To the Editor
Vitiligo is an autoimmune disease characterized by areas of skin depigmentation caused by the immune system targeting melanocytes (Ezzedine et al., 2015). The onset of the disease can occur at any age and is often associated with adverse psychosocial effects as well as comorbid autoimmune conditions (Ahmed et al., 2013; Dahir and Thomsen, 2018; Gill et al., 2016; Nguyen et al., 2016; Rzepecki et al., 2018; Sheth et al., 2013; Wu and Cohen, 2019). Estimates of the point prevalence of vitiligo vary across published sources, with a recent analysis of insurance claims reporting a diagnosed prevalence of 0.05%, whereas a meta-analysis gave estimates of 0.2% in population-based studies and 1.8% in hospital-based studies (Lim et al., 2017; Zhang et al., 2016). Published data on the incidence of vitiligo are scant. Given this variation in reported prevalence and the paucity of data on incidence, we conducted a retrospective, observational study using the IBM MarketScan Commercial and Medicare Supplemental database to estimate the annual diagnosed prevalence and incidence of vitiligo among the employer-sponsored insurance (ESI) population in the United States of America (US). Annual incidence and prevalence trends were compared over 5 years. The MarketScan Commercial Claims and Encounters database contains de-identified data from active employees, early retirees, COBRA continuers, and dependents insured by employer-sponsored plans (i.e., persons not eligible for Medicare). The Medicare Supplemental database contains Medicare-eligible retirees with commercially available Medicare Advantage supplemental plans.
Our analysis identified prevalent cases of vitiligo as patients with ≥1 inpatient or outpatient claim for vitiligo (International Classification of Disease–Clinical Modification 9/10: 709.01, L80, or H02.731-H02.739) between January 1, 2013, and December 31, 2017. Continuous health plan enrollment was assessed for each year, and patients with a claim for vitiligo from previous calendar years were carried over to the year of analysis if continuous enrollment criteria were met. This cohort of patients served as the numerator for calculating annual diagnosed prevalence referred to as prevalence hereon. The denominator for calculating the annual diagnosed prevalence was the total number of insured members with continuous enrollment in each calendar year. Diagnosed incident cases of vitiligo, referred to as incidence hereon, were identified as patients with ≥1 inpatient or outpatient claim for vitiligo during the same time period used to calculate prevalence and no evidence of vitiligo in the previous 12 months. The denominator for calculating the annual incidence was the total number of insured members with continuous enrollment in each calendar year and no evidence of vitiligo in the 12 months before the first claim for vitiligo. Estimates of annual prevalence and incidence were calculated for the overall cohort as well as for adult (aged ≥18 years) and pediatric (aged <18 years) patients. A sensitivity analysis of both prevalence and incidence was conducted to account for the potential misdiagnosis of vitiligo. It used a more restricted criteria for vitiligo that included patients with ≥1 inpatient claim or ≥2 outpatient claims for vitiligo. Among patients with ≥2 outpatient claims for vitiligo, the first outpatient claim was required to be a diagnosis for vitiligo. The second outpatient claim could have been (i) a diagnosis of vitiligo that was ≥30 days apart from the first vitiligo diagnosis claim or (ii) a phototherapy procedure (Current Procedural Terminology codes: 96912, 96900, 96910) that may have occurred within ≤30 days of the first vitiligo diagnosis claim. All estimates were weighted to 2018 national estimates of the US ESI population using MarketScan Commercial Insurance weights that were constructed using the public-use microdata sample of the American Community Survey by the US Census Bureau (US Census Bureau, 2020). The proportion of patients with a first claim for vitiligo diagnosis from a primary care provider or dermatologist was also investigated. All statistical analyses were conducted using SAS v9.4 software (Cary, NC). All study data were de-identified and fully compliant with Health Insurance Portability and Accountability Act Regulations (45 Code of Federal Regulations 164.514e); therefore, approval from an institutional review board was not required, and informed consent was not obtained.
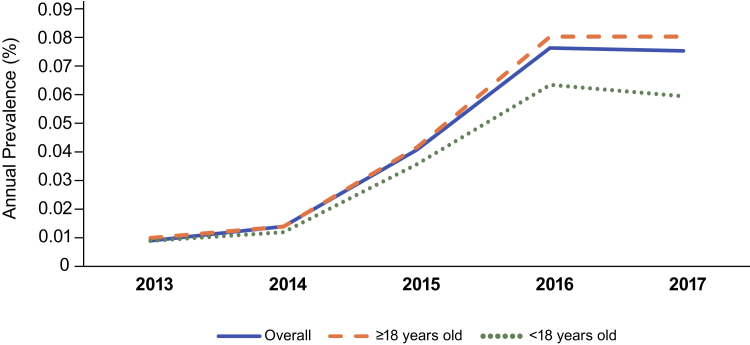
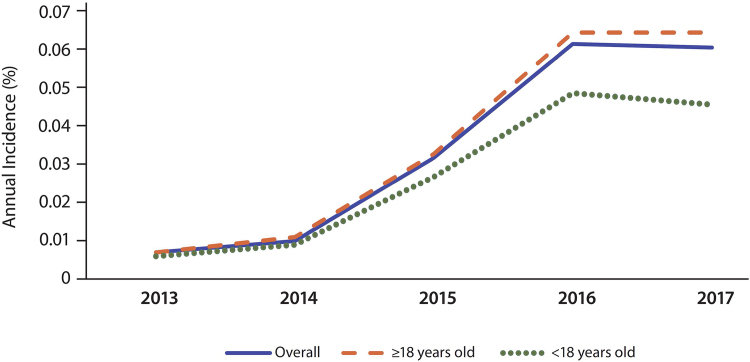
Our results showed that there were 107,612 patients with vitiligo in the prevalence cohort in 2017, up from 11,239 patients in 2013, with annual prevalence increasing from 0.009% to 0.076% during the 5-year observation period (Figure 1 and Table 1). Stratification into adult and pediatric patients showed similar trends to the overall cohort. In 2017, there were 85,821 newly diagnosed cases of vitiligo in the incidence cohort, which represented an increase in annual incidence from 0.007% to 0.061% during the 5-year observation period (Figure 2 and Table 2). Similar to prevalence, stratification into adult and pediatric patients showed similar trends to the overall cohort. Results from the sensitivity analysis were consistent with the primary analysis in showing an increase in prevalence and incidence over time for the overall cohort as well as for the adult and pediatric subgroups. Approximately 50% of the first claims for vitiligo diagnosis were initiated by a dermatologist in each of the 5 years from 2013 to 2017, and approximately 10% were from primary care physicians.
Figure 1.
Annual prevalence of vitiligo among individuals with employer-sponsored insurance in the United States. Overall data are those for adults and adolescents. Prevalence was based on 1 or more inpatient or outpatient claim.
Table 1.
Annual Prevalence of Vitiligo Among Individuals with Employer-Sponsored Insurance in the United States
| Population and Variable | Year |
||||
|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | |
| All ages | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 11,239 | 16,091 | 51,048 | 98,697 | 107,612 |
| Patients with continuous health plan enrollment (denominator), n | 119,443,347 | 118,266,837 | 125,870,232 | 128,795,066 | 140,998,102 |
| Annual prevalence, % | 0.009 | 0.014 | 0.041 | 0.077 | 0.076 |
| Sensitivity analysis numerator, n | 4,244 | 6,216 | 18,876 | 28,277 | 31,935 |
| Sensitivity analysis annual prevalence, % | 0.004 | 0.005 | 0.015 | 0.022 | 0.023 |
| Age ≥18 years | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 8,927 | 12,840 | 41,165 | 80,895 | 88,289 |
| Patients with continuous health plan enrollment (denominator), n | 92,846,379 | 92,036,794 | 98,202,751 | 100,177,023 | 108,927,783 |
| Annual prevalence, % | 0.010 | 0.014 | 0.042 | 0.081 | 0.081 |
| Sensitivity analysis numerator, n | 3,214 | 4,646 | 14,288 | 22,166 | 25,170 |
| Sensitivity analysis annual prevalence, % | 0.004 | 0.005 | 0.015 | 0.022 | 0.023 |
| Age <18 years | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 2,312 | 3,251 | 9,883 | 17,802 | 19,323 |
| Patients with continuous health plan enrollment (denominator), n | 26,596,968 | 26,230,043 | 27,667,481 | 27,718,043 | 32,070,319 |
| Annual prevalence, % | 0.009 | 0.012 | 0.036 | 0.064 | 0.060 |
| Sensitivity analysis numerator, n | 1,030 | 1,571 | 4,588 | 6,110 | 6,765 |
| Sensitivity analysis annual prevalence, % | 0.004 | 0.006 | 0.017 | 0.022 | 0.021 |
Figure 2.
Annual incidence of vitiligo among individuals with employer-sponsored insurance in the United States. Overall data are those for adults and adolescents. Incidence was based on 1 or more inpatient or outpatient claim.
Table 2.
Annual Incidence of Vitiligo Among Individuals with Employer-Sponsored Insurance in the United States
| Population and Variable | Year |
||||
|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | |
| All ages | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 8,319 | 11,896 | 39,940 | 78,834 | 85,821 |
| Patients with continuous health plan enrollment (denominator), n | 119,434,412 | 118,255,211 | 125,842,664 | 127,844,265 | 140,901,558 |
| Annual incidence, % | 0.007 | 0.010 | 0.032 | 0.062 | 0.061 |
| Sensitivity analysis numerator, n | 2,362 | 3,500 | 11,620 | 17,390 | 20,446 |
| Sensitivity analysis annual incidence, % | 0.002 | 0.003 | 0.009 | 0.014 | 0.015 |
| Age ≥18 years | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 6,727 | 9,644 | 32,571 | 65,294 | 70,952 |
| Patients with continuous health plan enrollment (denominator), n | 92,839,434 | 92,027,575 | 98,180,722 | 100,136,233 | 108,849,402 |
| Annual incidence, % | 0.007 | 0.011 | 0.033 | 0.065 | 0.065 |
| Sensitivity analysis numerator, n | 1,765 | 2,585 | 8,748 | 13,698 | 16,116 |
| Sensitivity analysis annual incidence, % | 0.002 | 0.003 | 0.009 | 0.014 | 0.015 |
| Age <18 years | |||||
| Patients meeting vitiligo definition and continuously enrolled in a health plan (numerator), n | 1,592 | 2,252 | 7,369 | 13,540 | 14,869 |
| Patients with continuous health plan enrollment (denominator), n | 26,594,977 | 26,227,636 | 27,661,942 | 27,708,032 | 32,052,157 |
| Annual incidence, % | 0.006 | 0.009 | 0.027 | 0.049 | 0.046 |
| Sensitivity analysis numerator, n | 597 | 915 | 2,873 | 3,692 | 4,331 |
| Sensitivity analysis annual incidence, % | 0.002 | 0.004 | 0.010 | 0.013 | 0.014 |
Although healthcare claims are commonly used to estimate disease burden, including prevalence and incidence, our retrospective, observational analysis has some limitations that are well recognized with the use of claims data for such estimation (Broder et al., 2017; Konrad et al., 2019). First, insurance claim data are collected for payment purposes and may have inherent limitations when used for research purposes, such as International Classification of Disease–Clinical Modification codes not allowing the identification of segmental or nonsegmental subtypes of vitiligo. The International Classification of Disease–Clinical Modification 9/10 codes of vitiligo assume that the clinician followed formal diagnostic criteria. If the formal diagnostic criteria are not met, a misdiagnosis could result. The other International Classification of Disease–Clinical Modification codes used do not include other areas of the body that vitiligo commonly affects, such as the neck, hands, and skin creases. This methodology for identifying subjects with vitiligo has not been validated. Second, our results may underestimate the real-world prevalence and incidence of vitiligo due to the minimal or absent healthcare-seeking behavior of some patients with this condition, which may in turn be influenced by the absence of approved pharmacologic treatments and restrictions on the insurance coverage for non-pharmacologic treatments, such as phototherapy. Indeed, we note our diagnosed prevalence estimates are lower than those of population-based studies, including a recent US-based study that estimated the diagnosed prevalence of vitiligo at 0.46%–0.77% (Gandhi et al., 2022), but comparable to a previous claims study that used the MarketScan database, Milliman Medicare Part D Claims database, and Milliman Medicaid Consolidated Health Cost Guidelines Sources Database and reported vitiligo prevalence at 0.05%. Third, data were limited to US enrollees with commercial health insurance and therefore may not be generalizable to other populations, such as those solely insured through government funded programs, such as Medicare, Medicaid, and Veterans Affairs, the uninsured, and those outside the US. Fourth, there was potential for inaccurate classification of the diagnosis of vitiligo when using data obtained from a single insurance claim, although the trends we observed were consistent in the sensitivity analysis. Fifth, race is not captured in IBM MarketScan, so we were unable to determine the variation in prevalence or incidence by race. Sixth, incident cases may be overestimated, as our study included a preindex observation period of 12 months with no diagnosis of vitiligo to identify incident cases, but it is possible that some of the cases identified may have had a previous claim that predated the observation period. In addition, new plan enrollees may have had a vitiligo diagnosis over the past several years but may be identified as an incident case in the current plan by virtue of their first observed claim in the current plan. Finally, the differences in vitiligo prevalence observed over time within this study could be due to a change in the underlying health plans, including the enrolled patient population that comprised the MarketScan database. The shifts in underlying plan characteristics may explain the changes observed. The increases in prevalence and incidence over time observed in this study may also be supported by the increases in prevalence and incidence estimates observed for autoimmune conditions like thyroid disease that are comorbid with vitiligo (Leese et al., 2008). Future studies may investigate trends in vitiligo-related comorbidities over time as explanatory empirical evidence. Nevertheless, our study strengths include the evaluation of annual trends for the incidence and prevalence of vitiligo over 5 years and addresses earlier literature gaps on the nonavailability of such trends. The study used a large database of commercially insured US populations. Large databases created by healthcare operations are frequently updated, cover large populations, and are well suited for estimating prevalence and incidence, as well as analyzing trends over time.
In conclusion, there were 107,612 patients diagnosed with vitiligo and 85,821 newly diagnosed cases among the US ESI population in 2017. Our estimate of the annual diagnosed prevalence of vitiligo in 2017 (0.076%) was similar to the estimate reported by a previous analysis of insurance claims data (Lim et al., 2017). The annual diagnosed prevalence and incidence of vitiligo in the US both increased more than 5-fold in the 5-year period between 2013 and 2017. The cause of this significant increase warrants further investigation, including consideration of potential factors such as better access to medical care, greater awareness and better tools for vitiligo diagnosis, trends in associated comorbidities, and last but not the least, evolving diversity of the US population that may have contributed to the underlying genetic variation and population lifestyle changes that resulted in a higher incidence and prevalence over time.
Summary
Vitiligo is an autoimmune disease characterized by areas of skin depigmentation. Estimates of the point prevalence of vitiligo vary between 0.05% (insurance claims), 0.2% (population-based studies), and 1.8% (hospital-based studies). Data on the incidence of vitiligo are scant. We performed an observational, retrospective database study to estimate the annual diagnosed prevalence and incidence of vitiligo among the ESI population in the US. Data from the IBM MarketScan database were used to identify patients with an ≥1 inpatient or outpatient claim for vitiligo from January 1, 2013, through December 31, 2017. Estimates of the annual diagnosed prevalence and incidence were calculated for the overall cohort and adult (aged ≥18 years) and pediatric (aged <18 years) patients. There were 107,612 patients diagnosed with vitiligo and 85,821 newly diagnosed cases among the ESI population in the US in 2017. Our estimate of the annual diagnosed prevalence of vitiligo in 2017 (0.076%) was similar to the estimate reported by a previous analysis of insurance claims data. The annual diagnosed prevalence and incidence of vitiligo both increased more than 5-fold in the 5-year period between 2013 and 2017. The cause of this significant increase warrants further investigation.
Data availability statement
De-identified claims data from the IBM MarketScan Commercial and Medicare Supplemental database were used for study purposes. Minimal data sets necessary to interpret and or replicate data in this paper are available upon request to the corresponding author.
ORCIDs
Markqayne Ray: http://orcid.org/0000-0001-8691-3756
Kavita Gandhi: http://orcid.org/0000-0002-4521-2467
Keisha Maughn: http://orcid.org/0000-0001-7233-7487
Amit G. Pandya: http://orcid.org/0000-0002-3916-2651
Conflict of Interest
MR and KG were employees of Pfizer at the time of study conduct and analyses; therefore, MR and KG may hold stock and/or stock options with Pfizer. KG is currently an employee of Janssen Pharmaceuticals and holds stock options of Johnson and Johnson. KM is an employee of STATinMED Research; STATinMED Research received payment from Pfizer for participation in this study. AGP declares acting as a consultant for AbbVie, Arcutis, Avita, Chromaderm, Immune Tolerance Network, Incyte, Pfizer, Twi, Viela Bio, and Villaris and holds stock or stock options in Tara Medical and Zerigo Health.
Acknowledgments
This study was sponsored by Pfizer. The authors gratefully acknowledge Sujana Borra, Ila Sruti, and Lang Xu, formerly of STATinMED Research (Plano, TX), for their contributions to the statistical analyses conducted during this study. Medical writing support was provided by David Wateridge, PhD and Rency Mathew, PhD of Engage Scientific Solutions and Nicola Gillespie, DVM, of Health Interactions, and was funded by Pfizer.
Author Contributions
Conceptualization: MR, KG, KM, AGP; Data Curation: MR, KG, KM; Writing – Original draft Preparation: MR, KG, KM, AGP; Writing – Review and Editing: MR, KG, KM, AGP
Accepted manuscript published online XXX; corrected proof published online XXX
Footnotes
Cite this article as: JID Innovations 2023;X:100199
References
- Ahmed A., Leon A., Butler D.C., Reichenberg J. Quality-of-life effects of common dermatological diseases. Semin Cutan Med Surg. 2013;32:101–109. doi: 10.12788/j.sder.0009. [DOI] [PubMed] [Google Scholar]
- Broder M.S., Cai B., Chang E., Neary M.P. Epidemiology of gastrointestinal neuroendocrine tumors in a U.S. commercially insured population. Endocr Pract. 2017;23:1210–1216. doi: 10.4158/EP171879.OR. [DOI] [PubMed] [Google Scholar]
- Dahir A.M., Thomsen S.F. Comorbidities in vitiligo: comprehensive review. Int J Dermatol. 2018;57:1157–1164. doi: 10.1111/ijd.14055. [DOI] [PubMed] [Google Scholar]
- Ezzedine K., Eleftheriadou V., Whitton M., van Geel N. Vitiligo. Lancet. 2015;386:74–84. doi: 10.1016/S0140-6736(14)60763-7. [DOI] [PubMed] [Google Scholar]
- Gandhi K., Ezzedine K., Anastassopoulos K.P., Patel R., Sikirica V., Daniel S.R., et al. Prevalence of vitiligo among adults in the United States. JAMA Dermatol. 2022;158:43–50. doi: 10.1001/jamadermatol.2021.4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill L., Zarbo A., Isedeh P., Jacobsen G., Lim H.W., Hamzavi I. Comorbid autoimmune diseases in patients with vitiligo: a cross-sectional study. J Am Acad Dermatol. 2016;74:295–302. doi: 10.1016/j.jaad.2015.08.063. [DOI] [PubMed] [Google Scholar]
- Konrad R., Zhang W., Bjarndóttir M., Proaño R. Key considerations when using health insurance claims data in advanced data analyses: an experience report. Health Syst (Basingstoke) 2019;9:317–325. doi: 10.1080/20476965.2019.1581433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leese G.P., Flynn R.V., Jung R.T., Macdonald T.M., Murphy M.J., Morris A.D. Increasing prevalence and incidence of thyroid disease in Tayside, Scotland: the Thyroid Epidemiology Audit and Research Study (TEARS) Clin Endocrinol (Oxf) 2008;68:311–316. doi: 10.1111/j.1365-2265.2007.03051.x. [DOI] [PubMed] [Google Scholar]
- Lim H.W., Collins S.A.B., Resneck J.S., Jr., Bolognia J.L., Hodge J.A., Rohrer T.A., et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76:958–972.e2. doi: 10.1016/j.jaad.2016.12.043. [DOI] [PubMed] [Google Scholar]
- Nguyen C.M., Beroukhim K., Danesh M.J., Babikian A., Koo J., Leon A. The psychosocial impact of acne, vitiligo, and psoriasis: a review. Clin Cosmet Investig Dermatol. 2016;9:383–392. doi: 10.2147/CCID.S76088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rzepecki A.K., McLellan B.N., Elbuluk N. Beyond traditional treatment: the importance of psychosocial therapy in vitiligo. J Drugs Dermatol. 2018;17:688–691. [PubMed] [Google Scholar]
- Sheth V.M., Guo Y., Qureshi A.A. Comorbidities associated with vitiligo: a ten-year retrospective study. Dermatology. 2013;227:311–315. doi: 10.1159/000354607. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau American Community Survey (ACS) 2020. https://www.census.gov/programs-surveys/acs
- Wu J.H., Cohen B.A. The stigma of skin disease. Curr Opin Pediatr. 2019;31:509–514. doi: 10.1097/MOP.0000000000000792. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Cai Y., Shi M., Jiang S., Cui S., Wu Y., et al. The prevalence of vitiligo: a meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0163806. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified claims data from the IBM MarketScan Commercial and Medicare Supplemental database were used for study purposes. Minimal data sets necessary to interpret and or replicate data in this paper are available upon request to the corresponding author.