胸痛是急诊科常见的主诉,食管异物(esophageal foreign body,EFB)的摄入是导致胸痛的重要原因之一,并可能引起一系列危及生命的情况。在本文中我们报道了一例病例:一名67岁的中国女性因胸痛入住当地医院,因患者两年前曾有心肌梗死病史,当地医院以急性冠脉综合征对症治疗,然而患者的症状始终不缓解且出现发热,转至我院后行胸部CT提示食管异物伴食管穿孔。患者紧急接受了内镜下食管异物取出术,取出一根长约3 cm的鸭骨头。考虑到中国有着多元的饮食文化,许多中国人习惯啃食鸡骨、鸭骨和猪骨,这会大大增加成人食管异物摄入的风险。本病例旨在提高急诊医师对于食管异物引发胸痛的意识,并提示了通过及时的内镜下治疗可以大大降低食管溃疡、食管出血、肺部感染等并发症的发生风险,进而改善患者预后,缩短住院时间。
Keywords: 食管异物, 胸痛, 食管穿孔
Chest pain is one of the most common complaints in the emergency department. Diseases of the heart, aorta, lungs, esophagus, stomach, mediastinum, pleura, and abdominal viscera can all cause chest discomfort (Gulati et al., 2021; Jiao et al., 2021; Lu et al., 2022). Clinicians in the emergency department are expected to immediately recognize life-threatening chest pain (Jiao et al., 2021). Delayed diagnosis further increases the risk of complications and mortality (Liu et al., 2021). In this case, we present an elderly Chinese female who had a history of myocardial infarction two years previously, with chest pain eventually found to be caused by ingestion of a duck bone.
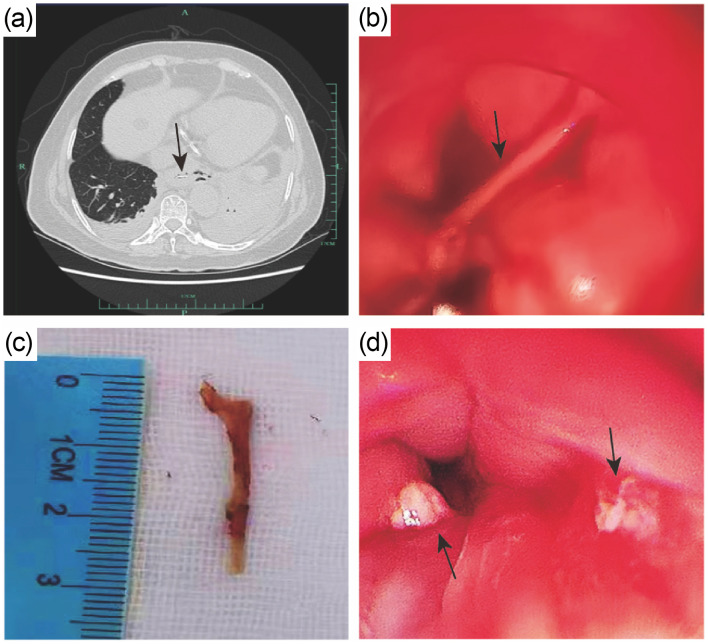
A 67-year-old Chinese woman was presented to the emergency department of the First Affiliated Hospital, Zhejiang University School of Medicine (Hangzhou, China), with recurrent chest pain lasting 4 d. Considering that she had a history of myocardial infarction and had undergone a right distal coronary stent implantation performed two years earlier, she was admitted to the local hospital on the first day with an initial diagnosis of acute coronary syndrome. However, the laboratory tests (including myocardial enzyme spectrum, troponin, and cardiac ultrasound) did not reveal any significant abnormality. The electrocardiogram showed paroxysmal atrial fibrillation. Initially, no chest X-ray was performed. Despite receiving conservative treatment of antiischemic and antiplatelet therapy and ventricular rate control for atrial fibrillation to improve her heart symptoms, the patient still suffered from chest pain, accompanied by fever (the highest body temperature was 38.9 ℃) and mildly poor appetite, but no dysphagia or salivation. The laboratory tests showed a gradually increased level of C-reactive protein (101.74 mg/L). The patient was subsequently transferred to our hospital. After taking a comprehensive medical history, we found that she had eaten a cooked duck four days earlier. A computed tomography (CT) scan of the chest was then performed, and indicated a sharp foreign body at the lower end of the esophagus with perforation; there was also pleural effusion on both sides with collapsed lung tissue (Fig. 1a). An emergency endoscopy for esophageal foreign body (EFB) removal was performed under general anesthesia (Figs. 1b and 1d; Video S1) and a duck bone about 3 cm in length was removed from her esophagus (Fig. 1c). The patient’s chest pain was greatly relieved after the operation. Considering the age of the patient and the esophageal perforation with pulmonary and pleural inflammation, we administered broad-spectrum antibiotics (linezolid and meropenem) intravenously for 3 d. The levels of inflammatory indicators gradually decreased and the chest pain disappeared. The patient was discharged 12 d after admission. At a one-month follow-up, the patient had a favorable outcome.
Fig. 1. Images of the esophageal foreign body. (a) The chest computed tomography (CT) suggested a foreign body at the end of the esophagus (indicated by the black arrow). Gas accumulation on the left side and perforation was found, along with bilateral pneumonia, bilateral pleural effusion, and partial distension of the left lower lobe. (b) A foreign body (indicated by the black arrow) was inserted into the wall of the esophagus at 35 cm of the esophagus from the incisor, and produced pus emission. (c) The esophageal foreign body: a duck bone approximately 3 cm in length. (d) The mucosa of the upper esophagus was swollen after removal of the foreign body.
Ingestion of a foreign body can cause chest pain, and the esophagus is the most frequent site of obstruction in the gastrointestinal tract due to luminal narrowing. In cases of EFB ingestion, patients may experience life-threatening symptoms such as cervical abscesses, mediastinitis, aortoesophageal abscesses, tracheoesophageal fistulae, pneumonia, pneumothorax, or hemorrhage; these often occur in association with aortic pseudoaneurysms, aortoesophageal fistulae, or aortic dissection (Zhao and Lu, 2014; Ruan et al., 2020), most of which are caused by esophageal perforation (Ruan and Lu, 2020). All EFBs should be removed within 24 h. Emergency endoscopy is preferably performed within 2–6 h on patients with complete esophageal obstruction, disk batteries, or sharp-pointed objects in the esophagus, since the risk of complications increases dramatically over time (Birk et al., 2016).
China has a diverse food culture, and many Chinese people are accustomed to gnawing on chicken, duck, and pork bones, greatly increasing the risk of EFBs in adults (Ruan et al., 2020). In this case, the patient’s previous history of coronary artery disease and inflammatory manifestations interfered with the initial diagnosis. Therefore, it is of great importance for clinicians to ask detailed questions about disease onset, not only with regard to past medical history, but also diet. When a young clinician is faced with a patient with multiple clinical symptoms, he or she should follow the principle of monism whenever possible, meaning that they should attempt to explain two or more clinical manifestations as being caused by one disease or pathophysiological mechanism.
In conclusion, EFB is often overlooked by clinicians as a cause of chest pain due to less detailed etiological factors. Even if the patient has a history of heart disease, the possibility of EFB ingestion must be considered. Timely endoscopic intervention can prevent complications such as esophageal ulcers, esophagorrhagia, and pulmonary infection, leading to a better prognosis and a shorter hospital stay.
Supplementary information
Acknowledgments
This work was supported by the Key Research and Development Program of Zhejiang Province (No. 2019C03076), China.
Author contributions
Chengfan QIN studied the concept and prepared the first draft of the manuscript. Yunmei YANG made critical revisions to the article. Yuanqiang LU checked and confirmed the final version. All authors have read and approved the final manuscript.
Compliance with ethics guidelines
Chengfan QIN, Yunmei YANG, and Yuanqiang LU declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013. Informed consent was obtained from the patient for being included in the study. This study protocol was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (Study ID: 20230164).
References
- Birk M, Bauerfeind P, Deprez PH, et al. , 2016. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy, 48(5): 489-496. 10.1055/s-0042-100456 [DOI] [PubMed] [Google Scholar]
- Gulati M, Levy PD, Mukherjee D, et al. , 2021. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation, 144(22): e368-e454. 10.1161/CIR.0000000000001029 [DOI] [PubMed] [Google Scholar]
- Jiao Y, Wang JH, Yang X, et al. , 2021. Evaluation of the prognostic ability of serum uric acid for elderly acute coronary syndrome patients with diabetes mellitus: a prospective cohort study. J Zhejiang Univ-Sci B (Biomed & Biotechnol), 22(10): 856-865. 10.1631/jzus.B2000637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CY, Chen SX, Zhang HF, et al. , 2021. Bioinformatic analysis for potential biological processes and key targets of heart failure-related stroke. J Zhejiang Univ-Sci B (Biomed & Biotechnol), 22(9): 718-732. 10.1631/jzus.B2000544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu JQ, Liu JY, Li A, 2022. Roles of neutrophil reactive oxygen species (ROS) generation in organ function impairment in sepsis. J Zhejiang Univ-Sci B (Biomed & Biotechnol), 23(6): 437-450. 10.1631/jzus.B2101075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WS, Lu YQ, 2020. The life-saving emergency thoracic endovascular aorta repair management on suspected aortoesophageal foreign body injury. World J Emerg Med, 11(3): 152-156. 10.5847/wjem.j.1920-8642.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WS, Li YN, Feng MX, et al. , 2020. Retrospective observational analysis of esophageal foreign bodies: a novel characterization based on shape. Sci Rep, 10: 4273. 10.1038/s41598-020-61207-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao XH, Lu YQ, 2014. Multiple embolisms resulted from a huge fishbone piercing the left atrium. Intensive Care Med, 40(4): 621-622. 10.1007/s00134-014-3232-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.