Abstract
Introduction
Otomycosis is a fungus-causing superficial infection of the external auditory canal that is common in otolaryngology practice. Though it is a worldwide infection, but is more prevalent in warm and humid regions. There has been rise in the occurrence of otomycosis in the last few years because of the extensive usage of antibiotic eardrops. Other influencing reasons for the occurrence of otomycosis is swimming, an immunocompromised host (e.g.: DM, AIDs) pregnancy, post-canal wall down mastoidectomy, tympanic membrane perforation, hearing aids and self-inflicted injuries.
Methods
Approval from the institutional ethics committee and penned informed agreement from all patients involved in the examination were obtained. 40 patients were included in the study, starting from 1stAugust to 30th September 2021, which emphasized on otomycosis infection with central tympanic membrane perforation. Physical findings such as whitish ear discharge and the presence of hyphae in the EAC, the ear drum, the middle ear mucosa were used to diagnose otomycosis.
Result
20 patients of patched group and 20 patients of non-patched group did not visit for follow up. Data here is for patients who followed-up for 3 weeks. Any significant observation regarding statistical variation in the age, size of perforation, mycological analysis and pure tone audiometry among the two groups were not seen.
Conclusion
To conclude, we state that treatment with clotrimazole solution in patched group is safe in managing otomycosis with tympanic membrane perforation. Otomycosis is a fungus causing surface infection of the external auditory canal that otolaryngologists routinely diagnose by medical examination. In acute otomycosis, overgrowth of the fungus in the external auditory canal is due to increased humidity.
Keywords: Otomycosis, Fungal infection, Ear surgery, Tympanic membrane perforation, Castellani’s solution
Introduction
Otomycosis is a fungus causing superficial infection of the external auditory canal that is common in otolaryngology practices. Though it is a worldwide infection, but is more prevalent in warm and humid regions. There has been increase in the occurrence of otomycosis in last few years because of the extensive usage of antibiotic eardrop. [1] Other influencing reasons for the occurrence of otomycosis are swimming, immunocompromised host (e.g.: DM, AIDs), pregnancy, post-canal wall down mastoidectomy, tympanic membrane perforation, hearing aids and self-inflicted injuries (e.g., by cotton swabs). A majority of the diagnoses are clinical. The most prevalent fungal pathogenic microbes are Aspergillus and Candida species. Of all the cases, 9% of otitis externa are caused by fungal pathogens, but this figure seems to rising, apparently due to the excessive usage of topical antibiotics. Treatment suggestions include local debridement along with antifungal drugs. An occasionally reported problem of otomycosis is tympanic membrane perforation. The prevalence of tympanic membrane perforation in otomycosis was estimated to be 11% in a medical assessment and it was commonly seen in otomycosis caused by Candida species. [2, 3]
The chief symptom for otomycosis is itching, which is often referred to as one of the distinctive finding’s in up to 93% in certain studies. Ear ache and hearing loss are the other common symptoms in this infection. Treatment with the topical clotrimazole give good results against both Aspergillus and Candida species. But, if the otomycosis persists then systemic antifungal and topical antifungal medication is essential. [4].
The main objective of this analysis was to figure out, the percentage of individuals having perforated tympanic membrane with otomycosis and to discuss the various treatment options. [5].
Methods
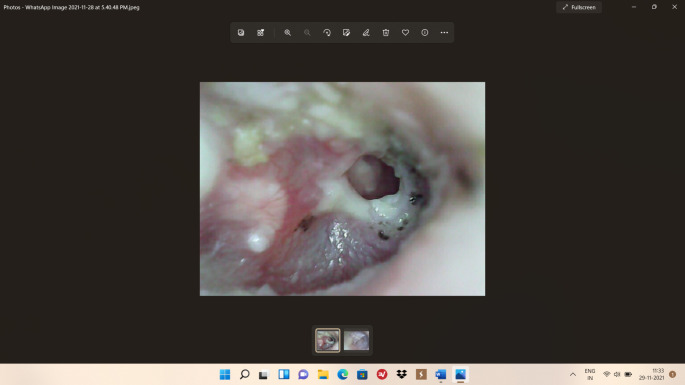
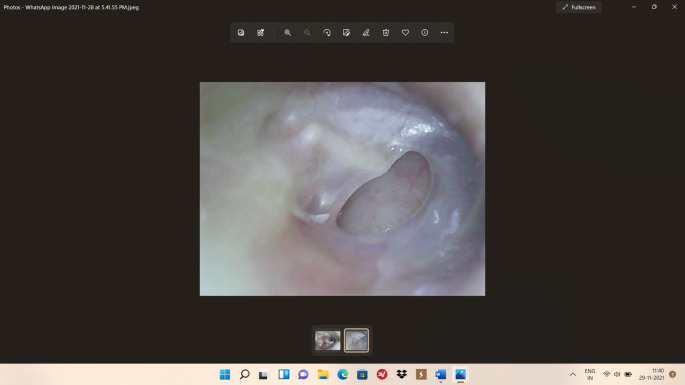
Approval from the regional ethics committee and penned informed agreement from all patients involved in the examination were obtained. 40 patients were included in the study, starting from 1st August to 30th September-2021, which focused on otomycosis infection with tympanic membrane perforation. Otomycosis (Fig. 1) was diagnosed based on the physical findings such as whitish ear discharge and appearance of hyphae in the external auditory canal, ear drum or middle ear mucosa. The study excluded individuals with retraction pocket, cholesteatoma, preceding ear surgery, psoriasis, seborrheic dermatitis, eczema, earlier use of antibiotics, topical corticosteroids or antifungal medicine and patients with a hearing aid in the affected ear. Diabetes mellitus and other chronic granulomatous diseases were identified as co-morbidities. These 40 patients were further sub-divided into two sub-groups: patched and the un-patched group. After secretions and otomycosis debris are cleaned from the external auditory canal, Castellani’s solution (containing 0.08 g boric acid, 0.4 g phenol, 0.04 g fuchsine, 0.8 g resorcinol, 0.4 mL acetone, 0.85 mL alcohol, and 10 mL distilled water) was applied in the external auditory canal using port cotton in both groups. Antifungal medications, either systemic or topical, was not administered. The perforated tympanic membrane was coated with a sterilised patch of carbon paper and soaked in Castellani’s solution in patients in the Patched group to block discharge from the middle ear to the external auditory canal. (Fig. 2)
Fig. 1.
Tympanic membrane perforation with Otomycosis
Fig. 2.
Tympanic membrane perforation with no Otomycosis
The intensity of Otomycosis was ranked based on the physical findings and the presence of spore/hyphae in the EAC, tympanic membrane and middle ear. ‘0 = none’ (no mycotic infection), ‘1 = mild’ (mycotic hyphae on any one wall of the EAC), ‘2 = moderate’ (mycotic hyphae on any two walls of the EAC) and ‘3 = severe’ (mycotic hyphae on two or more sides of the EAC and on the tympanic membrane). Overall dryness was considered as successful recovery (score = 0) with no hyphae or discharge in the EAC.
The patients were followed up on the 1st, 2nd and 3rd weeks during which the fluid and debris from the EAC were removed. All patients were inspected under an otoscope at every visit, Castellani’s solution was applied to EAC with port cotton only once per visit and the current disease severity score was noted. Castellani’s solution was not used if the patient had made a complete recovery (score = 0), but the patient was advised to return the following week for consecutive follow-up. The following parameters were used to compare the prognosis of patients in the patched and non-patched groups: (1) number of patients by disease severity score at each visit, (2) time taken for complete healing process (disease severity score = 0), and (3) number of patients with relapse after full recovery during follow-up.
Statistical analysis
SPSS version 23.0 was used for statistical analysis (SPSS Inc., IBM, Armonk, New York, United States of America). The Chi-square test was used to evaluate gender variation and the student’s t-test was used to evaluate age difference between patients in the patched and non-patched group. The Chi-square test was further used to contrast categorical differences in two groups, like the number of cases based on disease intensity score at weekly visits, the number of patients who experienced disease recurrence during the examination and the number of patients who had co-morbidities. The time taken by patients in the patched and non-patched groups to fully recover was compared using the Mann-Whitney U test. P-value of 0.05 is considered as statistically significant.
Result
20 patients of patched group and 20 patients of non-patched group did not visit for follow up. Data here is for patients who followed-up for 3 weeks. Any significant observation regarding statistical variation in the age, size of perforation, mycological analysis and pure tone audiometry among the two groups were not seen (Table 1).
Table 1.
Demographic characteristic of patients
| Patched group | Non patched group | |
|---|---|---|
| No of patients | 20 | 20 |
|
Age(yrs.) Range Mean |
25-45yrs 35yrs |
25-45yrs 35yrs |
| Male | 12 | 11 |
| Female | 8 | 9 |
In patched group, patients took the treatment well and were satisfied. 5 patients (12%) experienced slight burning sensation in ear for one or two days after taking treatment. In all the patients, pruritis steadily alleviated within the initial one week. 9 patients (23%) required removal of certain fungal clusters by suction in second visit. By the completion of treatment, every patient’s external ear canal skin and tympanic membrane appeared normal. The pure tone audiometry averaged 20 ± 5dB. (Table 2)
Table 2.
Mean Pure Tone Audiometry
| Patched group | Non patched group | |
|---|---|---|
| Mean PTA | 20 ± 5 dB | 30 ± 5 dB |
In non-patched group patients, itching got subsided but the feeling of obstruction and discharge was observed in the ear. In all the patients, after 3 weeks of treatment, skin of external ear canal appeared normal and the debris was cleared off from. The average pure tone audiometry was 30 ± 5dB. (Tables 2 and 3)
Table 3.
Size of TM perforation
| Patched group | Non patched group | |
|---|---|---|
| Small | 8 | 7 |
| Medium | 12 | 13 |
Statistically substantial variation among the 2 groups was not seen as far as the PTA was concerned. During the follow up period of 3 weeks, 5 non-patched group patients experienced relapse of otomycosis while there was no relapse seen in patched group patients. This is statistically important. 3 patients (16.5%) of patched group and 1 patient (5%) of non-patched group had complete closure of the perforation of tympanic membrane by the end of 3 months. (Table 4)
Table 4.
Treatment & follow up
| Patched group | Non patched group | |
|---|---|---|
| Treatment period (weeks) | 3 Weeks | 3 Weeks |
| Post-treatment PTA (dB) | 10 ± 5 | 20 ± 5 |
| Perforation closure | 3 | 1 |
| Recurrence after 3 months | 0 | 5 |
PTA: pure tone audiometry TM: tympanic membrane dB: decibel
Discussion
Disease relapse rates and severity score in patched group patients improved significantly in the first, second and third weeks of follow-up, according to the current research. At all the visits, the patched group had a much higher percentage of patients who had achieved a complete recovery. [6].
Otomycosis is a persistent fungal infection of the ear (EAC) with an acute onset. It is more prevalent in chronic otitis media and in the cavity of a canal wall down mastoidectomy. Swimming, warm climate, dry and dusty work space, loss of cerumen, immunological suppressants and tympanic membrane damage are few of the factors to develop otomycosis. Quite possibly the main factor for otomycosis is long term exposure to moisture. [7].
The most frequent fungi that cause otomycosis are moulds (Aspergillus), yeast (Candida species), and dermatophytes. In a recent investigation, we observed bilateral fungal infection in ten of the forty otomycosis patients with chronic otitis media being the most common determinant. During our investigation, we noticed that Aspergillus species accounted for 56.6%, Candida species for 16.7%, and Penicillium species for 10%. In 46.3% of cases, there was a mixed infection. A significant relevant history, oto-microscopy and mycological examination are usually used to diagnose EAC fungal infection. [8].
Otomycosis is a non-invasive infection that can be acute or chronic and it usually recurs in individuals who have a perforated tympanic membrane. The infection frequently affects both the EAC and the tympanic membrane. Otomycosis was assessed in our study depending on the physical symptoms and the extent of the hyphae in the EAC and tympanic membrane. [9].
Otomycosis by its own can also lead to perforation of tympanic membrane (Kumar KR et al. 1984). Adults with tympanic membrane perforation and ear discharge are usually affected by otomycosis. Chronic otomycosis develop clinical symptoms that are most commonly found in the external auditory canal. The symptoms that characterize these people are long-term ear discharge and pruritis. In the treatment of otomycosis, blocking the perforation of the tympanic membrane with a paper patch has a dual effect. [10] On one hand the paper patch stops fungus from reaching the middle ear and preserving the middle ear against infection, it also lessens the moisture in the EAC, thus making the treatment of otomycosis considerably easy. [11].
Antifungal medication come in a variety of forms, including ointment, spray, solution, gel and cream. These drugs are not used to treat otomycosis with perforated tympanic membrane, as these drugs contains small-particles which can cause irritation and growth of granulation tissue in the middle ear. Topical medicines are unsuitable for patients with perforated tympanic membrane. Systemic antifungal treatment is needed refractory cases. Itraconazole is often used to treat superficial otitis externa, while voriconazole to treat any invasion. If the perforation does not heal, tympanoplasty is advisable. [12].
Otomycosis is a contraindication for middle ear surgery. Because of the possibility of the fungal infection spreading to the middle ear or beyond, tympanoplasty is not recommended in individuals with otomycosis. Infection might potentially result in the transplant failure. [13].
In the present study, closure with paper patch and treatment with Castellani’s solution reduced the recurrence rate of fungal infections and shortened the recovery period. After fungal debridement or cleansing, Castellani’s solution, a well-known topical medicine is applied to the EAC. When applied through a perforated tympanic membrane, Başal et al. observed that Castellani’s solution did not cause any middle ear mucosa inflammation in rats (Basal Y et al. 2015). The ototoxic effects of topical antifungal medications are not clearly known. They can cause sensorineural hearing loss in patients with tympanic membrane perforation. [14] Now a days, Alcohol based solvents and antiseptics are found in antifungal ear drops which may enter the cochlea through the round window, causing oto-toxicity. During a seven-day experiment, five topical antifungal medications were applied to the external ear of mice. Clotrimazole, miconazole and tolnaftate are three antimycotic drugs which are safe, compared to nystatin in treating otomycosis with a perforated tympanic membrane. Closure of the perforation using paper patch defends the inner ear from the possible ill effects of topical drug toxicity.
At first, cautious drying and clearing of external auditory canal by suction evacuation is done. Syringing of external auditory canal is avoided as the infection may spread into the deeper anatomical sites, especially when the tympanic membrane is perforated and is not visible due to obstructed debris over it. If the conveniences of suction evacuation are not available, syringing can be done under all aseptic precautions using normal saline with antifungal powder. The ear should be cleaned and dried up completely after syringing as moisture can enhance the fungal growth. Even though slightly painful, methylated spirit can be used to dry the ear. [15].
Conclusions
To conclude, we state that treatment with clotrimazole solution in patched group is safe in managing otomycosis with tympanic membrane perforation. Otomycosis is a fungus causing surface infection of the external auditory canal that otolaryngologists routinely diagnose. In acute otomycosis, the use of proper topical antifungal drugs along with repeated cleaning of the debris generally leads to resolution in majority of the cases. Chronic form of otomycosis occur in about 10% of the cases.
Patients who had a perforated tympanic membrane may lead to chronic otitis media which can damage the middle ear ossicles leading to hearing impairment. Closure of the perforated tympanic membrane by a paper patch and topical application of Castellani’s solution was found to be a useful and a safe procedure. In patients with perforated eardrums, this method removes the infection in a short span of time and decreases the possibility of relapse.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Gur paramjeet Singh gill, Email: gpsgill67@gmail.com.
Vineet Panchal, Email: vinny.478@gmail.com.
Rupinder Bakshi, Email: rupindergill1@yahoo.co.in.
References
- 1.Paulose KO, Al Khalifa S, Shenoy P, Sharma RK. Mycotic infection of the ear (otomycosis): a prospective study. J Laryngol Otol. 1989;103:30–35. doi: 10.1017/S0022215100107960. [DOI] [PubMed] [Google Scholar]
- 2.Pradhan B, Tuladhar NR, Amatya RM. Prevalence of otomycosis in outpatient department of otolaryngology in Tribhuvan University Teaching Hospital, Kathmandu, Nepal. Ann OtolRhinolLaryngol. 2003;112:384–387. doi: 10.1177/000348940311200416. [DOI] [PubMed] [Google Scholar]
- 3.Jackman A, Ward R, April M, Bent J. Topical antibiotic induced otomycosis. Int J PediatrOtorhinolaryngol. 2005;69:857–860. doi: 10.1016/j.ijporl.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 4.Kaya AD, Kiraz N. In vitro susceptibilities of Aspergillus spp. causing otomycosis to amphotericin B, voriconazole and itraconazole. Mycoses. 2007;50:447–450. doi: 10.1111/j.1439-0507.2007.01409.x. [DOI] [PubMed] [Google Scholar]
- 5.Araiza J, Canseco P, Bonifaz A. Otomycosis: clinical and mycological study of 97 cases. Rev LaryngolOtolRhinol (Bord) 2006;127:251–254. [PubMed] [Google Scholar]
- 6.Ho T, Vrabec JT, Yoo D, Coker NJ. Otomycosis: clinical features and treatment implications. Otolaryngol Head Neck Surg. 2006;135(5):787–791. doi: 10.1016/j.otohns.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Kurnatowski P, Filipiak A. Otomycosis: prevalence, clinical symptoms, therapeutic procedure. Mycoses. 2001;44(11–12):472–479. doi: 10.1046/j.1439-0507.2001.00689.x. [DOI] [PubMed] [Google Scholar]
- 8.Hurst WB. Outcome of 22 cases of perforated tympanic membrane caused by otomycosis. J Laryngol Otol. 2001;115(11):879–880. doi: 10.1258/0022215011909486. [DOI] [PubMed] [Google Scholar]
- 9.Kumar KR. Silent perforation of tympanic membrane and otomycosis. Indian J Otolaryngol. 1984;36(4):161–162. doi: 10.1007/BF02993694. [DOI] [Google Scholar]
- 10.Viswanatha B, Sumatha D, Vijayashree MS. Otomycosis in immunocompetent and immunocompromised patients: comparative study and literature review. Ear Nose Throat J. 2012;91(3):114–121. doi: 10.1177/014556131209100308. [DOI] [PubMed] [Google Scholar]
- 11.Pata YS, Oztürk C, Akbaş Y, Unal M, Görür K, Ozcan C. Microbiology of cerumen in patients with recurrent otitis externa and cases with open mastoidectomy cavities. J Laryngol Otol. 2004;118:260–262. doi: 10.1258/002221504323011978. [DOI] [PubMed] [Google Scholar]
- 12.Özcan C, Ünal M, Görür K, Öztürk C, Delialioğlu N. Otomycosis: a clinicomycological study and efficacy of alcohol boric solution in treatment. KBB Klinikleri. 2000;2:71–75. [Google Scholar]
- 13.Song JE, Haberkamp TJ, Patel R, Redleaf MI. Fungal otisis externa as a cause of tympanic membrane perforation: a case series. Ear Nose Throat J. 2014;93:332–336. doi: 10.1177/014556131409300811. [DOI] [PubMed] [Google Scholar]
- 14.Vennewald I, Klemm E. Otomycosis: diagnosis and treatment. Clin Dermatol. 2010;28(2):202–211. doi: 10.1016/j.clindermatol.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Başal Y, Günel C, Eryılmaz A, Tuğrul I, Toka A, Kaçar F, et al. The effects of topical Burow’s and Castellani’s Solutions on the middle ear mucosa of rats. J Int Adv Otol. 2015;11:253–256. doi: 10.5152/iao.2015.715. [DOI] [PubMed] [Google Scholar]