Introduction
Abortive hemangiomas (AH) or minimal or arrested growth hemangiomas constitute a distinct subgroup of infantile hemangioma (IH) with a characteristic clinical presentation and natural history that are often clinically confused with other vascular anomalies (VA) [1,2]. Dermoscopy can be a useful tool for distinguishing VAs that may be clinically similar such as IH precursor lesions, port wine stains (PWS) and, probably, AH [3]. However, dermoscopy pattern of AH has only been previously described by Toledo-Alberola et al in 2 cases [4].
Case Presentation
The aim of this study was to evaluate the dermoscopy findings of an AH single-center case series, comparing these findings with those described in other clinically similar VAs such as IH precursor lesions and PWS. We evaluated the dermoscopy patterns and structures of 11 consecutives clinically diagnosed AH cases in our pediatric dermatology department, assessed during 2021, and we compared these findings with those described for IH precursor lesions and PWS.
Clinical and demographic findings are summarized in Table 1. Serpinginous or tortuous vessels, punctate vessels and vascular lacunae were observed in 100% of the cases clinically diagnosed as AH (Figures 1 and 2).
Table 1.
Clinical and demographic findings.
| Patient | Demographic characteristics | Dermoscopy findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age at diagnosis (years) | Age occurrence | Sex | Location | Treatment | Associate lesions | Additional tests | Serpinginous/tortuous vessels | Puntiform vessels | Vascular lacunae | |
| 1 | 6 | First days | M | Right leg | Timolol | - | - | Yes | Yes | Yes |
| 2 | 1 | Unknown | M | Left buttock | Timolol | Infantile hemangioma | - | Yes | Yes | Yes |
| 3 | 2 | Birth | F | Left knee | Timolol | - | Echography and doppler | Yes | Yes | Yes |
| 4 | 2 | Birth | M | Left thigh | Timolol | - | - | Yes | Yes | Yes |
| 5 | 0 | Birth | F | Sacral fossa | - | Spinal echography | Yes | Yes | Yes | |
| 6 | 1 | Birth | F | Right external malleolus | Timolol | - | - | Yes | Yes | Yes |
| 7 | 1 | Birth | F | Left hand | Timolol | - | Soft tissue Echography | Yes | Yes | Yes |
| 8 | 14 | Unknown | M | Abdomen | - | - | Yes | Yes | Yes | |
| 9 | 6 | First days | F | Right lumbar | Timolol + Propanolol | - | - | Yes | Yes | Yes |
| 10 | 2 | Birth | M | Neck | - | - | Yes | Yes | Yes | |
| 11 | 1 | Birth | F | Right thigh | Timolol | - | - | Yes | Yes | Yes |
Figure 1.
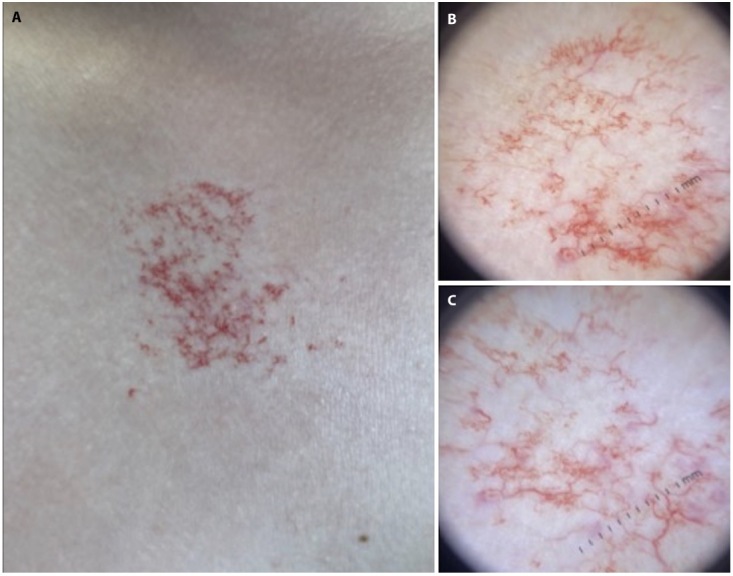
(A) Clinically macule with telangiectasias erythematous background. (B,C) Dermoscopy image showing serpiginous or tortuous vessels, punctate vessels and vascular lacunae.
Figure 2.
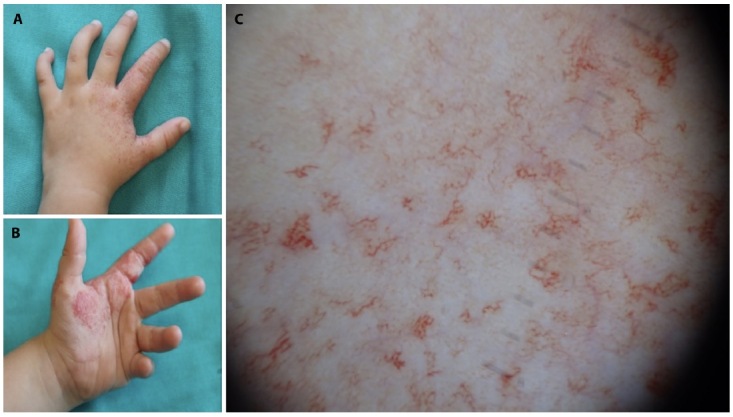
(A,B) Telangiectasias on an erythematous or reticulated background. (C) Dermoscopy image showing serpiginous or tortuous vessels, punctate vessels and vascular lacunae.
Conclusions
AH is a distinctive variant of IH present from birth in most cases, and, with little ability to proliferate. Although they could be clinically similar to other VAs they have different morphologic and immunostaining patterns. On histology, they show dilated thin-walled vessels within the superficial dermis, with a GLUT-1 positivity immunostaining demonstrating a clear distinction between AH and PWS or congenital hemangiomas [1,2]. Dermoscopic examination may facilitate the identification of AH for early diagnosis and treatment. In our case series, serpiginous or tortuous vessels, punctate vessels and vascular lacunae was observed in 100% of the cases clinically diagnosed as AH. IH precursor lesions dermoscopy features have been described as large linear vessel and branching vessels with erythematous background [5]. On the other hand, linear vessels, reticular vessels, sausage-like vessels, dots or globules vessels and mixed vessels, as well as white circles and whitish veil have been described in PWS [6]. When comparing our findings in AH, with those described IH precursor lesions and PWS, we found these to be differential and characteristic of AH. As limitations, no control group was included, therefore, no definitive conclusions could be made.
Dermoscopy might improve the clinical diagnosis of AH. It might help distinguish AH from IH precursor or PWS. More studies including other lesions are needed to confirm our findings.
Footnotes
Funding: This research was supported by the Dermatology Department of the Clinical Universitary Hospital of Valencia.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Martin JM, Sanchez S, González V, Cordero P, Ramon D. Infantile hemangiomas with minimal or arrested growth: A retrospective case series. Pediatr Dermatol. 2019;36(1):125–131. doi: 10.1111/pde.13695. [DOI] [PubMed] [Google Scholar]
- 2.Rodríguez Bandera AI, Sebaratnam DF, Wargon O, Wong L-CF. Infantile hemangioma. Part 1: Epidemiology, pathogenesis, clinical presentation and assessment. J Am Acad Dermatol. 2021:1379–1392. doi: 10.1016/j.jaad.2021.08.019. [DOI] [PubMed] [Google Scholar]
- 3.Piccolo V, Russo T, Moscarella E, Brancaccio G, Alfano R, Argenziano G. Dermatoscopy of Vascular Lesions. Dermatol Clin. 2018;36(4):389–395. doi: 10.1016/j.det.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Toledo-Alberola F, Betlloch-Mas I, Cuesta-Montero L, et al. Abortive hemangiomas. Description of clinical and pathological findings with special emphasis on dermoscopy. Eur J Dermatol. 2010;20(4):497–500. doi: 10.1684/ejd.2010.0959. [DOI] [PubMed] [Google Scholar]
- 5.Sun Y, Hu SCS. Dermoscopy as a diagnostic aid in the precursor stage of infantile hemangioma. Int J Dermatol. 2022;61(2):e54–e55. doi: 10.1111/ijd.15841. [DOI] [PubMed] [Google Scholar]
- 6.Huang Y, Yang J, Li Z, Zhang L, Sun L, Bi M, Wang L. Dermoscopic features of port-wine stains: A study of 264 cases. Australas J Dermatol. 2021;62(2):e201–e206. doi: 10.1111/ajd.13470. [DOI] [PubMed] [Google Scholar]


