Abstract
Background
Mental health and substance use disorders disproportionately affect people with HIV (PWH), and may have been exacerbated during COVID-19. The Promoting Access to Care Engagement (PACE) trial was designed to assess the effectiveness of electronic screening for mental health and substance use in HIV primary care and enrolled PWH from October 2018 to July 2020. Our objective here was to compare screening rates and results for PWH before (October 2018 – February 2020) and early in the COVID-19 pandemic (March-July 2020).
Methods
Adult (≥ 18 years) PWH from 3 large HIV primary care clinics in a US-based integrated healthcare system were offered electronic screening online or via in-clinic tablet computer every 6 months. Screening completion and results (for depression, suicidal ideation, anxiety, and substance use) were analyzed using logistic regression with generalized estimating equations to estimate prevalence ratios (PR) before and after the start of the regional COVID-19 shelter-in-place orders on March 17, 2020. Models adjusted for demographics (age, sex, race/ethnicity), HIV risk factors (men who have sex with men, injection drug use, heterosexual, other), medical center, and modality of screening completion (online or tablet). We conducted qualitative interviews with providers participating in the intervention to evaluate how the pandemic impacted patient care.
Results
Of 8,954 eligible visits, 3,904 completed screenings (420 during COVID, 3,484 pre-COVID), with lower overall completion rates during COVID (38% vs. 44%). Patients completing screening during COVID were more likely to be White (63% vs. 55%), male (94% vs. 90%), and MSM (80% vs., 75%). Adjusted PRs comparing COVID and pre-COVID (reference) were 0.70 (95% CI), 0.92 (95% CI), and 0.54 (95% CI) for tobacco use, any substance use, and suicidal ideation, respectively. No significant differences were found by era for depression, anxiety, alcohol, or cannabis use. These results were in contrast to provider-reported impressions of increases in substance use and mental health symptoms.
Conclusion
Findings suggest PWH had modest declines in screening rates early in the COVID-19 pandemic which may have been affected by the shift to telemedicine. There was no evidence that mental health problems and substance use increased for PWH in primary care.
Trial registration
NCT03217058 (First registration date: 7/13/2017); https://clinicaltrials.gov/ct2/show/NCT03217058
Keywords: HIV, Screening, Substance use, Mental Health, COVID-19
Introduction
Depression, anxiety, and substance use disorders disproportionately affect people with HIV (PWH) compared with people without HIV, and are associated with poor HIV clinical outcomes (e.g., HIV viral control) [1, 2] and increased mortality. [3, 4] The COVID-19 pandemic was anticipated to exacerbate these issues among PWH.
At the pandemic outset, concerns were raised about potential increases in depression, anxiety, and alcohol and drug use in the general population and in vulnerable subgroups. [5, 6] In the first year of the pandemic, global prevalence of anxiety and depression increased by 25%. [7] Use of alcohol and cannabis also increased, particularly in people with anxiety and depression. [8] For PWH, worsening of mental health care access and increases in alcohol and substance use were also anticipated. [9–12] Despite these concerns, few studies have examined the impact of the COVID-19 pandemic on mental health and substance use among PWH, nor have studies evaluated potential changes in screening for these problems. In studies of early COVID-19 responses in PWH, specifically, heightened anxiety and depression were reported but changes in in substance use were not consistently found. [13–16] To our knowledge, no studies have examined differences in screening rates and prevalence of substance use and mental health symptoms in PWH delivered in the context of primary care. The current study leveraged data from an HIV primary care-based trial implemented prior to and continuing through the start of the early COVID era in order to address these important questions.
The Promoting Access to Care Engagement (PACE) trial implemented computerized, self-reported screening for mental health disorders and substance use in conjunction with HIV primary care appointments, with referral to behavioral health specialists for treatment. [17] The PACE trial implemented screening at three HIV primary care clinics prior to the onset of the COVID-19 pandemic, which continued into the early months of the pandemic. The current analysis aimed to compare differences in screening rates and prevalence of self-reported depression, suicidal ideation, anxiety, and substance use among PWH before and early in the pandemic. We supplemented these findings with qualitative interviews with HIV primary care providers regarding their perspectives on the pandemic’s impact on the health of their patients.
Methods
The PACE trial combined mental health and substance use screening measures into a single, self-report questionnaire systematically administered via online secure message or in-clinic tablets. The questionnaire was offered every 6 months to PWH, in connection with their regular primary care appointments. [17] PACE was completed in the three largest HIV primary care clinics (Oakland, Sacramento, and San Francisco) in Kaiser Permanente Northern California, which collectively serve over 5000 PWH (roughly half of all PWH in the health system). Eligible participants were all adult (≥ 18 years) PWH attending HIV care visits with participating providers from October 2018 to July 2020, at which time the study was scheduled to be completed. PWH could complete the questionnaire via online secure messaging up to two weeks prior to a scheduled visit or in clinic on a tablet. After the onset of the COVID-19 pandemic, telemedicine visits were included since in person visits were limited for several months.
The questionnaire combined several measures into a single instrument that was sent to the patient prior to their visit: The Tobacco, Alcohol, Prescription medication and other Substance use (TAPS) instrument [18] was used to assess substance use, the Patient Health Questionnaire (PHQ-9) [19] was used for depression and the Generalized Anxiety Disorder (GAD-2) [20] was used for anxiety. These measures have previously been validated for electronic self-administration. [21] The TAPS tool, specifically, has high levels of specificity and sensitivity across substances, as well as a high level of patient acceptability, with 99% of participants comfortable answering questions and 95% of participants comfortable sharing their results with their provider. [22] We defined a positive screen for depression as PHQ-9 score ≥ 10, suicidal ideation as PHQ-9 question 9 score > 0, anxiety as GAD-2 score ≥ 3, and substance use as a TAPS score ≥ 1 for each substance. “Any substance use” was defined as a positive screen for at least one substance. To evaluate how representative the screened sample was of the eligible primary care population of PWH at the three study sites, we compared demographic and clinical characteristics of those who completed the questionnaire with those who did not complete it, using chi-square and t-tests for comparison between groups.
We compared the proportion of eligible visits with a completed screen, and the proportion of positive screens for depression, suicidal ideation, anxiety, and substance use before and after the start of regional COVID-19 shelter-in-place orders on March 17, 2020. We estimated adjusted prevalence ratios (aPRs) using generalized estimating equations (GEE) with robust standard errors to account for multiple visits contributed by patients. Models were adjusted for demographics (age, sex, self-reported race/ethnicity); HIV risk factors (men who have sex with men [MSM], injection drug use [IDU], Heterosexual, Other); Medical Center (Oakland, Sacramento, San Francisco); and screening modality (online, tablet). Analyses were performed using Proc Genmod in SAS v. 9.4 (Cary, NC).
To evaluate how the COVID-19 pandemic impacted patient care, particularly screening and treatment for mental health and substance use, we also conducted interviews with an HIV care provider from each site (including authors JF and MNL). We used convenience sampling to select a participating HIV provider at each study site after the onset of the pandemic. Verbal informed consent was obtained from providers, who did not receive compensation for participation. Interviews lasted approximately 30 min and were audio recorded and transcribed.
We used a thematic approach to analyze qualitative interview data, combining deductive and inductive reasoning, for coding and analysis. [23, 24] This approach was chosen to identify and evaluate both explicit and implicit perspectives provided by interviewees, which were identified as both themes and sub-themes. Two authors (AA & ANL) independently coded all of the transcripts. Differences in coding were resolved via consensus, and final codebooks were established. Data analysis was managed using NVivo statistical software version 12 (QSR International) and followed standard methods for qualitative research to ensure analysis was systematic and verifiable. [25, 26]
All study procedures were approved by the Kaiser Permanente Northern California and University of California, San Francisco Institutional Review Boards and carried out in accordance with required guidelines and regulations.
Results
Over the course of the entire intervention period (October 2018 through July 2020), there were 8,954 eligible visits (7,849 pre-COVID and 1,105 during early COVID) scheduled by 4,134 unique PWH. Of the 7,849 eligible visits pre-COVID, 3,484 screenings were completed (44%) and of the 1,105 eligible visits during early COVID, 420 screenings were completed (38%).
Demographics
Regarding the representativeness of individuals who completed a screen compared with the eligible primary care population of PWH, individuals who did not complete a screen were less likely to be White (45% vs. 56%) and more likely to be Hispanic (22% vs. 15%) compared with PWH who had at least one screen (p < 0.01) (Table 1). Minor differences were also noted in age and HIV control (p < 0.01), while gender and HIV risk group did not significantly differ between PWH who did or did not complete a screen. Among PWH who completed a screen, the pre- and early-COVID samples had some similarities in demographics (age [median = 55 vs. 58], and risk group [6% vs. 5% IDU] (p ≤ 0.01); however, patients during COVID were more likely to be White (63% vs. 55%), male (94% vs. 90%), and MSM (80% vs. 75%) than pre-COVID (p ≤ 0.01) (Table 2).
Table 1.
Demographic and clinical characteristics of persons with HIV eligible for primary care-based substance use and mental health screening, stratified by screening completion (N = 4134)
| Characteristic | Completed ≥ 1 screen N = 2865 |
No screen completed N = 1269 |
p-value |
|---|---|---|---|
| Men | 2629 (92%) | 1152 (91%) | 0.2971 |
| Race and ethnicity | < .0001 | ||
| Asian or Pacific Islander | 198 (7%) | 88 (7%) | |
| Black | 558 (19%) | 278 (22%) | |
| Hispanic | 419 (15%) | 277 (22%) | |
| White | 1602 (56%) | 574 (45%) | |
| Other/unknown | 88 (3%) | 52 (4%) | |
| Age, years | 54 (13) | 51 (13) | < .0001 |
| HIV risk group | 0.0615 | ||
| MSM | 2170 (76%) | 922 (73%) | |
| IDU | 185 (6%) | 103 (8%) | |
| Heterosexual or other | 510 (18%) | 244 (19%) | |
| CD4 count, a cells/µL | 674 (306) | 639 (302) | 0.0023 |
| HIV RNA < 200 copies/mL a | 2678 (96%) | 1111 (93%) | 0.0001 |
| Insurance type | 0.0405 | ||
| Private | 1968 (69%) | 885 (70%) | |
| Medicare | 732 (26%) | 287 (23%) | |
| Medicaid | 142 (5%) | 85 (7%) | |
| Other | 23 (1%) | 12 (1%) | |
| NDI quartile b | 0.9927 | ||
| 1 (least deprived) | 717 (25%) | 315 (25%) | |
| 2 | 726 (25%) | 319 (25%) | |
| 3 | 704 (25%) | 317 (25%) | |
| 4 (most deprived) | 712 (25%) | 317 (25%) |
Numbers are N (%) or mean (SD). Abbreviations: IDU, injection drug use; MSM, men who have sex with men; NDI, neighborhood deprivation index; SD, standard deviation.
a Closest measurement within six months before or after screening date, or first eligible visit for patients with no completed screen.
b Calculated according to Messer et al. (2006) and divided in quartiles based on the distribution of the entire patient sample.
Table 2.
Characteristics of patients screened before COVID and during early COVID, including multiple screens per patient.
| Before COVID | Early COVID | |||
|---|---|---|---|---|
| Eligible visits, n | 7849 | - | 1105 | - |
| Screenings completed, n (%) | 3484 | 44% | 420 | 38% |
| Patient Characteristics, n (%) | ||||
| Age, median (IQR) | 55 | 46–62 | 58 | 48–66 |
| Sex | ||||
| Male | 3147 | 90% | 395 | 94% |
| Female | 337 | 10% | 25 | 6% |
| Risk group | ||||
| MSM | 2621 | 75% | 338 | 80% |
| Heterosexual | 465 | 13% | 34 | 8% |
| IDU | 217 | 6% | 21 | 5% |
| Other | 181 | 5% | 27 | 6% |
| Race | ||||
| White | 1914 | 55% | 264 | 63% |
| Black | 718 | 21% | 57 | 14% |
| Hispanic | 513 | 15% | 66 | 16% |
| Other | 181 | 5% | 27 | 6% |
| Appointment Facility | ||||
| Oakland | 1516 | 44% | 152 | 36% |
| Sacramento | 878 | 25% | 66 | 16% |
| San Francisco | 1090 | 31% | 202 | 48% |
| Answer Modality | ||||
| Exam Room Computer | 19 | 1% | 0 | 0% |
| Online | 2265 | 65% | 419 | 100% |
| Tablet | 1200 | 34% | 1 | 0% |
Notes: IQR, interquartile range; MSM, men who have sex with men; IDU, intravenous drug use
Screening rates
Of 7,849 eligible visits pre-COVID, 3,484 (44%) had a completed screen, compared with 420 of 1,105 eligible visits (38%) during early COVID (Table 2). By clinic, screening rates pre- and early-COVID decreased in Oakland (41% of all eligible appointments vs. 30%) and Sacramento (59% vs. 39%) but increased in San Francisco (41% vs. 48%) (Table 3). Overall screening completion decreased during early COVID vs. pre-COVID (38% vs. 44% of eligible visits; adjusted prevalence ratio [aPR] = 0.74, 95% CI = 0.65–0.85).
Table 3.
Screening completion rates before COVID and during early COVID by site
| Before COVID | Early COVID | |||||
|---|---|---|---|---|---|---|
| Site | Attached | Completed. | Rate | Attached | Completed | Rate |
| OAK | 3,662 | 1,516 | 41% | 513 | 152 | 30% |
| SAC | 1,497 | 878 | 59% | 169 | 66 | 39% |
| SFO | 2,690 | 1,090 | 41% | 423 | 202 | 48% |
| Total | 7,849 | 3,484 | 44% | 1,105 | 420 | 38% |
Notes: *All p-values < .0001
Screening results
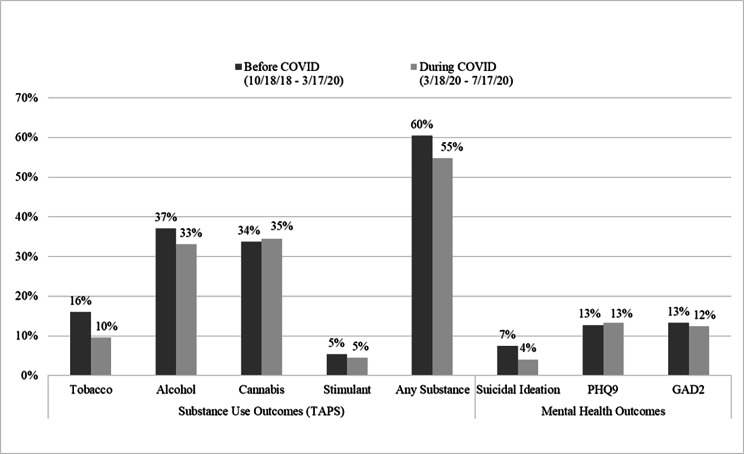
No significant differences were found during early COVID vs. pre-COVID in prevalence of depression (13% vs. 13%), anxiety (12% vs. 13%), alcohol use (33% vs. 37%) or cannabis use (35% vs. 34%) (Fig. 1). During early COVID, patients were less likely to report tobacco use (aPR = 0.70, 95% CI = 0.53–0.93), any substance use (aPR = 0.92, 95% CI = 0.84–1.00), and suicidal ideation (aPR = 0.54, 95% CI = 0.33–0.86) (Table 4).
Fig. 1.
Unadjusted Screening Results Before COVID vs. During Early COVID
Table 4.
Prevalence Ratios for Substance Use and Depression/Anxiety during early COVID compared to before COVID
| Unadjusted PR (95% CI) | p | Adjusted PR (95% CI)a | p | ||
|---|---|---|---|---|---|
| Substance Use (TAPS ≥ 1) | |||||
| Tobacco | 0.60 (0.45–0.80) | 0.001 | 0.70 (0.53–0.93) | 0.013 | |
| Alcohol | 0.89 (0.78–1.02) | 0.105 | 0.92 (0.81–1.05) | 0.222 | |
| Cannabis | 1.09 (0.90–1.17) | 0.712 | 1.03 (0.90–1.17) | 0.674 | |
| Stimulant | 0.84 (0.53–1.32) | 0.443 | 0.78 (0.50–1.22) | 0.271 | |
| Any Substance b | 0.91 (0.83–0.99) | 0.026 | 0.92 (0.84–1.00) | 0.043 | |
| Suicidal Ideation, Depression, Anxiety | |||||
| Suicidal Ideation | 0.54 (0.34–0.87) | 0.012 | 0.54 (0.33–0.86) | 0.01 | |
| Depression | 1.05 (0.82–1.35) | 0.709 | 1.11 (0.86–1.43) | 0.413 | |
| Anxiety | 0.94 (0.72–1.22) | 0.621 | 1.05 (0.80–1.36) | 0.738 | |
a Adjusted for age, sex, race/ethnicity, risk (MSM, IV Drug Use, Heterosexual, Other), and medical center
b Any substance includes: tobacco, alcohol, cannabis, stimulants, heroin, opioids, sedatives, Rx stimulant, IV drug use, and other drug use
We identified four major themes related to the impact of COVID on the care provision from the provider interviews, with subthemes identified for each (Table 5), Providers completing qualitative interviews at all three sites identified the shift to telemedicine as a significant contributor to differences pre-COVID and during early COVID, reporting changes to the patient rooming process during the shift to virtual visits, such as the transition to virtual exam rooms as well as limited appointment times requiring medical assistants to triage non-COVID patient screening as major factors. Additionally, the option to complete the survey via in-clinic tablet was no longer available due to fears related to COVID transmission, making access to technology an important consideration. Finally, under the theme of “Impact on substance use and mental health symptoms”, increases in patient-reported mental health symptoms were also reported by all providers. Providers at Oakland and San Francisco described an increase in patients’ alcohol use and smoking, while the providers at the Sacramento site felt that there were no major shifts in alcohol or drug use reported by patients.
Table 5.
Major themes and sub-themes identified in qualitative interviews with participating providers
| Major Themes | Sub-themes |
|---|---|
| 1. Access to HIV Care | Frequency of primary care visits |
| Frequency of HIV labs | |
| Access to antiretroviral therapy | |
| 2. Shift to Telemedicine | Physician workload |
| Appointment time limitations | |
| Ability to view screening results in EHR | |
| Mode of administration/Access to technology | |
| Staffing changes | |
| 3. Impact on Substance Use & Mental Health symptoms | Alcohol Use |
| Drug use | |
| Depression | |
| Anxiety | |
| 4. Impact on Substance Use & Mental Health treatment | Impact on provider referrals to specialty care |
| Impact on behavioral health services |
Notes: EHR, electronic health record
Discussion
In this study of PWH asked to complete substance use and mental health screening prior to regular HIV primary care appointments both before and after the onset of the COVID pandemic, overall mental health and substance use screening rates decreased. Self-reported suicidal ideation, tobacco use, and any substance use also decreased.
One possible explanation for the decrease in screening rates is that the questionnaire was intended to be given prior to regularly scheduled primary care visits, many of which were cancelled or delayed due to COVID transmission risk, resulting in reduced care engagement by PWH. This may have resulted in lower completion rates for appointments that shifted from in-person visits to telemedicine. Similarly, other studies have also shown decreases in care during this time for the general population [27], as well as PWH [28, 29].
Online completions required patients to have access to KP.org secure messaging to complete the questionnaire online prior to their appointment. Prior to COVID, the Oakland and Sacramento sites had similar rates for tablet (in-person) vs. online screening completion, while San Francisco skewed heavily towards online completions. During early COVID, the majority of completed appointments across all three sites shifted to a telemedicine (online) model. San Francisco was the only site that saw an increase in screening rates, which may indicate that their population was more comfortable with virtual care delivery, as compared with the other two sites.
Across all three sites, PWH who completed the study questionnaire during early COVID were more likely to be White, male, and MSM as compared with pre-COVID. It is worth noting that the demographics of the San Francisco site reflect the older, White MSM who make up the population of PWH in the city, as compared with the Oakland and Sacramento sites, who are younger and include greater proportions of racial/ethnic minority PWH, women, and heterosexual PWH [17]. Previous studies have shown PWH who do not identify as White to be less likely to utilize telehealth services compared with White patients. [28, 30] Our results also are consistent with prior findings that older PWH are more likely to attend telemedicine visits compared with younger patients due to a variety of potential factors such as familiarity with telephone appointments or lowering of barriers such as time or travel [15, 31], which may be particularly relevant in the context of COVID exposure fears.
No differences were found in self-reported levels of depression and anxiety. These results are in contrast to previous work showing increases in depression and anxiety in PWH during the early pandemic [14], including a recent meta-analysis by Lee et al. that found that the pooled prevalence rates of depression and anxiety among PWH were 16.9% (95% confidence interval [CI]: 3.8-30.0%) and 23.0% (95% CI: 12.0-34.0%), respectively [32]. However, similar results have been reported by Pizzirusso and colleagues and may be reflective of PWH being more engaged with care at the onset of the pandemic, as well as greater levels of psychological resiliency in older populations [33].
Although no differences were found in reported depression and anxiety, we did find a decrease in potential suicidal ideation during early vs. pre-COVID. Little has been published on suicidality in PWH during the early pandemic. One mixed methods study of PWH in the United Kingdom (UK) during a similar time period (May-July 2020) found 19.8% reporting suicidal thoughts at any point. [34] This study adds to this literature by examining a sample of PWH engaged in care in the United States (US) as well as being able to compare self-reported mental health outcomes both before and during the early COVID-19 pandemic. Studies in both the UK and the US have found that PWH reported higher levels of resilience and that prior experience with an infectious disease with potentially deadly consequences may have better equipped them emotionally for the pandemic compared with people without HIV. [34–36]
Finally, we also noted decreases in tobacco use and any substance use, and no differences for alcohol or cannabis use. These findings are consistent with prior work showing that smoking and illicit drug use were lower in PWH during the pandemic. [15, 16, 35] The pandemic decreased availability of illicit substances through supply chain disruption as well as lockdown and social distancing requirements limiting opportunities to engage in social use [5], factors that could have contributed to the reductions we found in this sample.
Although reasons for the contrasting observations of clinicians and patient-reported symptoms are not clear, it is possible that concerns about patient well-being during the pandemic may have influenced provider’s perceptions, or that contact with a small number of higher-severity patients (including perhaps ones who did not complete screening) influenced their perceptions.
Strengths & limitations
The PACE trial occurred during normal primary care visits in an integrated healthcare system with a diverse patient population. We had a large sample size and a substantial number of respondents who completed screening both pre- and during early COVID. However, there were some study limitations. First, our screening process was tied to upcoming attendance at primary care visits. While uncoupling screenings from visits might have increased the pool of individuals invited to complete screening questionnaires, it could also reduce the screening completion rate because most members of the healthcare system have been accustomed to receiving screening questionnaires prior to upcoming appointments of all types through the patient portal system. Linking screenings to upcoming visits may increase motivation to complete questionnaires, since patients anticipate that providers may expect a response. Primary care visits are a key component of routine health care in most settings and having screenings tied to upcoming primary care visits could make our results more generalizable to a variety of healthcare settings.
Our results were also based on self-report, which may result in underestimation of substance use. [37] However, the same technology and approach was utilized both pre- and during-COVID, which likely resulted in similar levels of underreporting in both time periods. There is a theoretical potential for changes in reporting patterns during the pandemic, e.g., due to either increased stigmatization [38] or normalization of substance use and mental health problems [39], although this has not been reported on to date. Self-administered questionnaires may also minimize response bias and promote accurate reporting. Additionally, although findings were adjusted for demographics, HIV risk factors, setting, and screening modality, some groups were small, particularly during the COVID period, which may have led to residual confounding. Finally, the COVID study period was relatively short (four months) and therefore only reflects the early phase of the pandemic. During this time, all primary care in the region quickly shifted to a telemedicine model and guidelines and recommendations for care engagement changed rapidly. Therefore, results may also reflect a shift in the patient population to those who were more adept at accessing telehealth or who were less likely to use substances than those who did not access care during the pandemic. However, it is important to note that this screening was embedded in routine HIV primary care, which may make it more generalizable to other HIV-positive populations than a randomized clinical trial, and that PWH in our study setting had high levels of secure messaging access and patient portal use prior to COVID.
Conclusion
We observed a decrease in substance use and mental health screening rates for PWH during early COVID, which may reflect reduced patient engagement with telemedicine in certain populations of PWH early in the pandemic. Contrary to expectations and to provider perceptions, we also found decreased tobacco and substance use and decreased suicidal ideation during the early months of the pandemic, which may reflect resiliency in this population. Care delivery is likely shifting to greater use of virtual visits over the long term, and future research should focus on longer-term outcomes and effective ways to screen for substance use and mental health symptoms in an increasingly remote-care environment.
Acknowledgements
We wish to thank Sujaya Parthasarathy for assistance in study design, and Hannah Jang, Courtney Ellis, and Gina Smith-Anderson for assistance in project management. We thank Gary Zin, Nancy Facher, and Nicholas Shapiro at The Permanente Medical Group Consulting Services for technical assistance; and the clinic staff at the Kaiser Permanente HIV primary care clinics in Oakland, Sacramento, and San Francisco.
List of Abbreviations
- aPR
Adjusted Prevalence Ratio
- GAD-2
Generalized Anxiety Disorder
- GEE
Generalized estimating equations
- IDU
Injection Drug Use
- MSM
Men who have sex with men
- PACE
Promoting Access to Care Engagement Trial
- PHQ-9
Patent Health Questionnaire
- PWH
People with HIV
- TAPS
Tobacco, Alcohol, Prescription medication and other Substance use instrument
Authors’ contributions
ANL contributed to project design, data acquisition and analysis, data interpretation, and manuscript generation. TML contributed to project design, data acquisition and analysis. TDM contributed to data interpretation. AL contributed to project design, data acquisition, data interpretation. AA contributed to data acquisition and analysis. JF, CBH, and ML contributed to project design and data interpretation. MJS and DDS designed the project, interpreted the data, and contributed to manuscript development and revision.
Funding
This study was supported by the National Institute on Drug Abuse (R01DA043139), the National Institute on Alcohol Abuse and Alcoholism (K24AA025703), and the Dolby Family Center for Mood Disorders at the University of California, San Francisco.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Waivers of informed consent and HIPAA authorizations were obtained for the data only portion by Kaiser Permanente Northern California and University of California, San Francisco Institutional Review Boards and study procedures were approved by Kaiser Permanente Northern California and University of California, San Francisco Institutional Review Boards. Verbal informed consent was obtained from providers participating in the qualitative interviews and no compensation was provided for participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Koenig LJ, Khurana N, Islam MH, Gopalappa C, Farnham PG. Closing the gaps in the continuum of depression care for persons with HIV: modeling the impact on viral suppression in the United States. AIDS. 2023. Mar 6. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 2.Bershteyn A, Richard E, Zhou Q, Khan MR, Scheidell JD, Manandhar-Sasaki P, et al. Potential health benefits of integrated screening strategies for alcohol, tobacco, other substance use, depression, anxiety, and chronic pain among people living with HIV in the USA: a mathematical modelling study. Lancet HIV. 2023;10(2):e118–e25. doi: 10.1016/S2352-3018(22)00361-7. [DOI] [PubMed] [Google Scholar]
- 3.DeLorenze GN, Satre DD, Quesenberry CP, Tsai AL, Weisner CM. Mortality after diagnosis of psychiatric disorders and co-occurring substance use disorders among HIV-infected patients. AIDS Patient Care STDS. 2010;24(11):705–12. doi: 10.1089/apc.2010.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chichetto NE, Kundu S, Freiberg MS, Butt AA, Crystal S, So-Armah KA, et al. Association of Syndemic Unhealthy Alcohol Use, cigarette use, and Depression with all-cause mortality among adults living with and without HIV infection: Veterans Aging Cohort Study. Open Forum Infect Dis. 2019;6(6):ofz188. doi: 10.1093/ofid/ofz188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaami S, Marinelli E, Varì MR. New Trends of substance abuse during COVID-19 pandemic: an International Perspective. Front Psychiatry. 2020;11:700. doi: 10.3389/fpsyt.2020.00700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satre DD, Iturralde E, Ghadiali M, Young-Wolff KC, Campbell CI, Leibowitz AS, et al. Treatment for anxiety and Substance Use Disorders during the COVID-19 pandemic: Challenges and strategies. J Addict Med. 2020;14(6):e293–e6. doi: 10.1097/ADM.0000000000000755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Mental Health and COVID-19: Early evidence of the pandemic’s impact. 2022. WHO/2019-nCoV/Sci_Brief/Mental_health/2022.1. Accessed April 26, 2022. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1
- 8.National Institute on Drug Abuse. COVID-19 & Substance Use. 2022 [updated February 25, 2022. Accessed April 26, 2022. Available from: https://nida.nih.gov/drug-topics/comorbidity/covid-19-substance-use
- 9.Kuman Tunçel Ö, Pullukçu H, Erdem HA, Kurtaran B, Taşbakan SE, Taşbakan M. COVID-19-related anxiety in people living with HIV: an online cross-sectional study. Turk J Med Sci. 2020;50(8):1792–800. doi: 10.3906/sag-2006-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parisi CE, Varma DS, Wang Y, Vaddiparti K, Ibañez GE, Cruz L, et al. Changes in Mental Health among People with HIV during the COVID-19 pandemic: qualitative and quantitative perspectives. AIDS Behav. 2022;26(6):1980–91. doi: 10.1007/s10461-021-03547-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carrico AW, Horvath KJ, Grov C, Moskowitz JT, Pahwa S, Pallikkuth S, et al. Double Jeopardy: Methamphetamine Use and HIV as Risk factors for COVID-19. AIDS Behav. 2020;24(11):3020–3. doi: 10.1007/s10461-020-02854-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochstatter KR, Akhtar WZ, Dietz S, Pe-Romashko K, Gustafson DH, Shah DV, et al. Potential influences of the COVID-19 pandemic on Drug Use and HIV Care among People living with HIV and Substance Use Disorders: experience from a pilot mHealth intervention. AIDS Behav. 2021;25(2):354–9. doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hong C, Queiroz A, Hoskin J. The impact of the COVID-19 pandemic on mental health, associated factors and coping strategies in people living with HIV: a scoping review. J Int AIDS Soc. 2023;26(3):e26060. doi: 10.1002/jia2.26060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Javanbakht M, Rosen A, Ragsdale A, Richter EI, Shoptaw S, Gorbach PM. Interruptions in Mental Health Care, Cannabis Use, Depression, and anxiety during the COVID-19 pandemic: findings from a cohort of HIV-Positive and HIV-Negative MSM in Los Angeles, California. J Urban Health. 2022;99(2):305–15. doi: 10.1007/s11524-022-00607-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meanley S, Choi SK, Thompson AB, Meyers JL, D’Souza G, Adimora AA, et al. Short-term binge drinking, marijuana, and recreational drug use trajectories in a prospective cohort of people living with HIV at the start of COVID-19 mitigation efforts in the United States. Drug Alcohol Depend. 2022;231:109233. doi: 10.1016/j.drugalcdep.2021.109233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pytell JD, Shen NM, Keruly JC, Lesko CR, Lau B, Fojo AT, et al. The relationship of alcohol and other drug use during the COVID-19 pandemic among people with or at risk of HIV; a cross-sectional survey of people enrolled in collaborating Consortium of cohorts producing NIDA Opportunities (C3PNO) cohorts. Drug Alcohol Depend. 2022;241:109382. doi: 10.1016/j.drugalcdep.2022.109382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satre DD, Anderson AN, Leibowitz AS, Levine-Hall T, Slome S, Flamm J, et al. Implementing electronic substance use disorder and depression and anxiety screening and behavioral interventions in primary care clinics serving people with HIV: protocol for the promoting Access to Care Engagement (PACE) trial. Contemp Clin Trials. 2019;84:105833. doi: 10.1016/j.cct.2019.105833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McNeely J, Adam A, Rotrosen J, Wakeman SE, Wilens TE, Kannry J, et al. Comparison of methods for Alcohol and Drug Screening in Primary Care clinics. JAMA Netw Open. 2021;4(5):e2110721. doi: 10.1001/jamanetworkopen.2021.10721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Spangenberg L, Glaesmer H, Boecker M, Forkmann T. Differences in Patient Health Questionnaire and Aachen Depression Item Bank scores between tablet versus paper-and-pencil administration. Qual Life Res. 2015;24(12):3023–32. doi: 10.1007/s11136-015-1040-5. [DOI] [PubMed] [Google Scholar]
- 22.McNeely J, Wu LT, Subramaniam G, Sharma G, Cathers LA, Svikis D, et al. Performance of the Tobacco, Alcohol, prescription medication, and other Substance Use (TAPS) Tool for Substance Use Screening in Primary Care Patients. Ann Intern Med. 2016;165(10):690–9. doi: 10.7326/M16-0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 24.Luborsky M. The identification and analysis of themes and patterns. In: Gubrium JF, Sankar A, editors. Qualitative methods in Aging Research. New York, NY: Sage; 1994. pp. 189–210. [Google Scholar]
- 25.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 26.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 27.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and Content of Primary Care Office-Based vs Telemedicine Care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friedman EE, Devlin SA, Gilson SF, Ridgway JP. Age and racial disparities in Telehealth Use among People with HIV during the COVID-19 pandemic. AIDS Behav. 2022;26(8):2686–91. doi: 10.1007/s10461-022-03607-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGinnis KA, Skanderson M, Justice AC, Akgün KM, Tate JP, King JT, Jr, et al. HIV care using differentiated service delivery during the COVID-19 pandemic: a nationwide cohort study in the US Department of Veterans Affairs. J Int AIDS Soc. 2021;24(Suppl 6):e25810. doi: 10.1002/jia2.25810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dandachi D, Dang BN, Lucari B, Teti M, Giordano TP. Exploring the attitude of patients with HIV about using Telehealth for HIV Care. AIDS Patient Care STDS. 2020;34(4):166–72. doi: 10.1089/apc.2019.0261. [DOI] [PubMed] [Google Scholar]
- 31.Budak JZ, Scott JD, Dhanireddy S, Wood BR. The impact of COVID-19 on HIV Care provided via Telemedicine-Past, Present, and Future. Curr HIV/AIDS Rep. 2021;18(2):98–104. doi: 10.1007/s11904-021-00543-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee KW, Ang CS, Lim SH, Siau CS, Ong LTD, Ching SM, et al. Prevalence of mental health conditions among people living with HIV during the COVID-19 pandemic: a rapid systematic review and meta-analysis. HIV Med. 2022;23(9):990–1001. doi: 10.1111/hiv.13299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pizzirusso M, Carrion-Park C, Clark US, Gonzalez J, Byrd D, Morgello S. Physical and Mental Health Screening in a New York City HIV Cohort during the COVID-19 pandemic: a preliminary Report. J Acquir Immune Defic Syndr. 2021;86(3):e54–e60. doi: 10.1097/QAI.0000000000002564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pantelic M, Martin K, Fitzpatrick C, Nixon E, Tweed M, Spice W, et al. I have the strength to get through this using my past experiences with HIV”: findings from a mixed-method survey of health outcomes, service accessibility, and psychosocial wellbeing among people living with HIV during the Covid-19 pandemic. AIDS Care. 2022;34(7):821–7. doi: 10.1080/09540121.2021.1975628. [DOI] [PubMed] [Google Scholar]
- 35.Diaz-Martinez J, Tamargo JA, Delgado-Enciso I, Liu Q, Acuña L, Laverde E, et al. Resilience, anxiety, stress, and substance use patterns during COVID-19 pandemic in the Miami Adult Studies on HIV (MASH) Cohort. AIDS Behav. 2021;25(11):3658–68. doi: 10.1007/s10461-021-03292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tamargo JA, Martin HR, Diaz-Martinez J, Trepka MJ, Delgado-Enciso I, Johnson A, et al. COVID-19 testing and the impact of the pandemic on the Miami Adult Studies on HIV Cohort. J Acquir Immune Defic Syndr. 2021;87(4):1016–23. doi: 10.1097/QAI.0000000000002680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hormes JM, Gerhardstein KR, Griffin PT. Under-reporting of alcohol and substance use versus other psychiatric symptoms in individuals living with HIV. AIDS Care. 2012;24(4):420–3. doi: 10.1080/09540121.2011.608795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS–a systematic review. Alcohol Alcohol. 2010;45(2):159–66. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- 39.Substance Abuse and Mental Health Services Administration ahd Helath Resources and Services Administration . The case for behavioral health screening in HIV Care Settings. HHS publication no SMA-16-4999. Rockville, MD: substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.