Abstract
Extratemporal facial nerve schwannomas are rare entity. Pre-operative assessment is mostly inconclusive with differential diagnosis of parotid tumors. We hereby report a case of 28 years female who presented with painless swelling in right parotid region with normal facial nerve function. Ultrasonography was suggestive well circumscribed and homogenous mass arising from the deep lobe of parotid gland. The Fine-needle aspiration cytology came out to be inconclusive. For further characterization of the tumor contrast enhanced MR imaging was performed. The MR imaging revealed well-defined cystic, heterogeneous, pear-shaped mass lesion situated near the stylomastoid foramen. Post operatively the mass came out to be schwannoma on histopathological examination.
Keywords: Extratemporal, Schwannoma, Facial nerve, Histopathological examination
Introduction
A neurilemmoma or schwannoma, is an ectodermal benign encapsulated tumor originating from Schwann's cells. Facial nerve schwannomas are rare, the majority of them originate from the temporal segment with very few about 9% being extratemporal in origin [1].
Preoperative diagnosis is difficult as the usual presentation is of slow growing mass in parotid region which is easily confused with parotid tumors. As tumor originates from the nerve sheath, large tumors compress the nerve and cause dysfunction rather than invading the nerve as occurs in malignant lesions. 20% cases present with facial nerve involvent [2] but post operatively facial nerve palsy is common because of its close proximity to the nerve fibers. Post operative histopathology usually makes the confirmatory diagnosis. As there is a very low chance of recurrence; the treatment of choice is surgical excision [3]. Post operative morbidities could be minimized by intraoperative use of microscope and facial nerve monitoring.
Case Report
A 28-year-old female presented to the ENT Outpatient Department with a complain of right parotid swelling. The patient’s only complaint was of a painless mass at the right infra-auricular region for the last 1 year, there was no complain of facial weakness, inability to close the eye, or deviation of angle of the mouth. The swelling gradually increased in size and was not associated with pain or fever, there was no history of weight loss, restriction of jaw movement, ear discharge and decreased hearing. The clinical examination revealed a nontender 3*2-cm swelling, with smooth surface and well-defined margins, non-mobile, not adherent to the overlying skin, but fixed to the underlying tissue. The patient had House-Brackmann Grade 1 facial nerve function (Fig. 1). Ultrasonography finding was suggestive of right parotid gland deep lobe tumour, lying in close relation to stylomastoid foramen, the lesion was superficial to internal jugular vein. Fine-needle aspiration cytology was performed but did not produce diagnostic material. MR imaging with the contrast enhancement was performed to know the nature of mass along with detailed extent of it. Contrast-enhanced MR imaging of the neck revealed a tumour (19x17x33mm APxTxCC) well-defined cystic, heterogeneous, pear-shaped mass lesion arising from the facial nerve on right side extending extracranial from the stylomastoid and lying in the right parotid region in close proximity to its deep lobe (Figs. 2, 3). Contrast-Enhanced Magnetic Resonance Imaging (CE-MRI) gave the impression of two differentials, pleomorphic adenoma and facial nerve schwannoma. Keeping in view of clinical, cytological and radiological profiles, we planned for right-sided total parotidectomy with Modified Blair’s incision.
Fig. 1.

Preoperative House-Brackmann Grade 1 facial nerve function
Fig. 2.
CE-MRI of the neck revealing a tumour well-defined cystic, heterogeneous, pear-shaped mass lesion arising from the facial canal on right side extending extracranial from the stylomastoid and lying in the right parotid region in close proximity to its deep lobe
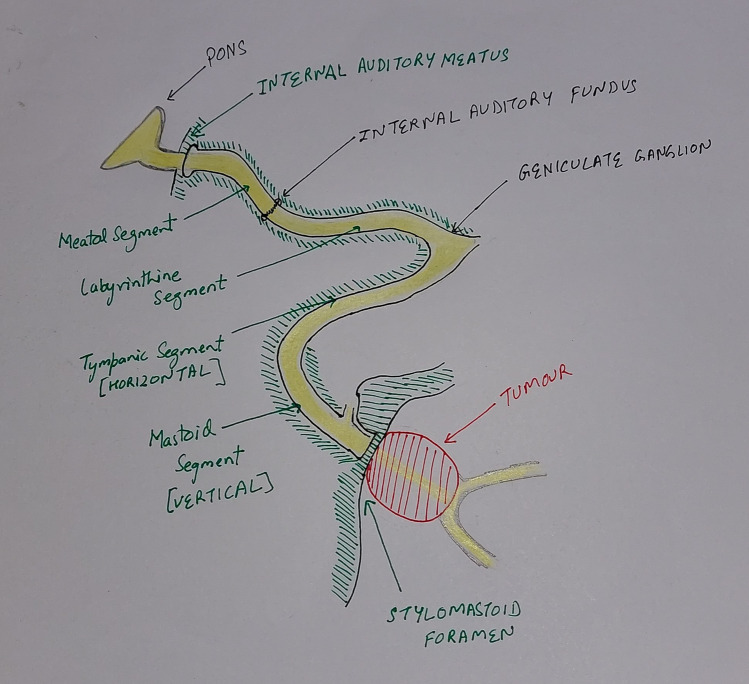
Fig. 3.
Diagram depicting site of lesion
The surgical excision of this tumour was challenging because of its deep location, origin from the facial nerve and proximity to blood vessels. Intra-operatively surprisingly, the tumor was seen to be arising from the main trunk of the facial nerve in close proximity to the stylomastoid foramen. The facial nerve monitor identified a thin sheath of nerve fibers covering the tumor (Fig. 4). The mass was well encapsulated with normal adjoining parotid tissue and was removed in toto and sent for histopathological examination (Fig. 5). The thin sheath of nerve fibers was successfully dissected and preserved under the guidance of nerve monitor. Histopathology showed encapsulated hypercellular and hypocellular areas with palisading of spindle cells (Fig. 6). Immuno-histochemistry reviled highly positive for S-100 marker, thus giving an impression of Schwannoma (Fig. 7). Postoperative recovery of the patient was good with no facial nerve palsy.
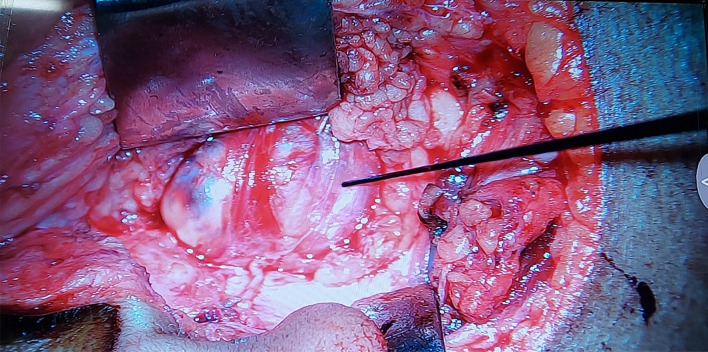
Fig. 4.
Thin sheath of nerve fibers covering the tumor
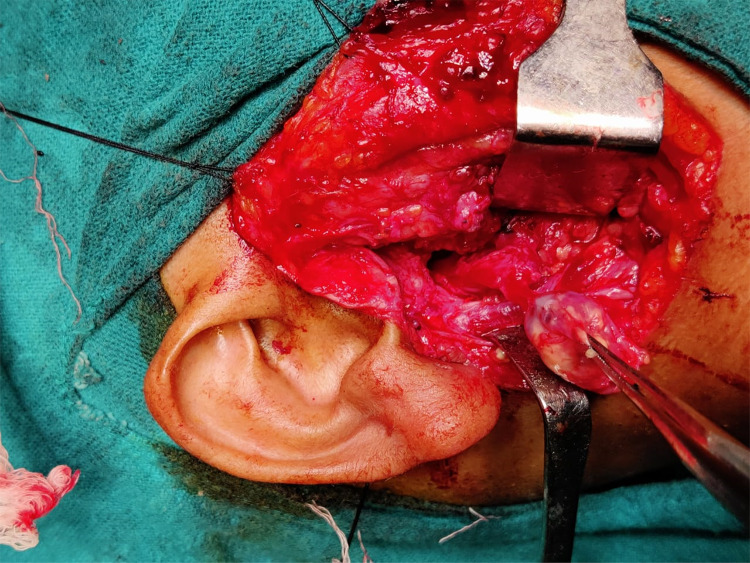
Fig. 5.
Well encapsulated with normal adjoining parotid tissue and was removed in toto
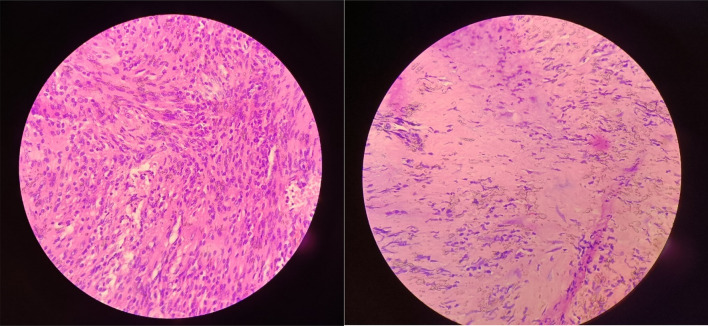
Fig. 6.
Histology Antoni A (×100) Antoni B (×100)
Fig. 7.
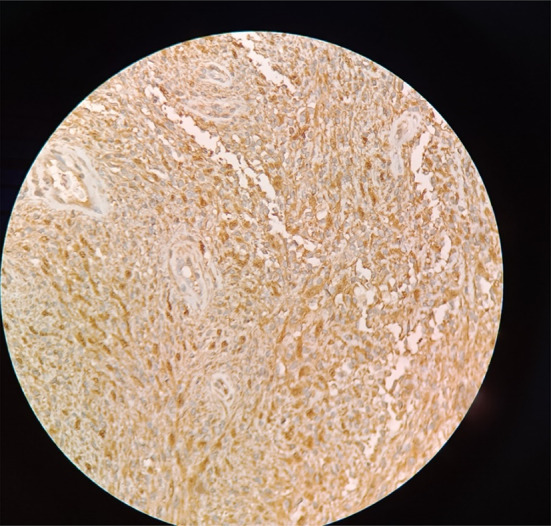
Immunohistochemistry S-100 POSITIVE
Discussion
Schwannomas are rare benign, slow-growing, encapsulated tumors that arise from Schwann cells. Till date, very few cases of extratemporal facial nerve schwannomas had been reported in the literature, though its first description was back in 1927 [4]. Preoperative diagnosis of extratemporal facial nerve schwannoma still remains a tough grind because of its rarity and discrepant features. In a study of 3722 diagnosed cases of schwannomas, only 29 cases of facial schwannoma were found and out of these, only eight arose from intra-parotid portion of the facial nerve [5]. In another study, there were only seven cases of facial schwannoma out of 113 patients of nerve sheath tumors of the head-and-neck region [6].
Even though the tumor arises from the facial nerve, contradictorily in majority of the cases there is no involvement of the nerve, and the most common presenting feature is that of asymptomatic parotid swelling which mimics a benign parotid swelling. The clinical presentation remains discrepant, from an asymptomatic mass to a painful parotid mass with facial nerve dysfunction [7], so it remains troublesome to make its preoperative diagnosis. FNAC in majority of the cases, is nonspecific and may even go in favor of pleomorphic adenoma [8]. Histopathological examination is diagnostic, revealing two patterns of histology: Antoni A and Antoni B, Antoni A regions are compact and cellular, with elongated spindle cells and whorling or palisading nuclei, aligned in rows (Verocay bodies). Antoni type B histology is loose and much less cellular, with a spongy appearance. These tumors are S-100 positive on Immunochemistry. Treatment of extratemporal schwannoma is surgical excision. Intra-operatively if the tumor seems to be adherent to the facial nerve, frozen section examination should be done to rule out malignancy [9]. The involvement of the main trunk of the facial nerve usually results in unsatisfactory outcomes thus, the surgery should be aimed at the preservation of the facial nerve functions as much as possible [10]. Use of microscope along with the facial nerve monitoring can help to increase the chances of facial nerve preservation.
In this case, preoperatively although the diagnosis was not certain, we were able to completely dissect the tumor and also successfully preserve the nerve. Intra-operatively the mass was seen to be arising from the main trunk of the facial nerve, which was later confirmed as schwannoma on histopathology.
Conclusion
Extratemporal facial nerve schwannomas are rare and very few of them will present with facial palsy. They should be kept in the differential diagnosis of parotid swellings, even though it is exceedingly difficult to make a diagnosis of schwannoma preoperatively. It is sometimes extremely difficult to preserve the facial nerve function because some fibers might get injured during surgery because of uncertainty; hence, the use of a facial nerve monitor along with a microscope intraoperatively is a boon for the surgeon.
Declrations
Conflict of interest
All author declares no conflict of interest.
Consent to participate
The authors certify that they have obtained all appropriate patient consent forms. Consent was taken for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pawan Kumar Mishra, Email: pawan93.94@gmail.com.
Nainsi Gupta, Email: girl.nainsi@gmail.com.
Aftab Ahmed, Email: aftab2k3@gmail.com.
Murad Ahmed, Email: muraddd3140@gmail.com.
S. C. Sharma, Email: scsharmaent@yahoomail.com
References
- 1.Gross BC, Carlson ML, Moore EJ, Driscoll CL, Olsen KD. The intraparotid facial nerve schwannoma: a diagnostic and management conundrum. Am J Otolaryngol. 2012;33:497–504. doi: 10.1016/j.amjoto.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Seo BF, Choi HJ, Seo KJ, Jung SN. Intraparotid facial nerve schwannomas. Arch Craniofac Surg. 2019;20:71–74. doi: 10.7181/acfs.2018.02250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ulku CH, Uyar Y, Acar O, Yaman H, Avunduk MC. Facial nerve schwannomas: a report of four cases and a review of the literature. Am J Otolaryngol. 2004;25:426–431. doi: 10.1016/j.amjoto.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Simone M, Vesperini E, Viti C, Camaioni A, Lepanto L, Raso F. Intraparotid facial nerve schwannoma: two case reports and a review of the literature. Acta Otorhinolaryngol Ital. 2018;38:73–77. doi: 10.14639/0392-100X-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caughey RJ, May M, Schaitkin BM. Intraparotid facial nerve schwannoma: diagnosis and management. Otolaryngol Head Neck Surg. 2004;130:586–592. doi: 10.1016/j.otohns.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Tabriz HM, Razmpa E, Abdollahi A. Head and neck nerve sheath tumors: a 10-year evaluation in Iran. Iran J Pathol. 2009;4:118–122. [Google Scholar]
- 7.Ma Q, Song H, Zhang P, Hou R, Cheng X, Lei D. Diagnosis and management of intraparotid facial nerve schwannoma. J Craniomaxillofac Surg. 2010;38:271–273. doi: 10.1016/j.jcms.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Assad L, Treaba D, Ariga R, Bengana C, Kapur S, Bhattacharya B, et al. Fine-needle aspiration of parotid gland schwannomas mimicking pleomorphic adenoma: a report of two cases. Diagn Cytopathol. 2004;30:39–40. doi: 10.1002/dc.10355. [DOI] [PubMed] [Google Scholar]
- 9.Fyrmpas G, Konstantinidis I, Hatzibougias D, Vital V, Constantinidis J. Intraparotid facial nerve schwannoma: management options. Eur Arch Oto Rhino Laryngol. 2008;265:699–703. doi: 10.1007/s00405-007-0521-8. [DOI] [PubMed] [Google Scholar]
- 10.Li S, Lu X, Xie S, Li Z, Shan X, Cai Z. Intraparotid facial nerve schwannoma: a 17-year, single-institution experience of diagnosis and management. Acta Oto Laryngol. 2019;139:444–450. doi: 10.1080/00016489.2019.1574983. [DOI] [PubMed] [Google Scholar]