Background:
Orbital floor fractures are among the most common facial injuries. Although urgent surgical repair may be indicated, most patients require interval follow-up to assess for symptom onset and need for definitive operative intervention. This study aimed to evaluate the time to operative indication after these injuries.
Methods:
A retrospective review was conducted of all patients with isolated orbital floor fractures at a tertiary academic medical center from June 2015 to April 2019. Patient demographic and clinical data were recorded from the medical record. Time until operative indication was evaluated by the Kaplan-Meier product limit method.
Results:
Of 307 patients meeting inclusion criteria, 9.8% (30/307) developed indications for repair. Among these, 60% (18/30) were recommended surgery on the day of initial evaluation. Of 137 follow-up patients, 8.8% (12/137) developed operative indications based on clinical evaluation. The median period to decision for surgery was 5 days (range, 1–9). No patients developed symptoms suggesting the need for surgery beyond 9 days after trauma.
Conclusions:
Our investigation demonstrates that only about 10% of patients presenting with isolated orbital floor fracture develop an indication for surgery. For patients undergoing interval clinical follow-up, we found that patients demonstrated symptoms within 9 days of trauma. No patients demonstrated need for surgery beyond 2 weeks of injury. We believe these findings will assist to establish standards of care and inform clinicians on the appropriate length of follow-up for these injuries.
Takeaways
Question: What is the timeline of development of operative indication for isolated orbital floor fracture?
Findings: Of 307 patients, 9.8% developed indications for repair. Among surgical patients, 60% were recommended operative intervention on the day of initial evaluation. The median period to decision for surgery was 5 days (range: 1–9). No patients developed symptoms suggesting need for surgery beyond 9 days after trauma.
Meaning: Only about 10% of patients presenting with isolated orbital floor fracture develop an indication for surgery. For patients undergoing interval clinical follow-up, we found that patients demonstrated symptoms within 9 days of trauma. No patients demonstrated need for surgery beyond 2 weeks of injury.
INTRODUCTION
Orbital floor fractures are among the most common facial fractures evaluated within the emergency department (ED) nationwide.1 Violation of the orbital floor may result in distortion of volume and shape of the orbit, often causing visual disturbance or adverse cosmetic sequelae.2 Whereas urgent surgical repair is indicated in those who present with severe enophthalmos, extraocular muscle entrapment with concern for ischemia, or unresolving oculocardiac reflex, there remains a large proportion of patients for whom interval follow-up and posttraumatic surveillance is necessary to assess for symptom resolution and need for definitive operative intervention.3–10 Various studies have been conducted to identify objective parameters or fracture patterns that predict onset of visual symptoms to further guide operative decision-making. Recently, our group defined morphometric parameters, such as degree of muscle herniation and change in orbital volume, to more reliably risk stratify patients who present with isolated (“pure”) orbital floor fractures.11
Risk stratification for symptom onset after injury remains a central component of the workup and management of orbital blowout fractures, where low-risk patients can be reliably treated nonoperatively versus their high-risk counterparts who require reconstruction. However, there remains a gap in knowledge regarding the optimal method and timing of clinical evaluation for moderate-risk cohorts. Patients who do not require emergent surgical management are often evaluated for weeks after injury in an outpatient setting to determine the need for surgery. It is suggested that traumatic edema may contribute to certain symptoms (eg, acute diplopia), while masking others, such as enophthalmos or hypoglobus.5 Therefore, interval evaluation is often recommended to allow for resolution of edema, thereby revealing the presence of persistent visual dysfunction or significant cosmetic deformity, which are commonly accepted as indications for delayed operative intervention.5,12
Despite the acceptance of certain bona fide surgical indications, the optimal timing for posttraumatic assessment of these symptoms has not yet been characterized. It is thought that symptom onset occurs within 2 weeks of orbital floor injury; however, this claim remains unsupported by evidence or scientific rigor.4,5,13 Evaluation of the natural history of symptom onset after pure orbital floor fractures is of paramount importance for patient counseling, management of expectations, and clinical resource allocation. The goal of this study was to evaluate the timing of symptom onset (and therefore operative decision-making), for isolated orbital floor fractures to better standardize treatment paradigms, and guide perioperative planning.
METHODS
Study Design and Patient Population
This study adheres to all pertinent institutional research policies and procedures, and institutional review board approval was obtained and maintained throughout the study period. A retrospective review of a prospectively maintained Research Electronic Data Capture (REDCap) database was performed for all patients with isolated orbital floor fractures who were evaluated by the plastic surgery department at a tertiary academic medical center. The study period extended between January 2015 and August 2019. Patients with concurrent LeFort II/III, naso-orbito-ethmoid, and zygomaticomaxillary complex fractures were excluded.
Data Collection and Analysis
Patient demographic data, such as age at presentation, sex (man versus woman), race, ethnicity, and preferred language were documented. Pertinent social history included insurance status, mental health diagnosis, and history of smoking, alcohol, or illicit drug use were also recorded. Clinical characteristics (including diplopia, hypoglobus, enophthalmos, and orbital muscle entrapment) were recorded at initial presentation in the ED, as well as at subsequent outpatient follow-up appointments. Hypoglobus was measured with a McCoy facial trisquare device, and enophthalmos was assessed by a Hertel exophthalmometer. Significant fracture size, defined as a defect involving more than 50% of the orbital floor area on computed tomography, was also documented. Choice of clinical management, whether surgical or conservative, was also recorded for each patient. In our institution, accepted operative indications for repair include muscle entrapment, persistent diplopia beyond the index visit (after the resolution of acute traumatic edema), and significant fracture size.3–10 Although the presence of visible enophthalmos or hypoglobus (≥2 mm) was identified as an operative indication for the study, this was not utilized clinically as an absolute indication for surgery. Instead, such findings were discussed with the patient, who made the final decision regarding interest in proceeding with surgical intervention. The time to operative decision for each surgical patient was calculated. Data such as surgeon specialty and type of surgical incision were also recorded.
Statistical Analysis
Data were analyzed using IBM SPSS version 25 (IBM Corp., Armonk, N.Y.). Patient characteristics, clinical risk factors, and time interval to decision for operative intervention were summarized using descriptive statistics. Categorical variables were compared using chi-square or Fisher exact test. Continuous variables were compared using Student t test or Wilcoxon rank sum test. Time until operative decision (in days) was evaluated by the Kaplan-Meier product limit method. Statistical significance was defined as a value of P less than 0.05.
RESULTS
Patient Characteristics
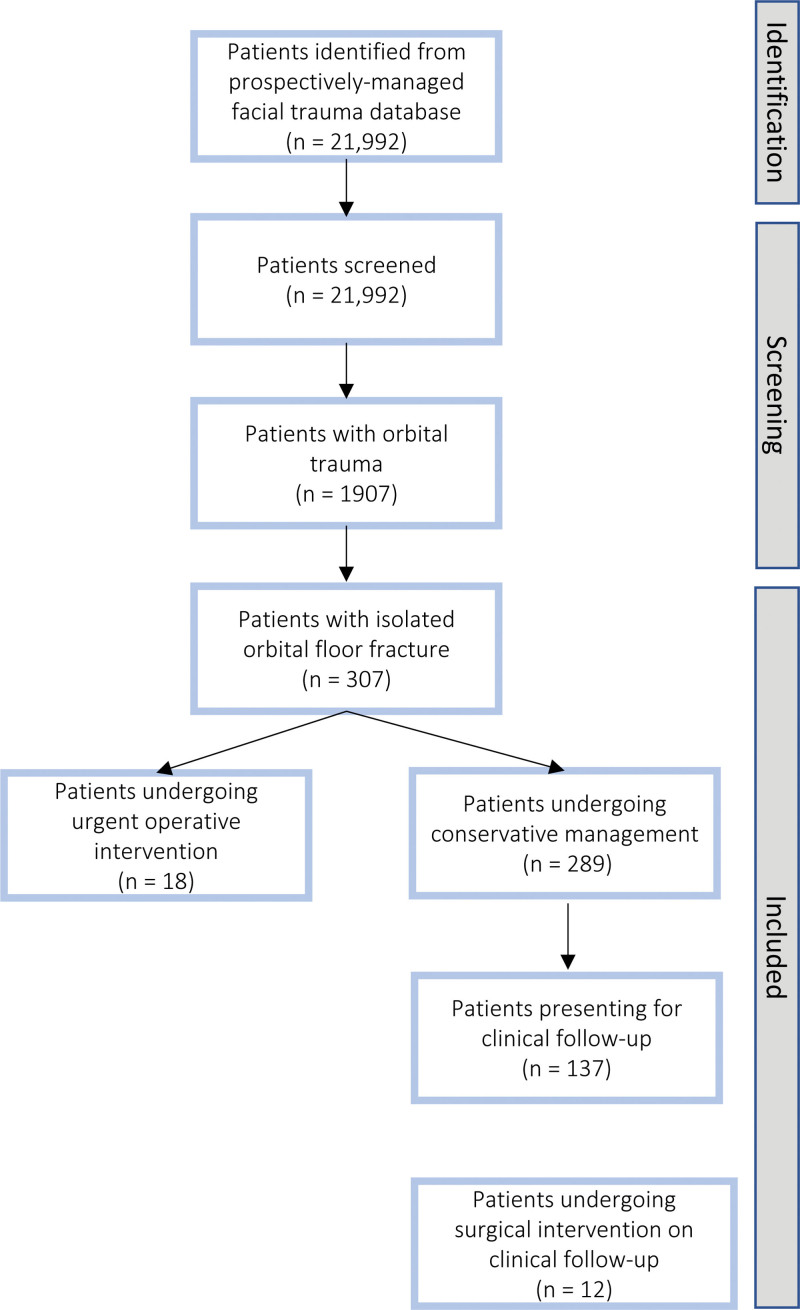
Of the 1907 patients with orbital trauma identified during the study period, 1600 (83.9%) demonstrated concomitant facial bony injuries and were therefore excluded. The remaining 307 patients with pure orbital floor fractures were included, and their medical records were reviewed (Fig. 1). Included patients averaged 45.4 ± 23.3 years of age. An estimated 36.2% were women and 71.7% were White (Table 1). Mean age between operative (35.0 ± 19.1 years) and nonoperative (46.6 ± 23.5) groups was significantly different (p = 0.01). No socioeconomic risk factors, such as homeless status, alcohol abuse, or mental health disorder, varied between cohorts.
Fig. 1.
Flow chart of patient identification, inclusion, and exclusion criteria, for patients with isolated orbital floor fractures undergoing either surgical or conservative management.
Table 1.
Sociodemographic Data for All Patients with Isolated Orbital Floor Fractures
| Variable | Total | Operative Management | P | |
|---|---|---|---|---|
| No | Yes | |||
| Total, n (row %) | 307 | 277 (90.2) | 30 (9.8) | |
| Age | ||||
| Mean (SD) | 45.4 (23.3) | 46.6 (23.5) | 35.0 (19.1) | |
| Median (range) | 41 (5–99) | 43 (5–99) | 29 (10–90) | 0.01 |
| Gender | ||||
| Women | 111 (36.2) | 104 (37.5) | 7 (23.3) | 0.24 |
| Men | 195 (63.5) | 172 (62.1) | 23 (76.7) | |
| Other | 1 (0.3) | 1 (0.4) | 0 (0.0) | |
| Race | ||||
| Asian/Pacific Islander | 3 (1.0) | 3 (1.1) | 0 (0.0) | 0.69 |
| Black or African American | 31 (10.1) | 27 (9.7) | 4 (13.3) | |
| Native American or American Indian | 1 (0.3) | 1 (0.4) | 0 (0.0) | |
| White | 220 (71.7) | 197 (71.1) | 23 (76.7) | |
| Other | 52 (16.9) | 49 (17.7) | 3 (10.0) | |
| Hispanic/Latino | ||||
| Yes | 51 (16.6) | 48 (17.3) | 3 (10.0) | 0.44 |
| No | 256 (83.4) | 229 (82.7) | 27 (90.0) | |
| Preferred language | ||||
| English | 272 (88.6) | 244 (88.1) | 28 (93.3) | 0.44 |
| Spanish | 27 (8.8) | 26 (9.4) | 1 (3.3) | |
| Other | 8 (2.6) | 7 (2.5) | 1 (3.3) | |
| Homeless | ||||
| Yes | 8 (2.6) | 8 (2.9) | 0 (0.0) | 1.00 |
| No | 299 (97.4) | 269 (97.1) | 30 (100.0) | |
| Alcohol abuse | ||||
| Yes | 26 (8.5) | 23 (8.3) | 3 (10.0) | 0.77 |
| No | 215 (70.0) | 193 (69.7) | 22 (73.3) | |
| Unknown | 66 (21.5) | 61 (22.0) | 5 (16.7) | |
| Smoker | ||||
| Yes | 90 (29.3) | 80 (28.9) | 10 (33.3) | 0.70 |
| No | 164 (53.4) | 150 (54.2) | 14 (46.7) | |
| Unknown | 53 (17.3) | 47 (17.0) | 6 (20.0) | |
| Drug abuse | ||||
| Yes | 24 (7.8) | 21 (7.6) | 3 (10.0) | 0.50 |
| No | 197 (64.2) | 176 (63.5) | 21 (70.0) | |
| Unknown | 86 (28.0) | 80 (28.9) | 6 (20.0) | |
| Mental health disorder | ||||
| Yes | 68 (22.1) | 60 (21.7) | 8 (26.7) | 0.52 |
| No | 231 (75.2) | 210 (75.8) | 21 (70.0) | |
| Unknown | 8 (2.6) | 7 (2.5) | 1 (3.3) | |
| Has insurance | ||||
| Yes | 233 (75.9) | 209 (75.5) | 24 (80.0) | 0.79 |
| No | 64 (20.8) | 58 (20.9) | 6 (20.0) | |
| Unknown | 10 (3.3) | 10 (3.6) | 0 (0.0) | |
| Has PCP | ||||
| Yes | 182 (59.3) | 164 (59.2) | 18 (60.0) | 0.82 |
| No | 115 (37.5) | 103 (37.2) | 12 (40.0) | |
| Unknown | 10 (3.3) | 10 (3.6) | 0 (0.0) | |
Symptomatology at Index Presentation
Symptoms experienced during ED visits were significantly different between operative and nonoperative groups. Patients who underwent operative intervention more frequently experienced acute diplopia (P < 0.01), muscle entrapment (P < 0.01), retrobulbar hematoma (P = 0.02), and acute enophthalmos (P = 0.04) (Table 2). Canthotomy procedure in the ED was also predictive of operative intervention (P < 0.01). Among our primary endpoints, acute diplopia in the ED was the most frequently reported (15%), independent of operative status.
Table 2.
Symptoms Experienced in ED for All Patients
| Variable | Total | Operative Management | P | |
|---|---|---|---|---|
| No | Yes | |||
| Total, n (row %) | 307 | 277 (90.2) | 30 (9.8) | |
| Acute diplopia | ||||
| Yes | 46 (15.0) | 28 (10.1) | 18 (60.0) | <0.0001 |
| No | 261 (85.0) | 249 (89.9) | 12 (40.0) | |
| Acute hypoglobus | ||||
| Yes | 5 (1.6) | 3 (1.1) | 2 (6.7) | 0.08 |
| No | 302 (98.4) | 274 (98.9) | 28 (93.3) | |
| Acute enophthalmos | ||||
| Yes | 9 (2.9) | 6 (2.2) | 3 (10.0) | 0.047 |
| No | 298 (97.1) | 271 (97.8) | 27 (90.0) | |
| Muscle entrapment | ||||
| Yes | 8 (2.6) | 1 (0.4) | 7 (23.3) | <0.0001 |
| No | 299 (97.4) | 276 (99.6) | 23 (76.7) | |
| Retrobulbar hematoma | ||||
| Yes | 12 (3.9) | 8 (2.9) | 4 (13.3) | 0.02 |
| No | 295 (96.1) | 269 (97.1) | 26 (86.7) | |
| Canthotomy procedure | ||||
| Yes | 6 (2.0) | 2 (0.7) | 4 (13.3) | 0.001 |
| No | 299 (97.4) | 276 (99.6) | 23 (76.7) | |
Timing of Follow-up and Decision for Operative Intervention
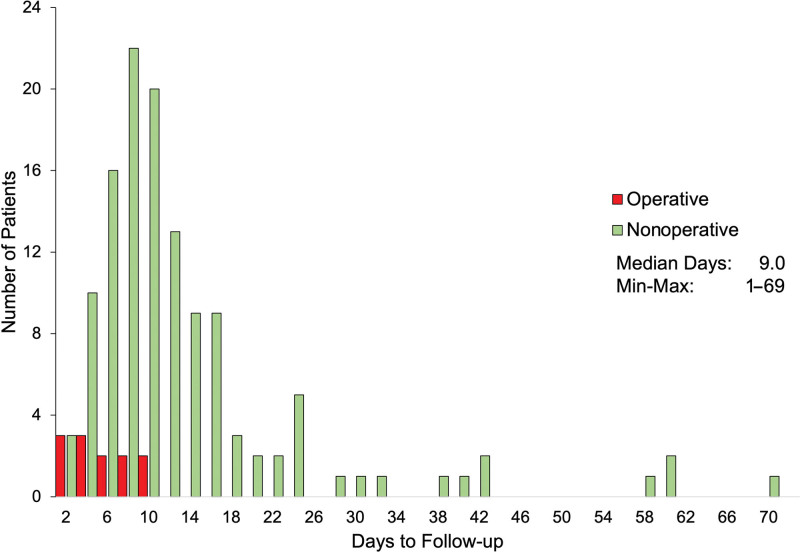
Of 307 patients presenting with pure orbital floor fracture in the ED, 81.4% (250/307) were recommended serial follow-up evaluation (Table 3). Of those requested for follow-up, 54.8% (137/250) presented for their visit. The mean period to first and second follow-up visits were 12.4 ± 11.6 and 26.4 ± 21.9 days, respectively. A graph demonstrating the number of days to clinical follow-up is shown for both operative and nonoperative patients (Fig. 2).
Table 3.
Follow-up Data among All Patients Presenting with Isolated Orbital Floor Fracture
| Variable | Total |
|---|---|
| Total cohort, n (row %) | 307 |
| Follow-up visit requested | |
| Yes | 250 (81.4) |
| No | 57 (18.6) |
| Patient adherence to follow-up visit | |
| Yes | 137 (54.8) |
| No | 113 (45.2) |
| Days to first follow-up visit | |
| Mean (SD) | 12.4 (11.6) |
| Median (range) | 9.0 (1–69) |
| Days to second follow-up visit (since first follow-up) | |
| Mean (SD) | 26.4 (21.9) |
| Median (range) | 22 (5–105) |
| Decision made for operative intervention | |
| Total cohort (n = 307) | 30 (9.8) |
| Urgently (of n = 307 patients presenting to ED) | 18 (5.9) |
| On clinical follow-up (of n = 137 follow-up patients) | 12 (8.8) |
Fig. 2.
Bar chart demonstrating the distribution of days to first follow-up visit for operative (red) and nonoperative (green) patients.
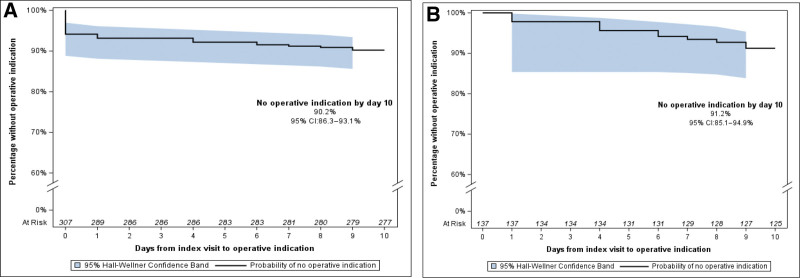
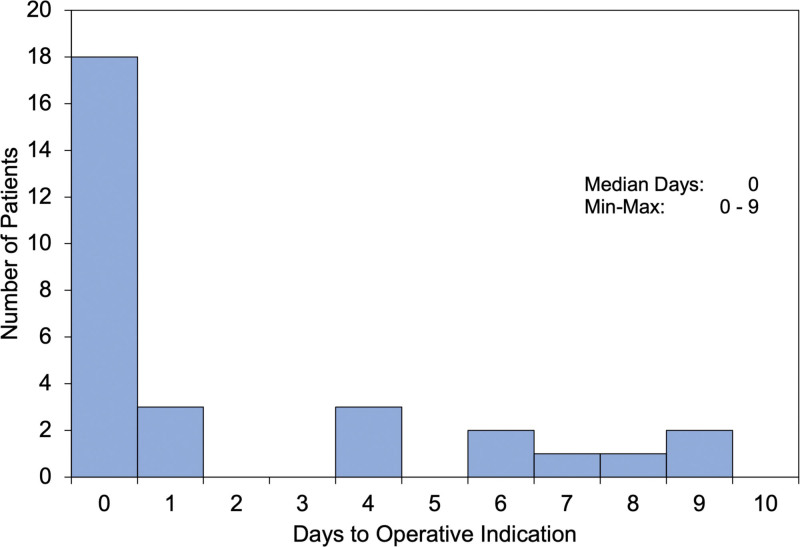
Among the total cohort, 9.8% (30/307) developed an indication for operative intervention (Table 3). Surgical recommendation at index presentation to the ED was made for 5.9% (18/307) of all patients. Of those patients presenting for follow-up, 8.8% (12/137) developed symptoms necessitating surgery. Kaplan-Meier survival curves illustrating the proportion of patients proceeding to operative intervention over time are shown in Figure 3. Of the 30 patients undergoing reconstruction, 60% (18/30) demonstrated an indication for surgery at the index visit (“day 0”) (Table 4). The remaining 40% (12/30) of patients developed surgical indications on follow-up after the traumatic incident. The mean period to decision for surgery among follow-up patients was 5.0 ± 2.9 days (Table 4). When including patients who were recommended for surgery on day 0, the mean period to surgical recommendation was 2.0 ± 3.1 days.
Fig. 3.
Kaplan-Meier survival curves illustrating the percentage without operative indications over time for (A) all patients (n = 307), and (B) patients presenting for follow-up (n = 137).
Table 4.
Operative Indication and Surgical Decision-making Data
| Variable | Total |
|---|---|
| Operative patients, n (row %) | 30 |
| Decision for surgical intervention | |
| Urgent | 18 (60) |
| On follow-up | 12 (40) |
| Days from index visit to operative indication* | |
| Mean (SD) | 2.0 (3.1) |
| Median (range) | 0 (0–9) |
| Days from index visit to operative indication† | |
| Mean (SD) | 5.0 (2.9) |
| Median (range) | 5.0 (1–9) |
| Prevalence of indications (n = 38)‡ | |
| Size of fracture | 15 (50.0) |
| Persistent diplopia | 8 (26.7) |
| Muscle entrapment | 7 (23.3) |
| Significant delayed enophthalmos | 3 (10) |
| Significant acute enophthalmos | 3 (10) |
| Significant acute hypoglobus | 2 (6.7) |
| Significant delayed hypoglobus | 0 (0) |
| Surgeon department | |
| Plastic surgery | 20 (66.7) |
| Ophthalmology | 10 (33.3) |
| Surgical incision | |
| Transconjunctival | 25 (83.3) |
| Infraorbital | 3 (10.0) |
| Subciliary | 2 (6.7) |
| Implant type | |
| Alloplastic | 30 (100) |
| Autologous | 0 |
All operative patients.
Only operative patients evaluated by clinical follow-up.
Indicators greater than number of surgical patients, as some patients experienced multiple indicators.
A distribution for the number of days to surgical recommendation is shown in Figure 4 for all operative patients. Most follow-up patients who ultimately proceeded to surgery developed symptoms within 1 week of injury (75%, 9/12). Beyond 1 week, 2.2% (3/137) of all follow-up patients developed an operative indication. No patients were recommended for surgery later than 9 days after the traumatic incident. Among follow-up patients undergoing conservative management (91.2%, 125/137), none developed symptoms portending surgery, such as persistent diplopia or significant eye displacement, throughout the duration of their outpatient course.
Fig. 4.
Histogram illustrating distribution of days from index visit to operative indication for all patients undergoing surgical management (n = 30).
Frequency of Surgical Indications
The most frequent indications for surgical management were size of fracture (50%), persistent diplopia (26.7%), and muscle entrapment (23.3%) (Table 4). Among follow-up patients initially presenting with diplopia in the ED (n = 28), this symptom spontaneously resolved in 71.4% (20/28) over the course of serial outpatient follow-up. The remaining eight patients with persistent diplopia were recommended for and underwent surgery. Significant enophthalmos in either an acute or delayed fashion was present in 20% (6/30) of operative patients (Table 4). Among follow-up patients initially presenting with acute enophthalmos (n=6) at the index visit (Table 2), only three (50%) developed significant enophthalmos in a delayed fashion on serial clinical examination. Most operative patients underwent repair by a plastic surgeon (66.7%), via a transconjunctival incision (83.3%). All patients had placement of an alloplastic implant; none underwent autologous reconstruction.
DISCUSSION
This study represents the first effort to document the natural history of operative indications after isolated orbital floor fracture. We discovered three main findings. First, fewer than one in 10 patients (9.8%) developed an evidence-based5,12 justification for surgical reconstruction after injury. Second, for operative patients, the recommendation for surgery is most often made in the acute setting (60%). Thus, the minority of operative patients are recommended surgery by means of follow-up examination. Third, for moderate-risk patients who were found to be operative candidates on follow-up, symptoms typically emerged within 9 days of injury, and on average, the decision to operate was made on day 5.
As part of this effort to document symptom development after injury, we first discovered that few patients with isolated orbital floor fractures go on to require definitive operative repair. In fact, among our cohort of 307 patients, greater than 90% did not develop a clear indication for surgical intervention. We consider evidence-based indications to be those commonly cited in the literature.4–10 In the acute setting, these include muscle entrapment, large fracture size (> 50% of floor area), unresolving oculocardiac reflex, and significant enophthalmos or hypoglobus. On follow-up, indications for delayed repair include persistent diplopia or significant eye displacement. Our finding that few patients require repair has been corroborated by similar studies of pure orbital floor fractures in the pediatric population.14,15 In a retrospective review identifying 25 isolated orbital fractures, only 12% developed either enophthalmos, vertical orbital dystopia, or muscle entrapment, and therefore underwent surgical reconstruction.14 The remaining patients were managed conservatively by follow-up for an average period of 13 months, with no patients reportedly developing symptoms. The present study finds similar results and supports the conclusion that pure orbital floor fractures without acute operative signs ought to be managed conservatively in the outpatient setting. Notably, no patients in our dataset showed signs of trapdoor fracture.
Clinical follow-up of these injuries is well accepted; however, the timing and duration of follow-up after injury remains controversial and unclear. Prior guidelines recommended that patients without acute operative indications should be evaluated at a 2-week follow-up visit after the traumatic incident, with weekly interval follow-up to monitor for symptom resolution.4,5,13 Our evidence suggests that operative patients will develop a surgical indication sooner than this interval—on average 5.0 days after injury. Therefore, it may instead be beneficial to evaluate patients at 1 week (5 – 10 days) after trauma rather than at a 2-week visit in order to expedite surgical intervention. In doing so, most patients who go on to develop surgical indications may receive more timely care, as studies suggest that delayed intervention may result in poorer outcomes, such as decreased resolution of diplopia and enophthalmos.16 Demographically, we additionally discovered that patients proceeding to operative intervention were younger than those undergoing conservative management (mean age 35.2 ± 19.1 years, P = 0.01). Therefore, for young patients who are more likely to necessitate definitive surgical repair, we suggest that follow-up after the traumatic incident should not be delayed beyond 1 week of trauma. We also discovered that very few patients (2.2%, 3/137) develop operative indications during follow-up visits beyond 1 week of trauma.
Previously published guidelines have recommended serial clinical follow-up for low- and medium-risk patients on the basis that acute diplopia may spontaneously improve and eye displacement may be unmasked with resolution of traumatic edema.6 However, these recommendations have not been rigorously validated by scientific study, and it remains unknown how often this resolution occurs. In our investigation, we aimed to address this gap. We discovered that acute diplopia and enophthalmos improved in 71.4% and 50% of patients, respectively, within 9 days of trauma. Therefore, symptoms ought to resolve in most instances with follow-up visits timed at this interval. Should these symptoms not resolve, surgeon discretion ought to be used to decide between repeat follow-up or definitive operative intervention. We believe this finding will guide patient counseling as well as provider expectation in the future evaluation of these injuries.
We suggest that surgeons may be reasonably certain that operative indications will no longer arise after the early posttraumatic period. Therefore, weekly follow-up after these injuries beyond this timeframe may not offer great clinical utility. Indeed, it is the senior author’s practice to follow moderate-risk patients closely on a weekly basis for the first 2 weeks after injury. Thereafter, if operative indications have not declared themselves by this point, patients are seen 1 month later, followed by a final 3 month evaluation. Utilizing this protocol, no patients demonstrated worsening symptoms or requested surgical intervention after the second week visit. Based upon the study findings, even this protocol may be overly conservative.
This study is not without notable limitations. Our cohort includes only patients with “pure” orbital floor fractures, excluding patients bearing other coexisting facial injuries such as naso-orbito-ethmoid, ZMC, and LeFort II/III fractures (“impure” fractures), which frequently accompany orbital floor fractures. Most often, orbital floor fractures occur as part of a constellation of broader fracture patterns. Therefore, the population studied here likely represents a minority of patients presenting with these injuries, and the conclusions drawn regarding symptom onset must be extrapolated judiciously to other clinical contexts. As part of our study design, however, we intentionally excluded patients with other fracture types to minimize potential confounding bases for symptom development. The small sample size of our operative cohort was a significant limitation. Although our initial cohort of 307 fractures seemed robust initially, the number of surgical patients among this group (30) was far fewer than anticipated, presumably secondary to employment of a more evidence-based approach towards decision for surgery. Our sample size of operative patients was further subdivided into urgent and delayed cohorts, with the latter group consisting of only 12 patients. These small sample sizes, however, are key findings in themselves, demonstrating that few patients with these injuries require surgical intervention, suggesting that more aggressive approaches may be detrimental to patient care. Few articles are written on this subject, however, possibly limited by the low percentage of patients actually undergoing surgery. Lastly, as is often the case among patients presenting with trauma, we noted significant attrition (45.2%) of our follow-up cohort. Exclusion bias is a weakness of any retrospective study, and this limitation is further augmented in many trauma investigations in which patients do not routinely present for follow-up care. In this study, patients lost to follow-up could not undergo assessment for the development of operative indications. It is possible that some of these patients may have developed persistent symptoms; however, we believe that many of them likely did not develop significant symptoms warranting surgery, as in these instances they would have likely presented for evaluation. Nonetheless, we acknowledge that our conclusions will require validation by larger, prospective cohort studies and in other populations where attrition may be less significant.
CONCLUSIONS
We discovered that only about 10% of patients with isolated orbital blowout fractures meet commonly accepted criteria for operative intervention and that patients are unlikely to develop symptoms portending surgical management later than 10 days after trauma. We believe these findings will guide future standards of care and have shared our own protocol for follow-up evaluation of pure orbital blowout fractures.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Roth FS, Koshy JC, Goldberg JS, et al. Pearls of orbital trauma management. Semin Plast Surg. 2010;24:398–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shokri T, Alford M, Hammons M, et al. Management of orbital floor fractures. Facial Plast Surg. 2019;35:633–639. [DOI] [PubMed] [Google Scholar]
- 3.Cruz AAV, Eichenberger GCD. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol. 2004;15:416–421. [DOI] [PubMed] [Google Scholar]
- 4.Burnstine MA. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol. 2003;14:236–240. [DOI] [PubMed] [Google Scholar]
- 5.Gart MS, Gosain AK. Evidence-based medicine: orbital floor fractures. Plast Reconstr Surg. 2014;134:1345–1355. [DOI] [PubMed] [Google Scholar]
- 6.Boyette JR, Pemberton JD, Bonilla-Velez J. Management of orbital fractures: challenges and solutions. Clin Ophthalmol Auckl NZ. 2015;9:2127–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellis E. Orbital trauma. Oral Maxillofac Surg Clin N Am. 2012;24:629–648. [DOI] [PubMed] [Google Scholar]
- 8.Liao JC, Elmalem VI, Wells TS, et al. Surgical timing and postoperative ocular motility in type B orbital blowout fractures. Ophthal Plast Reconstr Surg. 2015;31:29–33. [DOI] [PubMed] [Google Scholar]
- 9.Burnstine MA. Clinical recommendations for repair of isolated orbital floor fractures: an evidence-based analysis. Ophthalmology. 2002;109:1207–1210; discussion 1210–1211; quiz 1212–1213. [DOI] [PubMed] [Google Scholar]
- 10.Jordan DR, Allen LH, White J, et al. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthal Plast Reconstr Surg. 1998;14:379–390. [DOI] [PubMed] [Google Scholar]
- 11.Basta MN, Rao V, Roussel LO, et al. Refining indications for orbital floor fracture reconstruction: a risk-stratification tool predicting symptom development and need for surgery. Plast Reconstr Surg. 2021;148:606–615. [DOI] [PubMed] [Google Scholar]
- 12.Alinasab B, Borstedt KJ, Rudström R, et al. New algorithm for the management of orbital blowout fracture based on prospective study. Craniomaxillofacial Trauma Reconstr. 2018;11:285–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawes MJ, Dortzbach RK. Surgery on orbital floor fractures. Influence of time of repair and fracture size. Ophthalmology. 1983;90:1066–1070. [DOI] [PubMed] [Google Scholar]
- 14.Losee JE, Afifi A, Jiang S, et al. Pediatric orbital fractures: classification, management, and early follow-up. Plast Reconstr Surg. 2008;122:886–897. [DOI] [PubMed] [Google Scholar]
- 15.Gerbino G, Roccia F, Bianchi FA, et al. Surgical management of orbital trapdoor fracture in a pediatric population. J Oral Maxillofac Surg. 2010;68:1310–1316. [DOI] [PubMed] [Google Scholar]
- 16.Jazayeri HE, Khavanin N, Yu JW, et al. Does early repair of orbital fractures result in superior patient outcomes? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2020;78:568–577. [DOI] [PubMed] [Google Scholar]