Abstract
Objective:
Evaluate clinical improvement as measured by patient-reported outcomes (PROs) during the 1 to 2-year interval.
Study Design:
Retrospective Cohort.
Methods:
A single-institution registry of ASD patients undergoing surgery was queried for patients with ≥6 level fusions. Demographics and radiographic variables were collected. PROs collected were the ODI and SRS-22r scores at: preoperative, 1-year and 2-years. Outcome measures of clinical improvement during the 1-2 year time interval were: 1) group medians, 2) percent minimum clinically important difference (MCID), and 3) percent minimal symptom scale (MSS)(ODI < 20 or SRS-pain + function >8). Wilcoxon rank-sum tests, chi-squared tests, Kruskal-Wallis tests, and logistic regression were performed.
Results:
157 patients undergoing ASD surgery with minimum of 1-year follow-up were included. Mean age was 53.2 and mean instrumented levels was 13.1. Preoperative alignment was: Neutral Alignment (NA) 49%, Coronal Malalignment (CM) 17%, Sagittal Malalignment (SM 17%), and Combined Coronal/Sagittal Malalignment (CCSM) 18%. Preoperative to 1-year, and preoperative to 2-years, all ODI/SRS-22r significantly improved (P < .001). In all patients, the only significant improvement in PROs between 1-and 2-year postoperative were those reaching ODI MCID (69% 1-year vs. 84% 2-years; P < .001). Subgroup analysis: ≥55 years had an improved median ODI (18 vs. 8; P = .047) and an improved percent achieving ODI MCID (73% vs. 84%, P = .048). CCSM patients experienced significant improvement in SRS-appearance score (75% vs. 100%; P = .050), along with those with severe preoperative SM >7.5 cm (73% vs. 100%; P = .032).
Conclusions:
Most ASD patients experience the majority of PRO improvement by 1-year postoperative. However, subsets of patients that may continue to improve up to 2-years postoperative include patients ≥55 years, combined coronal/sagittal malalignment, and those with severe sagittal malalignment ≥7.5 cm.
Keywords: adult spine deformity, patient reported outcomes, postoperative outcomes, minimum clinically important difference, spine surgery
Introduction
Adult spinal deformity (ASD) has a prevalence of 3% to 50% depending on age group, with some reporting as high as 68% in individuals older than 65 years.1,2 Though not all patients with ASD are symptomatic, many suffer from pain, disability, aesthetic, or mental health problems. 2 Patients with severe thoracolumbar deformity have a health state comparable to patients with uncontrolled diabetes, rheumatoid arthritis, and loss of limb. 3 Surgical intervention can significantly help these patients and improve their quality of life.4,5
Despite opportunity for significant improvement after ASD surgery, morbidity can be high, and the recovery process is long and arduous even after a perfectly executed ASD operation.6,7 Patient reported outcomes (PROs) often decrease during the early recovery period, yet clinical improvement is seen from 3-months to 1-year postoperative.8-10 In ASD patients with preoperative neurological deficits, motor scores show incremental improvement at discharge, 6-week, and 6-month in 52%, 67%, and 83% of patients, respectively. 11 However, little is known how much, or if any improvement takes place beyond the 1-year period. Moreover, the recovery dynamics in certain patient populations or after different operative approaches is an area still under investigation. Studies have shown that elderly and frail patients may improve their PROs more than younger patients up to 2-years postoperative.10,12 Understanding the exact time window of improvement after ASD surgery can help guide pre- and postoperative recovery expectations for patients and surgeons. While several studies evaluate clinical improvement at 1 and 2-years compared to preoperative, few have scrutinized if continued improvement takes place during the 1 to 2-year time period.
Given our incomplete understanding of the recovery process after ASD surgery, we attempted to further study the duration of improvement after ASD surgery. In a cohort of ASD patients undergoing corrective surgery, we sought to evaluate clinical improvement as measured by PROs during the 1- to 2-year interval.
Methods
Study Design
The current study was a retrospective cohort study based on prospectively collected data from a single institution consisting of 2 spine deformity surgeons (LGL/RAL). Following institutional review board approval (#AAAR6504), data was collected on all ASD patients undergoing ASD surgery between 06/01/2015-12/31/2019. No funding was received for this study. A HIPAA form B, waiver for informed consent, was obtained.
Patient Population
Preoperative enrollment criteria were similar to prior studies of ASD patients.13,14 The inclusion criteria were: age ≥18 years undergoing ≥6 level instrumented fusion with at least 1 of the following radiographic criteria (Cobb angle > 30°, SVA > 5 cm, coronal vertical axis (CVA) > 3 cm, pelvic tilt (PT) of > 25°, or thoracic kyphosis (TK) > 60°). All patients underwent a standing full-body or full-spine low dose Stereoradiograph (EOS Imaging, Paris, France) prior to surgery.
Independent Variables
Demographic and operative variables were collected, including age, sex, body mass index (BMI), diagnosis, primary vs. revision surgery, preoperative alignment status, total instrumented levels (TIL), 3 column osteotomy (3CO), operative time, estimated blood loss (EBL), length of stay, complications, and reoperations. Preoperative x-rays were evaluated, and both the coronal vertical axis (CVA) and sagittal vertical axis (SVA), both continuous variables measured in centimeters (cm), were obtained. The CVA was obtained by subtracting the coronal C7-plumb-line (C7PL-a vertical line dropped from the middle of the C7 vertebral body) distance, from the central sacral vertical line (CSVL—a vertical line that passes through the center of the sacrum). 15 Similarly, the SVA is the distance from the sagittal C7PL, a vertical line drawn from the middle of the C7 body, and the posterior superior aspect of the S1 vertebral body. 15 Though CVA to the left is considered negative and to the right is positive, absolute values were used given the lack of clinical difference between left and right. Patients were then then broken down into the following 4 groups based on preoperative alignment: 1) Neutral alignment (NA): CVA <3 cm & SVA < 5 cm; 2) Coronal malalignment only (CM): CVA >3 cm; 3) Sagittal malalignment only (SM): SVA >5 cm; and 4) Coronal and sagittal malalignment (CCSM): both CVA >3 cm & SVA >5 cm. Additional radiographic information was obtained including max coronal Cobb angle, L4 tilt, and L5 tilt.
Patient-Reported Outcomes
The 2 PRO variables used were: 1) Oswestry Disability Index (ODI) version 2.1a,16,17 and 2) Scoliosis Research Society (SRS-22r) Instrument. 18 The ODI gives a single score, with higher values corresponding to worse function. The SRS-22r gives a total score and several sub-domains rated 1-5, with lower values corresponding to worse function. Determined a-priori based on clinical relevance, the SRS-22r subdomains included were: function, appearance, mental health, and pain.
With each PRO, the 3 outcome measures of clinical improvement during the 1-2 year time interval were: 1) group medians, 2) percent minimum clinically important difference (MCID), and 3) percent with minimal symptom scale (MSS) (ODI < 20 or SRS-pain + function >8).
Three time points of each PRO were collected: baseline, 1-year, and 2-years postoperative. Though outside the focus of this manuscript, changes in PROs were assessed from preoperative to both postoperative time points to evaluate the impact of surgery. The a-priori objective was to assess changes during the 1-year to 2-year postoperative time period. Thus, the majority of the analysis included values from only these time points.
Sub-Group Analysis
After the whole cohort was analyzed, specific sub-groups were assessed a-priori to determine specific populations more or less predisposed to improvement during 1- to 2-year postoperative time period. These sub-groups were the following:
Age: dichotomized to patients >55-years-old
Global alignment(3 groups): CM (CVA >3 cm & SVA < 5 cm; SM (SVA >5 cm & CVA < 3 cm); CCSM (both CVA CVA >3 cm & SVA >5 cm.
Deformity severity(3 groups) CVA >5 cm, SVA >7.5 cm, max Cobb angle >60°
Invasiveness of surgery(2 variables): TIL and 3CO.
Complication status(2 variables): Presence of any postoperative complication or revision spine surgery.
Statistical Analysis
Descriptive statistics were used to summarize patient demographics and radiographic data. Categorical data was presented as frequencies and percentages, whereas continuous data was present with mean and standard deviations (SD). The PROs used were determined to not be normally distributed based on the Shapiro-Wilk test (P < .05), and thus non-parametric testing was used. To assess changes from preoperative to postoperative, Wilcoxon-rank-sum tests were used to compare groups at 1-year and 2-years postoperative to preoperative. Kruskal-Wallis tests were used to compare PROs across 4 groups based on alignment (NA, CM, SM, CCSM) at each time point. To determine differences between the 1- and 2-year time interval, Wilcoxon-rank-sum tests were used for continuous data (raw PRO scores), whereas Chi-squared proportion tests were used for count data (percent achieving MCID and MSS). MCID threshold values were set in accordance with prior studies: −12.8 for ODI, +0.375 for SRS-function, +0.800 for SRS-appearance, and +0.587 for SRS-pain.19-23 MCID values for SRS-mental health were not used due to limited prior use. Values for MSS of ODI < 20 were used based on prior studies, and the MSS values of SRS-pain + function >8 were chosen based on similar methodology. Statistical significance was set at an alpha level of ≤ 0.05. Due to a potentially large number of tables, only significant results of each sub-group analysis are summarized. All statistical analyzes were performed in STATA version 14 (StataCorp LP, College Station, Texas).
Results
Demographics
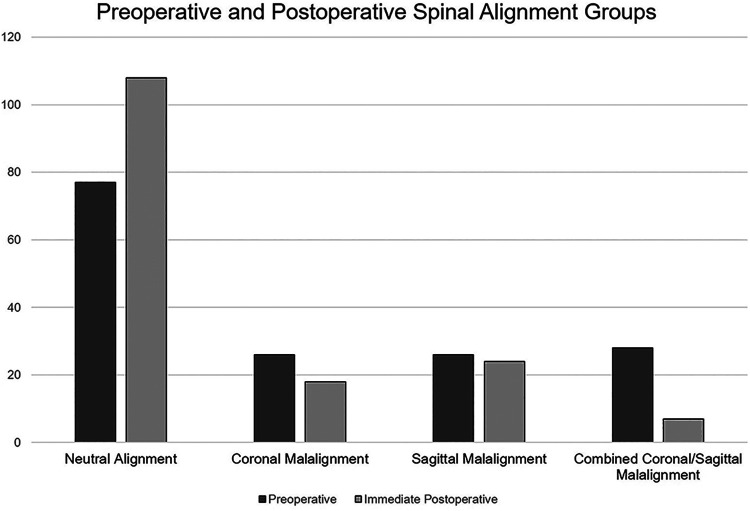
A total 157 patients undergoing ASD surgery had 1-year follow-up, and 88 had 2-year follow-up with appropriate PROs. Mean age was 50.9 years and 67% were female (Table 1). Sixty percent (94/157) of patients presented as revision cases, having undergone previous spinal fusion surgery, and the average TIL for the current deformity surgery was 13.4. Furthermore, though mean SVA was 3.1, a wide range of positive and negative values was seen (−8.8 to 24.8). Breakdown of each deformity into each category is seen at preoperative and immediate postoperative: NA, CM, SM, and CCSM (Figure 1). Though different sample sizes were used for the 1-year and 2-year samples, both groups were similar in all demographics and operative variables (Table 2).
Table 1.
Demographic and Operative Variables.
| Variable | Value |
|---|---|
| Age, mean ± SD | 50.9 ± 17.5 |
| Female, n (%) | 105 (67%) |
| ASA | |
| 1 / 2 / 3 | 15 (10%) / 97 (62%) / 45 (28%) |
| BMI, mean ± SD | 25.6 ± 5.8 |
| Depression, n (%) | 31 (20%) |
| Diagnosis, n (%) | |
| AdIS | 82 (52%) |
| Degenerative | 75 (48%) |
| Revision, n (%) | 94 (60%) |
| Preop SVA (cm), mean ± SD (range) | 3.6 ± 6.4 ( −8.8, 24.8) |
| Preop CVA (cm), mean ± SD (range) | 2.8 ± 2.6 (0.1, 19.8) |
| Max Cobb (°), mean ± SD (range) | 42.6 ± 26.3 (1.2, 131.7) |
| TIL | 13.4 ± 4.0 (6-25) |
| 3CO | 22 (14%) |
| Operative time, mean ± SD | 469.9 ± 130.7 (135-924) |
| EBL | 1263.5 ± 777.3 |
| LOS, mean ± SD | 7.5 ± 7.0 |
| Complication | 29 (19%) |
| Reoperation | 24 (15%) |
Figure 1.
Preoperative and postoperative global spinal alignment groups.
Table 2.
Comparison of 1- and 2-Year Cohorts.
| Variable | 1-year N = 157 | 2-year N = 88 | P-value |
|---|---|---|---|
| Age, mean ± SD | 50.9 ± 17.5 | 53.1 ± 16.8 | .339 |
| Female, n (%) | 105 (67%) | 62 (71%) | .512 |
| ASA, n (%) 1 / 2 / 3 |
15 (10%) / 97 (62%) / 45 (28%) |
8 (9%) / 57 (65%) / 23 (26%) |
each > .05 |
| BMI, mean ± SD | 25.6 ± 5.8 | 25.8 ± 6.5 | .805 |
| Depression, n (%) | 31 (20%) | 18 (21%) | .852 |
| Diagnosis, n (%) | |||
| AdIS | 82 (52%) | 41 (47%) | .652 |
| Degenerative | 75 (48%) | 47 (53%) | |
| Revision, n (%) | 94 (60%) | 66 (62%) | .758 |
| Preop SVA (cm), mean ± SD (range) | 3.6 ± 6.4 ( −8.8, 24.8) | 3.7 ± 6.3 ( −7.9, 23.2) | .906 |
| Preop CVA (cm), mean ± SD (range) | 2.8 ± 2.6 (0.1,19.8) | 2.9 ± 2.9 (0.1, 20.0) | .782 |
| Max Cobb (°), mean ± SD (range) | 42.6 ± 26.3 (1.2, 131.7) | 40.5 ± 25.6 (1.2, 108.3) | .546 |
| TIL, mean ± SD (range) | 13.4 ± 4.0 (6-25) | 13.1 ± 4.6 (6-25) | .594 |
| 3CO, mean ± SD (range) | 22 (14%) | 15 (17%) | .529 |
| Operative time, mean ± SD (range) | 469.9 ± 130.7 (135-924) | 461.9 ± 138.9 (135-924) | .654 |
| EBL, mean ± SD | 1263.5 ± 777.3 | 1258 ± 879.6 | .960 |
| LOS, mean ± SD | 7.5 ± 7.0 | 7.2 ± 6.3 | .739 |
| Complication, n (%) | 29 (19%) | 16 (18%) | .847 |
| Reoperation, n (%) | 24 (15%) | 15 (17%) | .680 |
Change From Preoperative to Postoperative
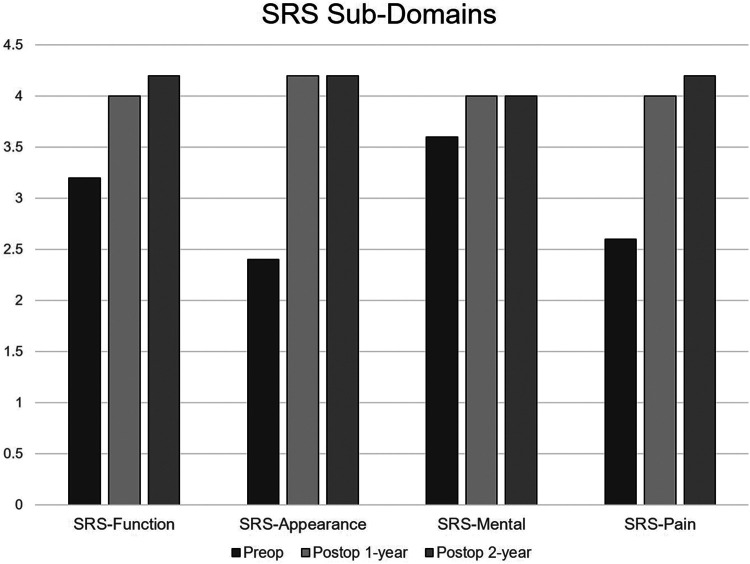
All PROs showed significant improvement from preoperative to 1-year and preoperative to 2-years postoperative (Figure 2). Significant improvement was seen at both the preoperative to 1-year interval, and the preoperative to 2-year interval (each < .001). From the time interval of preoperative, 1-year, and 2-years postoperative, the following median PRO values were seen—ODI: 38, 14, 10; SRS-function: 3.2, 4, 4.2; SRS-appearance: 2.4, 4.2, 4.2; SRS-mental health: 3.6, 4, 4; and SRS-pain: 2.6, 4, 4.2 (Figure 3).
Figure 2.
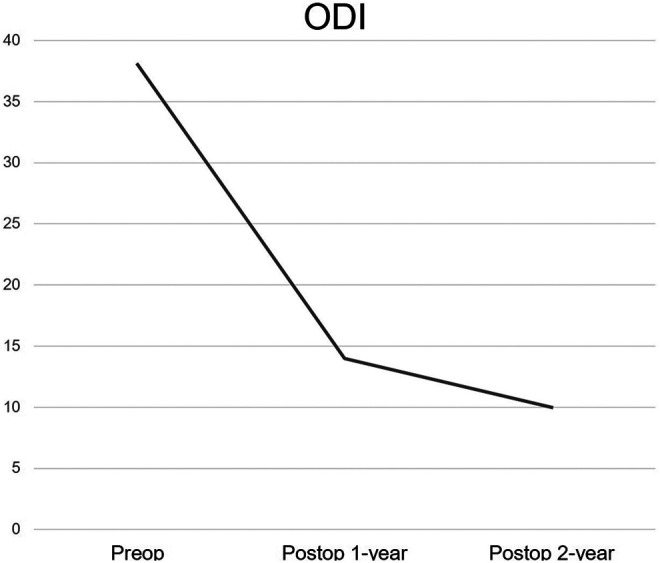
ODI at preoperative, 1-year, and 2-years.
Figure 3.
SRS-22r sub-domains at preoperative, 1-year, and 2-years.
Regarding radiographic data, preoperative to immediate postoperative radiographic parameters all improved significantly (Table 3). With respect to changes in PROs based on alignment status, preoperatively, there was a significant difference in baseline ODI among each alignment group, with both SM and CCSM having significantly worse ODI (P = .007) than NA and CM. Postoperatively, all groups displayed similar PROs, despite residual malalignment occurring in 18 patients with CM, 24 patients with SM, and 7 patients with CCSM (Table 4). Though postoperative SM and CCSM patients displayed slightly inferior ODI at 1 and 2-years, these were not significantly different from the NA and CM group.
Table 3.
Changes in Radiographic Values From Preoperative to 2-Year Postoperative.
| Preoperative | 2-years postoperative | P-value | |
|---|---|---|---|
| CVA (cm), mean ± SD | 2.8 ± 2.6 | 1.7 ± 1.3 | < .001* |
| SVA (cm), mean ± SD | 3.6 ± 6.4 | 1.1 ± 3.9 | < .001* |
| Max Cobb (°), mean ± SD | 42.6 ± 26.3 | 19.1 ± 11.6 | < .001* |
| L4 tilt (°), mean ± SD | 10.0 ± 8.3 | 4.6 ± 4.3 | < .001* |
| L5 tilt (°), mean ± SD | 6.4 ± 6.2 | 3.5 ± 3.5 | < .001* |
Abbreviations: CVA, coronal vertical axis; SVA, sagittal vertical axis.
* Denotes statistically significant.
Table 4.
PROs at Preoperative, 1-Year Postoperative, and 2-Years Postoperative by Alignment Group.
| Neutral alignment | Coronal malalignment | Sagittal malalignment | Combined coronal/sagittal malalignment | P-value | |
|---|---|---|---|---|---|
| Preoperative | N = 77 | N = 26 | N = 26 | N = 28 | |
| ODI, mean ± SD | 31.2 ± 19.6 | 31.2 ± 20.1 | 43.4 ± 18.0 | 48.0 ± 14.1 | .007* |
| Postoperative | N = 108 | N = 18 | N = 24 | N = 7 | |
| ODI 1y, mean ± SD | 16.5 ± 16.9 | 17.2 ± 16.8 | 22.4 ± 20.0 | 23.7 ± 17.4 | .329 |
| ODI 2y, mean ± SD | 15.9 ± 18.5 | 11.8 ± 13.2 | 16.5 ± 18.1 | 21.0 ± 19.6 | .738 |
Abbreviation: ODI, Oswestry Disability Index.
* Denotes statistically significant.
Changes From 1 to 2-Years
In all patients, changes during the 1- to 2-year interval are summarized (Table 5). With respect to median values of each PRO, no statistically significant changes occurred during the 1- to 2-year interval. The same trend was seen for patients achieving MSS. However, 1 significant finding of more patients achieving MCID for ODI at 2-years than 1-year was found (69% vs. 84%, P < .001).
Table 5.
Changes in PROs From 1 to 2-Year Postoperative.
| All patients | |||
|---|---|---|---|
| 1-year postop | 2-Year Postop | P-value | |
| Values | |||
| ODI, median (IQR) (157/88) | 14 (2-26) | 10 (0-26) | .174 |
| SRS-function, median (IQR); (109/57) | 4.0 (3.2-4.4) | 4.0 (3.6-4.4) | .961 |
| SRS-appearance, median (IQR); (109/57) | 4.2 (3.6-4.8) | 4.0 (3.6-4.4) | .238 |
| SRS-mental, median (IQR); (109/57) | 4.0 (3.6-4.4) | 4.0 (3.8-4.4) | .526 |
| SRS-pain, median (IQR); (109/57) | 4.0 (3.2-4.6) | 4.0 (3.0-4.8) | .452 |
| MCID | |||
| ODI, n (%) | 69% | 84% | < .001* |
| SRS-function, n (%) | 59% | 61% | .738 |
| SRS-appearance, n (%) | 79% | 77% | .800 |
| SRS-pain, n (%) | 66% | 63% | .710 |
| Minimum symptom scale | |||
| ODI <20, median (IQR) | 35% | 31% | .489 |
| SRS-pain/function >8 | 50% | 62% | .196 |
* Denotes statistically significant.
Sub-Group Analysis
Among all sub-groups, only significant results are summarized (Table 6). Patients >55-years had a significant change in median ODI value (18 vs. 8, P = .047) and percent achieving ODI MCID (73% vs. 84%, P = .048). With respect to global alignment, no significant changes were found for CM and SM patients, yet CCSM patients had a significant improvement in percent achieving MCID SRS-appearance score (75% vs. 100%, P = .050). With respect to more severe deformity, no significant results were found for patients with CM >5 cm and max Cobb angle >60°, yet patients with severe SM (SVA > 7.5 cm) had a similar significant improvement in percent achieving MCID in SRS-appearance during the 1- to 2-year interval (73% vs. 100%, P = .032). With respect to invasiveness of surgery and complication status, no significant changes took place during the 1- to 2-year postoperative interval.
Table 6.
Sub-Group Analysis of Changes in PROs From 1 to 2-Year Postoperative.
| Sub-group analysis (significant results only) | |||
|---|---|---|---|
| 1-year postop | 2-year postop | P-value | |
| 1. Age >55Y | |||
| ODI, median (IQR) | 18 (4-28) | 8 (0-26) | .047* |
| % achieving MCID | 73% | 84% | .048* |
| 2. Global alignment | |||
| Combined coronal/sagittal malalignment % achieving MCID SRS-appearance |
75% |
100% |
.050* |
| No significant changes for coronal malalignment-only or sagittal malalignment only | |||
| 3. Severity of deformity | |||
| Severe sagittal malalignment >7.5 cm % achieving MCID SRS-appearance |
73% |
100% |
.032* |
| No significant changes for severe coronal malalignment >5 cm or max Cobb angle >60° | |||
| 4. Invasiveness of surgery | |||
| No significant changes for 3 column osteotomy or total instrumented levels | |||
| 5. Complication status | |||
| No significant changes for complication or reoperation | |||
* Denotes statistically significant.
Discussion
The current study sought to determine whether some ASD patients undergoing spinal reconstruction experience improvement in PROs from 1- to 2-years postoperative. As expected, all patients significantly improved from preoperative to both follow-up time points. During the 1- to 2-year interval, the only significant improvement in PROs among all patients was those reaching ODI MCID. We found that certain populations experienced significant improvement in the 1- to 2-year period on subgroup analysis. Specifically, individuals >55-years old had an improved median ODI and improved percent achieving ODI MCID. Furthermore, those with CCSM had significant improvement in percent achieving MCID SRS-appearance scores, as did patients with severe preoperative SM (>7.5 cm). These findings have implications for patients and surgeons to understand the recovery trajectory after ASD surgery.
With an aging U.S. population, 24 older ASD patients will continue to require surgery, and understanding the trajectory of their recovery is important. 2 Though more medically frail and with an inherently higher risk of complications, it is generally agreed upon that ASD surgery offers improvement in older adults. In patients ≥65 years, Li et al 5 found that patients undergoing surgery had significantly less pain and improved quality of life, self-image, mental health, and satisfaction compared to those undergoing non-operative treatment. 5 Evidence also suggests that with time, complications after ASD surgery in patients ≥75 years have significantly decreased from 26.7% in 2003 to 8.6% in 2012.8,25 With respect to length of recovery, while the literature shows overall positive clinical outcomes in older patients with multi-year follow-up,6,26-28 limited analysis exists for the timeline of improvement, and when this improvement may stop. Scheer et al 10 found that older patients had significantly greater improvement than younger patients at 6-weeks, 1-year, and 2-years postoperative. 10 The authors hypothesized that elderly patients’ poorer baseline function led to more opportunity for improvement. Furthermore, multiple studies have demonstrated that older age is associated with increased postoperative complications, longer length of stay, and reoperation. Likewise, a recent report by Lee et al 29 demonstrated a statistically significant difference in age, where elderly patients experienced higher rates of readmissions at 2-years postoperative (51.3 vs. 59.6, P = 0.013). Additionally, the authors showed that inpatient complications did not negatively impact 2-year PROs, and patients with a readmission/reoperation had significant improvement in their 2-year SRS and ODI scores compared to their 1-year and preoperative values in a cohort where the average age was 56-years-old. An additional prospective, multicenter, international study of 77 ASD patients followed for 5-years postoperative confirmed this trend that PROs were similar between patients who endured a major, surgery-related complication compared to those who did not. 30 Taken together, these data imply that older patients’ recovery window may be longer given the extended recovery dynamic.6,31-33 Adding to this literature, we found that from 1- to 2-years postoperative, individuals >55 years improved significantly on ODI and percent achieving ODI MCID. Potential explanations for these findings include more time needed to improve aerobic conditioning, regain muscle strength, or recover from prior complications.
Multiple groups have reported that sagittal malalignment is a strong driver of disability before and after ASD surgery.34-36 A recent study by Pierce et al found that patients classified as severely frail, which included individuals with severe SM >8 cm, had overall better PROs at 1- and 3-years compared to less frail and better aligned patients. 12 In a cohort of patients with SVA >4 cm, sagittal alignment initially worsened immediately after surgery, yet began to meaningfully correct between 6-weeks and 6-months. 37 Interestingly, patients undergoing minimally-invasive ASD correction with severe SM >9.5 cm patients did not experience the same postoperative improvement in PROs than those without SM, which may have to do with surgical approach. 38 We found that patients with severe preoperative SM >7.5 cm experienced continued improvement during the 1- to 2-year interval in SRS-appearance scores. Taken together, the effect of severe SM on recovery kinetics is not fully understood, but improvement after severe SM correction may extend to 2-years postoperative.
Combined coronal and sagittal malalignment (CCSM) is an area with relatively limited investigation, and our results showed that patients with CCSM significantly improved in SRS-appearance score from 1- to 2 years. Coronal alignment itself has been underemphasized in ASD surgery, with operative goals less defined. 39 Recent reports have begun to study the role of coronal alignment parameters, as CM has been shown to lead to significant pain, disability, and poor cosmesis.39-43 CCSM is an even less studied phenomenon in ASD, with a 3 patient case series of such patients describing good correction results, but without much PRO data. 44 With 18% of our cohort classified as CCSM, a sizeable number of ASD patients may fall into this category. Additional research is required to learn more about this challenging patient population, and our evidence suggests this may be a risk factor for continued improvement during the 1- to 2-year interval.
The current data provides a more nuanced understanding into the dynamics of improvement after ASD surgery. Further information on the timeline of recovery helps patients and their surgeons understand the postoperative experience. It is our hope that the current data advances our knowledge of clinical improvement in patients with SM and CCSM. In future studies, more sensitive PROs may yield different results. We used mainly LEGACY measures in this study, and newer studies evaluating PROMIS scores 45 that are less prone to floor and ceiling effects, should be studied. Lastly, continued study of alignment groups and associated disability are needed. Though a proportion of patients still had coronal and/or sagittal malalignment (CM 11%, SM 15%, CCSM 4%) postoperatively, their 1-year and 2-year PROs were similar to those with NA.
The present study is not without limitation. First, several statistical tests were run, which increases our chance of Type 1 error; however, these were all stated a-priori and meant to find potentially significant trends. We have been careful to not over-conclude our results and give them more credence than they deserve. The statistically significant findings are viewed with caution as empirical data that some patients may improve during the 1- to 2-year time interval, which can be used to discuss with patients and families in the preoperative and postoperative setting. Second, as a single-center, retrospective study, these results require confirmation in multi-center, prospective trials. To that end, only 2 surgeons were included in the current sample, and different trends may be seen with a large group of surgeons and different surgical techniques and approaches. Third, only 2 primary outcome measures, ODI and SRS-22r, were used, which are both subject to some potential floor and ceiling effects. Fourth, inconsistent sample sizes were seen between the 1- and 2-year time interval, but it was determined that both groups were similar and almost identical in several demographic and operative variables.
Conclusions
In patients undergoing adult spinal deformity (ASD) surgery, most patients reported maximum outcome status by 1-year postoperative; however, a subset of patients may still improve ODI MCID from 1- to 2-years postoperative. Empirical results confirm that the subset of patients that may continue clinically significant improvement after 1-year are those 55 years and older, having combined preoperative coronal/sagittal malalignment, and severe preoperative sagittal malalignment ≥7.5 cm preoperative.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yong Shen, BA  https://orcid.org/0000-0002-4866-838X
https://orcid.org/0000-0002-4866-838X
Meghan Cerpa, MPH  https://orcid.org/0000-0002-5931-7067
https://orcid.org/0000-0002-5931-7067
Nathan J. Lee, MD  https://orcid.org/0000-0001-9572-5968
https://orcid.org/0000-0001-9572-5968
Alex S. Ha, MD  https://orcid.org/0000-0001-8057-9996
https://orcid.org/0000-0001-8057-9996
References
- 1.Kebaish KM, Neubauer PR, Voros GD, Khoshnevisan MA, Skolasky RL. Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender. Spine (Phila Pa 1976). 2011;36(9):731–736. doi:10.1097/BRS.0b013e3181e9f120 [DOI] [PubMed] [Google Scholar]
- 2.Diebo BG, Shah NV, Boachie-Adjei O, et al. Adult spinal deformity. Lancet. 2019;394(10193):13–19. doi:10.1016/S0140-6736(19)31125-0 [DOI] [PubMed] [Google Scholar]
- 3.Bess S, Line B, Fu KM, et al. The health impact of symptomatic adult spinal deformity: comparison of deformity types to United States population norms and chronic diseases. Spine (Phila Pa 1976). 2016;41(3):224–233. doi:10.1097/BRS.0000000000001202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976). 2009;34(20):2171–2178. doi:10.1097/BRS.0b013e3181a8fdc8 [DOI] [PubMed] [Google Scholar]
- 5.Li G, Passias P, Kozanek M, et al. Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine (Phila Pa 1976). 2009;34(20):2165–2170. doi:10.1097/BRS.0b013e3181b3ff0c [DOI] [PubMed] [Google Scholar]
- 6.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007;32(20):2238–2244. doi:10.1097/BRS.0b013e31814cf24a [DOI] [PubMed] [Google Scholar]
- 7.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery incidence, risk factors, and clinical impact. Spine (Phila Pa 1976). 2016;41(22):1718–1723. doi:10.1097/BRS.0000000000001636 [DOI] [PubMed] [Google Scholar]
- 8.Passias PG, Poorman GW, Jalai CM, et al. Morbidity of adult spinal deformity surgery in elderly has declined over time. Spine (Phila Pa 1976). 2017;42(16):E978–E982. doi:10.1097/BRS.0000000000002009 [DOI] [PubMed] [Google Scholar]
- 9.Yoshida G, Boissiere L, Larrieu D, et al. Advantages and disadvantages of adult spinal deformity surgery and its impact on health-related quality of life. Spine (Phila Pa 1976). 2017;42(6):411–419. doi:10.1097/BRS.0000000000001770 [DOI] [PubMed] [Google Scholar]
- 10.Scheer JK, Mundis GM, Klineberg E, et al. Postoperative recovery after adult spinal deformity surgery: comparative analysis of age in 149 patients during 2-year follow-up. Spine (Phila Pa 1976). 2015;40(19):1505–1515. doi:10.1097/BRS.0000000000001062 [DOI] [PubMed] [Google Scholar]
- 11.Lenke LG, Fehlings MG, Shaffrey CI, et al. Neurologic outcomes of complex adult spinal deformity surgery: results of the prospective, multicenter scoli-RISK-1 study. Spine (Phila Pa 1976). 2016;41(3):204–212. [DOI] [PubMed] [Google Scholar]
- 12.Pierce KE, Passias PG, Alas H, et al. Does patient frailty status influence recovery following spinal fusion for adult spinal deformity?: an analysis of patients with 3-year follow-up. Spine (Phila Pa 1976). 2020;45(7):E397–E405. doi:10.1097/BRS.0000000000003288 [DOI] [PubMed] [Google Scholar]
- 13.Baum GR, Ha AS, Cerpa M, et al. Does the global alignment and proportion score overestimate mechanical complications after adult spinal deformity correction? J Neurosurg Spine. 2021:1–7. doi:10.3171/2020.6.SPINE20538 [DOI] [PubMed] [Google Scholar]
- 14.Yilgor C, Sogunmez N, Boissiere L, et al. Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 2017;99(19):1661–1672. doi:10.2106/JBJS.16.01594 [DOI] [PubMed] [Google Scholar]
- 15.Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine. 2012;16(6):547–564. doi:10.3171/2012.2.SPINE11320 [DOI] [PubMed] [Google Scholar]
- 16.Fairbank JCT, Davies JB, Couper J, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. doi:10.1007/978-3-642-28753-4_101584 [PubMed] [Google Scholar]
- 17.Fairbank JCT, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000;25(22):2940–2952. doi:10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 18.Asher MA, Lai SM, Glattes RC, Burton DC, Alanay A, Bago J. Refinement of the SRS-22 health-related quality of life questionnaire function domain. Spine (Phila Pa 1976). 2006;31(5):593–597. doi:10.1097/01.brs.0000201331.50597.ea [DOI] [PubMed] [Google Scholar]
- 19.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J. 2008;8(6):968–974. doi:10.1016/j.spinee.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 20.Crawford CH, Glassman SD, Bridwell KH, Berven SH, Carreon LY. The minimum clinically important difference in SRS-22 R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976). 2015;40(6):377–381. doi:10.1097/BRS.0000000000000761 [DOI] [PubMed] [Google Scholar]
- 21.Kelly MP, Lurie JD, Yanik EL, et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am. 2019;101(4):338–352. doi:10.2106/JBJS.18.00483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu S, Diebo BG, Henry JK, et al. The benefit of nonoperative treatment for adult spinal deformity: identifying predictors for reaching a minimal clinically important difference. Spine J. 2016;16(2):210–218. doi:10.1016/j.spinee.2015.10.043 [DOI] [PubMed] [Google Scholar]
- 23.Yuksel S, Ayhan S, Nabiyev V, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J. 2019;19(1):71–78. doi:10.1016/j.spinee.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 24.O’Lynnger TM, Zuckerman SL, Morone PJ, Dewan MC, Vasquez-Castellanos RA, Cheng JS. Trends for spine surgery for the elderly: implications for access to healthcare in North America. Neurosurgery. 2015;77(Suppl 4):S136–S141. doi:10.1227/NEU.0000000000000945 [DOI] [PubMed] [Google Scholar]
- 25.Sing DC, Berven SH, Burch S, Metz LN. Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J. 2017;17(5):627–635. doi:10.1016/j.spinee.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 26.Drazin D, Shirzadi A, Rosner J, et al. Complications and outcomes after spinal deformity surgery in the elderly: review of the existing literature and future directions. Neurosurg Focus. 2011;31(4):E3. doi:10.3171/2011.7.FOCUS11145 [DOI] [PubMed] [Google Scholar]
- 27.Hassanzadeh H, Jain A, El Dafrawy MH, et al. Clinical results and functional outcomes of primary and revision spinal deformity surgery in adults. J Bone Joint Surg Am. 2013;95(15):1413–1419. doi:10.2106/JBJS.L.00358 [DOI] [PubMed] [Google Scholar]
- 28.Crawford CH, Carreon LY, Bridwell KH, Glassman SD. Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J. 2012;21(11):2165–2169. doi:10.1007/s00586-012-2310-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee NJ, Cerpa M, Leung E, Sardar ZM, Lehman RA, Lenke LG. Do readmissions and reoperations adversely affect patient-reported outcomes following complex adult spinal deformity surgery at a minimum 2 years postoperative? Spine Deform. 2021;9(3):789–801. doi:10.1007/s43390-020-00235-w [DOI] [PubMed] [Google Scholar]
- 30.Zuckerman SL, Cerpa M, Lenke LG, et al. Patient-reported outcomes after complex adult spinal deformity surgery: 5-year results of the scoli-risk-1 study. Glob Spine J. 2021. doi:10.1177/2192568220988276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine. 2016;25(4):486–493. doi:10.3171/2016.2.SPINE151345 [DOI] [PubMed] [Google Scholar]
- 32.Zhu F, Bao H, Liu Z, et al. Unanticipated revision surgery in adult spinal deformity: an experience with 815 cases at one institution. Spine (Phila Pa 1976). 2014;39(26B):B36–B44. doi:10.1097/BRS.0000000000000463 [DOI] [PubMed] [Google Scholar]
- 33.Klineberg EO, Passias PG, Jalai CM, et al. Predicting extended length of hospital stay in an adult spinal deformity surgical population. Spine (Phila Pa 1976). 2016;41(13):E798–E805. doi:10.1097/BRS.0000000000001391 [DOI] [PubMed] [Google Scholar]
- 34.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024–2029. doi:10.1097/01.brs.0000179086.30449.96 [DOI] [PubMed] [Google Scholar]
- 35.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V.Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35(25):2224–2231. doi:10.1097/BRS.0b013e3181ee6bd4 [DOI] [PubMed] [Google Scholar]
- 36.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013;38(13):E803–E812. doi:10.1097/BRS.0b013e318292b7b9 [DOI] [PubMed] [Google Scholar]
- 37.McDowell MM, Tempel ZJ, Gandhoke GS, et al. Evolution of sagittal imbalance following corrective surgery for sagittal plane deformity. Neurosurgery. 2017;81(1):129–134. doi:10.1093/neuros/nyx145 [DOI] [PubMed] [Google Scholar]
- 38.Mundis GM, Turner JD, Deverin V, et al. A critical analysis of sagittal plane deformity correction with minimally invasive adult spinal deformity surgery: a 2-year follow-up study. Spine Deform. 2017;5(4):265–271. doi:10.1016/j.jspd.2017.01.010 [DOI] [PubMed] [Google Scholar]
- 39.Bao H, Yan P, Qiu Y, Liu Z, Zhu F. Coronal imbalance in degenerative lumbar scoliosis: prevalence and influence on surgical decision-making for spinal osteotomy. Bone Joint J. 2016;98-B(9):1227–1233. doi:10.1302/0301-620X.98B9.37273 [DOI] [PubMed] [Google Scholar]
- 40.Bao H, Liu Z, Zhang Y, et al. Sequential correction technique to avoid postoperative global coronal decompensation in rigid adult spinal deformity: a technical note and preliminary results. Eur Spine J. 2019;28(9):2179–2186. doi:10.1007/s00586-019-06043-9 [DOI] [PubMed] [Google Scholar]
- 41.Plais N, Bao H, Lafage R, et al. The clinical impact of global coronal malalignment is underestimated in adult patients with thoracolumbar scoliosis. Spine Deform. 2020;8(1):105–113. doi:10.1007/s43390-020-00046-z [DOI] [PubMed] [Google Scholar]
- 42.Obeid I, Berjano P, Lamartina C, Chopin D, Boissière L, Bourghli A. Classification of coronal imbalance in adult scoliosis and spine deformity: a treatment-oriented guideline. Eur Spine J. 2019;28(1):94–113. doi:10.1007/s00586-018-5826-3 [DOI] [PubMed] [Google Scholar]
- 43.Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2- to 5-year follow-up study. J Spinal Disord Tech. 2015;28(9):341–347. doi:10.1097/BSD.0b013e3182aab2ff [DOI] [PubMed] [Google Scholar]
- 44.Cecchinato R, Berjano P, Aguirre MFI, Lamartina C. Asymmetrical pedicle subtraction osteotomy in the lumbar spine in combined coronal and sagittal imbalance. Eur Spine J. 2014;24:66–71. doi:10.1007/s00586-014-3669-0 [DOI] [PubMed] [Google Scholar]
- 45.Raad M, Jain A, Huang M, et al. Validity and responsiveness of PROMIS in adult spinal deformity: the need for a self-image domain. Spine J. 2019;19(1):50–55. doi:10.1016/j.spinee.2018.07.014 [DOI] [PubMed] [Google Scholar]