Abstract
Introduction:
The high prevalence among elderly individuals and potential adverse impact on their overall life quality make chronic musculoskeletal pain a significant public health concern. Chronic musculoskeletal pain is an important cause of self-medication, which must be addressed to avoid various side effects and improve elderly health. This study aimed to determine the prevalence of chronic musculoskeletal pain and its associated factors among individuals (age ≥60 years) in rural West Bengal and explore their perspectives and perceived barriers regarding pain and its management.
Method:
This mixed-method study was conducted in rural West Bengal from December 2021 to June 2022. The quantitative strand was conducted by interviewing 255 elderly participants (age ≥60 years) using a structured questionnaire. The qualitative strand was conducted via in-depth interviews of 10 patients with chronic pain. Quantitative data were analyzed using SPSS version 16, and chronic pain-related factors were analyzed using logistic regression models. Qualitative data were analyzed thematically.
Results:
Among the participants, 56.8% reported chronic musculoskeletal pain. The most frequently affected site was the knee joint. Comorbidity (adjusted odds ratio [aOR]=7.47, 95% confidence interval [CI]=3.2–17.5), age (aOR=5.16, 95% CI=2.2–13.5), depression (aOR=2.96, 95% CI=1.2–6.7) and over-the-counter drug usage (aOR=2.51, 95% CI=1.1–6.4) were significantly associated with chronic pain. Analgesic dependency, lack of motivation to adopt lifestyle modifications, lack of knowledge on analgesic side effects were considered pain management barriers.
Conclusion:
Managing comorbidities, providing mental support, generating awareness of analgesic side effects, strengthening healthcare facilities should be prioritized for holistic chronic musculoskeletal pain management.
Keywords: Chronic pain, Elderly, India, Rural Health
Introduction
Chronic pain is defined as pain that persists or recurs for longer than 3 months according to the International Association for the Study of Pain. Its global burden has been projected to be large and to increase further over time. Chronic pain contributes significantly to increasing the burden of non-communicable diseases worldwide.1 According to the World Health Organization, approximately 1.71 billion people worldwide are experiencing musculoskeletal conditions, of which chronic pain is a prominent feature.2 The focus on musculoskeletal pain and its burden has been one of the driving forces in the establishment of the International Bone and Joint Decade (2000–2010).3 Epidemiological studies across the globe have reported a higher prevalence of chronic musculoskeletal pain among elderly persons than among the general adult population.4 A number of key contextual factors influence the downstream impact of chronic musculoskeletal pain, such as the inability to maintain an independent lifestyle and disruption in productivity, social relationships and overall quality of life.5 In addition, the high prevalence of other comorbid conditions among elderly individuals further intensifies the challenging issue of pain management, as mere pharmaceutical management in this population is often ineffective and limited by side effects.6 Despite this fact, chronic pain has emerged as one of the significant reasons behind self-medication and unsolicited use of over-the-counter (OTC) analgesic drugs.7,8
The proportion of elderly persons in India has increased from 5.6% of the total population in 1961 to 8.65% in 2011, thus reflecting a nationwide phenomenon of population ageing.9 This gradual demographic transition necessitates the achievement of elderly health and well-being, which becomes largely jeopardised by the burden of chronic musculoskeletal pain compounded with the practice of self-medication. In India, where social security systems are inadequate, and health sector investment is low, a substantial disparity persists between urban and rural healthcare service access, which consequently points towards a deprived rural sector. Although there is considerable evidence of a high propensity of chronic musculoskeletal pain among elderly individuals, the perception of patients regarding pain management remains neglected in previous studies, thus mandating the need for qualitative exploration. Accordingly, the current study aimed to assess the prevalence of chronic pain and its associated factors among an elderly population in rural West Bengal. Moreover, a deeper insight into the participants’ perspectives and perceived barriers in regard to chronic musculoskeletal pain and its management was explored using a mixed-method approach.
Methods
Study design, setting andparticipants
This community-based mixed-method study (convergent parallel design: quantitative + qualitative) was conducted from December 2021 to June 2022 in villages situated in the service area of the Rural Health Unit and Training Centre at Singur, Hooghly district, West Bengal. A total of 64 villages catered by 2 primary health centres and 12 subcentres were included in this study. Elderly persons (age ≥60 years) residing in the study area were selected as the study participants. Only one elderly participant was selected from a single household. Those who were critically ill during data collection were excluded. Of the total surveyed elderly participants, those with chronic musculoskeletal pain were selected for in-depth interviews (IDIs) purposively to undertake the qualitative strand of the study.
Sample size determination
Cochran’s formula for determining the sample size was applied for the quantitative strand.10 The standard normal variate was taken as 1.96 (5% type-I error); estimated prevalence of chronic pain among elderly individuals as 47.6% as per a study conducted in rural Tamil Nadu, India; and relative error in precision as 20%.11 Considering a design effect of 2 and non-response allowance of 10%, the final estimated sample size was 245. The sample size for the qualitative strand was determined using the theory of data saturation.
Sampling design
Concurrent mixed-method sampling (multistage probabilistic sampling for the quantitative strand and purposive sampling for the quantitative strand) was used. A two-stage 15-cluster sampling technique was implemented using the probability proportional to the population size method. Each of the 64 villages was considered a cluster. In the first stage of sampling, 15 clusters were selected after line-listing the villages according to their population.
In the second stage, 17 participants were selected from each of the 15 selected clusters (cluster size=sample size/number of clusters; i.e. 245/15=17) using the random walk method. The random walk method was conducted in two steps. The first step was to select the starting point from the village, which was performed after identifying the centre of the village, from where a pen was rotated, and the starting point was selected by the direction of the pen-tip. The second step was to select the houses in the direction of the starting point, which was performed by writing the house number on pieces of paper and randomly drawing one piece of paper for selecting the first house, with the following houses subsequently selected in a clockwise direction until the desired sample was achieved.12 When two or more elderly individuals were present in the same household, the eldest person was selected. Eligible participants were approached to participate in the study with the help of the respective honorary health workers assigned in that area. Ultimately, a total of 255 elderly participants were surveyed.
Participants for the qualitative strand were selected via a combination of different purposive sampling techniques, such as convenient and maximum variation sampling.
Data collection techniques, tools andparameters
The quantitative strand of the study was conducted via face-to-face interviews using a pre-tested schedule. Local-language versions of the schedule were face- and content- validated by public health experts. The schedule encompassed the following domains:
a. Socio-demographic details, such as age, sex, education, marital status, caste, socioeconomic status and family type.
b. Self-medication practices (at least once in the past 3 months since the time of data collection). Self-medication was defined as the use of medicinal products by a consumer to treat self-recognised disorders or symptoms or the intermittent or continued use of a medication prescribed by a physician for chronic or recurring diseases or symptoms.13 Herein, the respondents were asked whether they had adopted any lifestyle modifications (e.g. weight reduction or exercise) to prevent the onset or deterioration of musculoskeletal pain.
c. Past medical records were reviewed to identify comorbidities among the participants.
d. Participants’ knowledge of pain medications and their side effects was assessed using a five-item questionnaire (Cronbach’s alpha=0.73). This questionnaire was developed by the authors of this present article. This was tested for internal consistency (Reliability) through Cronbach's alpha (0.73) and this instrument was again checked on the basis of expert judgment. It was face and content validated by the public health experts. A correct response for a particular question is given a score of ‘1’, while an incorrect response or ‘do not know’ response is given a score of ‘0’. Herein, the cut-off for having satisfactory knowledge was the 50th percentile of the total attainable score.
e. The mental health status of the participants was assessed using the Geriatric Depression Scale (Short Form) consisting of 15 items; a score of ≥5 is suggestive of the presence of depression.14
f. The outcome variable of the study was the presence of chronic musculoskeletal pain among the study participants. The participants were enquired whether they had any chronic musculoskeletal pain existing for 3 months or more. Thereafter, those who reported having chronic pain were interviewed using the Brief Pain Inventory questionnaire.15 This inventory uses a numeric rating scale (0–10) consisting of two parts about pain intensity and severity and a fTont-and-back human body diagram. The pain severity score is assessed using the following item: ‘Please rate your pain by circling the number that best describes your pain at its worst in the last week’. A score of 1–4 is denoted as ‘mild pain’, 5–6 as ‘moderate pain’ and 7–10 as ‘severe pain’. The pain interference score is calculated from the arithmetic mean of the scores attained on the seven questions of the Brief Pain Inventory. The site of pain is identified by asking respondents to show it in the diagram.
For the qualitative strand of the study, 10 IDIs were conducted among the participants with chronic musculoskeletal pain. Among them, three patients had severe pain; three had moderate pain; and four had mild pain according to the pain intensity scale of the Brief Pain Inventory. The participants were interviewed using a pre-tested, semi-structured interviewer guide. All IDIs were audiorecorded with prior consent obtained from the participants.
Statistical analysis
Quantitative data were analysed using SPSS (IBM Corp., Armonk, N.Y., USA, Version 28). Appropriate descriptive statistics were utilised for denoting the outcome variables as well as the independent variables. The Kruskal— Wallis test was used to compare the mean pain interference score among the categories of pain severity, with P<0.05 considered significant. After exclusion of multicollinearity (variance inflation factor of >5), the factors associated with chronic musculoskeletal pain among the participants were determined using a test of significance (P<0.05) via a univariate logistic regression analysis separately. All biologically plausible significant variables in the respective univariate analysis were included in the final multivariable models to estimate the adjusted odds ratios (aORs).
For the qualitative strand, the data obtained through the IDIs were simultaneously processed via a conventional thematic analysis in which themes and codes were explored. The records were listened to and transcribed verbatim using Microsoft Word version 16. The transcripts were read thoroughly; the important sentences were underlined; and the main ideas derived from them were labelled as codes. Appropriate codes were then placed under respective themes. The qualitative and quantitative strands of the study were integrated at the level of forming the research question, results and discussion.
Results
Of the 255 respondents, 145 (56.8%) reported having chronic musculoskeletal pain for 3 months or more. Among them, 61 (42%) were men, and 84 (58%) were women. As shown in Table 1, of all 255 participants, 141 (55.3%) were women, and 114 (44.7%) were men. The median age of the participants was 67 years (interquartile range=63–77 years). Approximately 45.8% (n=117) of the participants belonged to the young-old (60–69 years) age group, 44.7% to the old-old (70–79 years) age group and 9.5% to the very old (>80 years) age group. Of the total participants, 84.3% were Hindus, while 59.3% were living in a joint family. Approximately 26.7% had an educational level below primary school, and 39.2% belonged to socioeconomic class IV according to the modified B.G. Prasad Scale 2021.16
Table 1. Background characteristics of the respondents (N=255).
|
Parameter |
Categories |
Number (%) |
|---|---|---|
|
Age |
Young-old (60–69 years) |
117 (45.8) |
|
|
Older-old (70–79 years) |
114 (44.7) |
|
|
Oldest old (80 years and above) |
24 (9.5) |
|
Sex |
Female |
141 (55.3) |
|
|
Male |
114 (44.7) |
|
Religion |
Hindu |
215 (84.3) |
|
|
Muslim |
40 (15.7) |
|
Family |
Joint |
151 (59.3) |
|
|
Nuclear |
104 (40.7) |
|
Marital status |
Married |
145 (56.9) |
|
|
Widowed |
94 (36.8) |
|
|
Unmarried |
16 (6.3) |
|
Education$ |
Below primary |
68 (26.7) |
|
|
Primary |
57 (22.4) |
|
|
Middle |
49 (19.2) |
|
|
Secondary |
44 (17.2) |
|
|
Higher secondary |
25 (9.8) |
|
|
Graduate and above |
12 (4.7) |
|
Socio-economic status£ |
Class I (upper class) |
12 (4.7) |
|
|
Class II (upper middle class) |
17 (6.7) |
|
|
Class III (middle class) |
75 (29.4) |
|
|
Class IV (lower middle class) |
100 (39.2) |
|
|
Class V (lower class) |
51 (20) |
Below primary=illiterate and below the 5th standard, primary=passed the 5th standard, middle= passed the 8th standard, secondary=passed the 10th standard, higher secondary=passed the 12th standard
According to the B.G. Prasad Scale 2021
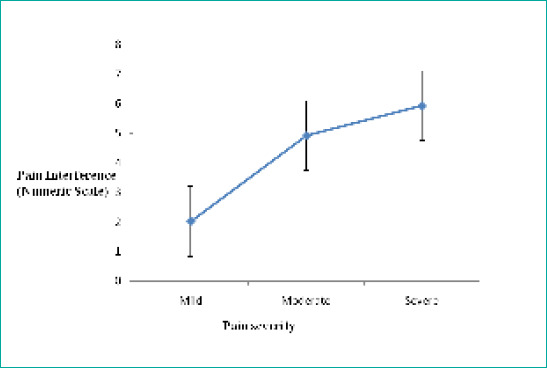
Among the study participants who reported having chronic musculoskeletal pain (n=145), 74.5% reported feeling it at a single location and 25.5% in multiple sites (Figure 1). The pain was most frequently located in the knee joint (49.6%), followed by the lower back (33.1%). Regarding the intensity, 52.4% reported mild pain; 33.4%, moderate pain; and 17.2%, severe pain. The mean pain intensity score among the total participants was 5.81. High pain interference scores were associated with greater pain intensity (Kruskal—Wallis H=75.56, P<0.001) (Figure 2).
Figure 1. Intensity of chronic pain among the male and female participants (n=l45).
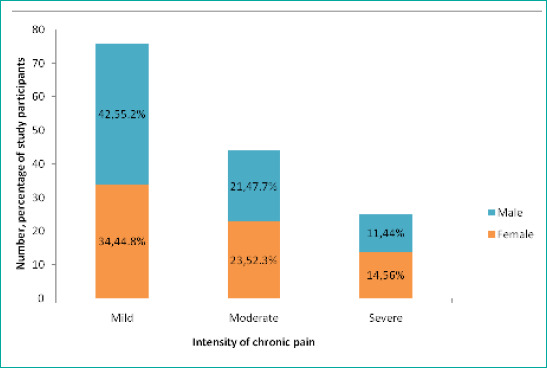
Figure 2. Pain interference in relation to pain severity (n=l45).
Regarding the knowledge of the participants on pain medication and its side effects, 51.2% of the total participants were found to have unsatisfactory knowledge (maximum score=5, minimum score=0, median score=3.62). A total of 117 (45.9%) elderly participants had used OTC medicines at least once in the past 3 months for any ailments. Among them, 82 (72.6%) were experiencing chronic musculoskeletal pain, all of whom had consumed OTC analgesics to alleviate their pain exacerbation.
Factors associated with chronic musculoskeletal pain among the participants
In the multivariable regression analysis model, four variables emerged as significantly associated with chronic musculoskeletal pain among the elderly individuals. These included age (aOR=5.16, 95% CI=2.2-13.5), comorbidity (aOR=7.47, 95% CI=3.2-17.5), use of OTC drugs (aOR=2.51, 95% CI=1.1–6.4) and depression (according to the Geriatric Depression Scale) (aOR=2.96, 95% CI=1.2–6.7). The non-significant Hosmer—Lemeshow test statistic (>0.05) indicated the goodness of fit of this model, and 46–63% of the variance of the outcome variable could be explained by this multivariable model (Cox and Snell’s R2=0.46, Nagelkerke’s R2=0.63) (Table 2).
Table 2. Multivariable logistic regression analysis of the determinants of chronic musculoskeletal pain (N=255).
|
Parameters |
Total no. (N=255) |
Chronic musculoskeletal pain present (n=145) |
Adjusted OR (95% CI) |
P-value$ |
|---|---|---|---|---|
|
Age | ||||
|
<70 years |
117 |
37 (32%) |
Ref (1) |
<0.001 |
|
≥70 years |
138 |
108 (78%) |
5.16 (2.2-13.5) |
|
|
Sex | ||||
|
Male |
114 |
61 (53%) |
Ref (1) |
0.501 |
|
Female |
141 |
84 (60%) |
1.21 (0.5-1.2) |
|
|
Comorbidity | ||||
|
Present |
146 |
111 (76%) |
7.47 (3.2-17.5) |
0.001 |
|
Absent |
109 |
34 (31.2%) |
Ref (1) |
|
|
Use of OTC drugs | ||||
|
Yes |
117 |
85 (72.6%) |
2.51 (1.1-5.8) |
0.025 |
|
No |
138 |
60 (43.5%) |
Ref (1) |
|
|
Lifestyle modification | ||||
|
Adopted |
46 |
32 (69.6%) |
1.52 (0.4-4.6) |
0.001 |
|
Not adopted |
209 |
113 (54%) |
Ref (1) |
|
|
Knowledge on pain medication and its side effects | ||||
|
Satisfactory |
95 |
63 (66.3%) |
1.34 (0.4-2.1) |
0.623 |
|
Unsatisfactory |
160 |
82 (51.2%) |
|
|
|
Depression £ | ||||
|
Present |
141 |
104 (73.8%) |
2.96 (1.2-6.7) |
0.001 |
|
Absent |
114 |
41 (36%) |
|
|
Hosmer—Lemeshow test statistic=0.76, Cox and Snell’s R2=0.46, Nagelkerke’s R2=0.63 CI: Confidence Interval Adjusted OR: Adjusted Odds Ratio
P<0.05 considered significant
According to the Geriatric Depression Scale
Qualitative exploratory findings
Through the IDIs, 10 participants (all with musculoskeletal pain persisting for 3 months or more: five elderly men and five elderly women) shared their perspectives on their experience with chronic musculoskeletal pain, its overall effect on lifestyle, their coping behaviour and perceived barriers to pain management.
The major theme that was generated through the qualitative exploration was barriers to the management of chronic musculoskeletal pain and its impact on quality of life, under which three major categories were found: i) behavioural barrier, ii) cognitive barrier and iii) physiological barrier.
Important codes emerged under the mentioned theme, which were aligned with the severity of pain. The participants with moderate and severe pain (n=6, including four elderly women and two elderly men; mean age=71.6 years) had similar responses. The major codes found from their interviews were as follows: i) dependency on pain medication; ii) physical inability to visit a health facility; iii) lack of knowledge; and iv) inability to help in household work. Meanwhile, the respondents with mild pain (n=4, including three men and one woman; mean age=65.6 years) had satisfactory knowledge regarding pain analgesics and were agile to move around and perform daily activities but lacked motivation to improve their lifestyle for preventing progression of pain towards chronicity, which yielded the extraction of a fifth code: v) lack of motivation to adopt lifestyle modifications (Table 3).
Table 3. Findings of the qualitative exploration through joint display.
|
Pain intensity* |
Interviewed patients with chronic pain |
Major categories |
Major qualitative codes |
Quotable quotes |
|---|---|---|---|---|
|
Severe and moderate |
6 (mean age=71.6 years) |
Physiological barrier |
Physical inability to visit a health facility |
‘Whenever my back pain increases, I send my grandson to buy analgesics from a local shop because at this age, it is impossible for me to visit a health centre and to wait for a long period’. (stated by an 81-year-old woman) |
|
Physiological barrier |
Inability to help in household chores |
“I was once very much active, but nowadays, I can’t help even a little in household works. Being this inactive makes me feel so down”. (stated by a 67-year-old woman) |
||
|
Cognitive barrier |
Lack of knowledge |
‘I think there is no harm in taking painkillers as long as the pain persists. To my knowledge, they have no side effects’. (stated by a 70-year-old woman) |
||
|
Behavioural barrier |
Dependency on pain medication |
“As long as I’m taking pain-killers, I get a little relief, but upon stopping medication, I feel the same pain again on both of my knees”. (stated by a 78-year-old man) |
||
|
Mild |
4 (mean age=65.6 years) |
Behavioural barrier |
Lack of motivation to adopt lifestyle modifications |
“One doctor told me to reduce weight and exercise. Initially, I tried for a few weeks, but nowadays, I don’t get much time to practice them”. (stated by a 62-year-old man) |
According to the Brief Pain Inventory (Short Form)
Discussion
This study estimated the prevalence of chronic pain and its associated factors among elderly individuals and simultaneously explored their perception about chronic pain and its management. The prevalence of chronic musculoskeletal pain among the respondents (age ≥60 years) was 56.8% in this study. The most commonly reported site of pain was the knee joint, followed by the lower back. Most participants had mild pain (52.4%), and pain interference in day-to-day life increased with increasing pain intensity.
Qualitative exploration revealed that most participants perceived chronic musculoskeletal pain as a major hindrance to daily activities they used to perform easily before. This was a particular perceived barrier that adversely affected their mental health. In addition, their insufficient knowledge of analgesics drove them towards pain-killer dependency instead of adopting lifestyle modifications. These findings evoke the need for cognitive behavioural interventions for pain management among elderly individuals.
The study conducted in the city of Goiania in Brazil by Pereira et al. showed a prevalence of chronic musculoskeletal pain of 52.8% among elderly individuals. Meanwhile, the present study reported a prevalence of 56.8%.17 It has been substantiated by some other population-based studies that women often have more propensity towards experiencing musculoskeletal pain than men.18 In the current study, although the prevalence of chronic pain was higher in the women (58%) than in the men (42%), no significant association was found between sex and chronic musculoskeletal pain in the multivariable regression model. Regarding the site of pain, the present study showed findings concordant to those of the study conducted by Panda et al. in Karnataka, India: The commonest sites of chronic pain were the lower back and knee.19
A study performed among an adult population in Poland reported that 91% of participants used OTC pain relievers.20 The current study reported that among all OTC drug users, those with chronic pain comprised the majority (72.6%). Another pan-Indian study conducted on chronic pain prevalence and treatment patterns by Dureja et al. showed that the majority (68%) of their respondents were treated with OTC medications.21
Among the four significant factors in the multivariable logistic regression model herein, the two most important were depression (according to the Geriatric Depression Scale) and presence of comorbidity. Some studies conducted previously worldwide have also showcased these two as major risk factors of chronic musculoskeletal pain. The study performed in Southern Germany by Bauer et al. indicated a fourfold risk of depressed mood (Geriatric Depression Scale-15 score of ≥5) in participants with chronic pain compared with that in participants with no pain.22 The narrative review conducted by Mills et al. on epidemiology and associated factors of chronic pain identified multimorbidity as an important determinant of chronic pain.23
The mixed-method study with an exploratory sequential design conducted in Tamilnadu, India, by Kirubakaran and Dongre showed that restriction of physical movements was a major perceived effect of chronic pain among elderly individuals.11 This is similar to the present finding that physical inability to visit a health facility and inability to help in household chores were perceived as physiological barriers.
This study carries certain limitations. Owing to the cross-sectional study design, no causal relationship could be established between the presence of chronic musculoskeletal pain and its risk factors. As the responses were mostly recall-based, bias is possible. Further, the biomedical cause of pain was not explored in the current study.
Conclusion
International law recognises pain management as a basic human right; nations are therefore ethically mandated to provide pain treatment as part of their core obligations under the right to health. In this context, the availability of drugs must be ensured to mitigate the complexity of elderly pain management, and services must be scaled up to provide non-pharmacological aids, such as physiotherapy, adequate mental support, elderly-friendly health facilities, generation of awareness on the perilous effects of consuming OTCs, curtailment of the dependency on analgesics and shift towards lifestyle modifications.
Supplementary tables
Table 1. Sites of chronic musculoskeletal pain among the study participants (n=145).
|
Sites* |
Men |
Women |
Total n (%) |
|---|---|---|---|
|
Neck |
1 |
3 |
4 (2.8) |
|
Shoulder |
5 |
7 |
12 (8.3) |
|
Upper limb |
6 |
9 |
15 (10.3) |
|
Lower back |
20 |
28 |
48 (33.1) |
|
Thigh |
6 |
4 |
10 (6.9) |
|
Knee |
14 |
58 |
72 (49.6) |
|
Calf muscle |
4 |
5 |
9 (6.2) |
|
Ankle |
1 |
5 |
6 (4.1) |
|
Foot |
3 |
9 |
12 (8.3) |
Multiple responses allowed
Table 2. Resp onses of the study participants regarding their knowledge about pain analgesics and side effects (N=255).
|
Questions |
Responses, n (%) |
||
|---|---|---|---|
|
Yes, n (%) |
No, n (%) |
Do not know, n (%) |
|
|
1. Name at least one pain-killer that you have heard of. |
89 (for correct answers) (35%) |
67 (for incorrect answers) (26.3%) |
99 (38.7%) |
|
2. One can use pain-killers as long as he/she wants. |
102 (40) |
86 (33.7) |
67 (26.3) |
|
3. Long-term use of pain-killers can cause gastric ulcer. |
65 (25.5) |
87 (34.1) |
103 (40.4) |
|
4. Long-term use of pain-killers can cause kidney dysfunction. |
45 (17.6) |
55 (21.6) |
155 (60.8) |
|
5. Consuming pain-killers may result in dependency. |
96 (37.6) |
82 (32.2) |
77 (30.2) |
Acknowledgement
The authors are grateful to the officer-in-charge and staff of the Rural Health Unit and Training Centre at Singur for their constant support and cooperation during the difficult pandemic phase throughout our study as well as to all respondents for their participation in this study.
Author Contributions
Dr. Trina Sengupta (Conceptualization/ Data curation / Formal Analysis/ Methodology/ Supervision/ Validation/ Visualization/ Writing — original draft / Publication Writing — review & editing)
Dr. Bobby Paul (Conceptualization/ Supervision/ Publication Writing — review & editing)
Dr. Ankush Banerjee (Data Analysis/ Supervision/ Publication Writing — review & editing)
Dr. Ranjan Das (Conceptualization/ Supervision/ Publication Writing — review & editing)
Dr. Riya Halder (Supervision/ Publication Writing - review & editing)
Ethical approval
All procedures in this study were conducted in accordance with the approved protocols of the Institutional Ethics Committee of All India Institute of Hygiene & Public Health. Written informed consent was obtained from the study participants for their anonymised information to be published in this article.
Conflicts of interest
The authors declare no potential conflicts of interest with respect to the research and authorship and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Data sharing statement
The raw data used in this study are available upon request to the corresponding author.
How does this paper make a difference in general practice?
This study focused holistically on chronic pain management among elderly individuals.
The findings emphasise the importance of lifestyle modifications alongside medications for pain management.
References
- 1.Jackson T, Thomas S, Stabile V, Shotwell M, Han X, McQueen K. A Systematic Review and Meta-Analysis of the Global Burden of Chronic Pain Without Clear Etiology in Low- and Middle- Income Countries: Trends in Heterogeneous Data and a Proposal for New Assessment Methods. [April 16; 2022 ];Anesth Analg. 2016 123(3):739–748. doi: 10.1213/ANE.0000000000001389. https://pubmed.ncbi.nlm.nih.gov/27537761/ [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Fact-Sheets About Musculoskeletal Conditions. Geneva: WHO; 2022. [April 2; 2022 ]. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions [Google Scholar]
- 3.Brooks P. Issues with chronic musculoskeletal pain. [April 6; 2022 ];Rheumatology (Oxford). 2005 44(7):831–833. doi: 10.1093/rheumatology/keh648. https://pubmed.ncbi.nlm.nih.gov/15840598/ [DOI] [PubMed] [Google Scholar]
- 4.Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders [published correction appears in J Pain. 2009 May;10(5):553. Demytteneare, K [added]] [April 5; 2022 ];J Pain. 2008 9(10):883–891. doi: 10.1016/j.jpain.2008.05.005. https://pubmed.ncbi.nlm.nih.gov/18602869/ [DOI] [PubMed] [Google Scholar]
- 5.Office of the Registrar General & Census Commissioner. Census of India (2011). New Delhi: 2011. [April 6; 2022 ]. https://censusindia.gov.in/nada/index.php/catalog/42619 [Google Scholar]
- 6.Hawker GA. The assessment of musculoskeletal pain. [April 7; 2022 ];Clin Exp Rheumatol. 2017 35 Suppl 107(5):8–12. https://pubmed.ncbi.nlm.nih.gov/28967361/ [PubMed] [Google Scholar]
- 7.Domenichiello AF, Ramsden CE. The silent epidemic of chronic pain in older adults. [April 10; 2022 ];Prog Neuropsychopharmacol Biol Psychiatry. 2019 93:284–290. doi: 10.1016/j.pnpbp.2019.04.006. https://pubmed.ncbi.nlm.nih.gov/31004724/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersson HI, Ejlertsson G, Leden I, Schersten B. Impact of chronic pain on health care seeking, self care, and medication. Results from a population-based Swedish study. [May 1; 2022 ];J Epidemiol Community Health. 1999 53(8):503–509. doi: 10.1136/jech.53.8.503. https://pubmed.ncbi.nlm.nih.gov/10562870/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilcox CM, Cryer B, Triadafilopoulos G. Patterns of use and public perception of over-the-counter pain relievers: focus on nonsteroidal antiinflammatory drugs. [May 3; 2022 ];J Rheumatol. 2005 32(11):2218–2224. https://pubmed.ncbi.nlm.nih.gov/16265706/ [PubMed] [Google Scholar]
- 10.Charan J, Biswas T. How to calculate sample size for different study designs in medical research?. [January 23; 2022 ];Indian J Psychol Med. 2013 35(2):121–126. doi: 10.4103/0253-7176.116232. https://pubmed.ncbi.nlm.nih.gov/24049221/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirubakaran S, Dongre AR. Chronic musculoskeletal pain among elderly in rural Tamil Nadu: Mixed-method study. [January 23; 2022 ];J Family Med Prim Care. 2019 8(1):77–85. doi: 10.4103/jfmpc.jfmpc_290_17. https://pubmed.ncbi.nlm.nih.gov/30911484/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skinner CJ. In: Probability Proportional to Size (PPS) Sampling. 1st ed. Balakrishnan N, Colton T, Everitt B, Piegorsch W, Ruggeri F, Teugels JL, editors. Wiley; 2016. [May 8; 2022 ]. Wiley StatsRef: Statistics Reference Online [Internet]. pp. 1–5.https://onlinelibrary.wiley.com/doi/10.1002/9781118445112.stat03346.pub2 [Google Scholar]
- 13.World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. Geneva: WHO; 2000. [April 2; 2022 ]. https://apps.who.int/iris/handle/10665/66154 [Google Scholar]
- 14.Lahiri A, Chakraborty A. Psychometric validation of geriatric depression scale - Short form among bengali-speaking elderly from a rural area of West Bengal: Application of item response theory. [January 24; 2022 ];Indian J Public Health. 2020 64(2):109–115. doi: 10.4103/ijph.IJPH_162_19. https://pubmed.ncbi.nlm.nih.gov/32584291/ [DOI] [PubMed] [Google Scholar]
- 15.Im DD, Jambaulikar GD, Kikut A, Gale J, Weiner SG. Brief Pain Inventory-Short Form: A New Method for Assessing Pain in the Emergency Department. Pain Med. 2020;21(12):3263–3269. doi: 10.1093/pm/pnaa269. https://pubmed.ncbi.nlm.nih.gov/32918473/ [DOI] [PubMed] [Google Scholar]
- 16.Majhi MM, Bhatnagar N. Updated B. G Prasad's classification for the year 2021: consideration for new base year 2016. [March 4; 2022 ];J Family Med Prim Care. 2021 10(11):4318–4319. doi: 10.4103/jfmpc.jfmpc_987_21. https://pubmed.ncbi.nlm.nih.gov/35136812/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pereira LV, de Vasconcelos PP, Souza LA, Pereira Gde A, Nakatani AY, Bachion MM. Prevalence and intensity of chronic pain and self-perceived health among elderly people: a population-based study. [April 6; 2022 ];Rev Lat Am Enfermagem. 2014 22(4):662–669. doi: 10.1590/0104-1169.3591.2465. https://pubmed.ncbi.nlm.nih.gov/25296151/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vieira EB, Garcia JB, Silva AA, Araujo RL, Jansen RC, Bertrand AL. Chronic pain, associated factors, and impact on daily life: are there differences between the sexes?. [April 8; 2022 ];Cad Saude Publica. 2012 28(8):1459–1467. doi: 10.1590/S0102-311X2012000800005. https://pubmed.ncbi.nlm.nih.gov/22892966/ [DOI] [PubMed] [Google Scholar]
- 19.Panda P, Vyas N, Dsouza SM, Boyanagari VK. Determinants of chronic pain among adults in urban area of Udupi, Karnataka, India. [April 9; 2022 ];Clin Epidemiol Glob Health. 2019 7(2):141–144. doi: 10.1016/j.cegh.2018.03.002. https://www.sciencedirect.com/science/article/abs/pii/S2213398418300162 [DOI] [Google Scholar]
- 20.Wojta-Kempa M, Krzyzanowski DM. Correlates of Abusing and Misusing Over-the-Counter Pain Relievers Among Adult Population of Wroclaw (Poland). [April 12; 2022 ];Adv Clin Exp Med. 2016 25(2):349–360. doi: 10.17219/acem/58887. https://pubmed.ncbi.nlm.nih.gov/27627570/ [DOI] [PubMed] [Google Scholar]
- 21.Dureja GP, Jain PN, Shetty N, et al. Prevalence of chronic pain, impact on daily life, and treatment practices in India. [April 15; 2022 ];Pain Pract. 2014 14(2):E51–E62. doi: 10.1111/papr.12132. https://pubmed.ncbi.nlm.nih.gov/24304963/ [DOI] [PubMed] [Google Scholar]
- 22.Bauer H, Emeny RT, Baumert J, Ladwig KH. Resilience moderates the association between chronic pain and depressive symptoms in the elderly. [May 2; 2022 ];Eur J Pain. 2016 20(8):1253–1265. doi: 10.1002/ejp.850. https://pubmed.ncbi.nlm.nih.gov/26914727/ [DOI] [PubMed] [Google Scholar]
- 23.Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. [May 2; 2022 ];Br J Anaesth. 2019 123(2):e273–e283. doi: 10.1016/j.bja.2019.03.023. https://pubmed.ncbi.nlm.nih.gov/31079836/ [DOI] [PMC free article] [PubMed] [Google Scholar]


