Abstract
Introduction: Benign paroxysmal positional vertigo is one of the common vestibular disorders encountered in ENT clinics with accompanying vertigo. Study to evaluate the additive effects of betahistine on Epley’s manoeuvre in treating posterior BPPV patients.
Material and Methods: Prospective study was conducted on 50 patients of posterior BPPV diagnosed by the Dix Hallpike test. Subjects were divided into Group A which received the Betahistine therapy along with the canalith repositioning technique (Epley’s manoeuvre) and the second group (Group B) which received the Epley’s manoeuvre alone. The patients were assessed at 1 week and 4 weeks by Visual Analogue Scale (VAS), Dizziness Handicap Inventory (DHI) and Short Form 36 (SF-36).
Results: At the end of 4 weeks, 2 patients in group A (E + B) had positive Dix-Hallpike and 23(92%) had negative Dix-Hallpike, while 11 patients in group B (E) had positive Dix-Hallpike and 14 (56%) had negative Dix-Hallpike with P value < 0.001. The Mean baseline (T0) Visual Analogue Scale (VAS) score in group A (E + B) was 8.60 ± 1.080 and in group B (E) was 8.92 ± 0.996. Post-treatment VAS score was significantly lower in both the groups and was significantly lower in group A(E + B) than in group B (E) (0.680 ± 1.930 vs. 3.96 ± 3.587, respectively, p-value < 0.001). The Mean baseline (T0) Dizziness Handicap Inventory (DHI) scores were similar in groups A and B (77.36 ± 9.49 vs. 80.00 ± 8.9, respectively, p = 0.271). After treatment, the DHI values were significantly lower in both groups. Group A had a better DHI score than group B (10.56 ± 17.12 vs. 44.72 ± 27.35, p < 0.001). The mean baseline (T0) Short Form 36 (SF-36) scores were also similar in groups A and B (19.53 ± 6.85 vs. 18.79 ± 5.50, p = 0.823). Post-treatment of 4 weeks, the SF-36 score significantly improved in both the groups and significantly improved in group A than group B (84.27 ± 17.28 vs. 46.53 ± 24.53, p < 0.001).
Conclusion: Betahistine therapy in conjunction with Epley’s manoeuvre leads to better symptom control and is more effective than Epley’s alone in treating BPPV patients.
Keywords: BPPV, vertigo, Epley’s manoeuvre, betahistine
Introduction
Vertigo, a subtype of dizziness is defined as an illusion of motion caused by a mismatch of information from the visual, vestibular and proprioceptive systems. It is a common symptom that may be a manifestation of several underlying etiologies and may occur due to damage within the inner ear, by afflictions of the brain stem and cerebellum, or may even be psychogenic in origin. [1, 2] 45 to 54% of the patients who attend the primary care physician with dizziness are estimated to be suffering from vertigo. [3].
Vertigo itself can either be of peripheral or central origin. [2] Acute onset vertigo with nausea and vomiting usually reflects damage to the vestibular system which may result in serious handicap with considerable psychological morbidity. [4] It can severely affect the individual’s quality of life, from being incompetent to undertake normal work or social activities to persistent sleep for several hours and an off-balance sensation lasting for several days. [5].
Benign paroxysmal positional vertigo (BPPV) is the most common peripheral vestibular disorder, accounting for 20% of all vertigo cases and the vast majority of all BPPV cases are of the posterior canal variant. [6, 7] BPPV was first described by Barany in 1921, attributing the disorder to otolith disease. [8] BPPV is idiopathic in nearly half of patients; however, head trauma, senility, inner ear diseases, prolonged rest, hypertension, hyperlipidemia, stroke, and migraine may constitute its secondary causes. [9] The acute sense of rotation of the surroundings or self, worsened by the changing position of the head and body, with the absence of associated neurological deficits, is its main manifestation. [10].
The bedside Dix-Hallpike test combined with a detailed history is the key to making the diagnosis of BPPV. [11] The mainstay treatment of BBPV is to perform an appropriate repositioning manoeuvre to move and/or liberate dislodged otoconia inside the involved canal and send them back to utriculus. For posterior canal BPPV, the manoeuvre developed by Epley is particularly effective. [12] But it was reported, despite the repositioning manoeuvres the symptoms of BPPV may continue to persist for up to more than 3 months in less than 20% of patients bringing a significantly negative impact on daily living. [13, 14] To amend this, several studies were performed with betahistine (histamine-like substance), to decrease the severity and attack frequency of vertigo owing to its effects of increasing labyrinthine microcirculation and suppressing the increased neuronal activity in vestibular receptor cells, afferent neurons, and vestibular nuclei. [15, 16]
It has been previously shown that betahistine improves the quality of life (QOL) of patients with peripheric vestibular vertigo by decreasing recurrence, and dizziness and bettering the general condition of the patients. [15, 17] Several other studies have also proved that the combination of betahistine and repositioning manoeuvres improve the outcomes, in comparison to manoeuvres alone but its use for BPPV remains still controversial. [18] In this prospective observational study, we aimed to evaluate the effects of betahistine in addition to Epley’s manoeuvre on the quality of life (QOL) indices of patients suffering from the most common form of BPPV-Posterior Semicircular Canal (PSC) BPPV.
Materials and Methods
The present prospective and observational study was conducted on 50 patients of BPPV in dept. of ENT, Rajindra Hospital, Patiala between December 2015 and October 2017. Ethical approval was obtained from the local institutional ethics committee and informed consent was taken from all the subjects. The inclusion criteria was-patients of BPPV above 18 years of age with positive Dix Hallpike test. The patients excluded were adults above 80 years of age, those suffering from cervical spondylosis, multiple semicircular canal disease, inner ear disease, unstable heart disease, vertigo caused by CNS lesions, migraine and patients on vestibulosuppressant and ototoxic medications.
A detailed Clinical History of each patient was taken and recorded. A total of 50 patients with vertigo were randomized into two groups of 25 each. One group (Group A) received the Betahistine therapy along with the canalith repositioning technique (Epley’s manoeuvre) and the second group (Group B) received Epley’s manoeuvre alone. The patients were assessed by a Visual Analogue Scale (VAS) for the severity of vertigo. The patients were asked to scale their symptoms of vertigo from 0 to 10, where 0 was no vertigo. The grading was 1–3 for mild vertigo, 4–7 for moderate and 8–10 was severe vertigo.
Additionally, all the patients were asked to fill out 2 quality of life questionnaires, Dizziness Handicap Inventory (DHI) and Short Form 36 (SF-36). Dizziness Handicap Inventory (DHI) consisting of 25 questions, and a total score (0–100 points) was obtained by summing ordinal scale responses, with higher scores indicating more severe handicap. In the SF-36 Health Survey questionnaire, we asked 36 questions to measure functional health and well-being from the patient’s point of view. The SF-36 consisted of eight scaled scores, which were the weighted sums of the questions in their section. The lower the SF-36 total score, the more the disability.
The selected group (A) of patients was treated by Epley’s manoeuvre along with betahistine 24 mg twice daily for a week or till the patients had complete resolution of symptoms. The other group (B) of patients was only treated by Epley’s manoeuvre alone. Epley’s manoeuvre was repeated a maximum of 2 times. Baseline information and clinical history of all the patients were collected and the procedures and treatment assigned to the study participants were documented. The patients were followed up for a total period of 4 weeks (T2) to assess the efficacy of the treatment using-Subjective resolution of symptomatic vertigo on change in posture, conversion of positive to negative Dix Hallpike test, Visual Analogue Scale for vertigo, DHI and SF-36 scores. Data was analyzed using descriptive statistics and a chi-square test. Suitable statistical software (SPSS15) was utilized for analysis and was presented in the form of tables, figures, graphs, and diagrams wherever necessary.
Results
A total of 50 subjects, 25 in Group A (Epley’s manoeuvre with betahistine) (E + B) and 25 in Group B (Epley’s manoeuvre alone) (E) were enrolled in this study. The mean age of group A (E + B) in the study population was 43.60 ± 12.96 years. The mean age of group B (E) in the study population was 46.96 ± 15.17 years. The majority of patients belonged to the age group 31–40 years (28%) followed by 51–60 years (24%). In Group A (E + B), 9 were males and 16 were females, with a similar composition to group B.
A total of 21 (42%) subjects had BPPV involving the left side and a total of 29 (58%) subjects had right-side involvement. Out of the 25 patients in group A (E + B), 20 patients had 1 Epley’s manoeuvre done and 5 had a total of 2 Epley’s manoeuvre done. In group B (E), 7 patients had 1 Epley’s manoeuvre done and 18 had a total of 2 Epley’s manoeuvre done. A majority (80%) of the patients in group A (E + B) received 1 week of betahistine therapy and only 20% received 4 weeks of betahistine. At the time of 2nd follow-up visit at 4 weeks, 2 patients in group A (E + B) had positive Dix-Hallpike and 23(92%) had negative Dix-Hallpike, while 11 patients in group B (E) had positive Dix-Hallpike and 14(56%) had negative Dix-Hallpike. P value came out to be < 0.001 and it was significant.
The Mean baseline (T0) Visual Analogue Scale (VAS) score in group A (E + B) was 8.60 ± 1.080 and in group B (E) was 8.92 ± 0.996. Post-treatment VAS score was significantly lower in both the groups and was significantly lower in group A(E + B) than in group B (E) (0.680 ± 1.930 vs. 3.96 ± 3.587, respectively, p-value < 0.001) (Table 1, Graph 1). The Mean baseline (T0) Dizziness Handicap Inventory (DHI) scores were similar in groups A and B (77.36 ± 9.49 vs. 80.00 ± 8.9, respectively, p = 0.271). After treatment, the DHI values were significantly lower in both groups. Group A had a better DHI score than group B (10.56 ± 17.12 vs. 44.72 ± 27.35, p < 0.001) (Table 2, Graph 2).
Table 1.
Pre and post treatment assessment by VAS scale between group A and Group B
| Time of follow up | Group | Mean VAS | S.D. | P-value | Significance |
|---|---|---|---|---|---|
|
T0 (Baseline) |
Group A (E + B) | 8.60 | 1.080 | 0.306 | NS |
| Group B (E) | 8.92 | 0.996 | |||
|
T1 (1 week) |
Group A (E + B) | 2.32 | 2.869 | 0.001 | HS |
| Group B (E) | 6.04 | 3.433 | |||
|
T2 (4 weeks) |
Group A (E + B) | 0.680 | 1.930 | < 0.001 | HS |
| Group B (E) | 3.96 | 3.587 |
Graph 1.

Pre and post treatment assessment by VAS scale between Group A and Group B
Table 2.
Pre and post treatment assessment by DHI scale between group A and Group B
| Time of follow up | Group | Mean DHI | S.D. | P-value | Significance |
|---|---|---|---|---|---|
|
T0 (Baseline) |
Group A (E + B) | 77.36 | 9.49 | 0.271 | NS |
| Group B (E) | 80.00 | 8.94 | |||
|
T1 (1 week) |
Group A (E + B) | 23.20 | 24.02 | < 0.001 | HS |
| Group B (E) | 61.52 | 25.20 | |||
|
T2 (4 weeks) |
Group A (E + B) | 10.56 | 17.12 | < 0.001 | HS |
| Group B (E) | 44.72 | 27.35 |
Graph 2.
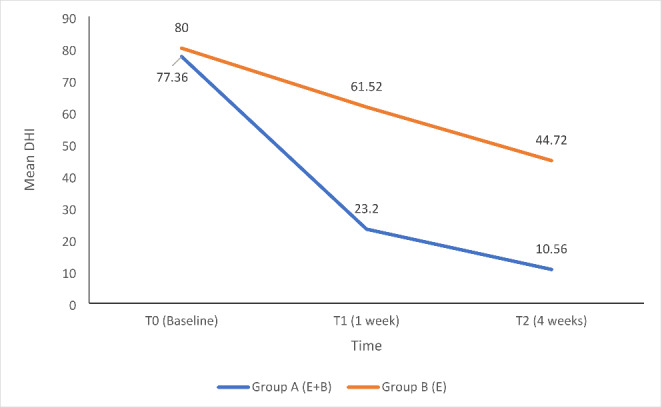
Pre and post treatment assessment by DHI scale between Group A and Group B
The mean baseline (T0) Short Form 36 (SF-36) score were also similar in groups A and B (19.53 ± 6.85 vs. 18.79 ± 5.50, p = 0.823). Post-treatment of 4 weeks, the SF-36 score significantly improved in both the groups and significantly improved in group A than group B (84.27 ± 17.28 vs. 46.53 ± 24.53, p < 0.001) (Table 3, Graph 3).
Table 3.
Pre and post treatment assessment by SF36 questionnaire between group A and Group B
| Time of follow up | Group | Mean SF-36 | S.D. | P-value | Significance |
|---|---|---|---|---|---|
|
T0 (Baseline) |
Group A (E + B) | 19.53 | 6.85 | 0.823 | NS |
| Group B (E) | 18.79 | 5.50 | |||
|
T1 (1 week) |
Group A (E + B) | 69.86 | 25.56 | < 0.001 | HS |
| Group B (E) | 30.98 | 19.11 | |||
|
T2 (4 weeks) |
Group A (E + B) | 84.27 | 17.28 | < 0.001 | HS |
| Group B (E) | 46.53 | 24.53 |
Graph 3.
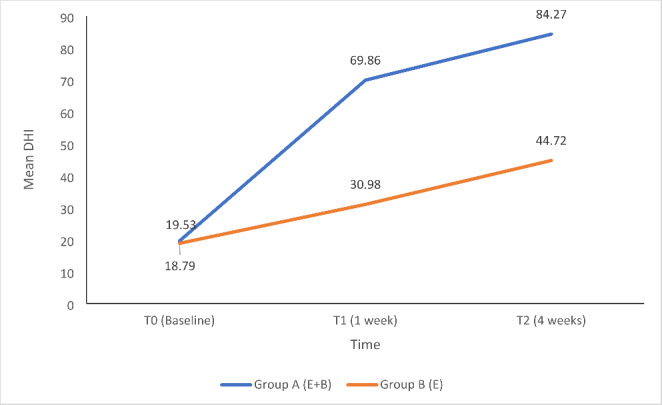
Pre and post treatment assessment by SF36 questionnaire between Group A and Group B
Discussion
Current modalities of treatment for BPPV include various repositioning manoeuvres ± vestibular rehabilitation exercises, pharmacological drugs and surgery in some of the resistant cases. Although otolith repositioning manoeuvres are the mainstay treatment of BPPV, betahistine has been popularised as a co-adjuvant treatment option for various disorders related to dizziness and vertigo. Being a histamine modulator, it improves the microcirculation of the inner ear with vasodilation and antagonises H3 receptors, thus increasing neurotransmitter release from the nerve endings. It also has a good safety profile with its typical dose ranging from 8 mg to 48 mg daily. [19].
To review this, several studies have been conducted to see if betahistine is additive to Epley’s manoeuvre for BPPV symptom resolution and in avoiding its recurrence. In a meta-analysis by Della Pepa et al., it was reported that betahistine when used in doses higher than 32 mg daily, effectively reduced symptoms in recurrent or persistent BPPV. [17].
Cavaliere et al. compared the effects of the Semont manoeuvre and Brandt-Daroff manoeuvre with or without betahistine treatment in a total of 103 subjects. In his study, he concluded that betahistine add-on therapy resulted in early recovery compared to the respective manoeuvre alone. [20] Similarly, Japneet K et al. in a study reported a success rate of 94.8% in treating BPPV with Epley’s along with betahistine as compared to 87.1% improvement rates in Epley’s manoeuvre alone groups. Moreover, the relapse rate was higher in Epley’s manoeuvre-alone group. [21] These results were similar to our study showing a 92% success rate in group A (Epley’s and betahistine) versus a 56% success rate in group B (Epley’s alone) with a significant p-value of < 0.001.
Vertigo can cause a significant negative impact on living whose severity can be assessed by various QOL (quality of life) indices. VAS is a subjective scale used to assess the severity of vertigo in BPPV patients. In the present study the mean baseline (T0) Visual Analogue Scale (VAS) score in group A (E + B) was 8.60 ± 1.080 and in group B (E) was 8.92 ± 0.996. Post-treatment (at 4 weeks) VAS score was significantly lower in both the groups and was significantly lower in group A(E + B) than group B (E) (0.680 ± 1.930 vs. 3.96 ± 3.587, respectively, p-value < 0.001).
Similar results were reported by K. Japneet, where the mean pre-treatment VAS score was 7.8 ± 0.942 in Epley’s alone group, and 7.77 ± 0.90 in Epley’s with the betahistine group. Post-treatment (at 4 weeks) VAS score was significantly lowered to 2.17 ± 1.28 in Epley’s alone group (p = 0.001) and to 1.5 ± 0.63 in Epley’s with betahistine group (p-0.001). [21].
Likewise in a study by Ibrahim Sayin et al. subjects were divided into the Epley manoeuvre + betahistine group (group A) and Epley manoeuvre only (group B) group with an overall success rate of 95% (96% in group A; 94% in group B, p = 0.024). Group A and B had similar baseline visual analog scale scores (6.98 ± 2.133 and 6.27 ± 2.148, respectively, p = 0.100). Post-treatment, the VAS score was significantly lower in both groups and was significantly lower in group A than group B (0.74 ± 0.853 vs. 1.92 ± 1.288, respectively, p = 0.000) which was similar to our study. [19].
For evaluation of the self-perceived handicapping effects imposed by diseases of the vestibular system, DHI (Dizziness handicap inventory) has also been proven to be a valuable tool. In our study, the mean baseline (T0) Dizziness Handicap Inventory (DHI) scores were similar in groups A and B (77.36 ± 9.49 vs. 80.00 ± 8.9, respectively, p = 0.271). But after treatment, the DHI values were significantly lower in both groups. Group A had a better DHI score than group B (10.56 ± 17.12 vs. 44.72 ± 27.35, p < 0.001).
In a similar study by Guneri EA (2012), the Epley’s with betahistine group had a mean pre-treatment DHI score of 60.75 ± 14.30 and Epley’s alone group had a mean pre-treatment DHI score of 45.27 ± 9.02. Post-treatment DHI score reduced to 10.42 ± 2.23 and 10.73 ± 2.12 respectively. This difference was statistically significant which showed that the improvement in symptoms was significantly better in the group receiving betahistine along with Epley’s manoeuvre. [22].
Likewise, Maslovara et al. reported the DHI score in the Epley’s with Betahistine group to be 70.45 ± 5.45 which improved to 7.52 ± 2.35 post-treatment with a p-value of 0.01 which was significant. The DHI score in the Epley’s alone group was 75.73 ± 5.90 improving to 10.5 ± 4.65 at T2 post-treatment with a P value of 0.01. The DHI score was also compared between the two groups and the result was statistically significant proving that Epley’s in combination with betahistine therapy yields better results. [23].
However, Acar et al. conducted a prospective study of 100 subjects (25 received the Epley manoeuvre + betahistine, 25 received the Epley manoeuvre + trimetazidine, 25 received the Epley manoeuvre + Gingko Biloba, and 25 underwent the Epley manoeuvre alone) and the results were assessed using the DHI questionnaire. After 3 and 5 days of treatment, the mean DHI scores of the groups receiving medication did not differ significantly from the mean DHI score of the control group (p > 0.005). This contrary result can be attributed to much short follow-up period for evaluation. [24].
Another scale of the SF-36 Health Survey questionnaire consists of 36 questions to measure functional health and well-being from the patient’s point of view. In the present study, the mean baseline (T0) Short Form 36 (SF-36) score were similar in groups A and B (19.53 ± 6.85 vs. 18.79 ± 5.50, p = 0.823). Post-treatment of 4 weeks, the SF-36 score significantly improved in both the groups and significantly improved in group A than group B (84.27 ± 17.28 vs. 46.53 ± 24.53, p < 0.001). Similar results were found in a study conducted by Maslovara et al. where the baseline SF-36 score in the Epley’s with betahistine group was 16.77 ± 5.90 which improved to 80.5 ± 15.63 post-treatment with a p-value of 0.01. The baseline SF-36 score in the Epley’s alone group was 18.77 ± 6.90 which improved to 50.5 ± 20.63 after treatment(p = 0.01). The SF-36 score was also compared between the two groups and the result was statistically significant. [23] Thus, as shown in the present study and various other studies, betahistine therapy in conjunction with Epley’s manoeuvre leads to better results than Epley’s alone in BPPV patients.
Limitations of the present study were the absence of betahistine-only or placebo control groups. Secondly, only patients suffering from posterior semi-circular canal BPPV were included in the study thus comparison of treatment results of various BPPV forms was not done.
Conclusion
BPPV is a common entity encountered in ENT and Neurology clinics these days which can be sometimes distressing to the patient causing much impairment in daily activities. In the present study, we concluded that betahistine in addition to Epley’s manoeuvre provided better symptom control in posterior BPPV patients and proved better in improving patients’ quality of life.
Authors’ Contributions
All authors contributed to the study design, data collection and analysis, manuscript drafting and revision. Final manuscript was read and approved by all the authors.
Funding
No funding was received for conducting this study.
Statement and Declarations
Conflicts of Interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics Approval
The study protocol was approved by local institutional ethic committee of Govt. Medical college and Rajindra Hospital and it was performed in accordance with the Code of Ethics of the World Medical Association according to the declaration of Helsinki of 1975, as revised in 2000
Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Strupp M, Dieterich M, Brandt T. The treatment and natural course of peripheral and central vertigo. Dtsch Arztebl Int. 2013;110:505–515. doi: 10.3238/arztebl.2013.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molnar A, McGee S. Diagnosing and treating dizziness. Med Clin North Am. 2014;98:583–596. doi: 10.1016/j.mcna.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician. 2010;82:361–368. [PubMed] [Google Scholar]
- 4.Furman JM, Balaban CD. Vestibular migraine. Ann NY Acad Sci. 2015;1343:90–96. doi: 10.1111/nyas.12645. [DOI] [PubMed] [Google Scholar]
- 5.Lacour M, van de Heyning PH, Novotny M, Tighilet B. Betahistine in the treatment of Meniere’s disease. Neuropsychiatr Dis Treat. 2007;3:429–440. [PMC free article] [PubMed] [Google Scholar]
- 6.Froehling DA, Bowen JM, Mohr DN, Brey RH, Beatty CW, Wollan PC et al (2000) The canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo: a randomized controlled trial. Mayo Clinic Proceedings. ;75(7): 695–700 [DOI] [PubMed]
- 7.Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) Can Med Assoc J. 2003;169(7):681–693. [PMC free article] [PubMed] [Google Scholar]
- 8.Bárány E. Diagnose yon krankheitserscheinungen im bereiche des otolithenapparates. Acta Otolaryngol. 1920;2(3):434–437. doi: 10.3109/00016482009123103. [DOI] [Google Scholar]
- 9.Von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710–715. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baloh R. Vestibular neuritis. N Engl J Med. 2003;11:1027–1032. doi: 10.1056/NEJMcp021154. [DOI] [PubMed] [Google Scholar]
- 11.Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Annals of Otology Rhinology & Laryngology. 1952;61(4):987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- 12.Wolf M, Hertanu T, Novikov I, Kronenberg J. Epley’s manoeuvre for benign paroxysmal positional vertigo: a prospective study. Clin Otolaryngol Allied Sci. 1999;24(1):43–46. doi: 10.1046/j.1365-2273.1999.00202.x. [DOI] [PubMed] [Google Scholar]
- 13.Lopez-Escamez JA, Gamiz MJ, Fernandez-Perez A, GomezFin ˜ana M. Long-term outcome and health-related quality of life in benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol. 2005;262:507–511. doi: 10.1007/s00405-004-0841-x. [DOI] [PubMed] [Google Scholar]
- 14.Korres S, Balatsouras DG, Ferekidis E. Prognosis of patients with benign paroxysmal positional vertigo treated with repositioning maneuvers. J Laryngol Otol. 2006;120:528–533. doi: 10.1017/S0022215106000958. [DOI] [PubMed] [Google Scholar]
- 15.Mira E, Guidetti G, Ghilardi L, et al. Betahistine dihydrochloride in the treatment of peripheral vestibular vertigo. Eur Arch Otorhinolaryngol. 2003;260:73–77. doi: 10.1007/s00405-002-0524-4. [DOI] [PubMed] [Google Scholar]
- 16.Dziadziola JK, Laurikainen EL, Rachel JD, Quirk WS. Betahistine increases vestibular blood flow. Otolaryngol Head Neck Surg. 1999;120:400–405. doi: 10.1016/S0194-5998(99)70283-4. [DOI] [PubMed] [Google Scholar]
- 17.Della Pepa C, Guidetti G, Eandi M. Betahistine in the treatment of vertiginous syndromes: a meta-analysis. Acta Otolaryngol Ital. 2006;26:208–215. [PMC free article] [PubMed] [Google Scholar]
- 18.Kanagalingam J, Hajioff D, Bennett S, Vertigo BMJ. 2005;330:523. doi: 10.1136/bmj.330.7490.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayin I, Koç RH, Temirbekov D, Gunes S, Cirak M, Yazici ZM (2022 May-Jun) Betahistine add-on therapy for treatment of subjects with posterior benign paroxysmal positional vertigo: a randomized controlled trial. Braz J Otorhinolaryngol 88(3):421–426 [DOI] [PMC free article] [PubMed]
- 20.Cavaliere M, Mottola G, Iemma M. Benign paroxysmal positional vertigo: a study of two maneuvers with and without betahistine. Acta Otolaryngol Ital. 2005;25:107–112. [PMC free article] [PubMed] [Google Scholar]
- 21.Kaur J, Shamanna K. Management of Benign Paroxysmal positional Vertigo: a comparative study between Epleys Manouvre and Betahistine. Int Tinnitus J. 2017;21(1):30–34. doi: 10.5935/0946-5448.20170007. [DOI] [PubMed] [Google Scholar]
- 22.Guneri EA, Kustutan O. The effects of betahistine in addition to epley maneuver in posterior canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2012;146:104–108. doi: 10.1177/0194599811419093. [DOI] [PubMed] [Google Scholar]
- 23.Maslovara S, Soldo SB, Puksec M, Balaban B, Penavic IP. Benign paroxysmal positional vertigo (BPPV): influence of pharmacotherapy and rehabilitation therapy on patients’ recovery rate and life quality. NeuroRehabilitation. 2012;31(4):435–441. doi: 10.3233/NRE-2012-00814. [DOI] [PubMed] [Google Scholar]
- 24.Acar B, Karasen RM, Buran Y Efficacy of medical therapy in the prevention of residual dizziness after successful repositioning maneuvers for Benign Paroxysmal Positional Vertigo (BPPV). BENT.2015;11:117 – 21 [PubMed]


