Abstract
Purpose/Objectives:
To describe and examine the relationship between caregiver burden and the affective disorders anxiety and depression in caregivers of patients with brain metastases.
Design:
Cross-sectional, descriptive, correlational.
Setting:
Moores Cancer Center at the University of California, San Diego.
Sample:
56 family caregivers of patients with brain metastases from solid tumors at other primary sites.
Methods:
Self-administered survey.
Main Research Variables:
Caregiver burden, anxiety, and depression.
Findings:
With the exception of caregiver esteem, no statistically significant relationships were noted between impact on schedule, a dimension of caregiver burden, and screening positive for affective disorders.
Conclusions:
Findings from this study support previous reports indicating that the odds of having anxiety and depressive symptoms are greater in family caregivers who report higher levels of caregiver burden.
Implications for Nursing:
The identification and management of caregiver burden are important considerations for a comprehensive cancer care program. Addressing the needs of the cancer caregiver, who is at heightened risk for various psychological, physical, financial, and social problems, is increasingly vital.
Keywords: Burden, Anxiety, depression
Brain metastases are diagnosed in 20%–40% of all patients with cancer, and the incidence continues to rise with the increasing number of long-term survivors (Schmieder, Keilholz, & Combs, 2016). Brain metastases are the most common intracranial tumors, and the annual incidence of brain metastases is more than 10 times greater than that of primary brain tumors. Although methodologic limitations are inherent in all studies on the incidence of brain metastases, current estimates in the United States suggest an incidence rate of about 10 per 100,000, with incidence ranging from 21,000–43,000 patients diagnosed per year to more than 100,000 patients when autopsy and clinical data are taken into consideration (Stelzer, 2013).
Family caregivers provide long-term care and are often the primary source of physical, social, and emotional support for patients. A caregiver is an unpaid individual who provides direct care to relatives or friends who are unable to provide for themselves (Hunt, 2003). Depending on their responsibilities, caregivers have been classified as primary caregivers if they mainly provide and/or assist with care recipients’ activities of daily living (ADLs). Caregivers are classified as secondary caregivers if they assist someone else with caregiving or provide support to care recipients, but are not primarily responsible for the day-to-day care of an individual or decisions regarding his or her care (Penrod, Kane, Kane, & Finch, 1995; Ryba, Johnson, Ulstad, & Owen, 2012).
Caregivers of Patients With Brain Metastases
Those who provide care to patients with brain metastases represent a unique and increasing population of cancer caregivers. They provide care to patients with a diagnosis that often heralds the start of the terminal phase of an advanced disease that can be manifested through worsening functional, cognitive, and neu-ropsychological impairment. Caregivers of patients with brain metastases not only acquire new care demands while facing the increasing intensity of existing demands, but also deal with physical and cognitive deterioration of their loved ones (Gerstenecker et al., 2014; Vaughan, 2012). Unfortunately, despite decades of research showing the negative emotional and physical responses of caregivers in the context of chronic illnesses (e.g., cancer, dementia), little caregiving research has been done in the field of neuro-oncology (Sherwood & Baer, 2011; Sherwood et al., 2016).
Burden
Caregiver burden, a negative response that has been studied extensively, is defined as the worrisome load borne by people providing care for another individual (Hunt, 2003). In addition, caregiver burden has been described as the physical, psychological or emotional, social, and financial problems experienced by caregivers resulting from changes in cognition and behavior of the patient and the patient’s subsequent need for care and supervision (Braithwaite, 1992; Paradise et al., 2015). Caregiver burden is multidimensional and dynamic in that it responds to fluctuations in demands and contextual variations during the caregiving experience (Chou, 2000; Perlick, Clarkin, & Sirey, 1995).
Anxiety and Depression
Anxiety and depression, other negative responses, have been studied in caregivers of patients with cancer (Lambert, Girgis, Lecathelinais, & Stacey, 2012; Lee et al., 2013; Sklenarova et al., 2015). However, few studies have focused on the subset of caregivers of patients with brain metastases. Caregivers of patients with advanced cancer have been reported to experience emotional stress, depression, and increased anxiety related to their caregiving activities (Mystakidou et al., 2013). In addition, caregivers of patients with brain tumors have also been reported to live with higher levels of anxiety and depressive symptoms compared to the general population (Finocchiaro et al., 2012). Affective symptoms of caregivers of patients with cancer may vary along the illness continuum and could be influenced by factors related to the patient’s deteriorating condition (Song et al., 2012). Therefore, the anxiety and depression experienced by caregivers of patients with brain metastases likely differ from those experienced by those caring for patients with early-stage disease or disease at different primary sites.
The Comprehensive Health Seeking and Coping Paradigm (Nyamathi, 1989) was adapted as the conceptual framework for this study to describe the relationship between antecedent, mediating, and dependent variables that influence caregivers’ perception of and behavior toward caregiver burden. It is a complex, multidimensional framework that depicts highly interactive relationships among its 12 components (Berg, Nyamathi, Christiani, Morisky, & Leake, 2005; Nyamathi, 1989; Nyamathi et al., 2010; Nyamathi, Stein, & Bayley, 2000; Washington, Moxley, & Taylor, 2009). For this study, caregiver burden was conceptualized as an immediate health outcome that could lead to long-term health outcomes that include anxiety and depression (see Figure 1).
FIGURE 1.
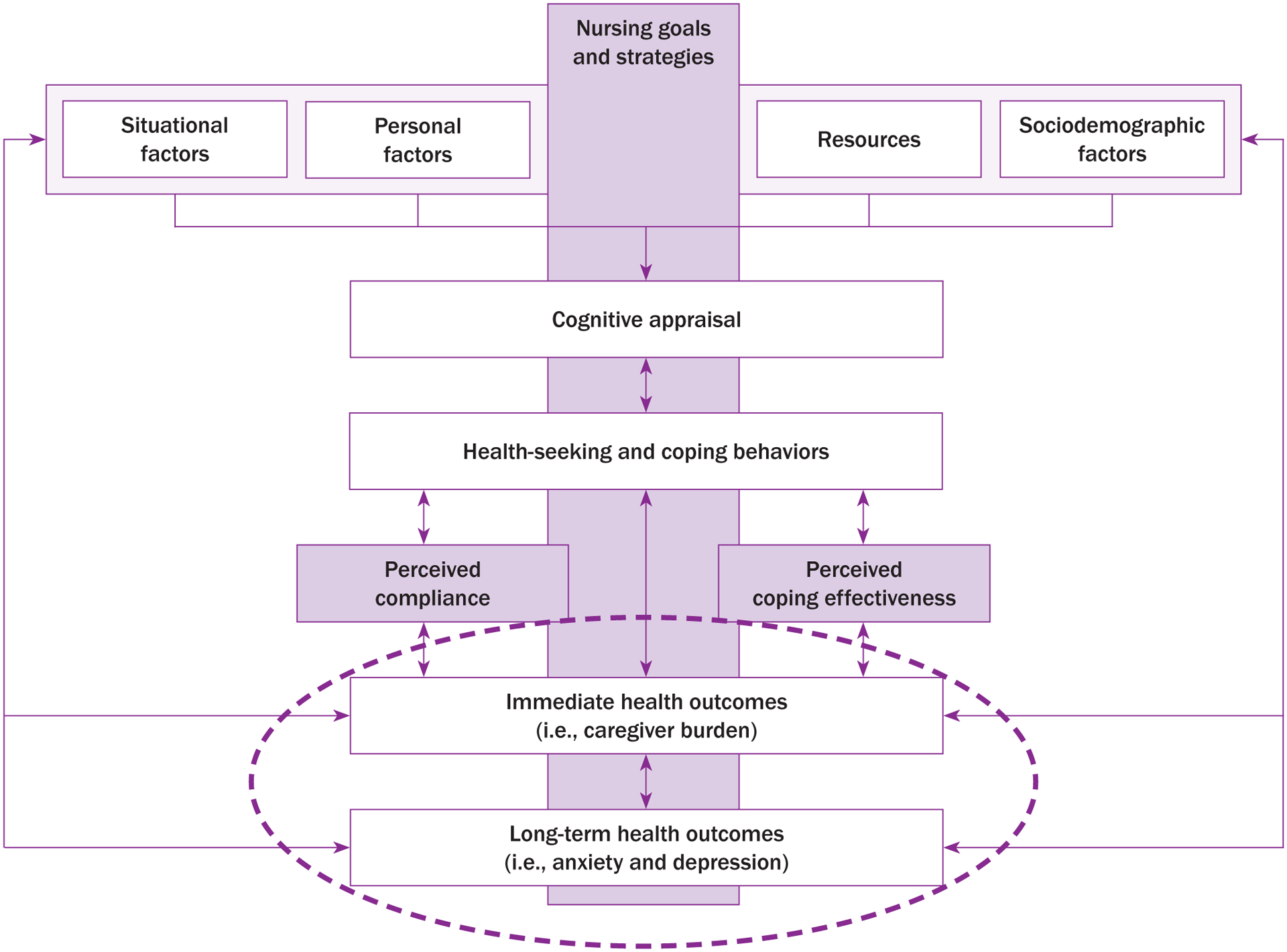
Adapted Comprehensive Health Seeking and Coping Paradigm
Note. From “Comprehensive Health Seeking and Coping Paradigm,” by A. Nyamathi, 1989, Journal of Advanced Nursing, 14, p. 284. Copyright 1989 by John Wiley and Sons. Adapted with permission.
The aim of this study was to describe anxiety, depression, and caregiver burden among caregivers of patients with brain metastases, an area that has not previously been studied. An additional aim was to examine the relationships between (a) caregiver burden and (b) anxiety and depression in caregivers of patients with brain metastases. The authors hypothesized that, similar to the findings in other patient and caregiver populations, increased caregiver burden was associated with increased anxiety and depression.
Methods
This study used a descriptive, cross-sectional design. Data for this study were obtained through a self-administered survey (about 90 minutes in length) that was completed by family caregivers of patients diagnosed with brain metastases from solid tumors. The survey packet had undergone pilot testing to identify potential problems with the questionnaire that could lead to biased answers. This multicampus study was approved by the University of California (UC) Institutional Review Board (IRB) Reliance Registry, with UC Los Angeles (academic affiliation) serving as the reviewing IRB and UC San Diego (study accrual site) serving as the relying IRB.
Sample
Convenience sampling was used to enroll eligible caregivers from the Moores Cancer Center at UC San Diego, a National Cancer Institute–designated comprehensive cancer center in southern California. Participant eligibility criteria included the following: (a) aged 18 years or older; (b) self-identified as the primary caregiver of a patient diagnosed with brain metastases from solid tumors; (c) able to speak, read, and understand English; (d) willing and able to complete a survey; (e) co-resided with the patient with brain metastases; and (f) provided a minimum of four hours of direct care for at least three days per week. Eligibility was not limited by relationship (e.g., spouse, parent, child, sibling, friend), length of the caregiving relationship, or intensity of care provided.
Of the 104 caregivers of patients with brain metastases who consented to participate, 56 completed the survey. The response rate was about 54%, which is similar to most mail-in surveys but lower than what has been reported in studies using comparable approaches (Hanly, Maguire, Hyland, & Sharp, 2015; Hartnett, Thom, & Kline, 2016). Because the survey was anonymous, the authors were precluded from analyzing the reasons for nonparticipation.
Procedure
Because patients with brain metastases meet the definition of human subjects, they were considered to be secondary subjects in this study. A waiver of informed consent for the secondary subjects was granted by the IRB because the study met the requirements outlined in 45 CFR 46.116(d). The caregivers of patients with brain metastases were recruited using flyers that described the study and included the criteria for enrollment and contact information for the study team. The flyers were distributed to physicians and staff in medical oncology offices, as well as the infusion center and radiation oncology department. Potential participants were identified by physicians and staff. Those who requested more information were subsequently approached by a member of the study team. The participants who consented were provided with a survey packet and cover letter stating the purpose of the study. The survey was self-administered and, on completion, was either mailed using a self-addressed stamped envelope or handed to a study team member on site. A $5 gift card was included in the packet as a token of appreciation for taking part in the study.
Outcome Measures
Caregiver data form:
The caregiver data form was developed from a literature review of cancer caregiving studies. The questions included caregiver and patient demographics, social and economic characteristics, description of relationship with the patient, and caregiver health status. Information about the patient, including the history of present illness, date of initial diagnosis, date of diagnosis of brain metastases, cancer treatment received, and comorbidities were also obtained.
Caregiver burden:
The Caregiver Reaction Assessment (CRA), an instrument that reflects the reactions of family members as they care for patients with cancer, was used to measure caregiver burden (Given et al., 1992). The CRA’s 24 items form five distinct uni-dimensional subscales: caregiver esteem (a positive subscale that measures enjoyment and importance of caregiving, 7 items), impact on finances (3 items), impact on health (4 items), impact on schedule (5 items), and lack of family support (5 items) (Sautter et al., 2014). Caregivers rated each item using a Likert-type scale ranging from 1 (strongly agree) to 5 (strongly disagree). A higher score on the caregiver esteem subscale indicates a more positive effect of caregiving, whereas higher scores on the other subscales indicate greater negative effects of caregiving in those domains (Given et al., 1992).
Internal consistency of the subscales was calculated using the Cronbach alpha, with findings ranging from 0.8–0.9. Construct validity of the CRA was explored by correlating the five subscales with the number of patient dependencies in ADLs and the caregiver’s level of depression. These two external variables were selected because of the way they relate to indicators of burden in conceptual models explaining the impact of caring on family members (i.e., number of dependencies in ADLs is commonly viewed as an indicator of stressful demands of care, leading to caregiver burden; caregiver depression is often viewed as an outcome).
Anxiety and depression:
The Hospital Anxiety and Depression Scale (HADS) was used to measure anxiety and depression. This 14-item tool yields subscale scores that classify individuals as having normal, borderline, or clinical anxiety or depression (Zigmond & Snaith, 1983). Each item is scored from 0–3. Total subscale scores range from 0–21 for either anxiety or depression, with scores of 8 or greater indicating emotional distress for both subscales. A literature review conducted by Bjelland, Dahl, Haug, and Neckelmann (2002) reported that correlations between the anxiety and depression subscales of the HADS varied from 0.4–0.74 (), with a Cronbach alpha for the anxiety subscale ranging from 0.68–0.93 () and from 0.67–0.9 () for the depression subscale. In addition, correlations between the HADS and other commonly used questionnaires ranged from 0.49–0.83 (Bjelland et al., 2002).
The HADS was used in a population of caregivers of patients with brain tumors (N = 100) and showed a mean anxiety score of 10.94 (SD = 4.06) and a mean depression score of 7.25 (SD = 3.99). A one-sample t test showed significant differences between caregivers and the control group for anxiety (p < 0.001) and depression (p < 0.001). Using a higher threshold (11 or greater) for anxiety and depression, 52% and 19% of caregivers demonstrated clinically relevant levels of anxiety and depression, respectively (Finocchiaro et al., 2012).
Statistical Analysis
All data were coded and placed into an SPSS®, version 21.0, file. Continuous variables were summarized with means and standard deviations, whereas categorical variables were expressed as frequencies and percentages. Specific items on the CRA and HADS subscales that were negatively worded were reverse coded so that a higher score indicated higher burden, heightened anxiety, or worse depression.
In scoring instruments, items missing within a subscale were imputed as the average of non-missing items in the subscale, assuming that data were missing at random. Logistic regression models were run in SPSS, version 21.0, to predict anxiety and depression as a function of each of the caregiver burden subscales (caregiver esteem, impact on finances, impact on health, impact on schedule, and lack of family support). In addition, a multivariable logistic regression was run for anxiety and for depression with the set of five caregiver burden subscale scores as predictors.
The variables were dichotomized using published scoring interpretation for the CRA and HADS subscales. The scores were added for each of the CRA subscale items and were dichotomized as high (4–5, which indicated agreement with statements or higher perceived burden) or low (1–3, which indicated disagreement with statements or lower perceived burden) (Sautter et al., 2014). For the HADS subscales, a score of 0–7 indicates absence of the condition (either anxiety or depression), whereas a score of 8 or greater indicates presence of the condition (Bjelland et al., 2002). A p value of less than 0.05 was considered to be indicative of statistical significance, and 95% confidence intervals (CIs) were calculated.
Results
From February 2014 to August 2015, the authors received 56 completed surveys from the 104 caregivers of patients with brain metastases. The average caregiver age was 56.3 years (SD = 14.9), and most caregivers were women (n = 39). Fifteen identified as being the primary caregiver for others, and 53 reported that they were covered by health insurance. Table 1 lists additional participant characteristics.
TABLE 1.
Characteristics of Caregivers of Patients With Brain Metastases (N = 56)
| Characteristic | n |
|---|---|
| Current health | |
| Same | 45 |
| Worse | 8 |
| Better | 3 |
| Education | |
| Grade school | 1 |
| High school | 1 |
| Some college | 18 |
| College graduate | 19 |
| Graduate degree | 16 |
| No response | 1 |
| Ethnicity | |
| Hispanic or Latino | 9 |
| Not Hispanic or Latino | 24 |
| Other | 1 |
| No response | 22 |
| Income ($) | |
| Less than 20,000 | 6 |
| 20,001–40,000 | 5 |
| 40,001–75,000 | 10 |
| Greater than 75,001 | 30 |
| No response | 5 |
| Length of time caring for patient | |
| Less than 6 months | 14 |
| 7–12 months | 7 |
| 13–23 months | 10 |
| Greater than 24 months | 24 |
| No response | 1 |
| Marital status | |
| With spouse or partner | 48 |
| Without spouse or partner | 6 |
| No response | 2 |
| Race | |
| Asian | 9 |
| Black or African American | 2 |
| White | 40 |
| No response | 5 |
| Relationship | |
| Spouse or significant other | 38 |
| Son or daughter | 9 |
| Parent | 3 |
| Brother or sister | 2 |
| Son-in-law or daughter-in-law | 1 |
| No response | 3 |
| Religion | |
| Christian | 37 |
| Unaffiliated | 12 |
| Other | 5 |
| No response | 2 |
| Self-assessment of health | |
| Excellent | 19 |
| Good | 29 |
| Fair | 7 |
| Poor | 1 |
Caregiver Burden, Anxiety, and Depression
Table 2 shows the mean scores of the respondents on the five CRA dimensions and the number of caregivers crossing the threshold for burden. Table 3 presents the severity of caregivers’ anxiety or depressive symptoms, as well as the number of caregivers who meet criteria for either anxiety or depression.
TABLE 2.
CB in Caregivers of Patients With Brain Metastases (N = 56)
| Burden Threshold | |||||
|---|---|---|---|---|---|
| Dimension of CB | Range | SD | n | % | |
| Caregiver esteem (7 items) | 7–35 | 28.95 | 4.06 | < 28 = 21 | 38 |
| ≥ 28 = 35 | 63 | ||||
| Impact on finances (3 items) | 3–15 | 7.69 | 3.31 | ≥ 12 = 9 | 16 |
| < 12 = 47 | 84 | ||||
| Impact on health (4 items) | 4–20 | 9.07 | 3.32 | < 16 = 54 | 96 |
| ≥ 16 = 2 | 4 | ||||
| Impact on schedule (5 items) | 5–25 | 17.57 | 4.4 | < 20 = 39 | 70 |
| ≥ 20 = 17 | 30 | ||||
| Lack of family support (5 items) | 5–25 | 10.43 | 3.68 | < 20 = 55 | 98 |
| ≥ 20 = 1 | 2 | ||||
CB—caregiver burden
Note. The 24-item Caregiver Reaction Assessment was used to measure CB. Caregivers rated each item using a Likert-type scale ranging from 1 (strongly agree) to 5 (strongly disagree). Higher scores indicate increased CB except in caregiver esteem.
Note. Because of rounding, percentages may not total 100.
TABLE 3.
Anxiety and Depression in Caregivers of Patients With Brain Metastases (N = 56)
| HADS ST (≥ 8) | |||||
|---|---|---|---|---|---|
| HADS SS | Range | n | % | n | % |
| Anxiety | 34 | 61 | |||
| Normal | 0–7 | 22 | 39 | ||
| Mild | 8–10 | 18 | 32 | ||
| Moderate | 11–14 | 10 | 18 | ||
| Severe | 15–21 | 6 | 11 | ||
| Depression | 29 | 52 | |||
| Normal | 0–7 | 27 | 48 | ||
| Mild | 8–10 | 22 | 39 | ||
| Moderate | 11–14 | 7 | 13 | ||
| Severe | 15–21 | - | - | ||
HADS—Hospital Anxiety and Depression Scale; SS—subscale; ST—screening threshold
Note. The 14-item HADS was used to measure anxiety and depression. Each item is scored from 0–3, and subscale scores range from 0–21 for either anxiety or depression.
Impact on schedule as predictor of anxiety and depression:
Schedule burden was a statistically significant predictor of anxiety and depression (see Table 4). The odds of having mild to severe anxiety were 7.9 times higher (95% CI [1.588, 39.238], p = 0.005) in caregivers who reported schedule burden as a result of their caregiving compared to caregivers who did not report schedule burden. Likewise, the odds of having mild to moderate depression were higher in caregivers who reported schedule burden compared to those who did not report schedule burden (odds ratio [OR] = 13.39, 95% CI [2.666, 67.268], p < 0.001).
TABLE 4.
Burden, Anxiety, and Depression OR and 95% CI (N = 56)
| Anxiety | Depression | |||||
|---|---|---|---|---|---|---|
| Dimension of CB | OR | 95% CI | p | OR | 95% CI | p |
| Caregiver esteem | 0.3 | [0.97, 0.932] | 0.034 | 0.766 | [0.259, 2.264] | 0.629 |
| Impact on finances | 1.357 | [0.302, 6.103] | 0.69 | 2.087 | [0.466, 9.346] | 0.329 |
| Impact on schedule | 7.895 | [1.588, 39.238] | 0.005 | 13.393 | [2.666, 67.268] | < 0.001 |
CB—caregiver burden; CI—confidence interval; OR—odds ratio
Note. High caregiver esteem was considered to be the control (no burden).
Note. No cases with negative outcome were in the no-burden group for the impact on health and lack of family support subscales.
Impact on finances, lack of family support, and impact on health:
Financial burden was not a significant predictor of anxiety and depression in caregivers. For family burden and health burden, no cases with negative outcomes were observed in the control (no burden) group.
Caregiver esteem as predictor of anxiety and depression:
Low caregiver esteem was a statistically significant predictor of anxiety (OR = 0.3, 95% CI [0.097, 0.932], p = 0.034) but not a statistically significant predictor of depression (OR = 0.766, 95% CI [0.259, 2.264], p = 0.629).
Discussion
Distinctive characteristics of brain metastases shape the nature of the caregiving experience. Brain metastases symbolize the beginning of the terminal phase of cancer, which is often marked by progressive focal neurologic deficits and the presence of symptoms that can lead to profound psychosocial distress for the care recipient and the caregiver (Argyriou et al., 2006; Dhandapani et al., 2015; Saria et al., 2015). Cancer caregiving has been shown to increase burden, a concept frequently used in caregiving research, either as a dependent or independent variable that is often operationalized as stress, distress, or strain (Chou, 2000).
Increased caregiver burden has been associated with high rates of psychological distress in advanced cancer and other chronic diseases (Finocchiaro et al., 2012; Papastavrou, Charalambous, Tsangari, & Karayiannis, 2012; Rumpold et al., 2016). For this study, the authors hypothesized that, similar to the findings in other caregiver populations, higher caregiver burden would be associated with increased anxiety and depression.
In this study, the CRA was used for its ability to discriminate between the different dimensions of caregiver burden. In a study exploring the association between hope and burden reported by caregivers of patients with advanced cancer, the mean scores for each of the negative domains of the CRA subscales ranged from 1.8 (SD = 0.6) for lack of family support to 2.7 (SD = 0.9) for impact on schedule, with a score of 4.1 (SD = 0.6) for caregiver esteem (Utne, Miaskowski, Paul, & Rustøen, 2013). The current authors found slightly higher but almost similar results in this sample, with mean scores for the negative domains ranging from 2.1 (SD = 0.7) for lack of family support to 3.5 (SD = 0.9) for impact on schedule, with a score of 4.1 (SD = 0.6) for caregiver esteem. Consistent with findings from other studies using the CRA to measure caregiver burden (Sautter et al., 2014; Utne et al., 2013), this study indicated impact on schedule as the most frequently perceived domain of burden experienced by caregivers of patients with advanced cancer.
Research reports have consistently described the high prevalence of anxiety and depression among cancer caregivers (Friðriksdóttir et al., 2011), noting that these symptoms can vary along the illness trajectory (Song et al., 2011). Higher anxiety and depression scores have been reported among caregivers during the palliative phase, more so than the curative phase, of cancer treatment, even though scores for patient symptom burden were similar (Valeberg & Grov, 2013). In addition, studies have shown that the psychological distress of cancer caregiving not only varies during the illness trajectory but also by diagnosis (Song et al., 2011).
For a closer comparison, data from a study involving 100 caregivers of patients with brain tumors suggest that caregivers of patients with brain tumors live with a clinically significant reduction in their quality of life and a higher level of anxiety. Using the HADS, the study reported a mean score of 10.94 (SD = 4.06) for anxiety and a mean score of 7.25 (SD = 3.99) for depression; these were relatively higher than normative data from a large population (, SD = 3.76 for anxiety, , SD = 3.07 for depression) (Finocchiaro et al., 2012). In the current study, the authors found that more than half of the sample screened positive for depression, and about two-thirds screened positive for anxiety. These findings are consistent with published literature suggesting that a higher rate of psychological distress exists among caregivers of patients with cancer, with anxiety being the most prevalent (Rumpold et al., 2016).
A comprehensive literature review of 16 quantitative and 3 qualitative research articles describing the experience of caregivers of patients with hematologic cancer undergoing a hematopoietic stem cell transplantation identified significant rates of caregiver distress (conceptualized as anxiety and depression) and reported that high levels of subjective burden were the most common predictors (Beattie & Lebel, 2011). The relationship between caregiver burden and psychological distress has been documented in conditions outside of oncology caregiving as well.
In an example involving caregivers of patients after stroke (N = 150), a more acute condition than metastatic cancer, path analysis showed a direct, significant association between caregiver burden and the caregiver’s emotional states (Jaracz, Grabowska-Fudala, & Kozubski, 2012). In 43 primary caregivers of children or adolescents with meningomyelocele, significantly higher levels of anxiety and depressive symptoms were reported in caregivers with higher burden than those with lower burden (Valença, de Menezes, Calado, & de Aguiar Cavalcanti, 2012). The results of the current study revealed that the odds of screening positive for an affective disorder were higher in caregivers of patients with brain metastases who reported higher levels of schedule burden.
The significant impact of caregiving on the caregivers’ daily schedule can be attributed to the complexity of cancer care. From initial diagnosis, patients with cancer and their caregivers face the daunting task of navigating the healthcare system, which has often been described as fragmented and inaccessible (Cantril & Haylock, 2013). The patients and their caregivers find themselves in labyrinthine pathways within the healthcare system, a visual metaphor for the journey that they unwillingly began immediately after hearing the words, “You have cancer.” In addition to managing their day-to-day responsibilities, these caregivers are asked to manage the patient’s medical needs that include, among other things, frequent encounters with healthcare professionals.
Data from published literature reveal that caregiver burden can be differentially expressed among caregivers. Caregiving involvement and caregiving outcomes differed among four types of caregivers (caregivers of individuals with cancer, dementia, or diabetes, or of frail older adults); caregivers of individuals with cancer or dementia reported greater levels of physical burden and psychological distress than did other caregivers (Kim & Schulz, 2008). One of the unwritten assumptions of this study was that caregiving for patients with brain metastases is some-what similar to caregiving for patients with dementia or Alzheimer disease; these are generally viewed as the most burdensome caregiving experiences faced by family members (Kim & Schulz, 2008). Findings from the current study supported previous reports indicating that the odds of having anxiety and depressive symptoms are higher in family caregivers who reported higher levels of caregiver burden.
Limitations
This study is limited by its small sample, which allowed for a cursory analysis but not a more indepth exploration of the relationships between the variables, including a lack of ability to control for co-variates. The cross-sectional design of the study precluded the authors from measuring changes in variables that are likely to change over time. In addition, although the study’s measure of caregiver burden (CRA) allowed investigations of the multidimensional nature of caregiver burden, it limited comparisons of the results with other measures of overall caregiver burden. Another limitation of the study is that the sample was not demographically diverse (ethnicity, income, relationship to care receiver). Growing evidence shows that demographic variables and the caregiver–care recipient relationship can differentially affect the caregiving experience. Also, the study design does not allow interpretation of the direction of causality. Although the data show that schedule burden can be a predictor of anxiety, a direct causal relationship between the two variables cannot be verified. Anxiety may precede the caregiving role, and the presence of anxiety and/or depression may have influenced the perception of burden. A future longitudinal study will help to establish causality among the variables. In consideration of these limitations, readers are cautioned to interpret this study’s conclusions as exploratory.
Implications for Nursing
This study highlights the psychological impact of burden on caregivers of patients with brain metastases. Oncology nurses have significantly contributed to the caregiving literature, particularly in the area of identifying and managing the needs of caregivers of patients with cancer (Kaltenbaugh et al., 2015; Northouse, 2012; Northouse, Katapodi, Schafenacker, & Weiss, 2012; Skalla, Smith, Li, & Gates, 2013; Whisenant, 2011). However, the evidence presented in many of these reports has yet to be adopted as the standard of care.
Oncology nurses need to continuously address caregiver burden and be ready to apply appropriate personalized interventions that are as unique as the caregiver’s experiences. Nurses need to be reminded that most family caregivers take on these caregiving responsibilities as an obligation and may knowingly suppress their needs to avoid contributing to the patient’s guilt or remorse over being the cause of burden. Caregivers may continue to suffer in silence as they juggle caregiving tasks and prioritize the needs of the patient over their own. Nurses must actively initiate the discussion about caregiver burden and integrate the well-being assessment of family caregivers into their plans of care. Enhancing the patient and caregiver experience may help to reduce burden (Lund, Ross, Petersen, & Groenvold, 2015), and improving communication and collaboration within the interdisciplinary healthcare team promotes a more efficient healthcare delivery system that is inclusive of the needs of family caregivers. In addition, oncology nurse navigators, who are experienced cancer nurses with disease-specific knowledge, can facilitate the implementation of patient- and family-centered care throughout the continuum of cancer care and affect patient and caregiver outcomes (McMullen, 2013).
Conclusion
Cancer caregivers represent the hidden morbidity of cancer. The identification and management of caregiver burden, a consequence of a number of inter-related conditions within the caregiving experience, are important considerations for a comprehensive cancer care program. As healthcare providers prepare to see an increase in patients with brain metastases, addressing the needs of the caregiver, the “other patient” who is at an increased risk for various psychological, physical, financial, and social problems, becomes increasingly significant.
Published research on caregiver burden has examined selected populations, with caregivers of patients with dementia and of patients at the end of life being two of the most studied groups. Results across studies examining single populations suggest that differences in caregiver burden may exist with different diseases. However, in the absence of direct comparisons within a single study, knowing whether these are true differences, or whether they result from differences in methods across the individual studies, is difficult (Garlo, O’Leary, Van Ness, & Fried, 2010).
Within neuro-oncology, caregiving research has focused on caregivers of patients with primary brain tumors and has remained relatively silent on the burden of caregivers of patients with brain metastases. In addition, limited exploration has taken place concerning the effects of collective (dyadic) characteristics of the caregiver and the patient on caregiver burden. Findings from this study contributed a more accurate description of caregiver characteristics within the context of caregiving for a loved one with brain metastases. These findings will support and direct future research efforts with the aim of improving the care of cancer caregivers.
Knowledge Translation.
Caregivers of patients with brain metastases represent a unique and increasing population of cancer caregivers.
The anxiety and depression experienced by caregivers of patients with brain metastases are different from those experienced by caregivers of patients with early-stage disease or of those with disease at different primary sites.
Oncology nurses need to continue to be perceptive of caregiver burden and be ready to administer appropriate, individualized interventions.
Acknowledgments
Saria and Nyamathi were supported through funding from the DAISY Foundation and the National Institutes of Health, respectively.
References
- Argyriou AA, Chroni E, Polychronopoulos P, Argyriou K, Papapetropoulos S, Corcondilas M, … Heras P (2006). Headache characteristics and brain metastases prediction in cancer patients. European Journal of Cancer Care, 15, 90–95. doi: 10.1111/j.1365-2354.2005.00621.x [DOI] [PubMed] [Google Scholar]
- Beattie S, & Lebel S (2011). The experience of caregivers of hematological cancer patients undergoing a hematopoietic stem cell transplant: A comprehensive literature review. Psycho-Oncology, 20, 1137–1150. doi: 10.1002/pon.1962 [DOI] [PubMed] [Google Scholar]
- Berg J, Nyamathi A, Christiani A, Morisky D, & Leake B (2005). Predictors of screening results for depressive symptoms among homeless adults in Los Angeles with latent tuberculosis. Research in Nursing and Health, 28, 220–229. doi: 10.1002/nur.20074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, & Neckelmann D (2002). The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research, 52, 69–77. [DOI] [PubMed] [Google Scholar]
- Braithwaite V (1992). Caregiving burden: Making the concept scientifically useful and policy relevant. Research on Aging, 14, 3–27. doi: 10.1177/0164027592141001 [DOI] [Google Scholar]
- Cantril C, & Haylock PJ (2013). Patient navigation in the on-cology care setting. Seminars in Oncology Nursing, 29, 76–90. doi: 10.1016/j.soncn.2013.02.003 [DOI] [PubMed] [Google Scholar]
- Chou KR (2000). Caregiver burden: A concept analysis. Journal of Pediatric Nursing, 15, 398–407. doi: 10.1053/jpdn.2000.16709 [DOI] [PubMed] [Google Scholar]
- Dhandapani M, Gupta S, Dhandapani S, Kaur P, Samra K, Sharma K, … Gupta SK (2015). Study of factors determining caregiver burden among primary caregivers of patients with intracranial tumors. Surgical Neurology International, 6, 160. doi: 10.4103/2152-7806.167084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finocchiaro CY, Petruzzi A, Lamperti E, Botturi A, Gaviani P, Silvani A, … Salmaggi A (2012). The burden of brain tumor: A single-institution study on psychological patterns in caregivers. Journal of Neuro-Oncology, 107, 175–181. doi: 10.1007/s11060-011-0726-y [DOI] [PubMed] [Google Scholar]
- Friðriksdóttir N, Saevarsdóttir P, Halfdánardóttir SÍ, Jónsdóttir A, Magnúsdóttir H, Olafsdóttir KL, … Gunnarsdóttir S (2011). Family members of cancer patients: Needs, quality of life and symptoms of anxiety and depression. Acta Oncologica, 50, 252–258. doi: 10.3109/0284186x.2010.529821 [DOI] [PubMed] [Google Scholar]
- Garlo K, O’Leary JR, Van Ness PH, & Fried TR (2010). Burden in caregivers of older adults with advanced illness. Journal of the American Geriatrics Society, 58, 2315–2322. doi: 10.1111/j.1532-5415.2010.03177.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstenecker A, Nabors LB, Meneses K, Fiveash JB, Marson DC, Cutter G, … Triebel KL (2014). Cognition in patients with newly diagnosed brain metastasis: Profiles and implications. Journal of Neuro-Oncology, 120, 179–185. doi: 10.1007/s11060-014-1543-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given CW, Given B, Stommel M, Collins C, King S, & Franklin S (1992). The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing and Health, 15, 271–283. doi: 10.1002/nur.4770150406 [DOI] [PubMed] [Google Scholar]
- Hanly P, Maguire R, Hyland P, & Sharp L (2015). Examining the role of subjective and objective burden in carer health-related quality of life: The case of colorectal cancer. Supportive Care in Cancer, 23, 1941–1949. doi: 10.1007/s00520-014-2551-2 [DOI] [PubMed] [Google Scholar]
- Hartnett J, Thom B, & Kline N (2016). Caregiver burden in end-stage ovarian cancer. Clinical Journal of Oncology Nursing, 20, 169–173. doi: 10.1188/16.CJON.169-173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt CK (2003). Concepts in caregiver research. Journal of Nursing Scholarship, 35, 27–32. doi: 10.1111/j.1547-5069.2003.00027.x [DOI] [PubMed] [Google Scholar]
- Jaracz K, Grabowska-Fudala B, & Kozubski W (2012). Caregiver burden after stroke: Towards a structural model. Neurologia i Neurochirugia Polska, 46, 224–232. doi: 10.5114/ninp.2012.29130 [DOI] [PubMed] [Google Scholar]
- Kaltenbaugh DJ, Klem ML, Hu L, Turi E, Haines AJ, & Hagerty Lingler J (2015). Using Web-based interventions to support caregivers of patients with cancer: A systematic review. Oncology Nursing Forum, 42, 156–164. doi: 10.1188/15.ONF.156-164 [DOI] [PubMed] [Google Scholar]
- Kim Y, & Schulz R (2008). Family caregivers’ strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health, 20, 483–503. doi: 10.1177/0898264308317533 [DOI] [PubMed] [Google Scholar]
- Lambert SD, Girgis A, Lecathelinais C, & Stacey F (2012). Walking a mile in their shoes: Anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Supportive Care in Cancer, 21, 75–85. doi: 10.1007/s00520-012-1495-7 [DOI] [PubMed] [Google Scholar]
- Lee Y-H, Liao Y-C, Liao W-Y, Shun S-C, Liu Y-C, Chan J-C, … Lai Y-H (2013). Anxiety, depression and related factors in family caregivers of newly diagnosed lung cancer patients before first treatment. Psycho-Oncology, 22, 2617–2623. doi: 10.1002/pon.3328 [DOI] [PubMed] [Google Scholar]
- Lund L, Ross L, Petersen MA, & Groenvold M (2015). The interaction between informal cancer caregivers and health care professionals: A survey of caregivers’ experiences of problems and unmet needs. Supportive Care in Cancer, 23, 1719–1733. doi: 10.1007/s00520-014-2529-0 [DOI] [PubMed] [Google Scholar]
- McMullen L (2013). Oncology nurse navigators and the continuum of cancer care. Seminars in Oncology Nursing, 29, 105–117. doi: 10.1016/j.soncn.2013.02.005 [DOI] [PubMed] [Google Scholar]
- Mystakidou K, Parpa E, Panagiotou I, Tsilika E, Galanos A, & Gouliamos A (2013). Caregivers’ anxiety and self-efficacy in palliative care. European Journal of Cancer Care, 22, 188–195. doi: 10.1111/ecc.12012 [DOI] [PubMed] [Google Scholar]
- Northouse LL (2012). Helping patients and their family caregivers cope with cancer. Oncology Nursing Forum, 39, 500–506. doi: 10.1188/12.ONF.500-506 [DOI] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Schafenacker AM, & Weiss D (2012). The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Seminars in Oncology Nursing, 28, 236–245. doi: 10.1016/j.soncn.2012.09.006 [DOI] [PubMed] [Google Scholar]
- Nyamathi A (1989). Comprehensive Health Seeking and Coping Paradigm. Journal of Advanced Nursing, 14, 281–290. doi: 10.1111/j.1365-2648.1989.tb03415.x [DOI] [PubMed] [Google Scholar]
- Nyamathi AM, Stein JA, & Bayley LJ (2000). Predictors of mental distress and poor physical health among homeless women. Psychology and Health, 15, 483–500. doi: 10.1080/08870440008402008 [DOI] [Google Scholar]
- Nyamathi AM, William RR, Ganguly KK, Sinha S, Heravian A, Albarrán CR, … Rao PR (2010). Perceptions of women living with AIDS in rural India related to the engagement of HIV-trained accredited social health activists for care and support. Journal of HIV/AIDS and Social Services, 9, 385–404. doi: 10.1080/15381501.2010.525474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papastavrou E, Charalambous A, Tsangari H, & Karayiannis G (2012). The burdensome and depressive experience of caring: What cancer, schizophrenia, and Alzheimer’s disease caregivers have in common. Cancer Nursing, 35, 187–194. doi: 10.1097/NCC.0b013e31822cb4a0 [DOI] [PubMed] [Google Scholar]
- Paradise M, McCade D, Hickie IB, Diamond K, Lewis SJ, & Naismith SL (2015). Caregiver burden in mild cognitive impairment. Aging and Mental Health, 19, 72–78. doi: 10.1080/13607863.2014.915922 [DOI] [PubMed] [Google Scholar]
- Penrod JD, Kane RA, Kane RL, & Finch MD (1995). Who cares? The size, scope, and composition of the caregiver support system. Gerontologist, 35, 489–497. doi: 10.1093/geront/35.4.489 [DOI] [PubMed] [Google Scholar]
- Perlick D, Clarkin JF, & Sirey JA (1995). Caregiver burden. Psychiatric Services, 46, 836. [DOI] [PubMed] [Google Scholar]
- Rumpold T, Schur S, Amering M, Kirchheiner K, Masel EK, Watzke H, & Schrank B (2016). Informal caregivers of advanced-stage cancer patients: Every second is at risk for psychiatric morbidity. Supportive Care in Cancer, 24, 1975–1982. doi: 10.1007/s00520-015-2987-z [DOI] [PubMed] [Google Scholar]
- Ryba KL, Johnson K, Ulstad K, & Owen G (2012, October). Caregiving in context: Understanding caregivers’ networks of support. Retrieved from http://www.wilder.org/Wilder-Research/Publications/Studies/Caregiving%20in%20Context/Caregiving%20in%20Context%20-%20Understanding%20Caregivers’%20Networks%20of%20Support,%20Full%20Report.pdf
- Saria MG, Piccioni D, Carter J, Orosco H, Turpin T, & Kesari S (2015). Current perspectives in the management of brain metastases. Clinical Journal of Oncology Nursing, 19, 475–479. doi: 10.1188/15.CJON.475-478 [DOI] [PubMed] [Google Scholar]
- Sautter JM, Tulsky JA, Johnson KS, Olsen MK, Burton-Chase AM, Lindquist JH, … Steinhauser KE (2014). Caregiver experience during advanced chronic illness and last year of life. Journal of the American Geriatrics Society, 62, 1082–1090. doi: 10.1111/jgs.12841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmieder K, Keilholz U, & Combs S (2016). The interdisciplinary management of brain metastases. Deutsches Arzteblatt International, 113, 415–421. doi: 10.3238/arztebl.2016.0415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood PR, & Baer MB (2011). Symptom management and psychological issues. In Allen DH & Rice LL (Eds.), Central nervous system cancers (pp. 115–133). Pittsburgh, PA: Oncology Nursing Society. [Google Scholar]
- Sherwood PR, Price TJ, Weimer J, Ren D, Donovan HS, Given CW, … Marsland AL (2016). Neuro-oncology family caregivers are at risk for systemic inflammation. Journal of Neuro-Oncology, 128, 109–118. doi: 10.1007/s11060-016-2083-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalla KA, Smith EM, Li Z, & Gates C (2013). Multidimensional needs of caregivers for patients with cancer. Clinical Journal of Oncology Nursing, 17, 500–506. doi: 10.1188/13.CJON.17-05AP [DOI] [PubMed] [Google Scholar]
- Sklenarova H, Krümpelmann A, Haun MW, Friederich H-C, Huber J, Thomas M, … Hartmann M (2015). When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer, 121, 1513–1519. doi: 10.1002/cncr.29223 [DOI] [PubMed] [Google Scholar]
- Song JI, Shin DW, Choi JY, Kang J, Baek YJ, Mo HN, … Lee OK (2012). Quality of life and mental health in the bereaved family members of patients with terminal cancer. Psycho-Oncology, 21, 1158–1166. doi: 10.1002/pon.2027 [DOI] [PubMed] [Google Scholar]
- Song JI, Shin DW, Choi JY, Kang J, Baik YJ, Mo H, … Kim EJ (2011). Quality of life and mental health in family caregivers of patients with terminal cancer. Supportive Care in Cancer, 19, 1519–1526. doi: 10.1007/s00520-010-0977-8 [DOI] [PubMed] [Google Scholar]
- Stelzer KJ (2013). Epidemiology and prognosis of brain metastases. Surgical Neurology International, 4(Suppl. 4), S192–S202. doi: 10.4103/2152-7806.111296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utne I, Miaskowski C, Paul SM, & Rustøen T (2013). Association between hope and burden reported by family caregivers of patients with advanced cancer. Supportive Care in Cancer, 21, 2527–2535. doi: 10.1007/s00520-013-1824-5 [DOI] [PubMed] [Google Scholar]
- Valeberg BT, & Grov EK (2013). Symptoms in the cancer patient: Of importance for their caregivers’ quality of life and mental health? European Journal of Oncology Nursing, 17, 46–51. doi: 10.1016/j.ejon.2012.01.009 [DOI] [PubMed] [Google Scholar]
- Valença MP, de Menezes TA, Calado AA, & de Aguiar Cavalcanti G (2012). Burden and quality of life among caregivers of children and adolescents with meningomyelocele: Measuring the relationship to anxiety and depression. Spinal Cord, 50, 553–557. doi: 10.1038/sc.2012.10 [DOI] [PubMed] [Google Scholar]
- Vaughan D (2012, September 17). Cancer patient’s mental illness may be an added challenge for caregiver. Retrieved from http://www.curetoday.com/publications/cure/2012/fall2012/cancer-patients-mental-illness-may-be-an-added-challenge-for-caregiver?p=1
- Washington OG, Moxley DP, & Taylor JY (2009). Enabling older homeless minority women to overcome homelessness by using a life management enhancement group intervention. Issues in Mental Health Nursing, 30, 86–97. doi: 10.1080/01612840802597580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisenant M (2011). Informal caregiving in patients with brain tumors [Online exclusive]. Oncology Nursing Forum, 38, E373–E381. doi: 10.1188/11.ONF.E373-E381 [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]


