Abstract
Objective
Antithrombotic therapy is essential for patients with atrial fibrillation (AF) and stable coronary artery disease (CAD) because of the high risk of thrombosis, whereas a combination of antiplatelets and anticoagulants is associated with a high risk of bleeding. We sought to develop and validate a machine-learning-based model to predict future adverse events.
Methods
Data from 2215 patients with AF and stable CAD enrolled in the Atrial Fibrillation and Ischaemic Events With Rivaroxaban in Patients With Stable Coronary Artery Disease trial were randomly assigned to the development and validation cohorts. Using the random survival forest (RSF) and Cox regression models, risk scores were developed for net adverse clinical events (NACE) defined as all-cause death, myocardial infarction, stroke or major bleeding.
Results
Using variables selected by the Boruta algorithm, RSF and Cox models demonstrated acceptable discrimination and calibration in the validation cohort. Using the variables weighted by HR (age, sex, body mass index, systolic blood pressure, alcohol consumption, creatinine clearance, heart failure, diabetes, antiplatelet use and AF type), an integer-based risk score for NACE was developed and classified patients into three risk groups: low (0–4 points), intermediate (5–8) and high (≥9). In both cohorts, the integer-based risk score performed well, with acceptable discrimination (area under the curve 0.70 and 0.66, respectively) and calibration (p>0.40 for both). Decision curve analysis showed the superior net benefits of the risk score.
Conclusions
This risk score can predict the risk of NACE in patients with AF and stable CAD.
Trial registration numbers
UMIN000016612, NCT02642419.
Keywords: atrial fibrillation, coronary artery disease, risk factors
WHAT IS ALREADY KNOWN ON THIS TOPIC
A combination of antiplatelet and anticoagulant agents has been an essential antithrombotic therapy for patients suffering from atrial fibrillation (AF) and coronary artery disease (CAD); however, the persistent issue of bleeding complications associated with antithrombotic therapy remains a concern.
WHAT THIS STUDY ADDS
This subanalysis of the Atrial Fibrillation and Ischaemic Events With Rivaroxaban trial developed a machine-learning-based risk prediction model for net adverse clinical events in patients with AF and CAD.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Managing the risk of both thromboembolic and bleeding events is crucial in the antithrombotic treatment of those patients. Using this risk score can prove beneficial in the decision-making process in clinical settings.
Introduction
Antiplatelet therapy is required for the secondary prevention of cardiovascular events in patients with coronary artery disease (CAD),1–3 and anticoagulant therapy is essential for the prevention of thromboembolic events in patients with atrial fibrillation (AF).4–6 A combination of antiplatelet and anticoagulant agents has been used in patients with AF and CAD; however, the high risk of antithrombotic therapy-related bleeding complications remains a problem. The AFIRE trial (Atrial Fibrillation and Ischaemic Events with Rivaroxaban in Patients with Stable Coronary Artery Disease) showed that rivaroxaban monotherapy was non-inferior in at reducing the risk of cardiovascular events or all-cause death and superior in at reducing the risk of major bleeding compared with a combination of rivaroxaban with a single antiplatelet drug in AF patients with stable CAD at ≥1 year after revascularisation or those with angiographically confirmed CAD not requiring revascularisation.7
Simple conventional risk scores, such as the CHADS2,8 CHA2DS2-VASc9 or HAS-BLED10 scores, have been widely used to estimate the individual risk of thromboembolic or bleeding events in patients with AF. In addition, the CHADS2 score is a useful prediction tool for cardiovascular or cerebrovascular events, even in CAD patients without AF.11 12 However, subanalysis of the AFIRE trial demonstrated that patients with major bleeding had a high risk of subsequent major adverse cardiac and cerebrovascular events, especially within 30 days after major bleeding,13 suggesting that a balanced risk assessment should be established to estimate the integrated risk of both thromboembolic and bleeding events in patients with AF and CAD.
To address this challenging issue, we conducted a post hoc analysis of the AFIRE trial to develop and validate a machine-learning-based risk prediction model for future net adverse clinical events (NACE) among patients with AF and stable CAD.
Methods
Study design and study participants
This study was a post hoc analysis of the AFIRE trial, a multicentre, randomised, open-label, parallel-group trial. The detailed study design, protocol, and results of the primary analysis of the AFIRE trial have been reported previously.7 14 Briefly, the AFIRE trial was conducted in 294 hospitals across Japan between 23 February 2015 and 30 September 2017 and included patients aged ≥20 years, diagnosed with AF with a CHADS2 score ≥1 and stable CAD at ≥1 year after revascularisation or those with angiographically confirmed CAD not requiring revascularisation. Patients with a history of stent thrombosis, coexisting active cancer or poorly controlled hypertension were excluded in the trial. Patients were randomised in a 1:1 ratio to receive either rivaroxaban (10 mg once daily for patients with a creatinine clearance rate (CCR) of 15–49 mL/min or 15 mg once daily for patients with a CCR≥50 mL/min) alone or rivaroxaban plus an antiplatelet drug (either aspirin or P2Y12 inhibitor). Patient follow-up was performed at baseline, 6 months and at the end of the trial, with additional follow-up for routine clinical care if needed. The study follow-up period was at least 24 months and up to 45 months.
The data were reviewed by an independent data and safety monitoring committee. In this post hoc analysis, 2215 patients in the modified intention-to-treat population from the AFIRE trial were analysed.
Outcome
The primary outcome of this study was NACE, consisting of all-cause death, myocardial infarction, stroke or major bleeding according to the criteria of the International Society on Thrombosis and Haemostasis.15
Candidate variables
After excluding of variables with >10% missing values and a correlation coefficient >0.7, 78 candidate variables at baseline were used to develop the risk prediction model as potential predictors of NACE (online supplemental table 1). Missing values were imputed by missForest,16 which is a non-parametric imputation method using a random forest model that can learn non-linearity, easily handle mixed-type data and calculate out-of-bag errors.
openhrt-2023-002292supp001.pdf (2.2MB, pdf)
Statistical analysis
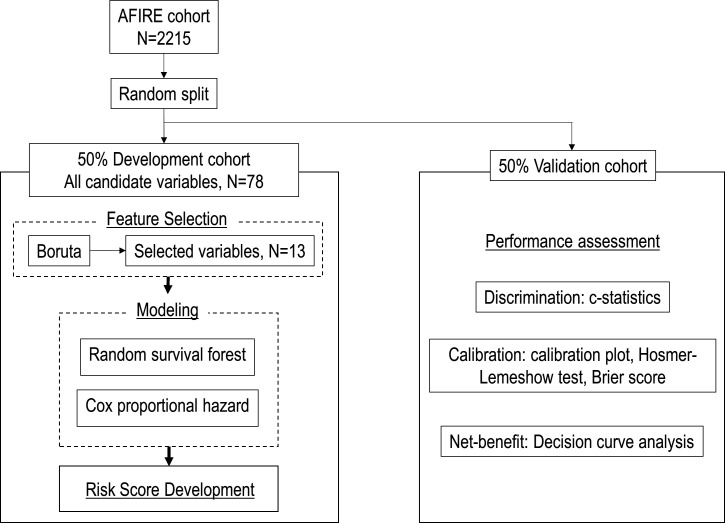
Based on the outcome, study participants were randomly assigned to a development (50%) or validation (50%) dataset. The development dataset was further divided into two (a training or tuning set, each 50%) to tune the hyperparameters. Categorical variables are presented as frequencies and percentages, and continuous variables are presented as medians and IQR. Using only data from the development dataset, feature selection and relationship modelling for risk prediction model development were conducted (figure 1).
Figure 1.
Study flow chart. Study design for the development and validation of the machine learning-based risk score model. AFIRE, Atrial Fibrillation and Ischaemic Events With Rivaroxaban.
Feature selection
From all candidate variables, we further identified 13 predictors (age, sex, treatment randomisation, body mass index (BMI), systolic blood pressure, diastolic blood pressure, CCR, type of AF, alcohol consumption, diabetes mellitus, heart failure, prior stent implantation and prior coronary artery bypass grafting) using a feature selection method with the Boruta algorithm, which is a wrapper around a random forest classification algorithm that can provide a numerical estimate of the feature importance without tuning the parameters and removing the variables that are less relevant than random probes by a statistical test.17
Model development and evaluation
The relationships between the outcomes and variables selected by the Boruta algorithm were assessed using Cox proportional hazard (PH) models and random survival forest (RSF) models,18 which is an ensemble tree-based classification method for the analysis of right-censored survival data. Each model was assessed based on Harrell’s concordance index (C-index) for discrimination performance and the Brier score for both discrimination and calibration performance in the development and validation datasets.
Risk score development and validation
For clinical use, a simple integer-based risk score to predict the outcome was developed based on each variable’s unadjusted HR, with statistical significance calculated from the Cox PH model in the development dataset. Continuous variables were categorised as follows: age (≥80 years, <80 years), BMI (<18.5, 18.5–25, ≥25), systolic blood pressure (<90, 90–140, ≥140), diastolic blood pressure (<60, 60–90, ≥90) and CCR (<30, 30–50, ≥50). The discrimination performance of the integer-based risk score was assessed using the area under the receiver operating characteristic curve (AUC-ROC) and its 95% CIs in the development and validation datasets. The calibration performance of the risk score was assessed using a calibration plot and Hosmer-Lemeshow test. Performance comparison of the new risk score with that of conventional risk scores, such as the CHADS2 (Congestive heart failure, Hypertension, Age ≥75 y, Diabetes mellitus, Stroke or TIA), CHA2DS2-VASc (Congestive heart failure, Hypertension, Age ≥75 y, Diabetes mellitus, Stroke or TIA, Vascular disease, Age 65-74 y, Sex category [female]) and HAS-BLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding, Labile INR, Elderly, Drugs) scores, was performed using ROC analysis, category and category-free net reclassification improvement, integrated discrimination improvement and decision curve analysis to indicate net benefit and clinical utility.19–21
Statistical analyses were performed using SPSS (V.23.0; IBM), R software, V.4.0.5 (The R Project for Statistical Computing) and Python (V.3.7.11, Python Software Foundation). Statistical significance was defined as a two-sided p<0.05.
Results
Study participants
Among the 2215 patients in the AFIRE trial, 1107 were included in the development cohort (median (IQR) age, 75 (69–80) years; 870 (78.6%) males) and 1108 in the validation cohort (median (IQR) age, 75 (69, 80) years; 881 (79.5%) males). During a median (IQR) follow-up of 24.1 (17.3–31.5) months, 215 patients (9.7%) suffered NACE (107 and 108 in the development and validation cohorts, respectively). Patient characteristics for the development and validation cohorts are presented in table 1. There were no statistical differences in demographic and physiological findings, antithrombotic regimen, type of AF, comorbidities, medical history, or prior revascularisation between the cohorts, except for the location of the culprit lesion, interventions other than revascularisation and prior bleeding complications.
Table 1.
Clinical characteristics
| Variables | Development cohort N=1107 |
Validation cohort N=1108 |
P value |
| Age, years | 75 (69, 80) | 75 (69, 80) | 0.723 |
| Male | 870 (78.6) | 881 (79.5) | 0.594 |
| BMI, kg/m2 | 24.2 (22.2, 26.6) | 24.2 (22.2, 26.5) | 0.782 |
| Systolic BP, mm Hg | 126 (116, 136) | 126 (116, 135) | 0.722 |
| Diastolic BP, mm Hg | 70 (64, 78) | 71 (64, 80) | 0.350 |
| Current smoker | 149 (13.5) | 143 (12.9) | 0.700 |
| Alcohol consumption | 0.369 | ||
| Daily | 202 (18.2) | 221 (19.9) | |
| Occasionally | 361 (32.6) | 374 (33.8) | |
| None | 544 (49.1) | 513 (46.3) | |
| Rivaroxaban monotherapy | 549 (49.6) | 558 (50.4) | 0.718 |
| Dose of rivaroxaban | 0.459 | ||
| 10 mg/day | 509 (46.0) | 501 (45.2) | |
| 15 mg/day | 588 (53.1) | 596 (53.8) | |
| Other | 2 (0.2) | 0 (0.0) | |
| Unknown | 8 (0.7) | 11 (1.0) | |
| Type of atrial fibrillation | 0.337 | ||
| Paroxysmal | 571 (51.6) | 605 (54.6) | |
| Persistent | 172 (15.5) | 167 (15.1) | |
| Permanent | 364 (32.9) | 336 (30.3) | |
| Hypertension | 955 (86.3) | 936 (84.5) | 0.233 |
| Diabetes mellitus | 460 (41.6) | 467 (42.1) | 0.777 |
| Dyslipidaemia | 774 (69.9) | 764 (69.0) | 0.622 |
| Angina pectoris | 714 (64.5) | 696 (62.8) | 0.410 |
| Heart failure | 398 (36.0) | 390 (35.2) | 0.711 |
| Liver dysfunction | 19 (1.7) | 22 (2.0) | 0.638 |
| Creatinine clearance | 59.8 (45.7, 75.0) | 58.7 (44.8, 74.0) | 0.322 |
| Haemorrhagic diathesis | 17 (1.5) | 15 (1.4) | 0.720 |
| Prior stroke | 158 (14.3) | 165 (14.9) | 0.680 |
| Transient ischaemic attack | 23 (2.1) | 25 (2.3) | 0.773 |
| Prior myocardial infarction | 381 (34.4) | 396 (35.7) | 0.514 |
| Prior PCI | 779 (70.4) | 785 (70.8) | 0.805 |
| Stent implantation | 718 (64.9) | 726 (65.5) | 0.743 |
| Type of stent | 0.802 | ||
| Drug-eluting | 480/718 (66.9) | 497/726 (68.5) | |
| Bare-metal | 179/718 (24.9) | 163/726 (22.5) | |
| Both types | 27/718 (3.8) | 28/726 (3.9) | |
| Unknown | 32/718 (4.5) | 38/726 (5.2) | |
| Cipher | 86/718 (12.0) | 88/726 (12.1) | |
| TAXUS | 32/718 (4.5) | 23/726 (3.2) | |
| Endeavour | 23/718 (3.2) | 29/726 (4.0) | |
| Xience | 187/718 (26.0) | 201/726 (27.7) | |
| Promus | 103/718 (14.3) | 112/726 (15.4) | |
| Nobori | 46/718 (6.4) | 38/726 (5.2) | |
| Other | 67/718 (9.3) | 97/726 (13.4) | |
| Prior CABG | 128 (11.6) | 124 (11.2) | 0.783 |
| Location of culprit lesion | |||
| Segment #1 | 113 (10.2) | 127 (11.5) | 0.342 |
| Segment #2 | 134 (12.1) | 123 (11.1) | 0.461 |
| Segment #3 | 111 (10.0) | 106 (9.6) | 0.716 |
| Segment #4PD | 20 (1.8) | 33 (3.0) | 0.071 |
| Segment #4AV | 24 (2.2) | 36 (3.2) | 0.117 |
| Segment #5 | 15 (1.4) | 31 (2.8) | 0.017 |
| Segment #6 | 251 (22.7) | 258 (23.3) | 0.732 |
| Segment #7 | 253 (22.9) | 298 (26.9) | 0.028 |
| Segment #8 | 17 (1.5) | 34 (3.1) | 0.016 |
| Segment #9 | 43 (3.9) | 37 (3.3) | 0.492 |
| Segment #10 | 2 (0.2) | 4 (0.4) | 0.687 |
| Segment #11 | 77 (7.0) | 71 (6.4) | 0.606 |
| Segment #12 | 44 (4.0) | 29 (2.6) | 0.074 |
| Segment #13 | 117 (10.6) | 125 (11.3) | 0.591 |
| Segment #14 | 34 (3.1) | 34 (3.1) | 0.997 |
| Segment #15 | 15 (1.4) | 10 (0.9) | 0.313 |
| Interventions other than PCI or CABG | 120 (10.8) | 158 (14.3) | 0.015 |
| Prior aortic aneurysm | 46 (4.2) | 30 (2.7) | 0.061 |
| Systemic embolism | 5 (0.6) | 6 (0.5) | 0.764 |
| Deep venous thrombosis | 8 (0.7) | 6 (0.5) | 0.591 |
| Pulmonary embolism | 3 (0.3) | 5 (0.5) | 0.726 |
| Peripheral artery disease | 70 (6.3) | 69 (6.2) | 0.926 |
| Other ischaemic disorder | 87 (7.9) | 104 (9.4) | 0.200 |
| Prior bleeding complication | 37 (3.3) | 22 (2.0) | 0.047 |
| Proton pomp inhibitor | 670 (60.5) | 687 (62.0) | 0.475 |
| NSAIDs | 29 (2.6) | 16 (1.4) | 0.050 |
Data are presented as n (%) or median (IQR).
AV, atrioventricular branch; BMI, body mass index; BP, blood pressure; CABG, coronary artery bypass grafting; NSAIDs, nonsteroidal anti-inflammatory drugs; PCI, percutaneous coronary intervention; PD, posterior descending branch.
Performance of development models and integer-based risk score
The 13 Boruta algorithm-selected variables had high C-index of 0.706 and 0.667 in the development and validation cohorts, respectively, when used with the RSF model (online supplemental table 2). Using the same variables as the Cox PH model, the discrimination performance was acceptable (C-index of 0.680 and 0.650 in the development and validation cohorts, respectively). The RSF model had low Brier scores of 0.081 and 0.080 in the development and validation cohorts, respectively (online supplemental table 2), indicating good calibration. Similarly, the Cox PH model had low Brier scores of 0.079 and 0.081 in the development and validation cohorts, respectively.
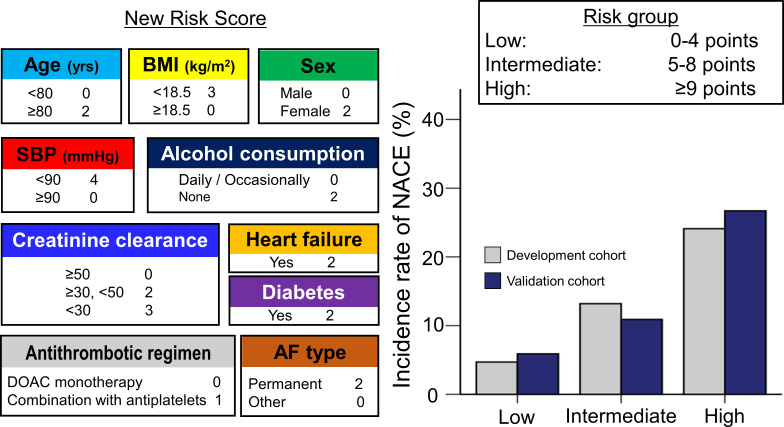
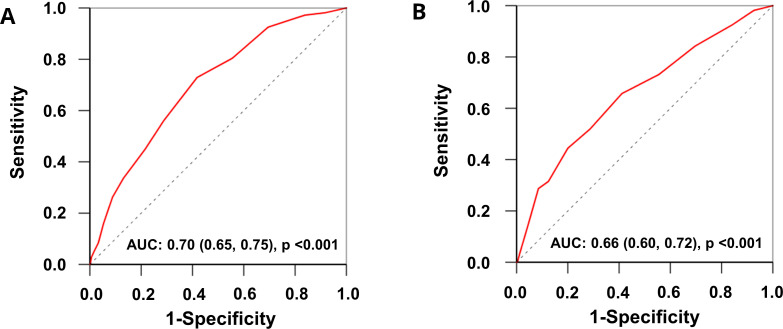
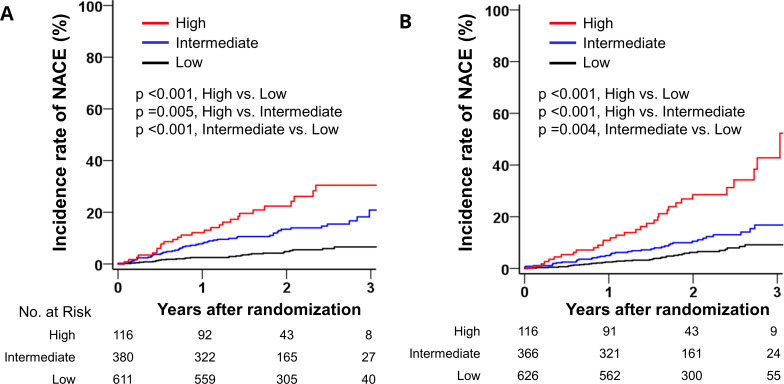
The β-coefficients, HRs and 95% CIs for each of the selected variables calculated using the Cox PH model are presented in table 2. Using the variables with statistical significance, an integer-based risk score for NACE was created (figure 2); according to each variable’s HR, a score for the risk of NACE was assigned (table 2). The new risk score model has a theoretical range of 0–23 and is divided into three risk groups: low (0–4 points), intermediate (5–8 points) and high (≥9 points). The new risk score model demonstrated good discrimination with a C-index of 0.70 (95% CI 0.65 to 0.75; figure 3A) and acceptable calibration (Hosmer-Lemeshow test; χ2 of 7.789, p=0.454; online supplemental figure 1a). The cumulative 3-year incidence of NACE increased in a graded fashion across the risk groups in the development cohort (figure 4A).
Table 2.
Cox proportional hazard parameter estimates and assigned score for the risk of NACE
| Variables | β-estimate | HR (95% CI) | P value | Score |
| Age, years | 0.044 | 1.05 (1.02 to 1.07) | 0.001 | |
| Elderly (age ≥80 years) | 0.706 | 2.03 (1.37 to 3.00) | <0.001 | 2 |
| Female | 0.488 | 1.63 (1.08 to 2.46) | 0.020 | 2 |
| Combination with antiplatelet agents | 0.392 | 1.48 (1.00 to 2.18) | 0.047 | 1 |
| BMI, kg/m2 | −0.068 | 0.93 (0.88 to 0.99) | 0.020 | |
| <18.5 | 1.062 | 2.89 (1.43 to 5.83) | 0.003 | 3 |
| ≥18.5, <25 | Ref | Ref | Ref | |
| ≥25 | −0.083 | 0.92 (0.61 to 1.38) | 0.690 | |
| Systolic BP, mm Hg | −0.013 | 0.99 (0.98 to 1.00) | 0.042 | |
| <90 | 1.540 | 4.66 (1.71 to 12.7) | 0.003 | 4 |
| ≥90, <140 | Ref | Ref | Ref | |
| ≥140 | −0.043 | 0.96 (0.58 to 1.58) | 0.865 | |
| Diastolic BP, mm Hg | −0.010 | 0.99 (0.97 to 1.01) | 0.227 | |
| <60 | 0.191 | 1.21 (0.73 to 2.02) | 0.465 | |
| ≥60, <90 | Ref | Ref | Ref | |
| ≥90 | −0.497 | 0.61 (0.22 to 1.66) | 0.332 | |
| Type of atrial fibrillation | ||||
| Paroxysmal | Ref | Ref | Ref | |
| Persistent | −0.035 | 0.97 (0.52 to 1.79) | 0.912 | |
| Permanent | 0.469 | 1.60 (1.07 to 2.40) | 0.023 | 2 |
| No alcohol consumption | 0.500 | 1.65 (1.04 to 2.62) | 0.035 | 2 |
| Diabetes mellitus | 0.416 | 1.52 (1.04 to 2.22) | 0.032 | 2 |
| Heart failure | 0.556 | 1.74 (1.19 to 2.55) | 0.004 | 2 |
| Prior stent implantation | 0.226 | 1.25 (0.84 to 1.88) | 0.273 | |
| Prior CABG | −0.632 | 0.53 (0.25 to 1.14) | 0.106 | |
| Creatinine clearance | −0.018 | 0.98 (0.97 to 0.99) | <0.001 | |
| ≥50 | Ref | Ref | Ref | |
| ≥30, <50 | 0.612 | 1.84 (1.23 to 2.78) | 0.003 | 2 |
| <30 | 1.150 | 3.16 (1.67 to 5.96) | <0.001 | 3 |
BMI, body mass index; BP, blood pressure; CABG, coronary artery bypass grafting; NACE, net adverse clinical event.
Figure 2.
The machine learning-based New Risk Score for NACE incidence and the three risk groups. The bar graph shows the incidence rate of NACE among the three risk groups in the development and validation cohorts. AF, atrial fibrillation; BMI, body mass index; DOAC, direct oral anticoagulant; NACE, net adverse clinical event; SBP, systolic blood pressure.
Figure 3.
The ROC curves for the machine learning-based risk score for predicting NACE incidence. The AUC (95% CI) of the risk score in the (A) development and (B) validation cohorts is shown. AUC, area under the curve; NACE, net adverse clinical events; ROC, receiver operating curve.
Figure 4.
Kaplan-Meier curves of NACE according to the three risk groups. Patients with AF and stable CAD were stratified into three risk groups according to their risk score for NACE. Kaplan-Meier curves show the cumulative incidence of NACE among the three risk groups in the (A) development and (B) validation cohorts. AF, atrial fibrillation; CAD, coronary artery disease; NACE, net adverse clinical event.
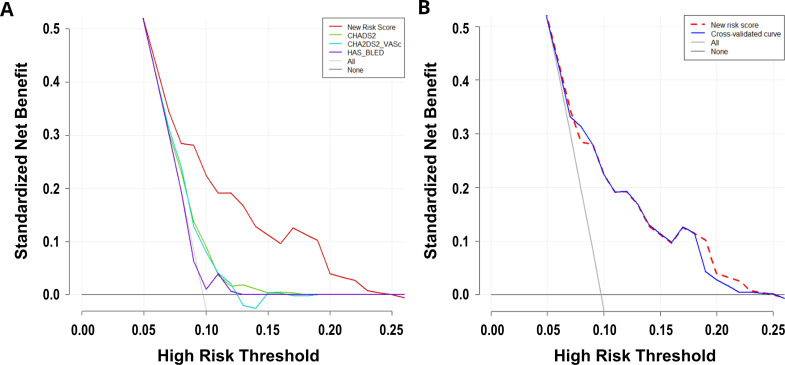
Validation and decision curve analysis of the integer-based risk score
In the validation cohort, the AUC of the new risk score was 0.66 (95% CI 0.60, 0.72; figure 3B) and the Hosmer-Lemeshow goodness-of-fit χ2 was 3.417 (p=0.906; online supplemental figure 1), indicating moderate discrimination and acceptable calibration, respectively. The cumulative 3-year incidence of NACE also increased in a graded fashion across the three risk groups in the validation cohort (figure 4B). The AUC of conventional risk scores such as the CHADS2, CHA2DS2-VASc and HAS-BLED scores were 0.57 (95% CI 0.51 to 0.62), 0.57 (95% CI 0.51 to 0.62) and 0.51 (95% CI 0.46 to 0.57), respectively (online supplemental figure 2). Compared with these conventional risk scores, the discrimination performance of the new risk score was significantly higher (online supplemental figure 2 and online supplemental table 3). The decision curves for the new and conventional risk scores for predicting NACE in the validation cohort are shown in figure 5A. The new risk score had a greater net benefit, with threshold probabilities of 5%–25% than the conventional risk scores. A 10-fold cross-validated decision curve of the new risk score showed a similar standardised net benefit at each threshold probability (figure 5B), indicating the robustness of the results.
Figure 5.
Decision curves for the new and conventional risk scores. (A) Decision curves for the new and conventional (CHADS2, CHA2DS2-VASc and HAS-BLED scores) risk scores to predict NACE incidence in patients with AF and stable CAD. (B) A 10-fold cross-validated decision curve for the new risk score to obtain a bias-corrected decision curve. AF, atrial fibrillation; CAD, coronary artery disease; NACE, net adverse clinical event; CHADS2, Congestive heart failure, Hypertension, Age ≥75 y, Diabetes mellitus, Stroke or TIA; CHA2DS2-VASc, Congestive heart failure, Hypertension, Age ≥75 y, Diabetes mellitus, Stroke or TIA, Vascular disease, Age 65-74 y, Sex category [female]; HAS-BLED, Hypertension, Abnormal renal/liver function, Stroke, Bleeding, Labile INR, Elderly, Drugs.
Discussion
This post hoc analysis of the AFIRE trial demonstrated the development and validation of a machine-learning-based risk score that integrated easily available clinical and laboratory data to predict future adverse clinical events in patients with AF and stable CAD. Patients in the high-risk group had a 3-year NACE risk of approximately 40%. This risk score substantially improved the discriminatory ability and clinical usefulness of adverse clinical events compared with conventional risk scores. Antithrombotic therapy is needed for patients with AF and stable CAD because of the high risk of ischaemic and thrombotic events, whereas a combination of antiplatelet therapy with anticoagulants is associated with a high risk of bleeding events. Given this clinically unresolvable dilemma, this machine learning-based risk score is comprehensive, easily available and clinically useful for predicting future adverse events. Based on this risk score, clinicians should reconsider patient management, and close follow-up and cardiovascular healthcare should be provided to high-risk patients.
Machine learning has advantages in prediction model development compared with traditional statistical methods that focus on inference and do not require a prior assumption of causality in variable selection and modelling. Many machine-learning-based risk prediction models have been reported for the diagnosis and prognosis of patients with CAD22–25 or AF,26–28 whereas there has only been one previous report of a machine learning-based prediction model for CAD patients complicated with AF.29 However, only one report showed a machine-learning prediction model for all-cause death among these patients. No established machine-learning-based risk score has been reported for the prediction of NACE combining thromboembolic events with bleeding events; therefore, this was the first study to develop a machine-learning-based risk prediction score for NACE with internal validation. In this study, we used the Boruta algorithm for variable selection and an RSF model in the development process of the prediction model, as well as the traditional Cox PH model for modelling and scoring. The Boruta algorithm is a novel feature selection algorithm to identify all relevant variables for outcomes and a wrapper built around a random forest classification algorithm, which can be performed quickly without tuning the parameters and provides a numerical estimate of feature importance.17 RSF is a random forest method for the analysis of right-censored survival data18 and can mathematically build binary recursive trees for all samples and obtain the maximal survival difference across daughter nodes with the application of bootstrap methods and the log-rank splitting rule.30 31 Although traditional statistical methods for survival data, such as the Cox PH model, rely on restrictive assumptions such as PHs, machine-learning-based methods can manage large multidimensional datasets of right-censored survival data without the need for assumptions of parametric distributions, interaction between variables, linear relationships with outcome and overfitting of models. Therefore, to avoid these mathematical issues, machine-learning approaches may be able to predict complex clinical outcomes such as NACE more accurately. Moreover, the integer-based risk score created in this study would be easy to use in clinical practice because it does not require nesting on a web-based platform or electronic medical record.
In patients with AF, the CHADS2 8 and CHA2DS2-VASc scores9 have been established as risk scores for thromboembolic events and the HAS-BLED score10 as the risk score for major bleeding events. However, this study showed that these conventional risk scores did not have a good predictive performance for NACE in patients with AF and stable CAD. Here, we developed and validated a machine learning-based risk score for NACE in these patients, and the risk score had modest discrimination and good calibration with good reclassification improvement compared with conventional risk scores. One of the responsible factors may be that the variable selection of the integer-based risk score was conducted by combining machine learning (Boruta algorithm) and classical statistical (Cox PH) methods. The variables selected for the risk score in this study, such as older age, low BMI, female sex, CCR, heart failure, diabetes and combination with antiplatelets, were included in other traditional risk scores for the assessment of thrombotic and bleeding events.10 32 33 Although most variables selected for the risk score can be interpreted and may be useful in understanding the underlying mechanism of clinical adverse events in patients with AF and stable CAD, the association between no alcohol consumption and high risk of NACE may be difficult to interpret. However, this can be explained by the following mechanism: among patients who do not have a drinking habit, some patients cannot consume alcohol because of decreased aldehyde dehydrogenase 2 (ALDH2) activity due to the ALDH2-deficient variant, which presents as alcohol flushing syndrome and is more common in East Asians than in other ethnic populations.34–37 The ALDH2-deficient variant is a risk factor for ischaemic heart diseases, such as coronary spasms38 and acute myocardial infarction.39 40 Based on these findings, alcohol consumption may have been selected as a candidate risk prediction score for NACE in this study. This machine-learning-based risk score is easy to use because it is based on information that is easily available in clinical settings and does not require testing results or information that is difficult to obtain.
This study had several limitations. First, the study population was Japanese and received a rivaroxaban dose of 10 or 15 mg once daily approved by Japan, rather than the once-daily dose of 20 mg approved globally, which may have caused selection bias. Additionally, because the study population included only patients who met the eligibility criteria of the AFIRE trial, we did not verify that the results of this study are applicable to patients in a real-world setting. To confirm generalisability, the risk score should be validated in other ethnic populations or settings. Second, because relevant information, such as haemoglobin,33 platelet count,33 complex percutaneous coronary intervention41 and control of chronic disease (diabetes mellitus and dyslipidaemia), was not captured in the AFIRE trial, the information was not included in the variable selection. Third, although discontinuation of antithrombotic therapy is a risk factor for thrombotic events, data for antithrombotic therapy adherence were not collected in the AFIRE trial and lack of data may have affected the results of this study.
In conclusion, this post hoc analysis of the AFIRE trial demonstrated the development and validation of a machine learning-based risk score that can predict future adverse clinical events in patients with AF and stable CAD. It is important to balance the risk of both thromboembolic and bleeding events in the antithrombotic management of these patients, and the application of this risk score can be useful for decision-making in clinical settings.
Footnotes
Twitter: @MasanobuIshii
Contributors: All authors have contributed to this manuscript. MI, EN and SN performed the statistical analysis. HO, KoK and SY handled funding and supervision. KoK, SY, MA, JA, TM, MN, KaM, NH, KaK, AH, KuM and HO acquired the data. KoK, SY, MA, JA, TM, MN, KaM, NH, KaK, AH, KuM and HO conceived and designed the study. MI drafted the manuscript. KoK and KT made critical revisions of the manuscript for key intellectual content. KoK accpets full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This work was supported by the Japan Cardiovascular Research Foundation based on a contract with Bayer Yakuhin.
Competing interests: KoK reports remuneration for lectures from Bayer Yakuhin, Daiichi-Sankyo, Novartis Pharma AG and Otsuka Pharmaceutical; has received trust research/joint research funds from Bayer Yakuhin, and Daiichi-Sankyo; and has received scholarship funds from Abbott Medical. SY reports grants from Takeda Pharmaceutical, Abbott and Boston Scientific, and personal fees from Daiichi-Sankyo and Bristol Myers Squibb. MA reports grants from the Japan Agency for Medical Research and Development; personal fees from Bristol Myers Squibb and Nippon Boehringer Ingelheim; and grants and personal fees from Bayer Yakuhin and Daiichi-Sankyo. JA reports personal fees from Bayer Yakuhin and Sanofi and grants and personal fees from Daiichi-Sankyo. TM reports grants from the Japan Cardiovascular Research Foundation, and personal fees from Nippon Boehringer Ingelheim, Daiichi-Sankyo, AstraZeneca and Bayer Yakuhin. MN reports grants and personal fees from Bayer Yakuhin, Daiichi-Sankyo and Sanofi and personal fees from Bristol Myers Squibb and Nippon Boehringer Ingelheim. KaM reports personal fees from Amgen Astellas BioPharma, Astellas Pharma, MSD, Bayer Yakuhin, Sanofi, Takeda Pharmaceutical, Daiichi-Sankyo, Nippon Boehringer Ingelheim and Bristol Myers Squibb. NH reports grants and personal fees from Bayer Yakuhin, Nippon Boehringer Ingelheim and personal fees from Bristol Myers Squibb. KaK reports grants from the Japan Cardiovascular Research Foundation grants and personal fees from Bayer Yakuhin, Daiichi-Sankyo, Sanofi, MSD and AstraZeneca, and personal fees from Bristol Myers Squibb and Nippon Boehringer Ingelheim. AH reports grants and personal fees from Boston Scientific Japan, Otsuka Pharmaceutical, Sanofi, Astellas Pharma, Bristol Myers Squibb, Daiichi-Sankyo, Bayer Yakuhin, Fukuda Denshi, Abbott Japan, Japan Lifeline, Takeda Pharmaceutical and Sumitomo Dainippon Pharma, and personal fees from Toa Eiyo, Nippon Boehringer Ingelheim, Amgen Astellas BioPharma, and AstraZeneca. HO reports personal fees from Towa Pharmaceutical, Bristol Meyers Squibb, Pfizer, Toa Eiyo, Bayer Yakuhin, and Novartis Pharma. KT received significant research grant from AMI, Bayer Yakuhin, Bristol-Myers K.K., EA Pharma, Mochida Pharmaceutical, and scholarship fund from AMI, Bayer Yakuhin, Boehringer Ingelheim Japan, Chugai Pharmaceutical, Daiichi-Sankyo, Edwards Lifesciences Corporation, Johnson & Johnson K.K., Ono Pharmaceutical, Otsuka Pharmaceutical, Takeda Pharmaceutical, and honoraria from Amgen K.K., Bayer Yakuhin, Daiichi-Sankyo, Kowa Pharmaceutical, Novartis Pharma K.K., Otsuka Pharmaceutical, Pfizer Japan, and belongs to the endowed departments donated by Abbott Japan, Boston Scientific Japan K.K., Fides-one, GM Medical, ITI, Kaneka Medix, Nipro, Terumo, Abbott Medical, Cardinal Heaith Japan, Fukuda Denshi, Japan Lifeline, Medical Appliance, Medtoronic Japan.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The data underlying this article will be shared on reasonable request to the corresponding author.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and the trial was conducted in accordance with the Declaration of Helsinki and approved by the institutional review boards of the Kumamoto University Hospital (Rinri No.2547) and all participating institutions. The data were reviewed by an independent data and safety monitoring committee. In this post hoc analysis, 2215 patients in the modified intention-to-treat population from the AFIRE trial were analysed. Participants gave informed consent to participate in the study before taking part.
References
- 1. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407–77. 10.1093/eurheartj/ehz425 [DOI] [PubMed] [Google Scholar]
- 2. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non–st-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation 2016;134:e123–155. 10.1161/CIR.0000000000000404 [DOI] [PubMed] [Google Scholar]
- 3. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: Executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 2022;145. 10.1161/CIR.0000000000001039 [DOI] [PubMed] [Google Scholar]
- 4. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task force on clinical practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2019;74:104–32. 10.1016/j.jacc.2019.01.011 [DOI] [PubMed] [Google Scholar]
- 5. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 2021;42:373–498. 10.1093/eurheartj/ehaa612 [DOI] [PubMed] [Google Scholar]
- 6. Andrade JG, Aguilar M, Atzema C, et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society comprehensive guidelines for the management of atrial fibrillation. Can J Cardiol 2020;36:1847–948. 10.1016/j.cjca.2020.09.001 [DOI] [PubMed] [Google Scholar]
- 7. Yasuda S, Ogawa H, AFIRE Investigators . Antithrombotic therapy for atrial fibrillation with stable coronary disease. Reply. N Engl J Med 2019;381:2481. 10.1056/NEJMc1914049 [DOI] [PubMed] [Google Scholar]
- 8. Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 2001;285:2864–70. 10.1001/jama.285.22.2864 [DOI] [PubMed] [Google Scholar]
- 9. Lip GYH, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach. Chest 2010;137:263–72. 10.1378/chest.09-1584 [DOI] [PubMed] [Google Scholar]
- 10. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation. Chest 2010;138:1093–100. 10.1378/chest.10-0134 [DOI] [PubMed] [Google Scholar]
- 11. Tabata N, Yamamoto E, Hokimoto S, et al. Prognostic value of the chads2 score for adverse cardiovascular events in coronary artery disease patients without atrial fibrillation-a multi-center observational cohort study. J Am Heart Assoc 2017;6:e006355. 10.1161/JAHA.117.006355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou X, Cao K, Kou S, et al. Usefulness of chads2 score for prognostic stratification of patients with coronary artery disease: a systematic review and meta-analysis of cohort studies. Int J Cardiol 2017;228:906–11. 10.1016/j.ijcard.2016.11.114 [DOI] [PubMed] [Google Scholar]
- 13. Kaikita K, Yasuda S, Akao M, et al. Bleeding and subsequent cardiovascular events and death in atrial fibrillation with stable coronary artery disease: insights from the afire trial. Circ Cardiovasc Interv 2021;14:e010476. 10.1161/CIRCINTERVENTIONS.120.010476 [DOI] [PubMed] [Google Scholar]
- 14. Yasuda S, Kaikita K, Ogawa H, et al. Atrial fibrillation and ischemic events with rivaroxaban in patients with stable coronary artery disease (AFIRE): protocol for a multicenter, prospective, randomized, open-label, parallel group study. Int J Cardiol 2018;265:108–12. 10.1016/j.ijcard.2018.04.131 [DOI] [PubMed] [Google Scholar]
- 15. Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692–4. 10.1111/j.1538-7836.2005.01204.x [DOI] [PubMed] [Google Scholar]
- 16. Stekhoven DJ, Bühlmann P. MissForest -- non-parametric missing value imputation for mixed-type data. Bioinformatics 2012;28:112–8. 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- 17. Kursa MB, Rudnicki WR. Feature selection with the boruta package. J Stat Soft 2010;36:1–13. 10.18637/jss.v036.i11 [DOI] [Google Scholar]
- 18. Ishwaran H, Kogalur UB, Blackstone EH, et al. Random survival forests. Ann Appl Stat 2008;2:820. 10.1214/08-AOAS169 [DOI] [Google Scholar]
- 19. Alba AC, Agoritsas T, Walsh M, et al. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA 2017;318:1377–84. 10.1001/jama.2017.12126 [DOI] [PubMed] [Google Scholar]
- 20. Leening MJG, Vedder MM, Witteman JCM, et al. Net reclassification improvement: computation, interpretation, and controversies: a literature review and clinician’s guide. Ann Intern Med 2014;160:122–31. 10.7326/M13-1522 [DOI] [PubMed] [Google Scholar]
- 21. Fitzgerald M, Saville BR, Lewis RJ. Decision curve analysis. JAMA 2015;313:409–10. 10.1001/jama.2015.37 [DOI] [PubMed] [Google Scholar]
- 22. Nakanishi R, Slomka PJ, Rios R, et al. Machine learning adds to clinical and CAC assessments in predicting 10-year CHD and CVD deaths. JACC Cardiovasc Imaging 2021;14:615–25. 10.1016/j.jcmg.2020.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson KM, Johnson HE, Zhao Y, et al. Scoring of coronary artery disease characteristics on coronary CT angiograms by using machine learning. Radiology 2019;292:354–62. 10.1148/radiol.2019182061 [DOI] [PubMed] [Google Scholar]
- 24. Abdar M, Książek W, Acharya UR, et al. A new machine learning technique for an accurate diagnosis of coronary artery disease. Comput Methods Programs Biomed 2019;179:104992. 10.1016/j.cmpb.2019.104992 [DOI] [PubMed] [Google Scholar]
- 25. Tamarappoo BK, Lin A, Commandeur F, et al. Machine learning integration of circulating and imaging biomarkers for explainable patient-specific prediction of cardiac events: a prospective study. Atherosclerosis 2021;318:76–82. 10.1016/j.atherosclerosis.2020.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Falsetti L, Rucco M, Proietti M, et al. Risk prediction of clinical adverse outcomes with machine learning in a cohort of critically ill patients with atrial fibrillation. Sci Rep 2021;11:18925. 10.1038/s41598-021-97218-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Herrin J, Abraham NS, Yao X, et al. Comparative effectiveness of machine learning approaches for predicting gastrointestinal bleeds in patients receiving antithrombotic treatment. JAMA Netw Open 2021;4:e2110703. 10.1001/jamanetworkopen.2021.10703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Firouznia M, Feeny AK, LaBarbera MA, et al. Machine learning-derived fractal features of shape and texture of the left atrium and pulmonary veins from cardiac computed tomography scans are associated with risk of recurrence of atrial fibrillation postablation. Circ Arrhythm Electrophysiol 2021;14:e009265. 10.1161/CIRCEP.120.009265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu X, Jiang J, Wei L, et al. Prediction of all-cause mortality in coronary artery disease patients with atrial fibrillation based on machine learning models. BMC Cardiovasc Disord 2021;21:499. 10.1186/s12872-021-02314-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leblanc M, Crowley J. Survival trees by goodness of split. Journal of the American Statistical Association 1993;88:457–67. 10.1080/01621459.1993.10476296 [DOI] [Google Scholar]
- 31. Taylor JMG. Random survival forests. J Thorac Oncol 2011;6:1974–5. 10.1097/JTO.0b013e318233d835 [DOI] [PubMed] [Google Scholar]
- 32. Baber U, Mehran R, Giustino G, et al. Coronary thrombosis and major bleeding after PCI with drug-eluting stents: risk scores from Paris. J Am Coll Cardiol 2016;67:2224–34. 10.1016/j.jacc.2016.02.064 [DOI] [PubMed] [Google Scholar]
- 33. Natsuaki M, Morimoto T, Yamaji K, et al. Prediction of thrombotic and bleeding events after percutaneous coronary intervention: credo‐kyoto thrombotic and bleeding risk scores. JAHA 2018;7. 10.1161/JAHA.118.008708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li H, Borinskaya S, Yoshimura K, et al. Refined geographic distribution of the oriental aldh2*504lys (nee 487lys) variant. Ann Hum Genet 2009;73:335–45. 10.1111/j.1469-1809.2009.00517.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yokoyama A, Omori T, Yokoyama T. Alcohol and aldehyde dehydrogenase polymorphisms and a new strategy for prevention and screening for cancer in the upper aerodigestive tract in East Asians. Keio J Med 2010;59:115–30. 10.2302/kjm.59.115 [DOI] [PubMed] [Google Scholar]
- 36. Yukawa Y, Muto M, Hori K, et al. Combination of adh1b*2/aldh2*2 polymorphisms alters acetaldehyde-derived DNA damage in the blood of Japanese alcoholics. Cancer Sci 2012;103:1651–5. 10.1111/j.1349-7006.2012.02360.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Liu X, Sun A. Aldehyde dehydrogenase-2 roles in ischemic cardiovascular disease. Curr Drug Targets 2017;18:1817–23. 10.2174/1389450117666160912174417 [DOI] [PubMed] [Google Scholar]
- 38. Mizuno Y, Harada E, Morita S, et al. Response to letter regarding article, "East Asian variant of aldehyde dehydrogenase 2 is associated with coronary spastic angina: possible roles of reactive aldehydes and implications of alcohol flushing syndrome.'' Circulation 2015;132:e383–4. 10.1161/CIRCULATIONAHA.115.018755 [DOI] [PubMed] [Google Scholar]
- 39. Mizuno Y, Hokimoto S, Harada E, et al. Variant aldehyde dehydrogenase 2 (aldh2*2) is a risk factor for coronary spasm and ST-segment elevation myocardial infarction. J Am Heart Assoc 2016;5:e003247. 10.1161/JAHA.116.003247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ishida T, Arima Y, Mizuno Y, et al. East Asian variant aldehyde dehydrogenase type 2 genotype exacerbates myocardial ischemia/reperfusion injury in men among patients with ST-segment elevation myocardial infarction -sex differences-. Eur Heart J 2020;41. 10.1093/ehjci/ehaa946.1579 [DOI] [PubMed] [Google Scholar]
- 41. Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with eacts: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2018;39:213–60. 10.1093/eurheartj/ehx419 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2023-002292supp001.pdf (2.2MB, pdf)
Data Availability Statement
Data are available on reasonable request. The data underlying this article will be shared on reasonable request to the corresponding author.