Abstract
Rhinolith is an uncommon condition that usually happens due to mineralisation of calcium and magnesium salts over a retained foreign body inside the nasal cavity for long period of time. Here we report one such case of a 33-year-old lady who presented to us with long standing intermittent epistaxis and on examination rhinolith was discovered.
Keywords: Huge, Staghorn, Rhinolith, Young adult
Introduction
Rhinolith is a Greek word which means stone in the nose [1]. It is a rare condition that happens due to deposition of calcium and magnesium over a foreign body intranasally. This foreign body can be endogenous or exogenous in nature [2, 3]. Endogenous causes are mucus plugs, blood clot and bone fragments whereas exogenous causes are papers, plastics, organic seeds and beads [1, 3]. The mineralization of the rhinolith takes time and it’s a slow process [3]. The symptoms may appear after few months or years [3]. Common presentations would be persistent or recurrent nasal foul smelling discharge, nasal bleed, nasal block and infections which normally involve only one side of the nose [3].
Recently, with the advancement of endoscopic technology, most of the foreign bodies in the nose can be detected early and removal can be done much quicker before the formation of rhinolith. This is the reason rhinolith has become very rare in this modern era.
We report a case of a 33-year-old lady who presented to us with chronic unilateral epistaxis and noted to have a large and bizarre looking rhinolith occupying the entire nasal cavity. Computer tomography findings, surgical removal and post-surgical management are discussed.
Case Presentation
A 33-year-old Chinese lady with underlying hypertension presented with the complaint of recurrent left sided epistaxis for the past 20 years associated with left nasal block and intermittent left nasal foul-smelling discharge. There was no facial pain or headache. Patient unable to recall any history of inserting foreign body into her nose when she was young. Patient also denied any trauma, loss of weight or loss of appetite.
On examination, patient appear pale and there was mucopurulent blood-stained discharge from left nose. Anterior rhinoscopy and nasal endoscopy showed irregular huge mass obstructing whole left nasal cavity which bled upon suctioning. No mass seen over right nasal cavity.
Computed tomography scan was ordered and the report came back as dystrophic coarsely calcified mass occupying whole left nasal cavity (Fig. 1), extending superiorly to roof, inferiorly the floor and posteriorly the choana with complete opacification of the left nasal cavity and left maxillary sinus (Fig. 2). Left inferior turbinate appear eroded with mild cortical bone erosion over the floor. The mass also extends through the posterior choanae to the nasopharynx. Considering the extend and shape of rhinolith we proceeded with endoscopic removal of rhinolith under general anaesthesia.
Fig. 1.
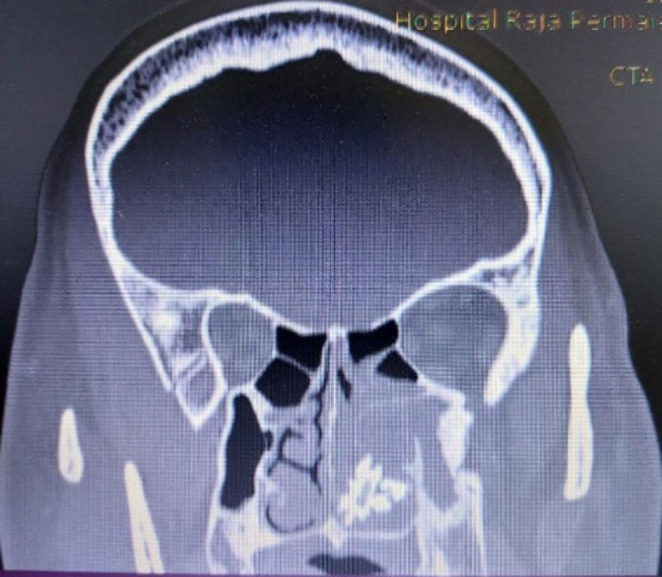
Coronal view of the computed tomography of paranasal sinuses revealed a densely calcified mass seen in the left nasal cavity
Fig. 2.
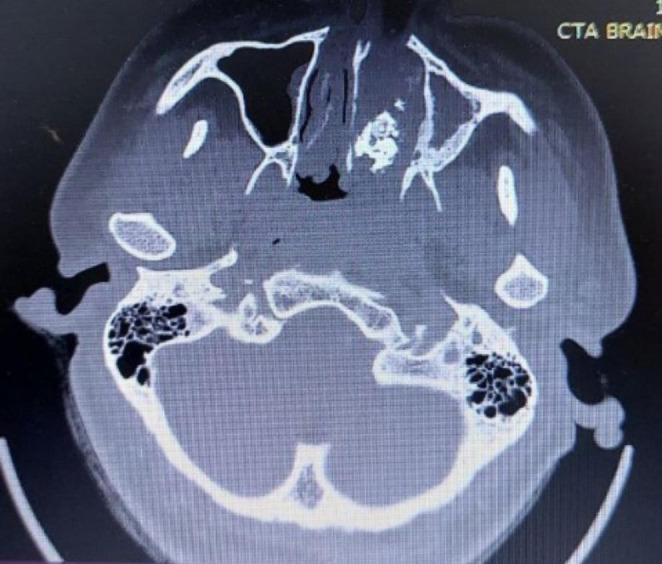
Axial view of the computed tomography of paranasal sinuses revealed a densely calcified mass seen in the left nasal cavity
Intraoperatively, a 0-degree nasal rigid endoscope could barely be introduced into the nasal cavity. There was a huge stony hard mass in the left nasal cavity with spicules and extensive granulation tissues surrounding it (Fig. 3). The granulation tissue bridges were cauterized and the rhinolith was completely removed in piecemeal (Fig. 4). Both the left inferior and middle turbinate were completely eroded. There was also an arterial bleeding from the nasal floor from the eroded segment likely a branch of descending palatine artery which stopped after cauterization. Estimated blood loss was 300mililitres. Nasal cavity was washed with copious amount of warm normal saline. Silastic splint was inserted to prevent adhesions of the raw area.
Fig. 3.
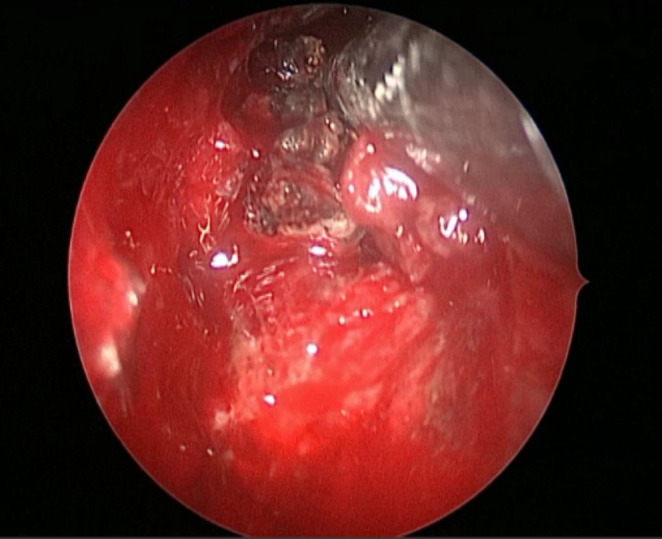
Rhinolith seen intraoperatively with surrounding granulation tissues
Fig. 4.

Rhinolith removed completely in piecemeal
Post operatively, patient was prescribed with alkaline nasal douching, corticosteroid nasal douche and oral antibiotic for 1week. Silastic splint was removed after 2 week and repeated nasal endoscopy showed a healing mucosa. She made a good post operative recovery and was symptom free subsequently.
Discussion
Mineralized foreign body was first described by Bartholini in 1654 as a stone hard foreign body which had grown around cherry stone [4]. Generally, the term rhinolith started to be used from 1845 [4]. The incidence of rhinolith is not common as is it only 1 in 10 000 Otorhinolaryngology outpatients. This is more commonly seen in children especially mentally challenged. Rhinolith in adult is considered a rare condition [3].
Although, most of the time etiology is unknown, the most common cause is retained foreign bodies. These foreign bodies normally get access into nasal cavity anteriorly, although some may enter posteriorly through vomiting or coughing [2].
Pathogenesis for the formation of rhinolith is still unclear. There are few theories involved in their formation such as impaction of foreign body, acute and chronic inflammation, demineralization of salts and mechanical obstruction of mucus and pus. Acute and chronic inflammation over the nasal mucosal lining may increase nasal discharge with high amount of calcium, magnesium, iron, carbonate, aluminium, glutamic acid and glycine. Over time, these may eventually form a huge stone like mass [5].
The symptoms usually won’t appear until the rhinolith is big enough to cause obstruction and destruction to surrounding structures [2]. Symptoms usually unilateral, even though there are reported bilateral rhinolith in some literature [5]. Complications like septal perforation, septal deviation, lateral nasal wall destruction, oro-antral fistula and or-nasal fistula are rare [5].
Rhinolith can be diagnosed clinically based on history, clinical examination and complementary test. Clinical examination should include anterior rhinoscopy and nasal endoscopy whenever available [1]. Although diagnosis is based on clinical ground, but it may be challenging in the presence of extensive inflammation around the foreign body [6]. Differential diagnosis like fungal sinusitis, osteoma, ossifying fibroma, odontomes, calcified polyps, granulomas, sarcomas and sinonasal malignancies need to be ruled out [2]. Simple x-rays and paranasal computed tomography scans are important to establish the diagnosis and will be helpful in surgical mapping for the removal of rhinolith [1].
The main aim in the management of rhinolith is to remove it without any complication. Either endoscopic or external open approaches can be used for a huge rhinolith although smaller one can be taken out in clinic followed by anterior nasal packing if needed. General anaesthesia is normally preferred as this procedure is very painful and has high risk of bleeding [3]. External open approaches like lateral rhinotomy and Caldwell Luc will only be considered when endoscopes are not available. Most of the time, endoscopes are used for better visualization and to reduce complications.
In some cases, raw areas are seen after removal of foreign body and silastic splint will be used to prevent synechiae formation [3]. In this case, there were extensive granulation tissues seen occupying the whole of left nasal cavity which bled upon removal of the rhinolith. The granulation tissues were managed by cauterization followed by silastic splint application which were kept for 2weeks and daily budesonide nasal irrigation to maximise the contact of steroid to nasal mucosa.
Conclusion
Although rhinolith is uncommon, high index of suspicion should present in all attending front liners especially when the patients present with unilateral nasal obstruction, bleeding and foul-smelling discharge. The patients should be sent to nearest available otorhinolaryngology centre for further evaluation and removal of the rhinolith.
Funding
The authors received no financial support for the research and publication of this article.
Declarations
Conflict of Interest
The authors shared no conflicts of interest in regards of the research and publication of this article.
Informed Consent
Written informed consent was obtained from the patient to be published in this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vijay V. Kumareysh, Email: kumareyshvijay@gmail.com
Norasnieda Md Shukri, Email: asnieda@usm.my.
References
- 1.Shah FA, George S, Reghunanden N (2010 Jul) A case presentation of a large rhinolith. Oman Med J 25(3):230–231. 10.5001/omj.2010.64 [DOI] [PMC free article] [PubMed]
- 2.Noh KB, Sachlin IS, Gazali N, Norasnieda Md Shukri Giant rhinolith: a case report. Egypt J Ear Nose Throat Allied Sci. 2017;18(2):155–157. doi: 10.1016/j.ejenta.2016.09.005. [DOI] [Google Scholar]
- 3.Ali M. Giant ’staghorn’ rhinolith in a 15-year-old girl. BMJ Case Rep. 2018;11:e227587. doi: 10.1136/bcr-2018-227587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brehmer D Randolf Riemann. The Rhinolith-A possible Differential diagnosis of a unilateral nasal obstruction. Case Reports in Medicine.2010 Jun.:845671.doi: 10.1155/2010/845671 [DOI] [PMC free article] [PubMed]
- 5.Tan Shi Nee, Salina H, Primuharsa Putra SHA. Huge rhinolith in adult. Turk Arch Otolarngol. 2014;52:148–150. doi: 10.5152/tao.2014.711. [DOI] [Google Scholar]
- 6.Chacko SP, Shere DS, Shetty AK, Sheth RK, Patangrao HD. Giant Rhinolith in a bizarre form. Int J Head Neck Surg. 2022;13(3):91–93. doi: 10.5005/jp-journals-10001-1533. [DOI] [Google Scholar]


