Abstract
Case report
Traumatic hip dislocations require prompt diagnosis and reduction to preserve the native joint. The classic irreducible posterior hip fracture-dislocation has been described as an immobile, slightly flexed, and internally rotated hip on physical exam. Classically, this irreducible pattern is associated with an ipsilateral femoral head fracture. The purpose of our report is to present an irreducible posterior hip dislocation with preserved motion in the setting of an unstable pelvic ring injury without associated femoral head pathology. Despite lacking clinical features of an irreducible hip, closed reduction in the emergency and operating rooms was unsuccessful, even after frame application for pelvis stability. Persistent irreducibility necessitated open reduction, where the femoral head was found to be buttonholed through the posterior hip capsule and blocking reduction.
Conclusion
A posteriorly dislocated hip with preserved motion in the setting of a concomitant unstable pelvic ring injury may belie the true locked nature of the femoroacetabular dislocation and high suspicion for femoral head incarceration is required. The description of this unique irreducible fracture pattern and the stepwise approach used for reduction may be useful for other surgeons who may encounter similar patterns of injury.
Keywords: Hip dislocation, Irreducible hip, Pelvic ring injury, Retained mobility, Open reduction
Introduction
Traumatic hip dislocations require prompt diagnosis and reduction to preserve the native joint. The irreducible posterior hip fracture-dislocation has been described by Mehta and Routt as an immobile, slightly flexed, and internally rotated hip on physical exam [1]. Classically, this irreducible pattern is associated with an ipsilateral femoral head fracture [1]. Early recognition of this pattern is important to avoid iatrogenic fracture of the femoral neck during attempted closed reduction.
The purpose of this report is to present an irreducible posterior hip dislocation with preserved motion in the setting of an unstable pelvic ring injury without associated femoral head pathology. Persistent irreducibility necessitated open reduction, where the femoral head was found to be buttonholed through the posterior hip capsule and blocking reduction. The description of this unique irreducible fracture pattern and the stepwise approach used for reduction may be useful for other surgeons who may encounter similar patterns of injury.
Case report
The patient was an otherwise healthy 18-year-old female who sustained multiple injuries after rolling 7–8 times following an all-terrain vehicle (ATV) crash. On arrival, a massive transfusion protocol was initiated for hemorrhagic shock and the patient was intubated. Her immediately apparent non-orthopaedic injuries included left rib fractures, left kidney injury, bilateral adrenal hemorrhages, and a left grade 3 hepatic laceration. An AP pelvis (Fig. 1A) showed a left posterior hip dislocation amidst complex pelvic ring fractures (described in detail in next paragraph). A traumatic Morelle-Lavelle lesion to the left hip was also apparent (Fig. 1B). A positive FAST ultrasound necessitated an urgent exploratory laparotomy. Prior to transport to the OR, one attempt at closed hip reduction by the on-call orthopaedic resident was unsuccessful. No neurologic examination was possible due to the patient's intubated and nonresponsive status, but distal pulses were palpable. Intra-abdominal procedures included a diverting colostomy and a primary repair of an intraperitoneal transmural bladder injury. A temporary abdominal binder was placed, and she was cleared for further orthopaedic procedures.
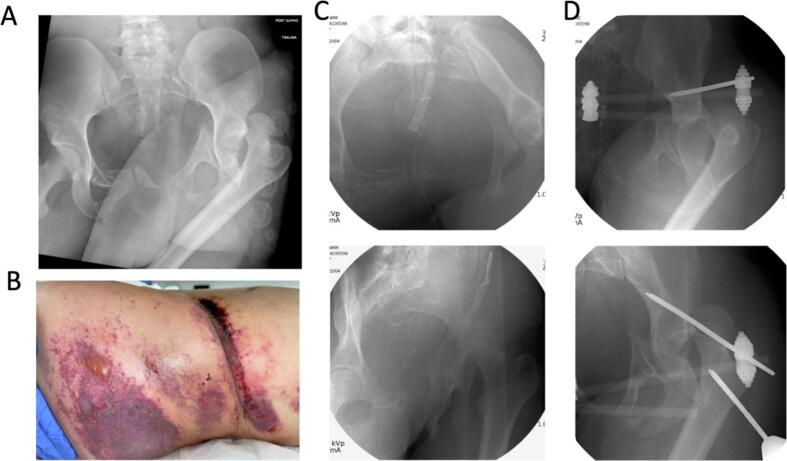
Fig. 1.
Initial injury and management. A) Portable pelvis AP radiograph showing posterior dislocation of the left hip, fractures of the right superior and inferior rami, left high pubic root, and left parasymphyseal fracture without clear involvement of the acetabulum. B) A large left Morelle-Lavelle lesion was present on the left flank. C) Inlet and left iliac oblique views showing the unstable left pelvic ring injury and posterior hip dislocation. D) The hip remained irreducible after placement of pelvis external fixator and with manipulation using a proximal femur Schanz pin.
Intra-operative fluoroscopy was first used to assess the fracture dislocation of the left hip (Fig. 1C). The inlet view of the pelvis showed a left displaced sacral fracture, left parasymphyseal fracture, left high pubic root fracture, and left posterior hip dislocation, with significant external rotation deformity of the associated hemipelvis. On the right, superior and inferior rami fractures were noted. An iliac oblique view did not show obvious posterior wall involvement of the dislocation, and the femoral head appeared intact. Under complete paralysis, closed reduction with standard reduction maneuvers was unsuccessful. On fluoroscopy and physical exam, the entire left hemipelvis was noted to move during reduction, which was considered a barrier to reduction. The pelvic ring was subsequently stabilized by placing an external fixator using supra-acetabular 5.0 Schanz pins bilaterally (Fig. 1D, top). The frame was then locked to stabilize the hemipelvis; however, repeated attempts at closed reduction remained unsuccessful. A Schanz pin was then placed percutaneously into the proximal femur to allow for direct manipulation of the dislocated segment, but the hip remained irreducible (Fig. 1D, bottom).
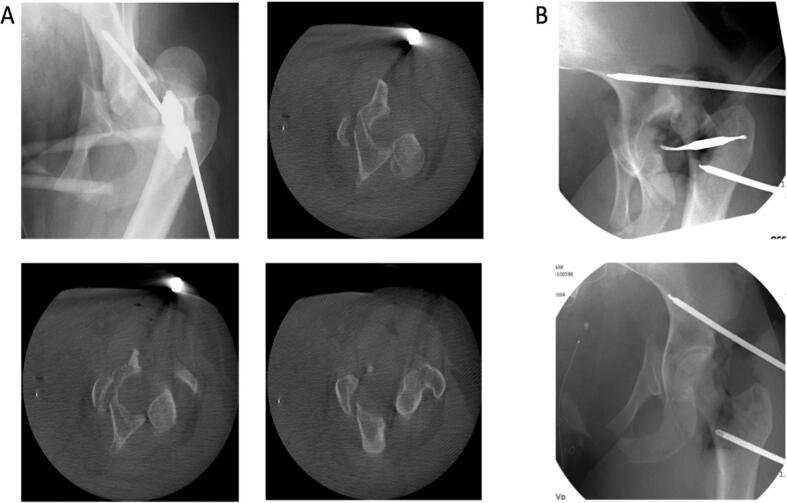
Intra-operative cross-section imaging of the pelvis was obtained using an O-arm spin to assess for possible causes of irreducibility. This revealed that the anteroinferior femoral head was tightly adherent to the posterior wall of the acetabulum, but without apparent posterior wall or femoral head pathology (Fig. 2A). The presentation at this point was consistent with an irreducible hip secondary to incarceration of the femoral head through the posterior capsule blocking reduction, as described by Mehta and Routt [1].An anterior approach to the hip was performed through a Smith-Peterson interval, and the external frame was temporarily relaxed to aid in exposure. An anterior exposure was selected so that a frame could be applied for pelvic ring stability, and because spinal precautions precluded lateral or prone positioning and thus access via a posterolateral approach. After careful dissection through the traumatically disrupted left hip capsule, the femoral head was found to be buttonholed through a rent in the posterior hip joint capsule with interposed anterior capsule and ligamentum blocking the reduction. (Fig. 2B, top). The left hip was ultimately reduced by enlarging the posterior capsular rent under direct vision, releasing the ligamentum teres, and then directly manipulating the proximal femur into a reduced position, using manual counter-pressure on the AIIS pin and acetabulum (Fig. 2B, bottom). After achieving the reduction, the patient's anterior hip approach was closed, and the external frame was secured. Afterwards, the patient returned to the ICU for further resuscitation.
Fig. 2.
Persistently irreducible left hip dislocation requiring open reduction. A) After placement of external fixator and Schanz pin into femur for closed reduction, intra-operative CT was performed to characterize the fracture and rule out additional acetabular and femoral neck fractures. The femoral head remained perched on the posterior wall. B) Intra-operative fluoroscopy images of the pre- and post-reduction after Smith-Peterson approach. In the top image, a freer elevator was used to localize the hip joint for the anterior capsulotomy; this was necessary because the dislocation and pelvic ring displacement created altered anatomy. Final reduction (bottom) was achieved after direct visualization of the femoral head and removal of interposed capsule and soft tissue. This immediately improved the alignment of the pelvic ring injury as well.
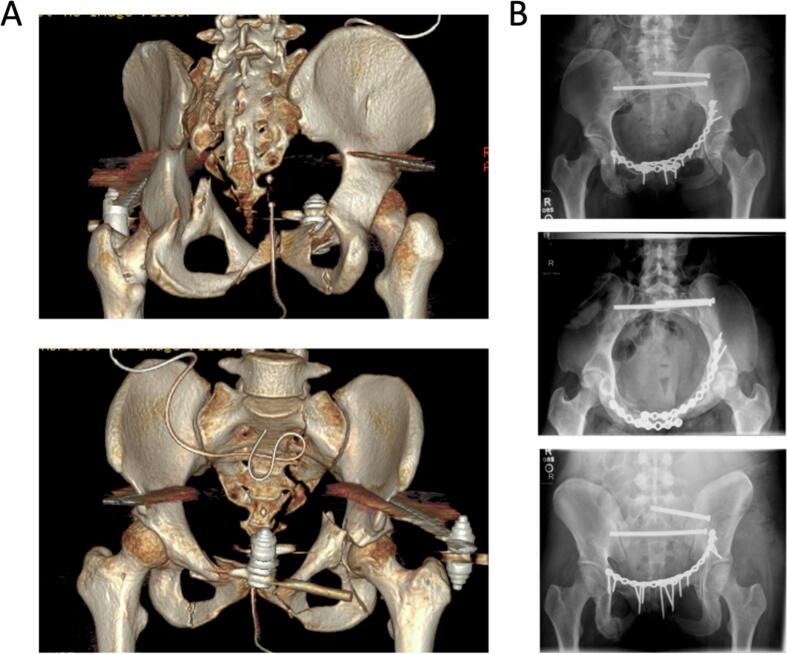
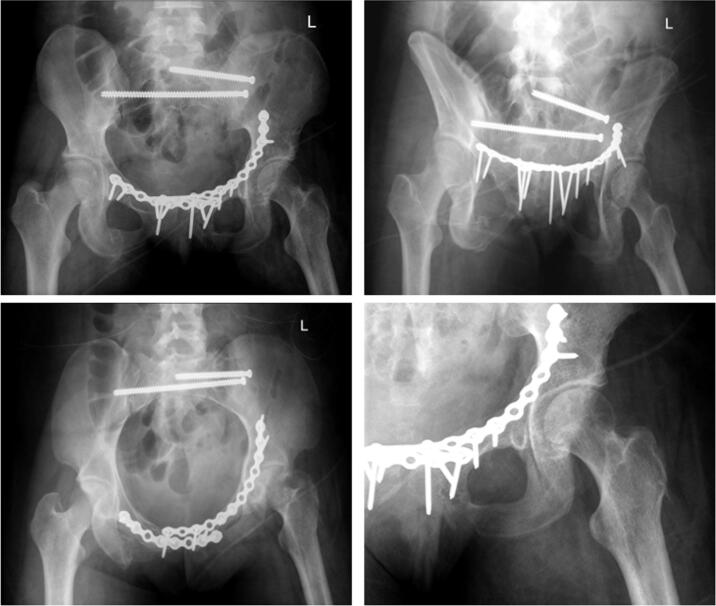
The patient was noted to have a left foot drop post-operatively with preserved plantarflexion. Cross-sectional imaging performed after the open reduction further characterized the pelvic ring injury (Fig. 3A). On post-operative day 3 from the open hip reduction, she underwent ORIF of her anterior pelvic ring and percutaneous screw fixation of her posterior ring (Fig. 3B). Her post-operative course was complicated by a saddle pulmonary embolism treated with anticoagulation and an inferior vena cava filter. The left thigh Morelle-Lavelle lesion was treated non-surgically. At 7 months post-injury, she underwent colostomy reversal. She has a persistent left foot drop for which she utilizes an AFO brace. Otherwise, she ambulates well without pain or other assistive devices. Imaging (Fig. 4) shows maintained alignment of pelvis hardware and fracture healing, and the left hip joint remains anatomically reduced without evidence of complications.
Fig. 3.
Definitive management of combined pelvic ring injury and irreducible hip requiring open reduction. A) A post-operative CT scan of the pelvis with frame in place showing complete zone 2 left sacrum injury, a high pubic root fracture extending to the anterior wall of the acetabulum. B) AP, inlet, and outlet views 1 month post-operative after treatment with percutaneous screw fixation of the posterior ring and open reduction internal fixation of the anterior ring.
Fig. 4.
Clockwise from upper left: 7-month post-operative AP, inlet, and outlet pelvis views showing ongoing healing of fractures and maintained hardware. On dedicated hip imaging, the joint remains congruent and scant heterotopic ossification about the greater trochanter is seen.
Discussion
Mehta and Routt have previously described the clinical and radiographic markers of irreducible hip dislocations [1]. They described seven irreducible femoral head fracture-dislocations without posterior acetabular fractures that all presented with the injured hip fixed in slight flexion with immobile neutral rotation and leg length discrepancy. Compared to the retained passive mobility observed with traditional hip dislocations and fracture-dislocations, these dislocations were defined by a complete immobility (“locked or fixed”) and required open reduction. In all cases in their series, surgical exploration through an anterior approach revealed that the proximal femur had herniated through a posterior-superior labral-bone traumatic interval, creating a tight tissue band blocking reduction. Other circumstances that may prevent concentric closed reduction include buttonholing of the femoral head through the posterior capsule and external rotators, displacement of the piriformis around the femoral neck or across the acetabulum, or fracture fragments or osteocartilaginous bodies in the acetabulum [2], [3], [4], [5], [6], [7], [8], [9]. All of these cases required open reduction.
The nature of this irreducible hip is unique as the hip dislocation was associated with an unstable ipsilateral pelvic ring injury secondary to complete sacral fracture. Due to the pelvic instability, the femoroacetabular dislocation did not have features of a mechanical block and the femur was amenable to passive mobility. Additionally, there was no associated femoral head fracture, although the femoral head was perched on the retroacetabular surface as noted in a subsequent intra-operative CT. The perceived motion of the femur was likely due to movement of the hemipelvis given the instability from the high pubic root and complete sacral fracture. As a result, the acetabulum was not anchored. Had the ipsilateral hemipelvis been stable, likely this dislocation would have presented with the traditional “locked or fixed” immobility. Such pelvic instability certainly contributed to the difficulty with closed reduction, even after application of the external frame. Indeed, there are inherent limitations of the external fixator especially for posterior pelvic stability. The lack of a posterior “tether” due to the complete ipsilateral sacral fracture negated much of the energy placed into axial traction during reduction. Significant counter traction on the AIIS pin was necessary to generate adequate hemipelvis stability for reduction, even after clearing the interposed soft tissue.
As the typical features of an irreducible hip dislocation were absent, this problem was difficult to predict. The combination of a posterior hip dislocation with associated pelvic and acetabular fractures has been rarely described in the literature. To the best of our knowledge, the only similar case report is that of Suzuki et al., who cited pelvic instability as a barrier to closed reduction for two cases that ultimately required open reduction [10]. In our case, a stepwise algorithm of escalating invasiveness was used to achieve reduction. This included attempted closed reduction, addition of a pelvic external fixator to increase ring stability, and direct manipulation of the proximal femur using a Schanz pin. Persistent irreducibility ultimately prompted an open reduction by an anterior approach. We believe that this sequence was the appropriate escalation of care, and we would not have changed our approach. Ultimately, the irreducibility of the hip was attributed to interposed anterior capsule and incarceration of the femoral head through the posterior capsule, further complicated by an unstable hemipelvis.
At last follow-up, imaging demonstrated a well-aligned pelvic ring, a congruent hip joint and healed fractures. The patient was ambulating without pain using an AFO brace due to persistent footdrop. The patient's unresponsive status upon arrival to our hospital precluded a neurologic exam, thus the timing of the nerve injury (post-injury or post-surgery) is unfortunately unknown.
In conclusion, a posteriorly dislocated hip in the setting of a concomitant unstable pelvic ring injury may be functionally irreducible, without the classic features of an irreducible fracture-dislocation. This case report may be useful for orthopaedic surgeons that encounter a similar injury pattern.
Declaration of competing interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Megerian, O'Donnell, and Fitzpatrick declare that they have no competing interests. Saiz reports the following: Orthopaedic Research Society (Board or committee member), Orthopaedic Trauma Association (Board or committee member). Lee reports the following: AO Foundation (Board or committee member), Globus Medical (IP royalties), Osteocentric (Stock or stock options), Osteocentric/SMY (Paid consultant), Synthes (Paid consultant, presenter, or speaker). Soles reports the following: Depuy, A Johnson & Johnson Company (Paid consultant), Orthopaedic Trauma Association (Board or committee member). Campbell reports the following: AAOS (Board or committee member), NSITE Medical INC. (Stock or stock options), Synthes (Paid consultant, presenter, or speaker), Takeda Pharmaceuticals (Research support).
Acknowledgements
None.
Footnotes
Investigation performed at University of California Davis Medical Center in Sacramento, CA.
No funding was utilized to carry out this research.
References
- 1.Mehta S., Routt M.L.C.J. Irreducible fracture-dislocations of the femoral head without posteriorWall acetabular fractures. J. Orthop. Trauma. 2008;22(10) doi: 10.1097/BOT.0b013e31818e2a86. [DOI] [PubMed] [Google Scholar]
- 2.Alyousif H., Aleisawi H., Alkaff H., Albusayes N. Terrible triad of the hip: a case report. Int. J. Surg. Case Rep. 2021;82 doi: 10.1016/j.ijscr.2021.105758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fageir M., Veettil M.K.P. Posterior dislocation of a native hip joint associated with ipsilateral per-trochanteric fracture: a rare case report. Trauma Case Rep. 2018;13:1–13. doi: 10.1016/j.tcr.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uzel A.P., Bertino R., Daculsi G., Yves Laflamme G., Gui-e L. Irreducible traumatic posterior hip dislocation with entrapment and a buttonhole effect. Chin. J. Traumatol. 2011;14(6):367–370. doi: 10.3760/cma.j.issn.1008-1275.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Duygulu F., Calis M., Argun M., Guney A. Unusual combination of femoral head dislocation associated acetabular fracture with ipsilateral neck and shaft fractures: a case report. J. Trauma Acute CareSurg. 2006;61(6) doi: 10.1097/01.ta.0000224898.83708.e1. [DOI] [PubMed] [Google Scholar]
- 6.McKee M.D., Garay M.E., Schemitsch E.H., Kreder H.J., Stephen D.J.G. Irreducible fracture-dislocation of the hip: a severe injury with a poor prognosis. J. Orthop. Trauma. 1998;12(4) doi: 10.1097/00005131-199805000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Slasky B.S., Liebergall M. Irreducible traumatic posterior dislocations of the hip. Emerg. Radiol. 1997;4(2):105–108. doi: 10.1007/BF01508038. [DOI] [Google Scholar]
- 8.Canale S.T., Manugian A.H. Irreducible traumatic dislocations of the hip. JBJS. 1979;61(1) [PubMed] [Google Scholar]
- 9.Slätis P., Latvala A. Irreducible traumatic posterior dislocation of the hip. Injury. 1974;5(3):188–193. doi: 10.1016/S0020-1383(74)80003-3. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki T., Smith W.R., Hak D.J., et al. Combined injuries of the pelvis and acetabulum: nature of a devastating dyad. J. Orthop. Trauma. 2010;24(5) doi: 10.1097/BOT.0b013e3181ca32af. [DOI] [PubMed] [Google Scholar]