Abstract
Purpose of Review
This review provides a historical perspective on the approach to radial tears and collates the currently available evidence on repair techniques, rehabilitation, and outcomes following the treatment of meniscus radial tears.
Recent Findings
Recent literature shows that the repair of meniscus radial tears reports improved patient-reported outcome scores with high return to function and activity. However, no single technique nor construct was proven better than the other.
Summary
Various methods of repairing radial tears can be employed, with biomechanical research supporting all-inside double vertical sutures, the addition of vertical “rip-stop” mattress sutures, and transtibial pullout augmentation. To ensure proper healing before undergoing physical therapy, it is crucial to abstain from weight-bearing and deep knee flexion for the first 6 weeks after surgery. Despite considerable heterogeneity in surgical techniques and rehabilitation protocols found in the current literature, studies reporting on radial repairs report positive results, with high healing rates and improved patient-reported outcomes.
Keywords: Meniscus radial tear, Meniscus repair, Postoperative outcomes
Introduction
The menisci are essential to the homeostasis of the knee joint, due to their key role in increasing tibiofemoral congruency, dynamic load distribution, joint stability, and proprioception [1, 2]. Injuries to the menisci remain one of the most common knee injuries in athletes and the elderly but can occur across all ages, sex, and activity levels [3]. At a reported incidence of 0.61 to 0.70 per 1000 person-years in the general population in the United States, the treatment for these injuries is an important current topic in orthopedic surgery. With surgical intervention on the uprise given the emerging emphasis on meniscal preservation meniscal surgeries cost nearly 4 billion dollars per year [4], and account for 10–20% of all orthopedic surgeries each year [3].
Numerous types of meniscal tears exist, among which radial tears comprise a subtype historically associated with relatively poor prognosis, often leading to early accelerated knee osteoarthritis [5]. Radial tears are unique because they are oriented perpendicular to the meniscal axis and disrupt the circumferential collagenous fibers in the peripheral end of the menisci. These fibers act by converting axial loads into tensile strains in the form of hoop stresses [2]. Damage to the circumferential fibers results in significant loss of function, leading to increased contact pressure [6], with prior evidence demonstrating a higher grade of cartilage damage, as well as higher rate and severity of meniscal extrusion in knees with a radial tear relative to other types of tear [7, 8]. Given their impactful consequences, high incidence—reports up to 28% of medial meniscus tears—and technically challenging treatment, radial tears are of particular importance.
Management of meniscal radial tears is complex and has changed drastically during the past decades. A deep understanding of meniscus anatomy, biomechanics, and their function during activities played a key role in the change of conception of present-day interventions. Continuous optimization in diagnostic methods, surgical repair techniques, and rehabilitation protocols resulted in improved short- and long-term outcomes of radial tear management. The objective of this review was to provide a historical perspective on the approach to radial tears and to collate the currently available evidence on repair techniques, rehabilitation, and outcomes following the treatment of meniscus radial tears.
Historic Perspective
There has been a dramatic change in the approach to meniscus tears in the past few decades [6, 9]. The exponential growth in the knowledge base pertaining to meniscus biomechanics, healing, and long-term outcomes [10] has fueled a paradigm shift from Smillie’s 1967 “If it is torn, take it out” [11] to the present-day “save the meniscus!” maxim [12].
Radial tears that encompass the avascular white-white zone of the meniscus have been historically considered irreparable, and therefore treated with meniscectomies [13–17]. While patients largely experience short-term symptomatic relief following a meniscectomy [18], an overwhelming number of studies ultimately demonstrated the deleterious effects of meniscal deficiency, whether biomechanically following a radial tear [10] or through what is now extensive long-term data on the degenerative consequences of meniscectomies—particularly of the lateral meniscus [12].
Improved understanding of several aspects pertinent to the menisci has since renewed the interest in extending the indications of meniscal repair to include radial tears, as opposed to only repairing the more amenable peripheric vertical tears. Biomechanically, numerous ex vivo studies demonstrated that large radial tears and root tears significantly decrease contact area and increased contact pressures in the affected compartment, functionally approximating a total meniscectomy [19, 20]. In consonance with the impaired biomechanics observed in cadaveric studies, multiple in vivo motion analysis studies reported that, despite symptomatic relief, partial meniscectomy led to significantly increased knee adduction and flexion moments post-operatively—parameters often associated with varying stages of knee osteoarthritis [21–23]. In terms of biological healing, a recent investigation by Chahla et al. demonstrated multipotent mesenchymal stromal progenitor cells and vascularization in the white-white zone of the meniscus, indicating its better healing potential than previously believed [24]. Additionally, in terms of clinical outcomes, a recent review by Everhart et al. revealed that meniscus repair failure rates in patients older than 40 years are comparable to those of younger patients [25]. This is important, given that radial tears are often of degenerative nature in older patients—particularly of the medial meniscus [5]. Finally, the past couple of decades have observed vastly modernized techniques and devices for meniscal repair, allowing for maximization of the biomechanical and biological aspects of surgical treatment [10, 26].
With all those factors in mind, radial tears extending into the circumferential fibers of the meniscus, especially into the periphery and meniscus-synovial junction, should always be repaired whenever possible, with an aim to restore native biomechanics and potentially prevent rapid degenerative progression.
Types of Common Radial Tears
Radial tears are cleavage tears arising from the central region (white-white) to the periphery (red-red) and can occur in all anteroposterior zones of the medial and lateral meniscus. They can be characterized according to their location within the meniscus, as affecting the anterior horn, body or posterior horn [2]. Whenever a radial tear is located within 1 cm of the meniscal root, it is considered a meniscal root tear [27].
Radial tears can be further divided in partial-thickness or full-thickness tears, which result in different biomechanical consequences. Cadaveric investigations suggest that tears up to 60% of meniscal width have little impact on load distribution function – albeit aforementioned in vivo evidence demonstrated pathological kinetic profile even during simple overground gait [2]. In light of that, partial meniscectomy is still often indicated for smaller partial “white-white” radial lesions. On the other hand, tears of 100% of the meniscal width (full-thickness tears) result in complete loss of meniscal function [28, 29] and can lead to the rapid development of knee osteoarthritis [30].
Regarding etiology, radial tears can be classified as either of traumatic or degenerative nature. Lateral meniscus radial tears are more frequently traumatic and associated with ACL injuries (33% vs 8% of medial meniscus radial tears) in younger patients [31]. Medial radial and root tears are typically degenerative, and as such, are unfortunately underdiagnosed [27].
Nakata et al. proposed a classification based on the morphology of radial tears. Type A tears were characterized as a radial split that extended to less than 50% of the width of the peripheral rim. Type B tears extended to more than 50%, further divided into the following two subtypes: type B1, a simple radial split tear; and type B2, a flap tear including a radial tear. A complete radial split tear, which extended to the peripheral rim was classified as Type C. Bucket-handle tears including a radial tear component were defined as Type D, most often traumatic and associated with ACL tears [27].
Repair Techniques and Biomechanics
Several repair techniques and suture configurations pertinent to radial tears have been developed and tested (Fig. 1). Repair constructs can differ based on surgical approach (inside-out, all-inside, and outside-in), use of a transtibial pullout augmentation, as well as the number, orientation, and pattern of suture placement. Technique choice must weigh factors such as potential iatrogenic damage to the meniscal tissue, neurovascular risk, technical ease of use, operative time, and cost.
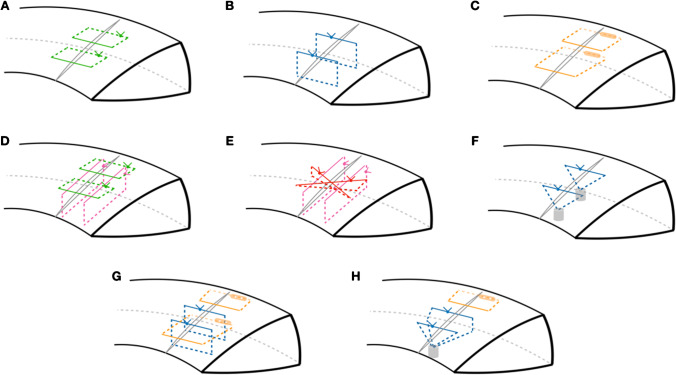
Fig. 1.
Schematic representation of key radial repair techniques. A Conventional horizontal inside-out repair (green); B suture-based all-inside double vertical repair (blue); C anchor-based all-inside horizontal repair (orange); D “hash-tag” construct, with inside-out horizontal repair reinforced with vertical mattress “rip-stop” sutures (pink); E “cross-tag” construct, with suture-based all-inside figure-of-eight configuration (red) reinforced with vertical mattress “rip-stop” sutures; F two-tunnel transtibial pullout repair; G hybrid suture-based double vertical and anchor-based all-inside horizontal repair (see Fig. 3); H hybrid double-vertical transtibial pullout with all-inside horizontal repair (see Fig. 2)
Traditionally, the repair of radial tears was performed using an inside-out approach with horizontal stitches across the tear edges (Fig. 1A) [32]. Advantages including considerably lower cost and the ability to deploy multiple sutures with minimal damage to the meniscus must be reconciled with the need for a posterior incision increasing the risk of neurovascular injury, postoperative pain, increased surgical time, need for an experienced assistant and needlestick injury to the surgical team [33]. More recently, all-inside repairs have gained exponential popularity due to significant improvements in device technology and technique [34]. Albeit more costly, modern all-inside repair is less time-consuming, less technically challenging, and reduces iatrogenic risk to neurovascular structures compared to alternative techniques, without sacrificing biomechanical strength or healing [26, 33, 35].
Specific to radial tears, all-inside repair has gained traction as the preferred technique as consistent evidence of biomechanical superiority has emerged [26]. Beamer et al. found that vertical all-inside repair (Fig. 1B) of a medial meniscus radial tear resulted in lower displacement, higher load to failure, and greater stiffness relative to conventional horizontal inside-out repair [36]. A later study by Branch et al. also demonstrated higher load to failure and superior construct stiffness of all-inside repair using varying all-inside suture configurations compared to a double horizontal inside-out construct [37]. Similarly, for lateral meniscus radial tears, a systematic review by Alentorn-Geli et al. found significantly higher construct stiffness following all-inside compared to inside-out techniques [38].
When comparing all-inside techniques, a study by Doig et al. reported that radial repairs with a meniscus-based all-inside all-suture construct (Fig. 1B) led to significantly less displacement after cyclic loading, as well as superior stiffness and load to failure when compared to capsule-based all-inside repair with anchors (Fig. 1C) [39]. These findings were reflected in a recent systematic review by Oosten et al., with suture-based configurations largely presenting favorable displacement and strength profiles [26].
In terms of suture configuration, the use of a double vertical repair has consistently shown favorable biomechanical properties [26]. This technique consists of passing two sutures vertically orientated in the borders of the lesion, parallel to the radial tear. The rationale behind a vertically oriented repair consists in positioning sutures transversally to the circumferential fibers of the meniscus. All-inside vertical repair generates higher load to failure and stiffness compared to inside-out horizontal repair [26, 36, 40]. The aforementioned review by Oosten et al. [26] found mixed results from studies examining horizontal and oblique sutures (Fig. 1D), suggesting that it may not be particularly beneficial to implement a crossing pattern during repair, while the authors recommend to otherwise focus on adding “rip-stop” suture reinforcements. Of note, the collated literature points to two main advancements in the modern arsenal of radial repairs are the addition of “rip-stop” sutures and the use of transtibial tunnel pullout [26].
Reinforcing repair constructs with a pair of vertical “rip-stop” mattress sutures (Fig. 1E) can minimize the risk of suture cut-out compared to non-reinforced repairs, and thus enhance the healing potential [26]. These combined repair configurations with vertical mattress include the “hash-tag”, “cross-tag” [41], “rebar” [42], and “tie-grip” [43] repairs. Multiple studies have found consistent superiority of suture configurations including rip-stop reinforcement sutures relative to non-reinforced constructs [37, 41, 44].
A novel transtibial tunnel repair technique (Fig. 1F) has shown favorable biomechanical outcomes regarding resistance to failure load and displacement, as reported by Bhatia et al. [45] and James et al. [46] There is, consonantly, ample evidence to support excellent biomechanical and clinical outcomes observed when using a similar two-tunnel pullout when repairing posterior root tears [47]. As tension is applied to the sutures, their crisscross orientation allows the re-apposition of the torn margins of the meniscus [46]. Transtibial pullout can be employed to augment multiple suture configurations, and performed with either a single tunnel or two tunnels. Recent investigations report reduced median gapping distance at the tear site, higher average load to failure, and less biomechanical variability between repairs when compared to a standard inside-out horizontal mattress [26, 45].
The all-inside double vertical repair and the transtibial two-tunnel technique combined with four horizontal inside-out sutures have shown to be the strongest regarding the load-to-failure, when compared to other 21 techniques within 20 studies in Oosten et al.’s review, including all-inside and inside-out repair with different configurations [26].
Authors’ Preference
Our typical indication for radial repair consists of a complete tear or a high-grade partial tear of over 2/3 of the width of the meniscus, as partial tearing under that threshold has been shown to result in minimal biomechanical changes [28]. Acute traumatic tears should always preferably be repaired, while repair indication in chronic degenerative tears will depend on meniscal tissue quality and accompanying degenerative changes in the joint with joint space under 3 mm, Kellgren-Lawrence grade ≥ III knee osteoarthritis and modified Outerbridge grade ≥ 3 chondral lesions comprising relative contraindications [27]. As mechanical malalignment may present a complicating factor and the postoperative rehabilitation of a radial repair entails a coinciding non-weightbearing period with an osteotomy, we advise considering realignment in knees with over 3° of mechanical varus or when the mechanical load-bearing axis of the limb (Mikulicz line) is beyond the edge of the correspondent tibial spine [48].
All-inside repairs are currently preferred by the senior author, given its favorable biomechanical profile, as well as the obviated need for accessory posterior incisions, and less cumbersome and time-consuming technique.
When repairing medial meniscus radial tears, our technique of choice is a hybrid construct with transtibial pullout of a double vertical all-suture repair with the addition of anchor-based all-inside stitches. The technique is schematically illustrated in Fig. 1H and detailed in Fig. 2. It is our belief that the addition of a more stable fixation on medial meniscus radial repairs better reproduces the native anatomy of the meniscotibial ligaments [2]. On the other hand, in radial tears of the lateral meniscus, given its higher mobility, our preferred technique is a similar combination of suture-based and anchor-based all-inside techniques without transtibial tunnel augmentation (schematically represented in Fig. 1G and detailed in Fig. 3). Whenever faced with a lateral meniscus tear far into the posterior horn, it is wise to avoid anchor-based repair, if possible, due to proximity to the popliteal artery.
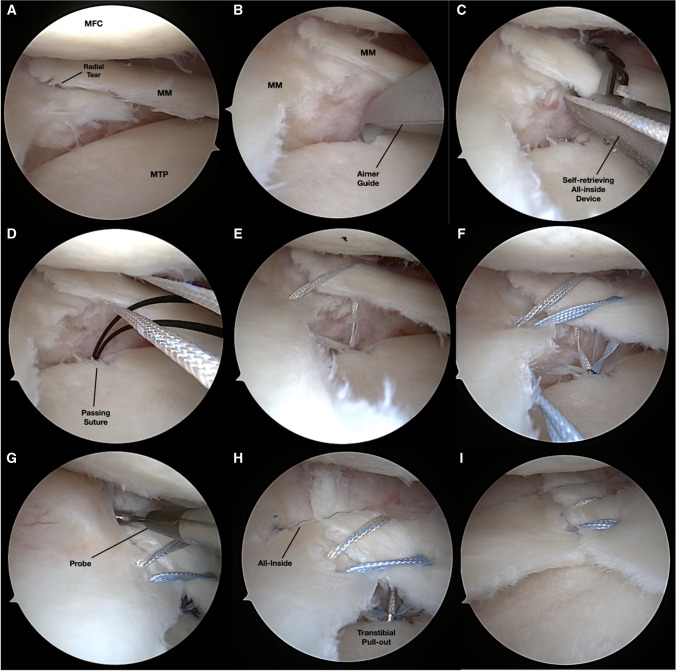
Fig. 2.
Authors’ preference for medial meniscus radial tears, as represented in Fig. 1H and seen in a left knee arthroscopy following pie-crusting of the superficial medial collateral ligament (A). A single transtibial tunnel is created with the aid of a curved aimer guide and metallic cannula (FirstPass Mini, Smith & Nephew) (B). An all-inside self-retrieving device (C) is used to pass a suture tape in a vertical mattress configuration across the borders of the radial tear (D–E); and pulled out of the tibial tunnel using a monofilament nitinol passing suture (D). These steps are then repeated with a second suture tape, producing a double vertical all-suture repair (F). The remaining gap identified with the use of a probe (G) is then closed using one anchor-based all-inside horizontal stitch (H). The all-inside suture in then tensioned and the knot cut, followed by manual tensioning of the transtibial pullout under arthroscopic visualization (I) and final fixation with an anchor (Footprint, Smith & Nephew) is carried out. MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau
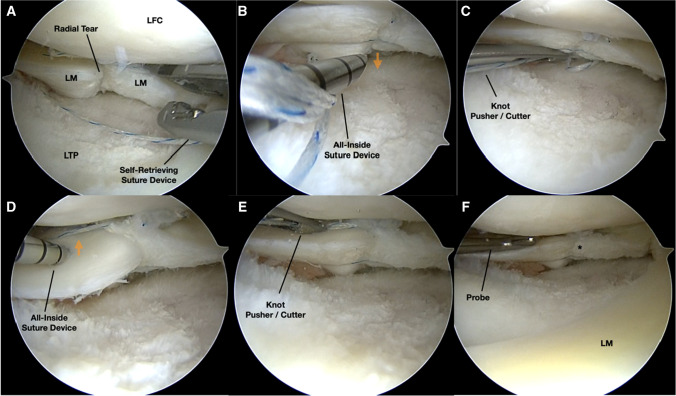
Fig. 3.
Authors’ preference for lateral meniscus radial tears, as represented in Fig. 1G and seen in a right knee arthroscopy (A). A self-retrieving all-inside device (Novostitch, Smith & Nephew) is used to deploy suture-based double vertical side-to-side sutures (A). The construct is then completed with the addition of two anchor-based all-inside horizontal sutures, the first attaching the inferior surface of the meniscus to the capsule (B, C) and the second through the superior aspect of the meniscus into the capsule (D, E). The final hybrid construct is then visualized with satisfactory apposition of the borders (*) and probed for adequate stability. LFC, lateral femoral condyle; LM, lateral meniscus; LTP, lateral tibial plateau
Rehabilitation
Adequate postoperative rehabilitation in a stepwise fashion is instrumental in the management of meniscal tears. Radial tears experience distraction forces and increased strain with axial loading [29]. Therefore, the effect of loading and deep flexion inherently increases the chances of repair failure. Simulated early postoperative weight-bearing induced significant and unrecoverable loosening of sutures following a root repair in a study by Steineman et al. [49]. Thereafter, emphasis on non-weightbearing (NWB) status is imperative during the first 6 weeks, during which range of motion (ROM) is also restricted to 90º. Our complete post-operative protocol is detailed in Table 1. Full clearance to return to sports participation typically takes place between 6 and 9 months.
Table 1.
Rehabilitation protocol following radial repair
| 0–4 weeks |
| • Non-weightbearing (NWB) in brace in extension with crutches until 6 weeks post-op |
| • Brace in extension for sleeping 0–2 weeks |
| • Active/passive ROM 0–90° |
| • Quadriceps sets, SLR, Heel Slides |
| • Patellar mobilization |
| 4–6 weeks |
| • Progress flexion until full ROM is achieved |
| • Maintain NWB status |
| 6–8 weeks |
| • Advance to weight-bearing as tolerated (WBAT) at 6 weeks post-op after transitioning to the unloader brace |
| • Discontinue immobilizer brace when quad strength adequate (typically around 6 weeks) |
| • Discontinue crutches when gait normalized |
| • Wall-sits to 90° |
| 8–12 weeks |
| • WBAT with use of unloader brace until 6 months post-op |
| • Full ROM |
| • Progress with closed-chain exercises |
| • Lunges from 0 to 90° |
| • Leg-press 0–90° |
| • Proprioception exercises |
| • Begin stationary bike |
| 12–16 weeks: |
| • Progress strengthening exercises |
| • Single leg strengthening |
| • Begin jogging and progress to running |
| • Sports-specific exercise |
Legend: ROM, range of motion; SLR, straight leg raise
Although there is no consensus for a standardized postoperative protocol, a systematic review by Spang et al. compared 6 protocols of publicly available academic residency programs and orthopedic sports medicine fellowships, the average time with a brace, time to return to sport, time to full range of motion, and time to full weight bearing [49, 50]. Protocols for radial tears were more likely to delay return to full range of motion than general protocols, with 7.3 weeks on average versus 6.7 weeks on average, respectively. Most studies waited until 8 weeks to return to full range of motion, compared to 6 weeks on non-radial meniscus repair. The recommended time in a brace was 1 week longer compared to non-radial meniscus repair. Most radial repair protocols reported 7–8 weeks in a brace. All radial repair protocols reported 7–8 weeks until full weight bearing was allowed, while non-radial repairs ranged from 2 to 12 weeks, with most studies reporting 6 weeks until full weight bearing was allowed. Considering the lack of data supporting safe early weight bearing and full range of motion, most protocols tend to be more conservative with radial tear repairs [50].
Results
In evaluating the healing rates of radial repairs through a second-look arthroscopy, numerous studies have found healing rates ranging from 60 to 86% [51••]. Magnetic resonance imaging assessment studies present a wider range of healing rates, and a mismatch between clinical outcomes and imaging findings, due to the difficulty in distinguishing signal changes with healing, scar tissue, and an unhealed tear. Approximately 90% of patients show imaging signs of at least partial healing following radial repairs [52, 53].
Patient-reported outcomes were analyzed in a recent systematic review by Milliron et al., with qualitative improvement in Lysholm, International Knee Documentation Committee (IKDC), Western Ontario and McMaster University Osteoarthritis index (WOMAC), and pain scores across the included studies. No single technique nor construct was proven better than the other [51••]. Although there is a scarcity of data specific to return to sports following radial repair, the improved patient-reported outcomes in conjunction with six studies reporting Tegner Activity Scale scores improving from 1–4 to 4.7–6.7 post-operatively, demonstrate that radial repair is effective in terms of return to function and activity [52, 54–57, 58•]. Although limited by largely low level of evidence studies—with absent clinical trials, and predominantly retrospective designs—the results were consistent across the studies. Publication bias in retrospective studies could also lead to misinterpretation of data since studies with negative results are often not accepted in journals. Another limitation of the current literature is the short period of follow-up (mean 35 months) [51••] Whether the observed healing rates are reflected in the long-term delayed progression of cartilage damage and joint degeneration is yet to be assessed.
Literature is still not clear as to which repair technique is superior to another. More randomized controlled studies with long-term follow-up are needed, comparing clinical outcomes of different techniques of radial meniscus repair. Furthermore, the impact of orthobiologics when added specifically to radial repair constructs is yet to be analyzed with methodologically robust investigations. Several techniques of biologic augmentation have been described, including trephination, fibrin-clot, and marrow-venting procedures, among others [59–61].
Conclusion
There has been an important paradigm shift in the management of radial tears of the menisci in the past decades. A deeper understanding of anatomy and biomechanics was the foundation for the development of novel treatments that focused on meniscus preservation and restoration of native anatomy. Different radial repair techniques can be used, with biomechanical evidence supporting all-inside double vertical sutures, the addition of vertical “rip-stop” mattress sutures, and transtibial pullout augmentation. Avoiding weight-bearing and deep flexion in the first 6 weeks following surgery is key to ensuring adequate healing before physical therapy progression.
Despite considerable heterogeneity in surgical techniques and protocols of rehabilitation across the current literature, the results of meniscal repair in radial tears trend positively, showing high healing rates and improved patient-reported outcomes. Whether the observed healing rates are reflected in the long-term delayed progression of cartilage damage and joint degeneration is yet to be assessed.
Declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Enzo S. Mameri, Email: enzomameri@gmail.com
Garrett R. Jackson, Email: grjackson.md@gmail.com
Felipe Gonzalez, Email: felipegonzalez818@gmail.com.
Daniel J. Kaplan, Email: Daniel.kaplan@rushortho.com
Harkirat Jawanda, Email: harkirat.jawanda@rushortho.com.
Anjay Batra, Email: anjay.batra@rushortho.com.
Zeeshan A. Khan, Email: Zeeshan.khan@rushortho.com
Jorge Chahla, Email: jachahla@msn.com.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Jackson GR, Meade J, Yu Z, Young B, Piasecki DP, Fleischli JE, et al. Outcomes and failure rates after revision meniscal repair: a systematic review and meta-analysis. Int Orthop. 2022;46(7):1557–1562. doi: 10.1007/s00264-022-05413-1. [DOI] [PubMed] [Google Scholar]
- 2.Mameri ES, Dasari SP, Fortier LM, Verdejo FG, Gursoy S, Yanke AB, et al. Review of meniscus anatomy and biomechanics. Curr Rev Musculoskelet Med. 2022;15(5):323–335. doi: 10.1007/s12178-022-09768-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams BG, Houston MN, Cameron KL. The epidemiology of meniscus injury. Sports Med Arthrosc Rev. 2021;29(3):e24–e33. doi: 10.1097/JSA.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 4.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;11:1–25. [PubMed] [Google Scholar]
- 5.Jarraya M, Roemer FW, Englund M, Crema MD, Gale HI, Hayashi D, et al. Meniscus morphology: does tear type matter? A narrative review with focus on relevance for osteoarthritis research. Semin Arthritis Rheum. 2017;46(5):552–561. doi: 10.1016/j.semarthrit.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6(1):35–45. doi: 10.1136/jisakos-2019-000380. [DOI] [PubMed] [Google Scholar]
- 7.Wu J, Huang JM, Zhao B, Cao JG, Chen X. Risk factors comparison for radial and horizontal tears. J Knee Surg. 2016;29(8):679–683. doi: 10.1055/s-0036-1572415. [DOI] [PubMed] [Google Scholar]
- 8.Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 9.Beaufils P, Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103(8S):S237-S44. 10.1016/j.otsr.2017.08.003. [DOI] [PubMed]
- 10.Mohamadi A, Momenzadeh K, Masoudi A, Walley KC, Ierardi K, Ramappa A, et al. Evolution of knowledge on meniscal biomechanics: a 40 year perspective. BMC Musculoskelet Disord. 2021;22(1):625. doi: 10.1186/s12891-021-04492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smillie IS. The current pattern of internal derangements of the knee joint relative to the menisci. Clin Orthop Relat Res. 1967;51:117–122. [PubMed] [Google Scholar]
- 12.Seil R, Becker R. Time for a paradigm change in meniscal repair: save the meniscus! Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1421–1423. doi: 10.1007/s00167-016-4127-9. [DOI] [PubMed] [Google Scholar]
- 13.Sgaglione NA. Editorial commentary: stay tuned: broadening our scope of knee meniscus radial tear repairs. Arthroscopy. 2016;32(9):1926–1927. doi: 10.1016/j.arthro.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 16.Eijgenraam SM, Reijman M, Bierma-Zeinstra SMA, van Yperen DT, Meuffels DE. Can we predict the clinical outcome of arthroscopic partial meniscectomy? A systematic review. Br J Sports Med. 2018;52(8):514–521. doi: 10.1136/bjsports-2017-097836. [DOI] [PubMed] [Google Scholar]
- 17.Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193 (Pt 2)(Pt 2):161–78. 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed]
- 18.Hohmann E, Angelo R, Arciero R, Bach BR, Cole B, Cote M, et al. Degenerative meniscus lesions: an expert consensus statement using the modified Delphi technique. Arthroscopy. 2020;36(2):501–512. doi: 10.1016/j.arthro.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 19.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–31. 10.2106/JBJS.G.00748. [DOI] [PubMed]
- 20.Ohori T, Mae T, Shino K, Fujie H, Hirose T, Tachibana Y, et al. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):342–351. doi: 10.1007/s00167-020-05915-8. [DOI] [PubMed] [Google Scholar]
- 21.Erhart-Hledik JC, Favre J, Andriacchi TP. New insight in the relationship between regional patterns of knee cartilage thickness, osteoarthritis disease severity, and gait mechanics. J Biomech. 2015;48(14):3868–3875. doi: 10.1016/j.jbiomech.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 22.Thorlund JB, Holsgaard-Larsen A, Creaby MW, Jørgensen GM, Nissen N, Englund M, et al. Changes in knee joint load indices from before to 12 months after arthroscopic partial meniscectomy: a prospective cohort study. Osteoarthritis Cartilage. 2016;24(7):1153–1159. doi: 10.1016/j.joca.2016.01.987. [DOI] [PubMed] [Google Scholar]
- 23.Hall M, Wrigley TV, Metcalf BR, Hinman RS, Cicuttini FM, Dempsey AR, et al. Mechanisms underpinning the peak knee flexion moment increase over 2-years following arthroscopic partial meniscectomy. Clin Biomech (Bristol, Avon) 2015;30(10):1060–1065. doi: 10.1016/j.clinbiomech.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Chahla J, Papalamprou A, Chan V, Arabi Y, Salehi K, Nelson TJ, et al. Assessing the resident progenitor cell population and the vascularity of the adult human meniscus. Arthroscopy. 2021;37(1):252–265. doi: 10.1016/j.arthro.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Everhart JS, Higgins JD, Poland SG, Abouljoud MM, Flanigan DC. Meniscal repair in patients age 40 years and older: a systematic review of 11 studies and 148 patients. Knee. 2018;25(6):1142–1150. doi: 10.1016/j.knee.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Oosten J, Yoder R, DiBartola A, Bowler J, Sparks A, Duerr R, et al. Several techniques exist with favorable biomechanical outcomes in radial meniscus tear repair-a systematic review. Arthroscopy. 2022;38(8):2557–78.e4. doi: 10.1016/j.arthro.2022.02.010. [DOI] [PubMed] [Google Scholar]
- 27.Cinque ME, Chahla J, Moatshe G, Faucett SC, Krych AJ, LaPrade RF. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52(13):872–876. doi: 10.1136/bjsports-2017-098942. [DOI] [PubMed] [Google Scholar]
- 28.Tachibana Y, Mae T, Fujie H, Shino K, Ohori T, Yoshikawa H, et al. Effect of radial meniscal tear on in situ forces of meniscus and tibiofemoral relationship. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):355–361. doi: 10.1007/s00167-016-4395-4. [DOI] [PubMed] [Google Scholar]
- 29.Jones RS, Keene GC, Learmonth DJ, Bickerstaff D, Nawana NS, Costi JJ, et al. Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin Biomech (Bristol, Avon) 1996;11(5):295–300. doi: 10.1016/0268-0033(96)00003-4. [DOI] [PubMed] [Google Scholar]
- 30.Badlani JT, Borrero C, Golla S, Harner CD, Irrgang JJ. The effects of meniscus injury on the development of knee osteoarthritis: data from the osteoarthritis initiative. Am J Sports Med. 2013;41(6):1238–1244. doi: 10.1177/0363546513490276. [DOI] [PubMed] [Google Scholar]
- 31.Bergkvist D, Dahlberg LE, Neuman P, Englund M. Knee arthroscopies: who gets them, what does the radiologist report, and what does the surgeon find? An evaluation from southern Sweden. Acta Orthop. 2016;87(1):12–16. doi: 10.3109/17453674.2015.1055179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nelson CG, Bonner KF. Inside-out meniscus repair. Arthrosc Tech. 2013;2(4):e453–e460. doi: 10.1016/j.eats.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vint H, Quartley M, Robinson JR. All-inside versus inside-out meniscal repair: a systematic review and meta-analysis. Knee. 2021;28:326–337. doi: 10.1016/j.knee.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Turman KA, Diduch DR, Miller MD. All-inside meniscal repair. Sports Health. 2009;1(5):438–444. doi: 10.1177/1941738109334219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Golz AG, Mandelbaum B, Pace JL. All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15(4):252–258. doi: 10.1007/s12178-022-09766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beamer BS, Masoudi A, Walley KC, Harlow ER, Manoukian OS, Hertz B, et al. Analysis of a new all-inside versus inside-out technique for repairing radial meniscal tears. Arthroscopy. 2015;31(2):293–298. doi: 10.1016/j.arthro.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 37.Branch EA, Milchteim C, Aspey BS, Liu W, Saliman JD, Anz AW. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sports Med. 2015;43(9):2270–2276. doi: 10.1177/0363546515591994. [DOI] [PubMed] [Google Scholar]
- 38.Alentorn-Geli E, Choi JH, Stuart JJ, Toth AP, Garrett WE, Taylor DC, et al. Inside-out or outside-in suturing should not be considered the standard repair method for radial tears of the midbody of the lateral meniscus: a systematic review and meta-analysis of biomechanical studies. J Knee Surg. 2016;29(7):604–612. doi: 10.1055/s-0035-1570113. [DOI] [PubMed] [Google Scholar]
- 39.Doig T, Fagan P, Frush T, Lovse L, Chen C, Lemos S. The all-inside all-suture technique demonstrated better biomechanical behaviors in meniscus radial tear repair. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3606–3612. doi: 10.1007/s00167-020-06078-2. [DOI] [PubMed] [Google Scholar]
- 40.Yeh SH, Hsu FW, Chen KH, Chiang ER, Chang MC, Ma HL. Repairing complete radial tears of the lateral meniscus: arthroscopic all-inside double vertical cross-suture technique is effective and safe with 2-year minimum follow-up. Arthroscopy. 2022;38(6):1919–1929. doi: 10.1016/j.arthro.2021.11.025. [DOI] [PubMed] [Google Scholar]
- 41.Stender ZC, Cracchiolo AM, Walsh MP, Patterson DP, Wilusz MJ, Lemos SE. Radial tears of the lateral meniscus-two novel repair techniques: a biomechanical study. Orthop J Sports Med. 2018;6(4):2325967118768086. doi: 10.1177/2325967118768086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Massey PA, McClary K, Sanders N, Myers M, Barton RS, Solitro G. Rebar repair of radial meniscus tears: a reinforced suture technique. Arthrosc Tech. 2020;9(7):e953–e957. doi: 10.1016/j.eats.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakanishi Y, Hoshino Y, Nagamune K, Yamamoto T, Nagai K, Araki D, et al. Radial meniscal tears are best repaired by a modified “cross” tie-grip suture based on a biomechanical comparison of 4 repair techniques in a porcine model. Orthop J Sports Med. 2020;8(7):2325967120935810. doi: 10.1177/2325967120935810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Buckley PS, Kemler BR, Robbins CM, Aman ZS, Storaci HW, Dornan GJ, et al. Biomechanical comparison of 3 novel repair techniques for radial tears of the medial meniscus: the 2-tunnel transtibial technique, a “hybrid” horizontal and vertical mattress suture configuration, and a combined “hybrid tunnel” technique. Am J Sports Med. 2019;47(3):651–658. doi: 10.1177/0363546518816949. [DOI] [PubMed] [Google Scholar]
- 45.Bhatia S, Civitarese DM, Turnbull TL, LaPrade CM, Nitri M, Wijdicks CA, et al. A novel repair method for radial tears of the medial meniscus: biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med. 2016;44(3):639–645. doi: 10.1177/0363546515615565. [DOI] [PubMed] [Google Scholar]
- 46.James EW, LaPrade CM, Feagin JA, LaPrade RF. Repair of a complete radial tear in the midbody of the medial meniscus using a novel crisscross suture transtibial tunnel surgical technique: a case report. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2750–2755. doi: 10.1007/s00167-014-3089-z. [DOI] [PubMed] [Google Scholar]
- 47.Perry AK, Lavoie-Gagne O, Knapik DM, Maheshwer B, Hodakowski A, Gursoy S, et al. Examining the efficacy of medial meniscus posterior root repair: a meta-analysis and systematic review of biomechanical and clinical outcomes. Am J Sports Med. 2022:3635465221077271. 10.1177/03635465221077271. [DOI] [PubMed]
- 48.Chung KS, Ha JK, Ra HJ, Kim JG. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy. 2016;32(7):1319–1327. doi: 10.1016/j.arthro.2015.12.046. [DOI] [PubMed] [Google Scholar]
- 49.Steineman BD, LaPrade RF, Haut Donahue TL. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: a biomechanical study. Arthroscopy. 2019;35(4):1232–1239. doi: 10.1016/j.arthro.2018.11.041. [DOI] [PubMed] [Google Scholar]
- 50.Carder SL, Messamore WG, Scheffer DR, Giusti NE, Schroeppel JP, Mullen S, et al. Publicly available rehabilitation protocols designated for meniscal repairs are highly variable. Arthrosc Sports Med Rehabil. 2021;3(2):e411–e419. doi: 10.1016/j.asmr.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.•• Milliron EM, Magnussen RA, A Cavendish P, P Quinn J, DiBartola AC, Flanigan DC. Repair of radial meniscus tears results in improved patient-reported outcome scores: a systematic review. Arthrosc Sports Med Rehabil. 2021;3(3):e967-e80. 10.1016/j.asmr.2021.03.002. This reference is very important because it is a recent systematic review of 12 studies showing that outcomes following radial repair report high outcomes at final follow-up in addition to a 62% complete healing rate. [DOI] [PMC free article] [PubMed]
- 52.Choi NH, Kim TH, Son KM, Victoroff BN. Meniscal repair for radial tears of the midbody of the lateral meniscus. Am J Sports Med. 2010;38(12):2472–2476. doi: 10.1177/0363546510376736. [DOI] [PubMed] [Google Scholar]
- 53.Haklar U, Kocaoglu B, Nalbantoglu U, Tuzuner T, Guven O. Arthroscopic repair of radial lateral meniscus [corrected] tear by double horizontal sutures with inside-outside technique. Knee. 2008;15(5):355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 54.Song HS, Bae TY, Park BY, Shim J, In Y. Repair of a radial tear in the posterior horn of the lateral meniscus. Knee. 2014;21(6):1185–1190. doi: 10.1016/j.knee.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 55.Anderson L, Watts M, Shapter O, Logan M, Risebury M, Duffy D, et al. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy. 2010;26(12):1625–1632. doi: 10.1016/j.arthro.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 56.Wu IT, Hevesi M, Desai VS, Camp CL, Dahm DL, Levy BA, et al. Comparative outcomes of radial and bucket-handle meniscal tear repair: a propensity-matched analysis. Am J Sports Med. 2018;46(11):2653–2660. doi: 10.1177/0363546518786035. [DOI] [PubMed] [Google Scholar]
- 57.Cinque ME, Geeslin AG, Chahla J, Dornan GJ, LaPrade RF. Two-tunnel transtibial repair of radial meniscus tears produces comparable results to inside-out repair of vertical meniscus tears. Am J Sports Med. 2017;45(10):2253–2259. doi: 10.1177/0363546517704425. [DOI] [PubMed] [Google Scholar]
- 58.Gan JZ, Lie DT, Lee WQ. Clinical outcomes of meniscus repair and partial meniscectomy: does tear configuration matter? J Orthop Surg (Hong Kong) 2020;28(1):2309499019887653. doi: 10.1177/2309499019887653. [DOI] [PubMed] [Google Scholar]
- 59.Chahla J, Kennedy NI, Geeslin AG, Moatshe G, Cinque ME, DePhillipo NN, et al. Meniscal repair with fibrin clot augmentation. Arthrosc Tech. 2017;6(6):e2065–e2069. doi: 10.1016/j.eats.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Srimongkolpitak S, Chernchujit B. Current concepts on meniscal repairs. J Clin Orthop Trauma. 2022;27:101810. 10.1016/j.jcot.2022.101810. [DOI] [PMC free article] [PubMed]
- 61.Mameri ES, Verdejo FG, Dasari SP, Kerzner B, Shah S, Kasson LB, et al. Repair of a horizontal cleavage tear of the lateral meniscus with circumferential compression stitches and marrow venting augmentation. Arthrosc Tech. 2022;11(11):e1937–e1944. doi: 10.1016/j.eats.2022.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]