Abstract
Study Design:
Retrospective study.
Objective:
To investigate the incidence, risk factors, and outcomes of pedicle screw loosening in degenerative lumbar scoliosis (DLS) undergoing long-segment spinal fusion surgery.
Methods:
One hundred and thirty DLS patients who underwent long-segment fusion surgery with at least a 12-month follow-up were studied. The incidence and risk factors of screw loosening were investigated. VAS, SRS-22, and ODI scores were obtained preoperatively and at follow-up.
Results:
One hundred and sixty-eight of 1784 (9.4%) screws showed evidence of loosening in 71 (54.6%) patients. Three patients required revision surgery. Screw loosening rates according to vertebral insertion level were lowest instrumented vertebra (LIV): 45.4%; uppermost instrumented vertebra (UIV):17.7%; one vertebra above the LIV: 0.5%; 2 vertebrae above the LIV: 0.4%. Multiple logistic regression analysis of possible risk factors indicated that preoperative lateral subluxation ≥8 mm (odds ratio [OR]: 2.68, 95% confidence interval [CI]: 1.16-6.20), osteopenia (OR: 5.52, 95% CI: 1.64-18.56), osteoporosis (OR: 8.19, 95% CI: 2.40-27.97), fusion to sacrum (OR: 2.55, 95% CI: 1.12-5.83), postoperative TLK greater than 10° (OR: 2.63, 95% CI: 1.14-6.04) and SVA imbalance (OR: 3.44, 95% CI: 1.17-10.14) were statistically significant. No difference was noted in preoperative, follow-up, and change of VAS, ODI, and SRS-22 scores.
Conclusions:
Screw loosening in DLS underwent long-segment surgery is common and tends to occur in the LIV or UIV. Lateral subluxation ≥8 mm, osteopenia, osteoporosis, fusion to the sacrum, postoperative TLK greater than 10°, and SVA imbalance were the independent influencing factors. Screw loosening can be asymptomatic, while longer-term follow-up is required.
Keywords: degenerative lumbar scoliosis, pedicle screw loosening, risk factors, HRQOL, osteoporosis
Introduction
Degenerative lumbar scoliosis (DLS) is a 3-dimensional spinal deformity with a lumbar Cobb measurement greater than 10°. DLS prevalence is reported variably and ranges from 6% to 68% and increases with age, with higher rates reported among elderly populations.1,2 Xu et al 3 screened the development of DLS in a group of 40 elders in the Chinese Han population, and they found an incidence of 13.3%. Patients with larger curves, significant scoliosis, and/or sagittal imbalance, or severe multilevel stenosis often need correction surgery with long level fusion.1,4
Pedicle screw fixation can provide 3-column fixation of the spine and is widely used to stabilize the thoracolumbar spine. However, pedicle screw loosening was still a common instrumentation-related complication, and the range of loosening rates reported varies from less than 1% to 15% in non-osteoporotic patients, 5 and even up to 60% in osteoporotic patients. 6 Screw loosening is affected by multifactorial. It has been shown that the older age,7,8 osteoporosis,9-11 long-segment fusion,8,9 larger PI, 8 failure to restore LL, 12 and insufficient correction (PI-LL >10°) 13 may lead to pedicle screw loosening. Osteoporosis is associated with reduced pullout strength and insertional torque. Long-segment spinal fixation needed for correction may exert higher mechanical forces. Thus, altered bone quality and multilevel fusion are the most frequently reported contributing factors to screw loosening. 9 It has been reported that DLS has a higher prevalence of osteoporosis than other lumbar degenerative diseases. 14 So the incidence of screw loosening may be high in DLS undergoing long-segment fusion.
Loosening rate data is reported in a vast number of clinical studies.7-12 However, the clinical relevance of screw loosening remains unclear. Tokuhashi et al 15 reported that pedicle screw loosening was highly correlated with pseudarthrosis. No significant difference between with and without screw loosening patients was found in the VAS score and ODI at final follow-up (12 months) after surgery in 62 postmenopausal women with osteoporosis. 16 Several other studies have reported similar results.8,12 In comparison, other studies reported that screw loosening might affect the clinical scores. Bokov et al 9 reported 97 cases of loosened screws out of 253 heterogeneous cases with lumbar degenerative diseases, and 39 of those complained of axial pain with ODI values over 40 and underwent revision surgery. Banno et al 13 compared the ODI values in adult spinal deformity (ASD), and they found baseline ODI values had improved significantly at the 2-year follow-up in the non-loosening group. In contrast, no significant improvement was observed in the loosening group.
Despite several clinical studies that reported screw loosening, the patients included were a heterogeneous group, and they may present with varying degrees and types of curvatures. The clinical and radiographic characteristics of DLS were much more different compared with other adult spinal deformities and lumbar degenerative diseases.13,17 Few reports exist on screw loosening after pedicle screw fixation in degenerative lumbar scoliosis (DLS) patients, and the etiology of screw loosening remains elusive. This study aimed to determine the risk factors of pedicle screw loosening and estimate the effect of screw loosening on health-related quality of life (HRQOL) after long instrumentation in patients with DLS.
Materials and Methods
Patients Population
This study was approved by the Ethical Committee of our institution (IRB00006761-M2018076). We retrospectively reviewed DLS patients who underwent corrective surgery between April 2009 to September 2017 in our hospital. Inclusion criteria were: 1) age ≥40 years; 2) ≥5 vertebrae were fused; 3) minimum 12-month follow-up, and 4) preoperative coronal Cobb ≥ 20°. Patients with other pathologies of scoliosis were excluded, including idiopathic scoliosis, traumatic scoliosis, ankylosing spondylitis, tuberculosis, and tumor. The patients with prior spinal surgery, postoperative infection, or using cement augmented pedicle screws were also excluded. All their medical records, radiological data, and clinical evaluations were retrospectively reviewed.
Demographics and Radiographic Evaluation
Demographic information collected included gender, age, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification preoperatively, and bone mineral density (BMD). Surgery data included operation duration, fusion levels, blood loss, and osteotomy classified by Schwab et al. 18 Each patient underwent a series of complete standing anteroposterior and lateral full-length spine radiographs preoperatively and ≤ 2weeks postoperatively. Preoperative and postoperative radiographic evaluation included Cobb angle, apical vertebral translation (AVT), coronal vertical axis from the central sacrum vertical line (CSVL), thoracic kyphosis (TK, T5-T12), thoracolumbar kyphosis (TLK, T10-L2), lumbar lordosis (LL, L1-S1), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), the difference between pelvic incidence and lumbar lordosis (PI-LL). C7-CSVL distance was measured as the horizontal distance between the center of the C7 plumb line to the CSVL line, and the coronal imbalance was defined as C7-CSVL> 30 mm. The sagittal vertical axis (SVA) was defined as the horizontal offset from the posterosuperior corner of S1 to the vertebral body of C7, and the sagittal imbalance was defined as SVA > 50 mm. 19 Lateral olisthesis (slip of one vertebral endplate on another) was measured at the apex vertebra. The rotation angle of the apical vertebrae was measured by the modified Nash-Moe method. 20 At the follow-up, lumbar radiographs were obtained for all patients. An initial halo sign (radiolucent line around the implant > 1 mm wide) followed by a double halo sign on later radiographs was defined as screw loosening, and CT scan was used only in suspect cases in the planar radiography to minimize radiological exposure and cost (Figure 1).7,8,10,21,22 Two spinal surgeons independently performed the assessments without referring back to previous imagines, and assessments were repeated after 2 weeks with the same diagnostic criteria to measure the intra-observer and inter-observer reproducibility and reliability. The patients were divided into loosening groups and non-loosening groups according to the presence of screw loosening at the final follow-up.
Figure 1.
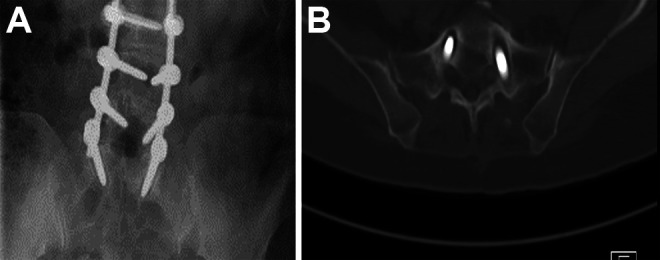
Evidence of screw loosening. Radiolucent areas around screws. Anteroposterior lumbar radiographs (left) and CT (right) of a patient with postoperative screw loosening.
HRQOL
The back and leg pain visual analog scale (VAS) score, Oswestry disability index (ODI), and the Scoliosis Research Society questionnaire-22 were recorded preoperatively and at the final follow-up to evaluate health status. The minimal clinically important difference (MCID) values used for each HRQOL were established by prior studies. Established MCID values were +1.2 for VAS back, +1.6 for VAS leg, −14.96 for ODI, +0.60 for SRS pain, +0.40 for SRS activity, +1.17 for SRS appearance, +0.420 for SRS mental, and +0.53 for SRS-22 subscore.23-26 The MCID criterion was used to assess improvements in outcomes at follow-up.
Statistical Analysis
The data was analyzed using SPSS software (ver. 22.0; SPSS, Inc., Richmond, CA, USA). The descriptive results were expressed as mean and standard deviation (SD) for continuous variables with an approximately normal distribution or median (interquartile range) otherwise. Categorical values were presented as frequency and percentage. Simple comparisons of continuous data between groups were carried out with the Student’s t-test or Mann Whitney U-test, depending on whether the distribution was normal or abnormal, respectively. Categorical variables were compared using the X2 test or Fisher’s exact test. Multiple logistic regression analysis using a stepwise method was performed to identify the independent risk factors of pedicle screw loosening. A significant difference was defined when a P value < 0.5.
Results
A total of 130 patients (26 men and 104 women) aged 40 to 79 years (mean, 62.89 ± 7.08) were included. The mean follow-up period was 34.4 months (range, 12-98 months). Eighty-five patients underwent osteotomy (76 posterior column osteotomies and 9 pedicle subtraction osteotomies). Osteopenia and osteoporosis were found in 53 (40.77%) patients and 52 (40.00%) patients, respectively. Signs of loosening of one or more screws were identified in 71 of 130 (54.6%) patients (62 patients were diagnosed in the planar radiography, and 54 patients’ CT were available, the other 9 suspected cases in the planar radiography were confirmed in the CT). The distribution (9 males and 50 females) and mean age (63.00 ± 6.60) of patients without apparent screw loosening were comparable. Compared with the non-loosening group, the loosening group had a significantly lower T-value (−1.4 ± 1.5 vs.−2.1 ± 1.0, P = .002), a higher proportion of osteoporosis, and fusion to the sacrum. There was no significant difference in BMI, hypertension, diabetes, UIV level, fusion levels, and osteotomy between the 2 groups (Table 1).
Table 1.
Comparison of Patient Characteristics Between the Pedicle Screw Loosening and Non-Loosening Groups.
| Loosening (-) (n = 59) | Loosening (+) (n = 71) | P-value | |
|---|---|---|---|
| Age (years) | 62.98 ± 6.56 (40-76) | 62.82 ± 7.52 (40-79) | .895 |
| Sex (female/male) | 50:9 | 54:17 | .218 |
| BMI (kg/m2) | 25.91 ± 4.31 | 25.68 ± 4.00 | .758 |
| T-value | −1.40 ± 1.48 | −2.12 ± 0.96 | .002 |
| Osteoporosis | 16 (27.12%) | 36 (50.70%) | <.001 |
| Hypertension | 25 (47.46%) | 33 (46.48%) | .639 |
| Diabetes | 10 (16.95%) | 12 (16.90%) | .994 |
| UIV at T10 and above | 15 (25.42%) | 16 (22.54%) | .700 |
| LIV at sacrum | 28 (47.46%) | 50 (70.42%) | .008 |
| Fusion levels | 5.81 ± 1.33 | 6.28 ± 1.98 | .362 |
| Osteotomy | |||
| PCO | 39 (66.10%) | 37 (52.11%) | |
| PSO | 3 (5.08%) | 6 (8.45%) | .150 |
Abbreviations: BMI, indicates body mass index; UIV, uppermost instrumented vertebra; LIV, lowest instrumented vertebra; PCO, posterior column osteotomy; PSO, pedicle subtraction osteotomy.
Boldface values indicate P < .05.
One hundred and sixty-eight of 1784 (9.4%) screws exhibited loosening signs, of which 164 (97.62%) screws had been inserted into the UIV or LIV. The numbers of loose screws according to vertebral insertion level were UIV (n = 260): 46 (17.7%); LIV (n = 260): 118 (45.4%); one vertebra above the LIV (LIV+1) (n = 260): 3(1.15%) and 2 vertebrae below the UIV (UIV+2) (n = 260): 1 (0.38%) (Table 2). In LIV, the screws inserted into S1 demonstrated the highest loosening rate. Three patients (1 in LIV and 2 in UIV) underwent revision surgery due to serious clinical outcomes. The diagnostic criteria of screw loosening showed excellent intra-observer and inter-observer reliability (ICC = 0.96 and 0.92, respectively), indicating that the assessments were reliable.
Table 2.
Screw Loosening Rate by Vertebral Insertion Level.
| Vertebral insertion level | Loosening in screw (%) | Loosening in patients (%) |
|---|---|---|
| Total | 9.42 (168/1784) | 54.62 (71/130) |
| LIV | 45.38 (118/260) | 50.77 (66) |
| L3 | 0.0 (0/4) | 0.0 (0/2) |
| L4 | 0.0 (0/4) | 0.0 (0/2) |
| L5 | 37.50 (36/96) | 41.67 (20/48) |
| S1 | 52.70 (78/148) | 59.46 (44/74) |
| S2AI | 50.00 (4/8) | 50.00 (2/4) |
| UIV | 17.69 (46/260) | 19.23 (25) |
| LIV+1 | 1.15 (3/260) | 1.54 (2) |
| LIV+2 | 0.38 (1/260) | 0.77 (1) |
Abbreviations: UIV, indicates uppermost instrumented vertebra; LIV, lowest instrumented vertebra; LIV+1, one vertebra above the LIV (LIV+1); LIV+2, 2 vertebrae below the UIV.
The comparison of preoperative and postoperative radiographical parameters between the loosening and non-loosening groups was in Table 3. The screw loosening group had a significantly higher rate of lateral subluxation larger than 8 mm (54.90% vs. 33.93%, P = .016), larger postoperative TLK, a higher proportion of postoperative TLK ≥10 (57.75% vs. 38.98%, P = .033); and larger postoperative SVA, a higher preoperative, and postoperative sagittal imbalance (SVA more than 50 mm). The preoperative, postoperative, and change in Cobb, AVT, CSVL, TK, LL, PT, SS, and PI-LL showed no significant differences between the 2 groups (P > .05).
Table 3.
Comparison of Radiographical Parameters Between the Loosening and Non-Loosening Groups.
| Loosening (-) (n = 59) | Loosening (+) (n = 71) | P-value | |
|---|---|---|---|
| Cobb(°) | |||
| Preoperative | 29.19 ± 8.27 | 31.83 ± 12.56 | .153 |
| Postoperative | 11.04 ± 6.56 | 13.03 ± 7.33 | .104 |
| Change in Cobb | 18.31 ± 6.93 | 19.04 ± 9.45 | .617 |
| AVT (mm) | |||
| Preoperative | 27.49 ± 13.34 | 27.60 ± 14.00 | .964 |
| Postoperative | 14.94 ± 7.79 | 17.10 ± 10.71 | .193 |
| Change in AVT | 12.55 ± 9.21 | 10.72 ± 11.11 | .319 |
| CSVL (mm) | |||
| Preoperative a | 12.66 [11.53, 22.38] | 14.19 [14.53, 21.11] | .189 |
| Postoperative | 20.41 ± 17.72 | 21.01 ± 13.50 | .831 |
| Change in CSVL | 19.92 ± 19.02 | 19.92 ± 17.15 | .999 |
| Apex vertebrae rotation (Nash-Moe), I: II: III: IV | 12:25:20:2 | 10:33:23:5 | .659 |
| Lateral olisthesis (mm) | 6.90 [6.74,8.67] | 8.36 [7.79,9.47] | .094 |
| Lateral olisthesis >8 mm (n) | 20 (33.90%) | 39 (54.93%) | .016 |
| TK(°) | |||
| Preoperative | 18.34 ± 14.61 | 19.81 ± 14.89 | .574 |
| Postoperative | 22.58 ± 10.03 | 22.25 ± 11.51 | .865 |
| TLK(°) | |||
| Preoperative | 12.20 [7.78, 17.86] | 14.10 [11.33, 20.41] | .307 |
| Postoperative | 7.50 ± 9.94 | 11.17 ± 10.09 | .042 |
| Postop TLK ≥10°(n) | 23 (38.98%) | 41 (57.75%) | .033 |
| Change in TLK | −5.80 ± 15.48 | −4.75 ± 17.56 | .722 |
| LL(°) | |||
| Preoperative | 29.34 ± 19.41 | 26.87 ± 17.33 | .445 |
| Postoperative | 40.56 ± 11.89 | 38.30 ± 11.80 | .281 |
| Change in LL | 11.22 ± 13.13 | 11.44 ± 13.77 | .929 |
| PT(°) | |||
| Preoperative | 25.24 ± 9.44 | 22.87 ± 10.05 | .173 |
| Postoperative | 20.04 ± 8.85 | 18.17 ± 9.46 | .249 |
| SS(°) | |||
| Preoperative | 25.79 ± 11.54 | 25.26 ± 10.24 | .782 |
| Postoperative | 30.95 ± 9.14 | 30.46 ± 8.67 | .752 |
| PI(°) | 51.03 ± 11.77 | 48.28 ± 10.63 | .167 |
| PI-LL(°) | |||
| Preoperative | 21.69 ± 16.47 | 21.08 ± 16.56 | .835 |
| Postoperative | 10.43 ± 10.70 | 10.32 ± 14.10 | .960 |
| SVA(mm) | |||
| Preoperative | 49.81 ± 42.08 | 59.17 ± 47.89 | .245 |
| Preop sagittal imbalance | 23 (38.98%) | 41 (57.75%) | .033 |
| Postoperative | 30.02 ± 24.19 | 42.26 ± 37.54 | .027 |
| Postop sagittal imbalance | 7 (11.86%) | 21 (29.58%) | .014 |
| Change in SVA | 44.86 ± 37.11 | 54.51 ± 41.18 | .170 |
Abbreviations: AVT, indicates apical vertebral translation; CVA, coronal vertical axis; TK, thoracic kyphosis; TLK, thoracolumbar kyphosis; LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope; SAV, sagittal vertical axis.
a Not meet the normal distribution, expressed as the median [95% confidence interval].
Boldface values indicate P < .05.
Table 4 shows the multivariate logistic regression analysis of possible risk factors for radiographic screw loosening. The analysis revealed that preoperative lateral subluxation larger than 8 mm (odds ratio [OR]: 2.68, 95%confidence interval [CI]: 1.16-6.20), osteopenia (OR: 5.52, 95% CI: 1.64-18.56), osteoporosis (OR: 8.19, 95% CI: 2.40-27.97), fusion to sacrum (OR: 2.55, 95% CI: 1.12-5.83), postoperative TLK lager than 10° (OR: 2.63, 95% CI: 1.14-6.04) and postoperative SVA imbalance (OR: 3.44, 95% CI: 1.17-10.14) were significantly associated with an increased OR for radiographic loosening.
Table 4.
Multivariate Analysis of Possible Risk Factors for Radiographic Loosening.
| Risk factors | Logistic regression | ||
|---|---|---|---|
| P | Odds Ratio | 95% CI | |
| Lateral listhesis ≥8 mm |
.021 | 2.68 | 1.16-6.20 |
| Bone mass normal | Reference | ||
| Osteopenia | .006 | 5.52 | 1.64-18.56 |
| Osteoporosis | .001 | 8.19 | 2.40-27.97 |
| Fused to sacrum | .027 | 2.55 | 1.12-5.83 |
| Post-op TLK≥10° | .023 | 2.63 | 1.14-6.04 |
| Post-op SVA imbalance | .025 | 3.44 | 1.17-10.14 |
Abbreviations: CI, indicates confidence interval; TLK, thoracolumbar kyphosis; SAV, sagittal vertical axis.
Bold indicates P < .05.
The overall clinical outcomes, measured by VAS (back and leg pain scores), SRS-22, and ODI, were significantly improved after surgery at last follow-up compared with status preoperatively (P < .001). Furthermore, patients had significant improvement in VAS back, VAS leg, SRS-22, and ODI scores regardless of whether screw loosening was present or absent. There were no significant differences between the 2 groups in preoperative and follow-up HRQOL scores, the change of HRQOL, and the percentage of patients who reached the MCID (Table 5).
Table 5.
Comparisons of the HRQOL Outcome Data Between the Loosening and Non-Loosening Groups.
| HRQOL | Loosening (-) (n = 59) | Loosening (+) (n = 71) | P-value |
|---|---|---|---|
| Pre-op VAS back | 6.56 ± 1.59 | 6.25 ± 1.90 | .328 |
| Pre-op VAS leg | 5.25 ± 2.43 | 5.94 ± 2.01 | .079 |
| Pre-op ODI | 55.71 ± 15.85 | 60.17 ± 14.88 | .101 |
| Pre-op SRS activity | 2.29 ± 0.58 | 2.35 ± 0.67 | .583 |
| Pre-op SRS pain | 2.40 ± 0.82 | 2.42 ± 0.90 | .880 |
| Pre-op SRS appearance | 2.15 ± 0.55 | 2.10 ± 0.51 | .585 |
| Pre-op SRS mental | 2.45 ± 0.57 | 2.52 ± 0.65 | .551 |
| Pre-op SRS subtotal | 2.32 ± 0.47 | 2.34 ± 0.54 | .784 |
| FU VAS back | 2.76 ± 1.92 | 3.13 ± 2.18 | .320 |
| FU VAS leg | 2.32 ± 2.05 | 2.25 ± 1.96 | .194 |
| FU ODI | 23.21 ± 17.74 | 29.10 ± 19.09 | .055 |
| FU SRS activity | 3.67 ± 0.69 | 3.45 ± 0.71 | .084 |
| FU SRS pain | 4.14 ± 0.69 | 3.92 ± 0.94 | .127 |
| FU SRS appearance | 4.08 ± 0.55 | 3.92 ± 0.81 | .204 |
| FU SRS mental | 4.10 ± 0.63 | 3.94 ± 0.68 | .175 |
| FU SRS subtotal | 4.00 ± 0.54 | 3.81 ± 0.65 | .074 |
| FU SRS satisfaction | 4.37 ± 0.67 | 4.15 ± 0.83 | .095 |
| Δ VAS back | 3.80 ± 2.12 | 3.13 ± 2.56 | .219 |
| Δ VAS leg | 2.93 ± 2.86 | 3.69 ± 2.68 | .094 |
| Δ ODI | 32.50 ± 21.06 | 31.07 ± 20.00 | .692 |
| Δ SRS activity | 1.38 ± 0.85 | 1.10 ± 0,88 | .136 |
| Δ SRS pain | 1.74 ± 1.03 | 1.50 ± 1.16 | .383 |
| Δ SRS appearance | 1.93 ± 0.74 | 1.82 ± 0.94 | .776 |
| Δ SRS mental | 1.65 ± 0.88 | 1.43 ± 0.87 | .074 |
| Δ SRS subtotal | 1.68 ± 0.69 | 1.46 ± 0.79 | .110 |
| Δ VAS back reached MCID (%) | 86.44% | 73.24% | .065 |
| Δ VAS leg reached MCID (%) | 69.49% | 81.69% | .104 |
| Δ ODI reached MCID (%) | 81.36% | 77.46% | .586 |
| Δ SRS activity reached MCID (%) | 84.75% | 78.87% | .390 |
| Δ SRS pain reached MCID (%) | 86.44% | 78.87% | .260 |
| Δ SRS appearance reached MCID (%) | 84.75% | 76.06% | .218 |
| Δ SRS mental reached MCID (%) | 94.92% | 88.73% | .207 |
| Δ SRS subtotal reached MCID (%) | 88.73% | 94.92% | .309 |
Abbreviations: VAS, indicates Visual Analog Scale; ODI, Oswestry Disability Index; SRS, Scoliosis Research Society; FU, follow-up; MCID, minimal clinically important difference.
Discussion
This study analyzed 1784 screws used in long-segment correction surgery in 130 patients with DLS. In a mean follow-up period of 34.4 months, 168 screws (9.4%) in 71 (54.6%) patients became loose. Revision surgery was performed in 3 patients, while most of the patients with loosed screws were asymptomatic and identified radiographically during regular follow-up. The clinical outcomes were equally improved regardless of screw loosening. Multivariate analysis revealed that preoperative lateral subluxation larger than 8 mm, osteopenia and osteoporosis, fusion to the sacrum, postoperative TLK lager than 10°, and postoperative SVA imbalance were independent factors affecting screw loosening.
Pedicle screw fixation was widely used in spine surgery for numbers of indications, such as degenerative disease, trauma, and deformity. It reduced the range of motion of the stabilized spine, increased the fusion rate, and was generally considered to be safe with relatively low complication rate associated with the device,27,28 however, one of the common complications widely reported in the literature was screw loosening. 5 Previous studies showed a vast range of screw loosening rates, ranged from less than 1% to 15% in patients with non-osteoporosis and much higher in osteoporosis subjects. 5 The primary diseases, length of fusion, bone mass, the follow-up duration, and the conventions used for the radiological assessment might all have an effect. The pedicle screw loosening rate was 54.6% in patients at final follow-up in the present study, showing a high loosening rate in corrective surgery with long-segment fusion in DLS. This could be mainly due to the patients included all undergoing long-segment instrumentation and high proportion combined with osteopenia or osteoporosis, and the latter was also identified as an independent risk factor in this study.
Fusion length was associated with the rates of loosening, and long-segment fusion increased the loosening rate. Kim et al 8 investigated the rate of S1 screw loosening in degenerative lumbar disease and concluded that the loosening rates according to the number of fusion levels were 2.0%, 26.8%, 50.0%, and 50.0% in 1, 2, 3, and 4 levels, and patients with 3 or 4 levels fusion had a significantly higher rate of S1 screw loosening comparing to 1 level fusion (P < .05). Zou et al 17 reported that the loosening rate was 53.3% and 78.8% for 3 and 4 levels. Tokuhashi et al 15 also reported similar results, and they found that the screw loosening rate was only 7.4% in patients with 1-level fused, while it was 42.9% in patients with 4levels or move levels fused at ≥3years follow-up. The mean vertebral levels fused in this study were 6.07 ± 1.73, and the screw loosening rate was 54.6%, which was close to the previous studies.
Our study also revealed that the rate of screw loosening in the UIV and LIV was higher than that in other levels, 19.2% and 50.8%, respectively. Banno et al 22 reported 20 of 63(31.7%) patients with ASD had screw loosening at a 2-year follow-up, of which 15 occurred in UIV and 8 in LIV. Uehara et al 29 showed that 83.7% loosening occurred in UIV and LIV, of which the rate was 9.6% and 5.4%, respectively, and proximity to UIV or LIV tended to increase screw loosening rate.
Screw loosening could be exacerbated by osteopenic or osteoporotic bone, which has a markedly lower capability to sustain stresses without failure. 5 Kim et al 8 also observed that comparing with the non-loosening group, the loosening group had a significantly lower T-value. It was confirmed that bone density was critical to pedicle screw pullout strength and stability in cadaver samples. 11 Recently, lower Hounsfield unit (HU) values measured on preoperative CT were reported significantly correlated with a higher risk of screw loosening.17,21 A biomechanical study had observed that screw insertional torque was significantly correlated with spine-areal BMD, total hip-area BMD, femoral neck-area BMD, and was most strongly associated with pedicle screw-BMD. 30
Fusion to S1 is also a significant contributor to screw loosening. The loosening rate of S1 has been reported about 15.6% to 46.5%, 31 which of the lumbar spine was about 10% to 20%. 7 Compared with the lumbar pedicle, the diameter of the sacrum pedicle is much larger, and the length is much shorter, which leads to a lack of cortical fixation of the screw-bone interface. Moreover, the sacrum was composed primarily of cancelous bone. 32 These anatomical factors may account for the high rate of screw loosening in S1. Although the proportion of S1 screw loosening was high, we did not find that its loosening impacted the quality of life of patients. Only 4 patients in the study underwent iliac fixation. Instrumentation down to the pelvic ring provides increased biomechanical strength to the lumbosacral construct but increases surgical trauma and risk and increases treatment cost. We usually used it for deformities requiring 3-column osteotomies in the lumbar spine, high-grade spondylolisthesis, sacrectomies, severe osteoporosis, revisions of previous fusions, and other cases.
Preoperative lateral subluxation larger than 8 mm, postoperative TLK larger than 10°, and postoperative SVA imbalance were independent factors associated with screw loosening in this study. Lateral subluxation is significantly associated with DLS curve progression and reoperation.20,33 Note that lateral subluxation is a 2-dimensional representation of a triaxial deformity consisting of axial rotation and lateral translation toward the convexity of the curve. A larger lateral subluxation means a severer deformity, and the mechanical stress of the vertebral body to the lateral side of the screw is also greater after correction surgery, but this needs to be further verified by biomechanical tests. TLK is the angle between the upper endplate of T10 and the lower endplate of L2, which is the junction area between the thoracic and lumbar vertebrae and the area that transfers the force from the thoracolumbar to the lumbar vertebrae, and greater TLK might result in a sagittal imbalance. In patients with sagittal malalignment, the longer lever arm distance from the gravity line yields a higher bending moment, affecting the distal end of the construct. 34 Patients with lumbar degenerative diseases are characterized by anterior sagittal imbalance. Normally, the spine keeps sagittal balance with a compensatory mechanism by reducing lumbar lordosis. 35 However, after lumbar fusion and fixation, the stress may increase on the paraspinal muscles and the fixation device of the posterior column, leading to increased stress on the screw and bone interface and further screw loosening.
Although there was a significant difference in the incidence of loosening in this study, no significant difference was observed in the final follow-up and the change in VAS score, SRS-22 scores, and ODI between the 2 groups. Although we did not evaluate bony union in our study, pedicle screw loosening may theoretically negatively influence bone fusion. However, successful bone fusion has previously been shown to be unrelated to the clinical outcome. 36 Previous studies have suggested that pedicle screw loosening itself not be a determinant of clinical outcomes.10,16 However, 3 patients underwent revision surgery due to severe clinical outcomes in our study. The screw loosening may exacerbate clinical symptoms, contributing to poor prognosis in the long-term period. Thus, we should continue the research to obtain long-period results.
The present study had some limitations. Firstly, it is a relatively small-sized retrospective study with a restricted number of patients. Secondly, the length and diameter of the screws were not analyzed. Moreover, the actual time occurrence of the screw loosening was earlier than that caught on imaging studies due to clinical silence. The real effect on clinical outcomes can only be determined by longer follow-up.
Conclusion
Pedicle screw loosening was not uncommon (9.4% of screws in 54.6% patients) after long-level fusion for DLS patients, which primarily occurred in the UIV or LIV. Preoperative lateral subluxation ≥8 mm, osteoporosis and osteopenia, fusion to sacrum, and postoperative TLK≥10° and SVA imbalance were significantly associated with screw loosening. Although there were few adverse effects on clinical outcomes, long-term follow-up is required to examine the impact of loosened screws.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Authors’ Note: Zhongqiang Chen, MD and Weishi Li, MD are authors contributed equally to this work and should be considered co-corresponding authors. The corresponding author declares the absence of any conflict of interest regarding the submitted manuscript. The funders had no role in study design, data collection, analysis, or decision to publish or prepare the manuscript. We had full access to all of the study data and took responsibility for data integrity and data analysis accuracy. The data is available on request from the corresponding author. Written informed consent was obtained from all patients when they were admitted to the hospital, in which the patients were informed that their data might be used for scientific research in the future under the premise that patient privacy is strictly protected. This study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2018076). All procedures performed in this study involving human participants followed the institutional and/or national research committee’s ethical standards and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Thus, informed consent was exempt from the requirement when we use the data in this study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Zhongqiang Chen, MD  https://orcid.org/0000-0002-6595-1910
https://orcid.org/0000-0002-6595-1910
References
- 1.Chen PG, Daubs MD, Berven S, et al. Surgery for degenerative lumbar scoliosis: the development of appropriateness criteria. Spine. 2016;41(10):910–918. [DOI] [PubMed] [Google Scholar]
- 2.Koerner JD, Reitman CA, Arnold PM, Rihn J. Degenerative lumbar scoliosis. JBJS Rev. 2015;3(4):01874474–201504000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Xu L, Sun X, Huang S, et al. Degenerative lumbar scoliosis in Chinese Han population: prevalence and relationship to age, gender, bone mineral density, and body mass index. Eur Spine J. 2013;22(6):1326–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glassman SD, Berven SH, Shaffrey CI, Mummaneni PV, Polly DW. Commentary: appropriate use criteria for lumbar degenerative scoliosis: developing evidence-based guidance for complex treatment decisions. Neurosurgery. 2017;80(3):E205–e212. [DOI] [PubMed] [Google Scholar]
- 5.Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24(5):1005–1016. [DOI] [PubMed] [Google Scholar]
- 6.El Saman A, Meier S, Sander A, Kelm A, Marzi I, Laurer H. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur J Trauma Emerg Surg. 2013;39(5):455–460. [DOI] [PubMed] [Google Scholar]
- 7.Wu JC, Huang WC, Tsai HW, et al. Pedicle screw loosening in dynamic stabilization: incidence, risk, and outcome in 126 patients. Neurosurg Focus. 2011;31(4):E9. [DOI] [PubMed] [Google Scholar]
- 8.Kim JB, Park SW, Lee YS, Nam TK, Park YS, Kim YB. The effects of spinopelvic parameters and paraspinal muscle degeneration on S1 screw loosening. J Korean Neurosurg Soc. 2015;58(4):357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bokov A, Bulkin A, Aleynik A, Kutlaeva M, Mlyavykh S.Pedicle screws loosening in patients with degenerative diseases of the lumbar spine: potential risk factors and relative contribution. Global Spine J. 2019;9(1):55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim JW, Park SW, Kim YB, Ko MJ. The effect of postoperative use of teriparatide reducing screw loosening in osteoporotic patients. J Korean Neurosurg Soc. 2018;61(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiser L, Huber G, Sellenschloh K, et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J. 2017;26(11):2891–2897. [DOI] [PubMed] [Google Scholar]
- 12.Kuo CH, Chang PY, Tu TH, et al. The effect of lumbar lordosis on screw loosening in dynesys dynamic stabilization: four-year follow-up with computed tomography. Biomed Res Int. 2015;2015:152435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Banno T, Hasegawa T, Yamato Y, et al. Prevalence and risk factors of iliac screw loosening after adult spinal deformity surgery. Spine. 2017;42(17):E1024–E1030. [DOI] [PubMed] [Google Scholar]
- 14.Zou D, Jiang S, Zhou S, et al. Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: a combination of DXA and hounsfield units. Spine. 2020;45(7):E406–E410. [DOI] [PubMed] [Google Scholar]
- 15.Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008;33(8):903–908. [DOI] [PubMed] [Google Scholar]
- 16.Ohtori S, Inoue G, Orita S, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 2013;38(8):E487–E492. [DOI] [PubMed] [Google Scholar]
- 17.Zou D, Muheremu A, Sun Z, Zhong W, Jiang S, Li W. Computed tomography hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine. 2020:1–6. [DOI] [PubMed] [Google Scholar]
- 18.Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014;74(1):112–120. [DOI] [PubMed] [Google Scholar]
- 19.Yuan L, Zeng Y, Chen Z, Li W, Zhang X, Ni J. Risk factors associated with failure to reach minimal clinically important difference after correction surgery in patients with degenerative lumbar scoliosis. Spine. 2020;45(24):E1669–E1676. [DOI] [PubMed] [Google Scholar]
- 20.Faraj SS, Holewijn RM, van Hooff ML, de Kleuver M, Pellise F, Haanstra TM. De novo degenerative lumbar scoliosis: a systematic review of prognostic factors for curve progression. Eur Spine J. 2016;25(8):2347–2358. [DOI] [PubMed] [Google Scholar]
- 21.Sakai Y, Takenaka S, Matsuo Y, et al. Hounsfield unit of screw trajectory as a predictor of pedicle screw loosening after single level lumbar interbody fusion. J Orthop Sci. 2018;23(5):734–738. [DOI] [PubMed] [Google Scholar]
- 22.Banno T, Hasegawa T, Yamato Y, et al. Assessment of the change in alignment of fixed segment after adult spinal deformity surgery. Spine (Phila Pa 1976). 2018;43(4):262–269. [DOI] [PubMed] [Google Scholar]
- 23.Carreon LY, Kelly MP, Crawford CH, III, et al. SRS-22R minimum clinically important difference and substantial clinical benefit after adult lumbar scoliosis surgery. Spine Deform. 2018;6(1):79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuksel S, Ayhan S, Nabiyev V, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J. 2019;19(1):71–78. [DOI] [PubMed] [Google Scholar]
- 25.Crawford CH, Glassman SD, Bridwell KH, Berven SH, Carreon LY. Minimum clinically important difference (MCID) in SRS-22R appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine J. 2014;14(suppl 11):S19. [DOI] [PubMed] [Google Scholar]
- 26.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J. 2008;8(6):968–974. [DOI] [PubMed] [Google Scholar]
- 27.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6(1):2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br. 2010;92(8):1061–1065. [DOI] [PubMed] [Google Scholar]
- 29.Uehara M, Takahashi J, Ikegami S, et al. Pedicle screw loosening after posterior spinal fusion for adolescent idiopathic scoliosis in upper and lower instrumented vertebrae having major perforation. Spine. 2017;42(24):1895–1900. [DOI] [PubMed] [Google Scholar]
- 30.Ishikawa K, Toyone T, Shirahata T, et al. A Novel method for the prediction of the pedicle screw stability: regional bone mineral density around the screw. Clin Spine Surg. 2018;31(9):E473–E480. [DOI] [PubMed] [Google Scholar]
- 31.Finger T, Bayerl S, Onken J, Czabanka M, Woitzik J, Vajkoczy P. Sacropelvic fixation versus fusion to the sacrum for spondylodesis in multilevel degenerative spine disease. Eur Spine J. 2014;23(5):1013–1020. [DOI] [PubMed] [Google Scholar]
- 32.McLachlin SD, Al Saleh K, Gurr KR, Bailey SI, Bailey CS, Dunning CE. Comparative assessment of sacral screw loosening augmented with PMMA versus a calcium triglyceride bone cement. Spine. 2011;36(11):E699–704. [DOI] [PubMed] [Google Scholar]
- 33.Kato M, Namikawa T, Matsumura A, Konishi S, Nakamura H. Radiographic risk factors of reoperation following minimally invasive decompression for lumbar canal stenosis associated with degenerative scoliosis and spondylolisthesis. Global Spine J. 2017;7(6):498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim YH, Ha KY, Chang DG, et al. Relationship between iliac screw loosening and proximal junctional kyphosis after long thoracolumbar instrumented fusion for adult spinal deformity. Eur Spine J. 2020;29(6):1371–1378. [DOI] [PubMed] [Google Scholar]
- 35.Barrey C, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013;6(suppl 6):S834–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997;22(24):2807–2812. [DOI] [PubMed] [Google Scholar]


