This cross-sectional study examines the health implications of physical, sexual, psychological, controlling behaviors, and economic abuse experienced by men.
Key Points
Question
Is men’s lifetime exposure to specific, any, and/or multiple types of intimate partner violence (IPV) associated with poor health outcomes?
Findings
In this cross-sectional study of 1355 ever-partnered men in New Zealand, exposure to IPV, particularly severe physical IPV, was associated with an increased likelihood of reporting poor health outcomes. However, associations with poor health were inconsistent, and a cumulative pattern by exposure to multiple types of IPV was not observed.
Meaning
Findings suggest that while men can experience IPV and its adverse health consequences, IPV against men does not consistently contribute to men’s poor health outcomes at the population level; gender-appropriate clinical approaches are needed if IPV against men is identified.
Abstract
Importance
Health implications of intimate partner violence (IPV) against men is relatively underexplored, although substantial evidence has identified associations between IPV and long-term physical health problems for women. Given the gendered differences in IPV exposure patterns, exploration of men’s IPV exposure and health outcomes using population-based samples is needed.
Objective
To assess the association between men’s lifetime IPV exposure and self-reported health outcomes.
Design, Setting, and Participants
This cross-sectional study analyzed data from the 2019 New Zealand Family Violence Study, which was conducted across 3 regions of New Zealand. The representative sample included ever-partnered men aged 16 years or older. Data analysis was performed between May and September 2022.
Exposures
Lifetime IPV against men by types (physical [severe or any], sexual, psychological, controlling behaviors, and economic abuse), any IPV (at least 1 type), and number of IPV types experienced.
Main Outcomes and Measures
The 7 health outcomes were poor general health, recent pain or discomfort, recent use of pain medication, frequent use of pain medication, recent health care consultation, any diagnosed physical health condition, and any diagnosed mental health condition.
Results
The sample comprised 1355 ever-partnered men (mean [SD] age, 51.3 [16.9] years), who predominantly identified as heterosexual (96.9%; 95% CI, 95.7%-97.8%). Half of the sample (49.9%) reported experiencing any lifetime IPV, of whom 62.1% reported at least 2 types. Of all sociodemographic subgroups, unemployed men had the greatest prevalence of reporting exposure to any IPV (69.2%) and all IPV types. After adjustment for sociodemographic factors, men’s exposure to any lifetime IPV was associated with an increased likelihood of reporting 4 of the 7 assessed health outcomes: poor general health (adjusted odds ratio [AOR], 1.78; 95% CI, 1.34-2.38), recent pain or discomfort (AOR, 1.65; 95% CI, 1.21-2.25), recent use of pain medication (AOR, 1.27; 95% CI, 1.00-1.62), and any diagnosed mental health condition (AOR, 1.66; 95% CI, 1.11-2.49). Specific IPV types were inconsistently associated with poor health outcomes. Any physical IPV exposure was associated with poor general health (AOR, 1.80; 95% CI, 1.33-2.43), recent pain or discomfort (AOR, 2.23; 95% CI, 1.64-3.04), and frequent use of pain medication (AOR, 1.69; 95% CI, 1.08-2.63), which appeared to be associated with exposure to severe physical IPV. Exposure to sexual IPV, controlling behaviors, and economic abuse was not associated with any assessed outcomes after sociodemographic adjustment. Experience of a higher number of IPV types did not show a clear stepwise association with number of health outcomes.
Conclusions and Relevance
Results of this study indicate that exposure to IPV can adversely affect men’s health but is not consistently a factor in men’s poor health at the population level. These findings do not warrant routine inquiry for IPV against men in clinical settings, although appropriate care is needed if IPV against men is identified.
Introduction
Intimate partner violence (IPV) is a global health and social issue that includes physical and psychological aggression, sexual coercion, and controlling behaviors within intimate relationships.1 As the most widespread type of violence against women in the world, IPV is considered a gendered issue.2 However, estimates suggest that approximately one-third of men also experience IPV in their lifetime.3 Intimate partner violence against men remains relatively underexplored in the literature, and existing research has often used small or nonrepresentative convenience samples.4,5,6,7 Furthermore, most research has gathered data on physical and/or sexual IPV exposure,8 whereas other IPV types (eg, psychological abuse and controlling behaviors) have been underassessed.9 Caution is needed about assumptions regarding similarities in the contexts and implications of IPV experienced by men and women, as evidence indicates that IPV patterns are gendered.4,5,10
While the health implications of men’s IPV exposure remain underexplored,7,11,12,13 evidence consistently shows that women’s IPV exposure is associated with a wide range of long-term physical (eg, cardiovascular, gynecological, endocrine, somatic, and neurological diseases) and mental (eg, depression, anxiety, suicide, and substance abuse) health issues.14,15,16,17,18 Limited research has examined IPV among gay and bisexual men, who have reported health outcomes of IPV that were similar to those reported by women who experienced violence from male partners,5 and has found greater implications of IPV in this population compared with heterosexual men.19 Globally, an estimated 40% to 70% of women who are murdered are killed by their intimate partners,20 and the proportion of homicides committed by an intimate partner is 6 times higher in homicides of women than men.21 The severity, frequency, and duration of IPV have been established as factors in worsened outcomes for women.14,20,22 Associations between trauma and physical health have been attributed to psychological, biological, social, and behavioral pathways.23,24,25 Stressors related to IPV are hypothesized to play a role in chronic inflammatory states, which can lead to adverse health outcomes.26,27 Posttraumatic stress disorder and depression, also associated with IPV severity and frequency, have been shown to play a role in worsened symptoms and progression of various health conditions and are purported to mediate between IPV and poor health.15,16,28,29
In research including men’s experiences, evidence suggests that IPV-related physical and mental health outcomes differ between men and women.10,11,12,30,31,32,33,34 For example, a 2005 study found that among those who were exposed to lifetime IPV, women reported a greater number of health issues (including cardiovascular diseases) than men and had larger effect sizes for most health conditions associated with IPV.31 A population-based US study35 found that men who were exposed to at least 1 type of IPV were considerably more likely to report 7 of 10 health conditions (excluding irritable bowel syndrome, diabetes, and hypertension), whereas women had increased risk for all 10 conditions. Another study36 indicated that men who were exposed to IPV were most likely to report externalized mental health issues such as behavioral disorders and substance use disorder, but women’s IPV experience was associated with a wider range of mental health outcomes.
Published findings from the population-based 2019 New Zealand Family Violence Study/He Koiora Matapopore (NZFVS)37 identified gendered differences in IPV exposure. It reported that men experienced fewer IPV acts than women: of those who experienced physical IPV, 8% of women reported more than 5 acts compared with less than 1% of men, and severe physical acts and injuries related to IPV were more prevalent in women. To determine if these gendered differences in patterns of IPV exposure differently altered health outcomes, IPV against men and its adverse health outcomes must be assessed separately from outcomes of IPV against women. This study sought to extend understanding and address the limitations of previous studies by assessing the association between men’s lifetime IPV exposure (disaggregated by IPV severity, IPV type, and cumulative exposure) and self-reported health outcomes using data from the NZFVS.
Methods
Methods for the 2019 NZFVS have been described elsewhere38 but are presented briefly herein. The NZFVS was a population-based retrospective cross-sectional survey based on the internationally standardized World Health Organization (WHO) Multi-Country Study on Women's Health and Domestic Violence Against Women questionnaire, which was adapted to the New Zealand context after consultation with governmental and expert advisors.38 The NZFVS was conducted from March 2017 to March 2019 across 3 regions, which accounted for approximately 40% of the New Zealand population and covered a range of ethnicities and urbanicity.38 This study adhered to the WHO ethical guidelines for the conduct of violence against women research. Ethics approval was granted by the University of Auckland Human Participants Ethics Committee.38 All participants provided written consent before the interview. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.39
Random sampling was conducted within primary sampling units, in which every second and sixth house from a random starting point was selected.38,40 Nonresidential and short-term residential properties, rest homes, and retirement villages were excluded. For survey discretion, only 1 randomly selected person per household was eligible to participate.38 Participants had to be 16 years of age or older, be able to speak conversational English, and have resided in the house for at least 4 nights a week for at least 1 month.38 Interviewers made up to 7 visits to each selected household to maximize recruitment.38
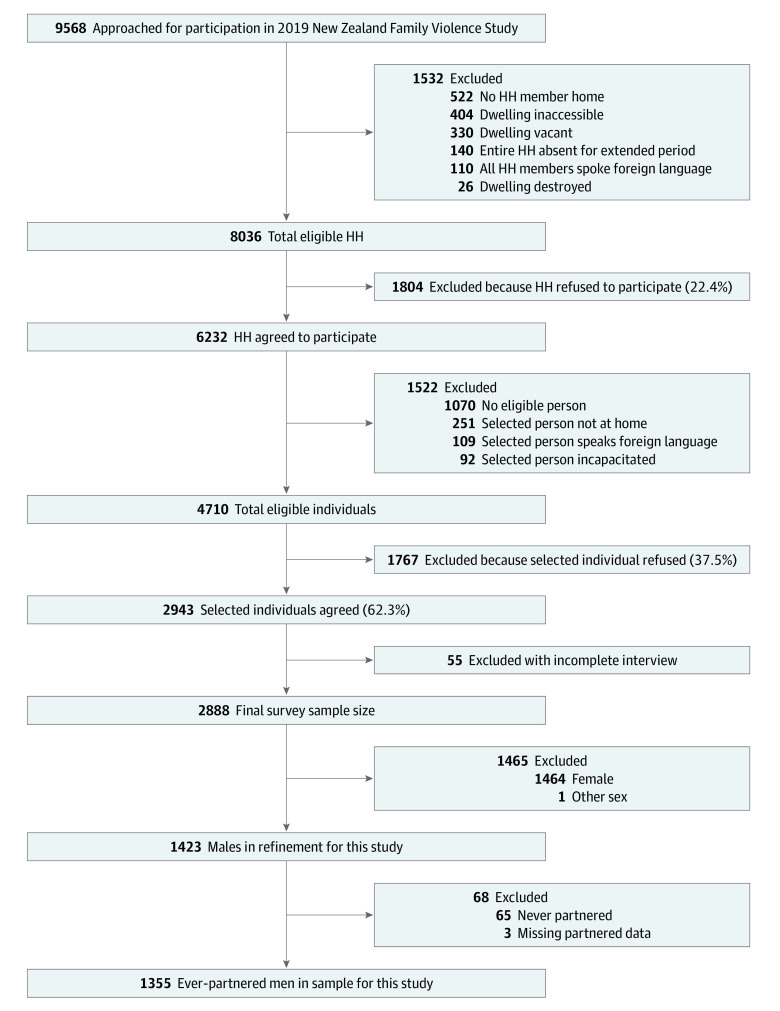
The NZFVS included complete interview data from 2887 total participants, including 1423 men, a response rate of 61.3% of the eligible men contacted (Figure). The ethnic and area deprivation composition of the NZFVS sample was closely representative of the New Zealand population, although Asian respondents, Māori men, and younger age groups were slightly underrepresented.38,41,42 For the present cross-sectional study, the data set was restricted to ever-partnered men (n = 1355), regardless of sexual orientation.
Figure. Flowchart of the 2019 New Zealand Family Violence Study Recruitment and Refinement for the Present Study Sample.
HH indicates household.
Seven self-reported health outcomes were assessed: poor general health, recent pain or discomfort, recent use of pain medication, frequent use of pain medication, recent health care consultation, any diagnosed physical health condition, and any diagnosed mental health condition. The responses were dichotomized (eTable in Supplement 1).
Participants’ exposure to IPV was assessed using questions pertaining to lifetime experience of violent behaviors of any current or previous partner (eTable in Supplement 1). Dichotomous variables (ever or never) were created for lifetime exposure (at least 1 act) to each of 5 IPV types (physical, sexual, psychological, controlling behaviors, and economic abuse). Physical IPV was disaggregated into moderate (eg, slapping and pushing) or severe (eg, kicking and choking) according to WHO classifications, which are based on the likelihood of inflicting injury.43 Severe physical IPV was defined as experiencing at least 1 severe physical behavior, whether or not moderate behaviors were present. Any lifetime IPV was defined as reported exposure to at least 1 IPV type. A count variable was produced for number of IPV types experienced (no exposure, 1, 2, 3, and 4 or 5).
Sociodemographic characteristics (age, prioritized ethnicity [including Asian; Māori; Middle Eastern, Latin American, and African; New Zealand European; and Pacific peoples], food security status, employment status, and educational level) were collected to examine the prevalence of health outcomes among population subgroups and to adjust for potential confounding in multivariable analyses (eTable in Supplement 1).
Statistical Analysis
All analyses were conducted in Stata, version 16.0 (StataCorp LLC).44 Survey functions were used to account for sampling methods by weighting data by the number of eligible participants in each household. There was less than 1% missing data for all exposure and outcome variables, except for economic abuse (1.9%).
Weighted proportions described the prevalence of IPV types by sociodemographic characteristics (Table 1) and exposure to multiple IPV types (Table 2 and Table 3). Bivariate and multivariable logistic regressions were run to calculate the odds of experiencing health outcomes for those who were exposed to different IPV types (compared with those who did not report experiencing each type), any IPV type (Table 2 and Table 3), and multiple IPV types (Table 4). Age and prioritized ethnicity were included in multivariable analyses to account for differences in health status across groups.45 Covariates for socioeconomic status (food security status, employment status, and educational level) improved model fit and were therefore included in multivariable analyses.
Table 1. Sociodemographic Characteristics and Prevalence of Lifetime IPV Exposure for Men in the 2019 New Zealand Family Violence Study.
| Characteristic | Participants, No. (%) | IPV type, No. (weighted %) | ||||||
|---|---|---|---|---|---|---|---|---|
| Physical | Sexual | Psychological | Controlling behaviors | Economic abuse | Any lifetime | |||
| Severe | Any | |||||||
| All participants | 1355 | 171 (12.8) | 391 (29.4) | 28 (2.1) | 545 (39.9) | 262 (20.2) | 158 (11.5) | 682 (49.9) |
| Age group, y | ||||||||
| 16-29 | 153 (15.6) | 23 (13.5) | 49 (29.6) | 8 (4.3) | 60 (35.0) | 43 (27.6) | 11 (4.9) | 76 (46.9) |
| 30-49 | 477 (34.0) | 54 (11.8) | 139 (29.0) | 8 (1.6) | 210 (44.2) | 99 (21.7) | 59 (12.7) | 258 (53.5) |
| 50-69 | 507 (36.7) | 81 (16.4) | 165 (34.5) | 11 (2.1) | 230 (45.1) | 102 (20.2) | 71 (14.6) | 279 (54.9) |
| ≥70 | 216 (13.7) | 13 (5.3) | 37 (16.2) | 1 (0.5) | 43 (20.3) | 17 (7.6) | 17 (7.7) | 67 (30.4) |
| Ethnicity | ||||||||
| Asian | 194 (17.4) | 14 (7.9) | 36 (21.6) | 1 (0.7) | 52 (28.3) | 34 (20.9) | 12 (6.5) | 72 (37.4) |
| Māori | 118 (8.9) | 29 (23.0) | 48 (37.2) | 6 (4.7) | 60 (46.0) | 35 (27.0) | 30 (25.9) | 68 (53.4) |
| Middle Eastern, Latin American, and African | 21 (1.5) | 1 (8.0) | 3 (16.7) | NA | 7 (41.7) | 6 (32.0) | 2 (8.0) | 8 (44.0) |
| New Zealand European | 940 (64.5) | 117 (13.2) | 282 (31.0) | 20 (2.3) | 396 (42.6) | 167 (18.2) | 102 (11.0) | 490 (52.4) |
| Pacific peoples | 80 (7.7) | 10 (10.1) | 22 (27.9) | 1 (0.8) | 30 (37.2) | 20 (25.6) | 12 (11.6) | 44 (55.0) |
| Educational level | ||||||||
| Primary and secondary | 578 (43.6) | 77 (13.6) | 162 (28.9) | 10 (1.8) | 217 (37.9) | 121 (20.9) | 72 (12.2) | 280 (48.9) |
| Tertiary | 774 (56.4) | 94 (12.3) | 229 (29.9) | 18 (2.3) | 328 (41.7) | 141 (19.8) | 86 (11.0) | 402 (50.9) |
| Food security status | ||||||||
| Secure | 1127 (82.6) | 126 (11.0) | 299 (26.9) | 18 (1.6) | 430 (37.8) | 195 (18.1) | 113 (10.0) | 542 (47.5) |
| Insecure | 219 (17.4) | 45 (21.9) | 90 (41.4) | 10 (4.6) | 113 (50.2) | 65 (29.8) | 44 (19.1) | 137 (61.8) |
| Employment status | ||||||||
| Student | 50 (5.8) | 2 (7.2) | 10 (20.6) | NA | 17 (28.9) | 11 (24.7) | 2 (2.2) | 21 (42.3) |
| Unemployed or houseworka | 81 (6.7) | 23 (31.5) | 33 (46.7) | 6 (8.4) | 43 (53.3) | 30 (36.5) | 24 (29.0) | 55 (69.2) |
| Employed | 973 (71.7) | 124 (12.3) | 296 (30.5) | 21 (2.0) | 412 (42.0) | 193 (20.2) | 109 (11.0) | 510 (51.6) |
| Retired | 249 (15.9) | 22 (9.5) | 52 (21.1) | 1 (0.4) | 73 (29.9) | 28 (12.2) | 23 (10.4) | 96 (38.0) |
Abbreviations: IPV, intimate partner violence; NA, not applicable.
Categories were combined due to low numbers reported for housework.
Table 2. Association Between Exposure to Physical and Sexual IPV and Health Outcomesa.
| Health outcome | No. of participants (weighted %) | Physical IPV | Sexual IPV | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Moderate | Severe | Any | |||||||
| OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | ||
| Poor general health | 293 (22.0) | 1.40 (0.99-1.97) | 1.34 (0.91-1.95) | 2.32 (1.60-3.37)c | 1.92 (1.32-2.80)c | 2.07 (1.56-2.75)c | 1.80 (1.33-2.43)c | 2.28 (1.03-5.06)c | 1.55 (0.58-4.17) |
| Recent pain or discomfort | 293 (20.0) | 1.66 (1.18-2.33)c | 1.71 (1.18-2.47)c | 2.65 (1.80-3.91)c | 2.03 (1.36-3.04)c | 2.50 (1.89-3.32)c | 2.23 (1.64-3.04)c | 3.24 (1.39-7.57)c | 2.10 (0.93-4.76) |
| Recent use of pain medication | 535 (38.0) | 1.09 (0.79-1.48) | 1.03 (0.75-1.42) | 1.58 (1.11-2.26)c | 1.33 (0.93-1.89) | 1.36 (1.06-1.74)c | 1.19 (0.93-1.53) | 1.29 (0.61-2.76) | 1.02 (0.50-2.08) |
| Frequent use of pain medication | 136 (9.1) | 1.24 (0.75-2.03) | 1.25 (0.75-2.08) | 2.23 (1.38-3.61)c | 1.76 (1.06-2.95)c | 1.90 (1.26-2.87)c | 1.69 (1.08-2.63)c | 0.97 (0.28-3.31) | 0.63 (0.15-2.57) |
| Recent health care consultation | 411 (28.4) | 0.91 (0.66-1.27) | 0.99 (0.70-1.39) | 1.39 (0.93-2.07) | 1.31 (0.89-1.95) | 1.14 (0.87-1.49) | 1.16 (0.88-1.52) | 1.07 (0.45-2.51) | 0.96 (0.39-2.34) |
| Any diagnosed physical health condition | 575 (39.8) | 0.96 (0.68-1.35) | 1.02 (0.72-1.45) | 1.27 (0.89-1.81) | 1.20 (0.82-1.76) | 1.11 (0.86-1.45) | 1.13 (0.86-1.49) | 1.36 (0.60-3.09) | 1.44 (0.65-3.15) |
| Any diagnosed mental health condition | 140 (9.6) | 1.14 (0.72-1.81) | 1.04 (0.64-1.68) | 2.26 (1.41-3.64)c | 1.55 (0.97-2.47) | 1.81 (1.24-2.65)c | 1.36 (0.92-1.99) | 4.14 (1.65-10.37)c | 2.17 (0.94-5.00) |
Abbreviations: AOR, adjusted odds ratio; IPV, intimate partner violence; OR, odds ratio.
Reference for each IPV type was no exposure to this type.
Adjusted for age, ethnicity, food security status, employment status, and educational level.
Statistically significant at P < .05.
Table 3. Association Between Exposure to Psychological, Controlling, and Economic IPV and Health Outcomesa.
| Health outcome | No. of participants (weighted %) | Psychological IPV | Controlling behaviors | Economic abuse | Any lifetime IPV | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | ||
| Poor general health | 293 (22.0) | 1.94 (1.45-2.59)c | 1.87 (1.38-2.53)c | 1.55 (1.10-2.17)c | 1.26 (0.88-1.81) | 1.82 (1.21-2.73)c | 1.47 (0.98-2.21) | 1.89 (1.42-2.52)c | 1.78 (1.34-2.38)c |
| Recent pain or discomfort | 293 (20.0) | 1.50 (1.12-2.00)c | 1.30 (0.95-1.77) | 1.28 (0.91-1.81) | 1.20 (0.83-1.73) | 1.58 (1.06-2.36)c | 1.16 (0.75-1.79) | 1.85 (1.39-2.46)c | 1.65 (1.21-2.25)c |
| Recent use of pain medication | 535 (38.0) | 1.34 (1.05-1.70)c | 1.11 (0.86-1.44) | 1.16 (0.85-1.58) | 1.13 (0.83-1.54) | 1.37 (0.96-1.96) | 1.03 (0.72-1.47) | 1.51 (1.20-1.90)c | 1.27 (1.00-1.62)c |
| Frequent use of pain medication | 136 (9.1) | 1.07 (0.71-1.61) | 0.94 (0.60-1.46) | 1.02 (0.62-1.69) | 1.01 (0.61-1.67) | 1.14 (0.64-2.02) | 0.71 (0.39-1.28) | 1.14 (0.76-1.72) | 0.99 (0.63-1.54) |
| Recent health care consultation | 411 (28.4) | 1.20 (0.93-1.54) | 1.28 (0.98-1.68) | 1.09 (0.77-1.54) | 1.21 (0.87-1.69) | 1.49 (1.03-2.14)c | 1.26 (0.87-1.82) | 1.16 (0.90-1.49) | 1.24 (0.95-1.61) |
| Any diagnosed physical health condition | 575 (39.8) | 1.07 (0.85-1.34) | 1.15 (0.89-1.47) | 0.88 (0.65-1.19) | 1.04 (0.76-1.42) | 1.27 (0.89-1.80) | 1.06 (0.72-1.57) | 1.08 (0.85-1.37) | 1.17 (0.91-1.52) |
| Any diagnosed mental health condition | 140 (9.6) | 2.05 (1.44-2.93)c | 1.56 (1.09-2.25)c | 1.76 (1.14-2.73)c | 1.50 (0.97-2.32) | 1.40 (0.84-2.33) | 0.97 (0.57-1.66) | 2.15 (1.46-3.16)c | 1.66 (1.11-2.49)c |
Abbreviations: AOR, adjusted odds ratio; IPV, intimate partner violence; OR, odds ratio.
Reference for each IPV type was no exposure to this type.
Adjusted for age, ethnicity, food security status, employment status, and educational level.
Statistically significant at P < .05.
Table 4. Association Between Number of IPV Types Experienced and Health Outcomesa.
| Health outcome | Number of IPV types | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 or 5 | |||||
| OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | OR (95% CI) | AOR (95% CI)b | |
| Poor general health | 1.56 (1.09-2.22)c | 1.64 (1.13-2.38)c | 1.81 (1.22-2.69)c | 1.83 (1.23-2.71)c | 1.92 (1.17-3.17)c | 1.51 (0.86-2.64) | 3.45 (2.03-5.86)c | 2.62 (1.51-4.55)c |
| Recent pain or discomfort | 1.65 (1.13-2.40)c | 1.56 (1.04-2.34)c | 1.61 (1.09-2.37)c | 1.51 (1.02-2.25)c | 2.15 (1.32-3.49)c | 1.94 (1.14-3.30)c | 2.84 (1.67-4.81)c | 1.95 (1.07-3.57)c |
| Recent use of pain medication | 1.76 (1.29-2.39)c | 1.48 (1.06-2.05)c | 1.38 (0.97-1.97) | 1.19 (0.84-1.68) | 0.99 (0.64-1.54) | 0.89 (0.56-1.43) | 2.15 (1.32-3.51) | 1.51 (0.94-2.44) |
| Frequent use of pain medication | 0.93 (0.51-1.68) | 0.83 (0.44-1.55) | 1.19 (0.69-2.07) | 1.11 (0.62-1.98) | 1.24 (0.64-2.37) | 1.08 (0.51-2.30) | 1.58 (0.75-3.33) | 1.08 (0.51-2.32) |
| Recent health care consultation | 1.19 (0.84-1.70) | 1.26 (0.88-1.81) | 0.90 (0.63-1.29) | 1.00 (0.69-1.44) | 1.35 (0.83-2.21) | 1.54 (0.93-2.53) | 1.58 (0.96-2.62) | 1.48 (0.90-2.44) |
| Any diagnosed physical health condition | 1.10 (0.80-1.51) | 1.18 (0.84-1.66) | 1.04 (0.74-1.48) | 1.17 (0.83-1.65) | 0.99 (0.65-1.53) | 1.19 (0.74-1.92) | 1.22 (0.76-1.95) | 1.12 (0.66-1.90) |
| Any diagnosed mental health condition | 1.84 (1.13-3.01)c | 1.61 (0.93-2.78) | 2.20 (1.31-3.69)c | 1.76 (1.04-2.97)c | 2.08 (1.08-4.01)c | 1.46 (0.79-2.69) | 3.18 (1.68-6.04)c | 1.87 (0.92-3.79) |
Abbreviations: AOR, adjusted odds ratio; IPV, intimate partner violence; OR, odds ratio.
Reference was no exposure (n = 667 [50.1%, weighted]).
Adjusted for age, ethnicity, food security status, employment status, and educational level.
Statistically significant at P < .05.
Results are reported herein with 95% CIs. Statistical significance was set at P < .05. Data analysis was performed between May and September 2022.
Results
A total of 1355 ever-partnered men, with a mean (SD) age of 51.3 (16.9) years, were included in the analysis. The sample predominantly identified as heterosexual (96.9%; 95% CI, 95.7%-97.8%) and was composed of 17.4% Asian; 8.9% Māori; 1.5% Middle Eastern, Latin American, and African; 64.5% New Zealand European; and 7.7% Pacific men. Sociodemographic characteristics of the sample are presented in Table 1.
Prevalence rates were 29.4% for physical IPV, 39.9% for psychological IPV, 2.1% for sexual IPV, 20.2% for controlling behaviors, and 11.5% for economic abuse. Half (49.9%) of the sample reported experiencing any of the 5 IPV types in their lifetime (Table 1). Among men with exposure to any IPV, the weighted percentage exposed to 1 type was 37.9%, 32.5% to 2 types, 17.5% to 3 types, and 12.2% to 4 or 5 types (Table 4). Of the full sample, 18.9% of men experienced 1 type of IPV, 16.2% experienced 2 types, 8.7% experienced 3 types, and 6.1% experienced 4 or 5 types (Table 4).
Men in the oldest age group (≥70 years) had the lowest prevalence of reporting exposure to any IPV (30.4%) and each IPV type, aside from economic abuse (Table 1). Pacific men had the highest prevalence of reporting any IPV exposure (55.0%), and Māori men had the highest prevalence of reported experience of each IPV type, except for economic abuse (Table 1). Asian men had the lowest prevalence of exposure to any IPV (37.5%) compared with respondents of other ethnicities. Of all sociodemographic subgroups, men who were unemployed or did housework had the greatest prevalence of reporting exposure to any IPV (69.2%) and each IPV type (Table 1). Due to a low number of nonheterosexual participants, analyses could not be run by sexual orientation subgroups. However, it is important to note that sexual IPV was disproportionately experienced by those who identified as either gay, bisexual, or other sexual identity (14.6%), and all other IPV types were experienced proportionately (approximately 3% of those with gay, bisexual, or other sexual identity).
Regardless of IPV exposure, the most common health outcome reported was any diagnosed physical health condition (39.8%), and 28.4% of men recently consulted a health care professional (Table 2). The least prevalent health outcome was frequent use of pain medication (9.1%).
Health outcomes were more prevalent among men 50 years or older, Māori and Pacific men, those with primary and secondary educational level, and those with food insecurity. For example, a diagnosed physical health condition was reported by 54.8% of men 50 years or older (vs 24.7% of those younger than 50 years), by 49.8% of Māori men (vs 44.1% of New Zealand European; 36.7% of Pacific; 32.0% of Middle Eastern, Latin American, or African; and 21.0% of Asian men), and by 46.2% of men with food insecurity status (vs 38.5% of those with food security).
Men’s exposure to severe physical IPV was associated with reports of poor general health (adjusted odds ratios [AOR], 1.92; 95% CI, 1.32-2.80), recent pain or discomfort (AOR, 2.03; 95% CI, 1.36-3.04), and frequent use of pain medication (AOR, 1.76; 95% CI, 1.06-2.95) (Table 2). Experience of moderate physical IPV was associated with increased likelihood of reporting recent pain or discomfort (AOR, 1.71; 95% CI, 1.18-2.47) but no other assessed health outcomes (Table 2).
Of the 5 IPV types, exposure to physical IPV was associated with the highest count of health outcomes (3) after adjustment for sociodemographic characteristics: poor general health (AOR, 1.80; 95% CI, 1.33-2.43), recent pain or discomfort (AOR, 2.23; 95% CI, 1.64-3.04), and frequent use of pain medication (AOR, 1.69; 95% CI, 1.08-2.63) (Table 2). Experience of psychological IPV was associated with increased likelihood of poor general health (AOR, 1.87; 95% CI, 1.38-2.53) and any diagnosed mental health condition (AOR, 1.56; 95% CI, 1.09-2.25) (Table 3). After adjustment for sociodemographic characteristics, exposure to controlling behaviors, sexual IPV, and economic abuse was not associated with any assessed health outcomes. After adjustment for sociodemographic characteristics, any lifetime IPV was associated with experiencing 4 of the 7 assessed health outcomes: poor general health (AOR, 1.78; 95% CI, 1.34-2.38), recent pain or discomfort (AOR, 1.65; 95% CI, 1.21-2.25), recent use of pain medication (AOR, 1.27; 95% CI, 1.00-1.62), and any diagnosed mental health condition (AOR, 1.66; 95% CI, 1.11-2.49) (Table 3).
There was minimal evidence of a cumulative association between number of IPV types experienced and health outcomes (Table 4). Exposure to recent pain or discomfort was the only health outcome associated with each number of IPV types. However, a clear stepwise association was not evident as AORs ranged from 1.51 (95% CI, 1.02-2.25) for exposure to 2 IPV types, to 1.56 (95% CI, 1.04-2.34) for 1 type, to 1.94 (95% CI, 1.14-3.30) for 3 types, and to 1.95 (95% CI, 1.07-3.57) for 4 or 5 types. Compared with those who were unexposed to IPV, men experiencing 4 or 5 IPV types were also significantly more likely to report poor general health (AOR, 2.62; 95% CI, 1.51-4.55).
Discussion
Prevalence rates of exposure to IPV against men in this study were slightly higher than in other studies. A review article46 found that prevalence rates ranged from 3.4% to 20.3% for physical IPV (29.4% in this sample), 7.3% to 37% for psychological IPV (39.9% in this sample), and 0.2% to 7% for sexual violence (2.1% in this sample).
Overall, exposure to any lifetime IPV against men was associated with increased likelihood of self-reporting 4 of the 7 assessed health outcomes. However, specific IPV types were inconsistently associated with poor health outcomes. Participants who reported exposure to any physical IPV had the greatest number of associations with the 7 assessed health outcomes. These associations appeared to be associated with exposure to severe, as opposed to moderate, physical IPV. Experiences with sexual IPV, controlling behaviors, and economic abuse were not associated with any of the assessed outcomes after adjustment for sociodemographic factors. While exposure to increasing numbers of IPV types did not clearly show a stepwise association with health outcomes, exposure to 4 or 5 IPV types was associated with an approximately 2-fold increased likelihood of reporting poor general health and recent pain or discomfort.
By comparison, a companion study to the 2019 NZFVS found evidence of associations between women’s lifetime IPV exposure and increased likelihood of reporting poor health outcomes across all specific IPV types (B. M. Mellar, MPH, unpublished data, 2022). Together, these findings support the assertions that IPV exposure affects the health of men and women differently and to varying degrees.10,11,12,30,31,32,33,34
The different health consequences observed for men and women with IPV exposure may be explained by gendered differences in the nature of the violence experienced.10 The present findings reinforce the results of a previous study35 that men’s exposure to severe physical violence was associated with increased odds of reporting a number of health conditions. Severe physical IPV entails acts that are more likely to inflict injuries or gradual bodily harm, which may be directly related to various health conditions.16,47 In the NZFVS, 43.7% of men who were exposed to any physical IPV were exposed to severe physical acts compared with 58.7% of women (B. M. Mellar, MPH, unpublished data, 2022). These results support previous evidence suggesting that men may be primarily subjected to moderate violent acts, whereas women are at increased risk of experiencing severe physical IPV.3,6,7,48 Similarly, a US population-based study found that differential patterns of abuse were associated with differences in health outcomes between men and women; women were over twice as likely to experience systematic abuse, defined by severe physical IPV and multiple IPV types, which conferred substantially increased risk for adverse health outcomes.10 Furthermore, lower reported prevalence of severe physical IPV among men may also signal less exposure to other IPV types (particularly sexual IPV),49,50 which may partially explain the fewer observed associations with health outcomes.
Psychological IPV has been posited as the most common type of IPV experienced by men,5,30 a finding supported by data from the present study. However, exposure to psychological IPV was associated with only 2 of the assessed health outcomes (poor general health and any diagnosed mental health condition) in the present study; psychological IPV was the only type associated with reporting of any diagnosed mental health condition. These associations are consistent with those reported in limited research on men’s experience of psychological IPV.13,30 For women, a greater number of associations were found between psychological IPV and health outcomes, which may be due to differences in the co-occurrence of IPV types experienced by men and women (B. M. Mellar, MPH, unpublished data, 2022). Women likely experience psychological IPV in combination with other IPV types,51 which may compound health consequences; however, the same may not be true for men. It is also possible that men were more likely to report infrequent or sporadic occurrences of IPV behaviors, whereas women’s reports of IPV may have identified chronic patterns of IPV that are associated with worse health outcomes.
Compared with men, women are more likely to experience IPV types that have been associated with worse health outcomes, including sexual IPV, controlling behaviors, and stalking.12,52,53 Experience of these IPV types and injurious acts likely contribute to findings that women are more likely to report fearing their violent partners.12,33,53,54 This claim is corroborated by the NZFVS findings, with a substantially higher proportion of women than men reporting being afraid of their partner (7.7% vs 1.5%; P < .001).37 Fear (or perceived danger)48 may play a key role in the development of posttraumatic stress disorder and associated outcomes, thus leading to worse health consequences for women with exposure to IPV.12 A qualitative study55 found that males who experienced IPV did not consider physical violence by women threatening and believed they were not subjected to coercive control tactics. In the present study, exposure to at least 1 controlling behavior was reported by 20.2% of men but was not associated with any health outcomes. In contrast, studies (including the NZFVS) exploring women’s exposure to controlling behaviors have found this IPV type to be consistently associated with numerous poor health outcomes (B. M. Mellar, MPH, unpublished data, 2022).56 This finding further substantiates claims that experience of controlling behaviors is a highly gendered phenomenon, and dynamics of power and control (which often underpin other IPV types) may play a crucial role in the differences in health outcomes between men and women who experience violent acts.57,58
Evidence suggests that exposure to multiple types of IPV (and other forms of violence) has a dose-response association with or cumulative implication for health outcomes.20,35 In the present study, a clear cumulative pattern was not observed with additional counts of IPV types reported by men, including for mental health conditions. This finding is in contrast to results of previous research.32 Of men who experienced any IPV in this study, 12.2% reported experiencing 4 or 5 IPV types. In the NZFVS, of the women who experienced IPV, 20.7% experienced 4 or 5 IPV types, and a strong cumulative pattern was observed (ie, significantly associated with all 7 health outcomes) (B. M. Mellar, MPH, unpublished data, 2022). The lower number of men who reported experiencing multiple IPV types in the present study may reflect a lower prevalence of such exposure in the wider population. This finding would contribute to the statistical failure of these IPV number groupings to be associated with health consequences, as the likelihood of type II error increases. In clinical practice, men who are exposed to multiple IPV types may experience worsened health outcomes, but this study did not find associations between multiple IPV exposures and disease burden at the population level.
Research has found that violence perpetrated by women is primarily retaliatory (rather than systematic) and motivated by self-defense and fear of their male partners.4,6,52,53,59 This pattern may help to explain the minimal implications for health outcomes observed in men who reported IPV exposure despite similar IPV prevalence for men and women.10
Strengths and Limitations
This study addressed a global gap in research on associations between IPV against men and their self-reported health outcomes. We purposefully designed this analysis to address underexplored IPV types using stringent sampling and data collection methods as well as a pretested and robust questionnaire based on the WHO Multi-Country Study on Women's Health and Domestic Violence Against Women. To our knowledge, this study was the first to explore the prevalence and health implications of IPV among men in New Zealand. The community-based sample reflected the broader New Zealand population, and not just those seeking help from health care or IPV support services.
Among the limitations of the study was that several sampling factors may have led to an underestimation of the prevalence of IPV, such as exclusion of inaccessible housing, men who could not speak English, and men residing in facilities such as prisons.38 While the NZFVS data collection was conducted in compliance with WHO’s recommendations for maximizing participant safety and disclosure,60 recall or social desirability biases may have compromised self-reported measures, including IPV exposure.22 Biases may be a particular issue for men’s IPV disclosure, as some research has indicated that men may underreport IPV against men due to stereotypes of masculinity and fears of ridicule.6 Furthermore, men may be less likely to seek health care than women,61,62 thus reflecting the lower prevalence of recent health care consultation, use of medication, and diagnoses of physical and mental conditions in the present study. The study possibly captured a relatively healthy sample by excluding those in rest homes and hospitals given that those who were unwell may have been less likely to participate, thus underestimating the prevalence of health outcomes. A few point estimates may be imprecise due to wide CIs. Furthermore, correlation does not equal causation; it is possible that those with poor health are more likely to experience IPV.
Use of single-measure thresholds (at least 1 act) for each IPV type may have captured sporadic occurrences rather than systematic patterns of violence or control. Other studies have suggested distinctions between typologies of situational couple violence and intimate terrorism.63 At present, there is lack of consensus in the field regarding when psychologically aggressive acts meet the thresholds for being defined as IPV.11,64 Analyses of the implications of specific IPV types for health are indicative, but independent associations could not be examined as different types often co-occur. Furthermore, this study did not differentiate between current and historical IPV, partner and nonpartner violence,5,65 or sexual orientation. Future research exploring IPV against men with diverse sexual identities is warranted, particularly for IPV-related behaviors that are unique to these groups.66
Conclusions
In this cross-sectional study, although men and women experienced different health outcomes of IPV, men’s exposure to IPV can still have adverse health consequences. The findings suggest that IPV exposure may not consistently contribute to the poor health of men at the population level and that routine inquiry for IPV against men is not warranted in clinical settings. However, appropriate care and services are needed if IPV against men is identified. While gender-appropriate needs should be factored into the design and delivery of violence prevention and intervention strategies, the nuances and complexity of relationship contexts and individual life spans must be considered with sensitivity to ensure safety and appropriate care for all who experience violence.
eTable. Variable Questions and Definitions From the 2019 New Zealand Family Violence Study Used in Analysis
Data Sharing Statement
References
- 1.World Health Organization . Intimate partner violence. Violence Info. Accessed October 21, 2021. https://apps.who.int/violence-info/intimate-partner-violence
- 2.World Health Organization . Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. 2021. Accessed February 1, 2022. https://apps.who.int/iris/handle/10665/341337
- 3.Rivara F, Adhia A, Lyons V, et al. The effects of violence on health. Health Aff (Millwood). 2019;38(10):1622-1629. doi: 10.1377/hlthaff.2019.00480 [DOI] [PubMed] [Google Scholar]
- 4.Fanslow JL, Hashemi L, Gulliver P, McIntosh T. Gender patterns in the use of physical violence against a violent partner: results of a cross-sectional population-based study in New Zealand. J Interpers Violence. 2022;37(23-24):NP22890-NP22920. doi: 10.1177/08862605211073094 [DOI] [PubMed] [Google Scholar]
- 5.Scott-Storey K, O’Donnell S, Ford-Gilboe M, et al. What about the men? a critical review of men’s experiences of intimate partner violence. Trauma Violence Abuse. 2022. Published online January 30, 2022. doi: 10.1177/15248380211043827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carmo R, Grams A, Magalhães T. Men as victims of intimate partner violence. J Forensic Leg Med. 2011;18(8):355-359. doi: 10.1016/j.jflm.2011.07.006 [DOI] [PubMed] [Google Scholar]
- 7.Reid RJ, Bonomi AE, Rivara FP, et al. Intimate partner violence among men prevalence, chronicity, and health effects. Am J Prev Med. 2008;34(6):478-485. doi: 10.1016/j.amepre.2008.01.029 [DOI] [PubMed] [Google Scholar]
- 8.Devries KM, Mak JYT, García-Moreno C, et al. Global health: the global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527-1528. doi: 10.1126/science.1240937 [DOI] [PubMed] [Google Scholar]
- 9.Fanslow J, Malihi Z, Hashemi L, Gulliver P, McIntosh T. Change in prevalence of psychological and economic abuse, and controlling behaviours against women by an intimate partner in two cross-sectional studies in New Zealand, 2003 and 2019. BMJ Open. 2021;11(3):e044910. doi: 10.1136/bmjopen-2020-044910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carbone-López K, Kruttschnitt C, Macmillan R. Patterns of intimate partner violence and their associations with physical health, psychological distress, and substance use. Public Health Rep. 2006;121(4):382-392. doi: 10.1177/003335490612100406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayes BE, Kopp PM. Gender differences in the effect of past year victimization on self-reported physical and mental health: findings from the 2010 National Intimate Partner and Sexual Violence Survey. Am J Crim Justice. 2020;45(2):293-312. doi: 10.1007/s12103-019-09510-7 [DOI] [Google Scholar]
- 12.Caldwell JE, Swan SC, Woodbrown VD. Gender differences in intimate partner violence outcomes. Psychol Violence. 2012;2(1):42-57. doi: 10.1037/a0026296 [DOI] [Google Scholar]
- 13.Dokkedahl SB, Kirubakaran R, Bech-Hansen D, Kristensen TR, Elklit A. The psychological subtype of intimate partner violence and its effect on mental health: a systematic review with meta-analyses. Syst Rev. 2022;11(1):163. doi: 10.1186/s13643-022-02025-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stubbs A, Szoeke C. The effect of intimate partner violence on the physical health and health-related behaviors of women: a systematic review of the literature. Trauma Violence Abuse. 2022;23(4):1157-1172. doi: 10.1177/1524838020985541 [DOI] [PubMed] [Google Scholar]
- 15.Dillon G, Hussain R, Loxton D, Rahman S. Mental and physical health and intimate partner violence against women: a review of the literature. Int J Family Med. 2013;2013:313909. doi: 10.1155/2013/313909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331-1336. doi: 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- 17.Bonomi AE, Thompson RS, Anderson M, et al. Intimate partner violence and women’s physical, mental, and social functioning. Am J Prev Med. 2006;30(6):458-466. doi: 10.1016/j.amepre.2006.01.015 [DOI] [PubMed] [Google Scholar]
- 18.El-Serag R, Thurston RC. Matters of the heart and mind: interpersonal violence and cardiovascular disease in women. J Am Heart Assoc. 2020;9(4):e015479. doi: 10.1161/JAHA.120.015479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J, Walters ML, Gilbert LK, Patel N. Sexual violence, stalking, and intimate partner violence by sexual orientation, United States. Psychol Violence. 2020;10(1):110-119. doi: 10.1037/vio0000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano RE, eds. World Report on Violence and Health. World Health Organization; 2002. doi: 10.1016/S0140-6736(02)11133-0 [DOI] [Google Scholar]
- 21.Stöckl H, Devries K, Rotstein A, et al. The global prevalence of intimate partner homicide: a systematic review. Lancet. 2013;382(9895):859-865. doi: 10.1016/S0140-6736(13)61030-2 [DOI] [PubMed] [Google Scholar]
- 22.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C; WHO Multi-country Study on Women’s Health and Domestic Violence Against Women Study Team . Intimate partner violence and women’s physical and mental health in the WHO Multi-country Study on women’s health and domestic violence: an observational study. Lancet. 2008;371(9619):1165-1172. doi: 10.1016/S0140-6736(08)60522-X [DOI] [PubMed] [Google Scholar]
- 23.Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl. 2002;26(6-7):715-729. doi: 10.1016/S0145-2134(02)00343-5 [DOI] [PubMed] [Google Scholar]
- 24.Black MC. Intimate partner violence and adverse health consequences: implications for clinicians. Am J Lifestyle Med. 2011;5(5):428-439. doi: 10.1177/1559827611410265 [DOI] [Google Scholar]
- 25.Schnurr PP, Green BL. A context for understanding the physical health consequences of exposure to extreme stress. In: Schnurr PP, Green BL, eds. Trauma and Health: Physical Health Consequences of Exposure to Extreme Stress. American Psychological Association; 2004:3-10. doi: 10.1037/10723-001 [DOI] [Google Scholar]
- 26.Liu X, Logan J, Alhusen J. Cardiovascular risk and outcomes in women who have experienced intimate partner violence: an integrative review. J Cardiovasc Nurs. 2020;35(4):400-414. doi: 10.1097/JCN.0000000000000654 [DOI] [PubMed] [Google Scholar]
- 27.Scott-Storey K. Cumulative abuse: do things add up? an evaluation of the conceptualization, operationalization, and methodological approaches in the study of the phenomenon of cumulative abuse. Trauma Violence Abuse. 2011;12(3):135-150. doi: 10.1177/1524838011404253 [DOI] [PubMed] [Google Scholar]
- 28.Dutton MA, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21(7):955-968. doi: 10.1177/0886260506289178 [DOI] [PubMed] [Google Scholar]
- 29.Coker AL, Weston R, Creson DL, Justice B, Blakeney P. PTSD symptoms among men and women survivors of intimate partner violence: the role of risk and protective factors. Violence Vict. 2005;20(6):625-643. doi: 10.1891/0886-6708.20.6.625 [DOI] [PubMed] [Google Scholar]
- 30.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260-268. doi: 10.1016/S0749-3797(02)00514-7 [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC) . Adverse health conditions and health risk behaviors associated with intimate partner violence–United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57(5):113-117. [PubMed] [Google Scholar]
- 32.Lagdon S, Armour C, Stringer M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: a systematic review. Eur J Psychotraumatol. 2014;5(1):24794. doi: 10.3402/ejpt.v5.24794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ansara DL, Hindin MJ. Psychosocial consequences of intimate partner violence for women and men in Canada. J Interpers Violence. 2011;26(8):1628-1645. doi: 10.1177/0886260510370600 [DOI] [PubMed] [Google Scholar]
- 34.Lalley-Chareczko L, Segal A, Perlis ML, Nowakowski S, Tal JZ, Grandner MA. Sleep disturbance partially mediates the relationship between intimate partner violence and physical/mental health in women and men. J Interpers Violence. 2017;32(16):2471-2495. doi: 10.1177/0886260515592651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilbert LK, Zhang X, Basile KC, Breiding M, Kresnow M-J. Intimate partner violence and health conditions among U.S. adults—National Intimate Partner Violence Survey, 2010–2012. J Interpers Violence. 2023;38(1-2):NP237-NP261. doi: 10.1177/08862605221080147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Afifi TO, MacMillan H, Cox BJ, Asmundson GJG, Stein MB, Sareen J. Mental health correlates of intimate partner violence in marital relationships in a nationally representative sample of males and females. J Interpers Violence. 2009;24(8):1398-1417. doi: 10.1177/0886260508322192 [DOI] [PubMed] [Google Scholar]
- 37.Fanslow JL, Malihi Z, Hashemi L, Gulliver P, McIntosh T. Prevalence of interpersonal violence against women and men in New Zealand: results of a cross-sectional study. Aust N Z J Public Health. 2022;46(2):117-126. doi: 10.1111/1753-6405.13206 [DOI] [PubMed] [Google Scholar]
- 38.Fanslow J, Gulliver P, Hashemi L, Malihi Z, McIntosh T. Methods for the 2019 New Zealand Family Violence Study- a study on the association between violence exposure, health and well-being. Kotuitui. 2021;16(1):196-209. doi: 10.1080/1177083X.2020.1862252 [DOI] [Google Scholar]
- 39.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800-804. doi: 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- 40.Hashemi L, Fanslow J, Gulliver P, McIntosh T. Exploring the health burden of cumulative and specific adverse childhood experiences in New Zealand: results from a population-based study. Child Abuse Negl. 2021;122:105372. doi: 10.1016/j.chiabu.2021.105372 [DOI] [PubMed] [Google Scholar]
- 41.Stats NZ. Age and sex by ethnic group (grouped total responses), for census night population counts, 2006, 2013, and 2018 censuses. Accessed August 25, 2021. https://nzdotstat.stats.govt.nz/wbos/Index.aspx?DataSetCode=TABLECODE8317#
- 42.Exeter DJ, Zhao J, Crengle S, Lee A, Browne M. The New Zealand Indices of Multiple Deprivation (IMD): a new suite of indicators for social and health research in Aotearoa, New Zealand. PLoS One. 2017;12(8):e0181260. doi: 10.1371/journal.pone.0181260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.García-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C. World Health Organization Multi-Country Study on Women’s Health and Domestic Violence Against Women. World Health Organization; 2005. Accessed February 2, 2022. https://apps.who.int/iris/handle/10665/43309
- 44.StataCorp. Statistical Software, Release 16. StataCorp LLC; 2019. [Google Scholar]
- 45.Ministry of Health . HISO 10001:2017. ethnicity data protocols. Accessed May 28, 2022. https://www.health.govt.nz/publication/hiso-100012017-ethnicity-data-protocols
- 46.Kolbe V, Büttner A. Domestic violence against men - prevalence and risk factors. Dtsch Arztebl Int. 2020;117(31-32):534-541. doi: 10.3238/arztebl.2020.0534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coker AL, Smith PH, Fadden MK. Intimate partner violence and disabilities among women attending family practice clinics. J Womens Health (Larchmt). 2005;14(9):829-838. doi: 10.1089/jwh.2005.14.829 [DOI] [PubMed] [Google Scholar]
- 48.Straus H, Cerulli C, McNutt LA, et al. Intimate partner violence and functional health status: associations with severity, danger, and self-advocacy behaviors. J Womens Health (Larchmt). 2009;18(5):625-631. doi: 10.1089/jwh.2007.0521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blasdell R. The co-occurrence of physical and sexual intimate partner violence among U.S. college females. IJCJS. 2021;16(1):97-109. doi: 10.5281/zenodo.4762461 [DOI] [Google Scholar]
- 50.Coker AL, Smith PH, McKeown RE, King MJ. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health. 2000;90(4):553-559. doi: 10.2105/AJPH.90.4.553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krebs C, Breiding MJ, Browne A, Warner T. The association between different types of intimate partner violence experienced by women. J Fam Violence. 2011;26(6):487-500. doi: 10.1007/s10896-011-9383-3 [DOI] [Google Scholar]
- 52.Swan SC, Gambone LJ, Caldwell JE, Sullivan TP, Snow DL. A review of research on women’s use of violence with male intimate partners. Violence Vict. 2008;23(3):301-314. doi: 10.1891/0886-6708.23.3.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Swan SC, Snow DL. A typology of women’s use of violence in intimate relationships. Violence Against Women. 2002;8(3):286-319. doi: 10.1177/107780120200800302 [DOI] [PubMed] [Google Scholar]
- 54.Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women. 2000;6(2):142-161. doi: 10.1177/10778010022181769 [DOI] [Google Scholar]
- 55.Nybergh L, Enander V, Krantz G. Theoretical considerations on men’s experiences of intimate partner violence: an interview-based study. J Fam Violence. 2015;31(2):191-202. doi: 10.1007/s10896-015-9785-8 [DOI] [Google Scholar]
- 56.Stöckl H, Penhale B. Intimate partner violence and its association with physical and mental health symptoms among older women in Germany. J Interpers Violence. 2015;30(17):3089-3111. doi: 10.1177/0886260514554427 [DOI] [PubMed] [Google Scholar]
- 57.Aizpurua E, Copp J, Ricarte JJ, Vázquez D. Controlling behaviors and intimate partner violence among women in Spain: an examination of individual, partner, and relationship risk factors for physical and psychological abuse. J Interpers Violence. 2021;36(1-2):231-254. doi: 10.1177/0886260517723744 [DOI] [PubMed] [Google Scholar]
- 58.Myhill A. Measuring coercive control: what can we learn from national population surveys? Violence Against Women. 2015;21(3):355-375. doi: 10.1177/1077801214568032 [DOI] [PubMed] [Google Scholar]
- 59.Carlsson L, Lysell H, Enander V, Örmon K, Lövestad S, Krantz G. Socio-demographic and psychosocial characteristics of male and female perpetrators in intimate partner homicide: a case-control study from Region Västra Götaland, Sweden. PLoS One. 2021;16(8):e0256064. doi: 10.1371/journal.pone.0256064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ellsberg M, Heise L, Peña R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plann. 2001;32(1):1-16. doi: 10.1111/j.1728-4465.2001.00001.x [DOI] [PubMed] [Google Scholar]
- 61.Santosh J, Crampton P. Gender differences in general practice utilisation in New Zealand. J Prim Health Care. 2009;1(4):261-269. doi: 10.1071/HC09261 [DOI] [PubMed] [Google Scholar]
- 62.Johnson L, Huggard P, Goodyear-Smith F. Men’s health and the health of the nation. N Z Med J. 2008;121(1287):69-76. [PubMed] [Google Scholar]
- 63.Johnson MP. A Typology of Domestic Violence Intimate Terrorism, Violent Resistance, and Situational Couple Violence. Northeastern University Press; 2010. [Google Scholar]
- 64.Heise L, Pallitto C, García-Moreno C, Clark CJ. Measuring psychological abuse by intimate partners: constructing a cross-cultural indicator for the sustainable development goals. SSM Popul Health. 2019;9:100377. doi: 10.1016/j.ssmph.2019.100377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scott-Storey K, O’Donnell S, Wuest J, MacIntosh J, Merritt-Gray M. Cumulative lifetime violence severity scale: development and initial testing among men. BMC Public Health. 2020;20(1):418. doi: 10.1186/s12889-020-08551-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Callan A, Corbally M, McElvaney R. A scoping review of intimate partner violence as it relates to the experiences of gay and bisexual men. Trauma Violence Abuse. 2021;22(2):233-248. doi: 10.1177/1524838020970898 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Variable Questions and Definitions From the 2019 New Zealand Family Violence Study Used in Analysis
Data Sharing Statement