Abstract
BACKGROUND
Maternal obesity has risen in the United States in recent decades.
OBJECTIVE
This study aimed to evaluate the impact of maternal obesity on the risk for spontaneous preterm delivery and the risk for overall preterm delivery among patients with cervical cerclage placement.
STUDY DESIGN
This was a retrospective study in which data from the California Office of Statewide Health Planning and Development linked birth file from 2007 to 2012 were used, yielding a total of 3654 patients with and 2,804,671 patients without cervical cerclage placement. Exclusion criteria included patients with missing information on body mass index, multiple gestation, anomalous pregnancies, and gestations <20 weeks or >42 weeks. Patients in each group were identified and were further categorized based on body mass index with the nonobese group defined as having a body mass index of <30 kg/m2, the obese group defined as having a body mass index of 30 to 40 kg/m2, and the morbidly obese group defined as having a body mass index >40 kg/m2. The risks for overall and spontaneous preterm delivery were compared between patients without obesity and those with obesity or those with morbid obesity patients. The analysis was stratified by cerclage placement.
RESULTS
Among patients who underwent cerclage placement, the risk for spontaneous preterm delivery was not significantly different in the obese and morbidly obese group when compared with the nonobese group (24.2% vs 20.6%; adjusted odds ratio, 1.18; 95% confidence interval, 0.97–1.43; and 24.5% vs 20.6%; adjusted odds ratio, 1.12; 0.78–1.62, respectively). However, among patients without cerclage placement, the obese and morbidly obese groups had a higher risk for spontaneous preterm delivery than the nonobese group (5.1% vs 4.4%; adjusted odds ratio, 1.04; 1.02–1.05; and 5.9% vs 4.4%; adjusted odds ratio, 1.03; 1.00–1.07, respectively). The risks for overall preterm delivery at <37 weeks’ gestation were higher for the obese and morbidly obese groups than for the nonobese group among patients with cerclage (33.7% vs 28.2%; adjusted odds ratio, 1.23; 1.03–1.46; and 32.1% vs 28.2%; adjusted odds ratio, 1.01; 0.72–1.43, respectively). Similarly, among patients without cerclage placement, the risks for preterm delivery at <37 weeks’ gestation were higher for the obese and morbidly obese groups than for the nonobese group (7.9% vs 6.8%; adjusted odds ratio, 1.05; 1.04–1.06; and 9.3% vs 6.8%; adjusted odds ratio, 1.10; 1.08–1.13, respectively).
CONCLUSION
Among patients who received a cervical cerclage for the prevention of preterm birth, obesity was not associated with an increased risk for spontaneous preterm delivery. However, it was associated with an overall increased risk for preterm delivery.
Key words: body mass index, cerclage, cerclage failure, morbid obesity, obesity, preterm delivery
AJOG Global Reports at a Glance.
Why was this study conducted?
Current literature on the risk for preterm delivery overall and for spontaneous preterm delivery among patients with obesity and morbid obesity with cervical cerclage is limited and contradictory, necessitating further elucidation.
Key findings
Among patients with cervical cerclage, obesity does not increase the risk for spontaneous preterm delivery. However, it is associated with an increased risk for overall preterm delivery.
What does this add to what is known?
This study provides further clarity on the risks for overall and spontaneous preterm delivery among patients with obesity with cervical cerclage. The findings of this study should be used in the counseling of patients with obesity who require cerclage placement and provide reassurance on the efficacy of cerclage in women with obesity. This study also highlights the risks for preterm delivery associated with obesity secondary to other medical indications.
Introduction
The prevalence of obesity among pregnant women was estimated to be between 18.5% and 38.3%.1, 2, 3, 4 Maternal obesity is a preventable and modifiable risk factor for many adverse pregnancy outcomes, including hypertensive disorders, gestational diabetes, thromboembolic events, stillbirths, cesarean deliveries,5, 6, 7, 8, 9, 10, 11 and preterm delivery.11, 12, 13
Spontaneous preterm birth contributed to approximately 60% of all preterm births,14,15 whereas medically indicated preterm birth contributed to the remaining 30% to 40% of all preterm births.16,17 The effect of obesity on each type of preterm delivery has been shown to be variable. Previous studies have demonstrated that obesity could be a protective factor against spontaneous preterm delivery.18,19 Existing laboratory data suggest that obesity may be associated with higher endogenous ghrelin production, which may inhibit oxytocin receptor activity and lead to suppression of spontaneous labor.20 Conversely, previous data also demonstrated that the presence of inflammatory biomarkers associated with obesity may play a role in the increased risk for spontaneous preterm birth.21 Meanwhile, other studies have shown that obesity is associated with an increased risk for medically indicated preterm delivery.22,23 One study demonstrated that as maternal body mass index (BMI) increased, the risks for both medically indicated and spontaneous preterm deliveries increased accordingly.24
Among patients with preexisting risks for preterm delivery that necessitate cervical cerclage placement, data on whether obesity affects the efficacy of cerclage placement are limited and conflicting. Among women with cerclage, it was shown that maternal obesity did not seem to impact the rates of overall preterm delivery25 and spontaneous preterm delivery.26 However, a retrospective study demonstrated that there was an inverse correlation between BMI and gestational age at delivery among patients with cervical cerclage.27 Some researchers theorized that the increased abdominal pressure on the cerclage may have contributed to cerclage failure.27,28
Thus far, the data on maternal obesity and preterm delivery among patients with cerclage are sparse and conflicting, necessitating further elucidation. Therefore, we aimed to evaluate the risk for preterm delivery associated with obesity among patients with cerclage using a large population-based cohort study. We hypothesized that maternal obesity increased the risks for spontaneous preterm delivery and overall preterm delivery among patients with cervical cerclage.
Materials and Methods
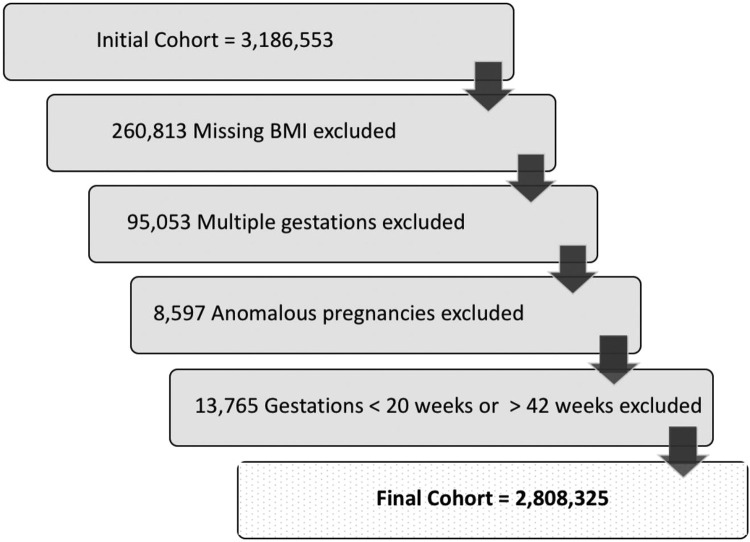
This was a retrospective study in which data from the California Office of Statewide Health Planning and Development linked birth file from 2007 to 2012 were used, which is a birth registry database that was linked to hospital discharge International Classification of Diseases, Ninth Revision (ICD-9), billing codes. Cohort exclusion criteria included patients with missing data on BMI, multiple gestation, anomalous pregnancies, and gestations <20 weeks or >42 weeks (Figure 1). Patients with cerclage placement were identified using hospital birth records. Patients in each group were identified and were further categorized based on maternal prepregnancy BMI, with the nonobese group defined as having a BMI of <30 kg/m2, the obese group as having a BMI of 30 to 40 kg/m2, and morbidly obese group as having a BMI >40 kg/m2. The primary outcome of interest was preterm delivery, defined as any delivery between 20+0/7 weeks and 36+6/7 weeks’ gestation. Furthermore, we evaluated the risk for severe prematurity, defined as deliveries up to 34+6/7 weeks’ gestation. The outcomes of interest were further delineated as deliveries following spontaneous labor based on ICD-9 code 644.0 to 644.2. The risk for preterm delivery associated with obesity was estimated separately for pregnancies that required cervical cerclage and pregnancies that did not require cerclage.
Figure 1.
The cohort selection
Nguyen. Obesity and preterm delivery risk with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023.
The demographics of interest are included Table 1. Categorical variables were compared between the 2 groups using the chi-square test. A 2-tailed P value of <.05 was used as the threshold for statistical significance. Logistic regression analysis was used to estimate the association between BMI group and the risk for preterm delivery. Odd ratios (ORs) with 95% confidence intervals (CIs) were calculated and adjusted ORs (aORs) were adjusted for race, insurance type, hypertension, preeclampsia, pregestational diabetes, gestational diabetes, history of preterm delivery, and maternal age. Bootstrapping was performed 50 times in the full sample to evaluate the risk for spontaneous preterm delivery given the relatively limited cohort of patients with a cerclage with morbid obesity. Statistical analyses were performed using Stata 14 (StataCorp, College Station, TX). This study was approved by the California State University – Fullerton Institutional Review Board (IRB# HSR-19-20-548).
Table 1.
Demographics of patients in the nonobese, obese, and morbidly obese groups
| Demographics | Nonobese | Obese (BMI 30.0–40.0 kg/m2) |
Morbidly obese (BMI ≥40 kg/m2) |
P value |
|---|---|---|---|---|
| 2,236,073 | 490,368 | 81,884 | ||
| Maternal age, mean±SD | 28.2±6.4 | 28.5±6.0 | 28.8±5.6 | <.0001 |
| Gestational age at delivery | 39 (38–40) | 39 (38–40) | 39 (38–40) | <.0001 |
| Race | ||||
| White | 41 | 53.3 | 46.3 | <.001 |
| Black | 1 | 1.6 | 2.4 | |
| Hispanic | 54.5 | 41.2 | 47.7 | |
| Asian | 0.9 | 0.5 | 0.5 | |
| Mix | 1.6 | 2.3 | 2 | |
| Other | 0.9 | 1.1 | 1.1 | |
| Chronic hypertension | 1 | 1.8 | 3.1 | <.001 |
| Preeclampsia | 2.6 | 4.9 | 7.6 | <.001 |
| Pregestational diabetes mellitus | 0.04 | 0.2 | 0.5 | <.001 |
| Gestational diabetes mellitus | 1.7 | 3.7 | 5.6 | <.001 |
| Private insurance | 50.7 | 40.8 | 40.8 | <.001 |
| History of preterm | 0.3 | 0.4 | 0.6 | <.001 |
| History of cesarean delivery | 13.2 | 21.6 | 28.4 | <.001 |
BMI, body mass index.
Nguyen. Obesity and preterm delivery risk with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023.
Results
This retrospective cohort study included 3654 pregnant patients with cerclage placement among which there were 184 patients with morbid obestiy, 832 patients with obesity, and 2638 patients without obesity. The group of 2,784,882 patients without cervical cerclage included 81,700 patients with morbid obesity, 489,536 patients with obesity, and 2,233,435 patients without obesity. The demographics of all patients in each BMI group are shown in Table 1. Compared with the population without obesity, the groups with obesity and morbid obesity demonstrated higher rates of pregestational and gestational complications including chronic hypertension, preeclampsia, pregestational diabetes, gestational diabetes, and higher rates of previous preterm delivery, and a history of cesarean delivery.
The risks for spontaneous preterm deliveries were not different between those who received a cerclage in the obese and morbidly obese groups and those in the nonobese group (24.2% vs 20.6%; aOR, 1.18; 0.97–1.43; and 24.5% vs 20.6%; aOR, 1.12; 0.78–1.62, respectively) (Table 2). However, among patients without cerclage placement, the obese and morbidly obese groups had a higher risk for spontaneous preterm delivery than the nonobese group (5.1% vs 4.4%; aOR, 1.04; 1.02–1.05; and 5.9% vs 4.4%; aOR, 1.03; 1.00–1.07, respectively). After bootstrapping was performed, the risks for spontaneous preterm delivery remained the same (Supplementary Table 1).
Table 2.
The risks for spontaneous preterm delivery among patients with and those without cerclage
| Cerclage groups | Obesity type | Spontaneous preterm deliverya | OR (95% CI) | Adjusted ORb (95% CI) |
|---|---|---|---|---|
| Cerclage placed | Nonobesec | 544 (20.6) | Ref | Ref |
| Obese | 201 (24.2) | 1.23 (1.02–1.47) | 1.18 (0.97–1.43) | |
| Morbidly obese | 45 (24.5) | 1.25 (0.88–1.77) | 1.12 (0.78–1.62) | |
| Without cerclage | Nonobese | 99,125 (4.4) | Ref | Ref |
| Obese | 25,102 (5.1) | 1.16 (1.15–1.18) | 1.04 (1.02–1.05) | |
| Morbidly obese | 4802 (5.9) | 1.34 (1.31–1.39) | 1.03 (1.00–1.07) |
BMI, body mass index; CI, confidence interval; OR, odds ratio.
The data are presented as number (percentage)
ORs were adjusted for maternal age, race, insurance type, hypertension, preeclampsia, pregestational diabetes mellitus, gestational diabetes mellitus, history of preterm delivery, and history of cesarean delivery
cPeople without obesity are those with a BMI <30 kg/m2, people with obesity are those with a BMI of 30 to 40 kg/m2, and those with morbid obesity have a BMI >40 kg/m2.
Nguyen. Obesity and preterm delivery risk with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023.
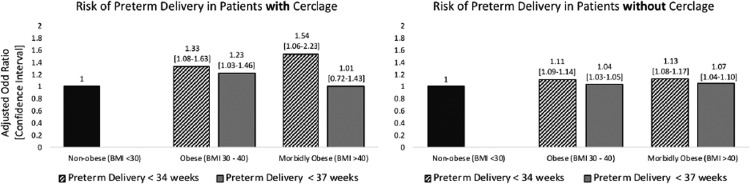
Among patients with cerclage placement, the rates of overall preterm delivery at <37 weeks’ gestation in the obese and morbidly obese groups were higher than those in the nonobese group (33.7% vs 28.2%; aOR, 1.23; 1.03–1.46; and 32.1% vs 28.2%; aOR, 1.01; 0.72–1.43, respectively) as demonstrated in Table 3. Similarly, the rates of preterm delivery at ≤34 weeks’ gestation in the obese group was higher than those in the nonobese group (21% vs 16.9%; aOR, 1.33; 1.08–1.63). The morbidly obese group carried the highest rate of preterm delivery at ≤34 weeks’ gestation when compared with the nonobese group (25% vs 16.9%; aOR, 1.54; 1.06–2.23) (Figure 2).
Table 3.
The risks for preterm delivery at <37weeks and <34 weeks of gestation among patients with obesity and morbid obesity and with and without cerclage
| Cerclage groups | Obesity type | N | Preterm <34 wka | P value | OR (95% CI) | Adjusted ORb(95% CI) | Preterm <37 wk | P value | OR (95% CI) | Adjusted OR(95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Cerclage placed | Nonobesec | 2638 | 445 (16.9) | .001 | Ref | Ref | 745 (28.2) | .009 | Ref | Ref |
| Obese | 832 | 175 (21.0) | 1.31 (1.08–1.60) | 1.33 (1.08–1.63) | 280 (33.7) | 1.29 (1.09–1.52) | 1.23 (1.03–1.46) | |||
| Morbidly obese | 184 | 46 (25.0) | 1.64 (1.16–2.33) | 1.54 (1.06–2.23) | 59 (32.1) | 1.20 (0.87–1.65) | 1.01 (0.72–1.43) | |||
| Without cerclage | Nonobese | 2,233,435 | 56,815 (2.5) | <.0001 | Ref | Ref | 153,620 (6.7) | <.0001 | Ref | Ref |
| Obese | 489,536 | 16,077 (3.3) | 1.30 (1.28–1.32) | 1.11 (1.09–1.14) | 39,417 (8.1) | 1.18 (1.17–1.20) | 1.04 (1.03–1.05) | |||
| Morbidly obese | 81,700 | 3195 (3.9) | 1.56 (1.50–1.62) | 1.13 (1.08–1.17) | 7724 (9.5) | 1.41 (1.38–1.45) | 1.07 (1.04–1.10) |
BMI, body mass index; CI, confidence interval; OR, odds ratio.
The data are presented as number (percentage)
ORs were adjusted for maternal age, race, insurance type, hypertension, preeclampsia, pregestational diabetes, gestational diabetes, history of preterm delivery, and history of cesarean delivery
People without obesity are those with a BMI <30 kg/m2, people with obesity are those with a BMI of 30 to 40 kg/m2, and those with morbid obesity have a BMI >40 kg/m2
Nguyen. Obesity and preterm delivery risk with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023.
Figure 2.
Risks for preterm delivery in patients with and without cervical cerclage
Nguyen. Obesity and preterm delivery risk with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023.
Among patients without cerclage placement, the obese and morbidly obese groups continued to demonstrate increased risks for preterm delivery when compared with the nonobese group, similar to the trend seen in the population of patients with cerclage (Figure 2). The rates for preterm delivery at <37 weeks’ gestation in the obese and morbidly obese groups were higher than that in the nonobese group (8.1% vs 6.7%; aOR, 1.04; 1.03–1.05; and 9.5% vs 6.7%; aOR, 1.07; 1.04–1.10, respectively). Similarly, the rates of preterm delivery <34 weeks’ gestation in the obese and morbidly obese group were higher than that in the nonobese group, (3.3% vs 2.5%; aOR, 1.11; 1.09–1.14; and 3.9% vs 2.5%; aOR, 1.13; 1.08–1.17, respectively).
Discussion
Principal findings
Among patients with cervical cerclage, there was no difference in the risk for spontaneous preterm delivery among all of the BMI groups. However, maternal obesity was associated with an overall increased risk for preterm delivery. Specifically, the risk for overall preterm delivery by 34 weeks’ gestation was 33% higher among women with obesity and 54% higher among women with morbid obesity. Together, these findings suggest that the primary reason for the observed increase in preterm delivery associated with obesity was because of medical indications.
Results in the context of what is known
Obesity continues to serve as one of the major risk factors for many adverse pregnancy complications. In existing literature, the association between obesity and preterm delivery in patients with cerclage has been conflicting. In one study, maternal obesity was observed to not have an impact on the gestational age at delivery among women with a cerclage,25 whereas another study showed that BMI was a significant predictor of preterm delivery.27
Our study has further elucidated the risks for preterm delivery. In the patient population at risk for preterm delivery with a need for cerclage placements, this study demonstrated that obesity was not associated with a higher risk for preterm delivery secondary to the onset of spontaneous labor. This finding reassuringly suggests that cerclage is as efficacious in preventing spontaneous preterm delivery in women with obesity as it is in women without obesity. However, the overall risk for preterm delivery was higher in the obese and morbidly obese groups. These findings suggest that medically indicated preterm deliveries may have been a major contributor to the observed increase in the overall preterm delivery in our study and in other published studies.27
In the population of pregnant patients without cervical cerclage, the mechanisms of how obesity impacts spontaneous preterm delivery is thought to be a consequence of the increased levels of cytokines causing prostaglandin production and matrix-degrading enzymes, which is associated with cervical ripening, weakening of the membranes, and preterm contractions.29,30 The results of this study demonstrated that among patients with cerclage, the impact of obesity and morbid obesity on spontaneous preterm delivery was mitigated such that the risks were the same as those of patients without obesity. Increased adipokines from visceral fats in patients with obesity have been shown to increase systemic inflammation,31,32 contributing to many obesity-related maternal complications, such as endothelial damage and insulin resistance seen in preeclampsia and gestational diabetes, respectively, among other gestational disorders.33, 34, 35 The results from this study of patients with obesity and morbid obesity with cerclage align with the current literature on their counterparts without cerclage, demonstrating the role of obesity in increasing the overall preterm delivery risks associated with other gestational disorders.
Other factors surrounding the cervical cerclage placement procedure could potentially play a role in cerclage effectiveness. Based on current knowledge, cerclage suture materials have been proposed to have differential effects on pregnancy loss. In a prospective cohort study, it was noted that the risk for pregnancy loss and preterm birth when using a monofilament suture was lower than when braided suture was used (7% vs 18%; relative risk, 0.34; 95% CI, 0.18–0.63; and 17% vs 28%; P=.0006, respectively).36 However, a recent, large randomized control trial (the Cerclage Suture Type for an Insufficient Cervix and its Effects on Health Outcomes trial) in which monofilament and braided suture for cervical cerclage were compared showed no difference in the primary outcome of pregnancy loss.37 The effects of different suture materials on preterm birth in obese and nonobese populations deserve further elucidation. Physicians who perform cerclage could also face technical challenges during placement because of obesity status, requiring expert skills. Furthermore, a retrospective study in which the effectiveness of the McDonald vs Shirodkar cerclage type was investigated suggested that in normal patients, when compared with patients who were overweight, cerclage type did not seem to impact pregnancy duration. However, when patients with obesity who received the McDonald cerclage were compared with those who received the Shirodkar cerclage, they had significantly longer pregnancies.38 The Shirodkar cerclage presented a more technically challenging procedure. Similar to any other surgical procedures, cerclage effectiveness, in large part, depend on the skills of the practitioners.
Clinical implication
Based on the results of this study, patients who meet the criteria for history-indicated cerclage should be counseled on the risk for preterm delivery associated with obesity and its link with medical indications and adverse pregnancy outcomes. Reassurance should be provided to patients with obesity because the procedure itself seemed to be equally efficacious in patients with obesity as in patients without obesity. More importantly, the results of this study could provide further information on risk stratification for pregnancies affected by obesity during preconception counseling and initial prenatal visits. As such, during preconception counseling, patients with a history of cerclage placement in a previous pregnancy should be encouraged to optimize their BMI before a future pregnancy to further lower their risk for preterm delivery.
Strengths and limitations
One of the main strengths of this study was the large cohort of patients with cerclage placement during pregnancy, which further allowed us to study the risks for preterm delivery in a relatively small subgroup of women with cerclage and a BMI of >40 kg/m2. The large cohort of patients with and without cerclage allowed us to evaluate the overall risk for preterm delivery associated with maternal obesity and to adjust for many of the common medical conditions that lead to medically indicated preterm deliveries. Furthermore, in this study, we were able to separately analyze the impact of obesity on the preterm delivery risks in the general population without cerclage placement to comprehensively evaluate whether these risks could persist in patients with cerclage. This study evaluated the impact of obesity on the risk for spontaneous preterm delivery while further assessing the overall risk for preterm delivery in this particular population.
We acknowledge the limitations of this study. Because of the nature of this study in that a population-based data registry was used, it is subject to data entry and coding errors. Furthermore, patients with history-indicated, ultrasound-indicated, or physical examination-indicated cerclage were grouped together, and the indications leading to cerclage placement and the appropriateness of cerclage placement could not be stratified further and evaluated because of the lack of specification in the data registry. In addition, we acknowledge the limited sample size of patients with morbid obesity with a cervical cerclage and the requirement for performing bootstrapping. We cannot fully determine the risk in this unique group and more studies would be needed to further elucidate this. Lastly, given the retrospective cohort study design, the findings should be interpreted within its limitation. As such, the findings may not necessarily establish causation between obesity and preterm delivery in the cerclage population, and thus, further randomized control trials are needed to evaluate this role.
Conclusion
Maternal obesity is not associated with an increased risk for spontaneous preterm delivery. Patients with obesity and morbid obesity should be reassured that cerclage does not seem to be differentially efficacious in preventing spontaneous preterm labor in this group when compared with cerclage in their counterparts without obesity, but they should be aware that they are still at risk for overall preterm delivery because of other gestational complications.
Footnotes
The authors report no conflict of interest.
Patient consent was not required because no personal information or details were included.
Cite this article as: Nguyen HY, Park B, Rossi J, et al. Impact of maternal obesity on preterm delivery in patients with cervical cerclage. Am J Obstet Gynecol Glob Rep 2023;XX:x.ex–x.ex.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2023.100211.
Appendix. Supplementary materials
References
- 1.Abrams BF, Laros RK. Prepregnancy weight, weight gain, and birth weight. Am J Obstet Gynecol. 1986;154:503–509. doi: 10.1016/0002-9378(86)90591-0. [DOI] [PubMed] [Google Scholar]
- 2.Naeye RL. Maternal body weight and pregnancy outcome. Am J Clin Nutr. 1990;52:273–279. doi: 10.1093/ajcn/52.2.273. [DOI] [PubMed] [Google Scholar]
- 3.Taffel SM, Keppel KG, Jones GK. Medical advice on maternal weight gain and actual weight gain. Results from the 1988 national maternal and infant health survey. Ann N Y Acad Sci. 1993;678:293–305. doi: 10.1111/j.1749-6632.1993.tb26132.x. [DOI] [PubMed] [Google Scholar]
- 4.Cogswell ME, Serdula MK, Hungerford DW, Yip R. Gestational weight gain among average-weight and overweight women - what is excessive? Am J Obstet Gynecol. 1995;172:705–712. doi: 10.1016/0002-9378(95)90598-7. [DOI] [PubMed] [Google Scholar]
- 5.Kumari AS. Pregnancy outcome in women with morbid obesity. Int J Gynaecol Obstet. 2001;73:101–107. doi: 10.1016/s0020-7292(00)00391-x. [DOI] [PubMed] [Google Scholar]
- 6.Greer IA. Anticoagulants in pregnancy. J Thromb Thrombolysis. 2006;21:57–65. doi: 10.1007/s11239-006-5578-5. [DOI] [PubMed] [Google Scholar]
- 7.Nohr EA, Bech BH, Davies MJ, Frydenberg M, Henriksen TB, Olsen J. Prepregnancy obesity and fetal death: a study within the Danish National Birth Cohort. Obstet Gynecol. 2005;106:250–259. doi: 10.1097/01.AOG.0000172422.81496.57. [DOI] [PubMed] [Google Scholar]
- 8.Vahratian A, Siega-Riz AM, Savitz DA, Zhang J. Maternal pre-pregnancy overweight and obesity and the risk of cesarean delivery in nulliparous women. Ann Epidemiol. 2005;15:467–474. doi: 10.1016/j.annepidem.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Yao R, Schuh BL, Caughey AB. The risk of perinatal mortality with each week of expectant management in obese pregnancies. J Matern Fetal Neonatal Med. 2019;32:434–441. doi: 10.1080/14767058.2017.1381903. [DOI] [PubMed] [Google Scholar]
- 10.Browne K, Park BY, Goetzinger KR, Caughey AB, Yao R. The joint effects of obesity and pregestational diabetes on the risk of stillbirth. J Matern Fetal Neonatal Med. 2021;34:332–338. doi: 10.1080/14767058.2019.1607287. [DOI] [PubMed] [Google Scholar]
- 11.Yogev Y, Catalano PM. Pregnancy and obesity. Obstet Gynecol Clin North Am. 2009;36 doi: 10.1016/j.ogc.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Salihu H, Mbah AK, Alio AP, et al. Nulliparity and preterm birth in the era of obesity epidemic. J Matern Fetal Neonatal Med. 2010;23:1444–1450. doi: 10.3109/14767051003678044. [DOI] [PubMed] [Google Scholar]
- 13.Räisänen S, Gissler M, Saari J, Kramer M, Heinonen S. Contribution of risk factors to extremely, very and moderately preterm births - register-based analysis of 1,390,742 singleton births. PLoS One. 2013;8:e60660. doi: 10.1371/journal.pone.0060660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. 2014;345:760–765. doi: 10.1126/science.1251816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cobo T, Kacerovsky M, Jacobsson B. Risk factors for spontaneous preterm delivery. Int J Gynaecol Obstet. 2020;150:17–23. doi: 10.1002/ijgo.13184. [DOI] [PubMed] [Google Scholar]
- 16.Gyamfi-Bannerman C, Ananth CV v. Trends in spontaneous and indicated preterm delivery among singleton gestations in the United States, 2005-2012. Obstet Gynecol. 2014;124:1069–1074. doi: 10.1097/AOG.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 17.Gracie S, Pennell C, Ekman-Ordeberg G, et al. An integrated systems biology approach to the study of preterm birth using “-omic” technology - a guideline for research. BMC Pregnancy Childbirth. 2011;11:71. doi: 10.1186/1471-2393-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hendler I, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: association between maternal body mass index and spontaneous and indicated preterm birth. Am J Obstet Gynecol. 2005;192:882–886. doi: 10.1016/j.ajog.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 19.Smith GCS, Shah I, Pell JP, Crossley JA, Dobbie R. Maternal obesity in early pregnancy and risk of spontaneous and elective preterm deliveries: a retrospective cohort study. Am J Public Health. 2007;97:157–162. doi: 10.2105/AJPH.2005.074294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hehir MP, Glavey SV v., Morrison JJ. Uterorelaxant effect of ghrelin on human myometrial contractility. Am J Obstet Gynecol. 2008;198:323. doi: 10.1016/j.ajog.2007.09.040. .e1–5. [DOI] [PubMed] [Google Scholar]
- 21.Wallenstein MB, Jelliffe-Pawlowski LL, Yang W, et al. Inflammatory biomarkers and spontaneous preterm birth among obese women. J Matern Fetal Neonatal Med. 2016;29:3317–3322. doi: 10.3109/14767058.2015.1124083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McDonald SD, Han Z, Mulla S, Beyene J. Knowledge Synthesis Group. Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta-analyses. BMJ. 2010;341:c3428. doi: 10.1136/bmj.c3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torloni MR, Betrán AP, Daher S, et al. Maternal BMI and preterm birth: a systematic review of the literature with meta-analysis. J Matern Fetal Neonatal Med. 2009;22:957–970. doi: 10.3109/14767050903042561. [DOI] [PubMed] [Google Scholar]
- 24.Cnattingius S, Villamor E, Johansson S, et al. Maternal obesity and risk of preterm delivery. JAMA. 2013;309:2362–2370. doi: 10.1001/jama.2013.6295. [DOI] [PubMed] [Google Scholar]
- 25.Prodromidou A, Frountzas M, Perrea D, Vlachos GD, Pergialiotis V. The impact of obesity on cervical cerclage efficacy: a systematic review of the literature. J Neonatal Perinatal Med. 2016;9:59–65. doi: 10.3233/NPM-16915058. [DOI] [PubMed] [Google Scholar]
- 26.Suhag A, Seligman N, Giraldo-Isaza M, Berghella V. Pre-pregnancy body mass index (BMI) and cerclage success. J Matern Fetal Neonatal Med. 2016;29:368–375. doi: 10.3109/14767058.2015.1006622. [DOI] [PubMed] [Google Scholar]
- 27.Poggi SH, Vyas NA, Pezzullo JC, Landy HJ, Ghidini A. Does increasing body mass index affect cerclage efficacy? J Perinatol. 2012;32:777–779. doi: 10.1038/jp.2011.198. [DOI] [PubMed] [Google Scholar]
- 28.Frezza EE, Shebani KO, Robertson J, Wachtel MS. Morbid obesity causes chronic increase of intraabdominal pressure. Dig Dis Sci. 2007;52:1038–1041. doi: 10.1007/s10620-006-9203-4. [DOI] [PubMed] [Google Scholar]
- 29.Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342:1500–1507. doi: 10.1056/NEJM200005183422007. [DOI] [PubMed] [Google Scholar]
- 30.Romero R, Gomez R, Ghezzi F, et al. A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am J Obstet Gynecol. 1998;179:186–193. doi: 10.1016/s0002-9378(98)70271-6. [DOI] [PubMed] [Google Scholar]
- 31.Soltani H, Fraser RB. A longitudinal study of maternal anthropometric changes in normal weight, overweight and obese women during pregnancy and postpartum. Br J Nutr. 2000;84:95–101. doi: 10.1017/s0007114500001276. [DOI] [PubMed] [Google Scholar]
- 32.Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S. Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes. 2007;56:1010–1013. doi: 10.2337/db06-1656. [DOI] [PubMed] [Google Scholar]
- 33.Ellulu MS, Patimah I, Khaza'ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13:851–863. doi: 10.5114/aoms.2016.58928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;15:2792–2800. doi: 10.1097/01.ASN.0000141966.69934.21. [DOI] [PubMed] [Google Scholar]
- 35.Ramsay JE, Ferrell WR, Crawford L, Wallace AM, Greer IA, Sattar N. Maternal obesity is associated with dysregulation of metabolic, vascular, and inflammatory pathways. J Clin Endocrinol Metab. 2002;87:4231–4237. doi: 10.1210/jc.2002-020311. [DOI] [PubMed] [Google Scholar]
- 36.Kindinger LM, MacIntyre DA, Lee YS, et al. Relationship between vaginal microbial dysbiosis, inflammation, and pregnancy outcomes in cervical cerclage. Sci Transl Med. 2016;8:350ra102. doi: 10.1126/scitranslmed.aag1026. [DOI] [PubMed] [Google Scholar]
- 37.Hodgetts Morton V, Toozs-Hobson P, Moakes CA, et al. Monofilament suture versus braided suture thread to improve pregnancy outcomes after vaginal cervical cerclage (C-STICH): a pragmatic randomised, controlled, phase 3, superiority trial. Lancet. 2022;400:1426–1436. doi: 10.1016/S0140-6736(22)01808-6. [DOI] [PubMed] [Google Scholar]
- 38.Figueroa R, Crowell R, Martinez A, Morgan M, Wakefield D. McDonald versus Shirodkar cervical cerclage for the prevention of preterm birth: impact of body mass index. J Matern Fetal Neonatal Med. 2019;32:3408–3414. doi: 10.1080/14767058.2018.1465037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.