemiology, natural history, risk factors, and prevention of Graves' orbitopathy. Front Endocrinol (Lausanne). 2020;11:615993. doi: 10.3389/fendo.2020.615993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ponto KA, Pitz S, Pfeiffer N, Hommel G, Weber MM, Kahaly GJ. Quality of life and occupational disability in endocrine orbitopathy. Dtsch Arztebl Int. 2009;106(17):283–289. doi: 10.3238/arztebl.2009.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ponto KA, Kahaly GJ. Quality of life in patients suffering from thyroid orbitopathy. Pediatr Endocrinol Rev. 2010;7(Suppl 2):245–249. [PubMed] [Google Scholar]
- 10.Ponto KA, Hommel G, Pitz S, Elflein H, Pfeiffer N, Kahaly GJ. Quality of life in a german graves orbitopathy population. Am J Ophthalmol. 2011;152(3):483–490.e1. doi: 10.1016/j.ajo.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 11.Ponto KA, Merkesdal S, Hommel G, Pitz S, Pfeiffer N, Kahaly GJ. Public health relevance of Graves' orbitopathy. J Clin Endocrinol Metab. 2013;98(1):145–152. doi: 10.1210/jc.2012-3119. [DOI] [PubMed] [Google Scholar]
- 12.Hoppe E, Lee ACH, Hoppe D, Kahaly GJ. Predictive factors for changes in quality of life after steroid treatment for active moderate-to-severe graves' orbitopathy: a prospective trial. Eur Thyroid J. 2021;9(6):313–320. doi: 10.1159/000508071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kahaly GJ. Immunotherapies for thyroid eye disease. Curr Opin Endocrinol Diabetes Obes. 2019;26(5):250–255. doi: 10.1097/MED.0000000000000493. [DOI] [PubMed] [Google Scholar]
- 14.Lee ACH, Kahaly GJ. Novel approaches for immunosuppression in graves' hyperthyroidism and associated orbitopathy. Eur Thyroid J. 2020;9(Suppl 1):17–30. doi: 10.1159/000508789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neag EJ, Smith TJ. 2021 update on thyroid-associated ophthalmopathy. J Endocrinol Invest. 2022;45(2):235–259. doi: 10.1007/s40618-021-01663-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee ACH, Riedl M, Frommer L, Diana T, Kahaly GJ. Systemic safety analysis of mycophenolate in Graves' orbitopathy. J Endocrinol Invest. 2020;43(6):767–777. doi: 10.1007/s40618-019-01161-z. [DOI] [PubMed] [Google Scholar]
- 17.Bartalena L, Marino M, Marcocci C, Tanda ML. Teprotumumab for Graves' orbitopathy and ototoxicity: moving problems from eyes to ears? J Endocrinol Invest. 2022;45(7):1455–1457. doi: 10.1007/s40618-022-01791-w. [DOI] [PubMed] [Google Scholar]
- 18.Lee ACH, Kahaly GJ. Pathophysiology of thyroid-associated orbitopathy. Best Pract Res Clin Endocrinol Metab. 2022 doi: 10.1016/j.beem.2022.101620. [DOI] [PubMed] [Google Scholar]
- 19.Hai YP, Saeed MEM, Ponto KA, Elflein HM, Lee ACH, Fang S, Zhou H, Frommer L, Langericht J, Efferth T, Kahaly GJ. A multicenter, single-blind, case-control, immunohistochemical study of orbital tissue in thyroid eye disease. Thyroid. 2022;32(12):1547–1558. doi: 10.1089/thy.2022.0173. [DOI] [PubMed] [Google Scholar]
- 20.Hai YP, Lee ACH, Frommer L, Diana T, Kahaly GJ. Immunohistochemical analysis of human orbital tissue in Graves' orbitopathy. J Endocrinol Invest. 2020;43(2):123–137. doi: 10.1007/s40618-019-01116-4. [DOI] [PubMed] [Google Scholar]
- 21.Fang S, Lu Y, Huang Y, Zhou H, Fan X. Mechanisms that underly T cell immunity in Graves' orbitopathy. Front Endocrinol (Lausanne). 2021;12:648732. doi: 10.3389/fendo.2021.648732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang Y, Fang S, Zhang S, Zhou H. Progress in the pathogenesis of thyroid-associated ophthalmopathy and new drug development. Taiwan J Ophthalmol. 2020;10(3):174–180. doi: 10.4103/tjo.tjo_18_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khong JJ, McNab AA, Ebeling PR, Craig JE, Selva D. Pathogenesis of thyroid eye disease: review and update on molecular mechanisms. Br J Ophthalmol. 2016;100(1):142–150. doi: 10.1136/bjophthalmol-2015-307399. [DOI] [PubMed] [Google Scholar]
- 24.Dik WA, Virakul S, van Steensel L. Current perspectives on the role of orbital fibroblasts in the pathogenesis of Graves' ophthalmopathy. Exp Eye Res. 2016;142:83–91. doi: 10.1016/j.exer.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 25.Taylor PN, Zhang L, Lee RWJ, Muller I, Ezra DG, Dayan CM, Kahaly GJ, Ludgate M. New insights into the pathogenesis and nonsurgical management of Graves orbitopathy. Nat Rev Endocrinol. 2020;16(2):104–116. doi: 10.1038/s41574-019-0305-4. [DOI] [PubMed] [Google Scholar]
- 26.Diana T, Ungerer M, Wuster C, Fassbender J, Li Z, Reimann A, Holthoff HP, Kanitz M, Kahaly GJ. A cyclic peptide significantly improves thyroid function, thyrotropin-receptor antibodies and orbital mucine/collagen content in a long-term Graves' disease mouse model. J Autoimmun. 2021;122:102666. doi: 10.1016/j.jaut.2021.102666. [DOI] [PubMed] [Google Scholar]
- 27.Kahaly GJ, Diana T, Olivo PD. Tsh receptor antibodies: relevance & utility. Endocr Pract. 2020;26(1):97–106. doi: 10.4158/EP-2019-0363. [DOI] [PubMed] [Google Scholar]
- 28.Kahaly GJ, Diana T, Kanitz M, Frommer L, Olivo PD. Prospective trial of functional thyrotropin receptor antibodies in Graves disease. J Clin Endocrinol Metab. 2020;105(4):e1006–e1014. doi: 10.1210/clinem/dgz292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diana T, Ponto KA, Kahaly GJ. Thyrotropin receptor antibodies and Graves' orbitopathy. J Endocrinol Invest. 2021;44(4):703–712. doi: 10.1007/s40618-020-01380-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahaly GJ, Wuster C, Olivo PD, Diana T. High titers of thyrotropin receptor antibodies are associated with orbitopathy in patients with Graves disease. J Clin Endocrinol Metab. 2019;104(7):2561–2568. doi: 10.1210/jc.2018-02705. [DOI] [PubMed] [Google Scholar]
- 31.Diana T, Olivo PD, Kahaly GJ. Thyrotropin receptor blocking antibodies. Horm Metab Res. 2018;50(12):853–862. doi: 10.1055/a-0723-9023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diana T, Kahaly GJ. Thyroid stimulating hormone receptor antibodies in thyroid eye disease-methodology and clinical applications. Ophthalmic Plast Reconstr Surg. 2018;34(4S Suppl 1):S13–S19. doi: 10.1097/IOP.0000000000001053. [DOI] [PubMed] [Google Scholar]
- 33.Hwang CJ, Afifiyan N, Sand D, Naik V, Said J, Pollock SJ, Chen B, Phipps RP, Goldberg RA, Smith TJ, Douglas RS. Orbital fibroblasts from patients with thyroid-associated ophthalmopathy overexpress CD40: CD154 hyperinduces IL-6, IL-8, and MCP-1. Invest Ophthalmol Vis Sci. 2009;50(5):2262–2268. doi: 10.1167/iovs.08-2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hou TY, Wu SB, Kau HC, Tsai CC. The role of oxidative stress and therapeutic potential of antioxidants in Graves' ophthalmopathy. Biomedicines. 2021 doi: 10.3390/biomedicines9121871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lanzolla G, Marcocci C, Marino M. Oxidative stress in graves disease and graves orbitopathy. Eur Thyroid J. 2020;9(Suppl 1):40–50. doi: 10.1159/000509615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marique L, Senou M, Craps J, Delaigle A, Van Regemorter E, Werion A, Van Regemorter V, Mourad M, Nyssen-Behets C, Lengele B, Baldeschi L, Boschi A, Brichard S, Daumerie C, Many MC. Oxidative stress and upregulation of antioxidant proteins, including adiponectin, in extraocular muscular cells, orbital adipocytes, and thyrocytes in Graves' disease associated with orbitopathy. Thyroid. 2015;25(9):1033–1042. doi: 10.1089/thy.2015.0087. [DOI] [PubMed] [Google Scholar]
- 37.Rotondo Dottore G, Ionni I, Menconi F, Casini G, Sellari-Franceschini S, Nardi M, Vitti P, Marcocci C, Marino M. Action of three bioavailable antioxidants in orbital fibroblasts from patients with Graves' orbitopathy (GO): a new frontier for GO treatment? J Endocrinol Invest. 2018;41(2):193–201. doi: 10.1007/s40618-017-0718-7. [DOI] [PubMed] [Google Scholar]
- 38.Marcocci C, Kahaly GJ, Krassas GE, Bartalena L, Prummel M, Stahl M, Altea MA, Nardi M, Pitz S, Boboridis K, Sivelli P, von Arx G, Mourits MP, Baldeschi L, Bencivelli W, Wiersinga W, O. European Group on Graves Selenium and the course of mild Graves' orbitopathy. N Engl J Med. 2011;364(20):1920–1931. doi: 10.1056/NEJMoa1012985. [DOI] [PubMed] [Google Scholar]
- 39.Rotondo Dottore G, Ionni I, Menconi F, Casini G, Sellari-Franceschini S, Nardi M, Vitti P, Marcocci C, Marino M. Antioxidant effects of beta-carotene, but not of retinol and vitamin E, in orbital fibroblasts from patients with Graves' orbitopathy (GO) J Endocrinol Invest. 2018;41(7):815–820. doi: 10.1007/s40618-017-0809-5. [DOI] [PubMed] [Google Scholar]
- 40.Yoon JS, Lee HJ, Chae MK, Lee EJ. Autophagy is involved in the initiation and progression of Graves' orbitopathy. Thyroid. 2015;25(4):445–454. doi: 10.1089/thy.2014.0300. [DOI] [PubMed] [Google Scholar]
- 41.Chai P, Ni H, Zhang H, Fan X. The evolving functions of autophagy in ocular health: a double-edged sword. Int J Biol Sci. 2016;12(11):1332–1340. doi: 10.7150/ijbs.16245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shibutani ST, Saitoh T, Nowag H, Munz C, Yoshimori T. Autophagy and autophagy-related proteins in the immune system. Nat Immunol. 2015;16(10):1014–1024. doi: 10.1038/ni.3273. [DOI] [PubMed] [Google Scholar]
- 43.Yang Z, Goronzy JJ, Weyand CM. Autophagy in autoimmune disease. J Mol Med (Berl) 2015;93(7):707–717. doi: 10.1007/s00109-015-1297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guo R, Li L, Su J, Li S, Duncan SE, Liu Z, Fan G. Pharmacological activity and mechanism of tanshinone IIA in related diseases. Drug Des Devel Ther. 2020;14:4735–4748. doi: 10.2147/DDDT.S266911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rhiu S, Chae MK, Lee EJ, Lee JB, Yoon JS. Effect of tanshinone IIA in an in vitro model of Graves' orbitopathy. Invest Ophthalmol Vis Sci. 2014;55(9):5900–5910. doi: 10.1167/iovs.14-14008. [DOI] [PubMed] [Google Scholar]
- 46.Feng F, Cheng P, Xu S, Li N, Wang H, Zhang Y, Wang W. Tanshinone IIA attenuates silica-induced pulmonary fibrosis via Nrf2-mediated inhibition of EMT and TGF-beta1/Smad signaling. Chem Biol Interact. 2020;319:109024. doi: 10.1016/j.cbi.2020.109024. [DOI] [PubMed] [Google Scholar]
- 47.Yuan L, Li Q, Zhang Z, Liu Q, Wang X, Fan L. Tanshinone IIA inhibits the adipogenesis and inflammatory response in ox-LDL-challenged human monocyte-derived macrophages via regulating miR-130b/WNT5A. J Cell Biochem. 2020;121(2):1400–1408. doi: 10.1002/jcb.29375. [DOI] [PubMed] [Google Scholar]
- 48.Ma BN, Li XJ. Resveratrol extracted from Chinese herbal medicines: a novel therapeutic strategy for lung diseases. Chin Herb Med. 2020;12(4):349–358. doi: 10.1016/j.chmed.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang LX, Li CX, Kakar MU, Khan MS, Wu PF, Amir RM, Dai DF, Naveed M, Li QY, Saeed M, Shen JQ, Rajput SA, Li JH. Resveratrol (RV): a pharmacological review and call for further research. Biomed Pharmacother. 2021;143:112164. doi: 10.1016/j.biopha.2021.112164. [DOI] [PubMed] [Google Scholar]
- 50.Meng T, Xiao D, Muhammed A, Deng J, Chen L, He J. Anti-inflammatory action and mechanisms of resveratrol. Molecules. 2021 doi: 10.3390/molecules26010229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gowd V, Kanika, Jori C, Chaudhary AA, Rudayni HA, Rashid S, Khan R. Resveratrol and resveratrol nano-delivery systems in the treatment of inflammatory bowel disease. J Nutr Biochem. 2022;109:109101. doi: 10.1016/j.jnutbio.2022.109101. [DOI] [PubMed] [Google Scholar]
- 52.Samsami-Kor M, Daryani NE, Asl PR, Hekmatdoost A. Anti-inflammatory effects of resveratrol in patients with ulcerative colitis: a randomized, double-blind placebo-controlled pilot study. Arch Med Res. 2015;46(4):280–285. doi: 10.1016/j.arcmed.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 53.Samsamikor M, Daryani NE, Asl PR, Hekmatdoost A. Resveratrol supplementation and oxidative/anti-oxidative status in patients with ulcerative colitis: a randomized, double-blind placebo-controlled pilot study. Arch Med Res. 2016;47(4):304–309. doi: 10.1016/j.arcmed.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 54.Kim CY, Lee HJ, Chae MK, Byun JW, Lee EJ, Yoon JS. Therapeutic effect of resveratrol on oxidative stress in Graves' orbitopathy orbital fibroblasts. Invest Ophthalmol Vis Sci. 2015;56(11):6352–6361. doi: 10.1167/iovs.15-16870. [DOI] [PubMed] [Google Scholar]
- 55.Li H, Min J, Chen Y, Li H, Zhang Y. Polydatin attenuates orbital oxidative stress in Graves' orbitopathy through the NRF2 pathway. Chem Biol Interact. 2020;315:108894. doi: 10.1016/j.cbi.2019.108894. [DOI] [PubMed] [Google Scholar]
- 56.Venkatesha SH, Dudics S, Astry B, Moudgil KD. Control of autoimmune inflammation by celastrol, a natural triterpenoid. Pathog Dis. 2016 doi: 10.1093/femspd/ftw059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Feng K, Chen H, Xu C. Chondro-protective effects of celastrol on osteoarthritis through autophagy activation and NF-kappaB signaling pathway inhibition. Inflamm Res. 2020;69(4):385–400. doi: 10.1007/s00011-020-01327-z. [DOI] [PubMed] [Google Scholar]
- 58.Li H, Yuan Y, Zhang Y, He Q, Xu R, Ge F, Wu C. Celastrol inhibits IL-1beta-induced inflammation in orbital fibroblasts through the suppression of NF-kappaB activity. Mol Med Rep. 2016;14(3):2799–2806. doi: 10.3892/mmr.2016.5570. [DOI] [PubMed] [Google Scholar]
- 59.Jing M, Yang J, Zhang L, Liu J, Xu S, Wang M, Zhang L, Sun Y, Yan W, Hou G, Wang C, Xin W. Celastrol inhibits rheumatoid arthritis through the ROS-NF-kappaB-NLRP3 inflammasome axis. Int Immunopharmacol. 2021;98:107879. doi: 10.1016/j.intimp.2021.107879. [DOI] [PubMed] [Google Scholar]
- 60.Yuan K, Li X, Lu Q, Zhu Q, Jiang H, Wang T, Huang G, Xu A. Application and mechanisms of triptolide in the treatment of inflammatory diseases-a review. Front Pharmacol. 2019;10:1469. doi: 10.3389/fphar.2019.01469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yan SX, Wang Y. Inhibitory effects of triptolide on interferon-gamma-induced human leucocyte antigen-DR, intercellular adhesion molecule-1, CD40 expression on retro-ocular fibroblasts derived from patients with Graves' ophthalmopathy. Clin Exp Ophthalmol. 2006;34(3):265–271. doi: 10.1111/j.1442-9071.2006.01190.x. [DOI] [PubMed] [Google Scholar]
- 62.Hu L, Wang Z, Li H, Wei J, Tang F, Wang Q, Wang J, Zhang X, Zhang Q. Icariin inhibits isoproterenol-induced cardiomyocyte hypertropic injury through activating autophagy via the AMPK/mTOR signaling pathway. Biochem Biophys Res Commun. 2022;593:65–72. doi: 10.1016/j.bbrc.2022.01.029. [DOI] [PubMed] [Google Scholar]
- 63.Luo Z, Dong J, Wu J. Impact of Icariin and its derivatives on inflammatory diseases and relevant signaling pathways. Int Immunopharmacol. 2022;108:108861. doi: 10.1016/j.intimp.2022.108861. [DOI] [PubMed] [Google Scholar]
- 64.Li H, Yuan Y, Zhang Y, Zhang X, Gao L, Xu R. Icariin inhibits AMPK-dependent autophagy and adipogenesis in adipocytes in vitro and in a model of Graves' orbitopathy in vivo. Front Physiol. 2017;8:45. doi: 10.3389/fphys.2017.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li H, Wang Y, Xu R. Pingmu decoction enhances apoptosis of orbital adipocytes derived from patients with Graves' ophthalmophathy. Mol Med Rep. 2012;6(6):1361–1366. doi: 10.3892/mmr.2012.1080. [DOI] [PubMed] [Google Scholar]
- 66.Zhang Y, Li H, Gao L, Zhang X, Xie R. Pingmu decoction induces orbital preadipocytes apoptosis in vitro. Evid Based Complement Alternat Med. 2017;2017:2109249. doi: 10.1155/2017/2109249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang Y, Hong M, Lian WW, Chen Z. Review of the pharmacological effects of astragaloside IV and its autophagic mechanism in association with inflammation. World J Clin Cases. 2022;10(28):10004–10016. doi: 10.12998/wjcc.v10.i28.10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chang X, Chen X, Guo Y, Gong P, Pei S, Wang D, Wang P, Wang M, Chen F. Advances in chemical composition, extraction techniques, analytical methods, and biological activity of astragali radix. Molecules. 2022 doi: 10.3390/molecules27031058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tian L, Zhao JL, Kang JQ, Guo SB, Zhang N, Shang L, Zhang YL, Zhang J, Jiang X, Lin Y. Astragaloside IV alleviates the experimental DSS-induced colitis by remodeling macrophage polarization through STAT signaling. Front Immunol. 2021;12:740565. doi: 10.3389/fimmu.2021.740565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Meng P, Yang R, Jiang F, Guo J, Lu X, Yang T, He Q. Molecular mechanism of astragaloside IV in improving endothelial dysfunction of cardiovascular diseases mediated by oxidative stress. Oxid Med Cell Longev. 2021;2021:1481236. doi: 10.1155/2021/1481236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li H, Zhang Y, Min J, Gao L, Zhang R, Yang Y. Astragaloside IV attenuates orbital inflammation in Graves' orbitopathy through suppression of autophagy. Inflamm Res. 2018;67(2):117–127. doi: 10.1007/s00011-017-1100-0. [DOI] [PubMed] [Google Scholar]
- 72.He Y, Yue Y, Zheng X, Zhang K, Chen S, Du Z. Curcumin, inflammation, and chronic diseases: how are they linked? Molecules. 2015;20(5):9183–9213. doi: 10.3390/molecules20059183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee JS, Kim J, Lee EJ, Yoon JS. Therapeutic effect of curcumin, a plant polyphenol extracted from curcuma longae, in fibroblasts from patients with Graves' orbitopathy. Invest Ophthalmol Vis Sci. 2019;60(13):4129–4140. doi: 10.1167/iovs.19-27376. [DOI] [PubMed] [Google Scholar]
- 74.Yu WK, Hwang WL, Wang YC, Tsai CC, Wei YH. Curcumin suppresses TGF-beta1-induced myofibroblast differentiation and attenuates angiogenic activity of orbital fibroblasts. Int J Mol Sci. 2021 doi: 10.3390/ijms22136829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li H, Ma C, Liu W, He J, Li K. Gypenosides protect orbital fibroblasts in Graves ophthalmopathy via anti-inflammation and anti-fibrosis effects. Invest Ophthalmol Vis Sci. 2020;61(5):64. doi: 10.1167/iovs.61.5.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wong WY, Lee MM, Chan BD, Ma VW, Zhang W, Yip TT, Wong WT, Tai WC. Gynostemma pentaphyllum saponins attenuate inflammation in vitro and in vivo by inhibition of NF-kappaB and STAT3 signaling. Oncotarget. 2017;8(50):87401–87414. doi: 10.18632/oncotarget.20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Song YN, Dong S, Wei B, Liu P, Zhang YY, Su SB. Metabolomic mechanisms of gypenoside against liver fibrosis in rats: an integrative analysis of proteomics and metabolomics data. PLoS One. 2017;12(3):e0173598. doi: 10.1371/journal.pone.0173598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen J, Li X, Hu Y, Liu W, Zhou Q, Zhang H, Mu Y, Liu P. Gypenosides ameliorate carbon tetrachloride-induced liver fibrosis by inhibiting the differentiation of hepatic progenitor cells into myofibroblasts. Am J Chin Med. 2017;45(5):1061–1074. doi: 10.1142/S0192415X17500574. [DOI] [PubMed] [Google Scholar]
- 79.Ma C, Li H, Liu W, Lu S, Li X, Chen J, Li K, Wang W. Therapeutic effect of gypenosides on antioxidant stress injury in orbital fibroblasts of Graves' orbitopathy. J Immunol Res. 2022;2022:4432584. doi: 10.1155/2022/4432584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li K, Li H, Xu W, Liu W, Du Y, He JF, Ma C. Research on the potential mechanism of gypenosides on treating thyroid-associated ophthalmopathy based on network pharmacology. Med Sci Monit. 2019;25:4923–4932. doi: 10.12659/MSM.917299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dolivo D, Weathers P, Dominko T. Artemisinin and artemisinin derivatives as anti-fibrotic therapeutics. Acta Pharm Sin B. 2021;11(2):322–339. doi: 10.1016/j.apsb.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Efferth T, Oesch F. The immunosuppressive activity of artemisinin-type drugs towards inflammatory and autoimmune diseases. Med Res Rev. 2021;41(6):3023–3061. doi: 10.1002/med.21842. [DOI] [PubMed] [Google Scholar]
- 83.Tong X, Chen L, He SJ, Zuo JP. Artemisinin derivative SM934 in the treatment of autoimmune and inflammatory diseases: therapeutic effects and molecular mechanisms. Acta Pharmacol Sin. 2022;43(12):3055–3061. doi: 10.1038/s41401-022-00978-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang M, Wu D, Xu J, Liu L, Jiao W, Yu J, Chen G. Suppression of NLRP3 inflammasome by dihydroarteannuin via the HIF-1alpha and JAK3/STAT3 signaling pathway contributes to attenuation of collagen-induced arthritis in mice. Front Pharmacol. 2022;13:884881. doi: 10.3389/fphar.2022.884881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.You X, Jiang X, Zhang C, Jiang K, Zhao X, Guo T, Zhu X, Bao J, Dou H. Dihydroartemisinin attenuates pulmonary inflammation and fibrosis in rats by suppressing JAK2/STAT3 signaling. Aging (Albany NY). 2022;14(3):1110–1127. doi: 10.18632/aging.203874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li D, Qi J, Wang J, Pan Y, Li J, Xia X, Dou H, Hou Y. Protective effect of dihydroartemisinin in inhibiting senescence of myeloid-derived suppressor cells from lupus mice via Nrf2/HO-1 pathway. Free Radic Biol Med. 2019;143:260–274. doi: 10.1016/j.freeradbiomed.2019.08.013. [DOI] [PubMed] [Google Scholar]
- 87.Liu X, Lu J, Liao Y, Liu S, Chen Y, He R, Men L, Lu C, Chen Z, Li S, Xiong G, Yang S. Dihydroartemisinin attenuates lipopolysaccharide-induced acute kidney injury by inhibiting inflammation and oxidative stress. Biomed Pharmacother. 2019;117:109070. doi: 10.1016/j.biopha.2019.109070. [DOI] [PubMed] [Google Scholar]
- 88.Yang S, Wang X, Xiao W, Xu Z, Ye H, Sha X, Yang H. Dihydroartemisinin exerts antifibrotic and anti-inflammatory effects in Graves' ophthalmopathy by targeting orbital fibroblasts. Front Endocrinol (Lausanne). 2022;13:891922. doi: 10.3389/fendo.2022.891922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu X, Wang L, Tan S, Chen Z, Wu B, Wu X. Therapeutic effects of berberine on liver fibrosis are associated with lipid metabolism and intestinal flora. Front Pharmacol. 2022;13:814871. doi: 10.3389/fphar.2022.814871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Och A, Och M, Nowak R, Podgorska D, Podgorski R. Berberine, a herbal metabolite in the metabolic syndrome: the risk factors, course, and consequences of the disease. Molecules. 2022 doi: 10.3390/molecules27041351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lu Q, Fu Y, Li H. Berberine and its derivatives represent as the promising therapeutic agents for inflammatory disorders. Pharmacol Rep. 2022;74(2):297–309. doi: 10.1007/s43440-021-00348-7. [DOI] [PubMed] [Google Scholar]
- 92.Wang S, Ren H, Zhong H, Zhao X, Li C, Ma J, Gu X, Xue Y, Huang S, Yang J, Chen L, Chen G, Qu S, Liang J, Qin L, Huang Q, Peng Y, Li Q, Wang X, Zou Y, Shi Z, Li X, Li T, Yang H, Lai S, Xu G, Li J, Zhang Y, Gu Y, Wang W. Combined berberine and probiotic treatment as an effective regimen for improving postprandial hyperlipidemia in type 2 diabetes patients: a double blinded placebo controlled randomized study. Gut Microbes. 2022;14(1):2003176. doi: 10.1080/19490976.2021.2003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Diao J, Chen X, Mou P, Ma X, Wei R. Potential therapeutic activity of berberine in thyroid-associated ophthalmopathy: inhibitory effects on tissue remodeling in orbital fibroblasts. Invest Ophthalmol Vis Sci. 2022;63(10):6. doi: 10.1167/iovs.63.10.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sabini E, Mazzi B, Profilo MA, Mautone T, Casini G, Rocchi R, Ionni I, Menconi F, Leo M, Nardi M, Vitti P, Marcocci C, Marino M. High serum cholesterol is a novel risk factor for Graves' orbitopathy: results of a cross-sectional study. Thyroid. 2018;28(3):386–394. doi: 10.1089/thy.2017.0430. [DOI] [PubMed] [Google Scholar]
- 95.Lanzolla G, Sabini E, Profilo MA, Mazzi B, Sframeli A, Rocchi R, Menconi F, Leo M, Nardi M, Vitti P, Marcocci C, Marino M. Relationship between serum cholesterol and Graves' orbitopathy (GO): a confirmatory study. J Endocrinol Invest. 2018;41(12):1417–1423. doi: 10.1007/s40618-018-0915-z. [DOI] [PubMed] [Google Scholar]
- 96.Naselli A, Moretti D, Regalbuto C, Arpi ML, Lo Giudice F, Frasca F, Belfiore A, Le Moli R. Evidence that baseline levels of low-density lipoproteins cholesterol affect the clinical response of Graves' ophthalmopathy to parenteral corticosteroids. Front Endocrinol (Lausanne). 2020;11:609895. doi: 10.3389/fendo.2020.609895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shahida B, Johnson PS, Jain R, Brorson H, Asman P, Lantz M, Planck T. Simvastatin downregulates adipogenesis in 3T3-L1 preadipocytes and orbital fibroblasts from Graves' ophthalmopathy patients. Endocr Connect. 2019;8(9):1230–1239. doi: 10.1530/EC-19-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wei YH, Liao SL, Wang SH, Wang CC, Yang CH. Simvastatin and ROCK inhibitor Y-27632 inhibit myofibroblast differentiation of Graves' ophthalmopathy-derived orbital fibroblasts via RhoA-mediated ERK and p38 signaling pathways. Front Endocrinol (Lausanne). 2020;11:607968. doi: 10.3389/fendo.2020.607968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wei YH, Liao SL, Wang CC, Wang SH, Tang WC, Yang CH. Simvastatin inhibits CYR61 expression in orbital fibroblasts in Graves' ophthalmopathy through the regulation of FoxO3a signaling. Mediators Inflamm. 2021;2021:8888913. doi: 10.1155/2021/8888913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lanzolla G, Sabini E, Leo M, Menconi F, Rocchi R, Sframeli A, Piaggi P, Nardi M, Marcocci C, Marino M. Statins for Graves' orbitopathy (STAGO): a phase 2, open-label, adaptive, single centre, randomised clinical trial. Lancet Diabetes Endocrinol. 2021;9(11):733–742. doi: 10.1016/S2213-8587(21)00238-2. [DOI] [PubMed] [Google Scholar]
- 101.Han Z, Cen C, Ou Q, Pan Y, Zhang J, Huo D, Chen K. The potential prebiotic berberine combined with methimazole improved the therapeutic effect of Graves' disease patients through regulating the intestinal microbiome. Front Immunol. 2021;12:826067. doi: 10.3389/fimmu.2021.826067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.He Q, Dong H, Gong M, Guo Y, Xia Q, Gong J, Lu F. New therapeutic horizon of Graves' hyperthyroidism: treatment regimens based on immunology and ingredients from traditional chinese medicine. Front Pharmacol. 2022;13:862831. doi: 10.3389/fphar.2022.862831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mortara L, Coco G, Pozzi C. Biomedicine and traditional Chinese medicine: a fruitful scientific and cultural interaction. Acta Biomed. 2022;93(1):e2022070. doi: 10.23750/abm.v93i1.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]