Abstract
Some have touted technology as a panacea for overcoming the isolation associated with COVID-19 mitigation policies; yet, these tools are not widely adopted by older adults. With data from the COVID-19 supplement to the National Health and Aging Trends Survey, we conduct adjusted Poisson regression modeling to examine digital communications use during COVID-19 and feelings of anxiety, depression, and loneliness during the COVID-19 pandemic among older adults (65+ years of age). Adjusted Poisson regression revealed that those who reported frequent use of video calls with friends and family (aPR = 1.22, 95% CI:1.06–1.41) and with healthcare providers (aPR = 1.22, 95% CI:1.03–1.45) were more likely to report feelings of anxiety than those not using these platforms; yet, reports of in-person visits with friends and family (aPR = 0.79, 95% CI: 0.66–0.93) and with healthcare providers (aPR = 0.88, 95% CI: 0.77–1.01) were associated with fewer feelings of depression and loneliness, respectively. Future research is needed to tailor digital technology to support older adults.
Keywords: older adults, mental health, digital communication, digital technologies, COVID-19
What this paper adds
• Before the COVID-19 pandemic, older adults have reported lower adoption of digital communication technologies than younger adults, particularly for healthcare-related contexts.
• Older adults were encouraged to adhere to stringent COVID-19 protocols, such as social distancing. These conditions could pose challenges to the ability for older adults to communicate with friends, family, and healthcare providers.
• We investigate use of digital communication technologies as compared to in-person communication among older adults during the COVID-19 pandemic and explore the relationship between use of digital communication technologies and feelings of anxiety and depression among older adults.
Applications of study findings
• Our results uncover demographic differences in use of digital communication tools during the COVID-19 pandemic and relationships between digital communication and feelings of depression and anxiety.
• Future research may consider developing tailored communication technologies to meet the needs of older adults as a means for preparing for future pandemics.
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has introduced sweeping changes to our daily lives (Czeisler et al., 2021). Due to the increased morbidity and mortality associated with COVID-19 among older adults (age 65 and above), these individuals have been strongly advised to adhere to strict mitigation guidelines, such as social distancing and avoiding in-person interactions with those outside their household (Lewnard & Lo, 2020). Social interaction and interpersonal communication are strong predictors of resiliency and mental health (Cohen, 2004) and, according to meta-analysis, personal connections reduce all-cause mortality risk (Holt-Lunstad et al., 2010). Although vital for curbing the spread of the virus, COVID-19 mitigation measures created concerns about increased risks of loneliness and mental health symptoms of depression, anxiety, and suicidal ideation among all adults (Czeisler et al., 2020), particularly among older adults who are already at risk for loneliness and adverse mental health symptoms (Cudjoe & Kotwal, 2020). According to a prospective survey study of community-dwelling older adults during COVID-19 conducted by Kotwal and colleagues, more than half of participants (54%) reported worsening feelings of loneliness as the COVID-19 pandemic waged on (Kotwal et al., 2021).
Technology has been argued to be a tool for alleviating the isolation associated with the COVID-19 pandemic and social distancing policies (Gabbiadini et al., 2020), and for delivering mental health services during the COVID-19 pandemic (Gould & Hantke, 2020). Nationally representative surveys indicate that technology use has increased among older adults in recent, pre-pandemic years. For example, 42% of older adults reporting smartphone ownership in 2017, up from 18% in 201 and 67% reported using the Internet in 2017 (Pew Research, 2017). However, technological tools may neither benefit all groups of older adults equally nor be accessible to all older adults. Those aged 80 and above were half as likely to report ever going online compared to those aged 65 to 69 (Pew Research, 2017). Further, digital literacy, which refers to the technical skills, cognitive abilities, and socio-emotional aspects of navigating digital technologies (Lankshear & Knobel, 2008), varies by socioeconomic status. According to a survey of patients from community health centers, older adults and racial/ethnic minorities were significantly less likely to report using digital technologies for health-related purposes, such as communicating with a provider, compared to younger, White adults (Bailey et al., 2015). Also, according to a study of older adults in a large health plan, Black, Latino, and Filipino older adults and those 75 years old and older were significantly less likely to own digital devices (e.g., computers, smartphones), use the Internet, and report being willing to use digital technology to perform healthcare-related tasks, such as communicating with a healthcare provider, than White participants or those age 65–74 years old (Gordon & Hornbrook, 2016).
Before the COVID-19 pandemic, older adults have lagged behind younger adults in the adoption of the Internet and digital communication technologies, particularly for healthcare-related contexts. In a systematic review of studies examining older adults’ views on electronic health services, such as doctor–patient communication, researchers identified significant barriers to using technology for health purposes. Results of this review highlight barriers such as feeling a technology was not “meant for me,” frustration regarding the time and effort needed to use a service, lack of prior experience, fear of making a mistake, concerns of data loss or losing a device, and judgmental language and tone (Hirvonen et al., 2020). According to the survey conducted by Kotwal and colleagues of older adults during the COVID-19 pandemic, two-thirds reported minimal or no use of digital communication tools, such as video chat with friends and family members, and those who reported feelings of loneliness during COVID-19 also reported frustration with digital technologies (Kotwal et al., 2021).
Therefore, research has demonstrated that older adults were lagging younger individuals before COVID-19 in their adoption of digital communication technologies and that race/ethnic minority is a demographic predictor of even lower adoption of digital communication tools. Despite this, there are gaps in the literature on the use of digital communication tools among older adults during the COVID-19 pandemic, and how use of digital tools for communication relates to feelings of anxiety and depression about the pandemic among older adults. We address these gaps in the literature by examining the demographic factors associated with the use of each communication modality (i.e., emails, video calls, phone calls, and in-person) to speak with friends and family during the COVID-19 pandemic (Research Question 1). Second, we examine the demographic factors associated with the use of the various communication modalities (i.e., emails, video calls, phone calls, and in-person) to speak with healthcare providers during the COVID-19 pandemic (Research Question 2). Third, we examine the associations between digital communication tools (i.e., emails, video calls, and phone calls) used for interpersonal communication and those tools used for doctor–patient communication during COVID-19 (Research Question 3). Fourth, we will examine the associations between interpersonal and doctor–patient communication modalities and feelings of anxiety or depression about the COVID-19 pandemic or feelings of loneliness during the COVID-19 pandemic (Research Question 4).
Materials and Methods
We analyzed data from the National Health and Aging Trends Study (NHATS), an annual in-home, longitudinal, nationally representative survey of Medicare beneficiaries (aged ≥65 years). NHATS administered a supplemental survey to their regular annual assessment to examine changes to daily life, among other areas, among older adults during the COVID-19 pandemic. The COVID-19 supplement was administered to NHATS participants between June and October 2020. Data for this study were taken from the COVID-19 supplement, including communication behavior with friends, family, and healthcare providers either in person or via digital technologies as well as feelings of anxiety or depression about the COVID-19 pandemic, and feelings of loneliness during the COVID-19 pandemic. The COVID-19 supplement received 3188 completed responses out of 3961 eligible NHATS participants (response rate = 80.5%) (Freedman & Hu, 2020). Our analysis of publicly available, de-identified data was considered exempt from IRB review.
Measures
We examined demographic predictors of communication via phone calls, email, video calls, and in-person with friends and family members during the COVID-19 pandemic. We also examined demographic predictors of doctor-patient communication via phone calls, email, video calls, and in-person visits during the COVID-19 pandemic. Finally, we assessed feelings of anxiety, depression, and loneliness among respondents.
Demographic characteristics
We examined age, coded as a categorical variable, distinguishing between participants aged 65 to 69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, and 90 years and older. Marital status was coded as either married/living with a partner, separated, divorced, widowed, or never married. We also examine self-reported gender (female or male). Participants were asked to report their health conditions, ranging from heart attack, heart disease, hypertension, arthritis, diabetes, lung disease, stroke, Alzheimer’s disease or related dementia, and cancer. Finally, participants’ race/ethnicity was coded as either White/Non-Hispanic, Black/Non-Hispanic, Hispanic/Latino, or other.
Interpersonal communication modalities with family and friends during the COVID-19 pandemic
We examined interpersonal communication on four modalities: phone, email, video calls, and in-person. Participants or proxies responded to the question, “During the COVID-19 outbreak, in a typical week, how often have you been in contact with family and friends not living with you by phone calls,” “… Emails, texts or social media messages,” “… video calls, including Zoom, FaceTime, and other online video platforms,” and “In-person visits.” Participants or proxies could then choose a response from the following options: “At least daily,” “A few times a week,” “About once a week,” “Less than once a week,” or “Never.”
Responses to all communication variables were dichotomized so that a value of 0 was assigned to responses of “Never,” while a value of 1 was assigned to responses “At least daily,” “A few times a week,” “About once a week,” and “Less than once a week.”
Doctor-patient communication modalities during the COVID-19 pandemic
We examined doctor-patient communication on four modalities during COVID-19: phone, email, video calls, and in-person visits. Participants responded to the question, “During the COVID-19 outbreak, how did you communicate with your usual health care provider?” Participants marked “Yes” or “No” to various options, including “Phone calls,” “Emails or texts or portal messages,” “Video calls (also called ‘telehealth’),” or “In-person visits.”
Feelings of anxiety, depression, and loneliness
We examined feelings of anxiety and depression about the COVID-19 pandemic. Participants responded to the questions, “During the COVID-19 outbreak, in a typical week, how worried or anxious have you felt about the outbreak” and “…sad or depressed about the outbreak?” Feelings of loneliness about the COVID-19 pandemic were assessed by asking participants, “During the COVID-19 outbreak, in a typical week, how often have you felt lonely?” Feelings of anxiety and depression about COVID-19 and feelings of loneliness during COVID-19 were assessed on the scales 1 “Every day,” 2 “Most days,” 3 “Some days,” 4 “Rarely,” and 5 “Never.” Responses to reports of feelings of anxiety, depression, and loneliness about COVID-19 were dichotomized so that “Every day,” “Most days,” and “Some days” were assigned a value of 1, and “Rarely” and “Never” were assigned a value of 0.
Statistical Analysis
We computed prevalence ratios using univariate Poisson regression with robust standard errors to identify the relationship between each demographic variable and self-reported communication modality for both interpersonal communication with friends and family (Research Question 1) and healthcare providers (Research Question 2). Next, to explore the relationships between digital technologies for friends and family and doctor–patient communication (Research Question 3), we computed adjusted prevalence ratios using multivariable Poisson regression with robust standard errors for responses to the questions assessing the use of each modality (i.e., email, video calls, and phone calls) with either friends and family or a healthcare provider. Finally, to examine differences in communication and feelings of anxiety, depression, and loneliness (Research Question 4), we computed adjusted prevalence ratios using multivariable Poisson regression with robust standard errors. All models were controlled for gender, marital status, age, a sum score of all self-reported health conditions, pre-COVID-19 mental health symptoms, and living alone. To control for pre-COVID mental health symptoms, we used responses to the PHQ-2 and GAD-2 from the survey wave prior to COVID-19. The sum total of responses to the PHQ-2 and GAD-2 of 3 or higher were coded as mental health symptoms (1) and 2 or lower coded as absence of such concerns (0) (Kroenke et al., 2001; Löwe et al., 2010). Finally, we created a new variable to indicate living alone (1), compared to living with a spouse, partner, or other (0). Significance was considered at p < 0.05. All analyses were conducted in Stata Version 16 (College Station, TX).
Results
Among the participants, 1.25% (n = 40) were age 65 to 69, 33.1% (n = 704) were age 70 to 74, 28.0% (n = 892) were age 75 to 79, 22.7% (n = 722) were age 80 to 84, 16.1% (n = 512) were age 85 to 89, and 10.0% (n = 318) were age 90 or above. The sample was comprised of 41.1% (n = 1343) males and 57.9% (n = 1845) females. The plurality of participants were either married or living with a partner (49.6%, n = 1580), while 50.4% were either widowed, divorced, or never married. Participants were mostly White, non-Hispanic (n = 2,426, 77.1%), followed by Black, non-Hispanic (n = 529, 16.8%), Hispanic (n = 128, 4.1%), and Other (n = 65, 2.1%). With regard to health conditions, 1.8% reported history of myocardial infarction (n = 58), 24.7% reported history of heart disease (n = 786), 73.4% reported high blood pressure (n = 2350), 73.1% reported arthritis (n = 2329), 27.9% reported diabetes (n = 889), 22.3% reported lung disease (n = 712), 2.1% reported history of stroke (n = 66), 6.0% reported dementia or Alzheimer’s disease (n = 192), and 6.1% reported cancer (n = 196). With respect to living situation, 36.6% reported living alone (n = 1632). Among participants, 22.4% (n = 1117) had mental health concerns as measured by the PHQ-2 before COVID-19 and 20.0% (n = 996) had mental health concerns as measured by the GAD-2 before COVID-19.
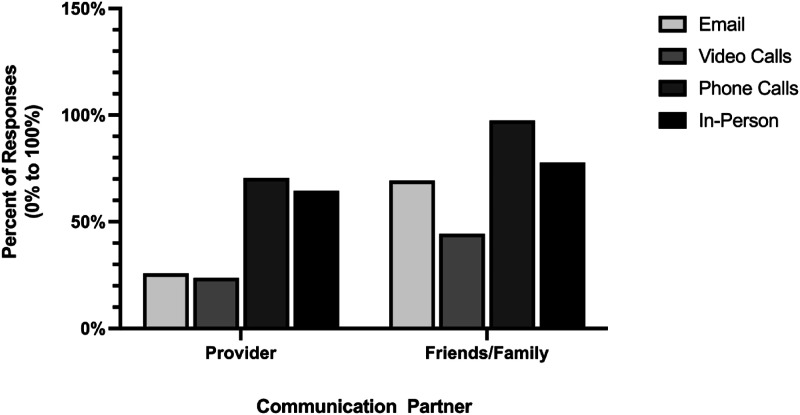
With respect to communication modalities, email with a provider was reported by 25.8% (n = 631), yet 69.3% (n = 1964) reported email with family and friends. Video calls with a provider were reported by 23.8% (n = 585), and 44.4% reported video calls with family and friends. Phone calling with a provider was reported by 70.5% (n = 1960); yet, 97% (n = 2943) reported phone calls with family and friends. In-person visits with providers were reported by 64.5% (n = 1814); yet, 77.8% (n = 2273) reported in-person visits with friends and family, as shown in Figure 1.
Figure 1.
Characteristics of communication by modality (email, video calls, phone calls, in-person) and communication partner (healthcare provider and friends/family) during the COVID-19 pandemic.
Regarding feelings of depression about COVID-19, these were reported by 22.5% (n = 707), feelings of anxiety about the COVID-19 pandemic were reported by 28.3% (n = 882), and feelings of loneliness due to the COVID-19 pandemic were reported by 34.9% (n = 1019).
Analysis of communication with friends and family by demographic factors revealed less email communication among older adults (85–89 years old: PR = 0.68, 95% CI: 0.48–0.98; age 90+: PR = 0.44, 95% CI: 0.30–0.65), compared to those 65–69 years of age. Use of video calls was also less common among adults 90 years of age and above (PR = 0.56, 95% CI: 0.35–0.91). Those that were either widowed or never married reported less use of email (widowed: PR = 0.73, 95% CI: 0.66–0.81; never married: PR = 0.60, 95% CI: 0.44–0.82) and video calls (widowed: PR = 0.74, 95% CI: 0.65–0.85; never married: PR = 0.63, 95% CI: 0.44–0.92), compared to those that were married. Use of emails was less common among Black individuals (PR = 0.71, 95% CI: 0.62–0.82) and Hispanic/Latino individuals (PR = 0.66, 95% CI: 0.50–0.87). Those living alone reported less use of email (PR = 0.72, 95% CI: 0.69–0.76), video calls (PR = 0.47, 95% CI: 0.44–0.55), and in-person communication (PR = 0.77, 95% CI: 0.73–0.81) than did those living with a spouse, partner, or other. Those with pre-COVID-19 mental health concerns reported less use of email (PHQ-2: PR = 0.60, 95% CI: 0.50–.74; GAD-2: PR = 0.77, 95% CI: 0.64–0.93) than did those without such concerns, as shown in Table 1.
Table 1.
Univariate Poisson Regressions Examining Demographic Characteristics and Friends and Family Communication Modalities during the COVID-19 Pandemic.
| Friends and Family Communication
Modalities Reported During the COVID-19 Pandemic (all Comparisons: “Never”) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emails (n = 1964) | Video Calls (n = 1256) | Phone Calls (n = 2943) | In-Person (n = 2273) | |||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| PR | Lower | Upper | PR | Lower | Upper | PR | Lower | Upper | PR | Lower | Upper | |
| Age | ||||||||||||
| 65–69 | Reference | |||||||||||
| 70–74 | 0.99 | [0.69 | 1.40] | 1.02 | [0.66 | 1.59] | 1.01 | [0.73 | 1.41] | 1.02 | [0.71 | 1.46] |
| 75–79 | 0.92 | [0.65 | 1.31] | 0.88 | [0.56 | 1.36] | 1.00 | [0.73 | 1.39] | 0.96 | [0.67 | 1.38] |
| 80–84 | 0.76 | [0.53 | 1.09] | 0.75 | [0.48 | 1.16] | 1.00 | [0.72 | 1.39] | 0.96 | [0.67 | 1.38] |
| 85–89 | 0.68 | [0.48 | 0.98] | 0.70 | [0.45 | 1.10] | 0.99 | [0.71 | 1.38] | 0.98 | [0.68 | 1.42] |
| 90+ | 0.44 | [0.30 | 0.65] | 0.56 | [0.35 | 0.91] | 0.98 | [0.70 | 1.37] | 0.96 | [0.66 | 1.39] |
| Marital status | ||||||||||||
| Married/living w/partner | Reference | |||||||||||
| Separated | 0.69 | [0.44 | 1.10] | 0.79 | [0.47 | 1.35] | 0.94 | [0.67 | 1.31] | 0.92 | [0.61 | 1.39] |
| Divorced | 0.88 | [0.76 | 1.01] | 0.83 | [0.70 | 0.99] | 1.00 | [0.89 | 1.12] | 0.98 | [0.86 | 1.12] |
| Widowed | 0.73 | [0.66 | 0.81] | 0.74 | [0.65 | 0.85] | 0.99 | [0.92 | 1.08] | 1.00 | [0.91 | 1.10] |
| Never married | 0.60 | [0.44 | 0.82] | 0.63 | [0.44 | 0.92] | 0.91 | [0.74 | 1.13] | 0.84 | [0.65 | 1.08] |
| Gender | ||||||||||||
| Male | Reference | |||||||||||
| Female | 0.97 | [0.88 | 1.06] | 0.97 | [0.87 | 1.08] | 1.00 | [0.93 | 1.08] | 0.99 | [0.91 | 1.08] |
| Health conditions | ||||||||||||
| Heart attack | 0.75 | [0.50 | 1.11] | 0.67 | [0.39 | 1.13] | 1.01 | [0.77 | 1.32] | 1.06 | [0.79 | 1.44] |
| Heart disease | 0.96 | [0.86 | 1.06] | 0.99 | [0.87 | 1.12] | 1.00 | [0.92 | 1.09] | 0.94 | [0.86 | 1.04] |
| Hypertension | 0.89 | [0.81 | 0.98] | 0.94 | [0.83 | 1.06] | 0.99 | [0.91 | 1.08] | 0.98 | [0.89 | 1.08] |
| Arthritis | 0.94 | [0.85 | 1.03] | 0.98 | [0.86 | 1.10] | 1.00 | [0.93 | 1.09] | 1.00 | [0.92 | 1.10] |
| Diabetes | 0.86 | [0.78 | 0.96] | 0.90 | [0.79 | 1.02] | 0.99 | [0.91 | 1.07] | 0.94 | [0.86 | 1.03] |
| Lung disease | 1.01 | [0.91 | 1.13] | 1.02 | [0.89 | 1.17] | 0.99 | [0.91 | 1.08] | 0.98 | [0.89 | 1.08] |
| Stroke | 0.85 | [0.61 | 1.18] | 0.91 | [0.61 | 1.35] | 1.01 | [0.79 | 1.29] | 1.04 | [0.79 | 1.38] |
| Alzheimer’s/Dementia | 0.41 | [0.31 | 0.54] | 0.84 | [0.66 | 1.08] | 0.84 | [0.72 | 0.99] | 0.81 | [0.68 | 0.98] |
| Cancer | 1.07 | [0.90 | 1.27] | 1.07 | [0.86 | 1.33] | 1.00 | [0.86 | 1.16] | 1.11 | [0.94 | 1.30] |
| Race/Ethnicity | ||||||||||||
| White/Non-Hispanic | Reference | |||||||||||
| Black/Non-Hispanic | 0.71 | [0.62 | 0.82] | 0.98 | [0.84 | 1.14] | 0.99 | [0.90 | 1.09] | 0.90 | [0.80 | 1.01] |
| Other | 0.93 | [0.69 | 1.27] | 1.14 | [0.80 | 1.63] | 1.01 | [0.78 | 1.29] | 0.78 | [0.57 | 1.08] |
| Hispanic/Latino | 0.66 | [0.50 | 0.87] | 0.89 | [0.65 | 1.21] | 0.97 | [0.81 | 1.17] | 0.70 | [0.55 | 0.91] |
| Living arrangement | ||||||||||||
| Living with spouse, partner, or other(s) | Reference | |||||||||||
| Alone | 0.72 | [0.69 | 0.76] | 0.47 | [0.44 | 0.50] | 0.98 | [0.93 | 1.02] | 0.77 | [0.73 | 0.81] |
| Pre-Covid mental health status | ||||||||||||
| PHQ-2 | 0.60 | [0.50 | 0.73] | 0.79 | [0.64 | 0.97] | 0.93 | [0.82 | 1.06] | 0.94 | [0.81 | 1.09] |
| GAD-2 | 0.77 | [0.64 | 0.93] | 0.82 | [0.66 | 1.03] | 0.94 | [0.82 | 1.08] | 0.83 | [0.71 | 0.98] |
Notes. Bold indicates significance at the p < 0.05 level.
Analysis of communication with a healthcare provider by demographic factors revealed less use of email with a healthcare provider among those 80–84 years of age (PR = 0.53, 95% CI: 0.31–0.90), 85–89 years of age (PR = 0.44, 95% CI: 0.25–0.77), and 90+ years of age (PR = 0.25, 95% CI: 0.13–0.48), compared to those 65–69 years of age. Those who were widowed were less likely to either email (PR = 0.53, 95% CI: 0.44–0.65) or use video calls (PR = 0.70, 95% CI: 0.58–0.85) to communicate with their healthcare provider, compared to those who were married or living with a partner. Those with Alzheimer’s disease or related dementia were less likely to use either email (PR = 0.62, 95% CI: 0.42–0.91) or phone (PR = 0.75, 95% CI: 0.61–0.92) to communicate with their healthcare provider. Phone use with a healthcare provider was more likely among both Black/non-Hispanic individuals (PR = 1.19, 95% CI: 1.06–1.34) and Hispanic/Latino individuals (PR = 1.25, 95% CI: 1.01–1.54) than White/Non-Hispanic individuals. Living alone was associated with less email (PR = 0.72, 95% CI: 0.61–0.86), video calls (PR = 0.76, 95% CI: 0.63–0.91) than those living with a spouse, partner, or other. Those with pre-COVID-19 anxiety as measured by the PHQ-2 reported less use of email with a provider (PR = 0.61, 95% CI: 0.43, 0.85), than did those without such concerns, as shown in Table 2.
Table 2.
Univariate Poisson Regressions Examining Demographic Characteristics and Doctor-Patient Communication Modalities during the COVID-19 Pandemic.
| Doctor-Patient Communication
Modalities Reported During the COVID-19 Pandemic (all Comparisons: “No”) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emails (n = 631) | Video Calls (n = 585) | Phone Calls (n = 1960) | In-Person (n = 1814) | |||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| PR | Lower | Upper | PR | Lower | Upper | PR | Lower | Upper | PR | Lower | Upper | |
| Age | ||||||||||||
| 65–69 | Reference | |||||||||||
| 70–74 | 0.87 | [0.51 | 1.47] | 1.09 | [0.56 | 2.13] | 0.99 | [0.67 | 1.45] | 1.42 | [0.86 | 2.33] |
| 75–79 | 0.74 | [0.44 | 1.24] | 0.97 | [0.50 | 1.90] | 1.01 | [0.69 | 1.48] | 1.44 | [0.87 | 2.36] |
| 80–84 | 0.53 | [0.31 | 0.90] | 0.76 | [0.39 | 1.50] | 1.02 | [0.69 | 1.50] | 1.51 | [0.92 | 2.49] |
| 85–89 | 0.44 | [0.25 | 0.77] | 0.75 | [0.38 | 1.50] | 1.00 | [0.67 | 1.48] | 1.46 | [0.88 | 2.42] |
| 90+ | 0.25 | [0.13 | 0.48] | 0.74 | [0.36 | 1.52] | 0.89 | [0.59 | 1.34] | 1.48 | [0.89 | 2.47] |
| Marital status | ||||||||||||
| Married/living w/partner | Reference | |||||||||||
| Separated | 0.63 | [0.28 | 1.42] | 0.87 | [0.41 | 1.84] | 1.11 | [0.76 | 1.62] | 1.06 | [0.77 | 1.45] |
| Divorced | 0.87 | [0.68 | 1.11] | 0.91 | [0.71 | 1.18] | 0.99 | [0.86 | 1.14] | 0.82 | [0.52 | 1.31] |
| Widowed | 0.53 | [0.44 | 0.65] | 0.70 | [0.58 | 0.85] | 0.96 | [0.87 | 1.06] | 0.93 | [0.80 | 1.08] |
| Never married | 0.68 | [0.42 | 1.11] | 0.81 | [0.50 | 1.32] | 0.87 | [0.66 | 1.14] | 0.97 | [0.87 | 1.07] |
| Gender | ||||||||||||
| Male | Reference | |||||||||||
| Female | 0.79 | [0.67 | 0.92] | 1.04 | [0.88 | 1.22] | 0.95 | [0.87 | 1.03] | 0.91 | [0.83 | 1.00] |
| Health conditions | ||||||||||||
| Heart attack | 0.69 | [0.33 | 1.45] | 0.68 | [0.30 | 1.52] | 1.19 | [0.88 | 1.62] | 1.14 | [0.82 | 1.59] |
| Heart disease | 1.03 | [0.86 | 1.23] | 1.28 | [1.07 | 1.53] | 1.03 | [0.94 | 1.15] | 1.13 | [1.02 | 1.25] |
| Hypertension | 1.00 | [0.84 | 1.20] | 1.15 | [0.95 | 1.39] | 1.07 | [0.97 | 1.19] | 1.07 | [0.96 | 1.19] |
| Arthritis | 1.02 | [0.86 | 1.22] | 1.25 | [1.04 | 1.52] | 1.10 | [0.99 | 1.22] | 1.08 | [0.97 | 1.20] |
| Diabetes | 0.90 | [0.76 | 1.08] | 1.04 | [0.87 | 1.25] | 1.09 | [0.99 | 1.20] | 1.06 | [0.96 | 1.18] |
| Lung disease | 1.14 | [0.95 | 1.37] | 1.12 | [0.92 | 1.35] | 1.05 | [0.95 | 1.16] | 1.05 | [0.94 | 1.18] |
| Stroke | 0.99 | [0.56 | 1.75] | 0.89 | [0.48 | 1.67] | 1.07 | [0.79 | 1.45] | 1.03 | [0.75 | 1.43] |
| Alzheimer’s/Dementia | 0.62 | [0.42 | 0.91] | 0.96 | [0.68 | 1.34] | 0.75 | [0.61 | 0.92] | 1.04 | [0.87 | 1.26] |
| Cancer | 1.08 | [0.80 | 1.46] | 1.28 | [0.96 | 1.72] | 0.99 | [0.82 | 1.19] | 1.13 | [0.94 | 1.35] |
| Race/Ethnicity | ||||||||||||
| White/Non-Hispanic | Reference | |||||||||||
| Black/Non-Hispanic | 0.86 | [0.67 | 1.09] | 1.19 | [0.95 | 1.48] | 1.19 | [1.06 | 1.34] | 1.01 | [0.89 | 1.15] |
| Other | 1.08 | [0.64 | 1.84] | 1.20 | [0.69 | 2.08] | 1.18 | [0.87 | 1.60] | 0.94 | [0.66 | 1.33] |
| Hispanic/Latino | 0.89 | [0.58 | 1.36] | 1.44 | [1.00 | 2.07] | 1.25 | [1.01 | 1.54] | 0.98 | [0.77 | 1.24] |
| Living arrangement | ||||||||||||
| Living with spouse, partner, or other(s) | Reference | |||||||||||
| Alone | 0.72 | [0.61 | 0.86] | 0.76 | [0.63 | 0.91] | 0.95 | [0.86 | 1.04] | 0.96 | [0.87 | 1.06] |
| Pre-Covid mental health status | ||||||||||||
| PHQ-2 | 0.61 | [0.43 | 0.85] | 1.17 | [0.90 | 1.53] | 0.99 | [0.85 | 1.16] | 1.02 | [0.87 | 1.19] |
| GAD-2 | 0.75 | [0.54 | 1.04] | 1.24 | [0.94 | 1.64] | 1.01 | [0.86 | 1.19] | 1.02 | [0.86 | 1.21] |
Notes. Bold indicates significance at the p < 0.05 level. PR is an abbreviation for prevalence ratio. PHQ-2 and GAD-2 were measured in 2019, the survey wave prior to COVID-19. PHQ-2 and GAD-2 responses were scored so that the sum total of responses to the two questions for each scale of 2 or less indicated no mental health concerns, and 3 or higher indicated a concern on either scale.
Adjusted Poisson regression analyses examining the relationships between the modalities of communication revealed that reports of using email to communicate with friends and family were related to reports of using email (aPR = 5.66, 95% CI: 4.02–7.95) and video (PR = 2.06, 95% CI: 1.62–2.62) to communicate with a healthcare provider during the COVID-19 pandemic. Reports of using the phone to communicate with friends and family were related to reports of using the phone to communicate with a healthcare provider during the COVID-19 pandemic (PR = 1.49, 95% CI: 1.03–2.15), Table 3.
Table 3.
Univariate Poisson Regressions Examining the Relationships between Communication with Friends and Family and Healthcare Providers during the COVID-19 Pandemic.
| Doctor-Patient Communication Modalities During the COVID-19 Pandemic | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emails | Video Calls | Phone Calls | In-Person | |||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| aPR | Lower | Upper | aPR | Lower | Upper | aPR | Lower | Upper | aPR | Lower | Upper | |
| Friends and family communication modalities during the COVID-19 pandemic | ||||||||||||
| Emails | 5.66 | [4.02 | 7.95] | 2.57 | [2.15 | 3.07] | 2.23 | [0.92 | 5.40] | 1.02 | [0.84 | 1.25] |
| Video calls | 2.06 | [1.62 | 2.62] | 2.60 | [2.16 | 3.13] | 1.79 | [0.85 | 3.80] | 0.91 | [0.74 | 1.11] |
| Phone calls | 1.10 | 0.89 | 1.23] | 1.07 | [0.96 | 1.17] | 1.49 | [1.03 | 2.15] | 1.05 | [0.94 | 1.17] |
| In-person | 0.00 | [0.89 | 1.22] | 0.93 | [0.84 | 1.03] | 1.06 | [0.77 | 1.45] | 1.08 | [0.96 | 1.21] |
| Doctor-patient communication modalities during the COVID-19 pandemic | ||||||||||||
| Emails | ||||||||||||
| Video calls | 2.86 | [2.42 | 3.38] | |||||||||
| Phone calls | 2.51 | [2.02 | 3.12] | 2.37 | [1.89 | 2.96] | ||||||
| In-person | 0.89 | [0.76 | 1.05] | 0.88 | [0.74 | 1.04] | 1.06 | [0.96 | 1.18] | |||
Notes. All models adjust for confounders (marital status, gender, age, a sum score of all self-reported health conditions, pre-COVID mental health symptoms, and living alone). Bold indicates significance at the <0.05 level. aPR is an abbreviation for adjusted prevalence ratio.
Adjusted Poisson regression analyses examining communication and feelings of anxiety, depression, and/or loneliness revealed that use of emails (aPR = 1.28, 95% CI: 1.08–1.52) and video calls for corresponding with friends and family (aPR = 1.22, 95% CI: 1.06–1.41) were associated with feelings of anxiety/worry. Similarly, use of email (aPR = 1.23, 95% CI: 1.01–1.45), video calls (aPR = 1.20, 95% CI: 1.01–1.41), and phone calls (aPR = 1.25, 95% CI: 1.06–1.46) for communicating with a healthcare provider was associated with feelings of anxiety/worry. Use of phone to communicate with a healthcare provider was associated with loneliness (aPR = 1.26, 95% CI: 1.05–1.52). On the other hand, visiting with friends and family in-person was associated with fewer feelings of depression (aPR = 0.82, 95% CI: 0.69–0.97). Similarly, in-person visits to a healthcare provider were associated with reduced feelings of loneliness (aPR = 0.84, 95% CI: 0.74–0.97), Table 4.
Table 4.
Adjusted Poisson Regression Models Examining the Relationship between Communication Modalities with Friends and Family and Healthcare Providers and Feelings of Anxiety, Depression, and Loneliness during the COVID-19 Pandemic.
| Feelings of Anxiety/Worry About COVID-19 (Comparison: “Rarely” or “Never”) | Feelings of Depression About COVID-19 (Comparison: “Rarely” or “Never”) | Feelings of Loneliness During COVID-19 (Comparison: “Rarely” or “Never”) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | |||||||
| aPR | Lower | Upper | aPR | Lower | Upper | aPR | Lower | Upper | |
| Friends and family communication during the COVID-19 pandemic | |||||||||
| Emails | 1.28 | [1.08 | 1.52] | 1.26 | [1.05 | 1.52] | 1.19 | [01.01 | 1.43] |
| Video calls | 1.22 | [1.06 | 1.41] | 1.16 | [0.98 | 1.35] | 1.12 | [0.96 | 1.26] |
| Phone calls | 1.63 | [0.93 | 2.82] | 1.88 | [1.00 | 3.53] | 1.16 | [0.61 | 2.06] |
| In-person | 0.92 | [0.78 | 1.07] | 0.82 | [0.69 | 0.97] | 0.90 | [0.77 | 1.07] |
| Doctor-patient communication during the COVID-19 pandemic | |||||||||
| Emails | 1.23 | [1.01 | 1.45] | 1.02 | [0.82 | 1.25] | 1.08 | [0.92 | 1.27] |
| Video calls | 1.20 | [1.10 | 1.41] | 1.15 | [0.98 | 1.41] | 1.07 | [0.94 | 1.26] |
| Phone calls | 1.25 | [1.06 | 1.46] | 1.26 | [1.05 | 1.52] | 1.17 | [1.05 | 1.37] |
| In-person | 0.90 | [0.78 | 1.04] | 0.93 | [0.79 | 1.10] | 0.84 | [0.74 | 0.97] |
Notes. All models adjust for confounders (marital status, gender, age, a sum score of all self-reported health conditions, pre-COVID mental health symptoms, and living alone). Bold indicates significance at the p < 0.05 level. aPR is an abbreviation for adjusted prevalence ratio.
Discussion
Our analysis of data collected during the COVID-19 pandemic among older adults in the US reveal demographic differences in in-person and digital communication with friends and family and with healthcare providers. Our results revealed less use of digital communication (email or video) with friends and family or healthcare providers among those 85 years of age and older compared to those age 65 to 69. Previous research demonstrates that adults report more feelings of frustration with digital technology than do younger adults (Kotwal et al., 2021), which could hinder utilization of these platforms, particularly among older adults. We also observed less use of digital communication with friends and family or healthcare providers in those widowed, never married, and those living alone. Previous research found older adults were interested in making video calls during COVID-19 to friends and loved ones, but required assistance, such as from a loved one or helper to do so (Sacco et al., 2020). Therefore, the presence of a spouse or partner in the household may serve as a source of information and support for the use of digital technologies.
Our findings show that Black/Non-Hispanic and Hispanic/Latino individuals were less likely to report using email for communication with friends and family. This may be due to less access to digital devices and the Internet. This finding is consistent with previous research demonstrating a disparity in access to and literacy relating to digital technologies among racial/ethnic minority groups as compared to Whites (Bailey et al., 2015; Kotwal et al., 2021; Lankshear & Knobel, 2008). On the other hand, Black/non-Hispanic and Hispanic/Latino individuals were more likely to use the phone with a healthcare provider than were White/non-Hispanic individuals. Our findings contrast previous research that shows Black individuals marked phone as less preferable than did White individuals for receiving test results from their dermatologist (Thareja et al., 2018). It is possible that the type of health information being communicated is an important consideration in understanding communication patterns and preferences.
Our study also demonstrated less use of digital communication as well as in-person visits with friends and family and with healthcare providers among those with Alzheimer’s disease. Those with Alzheimer’s disease or related dementia were also less likely to report communication with their healthcare provider via email or phone. It is possible that those with Alzheimer’s disease or related dementia had limited capacity to recall their communication platform and the specific modalities. It is also possible that these results do reflect less communication among those with this condition, which could further limit these individuals in their ability to maintain quality of life and progress with respect to treatment. Future research may consider using objective measures of communication (e.g., capturing the number of calls from logs in a smartphone device) to avoid the burden of self-report and reliance upon participants' memory, which could bias responses from individuals suffering from Alzheimer’s disease or related dementia.
Our results also revealed that those who reported using digital communication tools (e.g., video calls or emails) with healthcare providers also reported using these modalities for communication with friends and family during the COVID-19 pandemic. This could suggest that those who feel comfortable using digital media for communication with friends and family also feel comfortable using these platforms for communication with healthcare providers.
Finally, we found approximately 20% of participants reported feeling depression and 25% reported feeling anxious about the COVID-19 pandemic. These proportions of participants were slightly lower than pre-COVID-19 estimates of depression among older adults, which estimated approximately 30% of older adults suffer from depression (Zenebe et al., 2021), which is surprising because one could hypothesize that more older adults might experience feelings than those that meet a clinical diagnosis. On the other hand, prevalence of anxiety in older adults prior to COVID-19 was approximately 15%, which is lower than the reported feelings of anxiety about the COVID-19 pandemic in our study.
Our results exploring differences in communication modalities by feelings of depression or anxiety due to the COVID-19 pandemic found higher reports of digital communication with both friends and family and healthcare providers among those reporting feelings of anxiety about the COVID-19 pandemic. We also observed more in-person communication with both friends and family and healthcare providers among those reporting fewer feelings of depression and loneliness during the COVID-19 pandemic. There are several possible explanations for these findings. It is possible that those able to sustain in-person interactions received more social support and were able to buffer themselves against the mental health impacts of the COVID-19 pandemic. On the other hand, it is also possible that those with mental health concerns (e.g., feelings of depression or anxiety about the COVID-19 pandemic) were more reclusive and avoided in-person interactions. Given that the data analyzed in the present study were cross-sectional in nature, future research is needed to better understand the directionality of these relationships. Moreover, given that it has been argued that technology may alleviate isolation associated with the COVID-19 pandemic (Gabbiadini et al., 2020) it would be important to ensure these technologies do not impose undue stress or anxiety. It is also plausible that those using digital tools for communication were also consuming news that may have been unsettling and anxiety- or depression-inducing on digital platforms.
With the introduction of social distancing measures to curb the spread of COVID-19, older adults faced an elevated risk for isolation, fewer in-person interactions, and adverse mental health symptoms. Our study identified demographic differences in digital and in-person communication among by older adults with friends and family members and healthcare providers during the COVID-19 pandemic. We also uncover that those who report digital communication tools, such as video for calling, report using these modalities with friends and family members as well as with healthcare providers, suggesting that ease with a digital modality of communication in one domain, such as communicating with friends, may translate to confidence and ease with the modality in communication with a healthcare provider. Future research is needed to uncover the preferences, barriers, and facilitators to technology use among older adults and ways to preserve in-person interactions that appear to offer the most significant benefit to older adults in terms of mental health well-being. Some of these efforts may overcome previous research findings, which show technology and internet-supported interventions for older adults have not yielded positive results on mental health targets (Chipps et al., 2017). According to one literature review, there are nuanced barriers and facilitators to the adoption of technologies for health-related purposes, including misperceptions about technological performance, limited access, and low awareness about technology capabilities for health-related functions (Wildenbos et al., 2017).
Limitations
Our study is subject to several limitations. First, the NHATS is a nationally representative survey, which is a significant strength; yet, not all NHATS participants responded to the COVID-19 supplement. Second, the cross-sectional nature of these data is important to note and preclude the ability to draw causality or directionality of the relationships observed in this study. Therefore, it is possible that adverse mental health symptoms caused lower uptake of digital technology for communication. Still, it is also possible that the reverse is true, that lower use of digital technology or communication leads to worse mental health; yet, future research is necessary to make such claims. Another limitation of the present analysis is that these data were collected early in the COVID-19 pandemic when technology use may have been higher than normal due to strict mitigation guidelines, such as social distancing.
Conclusion
Older adults face an elevated risk poor mental health during the COVID-19 pandemic. Unfortunately, necessary public health measures to reduce risk of COVID-19 may have exacerbated the risk for loneliness and mental health concerns among these individuals. While technology has been touted as a tool for attenuating the mental health implications of social isolation and distancing, previous research shows these tools are underutilized among older adults. Our study documents demographic differences in digital and in-person communication with friends, family, and loved ones during COVID-19. We also discovered that in-person interactions with friends, family, and healthcare providers were associated with fewer mental health concerns. In contrast, interactions using digital technologies were associated with feelings of depression and anxiety about COVID-19. Future research may consider ways of tailoring technologies or bolstering digital literacy among older adult populations.
Acknowledgments
The authors respectfully acknowledge Dr. Brian Clagett for his biostatistics guidance.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Robbins reports consulting fees from Rituals Cosmetics BV, Denihan Hospitality Group, SleepCycle AB, Loóna Inc., Oura Ring Ltd., and Savoir Beds Ltd.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Robbins is supported on a grant from the NIH-NHLBI [K01HL150339].
ORCID iD
Rebecca Robbins https://orcid.org/0000-0003-0288-2505
References
- Bailey S. C., O’Conor R., Bojarski E. A., Mullen R., Patzer R. E., Vicencio D., Jacobson K. L., Parker R. M., Wolf M. S. (2015). Literacy disparities in patient access and health-related use of Internet and mobile technologies. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy, 18(6), 3079–3087. 10.1111/hex.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chipps J., Jarvis M. A., Ramlall S. (2017). The effectiveness of e-interventions on reducing social isolation in older persons: A systematic review of systematic reviews. Journal of Telemedicine and Telecare, 23(10), 817–827. 10.1177/1357633X17733773 [DOI] [PubMed] [Google Scholar]
- Cohen S. (2004). Social relationships and health. American Psychologist, 59(8), 676–684, 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- Cudjoe T. K. M., Kotwal A. A. (2020). “Social distancing” amid a crisis in social isolation and loneliness. Journal of the American Geriatrics Society, 68(6), E27, E29. 10.1111/jgs.16527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M. É., Howard M. E., Robbins R., Barger L. K., Facer-Childs E. R., Rajaratnam S. M. W., Czeisler C. A. (2021). Early public adherence with and support for stay-at-home COVID-19 mitigation strategies despite adverse life impact: A transnational cross-sectional survey study in the United States and Australia. BMC Public Health, 21(1), 503. 10.1186/s12889-021-10410-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M. É., Lane R. I., Petrosky E., Wiley J. F., Christensen A., Njai R., Weaver M. D., Robbins R., Facer-Childs E. R., Barger L. K., Czeisler C. A., Howard M. E., Rajaratnam S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24-30, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V., Hu M. (2020). COVID-19 supplement to the national health and aging Trends study user guide. Beta Release. Johns Hopskins Bloomberg School of Public Health. nhats.org. [Google Scholar]
- Gabbiadini A., Baldissarri C., Durante F., Valtorta R. R., De Rosa M., Gallucci M. (2020). Together apart: The mitigating role of digital communication technologies on negative affect during the COVID-19 outbreak in Italy. Frontiers in Psychology, 11, 554678. 10.3389/fpsyg.2020.554678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon N. P., Hornbrook M. C. (2016). Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. Journal of Medical Internet Research, 18(3), e50. 10.2196/jmir.5105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould C. E., Hantke N. C. (2020). Promoting technology and virtual visits to improve older adult mental health in the face of COVID-19. The American Journal of Geriatric Psychiatry, 28(8), 889–890. 10.1016/j.jagp.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirvonen N., Enwald H., Känsäkoski H., Eriksson-Backa K., Nguyen H., Huhta A.-M., Huvila I. (2020). Older adults’ views on eHealth services: A systematic review of scientific journal articles. International Journal of Medical Informatics, 135, 104031. 10.1016/j.ijmedinf.2019.104031 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T. B., Layton J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLOS Medicine, 7(7), Article e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal A. A., Holt-Lunstad J., Newmark R. L., Cenzer I., Smith A. K., Covinsky K. E., Escueta D. P., Lee J. M., Perissinotto C. M. (2021). Social isolation and loneliness among san francisco bay area older adults during the COVID-19 shelter-in-place orders. Journal of the American Geriatrics Society, 69(1), 20–29. 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankshear C., Knobel M. (2008). Digital literacies: Concepts, policies and practices. Peter Lang. [Google Scholar]
- Lewnard J. A., Lo N. C. (2020). Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet. Infectious Diseases, 20(6), 631–633. 10.1016/S1473-3099(20)30190-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1–2), 86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- Pew Research . (2017). Tech adoption climbs among older Americans. Pew Research Center: Internet, Science and Tech. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/ [Google Scholar]
- Sacco G., Lléonart S., Simon R., Noublanche F., Annweiler C., TOVID Study Group (2020). Communication technology preferences of hospitalized and institutionalized frail older adults during COVID-19 confinement: Cross-sectional survey study. JMIR MHealth and UHealth, 8(9), e21845. 10.2196/21845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thareja S., Fink M., Chen K.-H., Liu Y., Chen S. C., Stoff B. K. (2018). Race as a predictor of patient preferences for biopsy result communication. Journal of the American Academy of Dermatology, 78(6), 1223–1225. 10.1016/j.jaad.2017.11.054 [DOI] [PubMed] [Google Scholar]
- Wildenbos G. A., Peute L., Jaspers M. (2017). Facilitators and barriers of electronic health record patient portal adoption by older adults: A literature study. Studies in Health Technology and Informatics, 235, 308–312. 10.3233/978-1-61499-753-5-308 [DOI] [PubMed] [Google Scholar]
- Zenebe Y., Akele B., W/Selassie M., Necho M. (2021). Prevalence and determinants of depression among old age: A systematic review and meta-analysis. Annals of General Psychiatry, 20(1), 55. 10.1186/s12991-021-00375-x [DOI] [PMC free article] [PubMed] [Google Scholar]