Abstract
Aim: The aim of the study is to compare the effects of vestibular rehabilitation and pharmacological treatment in benign paroxysmal positional vertigo (BPPV). Materials and methods: Thirty patients (40.93 ± 8.66 years old) diagnosed with BPPV were recruited. Patients were equally divided into pharmacological control group and vestibular rehabilitation group. The pharmacological control group was further divided into Group A (n = 8, 2 doses/day, 24 mg betahistine) and Group B (n = 7, 1 dose/day, 50 mg dimenhydrinate in addition to betahistine). Patients in the rehabilitation group underwent repeated head and eye movements, and Epley or Barbecue Roll Maneuvers were applied for 4 weeks. Subjective assessment of vertigo was measured with the visual analog scale. Static balance parameters were measured with the tandem, one-legged stance, and Romberg tests. Dynamic visual acuity was measured with a Snellen chart, and vestibular dysfunction was measured with the Unterberger (Fukuda stepping) test. All parameters were evaluated before and after treatment. Results: Vestibular rehabilitation resulted in greater improvement in severity of vertigo, balance parameters except Romberg test, and vestibular dysfunction than pharmacological therapy (p < 0,001). There was no significant difference in dynamic visual acuity between groups (p = 0,24). The effects of medication with the active ingredients betahistine and dimenhydrinate were similar (p > 0,05). Conclusion: The vestibular rehabilitation method can positively change the severity of vertigo, balance ability, and vestibular dysfunction compared to pharmacological therapy. Dimenhydrinate administered in combination with betahistine was not superior to betahistine alone but can be recommended for its antiemetic effect.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-023-03598-4.
Keywords: Balance, Benign paroxysmal positional vertigo, Pharmacological therapy, Vertigo, Vestibular rehabilitation
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common peripheral vestibular disorder and accounts for 20% of all cases of vertigo. It was first described by Barany in 1921. It is characterized by sudden, brief attacks of vertigo triggered by certain head positions, such as turning the head to one side, getting out of bed, or leaning forward [1]. Vertigo usually lasts 5–10 s and does not last longer than 30 s [2].
There is no clear evidence on the epidemiology. Possible causes are: Aging, head trauma, various diseases of the inner ear, female gender, hormonal factors, familial predisposition, osteoporosis [3], and vitamin D deficiency[4] are risk factors. BPPV commonly occurs between the ages of 50–70 years but can occur in all age groups. The incidence is 11–64 per 100,000 [1]. Lifetime prevalence is estimated at 2,4%. Two theories explain the symptoms. The first is canalithiasis, which indicates that otoliths leaving the macula circulate in a semicircular canal, and the other is cupulolithiasis, which indicates attachment of these otoliths to the utricle. In both cases, there is increased sensitivity to head movement. Approximately 80% of BPPV cases are related to the posterior canal (PC) [5]. The Dix-Hallpike test, considered positive for vertigo symptoms and torsional delayed nystagmus, is the gold standard in the diagnosis of BPPV and is particularly used in the evaluation of PC involvement, whereas the supine roll test is preferred in the diagnosis of HC involvement [6].
Pharmacological treatments and vestibular rehabilitation methods are used in the treatment of BPPV. Surgery may also be performed in persistent cases [7]. Pharmacological treatment includes anticholinergics, antiemetics, benzodiazepines, calcium channel blockers, betahistine, corticosteroids, and other drugs [8]. Vestibular rehabilitation (VR) stimulates the vestibular system through head and eye movements and improves balance by developing central compensation. VR consists of components of adaptation, habituation, and substitution. Adaptation; gaze stabilization methods; habituation; optokinetic exercises; and substitution. It includes walking and balance activities under various conditions. It has also been shown to improve everyday functions and reduce symptoms of vertigo [9]. Initially, each trial will provoke dizziness, but the repetitive exercises will promote adaptation and compensation process resulting in resolution of symptoms[10]. The canalith repositioning maneuver developed by Epley is commonly used as VR [11].
This study aimed to compare the efficacy of pharmacotherapy initiated by an otolaryngologist and vestibular rehabilitation performed by a physical therapist with respect to the parameters of vertigo severity, balance, dynamic visual acuity, and vestibular dysfunction. In addition, the superiority of two different drugs (betahistine-dimenhydrinate) over each other was determined.
Methods
Participants
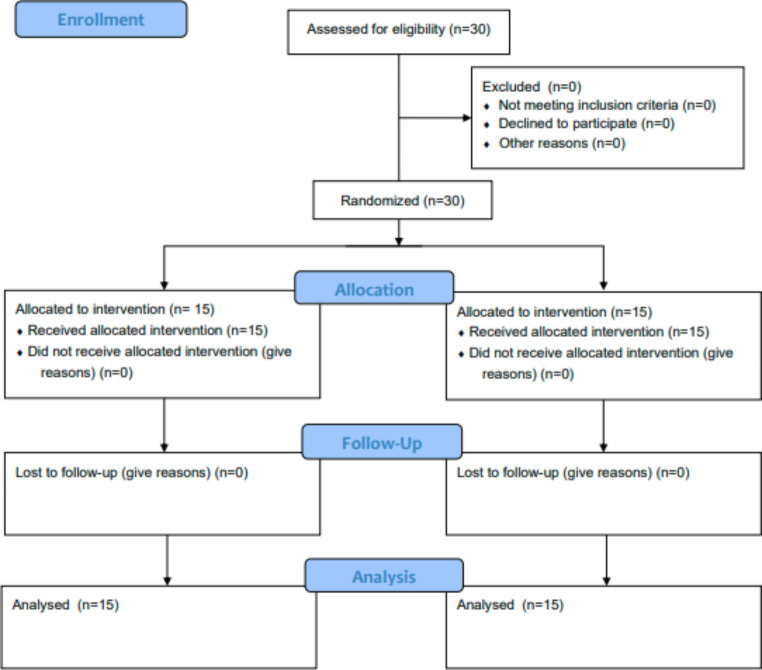
Thirty patients (40.93 ± 8.66) diagnosed with BPPV participated in the study. All patients had signed an informed consent form. Patients with a positive Dix-Hallpike test were randomly divided into two groups: the vestibular rehabilitation group (VRG) and the pharmacological control group (PCG). The flow of the study is shown in Fig. 1.
Fig. 1.
Flow diagram of the study
If patients were between 18 and 50 years of age, had a positive result on the Dix-Hallpike test, and had no spontaneous nystagmus, they were enrolled in the study. Patients with Meniere’s disease, vestibular neuritis, labyrinthitis, sudden sensory hearing loss, chronic otitis media, nonambulatory patients, vertigo due to central causes, and cardiac conditions were excluded from the study. In addition, patients who were uncooperative and had contraindications to canalith repositioning applications such as spinal deformity or disc pathology were excluded from the study.
Interventions
Vestibular Rehabilitation Group
Maneuvering and repetitive exercises were performed by a trained physiotherapist on the day of the clinic visit. The assessment and rehabilitation program was performed by a different physiotherapist. One physiotherapist conducted the assessment sessions while the other implemented the VR program. VR Protocols were performed in individual one-hour sessions once per week for four weeks. In addition to the maneuvers, we used repetitive vestibular exercises in our study. The maneuvers were performed following the exercises in the first session. In the following sessions, the maneuvers were repeated according to the patients’ needs. The protocol of repeated exercises consisted of four steps [12].
In the first session, patients performed head and eye movements in a sitting position. Patients initially moved their heads in different directions while focusing their eyes on a stationary object for 10 repetitions. Then, the patients followed the moving object with their eyes while their head was still. Afterward, patients did the same head movements for 10 repetitions with their eyes closed without focusing on any object. Finally, patients walked 40 m in a straight line.
In the second session, patients moved their heads in different directions in the Romberg, semi-tandem, and tandem positions while looking at a stationary object. Then, exercises for walking straight ahead and walking backward were performed. All exercises were performed in 10 repetitions with eyes open and closed.
In the third session, the level of exercises was gradually increased and emphasis was placed on dynamic movements. Participants were asked to move their head to the right and left while walking backward, holding their hands first at their sides and then on their backs. Then, participants performed tandem walking with their hands at their sides and then with their hands clasped behind and in front of them.
In the last session, patients performed the first week’s exercises once a day for four weeks with 10 repetitions to prevent potential attacks. We explained to the patients that they could stop doing the exercises after the four-week prevention program.
At the end of each exercise session, the therapist gave the patients home exercise programs that were to include 10 repetitions and three times daily.
12 of 15 patients (80%) had PC-BPPV; 3 patients (20%) had HC-BPPV. In the Dix-Hallpike test, patients sit on the examination table with their head turned approximately 45 degrees to the side (to the side being tested). The therapist holds the patient’s head and quickly brings the patient in the supine position with the head in hyperextension. When the patient is in this position, nystagmus is observed. The Epley maneuver begins by rotating the head 45 degrees to the affected side while the patient is sitting, and then the patient rapidly turns the supine position with the head hanging beyond the bed at approximately 30 degrees. Next, the patient rotates the head 90 degrees toward the unaffected side without raising it. Following this rotation, the patient turns the head and trunk 90 degrees to the unaffected side, facing the floor. Each position is held for approximately 1 min or until the resolution of symptoms and/or nystagmus. Then, the patient is brought slowly into an upright sitting position, completing the maneuver [13].
The supine roll test has been used in diagnosing patients with HC-BPPV. Because the horizontal canals are parallel to the plane of gravity, the test is performed in the supine position with the patient’s head flexed 30 degrees. In this position, the patient’s head is rapidly rotated 90 degrees to the left or right in the horizontal plane. The presence of nystagmus is observed, then the head is rotated to the midline and rapidly to the other side. This maneuver allows the patient to move away from the affected side in 90-degree increments. Initially, the patient is placed in the supine position with the head elevated 30 degrees. Then, the patient’s head (or entire body) is rotated 90 degrees to the affected side and maintained for 30 s or until the nystagmus and vertigo cease. From this position, the head is rotated to the neutral position, then 90 degrees to the unaffected side, and finally to the prone position. Each of these positions is maintained for 30 s or until the nystagmus and vertigo stop [14].
Based on a previous study, we did not recommend postural restraint after treatment [15].
Pharmacological Control Group
An otolaryngologist administered betahistine and/or dimenhydrinate to patients. Patients in this group were divided into two subgroups. The first group, Group A (n = 8, 53%), was selected from patients who received 24 mg of betahistine twice daily in the morning and evening for four weeks, while the other group, Group B (n = 7, 47%), began with 50 mg of dimenhydrinate once daily in combination with 24 mg of betahistine twice daily.
Participants in this group were instructed to maintain their activities of daily living in addition to pharmacological therapy.
Outcome Measures
All patients were evaluated before and after 4 weeks. Perceived vertigo severity was assessed with a visual analog scale (VAS); the static balance was measured with one-legged stance (OLS) test on firm and soft surfaces with eyes open and closed, Romberg test, and Tandem test; dynamic visual acuity (DVA) was assessed with Snellen chart; vestibular dysfunction was assessed with the Unterberger test with eyes closed. Balance tests were performed with a stopwatch. We evaluated the patients’ ability to maintain their balance for 30 s.
Statistical Analysis
The data were analyzed using a software package Statistical Package for Social Science 22.0 (SPSS for Windows, IBM Corp., Chicago, IL, USA). We determined that at least 15 patients in each group should be enrolled to achieve a power of 80% allowing type I error 0,1 and effect size 0,95. 30 BPPV patients were included in the study. Quantitive variables were summarized as mean ± SD. The normality of data was checked using Shapiro-Wilk test. Differences between groups at the initial assessment and at the final assessment were compared with the Mann-Whitney U test. The Wilcoxon test was used for all tests in Analysis to compare initial assessment and final assessment data within each group. The statistical significance value was set as p ≤ 0.05.
Results
We enrolled 30 patients in the study. There were no dropouts in the study. VRG and PCG consisted of 15 patients (n = 15, 50%; n = 15, 50%). In total, 30 patients completed the study. Eighteen (60%) of the patients were female and 12 (40%) were male. The VRG ranged in age from 18 to 50 years (mean 40,13 ± 8,72) and the PCG ranged in age from 25 to 50 years (mean 41,4 ± 8,82). The smoking and alcohol use of the patients were questioned. Table 1 shows the demographic characteristics of the study population.
Table 1.
Demographic characteristics of study population
| Group | ||
|---|---|---|
|
Vestibular Rehabilitation Group
(n=15) |
Pharmacological Control Group
(n=15) |
|
| Male/Female | 2/13 | 10/5 |
| Age, year min-max (mean) | 18-50 (40,13±8,72) | 25-50 (41,4±8,82) |
| Smoking/Alcohol | 3/2 | 6/0 |
Spontaneous nystagmus was not observed in any patient as a result of the videonystagmography evaluation.
Table 2 shows the intra-group and inter-group comparison of the values in the DVA, VAS, static balance, and vestibular dysfunction in the VRG and the PCG. When comparing the VRG and PCG before and after the intervention there were no significant differences in the value of the DVA, Romberg test, and Tandem test performed with eyes open (p > 0,05). According to the VAS results, the severity of dizziness decreased more in the VRG group (p < 0.01). More improvement was found in the VRG in the results of the Romberg test with eyes closed and standing on one leg, in which static balance was evaluated (p < 0.001; p ≤ 0.05). Vestibular dysfunction showed greater improvement in the VRG group (p < 0.001).
Table 2.
Intra-group and inter-group comparison of vestibular rehabilitation group and pharmacological control group in balance, dizziness, visual acuity and vestibular functions
| Vestibular Rehabilitation Group (n=15) | Pharmacological Control Group (n=15) | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Measures | Baseline Mean ± SD |
4 week Mean ± SD |
p* | Baseline Mean ± SD |
4 week Mean ± SD |
p* | Difference Mean ± SD |
p* |
| OLST FIRM EO right foot | 17,92 ± 15,15 | 29,05 ± 3,64 | 0,014* | 26,85 ± 7,62 | 27,25 ± 7,22 | 0,59 | 5,76 ± 11,47 | 0,01* |
| OLST FIRM EO left foot | 15,90 ± 14,69 | 30,00 ± 0,00 | 0,008* | 27,73 ± 7,15 | 28,31 ± 6,53 | 0,18 | 7,33 ± 12,36 | p<0,001* |
| OLST FIRM EC right foot | 8,32 ± 9,98 | 26,11 ± 6,89 | 0,001* | 12,45 ± 7,44 | 15,02 ± 7,18 | 0,02* | 10,17 ± 11,19 | p<0,001* |
| OLST FIRM EC left foot | 8,7 ± 11,26 | 25,60 ± 7,24 | 0,001* | 11,97 ± 7,99 | 14,28 ± 7,40 | 0,02* | 9,59 ±11,16 | p<0,001* |
| OLST SOFT EO right foot | 14,02 ± 14,61 | 28,81 ± 3,75 | 0,007* | 26,41 ± 5,85 | 27,86 ± 4,21 | 0,08 | 8,11 ± 12,06 | p<0,001* |
| OLST SOFT EO left foot | 14,05 ± 14,49 | 29,67 ± 1,27 | 0,006* | 25,34 ± 8,32 | 27,57 ± 6,53 | 0,11 | 8,11 ± 12,06 | p<0,001* |
| OLST SOFT EC right foot | 5,12 ± 8,37 | 22,58 ± 8,00 | 0,001* | 8,72 ± 4,58 | 12,42 ± 6,51 | 0,01* | 10,58 ± 10,36 | p<0,001* |
| OLST SOF EC left foot | 5,03 ± 8,09 | 22,78 ± 7,35 | 0,001* | 7,95 ± 6,48 | 10,18 ± 7,02 | 0,10 | 11,01 ± 10,32 | p<0,001* |
| DVA | 0,28 ± 0,22 | 0,07 ± 0,11 | 0,012* | 0,35 ± 0,31 | 0.24 ± 0,26 | 0,02* | -0,16 ± 0,23 | 0,24 |
| Romberg test | 27,48 ± 6,09 | 29,24 ± 2,92 | 0,10 | 27,61 ± 6,99 | 27,74 ± 6,86 | 0,31 | 0,94 ± 3,92 | 0,27 |
| Tandem test EC | 14,54 ± 12,18 | 30,00 ± 0,00 | 0,005* | 18,05 ± 11,04 | 22,97 ± 9,69 | 0,008* | 10,19 ± 11,60 | 0,05* |
| Unterberger test EO | 1,00 ± 0,00 | 1,00 ± 0,00 | 1,00 | 1,00 ± 0,00 | 1,13 ± 0,35 | 0,15 | 0,06 ±0,25 | 0,15 |
| Unterberger test EC | 1,86 ± 0,35 | 1,26 ± 0,45 | 0,007* | 1,40 ± 0,50 | 1,60 ±0,50 | 0,08 | -0,20 ± 0,66 | p<0,001* |
| VAS | 5,64 ± 2,04 | 0,95 ± 1,40 | 0,001* | 6,38 ± 1,58 | 4,49 ±1,88 | 0,001* | -3,29 ±2,40 | p<0,001* |
Abbreviations: OLST, One Legged Stance Test; EO, Eyes open; EC, Eyes Closed; DVA, Dynamic Visual Acuity; VAS, Visual Analog Scale; *p≤0,05. Wilcoxon test, Mann-Whitney U test
In all evaluations, there was no statistically significant difference between dimenhydrinate combined with betahistine and betahistine-only groups (p > 0,05) (Table 3).
Table 3.
Comparison of betahistine and dimenhydrinate combination and betahistine-only in balance, dizziness, visual acuity, and vestibular function.
| Group A (n = 8) | Group B (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Measures | Baseline Mean ± SD |
4 week Mean ± SD |
p* | Baseline Mean ± SD |
4 week Mean ± SD |
p* | Difference Mean ± SD |
p* |
| OLST FIRM EO right foot | 24,10 ± 9,89 | 24,85 ± 9,50 | 0,59 | 30,00 ± 0,00 | 30,00 ± 0,00 | 1,00 | 0,40 ± 2,11 | 0,56 |
| OLST FIRM EO left foot | 25,74 ± 9,63 | 26,83 ± 8,94 | 0,18 | 30,00 ± 0,00 | 30,00 ± 0,00 | 1,00 | 0,58 ± 1,76 | 0,17 |
| OLST FIRM EC right foot | 10,65 ± 5,60 | 13,51 ± 6,25 | 0,32 | 14,50 ± 9,14 | 16,74 ± 8,26 | 0,02* | 2,57 ± 4,19 | 0,64 |
| OLST FIRM EC left foot | 10,09 ± 10,08 | 13,16 ± 9,52 | 0,12 | 14,13 ± 4,53 | 15,56 ± 4,30 | 0,06 | 2.30 ± 4,38 | 0,14 |
| OLST SOFT EO right foot | 23,27 ± 6,66 | 26,00 ± 5,19 | 0,08 | 30,00 ± 0,00 | 30,00 ± 0,00 | 1,00 | 1,45 ± 3,73 | 0,14 |
| OLST SOFT EO left foot | 21,27 ± 9,90 | 25,46 ± 8,63 | 0,11 | 30,00 ± 0,00 | 30,00 ± 0,00 | 1,00 | 3,69 ± 5,79 | 0,24 |
| OLST SOFT EC right foot | 7,05 ± 5,01 | 12,79 ± 8,40 | 0,06 | 10,62 ± 3,44 | 11,98 ± 4,04 | 0,09 | 2,23 ± 9,23 | 0,81 |
| OLST SOF EC left foot | 6,99 ± 7,63 | 10,14 ± 9,12 | 0,32 | 7,95 ± 6,48 | 10,23 ± 4,26 | 0,23 | 1,45 ± 3,73 | 0,14 |
| DVA | 0,45 ± 0,36 | 0,28 ± 0,32 | 0,03* | 0,24 ± 0,22 | 0,20 ± 0,18 | 0,27 | 0,10 ± 0,21 | 0,26 |
| Romberg test | 25,52 ± 9,33 | 25,76 ± 9,20 | 0,31 | 30,00 ± 0,00 | 30,00 ± 0,00 | 1,00 | 0,12 ± 0,49 | 0,35 |
| Tandem test EC | 13,28 ± 10,62 | 21,56 ± 11,45 | 0,02* | 23,50 ± 9,48 | 24,59 ± 7,76 | 0,10 | 4,92 ± 8,44 | 0,18 |
| Unterberger test EO | 1,00 ± 0,00 | 1,00 ± 0,00 | 1,00 | 1,00 ± 0,00 | 1,28 ± 0,48 | 0,15 | 0,13 ± 0,35 | 0,11 |
| Unterberger test EC | 1,37 ± 0,51 | 1,5 ± 0,53 | 0,31 | 1,42 ± 0,53 | 1,71 ± 0,48 | 0,15 | 0,20 ± 0,41 | 0,45 |
| VAS | 7,18 ± 0,96 | 4,77 ± 12,27 | 0,01* | 5,45 ± 1,70 | 4,17 ± 1,43 | 0,01* | 1,88 ± 2,03 | 0,38 |
Abbreviations: OLST, One Legged Stance Test; EO, Eyes open; EC, Eyes Closed; DVA, Dynamic Visual Acuity; VAS, Visual Analog Scale; *p≤0,05. Wilcoxon test, Mann-Whitney U test
Discussion
In our study investigating the effects of VR on dizziness, balance, dynamic visual acuity, and vestibular dysfunction in BPPV patients, VR may improve dizziness, balance, and vestibular dysfunction more than pharmacological treatment. This study investigates the effect of maneuvering and repetitive exercises in BPPV disease.
In the literature, it has been reported that the Epley maneuver in PC-BPPV [16–18] and the BBQ maneuver in HC-BPPV provide rapid and effective recovery [19, 20]. In the VR method, repetitive exercises and maneuvers are applied together; thus, it is aimed to maximize the neuroplasticity of the central nervous system and improve the postural control system by using adaptation, habituation, and substitution approaches [21]. On the other hand, the most commonly used drugs in the treatment of peripheral vertigo are histamine modulators. Clinical trials have shown that betahistine, which facilitates vestibular compensation by increasing the microcirculation of the inner ear, is effective, safe, and highly tolerable for different types of peripheral vertigo [16, 22–24]. Wipperman J et al. [25] stated that antihistamine, antiemetic, and benzodiazepine were initially recommended for the treatment of vertigo and related nausea and vomiting. Sholtz et al. [23] used 40 mg of dimenhydrinate in 1275 BPPV patients to investigate the safety and efficacy of dimenhydrinate. They found it to be an effective and well-tolerated method of treating vertigo.
Our study showed that VR and pharmacological treatment alleviated dizziness. VR exercises combined with maneuvering exercises improve dizziness more than maneuvering alone [26, 27]. Martelluci et al., [28] evaluated patient’s dizziness level after CRP and indicated that CRP reduces patient’s severity of dizziness within 6 days. Moreno et al., [29] indicated that Epley maneuver reduces the severity of vertigo. Betahistine, on the other hand, relieves dizziness by improving inner ear microcirculation [22]. In our study, we determined that VR relieved dizziness more than medicated treatment. We attributed this to the fact that VR practices have been an active treatment method.
During the one-legged stance test and the tandem test performed on soft surface with eyes closed, it was observed that the patients showed more oscillation and had more difficulty while trying to maintain their balance. Postural control is impaired when visual inputs are absent and proprioceptive inputs are incorrect [30]. In previous studies, it was reported that postural control was affected and balance loss was experienced in BPPV patients [30, 31]. After VR, this amount of oscillation decreased and the balance capacity of the patients improved more than the PCG. The results of the test support the evidence from previous studies [21, 25] showing that repetitive exercises improve postural balance. No significant change was observed in both groups as a result of the Romberg test. This may be due to the fact that the vestibular compensation mechanism is active in patients and the Romberg test does not have sufficient sensitivity and specificity.
The DVA test measures a person’s eyesight versus rapid head movements by assessing the VOR. In patients with BPPV, nystagmus may occur with the change of head position due to cupula deflection [32]. As a result of our evaluation with the Snellen chart; In patients with BPPV, DVA insufficiency occurs due to decreased VOR. The results of our study showed that VR is effective in restoring gaze stability. The recovery mechanism may be resorption of otoliths after maneuver and induction of VOR adaptation by repeated exercises [33]. In the PCG, it was concluded that as a result of the dizziness suppressed by drugs, patient’s may have increased their social participation and thus they may have made VOR activating movements in their daily lives. There are some differences of opinion regarding age. Some researchers use age as an exclusion criterion, stating that older individuals cannot perform the test properly [32]. However, our study shows that VR improves dynamic visual acuity, regardless of the age of patients.
The Unterberger test is based on the vestibulospinal reflex (VSR) and is frequently used in the evaluation of labyrinth function. Closing the eyes during the test disables the VOR, allowing evaluation of the VSR and autolytic organs. Honaker et al., [34] stated in their study that the Unterberger test is not a reliable screening tool for peripheral vestibular asymmetry in patients with chronic dizziness. A rotation greater than 45° to either side during the test may indicate peripheral vestibular asymmetry. Although Unterberger stated that the rotation seen in the stepping test is always in the same direction as the slow phase of nystagmus, many studies examining the relationship between the rotation direction and the affected side did not report a correlation [35]. At the end of our study, we did not find a significant relationship between the direction of deviation and the BPPV-affected side. This may be due to the low sensitivity of the test in terms of direction determination. Although the sensitivity of the test is low, it has an important place in the prediction of BPPV prognosis. It has been observed that medicated treatment approaches do not provide an improvement in vestibular dysfunction. The reason for this may be that 4 weeks of pharmacotherapy is not enough.
Although there are previous studies using betahistine and dimenhydrinate for therapeutic purposes, there are very few studies comparing these two drugs. The results of the studies in the literature are controversial. Scholtz et al., [36] reported that drugs with cinnarizine combined with dimenhydrinate and betahistine active ingredient were well tolerated by patients and reduced symptoms. In a study they conducted, they found that the combination of 20 mg of cinnarizine and 40 mg of dimenhydrinate was more effective on the symptoms of vertigo in adults with peripheral vestibular disease compared to 16 mg of betahistine Inan et al., [37] reported that betahistine and dimenhydrinate drugs given in the early period were not superior to each other. Jalali et al., [38] reported that betahistine was more effective than dimenhydrinate after one week of pharmacological treatment. When we examine the results of our study; We observed that the use of dimenhydrinate combined with betahistine had no superiority over betahistine alone on the parameters of dizziness, balance, dynamic visual acuity, and vestibular dysfunction. In the indication of BPPV, dimenhydrinate is preferred because it has an anti-nausea and vomiting effect by reducing over-stimulated labyrinth activity.
Our study has several limitations. Initially, this study was single-center (performed in only one hospital) and therefore included a relatively small sample size in each group. Furthermore, follow-up sessions were not conducted. Moreover, we did not use the widely used Dizziness Handicap Inventory to assess the quality of life of patients with vestibular disorders. Future studies with larger sample sizes and longer treatment and follow-up sessions will enable both to evaluate the effectiveness of given maintenance exercise on remissions and to evaluate the effects of pharmacological therapy on vestibular dysfunction.
Conclusion
This study shows that VR and pharmacological therapy improve dynamic visual acuity in BPPV patients. However, different improvements were observed in dizziness severity, balance ability and vestibular dysfunction. VR provided greater improvement than pharmacological therapy. On the other hand, it was observed that only betahistine and betahistine combined dimenhydrinate applications were not superior to each other. Dimenhydrinate can be preferred because its antiemetic activity is evident.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgment
We would like to thank Prof. Dr. Z. Candan ALGUN for her guidance on the study design.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of Interest
The authors report no conflict of interests.
Consent for Publication
Patients signed informed consent regarding publishing their data.
Ethics Approval
This study was performed in line with the princi-ples of the Declaration of Helsinki. Ethics approval was obtained from the Istanbul Medipol University Non-Interventional Clinical Research Ethics Committee. (E-19383).
Clinical Trials Number
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Görkem ATA, Email: gata@medipol.edu.tr.
Ayşe Arzu ŞAKUL, Email: aasakul@medipol.edu.tr.
Gamze Kılıç, Email: fztgamzekilic@gmail.com.
Cengiz ÇELİKYURT, Email: cengizcelikyurt@gmail.com.
References
- 1.Kaur J, Shamanna K. Management of Benign Paroxysmal positional Vertigo: a comparative study between Epleys Manouvre and Betahistine. Int Tinnitus J. 2017;21:30–34. doi: 10.5935/0946-5448.20170007. [DOI] [PubMed] [Google Scholar]
- 2.Maslovara S, Soldo SB, Puksec M, et al. Benign paroxysmal positional Vertigo (BPPV): influence of pharmacotherapy and rehabilitation therapy on patients’ recovery rate and life quality. NeuroRehabilitation. 2012;31:435–441. doi: 10.3233/NRE-2012-00814. [DOI] [PubMed] [Google Scholar]
- 3.Ogun OA, Janky KL, Cohn ES, et al. Gender-based comorbidity in benign paroxysmal positional vertigo. PLoS ONE. 2014;9:e105546. doi: 10.1371/journal.pone.0105546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma K, Ojha T, Dabaria R, et al. Relation between posterior canal benign paroxysmal positional Vertigo and vitamin D Deficiency. Indian J Otolaryngol Head Neck Surg. 2022 doi: 10.1007/s12070-021-03070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celis-Aguilar E, Mayoral-Flores HO, Torrontegui-Zazueta LA, et al. Effectiveness of Brandt Daroff, Semont and Epley maneuvers in the treatment of Benign Paroxysmal positional Vertigo: a Randomized Controlled Clinical Trial. Indian J Otolaryngol Head Neck Surg. 2021 doi: 10.1007/s12070-021-02516-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nuti D, Zee DS, Mandalà M. Benign paroxysmal positional Vertigo: what we do and do not know. Semin Neurol. 2020;40:49–58. doi: 10.1055/s-0039-3402733. [DOI] [PubMed] [Google Scholar]
- 7.Herdman S, Clendaniel R (2014) Vestibular Rehabilitation. In: Vestibular Rehabilitation 4th Edition, 4th ed. p 50
- 8.Hain TC, Uddin M. Pharmacological treatment of vertigo. CNS Drugs. 2003;17:85–100. doi: 10.2165/00023210-200317020-00002. [DOI] [PubMed] [Google Scholar]
- 9.Wu P, Cao W, Hu Y, Li H. Effects of vestibular rehabilitation, with or without betahistine, on managing residual dizziness after successful repositioning manoeuvres in patients with benign paroxysmal positional vertigo: a protocol for a randomised controlled trial. BMJ Open. 2019;9:1–10. doi: 10.1136/bmjopen-2018-026711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yetiser S, Salturk Z. A review of the quality of life after therapeutic maneuvers in patients with benign paroxysmal positional Vertigo. Iran J Otorhinolaryngol. 2021;33:339–346. doi: 10.22038/IJORL.2021.55574.2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sacco RR, Burmeister DB, Rupp VA, Greenberg MR. Management of Benign Paroxysmal positional Vertigo: a Randomized Controlled Trial. J Emerg Med. 2014;46:575–581. doi: 10.1016/j.jemermed.2013.08.116. [DOI] [PubMed] [Google Scholar]
- 12.Rodrigues DL, Ledesma ALL, de Oliveira CAP, Bahmad F. Effect of vestibular exercises associated with repositioning maneuvers in patients with benign paroxysmal positional vertigo: a randomized controlled clinical trial. Otology and Neurotology. 2019;40:E824–E829. doi: 10.1097/MAO.0000000000002324. [DOI] [PubMed] [Google Scholar]
- 13.Lee JD, Shim DB, Park HJ, et al. A Multicenter Randomized double-blind study: comparison of the Epley, Semont, and Sham Maneuvers for the treatment of posterior canal benign paroxysmal positional Vertigo. Audiol Neurotology. 2014;19:336–341. doi: 10.1159/000365438. [DOI] [PubMed] [Google Scholar]
- 14.Gold DR, Morris L, Kheradmand A, Schubert MC (2014) Repositioning maneuvers for Benign Paroxysmal positional Vertigo. Curr Treat Options Neurol 16. 10.1007/s11940-014-0307-4 [DOI] [PubMed]
- 15.Balıkçı HH, Özbay İ. Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo. Auris Nasus Larynx. 2014;41:428–431. doi: 10.1016/j.anl.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Stambolieva K, Angov G. Effect of treatment with betahistine dihydrochloride on the postural stability in patients with different duration of benign paroxysmal positional vertigo. Int Tinnitus J. 2010;16:32–36. [PubMed] [Google Scholar]
- 17.Akula S, Reddy LS, Kiran AS, suresh AM. Clinical study of BPPV and the effectiveness of Canalolith Repositioning Manoeuvre in subjects of BPPV. Indian J Otolaryngol Head Neck Surg. 2022;74:96–102. doi: 10.1007/s12070-021-02779-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carnevale C, Arancibia-Tagle DJ, Rizzo-Riera E, et al. Efficacy of particle repositioning Manoeuvres in Benign positional paroxysmal Vertigo: a revision of 176 cases treated in a Tertiary Care Centre. Acta Otorrinolaringologica (English Edition) 2018;69:201–207. doi: 10.1016/j.otoeng.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Si L, Shen B, Li Y, et al. Clinical characteristics of patients with persistent apogeotropic and persistent geotropic direction-changing positional Nystagmus. J Clin Neurol (Korea) 2021;17:443–454. doi: 10.3988/jcn.2021.17.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zuma e Maia F, Ramos BF, Cal R et al (2020) Management of lateral semicircular canal benign paroxysmal positional Vertigo.Front Neurol11 [DOI] [PMC free article] [PubMed]
- 21.Martins e Silva DC, Bastos VH, de Oliveira Sanchez M, et al. Effects of vestibular rehabilitation in the elderly: a systematic review. Aging Clin Exp Res. 2015;28:599–606. doi: 10.1007/s40520-015-0479-0. [DOI] [PubMed] [Google Scholar]
- 22.Strupp M, Zwergal A, Feil K, et al. Pharmacotherapy of vestibular and cerebellar disorders and downbeat nystagmus: translational and back-translational research. Ann N Y Acad Sci. 2015;1343:27–36. doi: 10.1111/nyas.12774. [DOI] [PubMed] [Google Scholar]
- 23.Scholtz AW, Ilgner J, Loader B, et al. Cinnarizine and dimenhydrinate in the treatment of vertigo in medical practice. Wien Klin Wochenschr. 2016;128:341–347. doi: 10.1007/s00508-015-0905-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hahn A, Novotny M, Shotekov PM, et al. Comparison of cinnarizine / dimenhydrinate fixed combination with the Respective Monotherapies for Vertigo of various Origins. Clin Drug Investig. 2011;31:371–383. doi: 10.2165/11588920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Wipperman J. Dizziness and vertigo. Prim Care - Clin Office Pract. 2014;41:115–131. doi: 10.1016/j.pop.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Fujino A, Tokumasu K, Yosio S, et al. Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Sur. 1994;120:497–504. doi: 10.1001/archotol.1994.01880290013003. [DOI] [PubMed] [Google Scholar]
- 27.Ribeiro KMOB, de Freitas F, de Ferreira RV, et al. Effects of balance vestibular Rehabilitation Therapy in elderly with benign paroxysmal positional Vertigo: a randomized controlled trial. Disabil Rehabil. 2016;39:1198–1206. doi: 10.1080/09638288.2016.1190870. [DOI] [PubMed] [Google Scholar]
- 28.Martellucci S, Pagliuca G, de Vincentiis M, et al. Features of residual dizziness after Canalith Repositioning Procedures for Benign Paroxysmal positional Vertigo. Otolaryngol - Head Neck Surgery: official J Am Acad Otolaryngology-Head Neck Surg. 2016;154:693–701. doi: 10.1177/0194599815627624. [DOI] [PubMed] [Google Scholar]
- 29.Moreno JLB, Matos YR, Perez ER, et al. Effectiveness of the Epley manoeuvre in posterior canal benign paroxysmal positional vertigo: a randomised clinical trial in primary care. Br J Gen Pract. 2019;69:E52–E60. doi: 10.3399/bjgp18X700253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Çelebisoy N, Bayam E, Güleç F, et al. Balance in posterior and horizontal canal type benign paroxysmal positional vertigo before and after canalith repositioning maneuvers. Gait Posture. 2009;29:520–523. doi: 10.1016/j.gaitpost.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 31.Ribeiro KMOB, de Freitas F, de Ferreira RV, et al. Effects of balance vestibular Rehabilitation Therapy in elderly with benign paroxysmal positional Vertigo: a randomized controlled trial. Disabil Rehabil. 2017;39:1198–1206. doi: 10.1080/09638288.2016.1190870. [DOI] [PubMed] [Google Scholar]
- 32.Yetiser S, Ince D. Dynamic visual acuity in benign paroxysmal positional vertigo. Acta Otolaryngol. 2018;138:987–992. doi: 10.1080/00016489.2018.1498595. [DOI] [PubMed] [Google Scholar]
- 33.Herdman S, Schubert M, Das V, Tusa R. Recovery of dynamic visual acuity in unilateral vestibular hypofunction. Arch Otolaryngol Head Neck Surg. 2003;129:810–824. doi: 10.1001/archotol.129.8.819. [DOI] [PubMed] [Google Scholar]
- 34.Honaker JA, Boismier TE, Shepard NP, Shepard NT. Fukuda stepping test: sensitivity and specificity. J Am Acad Audiol. 2009;20:311–314. doi: 10.3766/jaaa.20.5.4. [DOI] [PubMed] [Google Scholar]
- 35.Taylan Cebi I, Karatas A. The assessment of fukuda stepping test results in prognosis of benign paroxysmal postural vertigo. Braz J Otorhinolaryngol. 2021 doi: 10.1016/j.bjorl.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scholtz AW, Hahn A, Stefflova B, et al. Efficacy and safety of a fixed combination of Cinnarizine 20 mg and Dimenhydrinate 40 mg vs Betahistine Dihydrochloride 16 mg in patients with peripheral vestibular Vertigo: a prospective, multinational, Multicenter, Double-Blind, Randomized, non-inferior. Clin Drug Investig. 2019;39:1045–1056. doi: 10.1007/s40261-019-00858-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Inan HC, Kirac M. An evaluation of the Effects of Betahistine and Dimenhydrinate on posterior canal benign paroxysmal positional Vertigo. Turk Arch Otorhinolaryngol. 2019;57:191–196. doi: 10.5152/tao.2019.4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jalali MM, Gerami H, Saberi A, Razaghi S. The impact of Betahistine versus Dimenhydrinate in the resolution of residual dizziness in patients with benign paroxysmal positional Vertigo: a Randomized Clinical Trial. Annals of Otology. Rhinology and Laryngology. 2020;129(5):434–440. doi: 10.1177/0003489419892285. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.