Abstract
Life-course theories on how social relationships affect mental health are limited in causal claims. The restrictions in social contact during the coronavirus pandemic provided a natural experiment that modified the frequency of in-person contact and allowed us to estimate the effect of changes in in-person social contact frequency on mental health in four large nationally representative age-cohorts of adults living in the UK. There was consistent evidence of a small but statistically significant effect of less frequent social contact on anxiety-depression. Online modes of social contact did not compensate for the restrictions in in-person social contact during the pandemic. Young adults who increased their online social media frequency during the pandemic experienced a deterioration in mental health. Life-course theories cannot ignore the importance of the mode of social contact for social relationships, especially during young adulthood.
Keywords: anxiety, causal, COVID-19, depression, instrumental variables, mental health, pandemic social-convoy model, social media, social relationships
The COVID-19 pandemic changed the way people interacted socially. Lockdowns and social distancing guidelines meant that people were restricted, at various times, in meeting others outside of their household in-person (‘household mixing’). There was some suggestion that online or telephone modes of social contact could compensate for the loss of in-person social contact in terms of preserving well-being. This study examined whether changes in social contact during the first year of the pandemic in the UK caused changes in mental health. We used the pandemic ‘natural experiment’ that induced changes in the way people interacted socially, to analyse how those changes in the mode of social interaction affected the mental health of adults living in the UK. This allowed us to draw causal inferences from the estimated effect of social relationships on mental health, addressing a key gap in existing research.
The pandemic adversely affected the mental health of populations (Patel et al., 2022; Prati and Mancini, 2021; Robinson et al., 2022), and in particular, adolescents and young adults (Niedzwiedz et al., 2021; Patel et al., 2022; Racine et al., 2021). There was a small but statistically significant increase in mental health symptoms in the early stages of the pandemic (March–April 2020), that declined in the following months (May–June 2020) (Prati and Mancini, 2021; Robinson et al., 2022). The lifting of the ‘Stay at Home’ order in England and Scotland improved mental health, after a large deterioration following the onset of the pandemic (Serrano-Alarcon et al., 2022). Some studies suggested that the mental health and well-being benefits of in-person social interactions could be replaced by digital and online social contact (David and Roberts, 2021; Pancani et al., 2021), although other studies did not find evidence of such compensation (Hawkley et al., 2021; Hu and Qian, 2021b). Moreover, other research suggested that the increase in mental health symptoms in the early part of the pandemic was more related to the perceived risk of infection and death, unemployment and financial worries (Robinson and Daly, 2021), and the burden of childcare and home-schooling (Chandola et al., 2022).
We first described how changes in in-person social contact (outside the household) affected the mental health of UK adults in the first year of the COVID-19 pandemic, and then examined whether these effects were moderated by changes in telephone and digital modes of social contact. We found little evidence to support the idea that online modes of social contact could compensate for the restrictions in in-person social contact during the pandemic. We also described whether there were differences in the effect of social contact across age-cohorts, as the youngest adults are known to have suffered the most in terms of their mental health both before and during the pandemic (Gagne et al., 2022). The key contribution of this study is the use of regional by period differences as exogenous determinants of changes in in-person social contact, to identify a causal effect of in-person social contact on mental health. This allowed us to show that while there was a causal effect of a reduction in in-person social contact on poorer mental health, this effect was small.
Theoretical Background and Hypotheses
House et al. (1988) argued that the lack of social relationships was just as important a risk factor for poor health as smoking, blood pressure, obesity and physical activity. A meta-analysis of 148 studies later concluded that the influence of social relationships on risk for mortality is comparable with well-established risk factors for mortality (Holt-Lundstad et al., 2010). The theoretical underpinnings of these associations come from life-course theories on social relationships and health, and in particular, Kahn and Antonucci’s (1980) social convoy theory. This theory conceptualised social relationships as a convoy in which individuals are surrounded by supportive others who move with them throughout the life-course. Key features of social relationships include the structural aspects of the social network, the exchange of support within relationships and the perceived quality of relationships. These relationships vary in their closeness, their quality, their function and their structure, and have been shown to influence health and well-being.
A key limitation of the social convoy model is the lack of consideration on changing modes of social interaction. The theory was developed prior to technological developments that enabled cheap and easy modes of remote social contact. The role of technology (internet, smartphones and social media) is now explicitly considered in an update of the theory (Antonucci et al., 2019). However, the theory remains equivocal about the impact of changing modes of social interaction on health and well-being, highlighting the potential for positive effects (such as the maintenance of strong ties over long distances) as well as negative effects (such as through the isolating nature of some social media).
Moreover, there is a lack of adequate consideration of the different typologies of digital social contact. In contrast to in-person, one-to-one and synchronous modes of social contact, digital and phone modes of social interaction can be one-to-one or one-to-many, as well as synchronous or asynchronous modes of communication. Each of these modes may have different effects on well-being, given the diversity in feedback (instant vs. delayed) and the presence or absence of complex non-verbal cues, such as facial expressions, gazes and gestures (Frith, 2009).
There is considerable debate around whether digital online social interactions (through social media platforms) have positive or negative effects on mental well-being, especially among adolescents and young adults (Valkenburg et al., 2022), but also in the older adult population (Stuart et al., 2022). Interactions online may not provide the same benefits to well-being as face-to-face interactions because of limited communication feedback and cues (Yang et al., 2013). Moreover, social media could lead to greater opportunities for social comparisons and negative interactions such as cyberbullying, which could lead to negative and lower well-being (Kowalski et al., 2014). Furthermore, with a greater amount of time spent online, there is a risk of mental overload due to multi-tasking, and displacement of health promoting activities such as sleep and exercise, which can lower well-being (Klimmt et al., 2017).
On the other hand, online social contacts could lead to greater informational and network resources, representing a new form of social capital, which in turn is linked to greater well-being (Ellison et al., 2007). Early on in the pandemic, several commentators suggested that online communication modes and video technology in particular can bridge social distances during the pandemic (Galea et al., 2020) and compensate for the lack of face-to-face in-person social contact (David and Roberts, 2021; Pancani et al., 2021). People were reminded that the government guidelines stipulated ‘physical distancing, not social distancing’. Online communication technologies could reduce social isolation through developing social connections with new people, gaining social support and boosting self-confidence, particularly among older adults (Jutai and Tuazon, 2022). This leads to the idea of a ‘compensation’ model, in which those who lack social support and networks may profit most from digital online social interactions. The ‘poor get richer’ hypothesis posits that people with fewer social resources (and smaller in-person social networks) may generally be more comfortable interacting online than face-to-face, and will therefore benefit most from online communication (McKenna et al., 2002).
The need to examine whether digital and online modes of communication compensated for a reduction in in-person social contact during the pandemic leads us to our first hypothesis (H1 – the compensation hypothesis): the beneficial effect of maintaining social contact through phone/digital/online modes was greater among people with reduced in-person social contact. We expect to find evidence of a significant interaction between in-person social contact and phone/digital/online contact modes in their effects on mental health.
An additional criticism of the social convoy model is that the empirical analysis has often been restricted to later life. We have previously shown that social relationships in early adulthood have a greater impact on stress and health compared with later life (Rouxel et al., 2022). Furthermore, the pandemic had much larger effects on the mental health of young adults compared with older adults, with young adults already having poorer levels of mental health before COVID-19 (Gagne et al., 2022; Knowles et al., 2022).
Adolescents and young adults who already had a high degree of social anxiety before the pandemic may not have been as adversely affected (in terms of mental health) by the pandemic restrictions in in-person social contact and the switch to digital and online modes of communication. Instead, it may be the young adults who changed their social contact behaviour to online modes because of the pandemic who may have suffered the most (‘rich get poorer’). There are also potential cohort differences in the effect of digital and online modes of communication on mental health, as digital communication modes may not suit older adults who have decreased internet access and lack digital communication skills. Older adults tend to use digital technology to maintain and preserve in-person relationships, rather than to make new connections. Moreover, while older adults may have increased their online modes of communication during the pandemic, this may not have compensated for their feelings of loneliness (Holaday et al., 2022). The debates around whether social media use and other forms of social contact have positive or negative effects on mental health that are different across age-cohorts leads us to our second hypothesis (H2 – the rich get poorer): young adults with weak pre-existing preferences for online social contact were more affected in terms of mental well-being by a reduction in in-person social contact during the pandemic compared with their age-peers with higher pre-pandemic online contact.
Another key limitation in the theoretical and empirical research on social relationships and health is a lack of causal analyses and in-depth consideration of simultaneous causation, reverse causality and unobserved confounding factors. Most studies on social relationships and health explicitly list reverse causation as a limitation. In longitudinal studies of social relationships and health that control for baseline health, there is an attempt to control for reverse causation. However, there may be other factors that drive the association between social relationships and future health that are not controlled for in observational analysis.
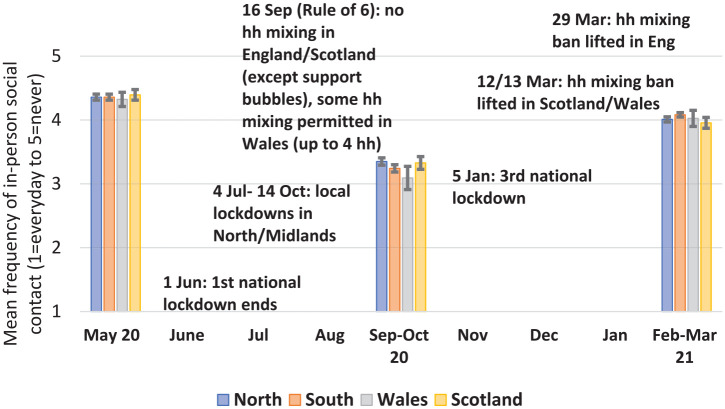
This study exploits the ‘natural experiment’ of regional differences in household mixing arising from pandemic-related government restrictions, to estimate the causal effect of social contact on mental health. The UK government and devolved authorities imposed a national lockdown on 23 March 2020, with residents across all regions and different countries of the UK required to stay at home except for essential reasons. These restrictions were in place during the period of the May 2020 survey of this study, when most people never met anyone outside their household and there were no regional differences in such contact (Figure 1). Restrictions in social contact were steadily eased across the UK in the summer, although there were much stricter restrictions in social contact (‘household mixing’) for residents in the north of England. This resulted in an increase in household mixing during the September–October survey compared with the May survey although adults in the north of England were more likely to never meet anyone outside their household. In England, household mixing was prohibited once again on 5 January 2021 until 29 March 2021, whereas the lifting of this ban was a little earlier in Scotland (on 12 March) and Wales (13 March). The period from May 2020 to March 2021 thus coincided with a reduction in government restrictions in household mixing by September–October 2020, although with considerably more restrictions in the north of England, as well as a subsequent return to greater restrictions in household mixing in all regions and countries in the first months of 2021.
Figure 1.
Mean (95% confidence intervals) of in-person social contact in the north of England, the south of England, Wales and Scotland from May 2020 to March 2021.
The need for stronger causal evidence for the association between social relationships and mental health leads us to our third hypothesis (H3 – causal hypothesis) – that the increase in poor mental health related to the decrease in in-person social contact is not affected by unmeasured time-varying confounding factors. Although all three hypotheses address the effect of social contact on mental health, it is only in the third hypothesis that we can weaken the assumptions around causal inference as we exploit the natural experiment of pandemic-related social restrictions. As these social restrictions targeted household mixing, we could not use the same natural experiment to examine hypotheses 1 and 2, which included other modes of social contact.
Methods
Data
The Centre for Longitudinal Studies carried out three surveys of the participants of four national longitudinal cohort studies during the coronavirus pandemic (Brown et al., 2021). The wave 1 survey was carried out at the height of lockdown restrictions in May 2020. The wave 2 survey was conducted in September/October 2020, a period when restrictions were lifted in some places. The wave 3 survey took place in February/March 2021, during the third UK lockdown. These studies follow large nationally representative groups of people since birth in the UK, and their ages ranged from 19 through to 63:
Millennium Cohort Study (MCS) (born 2000–2002) who were aged between 19 and 21 years;
Next Steps (born 1989–1990) who were aged 31–32 years;
1970 British Cohort Study (BCS70), who were 51 years;
1958 National Child Development Study (NCDS), who were aged 63 years.
The data are available for researchers to download from the UK Data Service. Further details on the studies and sampling design are detailed in Supplemental file S1.
Variables
Dependent Variables
A scale of anxiety and depression was created by combining responses to questions from the GAD-2 (Generalised Anxiety Disorder 2-item) (Kroenke et al., 2007) and the PHQ-2 (Patient Health Questionnaire 2-item) (Kroenke et al., 2003). The GAD-2 is a brief screening tool for generalised anxiety disorder with questions on ‘feeling nervous, anxious or on edge’ and ‘not being able to stop or control worrying’ over the last two weeks. The PHQ-2 enquires about the frequency of depressed mood and anhedonia with questions on ‘little interest or pleasure in doing things’ and ‘feeling down, depressed or hopeless’ over the last two weeks. Responses for both the GAD-2 and the PHQ-2 ranged from 1 (not at all), 2 (several days), 3 (more than half the days) and 4 (nearly every day). The alpha scale reliability coefficient of the four items was 0.88 at each wave. The mean of the four items at each wave was generated with a range from 1 to 4 with higher values indicating greater anxiety and depression.
The Kessler scale (Kessler et al., 2003) is a quantifier of non-specific psychological distress (only available in the MCS cohort). It consists of six questions about depressive and anxiety symptoms that a person has experienced in the last 30 days. Responses ranged from 1 (all of the time) to 5 (none of the time). The mean of the six items at each wave was generated with a range from 1 to 5 with higher values indicating greater psychological distress.
Independent Variables (Details in Online Supplemental Files S2 and S3)
Respondents were asked about the frequency of different modes of social contact: ‘In the last seven days, did you:
(1) meet up in-person with any of your family or friends who do not live with you;
(2) talk to family or friends who do not live with you via phone or video calls;
(3) keep in contact with family or friends you do not live with by email or text or other electronic messaging;
(4) take part in an online community activity, e.g. an online community group, online chat group, street or neighbourhood social media group?’
Respondents chose options between every day, 4–6 days, 2–3 days, 1 day and never. There was little correlation between the different modes of social contact except for some moderate correlation (around 0.45) between talking to family/friends via video or phone and contact by electronic message (see Supplemental file S2).
Pre-pandemic social media use frequency (MCS cohort only): respondents were asked ‘on a normal weekday, how many hours do you spend on social networking or messaging sites or apps on the internet such as Facebook, Twitter, WhatsApp, Instagram and Snapchat?’ Response categories included none, <30 minutes, 30–60 minutes, 1–2 hours, 2–3 hours, 3–5 hours, 5–7 hours, 7–10 hours, >10 hours. This was coded into a binary variable of less than 2 hours a day (28%) to 2 or more hours a day (72%). On average, people spend 2.5 hours a day on social media although younger people spend much more time on social media. A relatively low cut-off for daily social media use (at 2 hours) was chosen to identify a group of young adults who prior to the pandemic did not engage much with social media.
Covariates were chosen based on factors that have previously been associated with poor mental health during the pandemic and that could confound the effect of social contact on mental health (Chandola et al., 2022; Patel et al., 2022). COVID-19 symptoms and testing positive for COVID-19 were measured. Respondents were asked about their financial situation, comparing their current financial situation with before the coronavirus outbreak in terms of whether they were worse off, a little worse off, about the same, a little better off or much better off. They were also asked if they were a ‘key worker’, or if their work had been classified as critical to the COVID-19 response. Self-rated health was measured by responses to their rating of health as excellent, very good, good, fair or poor. This was coded into a binary variable of good health (excellent/very good) and poor health (good to poor). Household size was coded into people living alone or with others in the house.
Statistical Analyses
All statistical analyses were carried out in Stata (v14). The distribution of the anxiety-depression scale at each wave by the independent variables was examined. We used fixed effects linear regression models for H1 and H2 to analyse the effect of within person changes in the frequency of mode of social contact and the covariates on changes in anxiety-depression. Robust standard errors were used to adjust model-based standard errors to allow for violations of linear regression model assumptions that include homoscedasticity and normality of the errors (Mansournia et al., 2021). In Stata, xtreg fits regression models to panel data – see Online Supplemental file S1.1 for more details. Fixed effect models eliminate bias from time constant confounders, but time varying confounding could still bias estimates from these models. Moreover, strict exogeneity (e.g. the absence of reverse causation) is assumed.
To examine H1, we examined evidence for an interaction effect between in-person social contact and phone/digital/online modes of social contact. A smaller effect of in-person social contact on mental health among those who frequently used phone/digital/online modes of social contact more frequently would suggest some evidence for the compensation hypothesis.
For H2, we first examined whether there were any differences between the age-cohorts in the effect of the mode of social contact on mental health by stratifying the fixed effects models by age-cohort. A statistical test of interaction of age-cohort with mode of social contact was examined to see if there were significant differences in the pattens of mental health by age-group. We also analysed the youngest age-group (from MCS) separately; we examined whether there was a difference in the estimates of mental health from the fixed effects models for those with and without a preference for online social contact.
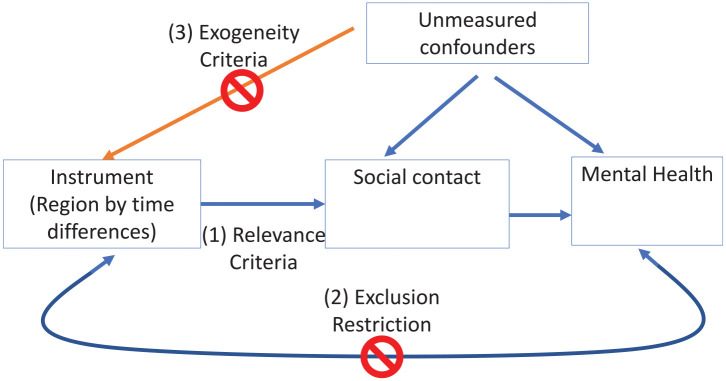
For H3, we conducted an instrumental variable analysis. An instrumental variable (IV) is a variable (Z) that is highly correlated with one of the independent variables (X) but is uncorrelated with the error term (Angrist et al., 1996). In Stata, xtivreg with the fe option uses the two-stage least-squares within estimator for fitting panel-data models in which some of the right-hand-side covariates are endogenous – see Figure 2 for an illustration.
Figure 2.
Criteria of instrumental variables models.
In Online Supplemental file S5.1 we detail how policy changes in household mixing across the pandemic and between the countries and regions of the UK affected the frequency of in-person social contact during the period May 2020 to March 2021. We argue that the pandemic-related social restrictions are a natural experiment that changed mode of social contact in the UK during the pandemic. We argue that this country/regional by time variation in social restriction policies had a causal effect on in-person social contact (the relevance criteria). The allocation of people to different treatment (policy) regimes is independent of other causes of mental health (exogeneity criteria).
In the IV analysis, there was one endogenous regressor (meeting up in-person with non-household people in the last week), and three instrumental variables used in the first stage. The instrumental variables were three dummy variables to indicate whether the observation was drawn from a wave 2 sample respondent living in either the south of England, Wales and Scotland, with the reference being an observation from either wave 1 or wave 3, or a person living in the north of England. The instrumental variables thus distinguish between people living in the north of England at wave 2, who were subject to greater restrictions in household mixing, and other regions/countries and periods.
Weights
The data depositors have calculated longitudinal weights that take account of the sample selection (design weights) as well as correct for non-response in the COVID-19 wave 1, 2 and 3 surveys. Most of the missing data in the samples at waves 1 and 2 was because of the application of the longitudinal wave 3 weights (Online Supplemental file S6 details missing data in the analytical sample and how the weights compensated for unit and item non-response). For the purposes of weighting, the target population of each cohort was defined as individuals born in the specified birth period of the cohort who are alive and still residing in the UK (Online Supplemental file S1). Details of the derivation of the weights are shown in the user guide (Brown et al., 2021). The longitudinal wave 3 weights were applied in all the descriptive statistics, fixed effects models and instrumental variables models.
Results
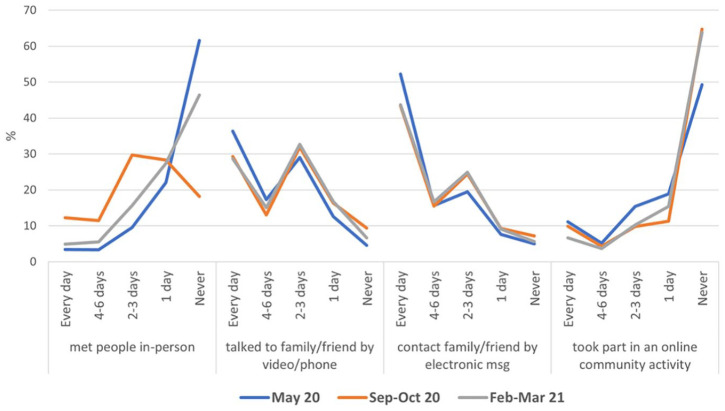
The mean (SD) of the anxiety-depression scale by the key variables in the analyses at each wave is presented in Table 1. The highest levels of anxiety-depression at any wave were among those who never met any family/friends (outside home) during the pandemic. Figure 3 illustrates the changing distribution of (the infrequency of) in-person social contact by wave, with the wave 2 line being much flatter compared with the steep increasing lines at waves 1 and 3. However, the distribution of the other (in)frequency of social contact variables by video/phone, email/text or social media use did not change much from May 2020 to February–March 2021.
Table 1.
Mean (SD) of anxiety-depression (range: 1–4) by mode of social contact and covariates.
| May 20 | n | Sep–Oct 20 | n | Feb–Mar 21 | n | |
|---|---|---|---|---|---|---|
| Met people in-person | ||||||
| Every day | 1.46 (0.64) | 267 | 1.52 (0.70) | 1510 | 1.61 (0.77) | 669 |
| 4–6 days | 1.41 (0.64) | 342 | 1.52 (0.66) | 1887 | 1.57 (0.70) | 833 |
| 2–3 days | 1.47 (0.63) | 972 | 1.52 (0.67) | 4788 | 1.59 (0.71) | 2413 |
| 1 day | 1.49 (0.64) | 2283 | 1.57 (0.71) | 3997 | 1.58 (0.70) | 4181 |
| Never | 1.54 (0.70) | 6375 | 1.63 (0.78) | 2237 | 1.63 (0.76) | 7032 |
| Talked to family/friend via video/phone | ||||||
| Every day | 1.53 (0.69) | 3777 | 1.58 (0.73) | 3947 | 1.62 (0.75) | 4293 |
| 4–6 days | 1.47 (0.63) | 1843 | 1.51 (0.66) | 2171 | 1.54 (0.68) | 2275 |
| 2–3 days | 1.49 (0.65) | 3118 | 1.50 (0.65) | 4737 | 1.57 (0.70) | 4988 |
| 1 day | 1.56 (0.71) | 1148 | 1.57 (0.72) | 2350 | 1.65 (0.76) | 2545 |
| Never | 1.70 (0.83) | 353 | 1.68 (0.78) | 1214 | 1.77 (0.86) | 1027 |
| Contacted family/friend by electronic message (msg) | ||||||
| Every day | 1.58 (0.70) | 5630 | 1.62 (0.74) | 6519 | 1.67 (0.76) | 6891 |
| 4–6 days | 1.46 (0.64) | 1685 | 1.49 (0.65) | 2536 | 1.56 (0.70) | 2556 |
| 2–3 days | 1.42 (0.63) | 1914 | 1.48 (0.65) | 3394 | 1.53 (0.69) | 3647 |
| 1 day | 1.44 (0.64) | 628 | 1.49 (0.66) | 1178 | 1.54 (0.72) | 1272 |
| Never | 1.50 (0.74) | 382 | 1.58 (0.78) | 792 | 1.60 (0.80) | 762 |
| Took part in an online community activity | ||||||
| Every day | 1.52 (0.66) | 1100 | 1.63 (0.74) | 1252 | 1.69 (0.77) | 981 |
| 4–6 days | 1.53 (0.68) | 588 | 1.57 (0.69) | 584 | 1.58 (0.65) | 577 |
| 2–3 days | 1.49 (0.63) | 1777 | 1.56 (0.67) | 1493 | 1.57 (0.67) | 1596 |
| 1 day | 1.50 (0.67) | 2106 | 1.53 (0.66) | 1852 | 1.56 (0.70) | 2377 |
| Never | 1.53 (0.70) | 4668 | 1.54 (0.71) | 9238 | 1.62 (0.75) | 9597 |
| Sex | ||||||
| Male | 1.44 (0.02) | 6205 | 1.47 (0.02) | 4654 | 1.50 (0.02) | 5397 |
| Female | 1.68 (0.02) | 6386 | 1.65 (0.02) | 5021 | 1.71 (0.02) | 5891 |
| COVID symptoms | ||||||
| No | 1.52 (0.01) | 9860 | 1.52 (0.01) | 9257 | 1.57 (0.01) | 9385 |
| Yes | 1.71 (0.03) | 2593 | 1.81 (0.04) | 1558 | 1.84 (0.04) | 1898 |
| Tested positive for COVID-19 | ||||||
| No | 1.56 (0.01) | 12,457 | 1.59 (0.01) | 16,984 | 1.64 (0.01) | 18,380 |
| Yes | 2.07 (0.4) | 50 | 1.64 (0.08) | 261 | 1.71 (0.04) | 1611 |
| Self-rated health | ||||||
| Excellent/Very Good | 1.40 (0.01) | 6740 | 1.39 (0.01) | 5916 | 1.42 (0.01) | 5605 |
| Good–Poor | 1.75 (0.02) | 5851 | 1.77 (0.02) | 4914 | 1.8 (0.02) | 5680 |
| Finances | ||||||
| Much worse off | 1.82 (0.05) | 1173 | 1.95 (0.06) | 841 | 1.98 (0.05) | 1161 |
| A little worse off | 1.6 (0.03) | 2910 | 1.62 (0.03) | 1865 | 1.66 (0.03) | 2027 |
| About the same | 1.53 (0.02) | 5841 | 1.53 (0.02) | 5701 | 1.56 (0.02) | 5022 |
| A little better off | 1.48 (0.02) | 2156 | 1.48 (0.03) | 1951 | 1.54 (0.03) | 2331 |
| Much better off | 1.49 (0.03) | 478 | 1.49 (0.05) | 458 | 1.51 (0.03) | 731 |
| Household (hh) size | ||||||
| More than 1 person | 1.56 (0.01) | 10,478 | 1.56 (0.01) | 8863 | 1.62 (0.01) | 9192 |
| Single person hh | 1.58 (0.03) | 2103 | 1.56 (0.03) | 1935 | 1.59 (0.04) | 2065 |
| Keyworker | ||||||
| Not in paid work | 1.66 (0.02) | 7281 | 1.75 (0.02) | 7176 | 1.82 (0.02) | 9352 |
| Keyworker | 1.46 (0.02) | 2837 | 1.49 (0.02) | 4627 | 1.53 (0.02) | 5862 |
| Not a keyworker | 1.39 (0.02) | 2396 | 1.45 (0.02) | 5430 | 1.47 (0.02) | 4717 |
Figure 3.
Trends in social contact, May 2020 to February–March 2021.
Table 2 shows the results of the fixed effects models predicting anxiety-depression by the social contact variables. In Model 1, a decrease in in-person social contact was associated with an increase in anxiety-depression. People who reduced their in-person social contact from four to six days/week to never had an increase of 0.04 (95% CI: 0.02–0.06) in anxiety-depression (Model 1). The effect of in-person social contact did not change when controlling for the other social contact variables (Model 2) or covariates (Model 3). Poor self-rated health, testing positive for COVID-19 and being financially much worse off during the pandemic increased levels of anxiety-depression. The size of the reduction in in-person social contact on poor mental health (0.04) was half that of the effect of poor self-rated health (0.08) and nearly a quarter of the effect of going from a very good to a very poor financial position (0.15).
Table 2.
Estimates (95% CI) of anxiety-depression from fixed effect models with mode of social contact and covariates.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Met people in-person (ref: 4–6 days) | |||
| Every day | 0.02 (−0.01, 0.05) | 0.02 (−0.01, 0.05) | 0.02 (−0.01, 0.05) |
| 2–3 days | 0.03 (0.004, 0.05) | 0.03 (0.004, 0.05) | 0.02 (0.003, 0.05) |
| 1 day | 0.04 (0.02, 0.06) | 0.04 (0.02, 0.06) | 0.04 (0.02, 0.06) |
| Never | 0.04 (0.02, 0.06) | 0.04 (0.02, 0.06) | 0.04 (0.02, 0.06) |
| Talked to family/friend via video/phone (ref: Every day) | |||
| 4–6 days | −0.003 (−0.02, 0.02) | −0.004 (−0.02, 0.02) | |
| 2–3 days | 0.003 (−0.02, 0.02) | 0.002 (−0.02, 0.02) | |
| 1 day | 0.03 (0.01, 0.06) | 0.03 (0.01, 0.06) | |
| Never | 0.04 (0.003, 0.07) | 0.04 (0.003, 0.07) | |
| Contacted family/friend by electronic msg (ref: Every day) | |||
| 4–6 days | 0.001 (−0.02, 0.02) | 0.001 (−0.02, 0.02) | |
| 2–3 days | <0.001 (−0.02, 0.02) | <0.001 (−0.02, 0.02) | |
| 1 day | 0.01 (−0.02, 0.04) | 0.01 (−0.02, 0.04) | |
| Never | −0.01 (−0.04, 0.02) | −0.01 (−0.05, 0.02) | |
| Took part in an online community activity (ref: Every day) | |||
| 4–6 days | <0.001 (−0.03, 0.03) | −0.003 (−0.03, 0.03) | |
| 2–3 days | −0.01 (−0.04, 0.01) | −0.02 (−0.04, 0.01) | |
| 1 day | 0.01 (−0.02, 0.03) | 0.01 (−0.02, 0.03) | |
| Never | 0.01 (−0.01, 0.04) | 0.01 (−0.01, 0.04) | |
| COVID infection (ref: no) | |||
| Yes | 0.01 (−0.01, 0.03) | ||
| Tested positive COVID-19 infection (ref: no) | |||
| Yes | 0.07 (0.04, 0.11) | ||
| Self-rated health (ref: Excellent/Very Good) | |||
| Good to Poor | 0.08 (0.06, 0.10) | ||
| Finances (ref: much worse off) | |||
| A little worse off | −0.09 (−0.13, −0.06) | ||
| About the same | −0.11 (−0.15, −0.08) | ||
| A little better off | −0.13 (−0.17, −0.09) | ||
| Much better off | −0.15 (−0.21, −0.09) | ||
| Household size (ref: more than 1 person) | |||
| Single person hh | 0.001 (−0.01, 0.01) | ||
| Keyworker (ref: not in work) | |||
| In work: keyworker | −0.01 (−0.04, 0.02) | ||
| In work: not keyworker | −0.01 (−0.03, 0.01) | ||
| Intercept | 1.51 (1.49, 1.52) | 1.49 (1.46, 1.52) | 1.57 (1.52, 1.61) |
| R-sq | 0.001 | 0.002 | 0.012 |
| within | 0.001 | 0.003 | 0.101 |
| between | 0.001 | 0.003 | 0.072 |
| n obs | 39,463 | 39,463 | 39,463 |
| n individuals | 16,090 | 16,090 | 16,090 |
| rho | 0.75 | 0.75 | 0.75 |
Note: Coefficients in bold indicate statistical significance at p < 0.05.
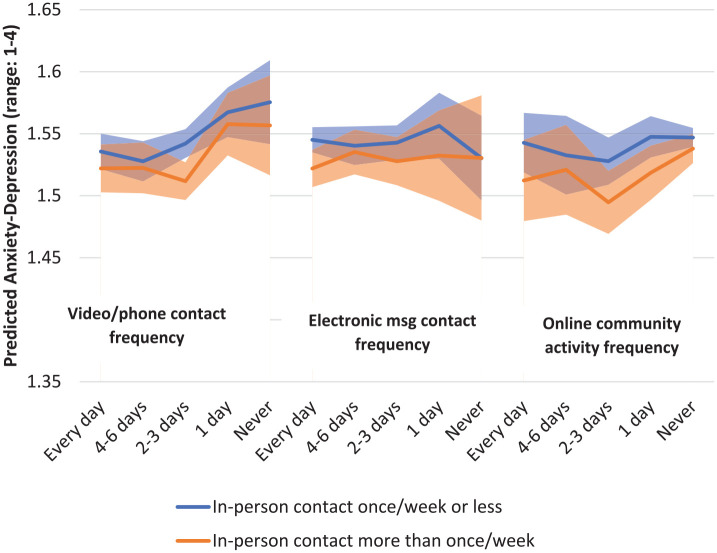
There was little evidence of a significant interaction between in-person social contact and the other social contact variables (Figure 4), suggesting no evidence for the compensation hypothesis (H1). We additionally tested the strict exogeneity assumption, which rules out feedback from the dependent variables to the explanatory variables. The weighted fixed effects models in Table 2 (Model 3) were re-estimated, this time including the explanatory variables lagged forward by one wave. The null hypothesis, that these lagged explanatory variables are strictly exogenous, was tested by examining the joint significance F-test of all the lagged variables. The significance of the F-test was 0.4, suggesting that there is no feedback observed and that the strict exogeneity assumption held.
Figure 4.
Predicted anxiety-depression (95% CI) derived by the interaction of in-person social contact with video/phone, electronic message and online community activity.
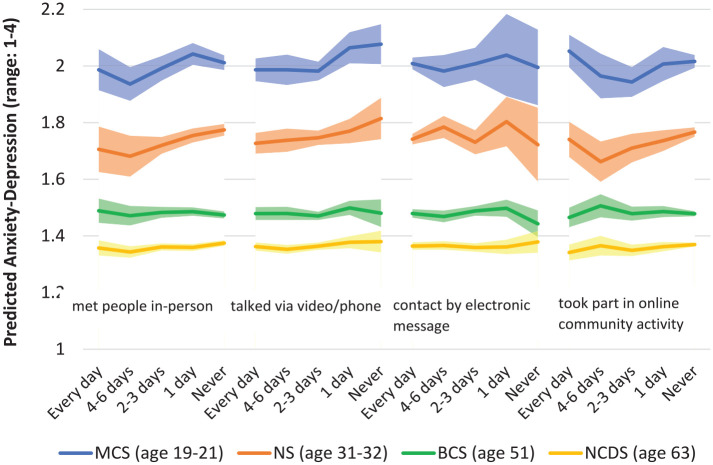
In Figure 5, we show the fixed effects estimates of the different modes of social contact on anxiety-depression by wave for each age-cohort. Some striking patterns can be observed. Firstly, the younger cohorts, particularly those aged around 20 years, had much higher levels of anxiety-depression. Moreover, the effect of less frequent in-person social contact and contact by video/phone on anxiety-depression appeared to be stronger in the younger compared with the older cohorts, although the formal test of statistical significance (the cohort by contact mode interaction) indicated that there was no statistical difference between the overall effects reported in Table 2 and the patterns observed in Figure 5 (see Online Supplemental file S7, Models 1 and 2). However, for frequency of social media use, a different U-shape pattern can be observed for the cohort aged 20, in contrast to the largely linear pattern observed for the other modes of social contact. Here, there was a statistically significant difference between the age-cohorts, with the effect of reducing social media frequency from daily to around two to six times a week being more negative (indicating better mental health) for the youngest age-cohort than the corresponding effect for those aged 62 (see Online Supplemental file S7, Model 4).
Figure 5.
Predicted anxiety-depression (95% CI) by mode of social contact and age-cohorts (see Supplemental file S7).
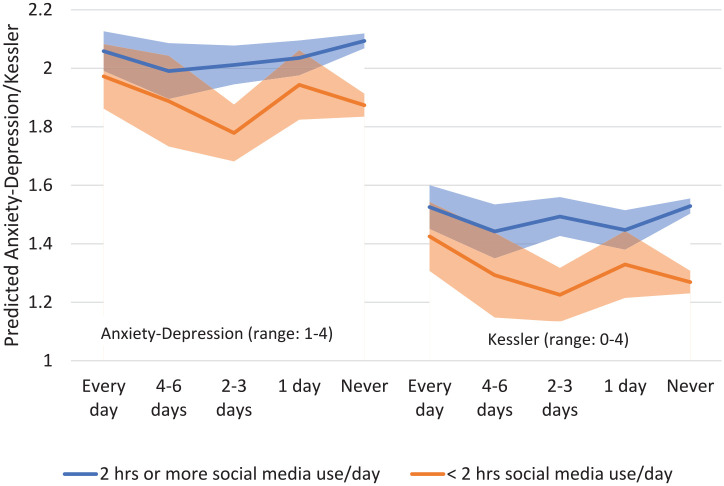
In Figure 6, we analyse just the youngest cohort aged 20. Restricting our analysis to this age-group enabled us to analyse an additional mental health measure, the Kessler psychological distress scale. Here, we examine the rich-get-poorer hypothesis (H2). Young adults who had lower social media use prior to the pandemic and daily social media use during the pandemic had the highest levels of anxiety-depression compared with young adults with similar (low) social media use prior to the pandemic but who only used social media two to three days a week. This was a pattern that was observed for both mental health variables. In contrast, for the young adults who had higher levels of social media use prior to the pandemic (greater than two hours a day), their social media use during the pandemic did not affect their mental health. Their mental health was consistently poorer (higher) than the group of young adults with lower social media use prior to the pandemic.
Figure 6.
Predicted Kessler scale and anxiety-depression (95% CI) by frequency of online community activity during the pandemic, stratified by pre-pandemic social media use hours among adults aged 20 (see Supplemental file S8).
H3 is examined in Table 3, which compares the coefficients from the fixed effects analysis of the effect of in-person social contact on anxiety-depression with the coefficients from the second stage of the IV analysis. The models analysed in Table 3 measure in-person social contact as a linear continuous variable. In the fixed effects model, a one unit increase in more frequent in-person social contact resulted in a 0.01 decrease in anxiety-depression. In the IV analysis, the endogenously predicted increase in in-person social contact resulted in a 0.02 decrease in anxiety-depression, with narrower confidence intervals compared with the fixed effects model. The larger IV estimates suggest stronger causal evidence of the effect of reduced in-person social contact on poorer mental health (H3).
Table 3.
Estimates (95% CI) from fixed effects (FE) models and second stage instrumental variable (IV) models predicting anxiety-depression.
| FE | Second stage IV | |
|---|---|---|
| Met people in-person more frequently (endogenous) | −0.01 (−0.01, −0.002) | |
| Predicted more frequent meetings in-person | −0.02 (−0.03, −0.01) | |
| Talked to family/friend via phone/video calls (ref: Every day) | ||
| 4−6 days | −0.005 (−0.02, 0.01) | −0.003 (−0.02, 0.02) |
| 2−3 days | 0.002 (−0.02, 0.02) | 0.002 (−0.02, 0.02) |
| 1 day | 0.03 (0.01, 0.06) | 0.03 (0.01, 0.06) |
| Never | 0.04 (0.01, 0.07) | 0.04 (0.01, 0.07) |
| Contact family/friend by electronic msg (ref: Every day) | ||
| 4−6 days | 0.002 (−0.01, 0.02) | 0.002 (−0.01, 0.02) |
| 2−3 days | 0.001 (−0.02, 0.02) | 0.001 (−0.02, 0.02) |
| 1 day | 0.01 (−0.02, 0.04) | 0.01 (−0.01, 0.04) |
| Never | −0.01 (−0.04, 0.03) | −0.01 (−0.04, 0.03) |
| Took part in an online community activity (ref: Every day) | ||
| 4−6 days | −0.004 (−0.03, 0.03) | −0.005 (−0.04, 0.03) |
| 2−3 days | −0.02 (−0.04, 0.01) | −0.02 (−0.04, 0.01) |
| 1 day | 0.005 (−0.02, 0.03) | 0.003 (−0.02, 0.03) |
| Never | 0.01 (−0.01, 0.04) | 0.01 (−0.01, 0.04) |
| COVID infection (ref: no) | ||
| Yes | 0.01 (−0.01, 0.03) | 0.01 (−0.01, 0.03) |
| Tested positive COVID−19 infection (ref: no) | ||
| Yes | 0.07 (0.03, 0.11) | 0.07 (0.03, 0.10) |
| Self-rated health (ref: Excellent/Very Good) | ||
| Good to Poor | 0.08 (0.06, 0.10) | 0.08 (0.06, 0.10) |
| Finances (ref: much worse off) | ||
| A little worse off | −0.09 (−0.13, −0.06) | −0.09 (−0.13, −0.06) |
| About the same | −0.11 (−0.15, −0.08) | −0.11 (−0.15, −0.08) |
| A little better off | −0.13 (−0.17, −0.09) | −0.13 (−0.17, −0.09) |
| Much better off | −0.15 (−0.21, −0.09) | −0.15 (−0.21, −0.10) |
| Household size (ref: more than 1 person) | ||
| Single person household | −0.01 (−0.03, 0.01) | −0.01 (−0.03, 0.01) |
| Keyworker (ref: not in work) | ||
| In work: keyworker | −0.01 (−0.04, 0.02) | −0.01 (−0.04, 0.02) |
| In work: not keyworker | −0.01 (−0.03, 0.01) | −0.004 (−0.03, 0.02) |
Note: Coefficients in bold indicate statistical significance at p < 0.05.
The assumptions and criteria of the IV analyses and sensitivity analyses are examined in Online Supplemental file S9.1. This shows strong evidence for the relevance criteria for instrumental variables analysis, little evidence of that the first stage equation is under identified and that the weak identification hypothesis can be rejected. The test for over-identification indicates little evidence against the null hypothesis, which is that the instruments are valid instruments. The lack of any country/region differences in anxiety-depression (Online Supplemental file S5.3) suggests that the exclusion restriction criteria holds. If there are no country/regional differences in anxiety-depression, the effect of changes in country/regional differences in household mixing policies on mental health is only through its effect on in-person social contact. We also conducted sensitivity analyses using cross-sectional instrumental variable models and found similar results to the panel models (Online Supplemental files S9.1 and S9.3).
Discussion
We found little evidence for the compensation hypothesis (H1). The reduction in mental health associated with reduced in-person social contact during the pandemic was not offset by online or telephone modes of social contact. Similar results have been found in the UK and the USA, albeit with limited data during the course of the pandemic and limited causal inference (Hu and Qian, 2021b). However, a reduction in phone/video contact was also associated with an increase in anxiety-depression, so there is some evidence that online and telephone modes of synchronous social contact that are largely one-to-one could influence mental health, even though they are not a substitute for in-person social contact. Asynchronous modes of communication like emails and text messages were not associated with mental health and neither was online social media engagement for older adults, although the pattern for young adults aged around 20 years was markedly different. Young adults who increased their online social media activity during the pandemic experienced a deterioration in their mental health (H2 – the rich get poorer). This result adds considerably to existing research that suggests greater online social media engagement is not good for the mental health of adolescents and young adults (Hancock et al., 2022; Marciano et al., 2021).
For hypotheses 1 and 2, we had to assume that there were no time-varying unmeasured confounders that were affecting modes of social contact and mental health. We could weaken this assumption for hypothesis 3, where we found stronger evidence of a causal effect of in-person social contact on anxiety-depression (H3). However, the effect of in-person social contact and the R-sq of the fixed effect models were small. The effect size of in-person social contact is about a quarter of the effect of financial position. It is important to remember that the periods of observation coincided with a general increase in in-person social contact in the UK from May 2020 to March 2021, rather than the sudden reduction in social contact at the start of the pandemic. It is possible that there may have been a much larger effect of a drastic reduction in in-person social contact at the start of the pandemic. Moreover, this study examined only one aspect of social relationships, the frequency of social contact. It is possible that the emotional content of social relationships may be more important in explaining mental health.
We make the following contributions to life-course theory on social relationships and mental health. Existing models like the social convoy model (Kahn and Antonucci, 1980) are not explicit about the importance of the mode of social contact. We find strong evidence that the mental health benefits of in-person modes of social contact cannot be substituted by online or asynchronous modes of social contact. We also address one of the major limitations of the social convoy model by adding to the causal claims about the importance of social relationships for mental health. Here we find consistent evidence of a causal effect of in-person social contact on mental health, using the natural experiment of COVID-19 pandemic social restrictions as an exogenous determinant of changes in social contact.
We additionally highlight the importance of young adulthood as a sensitive life-course period for the effect of social relationships on mental health (Orben et al., 2020), in contrast to a tendency on life-course research to focus on later-life relationships (Fuller et al., 2020). An increase in online social media contact was detrimental for the mental health of group of young adults who did not engage much with social media prior to the pandemic. This is similar to findings that adolescents and young adults with better mental health prior to the pandemic experienced a notable mental health decline during the pandemic (Gagne et al., 2022) while those with poor mental health prior to the pandemic experienced an improvement (Hu and Qian, 2021a). Life-course theories on social relationships and health need to explicitly consider differences between age-cohorts in the effect of digital and in-person modes of social contact on mental health.
Conclusion
The study provided strong evidence on how changes in the mode of social relationships during the COVID-19 pandemic in the UK affected the mental health of adults. There was little evidence to support the idea that online modes of social contact could compensate for the restrictions in in-person social contact during the pandemic. Young adulthood is a sensitive period of the life-course for social relationships, with increases in online social media frequency during the pandemic having adverse effects on mental health.
Supplemental Material
Supplemental material, sj-pdf-1-soc-10.1177_00380385231172123 for No Substitute for In-Person Interaction: Changing Modes of Social Contact during the Coronavirus Pandemic and Effects on the Mental Health of Adults in the UK by Patrick Rouxel and Tarani Chandola in Sociology
Acknowledgments
We thank the reviewers for their insights into the study. The Millennium Cohort Study, Next Steps, 1970 British Cohort Study and 1958 National Child Development Study are supported by the Centre for Longitudinal Studies, Resource Centre 2015-20 grant (ES/M001660/1) and other co-funders. The COVID-19 data collections in these four cohorts were funded by the UKRI grant (ES/V012789/1).
Biography
Patrick Rouxel is a postdoctoral researcher based in the Faculty of Social Sciences at the University of Hong Kong. He originally trained as a dentist and later in his career developed an interest in epidemiology and public health. He obtained his PhD in public health from University College London in 2014 and has since conducted research on the topic of social relationships and health.
Tarani Chandola is Professor of Medical Sociology based in the Department of Sociology, University of Hong Kong since 2021. He was previously the head of department of Social Statistics and the director of the Cathie Marsh Institute for Social Research at the University of Manchester. His research is primarily on the social determinants of health, focusing on health inequalities and psychosocial factors, and the analysis of longitudinal cohort studies. Much of his research is on stress at work, and its effects on health and related biomarkers.
Footnotes
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: funder: Economic and Social Research Council, ES/R008930/1 and ES/S012567/1 (TC); and ES/P010075/1 (PR).
ORCID iDs: Patrick Rouxel  https://orcid.org/0000-0003-0330-554X
https://orcid.org/0000-0003-0330-554X
Tarani Chandola  https://orcid.org/0000-0002-1864-3413
https://orcid.org/0000-0002-1864-3413
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Patrick Rouxel, University of Hong Kong, Hong Kong.
Tarani Chandola, University of Hong Kong, Hong Kong & University of Manchester, UK.
References
- Angrist JD, Imbens GW, Rubin DB. (1996) Identification of causal effects using instrumental variables. Journal of the American Statistical Association 91: 444–455. [Google Scholar]
- Antonucci TC, Ajrouch KJ, Webster NJ, et al. (2019) Social relations across the life span: Scientific advances, emerging issues, and future challenges. Annual Review of Developmental Psychology 1: 313–336. [Google Scholar]
- Brown M, Goodman A, Peters A, et al. (2021) COVID-19 Survey in Five National Longitudinal Studies: Waves 1, 2 and 3 User Guide (Version 3). London: UCL Centre for Longitudinal Studies and MRC Unit for Lifelong Health and Ageing. [Google Scholar]
- Chandola T, Kumari M, Booker CL, et al. (2022) The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychological Medicine 52: 2997–3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David ME, Roberts JA. (2021) Smartphone use during the COVID-19 pandemic: Social versus physical distancing. International Journal of Environmental Research and Public Health 18(3): 1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison NB, Steinfield C, Lampe C. (2007) The benefits of Facebook ‘friends’: Social capital and college students’ use of online social network sites. Journal of Computer-Mediated Communication 12: 1143–1168. [Google Scholar]
- Frith C. (2009) Role of facial expressions in social interactions. Philosophical Transactions of the Royal Society B: Biological Sciences 364(1535): 3453–3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller HR, Ajrouch KJ, Antonucci TC. (2020) The convoy model and later-life family relationships. Journal of Family Theory & Review 12: 126–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagne T, Nandi A, Schoon I. (2022) Time trend analysis of social inequalities in psychological distress among young adults before and during the pandemic: Evidence from the UK Household Longitudinal Study COVID-19 waves. Journal of Epidemiology and Community Health 76(5): 421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Merchant RM, Lurie N. (2020) The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine 180: 817–818. [DOI] [PubMed] [Google Scholar]
- Hancock J, Liu SX, Luo M, et al. (2022) Psychological well-being and social media use: A meta-analysis of associations between social media use and depression, anxiety, loneliness, eudaimonic, hedonic and social well-being. SSRN. DOI: 10.2139/ssrn.4053961. [DOI] [Google Scholar]
- Hawkley LC, Finch LE, Kotwal AA, et al. (2021) Can remote social contact replace in-person contact to protect mental health among older adults? Journal of the American Geriatrics Society 69(11): 3063–3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holaday LW, Oladele CR, Miller SM, et al. (2022) Loneliness, sadness, and feelings of social disconnection in older adults during the COVID-19 pandemic. Journal of the American Geriatrics Society 70(2): 329–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lundstad J, Smith TB, Bradley LJ. (2010) Social relationships and mortality risk: A meta-analytic review. PLoS Medicine 7: 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. (1988) Social relationships and health. Science 241: 540–545. [DOI] [PubMed] [Google Scholar]
- Hu Y, Qian Y. (2021. a) COVID-19 and adolescent mental health in the United Kingdom. Journal of Adolescent Health 69: 26–32. [DOI] [PubMed] [Google Scholar]
- Hu Y, Qian Y. (2021. b) COVID-19, inter-household contact and mental well-being among older adults in the US and the UK. Frontiers in Sociology 6: 714626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jutai JW, Tuazon JR. (2022) The role of assistive technology in addressing social isolation, loneliness and health inequities among older adults during the COVID-19 pandemic. Disability and Rehabilitation: Assistive Technology 17(3): 248–259. [DOI] [PubMed] [Google Scholar]
- Kahn RL, Antonucci TC. (1980) Convoys over the life course: Attachment, roles, and social support. In: Baltes PB, Brim O. (eds) Life-Span Development and Behavior. New York, NY: Academic Press, pp. 254–283. [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, et al. (2003) Screening for serious mental illness in the general population. Archives of General Psychiatry 60(2): 184–189. [DOI] [PubMed] [Google Scholar]
- Klimmt C, Hefner D, Reinecke L, et al. (2017) The permanently online and permanently connected mind mapping the cognitive structures behind mobile internet use. In: Vorderer P, Hefner D, Reinecke L, et al. (eds) Permanently Online, Permanently Connected Living and Communicating in a POPC World, 1st edn. New York, NY: Routledge, p. 11. [Google Scholar]
- Knowles G, Gayer-Anderson C, Turner A, et al. (2022) Covid-19, social restrictions, and mental distress among young people: A UK longitudinal, population-based study. Journal of Child Psychology and Psychiatry 63(2): 1392–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski RM, Giumetti GW, Schroeder AN, et al. (2014) Bullying in the digital age: A critical review and meta-analysis of cyberbullying research among youth. Psychological Bulletin 140(4): 1073–1137. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. (2003) The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care 41: 1284–1292. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, et al. (2007) Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine 146: 317–325. [DOI] [PubMed] [Google Scholar]
- McKenna KYA, Green AS, Gleason MEJ. (2002) Relationship formation on the internet: What’s the big attraction? Journal of Social Issues 58: 9–31. [Google Scholar]
- Mansournia MA, Nazemipour M, Naimi AI, et al. (2021) Reflection on modern methods: Demystifying robust standard errors for epidemiologists. International Journal of Epidemiology 50: 346–351. [DOI] [PubMed] [Google Scholar]
- Marciano L, Ostroumova M, Schulz PJ, et al. (2021) Digital media use and adolescents’ mental health during the Covid-19 pandemic: A systematic review and meta-analysis. Frontiers in Public Health 9: 793868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz CL, Green MJ, Benzeval M, et al. (2021) Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: Longitudinal analyses of the UK Household Longitudinal Study. Journal of Epidemiology and Community Health 75: 224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A, Tomova L, Blakemore S-J. (2020) The effects of social deprivation on adolescent development and mental health. The Lancet Child & Adolescent Health 4: 634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pancani L, Marinucci M, Aureli N, et al. (2021) Forced social isolation and mental health: A study on 1,006 Italians under COVID-19 lockdown. Frontiers in Psychology 12: 663799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel K, Robertson E, Kwong ASF, et al. (2022) Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Network Open 5: e227629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G, Mancini AD. (2021) The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine 51(2): 201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, McArthur BA, Cooke JE, et al. (2021) Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatrics 175: 1142–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E, Daly M. (2021) Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: Longitudinal evidence from the Understanding America Study. British Journal of Health Psychology 26: 570–587. [DOI] [PubMed] [Google Scholar]
- Robinson E, Sutin AR, Daly M, et al. (2022) A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders 296: 567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouxel P, Chandola T, Kumari M, et al. (2022) Biological costs and benefits of social relationships for men and women in adulthood: The role of partner, family and friends. Sociology of Health & Illness 44(1): 5–24. [DOI] [PubMed] [Google Scholar]
- Serrano-Alarcon M, Kentikelenis A, McKee M, et al. (2022) Impact of COVID-19 lockdowns on mental health: Evidence from a quasi-natural experiment in England and Scotland. Health Economics 31: 284–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart A, Katz D, Stevenson C, et al. (2022) Loneliness in older people and COVID-19: Applying the social identity approach to digital intervention design. Computers in Human Behavior Reports 6: 100179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valkenburg PM, Meier A, Beyens I. (2022) Social media use and its impact on adolescent mental health: An umbrella review of the evidence. Current Opinion in Psychology 44: 58–68. [DOI] [PubMed] [Google Scholar]
- Yang C-c, Brown BB, Braun MT. (2013) From Facebook to cell calls: Layers of electronic intimacy in college students’ interpersonal relationships. New Media & Society 16: 5–23. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-soc-10.1177_00380385231172123 for No Substitute for In-Person Interaction: Changing Modes of Social Contact during the Coronavirus Pandemic and Effects on the Mental Health of Adults in the UK by Patrick Rouxel and Tarani Chandola in Sociology