Abstract
Background
Splenic injury due to chest compressions is a rare and fatal complication that occurs immediately after cardiopulmonary resuscitation.
Case Presentation
Cardiopulmonary resuscitation was carried out using a mechanical chest compression device in a 74‐year‐old Japanese female patient who underwent cardiac arrest. Computed tomography postresuscitation revealed bilateral anterior rib fractures. Other traumatic findings were not observed. Coronary angiography revealed no new lesions; the cause of the arrest was hypokalemia. She received mechanical support with venoarterial extracorporeal membrane oxygenation and multiple antithrombotic agents. Her hemodynamic and coagulative condition became life‐threatening on day 4; abdominal ultrasound revealed massive bloody ascites. Only a minor splenic laceration was observed intraoperatively, despite massive bleeding. Furthermore, her condition stabilized after splenectomy and blood transfusion. Venoarterial extracorporeal membrane oxygenation was discontinued on day 5.
Conclusion
In patients with postcardiac arrest, delayed bleeding due to minor visceral injury should be considered, particularly for coagulation abnormalities.
Keywords: Blood coagulation disorder, cardiopulmonary resuscitation, chest compression, extracorporeal membrane oxygenation, splenic injury
Three days after mechanical cardiopulmonary resuscitation (CPR) and initiation of venoarterial extracorporeal membrane oxygenation, massive intra‐abdominal bleeding was detected, although the initial computed tomography scan did not show abdominal visceral injury. In post‐CPR patients, delayed bleeding from visceral injury should be considered, even after a certain time, especially in cases of coagulation abnormalities.
INTRODUCTION
High‐quality external chest compression is essential in cardiopulmonary resuscitation (CPR). However, various chest compression‐related injuries have been reported. Splenic injury is a rare and fatal complication of CPR that occurs immediately after resuscitation. 1 We report a case of mechanical CPR‐caused splenic injury that resulted in massive internal bleeding 4 days later, despite the absence of visceral injury on postresuscitation computed tomography (CT).
CASE REPORT
A 74‐year‐old Japanese female patient with a history of ischemic heart disease, nonvalvular atrial fibrillation, cerebral infarction, chronic kidney disease, and hypothyroidism was brought to the emergency department after a cardiac arrest at home. After a few minutes of manual CPR by her family and paramedics, mechanical CPR was initiated using the Lund University Cardiopulmonary Assist System‐2 device (Physio‐Control Inc.). The patient was defibrillated twice for ventricular fibrillation. She received multiple doses of epinephrine, and spontaneous circulation returned after 29 min of mechanical CPR. The device was used in its appropriate position.
However, as pulseless ventricular tachycardia was still observed, cardiac support with venoarterial extracorporeal membrane oxygenation (VA‐ECMO) was initiated. Coronary angiography revealed no new lesions in the coronary arteries. A noncontrast CT scan was carried out to investigate the cause of cardiac arrest. This revealed multiple bilateral anterior rib fractures due to the chest compressions, with no evidence of other injuries (Fig. 1). The cause of the arrest was considered to be hypokalemia (admission level K = 2.6 mmol/L) induced by multiple diuretic drugs. The patient was admitted to the intensive care unit for continued resuscitation. Furthermore, she received continuous infusions of unfractionated heparin based on active coagulation time. She was given prasugrel and apixaban because of her atrial fibrillation and high risk of stent thrombosis.
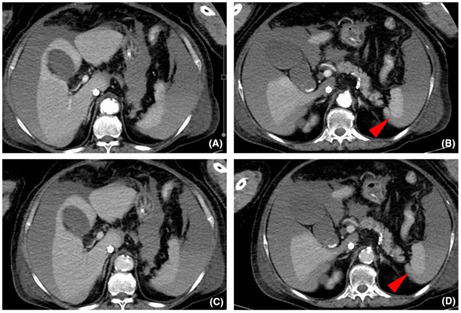
Fig. 1.
Computed tomography scan on admission of a 74‐year‐old woman who underwent cardiac arrest. (A–C) Sequence of images of the abdominal window showing no ascites or splenic injury. (D) Bilateral anterior rib fractures are seen (red arrowheads). (E, F) Coronal and sagittal images of the abdominal window showing no splenic injury.
On hospital day 3, her blood pressure gradually decreased, and ECMO flow could not be maintained the following day. The patient had already received more than 20 units of blood products and was on a high‐dose vasopressor. Blood examination revealed progressive coagulation abnormalities (Table 1). The results were as follows: activated partial thromboplastin time, 136 s; prothrombin time activity, 31%; and platelet count, 25 × 109/L. Abdominal ultrasound revealed an echo‐free space around the liver and spleen. An emergency laparotomy was carried out due to the massive bloody ascites observed on contrast‐enhanced CT (Fig. 2). Intraoperatively, a grade 2 splenic injury (according to the American Association for the Surgery of Trauma) was observed with a capsular tear and a 2 cm laceration at the inferior pole. The spleen was adherent to the retroperitoneum and diaphragm. The abdomen was temporarily closed using an open negative‐pressure therapy system, ABThera (KCI). The volume of blood loss was greater than 10 L. As the patient was hemodynamically stable the next day, VA‐ECMO was discontinued. Her coagulation abnormalities were resolved after management with the interruption of antithrombotic agents, surgical hemostasis, and blood transfusions. Abdominal closure was achieved on day 6. Histopathological examination of the excised splenic tissues was unremarkable. Tracheostomy was carried out on day 15, she was discharged from the intensive care unit on day 26, and transferred to a rehabilitation hospital on day 87 with no neurological deficits.
Table 1.
Results of laboratory values and blood transfusion in a 74‐year‐old Japanese woman who underwent cardiac arrest
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | |
|---|---|---|---|---|---|
| On admission | Laparotomy | ||||
| Laboratory values | |||||
| Prothrombin time activity (%) | 51 | 38 | 33 | 31 | 68 |
| aPTT (s) | 35 | 48 | 61 | 136 | 39 |
| Fibrinogen (mg/dL) | 392 | 323 | 215 | 304 | 319 |
| Hemoglobin (g/dL) | 10.9 | 9.0 | 8.1 | 9.3 | 9.5 |
| Platelet (109/L) | 230 | 129 | 60 | 25 | 159 |
| ACT at 05:00/11:00/17:00/23:00 h (s) | −/−/−/196 | 150/153/220/204 | 261/240/235/− | 190/286/209/128 | −/−/−/− |
| Blood transfusion | |||||
| Packed red blood cells (pack) | 0 | 2 | 6 | 22 | 2 |
| Fresh frozen plasma (unit) | 0 | 0 | 8 | 68 | 16 |
| Platelet concentrate (unit) | 0 | 0 | 10 | 60 | 10 |
ACT, active coagulation time; aPTT, activated partial thromboplastin time.
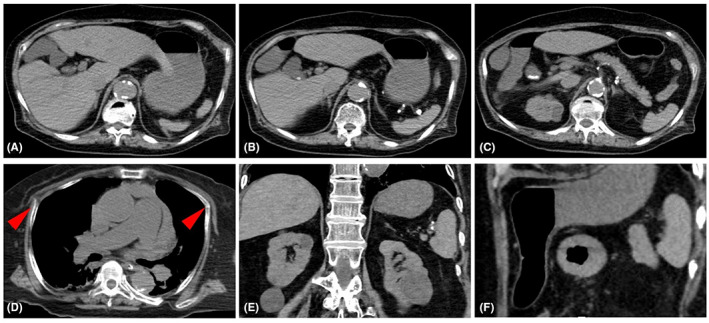
Fig. 2.
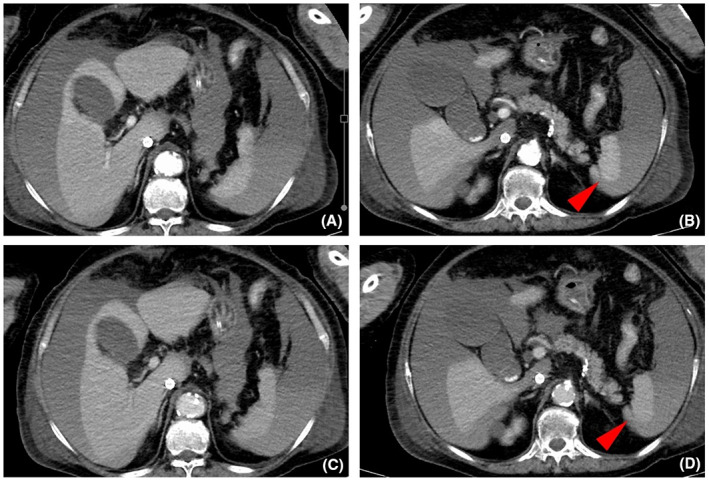
Computed tomography scan with abdominal contrast enhancement of a 74‐year‐old woman who underwent cardiac arrest, on day 4 of admission. (A, B) Arterial phase and (C, D) equilibrium phase. Imaging reveals massive ascites, with an average of 60 Hounsfield units and a suspicious lesion of splenic laceration (B, D, arrowheads) without contrast extravasation.
DISCUSSION
We present a case of delayed massive bleeding from a splenic injury after mechanical chest compression that was not observed on postresuscitation CT.
Splenic injuries after CPR are rare, with an incidence rate of approximately 0.3%. 1 Injuries to thoracic organs, such as the sternum, ribs, and lungs, are frequently reported. 2 Moreover, injuries to the abdominal viscera, including the stomach, liver, and kidneys, have also been reported. No significant difference is observed in the rate of life‐threatening injuries between manual and mechanical CPR. 2 Anatomically, it is difficult to transmit the force of chest compressions from the sternum to the spleen. Therefore, these injuries are rare compared to those of the liver or stomach. Left posterior rib fractures generally increase the suspicion of splenic injury. In contrast, splenic injury is suspected less in thoracic anterior rib fractures due to their anatomical position. In this patient, as the spleen was adhered to the diaphragm and retroperitoneum, a minor laceration could have been caused by the force of mechanical chest compressions transmitted to the spleen.
In this case, massive hemorrhage occurred later, despite the absence of visceral injury on postresuscitation CT. Several cases of splenic injury have been reported after CPR. 3 , 4 , 5 Patients diagnosed postmortem or immediately after CPR showed large lacerations or other concomitant fatal injuries. In contrast, delayed bleeding from a splenic injury rarely occurs after minor blunt trauma. 6 Common causes of delayed bleeding from splenic injury are pseudoaneurysms, pseudocysts, or disruption of the subcapsular hematoma. 7 To the best of our knowledge, delayed bleeding from splenic injury after CPR has rarely been reported. 8 , 9
Delayed bleeding is typically associated with coagulation abnormalities, specifically therapeutic anticoagulation, systemic thrombolytic therapy, antiplatelet therapy, thrombocytopenia, and coagulopathy. A case series identified coagulation abnormalities in 13 of the 15 patients with CPR‐related liver injury. 10 Antiplatelets and therapeutic anticoagulants are standard in patients with postcardiac arrest who undergo percutaneous coronary artery intervention or mechanical circulatory support. Coagulation abnormalities could destroy the subcapsular hematoma and dissolve the hemostatic thrombus, even in trivial injuries. In this case, various antithrombotic drugs given to the patient might have contributed to the delayed bleeding. Cardiopulmonary arrest is a serious condition that frequently leads to early death. Furthermore, as comatose or sedated patients cannot express their symptoms, bleeding can go unnoticed and be mistaken for the deterioration of the primary disease. Visceral injuries after CPR can be masked, leading to underreporting. Therefore, delayed bleeding due to visceral abdominal injury should be considered in patients with coagulation abnormalities after cardiac arrest.
Ultrasonography is essential for detecting intra‐abdominal bleeding and is the gold standard for investigating intrathoracic and abdominal fluids in primary trauma care. Thus, in patients with postcardiac arrest, repeat ultrasound should be carried out if there are signs of hemodynamic instability, decreased blood flow, or drainage insufficiency in ECMO. In such instances, early recognition of bleeding would have allowed consideration of minimally invasive treatment options, including transcatheter arterial embolization, ultimately avoiding fatal bleeding.
We report a case of delayed massive bleeding from splenic injury after mechanical CPR, despite the absence of visceral injury on postresuscitation CT. In post‐CPR patients, delayed bleeding from visceral injury should be considered, even after multiple days, particularly in cases of coagulation abnormalities.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: Written informed consent was obtained for the publication of the data in this article.
Registry and registration no. of the study/trial: N/A.
Animal studies: N/A.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
The authors would like to thank Drs. Y. Narumi, D. Nemoto, and K. Sako, the physicians involved in treating the patient.
REFERENCES
- 1. Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest 1987; 92: 287–91. [DOI] [PubMed] [Google Scholar]
- 2. Gao Y, Sun T, Yuan D et al. Safety of mechanical and manual chest compressions in cardiac arrest patients: a systematic review and meta‐analysis. Resuscitation 2021; 169: 124–35. [DOI] [PubMed] [Google Scholar]
- 3. Milling L, Leth PM, Astrup BS. Life‐threatening and suspicious lesions caused by mechanical cardiopulmonary resuscitation. Am. J. Forensic Med. Pathol. 2017; 38: 219–21. [DOI] [PubMed] [Google Scholar]
- 4. Salzman M, Friedman J. Bystander cardiopulmonary resuscitation‐induced splenic laceration and hepatosplenic hematoma. Am. J. Emerg. Med. 2012; 30: e1–2. [DOI] [PubMed] [Google Scholar]
- 5. Stallard N, Findlay G, Smithies M. Splenic rupture following cardiopulmonary resuscitation. Resuscitation 1997; 35: 171–3. [DOI] [PubMed] [Google Scholar]
- 6. Basukala S, Tamang A, Bhusal U, Sharma S, Karki B. Delayed splenic rupture following trivial trauma: a case report and review of literature. Int. J. Surg. Case Rep. 2021; 88: 106481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ruffolo DC. Delayed splenic rupture: understanding the threat. J. Trauma Nurs. 2002; 9: 34–40. [DOI] [PubMed] [Google Scholar]
- 8. Berlinerblau R, Marmolejos F, Bykofsky MM. Delayed rupture of the spleen after cardiac massage. JAMA 1980; 243: 364–5. [PubMed] [Google Scholar]
- 9. Subramani K, Thomas AN, Reeve RS. Occult splenic rupture with cardiovascular collapse: a report of three cases in critically ill patients. Intensive Care Med. 2002; 28: 1819–21. [DOI] [PubMed] [Google Scholar]
- 10. Meron G, Kurkciyan I, Sterz F et al. Cardiopulmonary resuscitation‐associated major liver injury. Resuscitation 2007; 75: 445–53. [DOI] [PubMed] [Google Scholar]


