Fulminant SSPE (Subacute Sclerosing Panencephalitis) has been defined as the development of at least 66% neurological disability within 3 months of the first neurological symptom and death or a severe neurological disability (exceeding 90%) within 6 months of onset. 1 This case emphasizes the highly fulminant presentation of SSPE as a hyperkinetic movement disorder, due to which the classical clinical features could not be appreciated.
A 13‐year‐old boy, born out of non‐consanguinity with normal birth and development, presented with fever and headache 1 month back. 1 week later, he developed symptoms of inattention, irritability, blunting of affect and motor and verbal perseveration. By week 2, he developed dystonic posturing of the left upper and lower limbs, florid choreoathetoid movements, and opisthotonus with grunting sounds (Video 1). This was followed by three episodes of seizures and altered sensorium. He was managed outside as a case of meningoencephalitis with intravenous ceftriaxone, acyclovir, and antiepileptics, with some improvement in his sensorium. However, his movement disorder and cognitive dysfunction worsened, and he presented to us by week 4 of symptom onset. On examination, he was stuporous. Fundus was normal. All deep tendon reflexes were present with a left striatal toe. Apart from the hyperkinetic movement disorder, involuntary vocalization in the form of screaming and singing was also present (Video 1). Keeping a possibility of autoimmune encephalitis, he was given pulse steroids followed by plasmapheresis with no improvement.
Video 1.
Video demonstrating severe dystonia affecting all four limbs and face. There are superimposed choreoathetoid movements and myoclonic jerks. Abnormal vocalization and opisthotonic posturing are evident in the latter part of the video.
Workup for Wilson's disease was normal. CSF (Cerebrospinal Fluid) revealed lymphocytic pleocytosis with slightly elevated protein and normal sugar and negative pan‐viral PCR and the autoimmune panel. MRI brain and FDG PET are depicted in Figures 1 and 2, respectively. Initial EEG showed delta wave slowing. The slow periodic myoclonus occurring every 2–4 s appeared 4 weeks into the illness and persisted despite administering valproate, levetiracetam and benzodiazepines. He was immunized for measles with a history of an exanthematous illness at 4 years of age. Measles CSF IgG antibodies titre by ELISA came out to be 625.
FIG. 1.
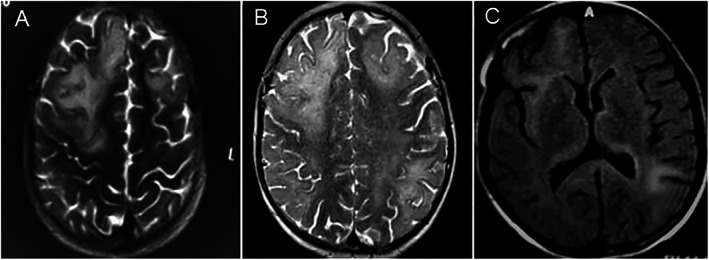
MRI Brain showing T2 hyperintensities in bilateral right >left frontoparietal lobes at 2 weeks of symptom onset involving both gray and white matter (A); Progression of T2 hyperintense lesions with relative sparing of occipital lobes at week 4 of symptom onset (B); Sparing of bilateral basal ganglia with involvement of thalamus bilaterally on FLAIR images.
FIG. 2.
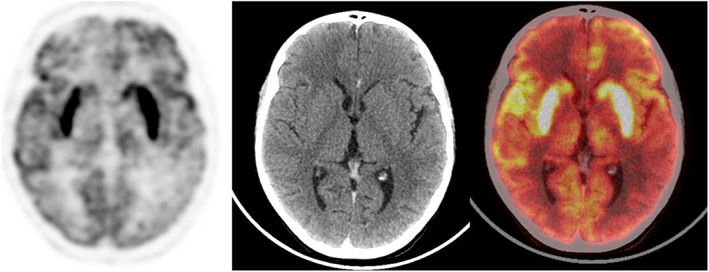
Transaxial FDG PET (A), CT (B) and fused PET/CT (C) images of the brain showing diffusely increased FDG uptake in bilateral basal ganglia with no definite morphological CT changes. Asymmetrically reduced FDG uptake is noted in the bilateral cerebral hemispheres, sparing the sensorimotor and left mesial temporal cortices.
Our case is unique in a few aspects. Firstly, fulminant SSPE is a rare presentation, while its presentation as a predominant movement disorder is even more unusual. 2 , 3 Most cases of fulminant SSPE usually present with cognitive impairment, myoclonus and visual loss. Our patient presented with movement disorders quite early in the course, and the classical slow myoclonus with characteristic EEG findings was evident only later (Video 2). Secondly, repetitive behaviors and vocalizations can occur in SSPE due to impairment of cortico‐striato‐thalamo‐cortical circuitry resulting from panencephalitis and white matter demyelination disrupting GABAergic and glutaminergic neurons. 4 Thirdly, the fulminant presentation in our patient raised the possibility of autoimmune encephalitis. Garg et al. have also described a case of fulminant SSPE that mimicked autoimmune encephalitis, although their patient's predominant manifestation was status epilepticus. 5 The red flags for a diagnosis of autoimmune encephalitis in our patient were the occurrence of slow periodic myoclonus and extensive MRI changes, which are unusual in autoimmune encephalitis. The occurrence of SSPE despite being vaccinated can be either due to subclinical infection before vaccination or poor maintenance of the cold chain.
Video 2.
Video showing classical slow myoclonus of SSPE. Periodic discharges are also shown.
Author Roles
(1) Research project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript Preparation: A. Writing of the first draft, B. Review and Critique.
P.Y.: 1B, 1C, 3A.
S.M.: 1B, 1C.
N.B.: 1C, 3B.
S.M.: 1A, 1B, 1C, 3A, 3B.
Disclosures
Ethical Compliance Statement: The authors confirm that the approval of an institutional review board was not required for this work. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines. We also confirm that the patient's guardian has given written informed consent for the publication of her video.
Funding Sources and Conflicts of Interest: No specific funding was received for this work. The authors declare that there are no conflicts of interest relevant to this work.
Financial Disclosures for the Previous 12 Months: The authors declare that there are no additional disclosures to report.
References
- 1. PeBenito R, Naqvi SH, Arca MM, Schubert R. Fulminating subacute sclerosing panencephalitis: Case report and literature review. Clin Pediatr (Phila) 1997. Mar;36(3):149–154. [DOI] [PubMed] [Google Scholar]
- 2. Rizvi I, Garg RK, Jain A, Malhotra HS, Kumar N, Uniyal R. Teaching video NeuroImages: An unusual case of fulminant subacute sclerosing panencephalitis. Neurology 2019. Mar 12;92(11):e1270. [DOI] [PubMed] [Google Scholar]
- 3. Panda PK, Sharawat IK. Early‐onset fulminant subacute Sclerosing Panencephalitis in a toddler. Indian Pediatr 2020. Jan 15;57(1):81–82. [PubMed] [Google Scholar]
- 4. Pandey S, Shukla T, Mishra A. The Spectrum of repetitive behaviors associated with subacute Sclerosing Panencephalitis. Mov Disord 2021. Feb;36(2):497–503. [DOI] [PubMed] [Google Scholar]
- 5. Garg RK, Kumar N, Rizvi I, Pandey S, Malhotra HS, Uniyal R. Fulminant subacute Sclerosing Panencephalitis mimicking autoimmune encephalitis. Pediatr Infect Dis J 2019. Mar;38(3):e64. [DOI] [PubMed] [Google Scholar]


