Abstract
Background
Survival for children with sickle cell disease (SCD) has improved significantly. However, patients with SCD still encounter several impediments to accessing adequate healthcare. Rural and medically underserved areas, such as parts of the Midwest, can exacerbate these barriers, separating children with SCD from subspecialists even further. Telemedicine has been a means to close these gaps in care for children with other special healthcare needs, but few studies have discussed how caregivers of children with SCD perceive its use.
Methods
The objective of this study is to understand the experiences of caregivers of pediatric SCD patients in a geographically diverse area in the Midwest in accessing care, and their perspectives of telemedicine. Caregivers of children with SCD completed an 88-item survey via a secured REDCap link either in-person or via secure text. Descriptive statistics (means, medians, ranges, frequencies) were performed for all responses. Univariate chi square tests were performed to analyze associations, particularly with telemedicine responses.
Results
The survey was completed by 101 caregivers. Nearly 20% of families traveled more than 1 hour to reach the comprehensive SCD center. Other than their SCD provider, caregivers reported their child having at least 2 other healthcare providers. Most barriers caregivers identified were financial or resource based. Almost a quarter of caregivers expressed feeling as though these barriers impacted their and/or their child’s mental health. Ease of access to team members, as well as scheduling, were common facilitators of care cited by caregivers. The majority were willing to participate in telemedicine visits, regardless of how far they lived from the SCD center, though many noted aspects requiring adaptation.
Conclusion
This cross-sectional study describes barriers to care experienced by caregivers of children with SCD, regardless of proximity to an SCD center, as well as caregiver perceptions of the usefulness and acceptability of telemedicine for SCD care.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-023-09383-x.
Keywords: Telemedicine, Telehealth, Sickle cell disease, Pediatric, Access to Health Care
Introduction
Sickle cell disease (SCD) is an inherited hematologic condition that affects approximately 100,000 individuals in the United States and carries with it potentially devastating complications. However, improved screening and preventative measures have led to increased survival to adulthood for children with SCD in the U.S.[1] Evidence-based, comprehensive SCD care has been shown to improve patient outcomes, but barriers to such care are well-described for children, as well as adults living with SCD.[2].
Children with SCD have also been shown to experience difficulty with transportation, extended wait times, and an inability to access subspecialty providers easily.[3] This has resulted in less than 70% of children with SCD receiving recommended clinical care, and fewer than half experiencing coordination of care between primary and subspecialty providers.[4] Further complicating issues is the fact that comprehensive sickle cell centers are most commonly located in major metropolitan areas, making it difficult for families in rural or medically underserved areas to access this type of comprehensive care.[5, 6].
Caregivers of children with special healthcare needs, such as SCD, also experience significant burdens. The physical, psychological, and financial stressors associated with caring for a child with a chronic disease contributes to this. Studies have shown that the amount of time caregivers spend each day to meet their child’s needs, as well as what they spend their time doing (e.g. physical care, supervision, etc.), introduce risks to their overall well-being.[7] Importantly, the psychological impact of this leads to symptoms of depression and anxiety, low levels of resilience, and poor family functioning.[8, 9].
Telemedicine, the delivery of healthcare from a distance with the use of audio and visual technology, has been an effective means of increasing access to subspecialty care, especially for those with chronic health conditions. Two main forms of telemedicine include: (1) Hub-and-spoke, in which an expert or specialist at a tertiary care center (hub) provides medical care virtually for a patient located at a remote clinic site (spoke), and (2) Direct-to-consumer, in which the expert or specialist provides virtual medical care directly to the patient who is often utilizing a smart phone or tablet in their home. Importantly, the feasibility of telemedicine in pediatric populations has been established, particularly during the recent COVID-19 pandemic.[10–12] Yet, there are still several gaps in the existing literature, barriers to accessing care specifically for pediatric patients with SCD have not been widely published, and little is known about how caregivers and patients with SCD feel regarding the use of technology like telemedicine for addressing these barriers [13].
The purpose of this study was to increase understanding of the experiences caregivers of children with SCD throughout a geographically diverse area of the Midwest have in accessing SCD care, as well as discern the caregiver perspective on the use of telemedicine for delivering comprehensive care.
Methods
Participants/procedure
Caregivers of patients with SCD seen at Riley Hospital for Children in Indianapolis, Indiana were contacted by the research team in-person or via secure text. The Riley SCD program serves patients throughout the state of Indiana, as well as parts of Kentucky and Illinois, all of whom were eligible for this survey. The primary location (i.e. hub) of the program is in Indianapolis, IN, which is in the center of the state. Satellite clinics and/or spoke telemedicine sites assist with providing specialized care in two additional cities, though patient care needs and navigation are streamlined through the hub in Indianapolis. Surveys were completed independently by caregivers via a secure Research Electronic Data Capture (REDCap) link. For surveys administered in-person, the research team was made available to provide clarification or aid with technological difficulties. Participants were compensated with a ten-dollar gift card for their time. This study was approved by the Indiana University Institutional Review Board (IRB).
Measure and analysis
An 88-item survey was developed based on previously performed semi-structured interviews with caregivers of children with SCD and the validated Barriers to Care Questionnaire (BCQ).[13, 14] The survey included questions regarding their experience accessing care, including barriers and facilitators of care, as well as their perspective on the use of telemedicine in SCD. Descriptive statistics (means, medians, ranges and frequencies) were performed for all responses to survey questions. Univariate chi-square tests were used to analyze possible associations between numbers of barriers reported and time (as a categorical variable) to SCD center, as well as between willingness to participate in telemedicine and prior telemedicine use, perceived positives/negatives of telemedicine, caregiver worry about others caring for their child, and time to SCD center.
Results
Participants
Of the 300 caregivers contacted, 101 completed the survey, resulting in a response rate of 34%. The majority had 1 child with SCD (range 1 to 4), with most having Hb SS genotype (n = 60) (Table 1). Most caregivers identified as the birth parent (n = 91), and 39% said they had no one else to share caregiving responsibilities with. 18% of families drove more than 1 hour to access comprehensive sickle cell care.
Table 1.
Baseline Characteristics of Caregivers and Children (N = 101)
| Caregivers | Children | |
|---|---|---|
| Race/Ethnicity (select all that apply) | ||
|
African American or Black African or Black Caribbean or Creole White Multiracial Hispanic/Latinx |
68% (n = 69) 22% (n = 22) 4% (n = 4) 8% (n = 8) 1% (n = 1) 0% (n = 0) |
78% (n = 79) 22% (n = 22) 2% (n = 2) 1% (n = 1) 1% (n = 1) 1% (n = 1) |
| Relation to Child with SCD | ||
|
Birth mother Birth father Adoptive mother Adoptive father Grandmother/Grandfather Other family member Protective guardian Other |
81% (n = 82) 9% (n = 9) 3% (n = 3) 0% (n = 0) 2% (n = 2) 1% (n = 1) 3% (n = 3) 1% (n = 1) |
- - - - - - - - |
| Number of Children with SCD | ||
|
1 child 2 children 3 children 4 or more children |
82% (n = 83) 15% (n = 15) 1% (n = 1) 1% (n = 1) |
- - - - |
| Child’s Sickle Cell Genotype | ||
|
SS SC SBeta + Thalassemia SBeta 0 Thalassemia I don’t know |
- - - - - |
59% (n = 60) 29% (n = 29) 5% (n = 5) 2% (n = 2) 6% (n = 6) |
Caregiver Burden
Caregivers reported having a median of 2 other healthcare providers that their child sees regularly. However, nearly 10% did not have an established primary care provider. Only 10% reported being uninsured themselves, and 3% reported their child being uninsured at the time of the survey, though 38% reported gaps in insurance for either themselves or their child at some point. Nearly 13% felt as though insurance, or the lack thereof, had prevented their child from receiving the care they needed at any point in time. 17% reported receiving financial support from their healthcare team to pay bills, reimburse gas, or purchase food.
42% of caregivers who identified as the birth parent reported not knowing they carried sickle cell trait prior to their child being born. Approximately 40% felt having a child with sickle cell disease impacted their daily stress and/or mental health. 63% of caregivers worried about others (e.g. school staff) caring for their child, and nearly 50% worried about the care and knowledge of medical providers other than their SCD team. 10% of caregivers reported their child not receiving the care they needed in the emergency department at some point in time, 8% reporting this concern when their child was hospitalized, and only 2% when seen in sickle cell clinic (Supplemental Table).
Barriers/Facilitators
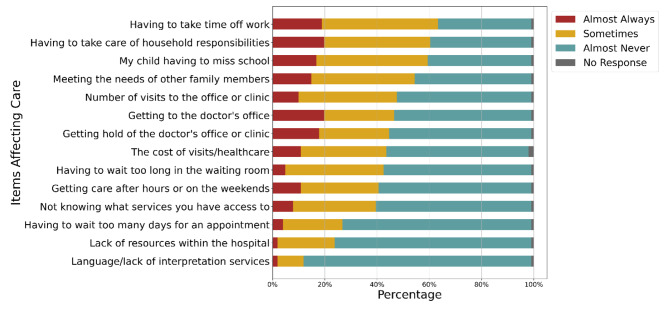
Caregivers identified a median number of 6 barriers to accessing SCD care, with other household responsibilities, childcare, lost time from work and school as the most common (Fig. 1). There was no statistically significant association between travel time to the clinic and the number of barriers identified (p = 0.1). Fifty-two caregivers reported being the primary caregiver for someone other than their child with SCD. About 20% of caregivers felt the barriers they experienced affected their and/or their child’s well-being and/or mental health at times, yet less than half reported their healthcare team ever discussing ways to address these barriers.
Fig. 1.
Items that affect ability to access medical care (N = 101)
Sixty-two caregivers reported sharing caregiving responsibilities with at least one other person, with nearly 70% (n = 69) stating they receive support from their family when needed. The majority of caregivers felt that it was always or sometimes true that the SCD clinic facilitated care by easy access to SCD staff, ease of scheduling appointments, and convenient times to schedule. Additionally, 17% of caregivers reported the SCD clinic/hospital supporting them through resources, with mental health support, food pantry, and housing assistance being the most common.
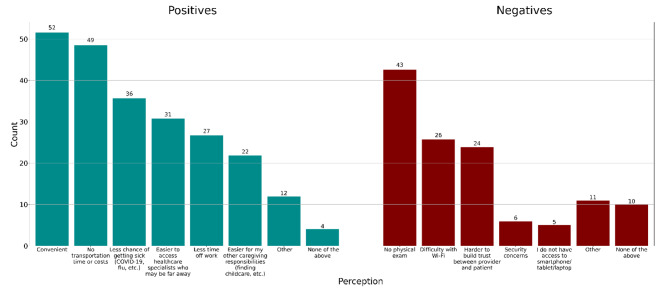
Telemedicine
40% of caregivers had participated in some form of telemedicine, the majority being direct-to-consumer. The most common positives of telemedicine reported were (1) convenience; (2) decreased transportation time/cost; (3) less chance of getting sick ; and (4) easier to access healthcare specialists (Fig. 2). However, nearly half of all respondents felt the lack of a physical exam was a negative for telemedicine, and about 25% (n = 24) stated it was harder to build trust via telemedicine. 81% (n = 82) were willing to participate in future telemedicine visits sometimes or always (Supplemental Table). This was similar for both SCD and other medical visits. There was no statistically significant association between willingness to participate in telemedicine and prior telemedicine use, perceived positives/negatives of telemedicine, caregiver worry about others caring for their child, or distance from SCD center (univariate analyses; all p > 0.05).
Fig. 2.
Perceived positives and negatives of telemedicine (N = 101)
Discussion
Access to care is a known challenge for patients with SCD, particularly because of a lack of comprehensive SCD treatment centers throughout the country. This study describes the perspectives of caregivers of children and adolescents with SCD, regardless of distance from an SCD center, in a Midwestern state with significant variation in medical resources.
While our study demonstrated similar barriers to those reported in other studies such as transportation and lost time from school and work, [15–17], the frequency of barriers reported varied, which suggests the importance of screening for barriers universally in SCD as needs may differ based on state/region. Additionally, participants in our study did report unique barriers not described in previous studies with caregivers, specifically regarding provider knowledge and bias leading to children with SCD not receiving the care they need. We had previously identified this in semi-structured interviews with caregivers who lived in rural or medically underserved areas far from the SCD center[13]. However, this concern was consistent amongst caregivers regardless of distance to the SCD center and supported by prior studies demonstrating lack of provider knowledge and comfort, as well as bias, leading to inequities in care delivery such as poor adherence to stroke screening, pneumococcal vaccination, and emergency department care [4, 18–23]. This highlights the importance of improved education and awareness regarding SCD and pain management, as well as bias, for medical providers.
Our statewide survey also demonstrated significant caregiver burden for those with a child with SCD. Caregivers reported a median of 6 barriers to accessing care and believed this impacted their and/or their child’s well-being and mental health. While it is well-known that caregivers of children with chronic diseases have increased stress, as well as increased mental health concerns, access to support for both remains limited in SCD.[8, 9, 24, 25] The implications of this are significant when considering how caregiver physical and mental health directly impact the health of the child and are linked with adverse outcomes for both.[26].
There is little literature expanding on what caregivers and/or patients believe are facilitators to accessing care for SCD, as much of what we consider to be facilitators is extrapolated from known or reported barriers. However, studies related to asthma care and mental health cite coordination of care, flexibility in scheduling, and addressing resource barriers as facilitators of care.[27, 28] In our study, caregivers identified several facilitators to accessing care, including accessibility of dedicated SCD team members, such as a nurse coordinator, as well as co-location of care and consolidation of appointments. Additional facilitators included the healthcare team assisting with resources, again pointing to the importance of screening universally for social determinants of health.
The COVID-19 pandemic led to increased adoption of telemedicine, specifically, the direct-to-consumer model. As a result, a significant percentage of caregivers who completed the survey had some experience with telemedicine. And while the majority of participants reported a willingness to participate in future telemedicine visits, many cited the concern for a lack of a physical exam with the direct-to-consumer model. Additionally, worries regarding building trust with healthcare team members that may be new to them was also one of the most common concerns raised by caregivers who had experienced direct-to-consumer telemedicine for both sickle cell disease visits, as well as other subspecialty visits. A small number of caregivers had participated in the hub-and-spoke model of telemedicine, but those that did, did not cite these concerns, which is consistent with the results of our previous qualitative work.[13].
Limitations to the study include the survey being limited to one state and institution. Though, Riley is the largest pediatric sickle cell center in the state and its catchment area is broad, therefore, representing a regionally diverse (rural, urban, suburban) population. Additionally, the response rate was 34%, and therefore, there may be variations or statistical significance that could not be ascertained with this response size.
Conclusion
The experiences of caregivers accessing healthcare for their child with SCD demonstrates significant caregiver burden and barriers to care regardless of nearness or accessibility of medical care. Additionally, while the majority are willing to participate in telemedicine for future sickle cell care, the negatives of telemedicine that caregivers reported are significant. Future studies should evaluate models of telemedicine care adapted for this specific population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all our patients with sickle cell disease and their families. Their courage and strength are an inspiration to us and the work we do.
Abbreviations
- SCD
Sickle Cell Disease
- REDCap
Research Electronic Data Capture
- IRB
Institutional Review Board
- BCQ
Barriers to Care Questionnaire
Author contributions
SAJ and AEC conceptualized and designed the study. SAJ supervised and obtained funding for the study. SAJ, RD, JB, and JEL developed the survey. SAJ and JB wrote the manuscript in consultation with RD, MDJ, JEL and AEC. SAJ, JB, MDJ, JEL, and AEC critically revised the manuscript. All authors read and approved the final manuscript.
Funding
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL143162. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data Availability
All data generated or analyzed during this study are included in this published article and its additional files.
Declarations
Competing interests
The authors have no conflicts of interest to disclose.
Ethics approval and consent to participate
Ethical approval for this study was obtained from Indiana University Institutional Review Board (IRB). All methods were carried out in accordance with relevant guidelines and regulations of the Indiana University IRB. Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115(17):3447–52. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288–94. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 3.Boulet SL, Yanni EA, Creary MS, Olney RS. Health status and healthcare use in a national sample of children with sickle cell disease. Am J Prev Med. 2010;38(4 Suppl):528–35. doi: 10.1016/j.amepre.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Raphael JL, Rattler TL, Kowalkowski MA, Brousseau DC, Mueller BU, Giordano TP. Association of care in a medical home and health care utilization among children with sickle cell disease. J Natl Med Assoc. 2013;105(2):157–65. doi: 10.1016/s0027-9684(15)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shankar SM, Arbogast PG, Mitchel E, Ding H, Wang WC, Griffin MR. Impact of proximity to comprehensive sickle cell center on utilization of healthcare services among children with sickle cell disease. Pediatr Blood Cancer. 2008;50(1):66–71. doi: 10.1002/pbc.21066. [DOI] [PubMed] [Google Scholar]
- 6.Farooq F, Mogayzel PJ, Lanzkron S, Haywood C, Strouse JJ. Comparison of US Federal and Foundation Funding of Research for Sickle Cell Disease and cystic fibrosis and factors Associated with Research Productivity. JAMA Netw Open. 2020;3(3):e201737. doi: 10.1001/jamanetworkopen.2020.1737. [DOI] [PubMed] [Google Scholar]
- 7.McCann D, Bull R, Winzenberg T. The daily patterns of time use for parents of children with complex needs: a systematic review. J Child Health Care. 2012;16(1):26–52. doi: 10.1177/1367493511420186. [DOI] [PubMed] [Google Scholar]
- 8.Penning MJ, Wu Z. Caregiver stress and Mental Health: impact of caregiving relationship and gender. Gerontologist. 2016;56(6):1102–13. doi: 10.1093/geront/gnv038. [DOI] [PubMed] [Google Scholar]
- 9.Toledano-Toledano F, Dominguez-Guedea MT. Psychosocial factors related with caregiver burden among families of children with chronic conditions. Biopsychosoc Med. 2019;13:6. doi: 10.1186/s13030-019-0147-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using Telemedicine to provide Pediatric Subspecialty Care to Children with Special Health Care needs in an Underserved Rural Community. Pediatrics. 2004;113(1):1–6. doi: 10.1542/peds.113.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Clawson BSM, Lacks M, Deaton AV, Hall B, Bach R. Complex Pediatric Feeding Disorders: Using Teleconferencing Technology to Improve Access To a Treatment Program.Pediatr Nurs. 2008;34. [PubMed]
- 12.Jacob SA, Carroll AE, Bennett WE. Jr. A feasibility study of telemedicine for paediatric sickle cell patients living in a rural medically underserved area.J Telemed Telecare. 2019:1357633X19883558. [DOI] [PMC free article] [PubMed]
- 13.Jacob SA, Daas R, Feliciano A, LaMotte JE, Carroll AE. Caregiver experiences with accessing sickle cell care and the use of telemedicine. BMC Health Serv Res. 2022;22(1):239. doi: 10.1186/s12913-022-07627-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seid M, Opipari-Arrigan L, Gelhard LR, Varni JW, Driscoll K. Barriers to care questionnaire: reliability, validity, and responsiveness to change among parents of children with asthma. Acad Pediatr. 2009;9(2):106–13. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Brennan-Cook J, Bonnabeau E, Aponte R, Augustin C, Tanabe P. Barriers to care for persons with Sickle Cell Disease: the Case Manager’s opportunity to improve patient outcomes. Prof Case Manag. 2018;23(4):213–9. doi: 10.1097/NCM.0000000000000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cabana MD, Kanter J, Marsh AM, Treadwell MJ, Rowland M, Stemmler P, et al. Barriers to Pediatric Sickle Cell Disease Guideline Recommendations. Glob Pediatr Health. 2019;6:2333794X19847026. doi: 10.1177/2333794X19847026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoegy D, Guilloux R, Bleyzac N, Gauthier-Vasserot A, Cannas G, Bertrand Y, et al. Sickle cell disease perceptions of caregivers, adolescent, and adult patients: barriers and facilitators to medical care adherence. J Adv Nurs. 2020;76(9):2391–400. doi: 10.1111/jan.14456. [DOI] [PubMed] [Google Scholar]
- 18.Haywood C, Jr, Tanabe P, Naik R, Beach MC, Lanzkron S. The impact of race and disease on sickle cell patient wait times in the emergency department. Am J Emerg Med. 2013;31(4):651–6. doi: 10.1016/j.ajem.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin OY, Thompson SM, Carroll AE, Jacob SA. Emergency Department Provider Survey regarding Acute Sickle Cell Pain Management. J Pediatr Hematol Oncol. 2020;42(6):375–80. doi: 10.1097/MPH.0000000000001843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whiteman LN, Haywood C, Jr, Lanzkron S, Strouse JJ, Feldman L, Stewart RW. Primary care providers’ comfort levels in caring for patients with Sickle Cell Disease. South Med J. 2015;108(9):531–6. doi: 10.14423/SMJ.0000000000000331. [DOI] [PubMed] [Google Scholar]
- 21.Haywood C, Jr, Lanzkron S, Hughes MT, Brown R, Massa M, Ratanawongsa N, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26(5):518–23. doi: 10.1007/s11606-010-1605-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee L, Smith-Whitley K, Banks S, Puckrein G. Reducing Health Care Disparities in Sickle Cell Disease: a review. Public Health Rep. 2019;134(6):599–607. doi: 10.1177/0033354919881438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glassberg JA. Improving Emergency Department-Based Care of Sickle Cell Pain. Hematol Am Soc Hematol Educ Program. 2017;2017(1):412–7. doi: 10.1182/asheducation-2017.1.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pitchik HO, Tofail F, Akter F, Sultana J, Shoab A, Huda TMN, et al. Effects of the COVID-19 pandemic on caregiver mental health and the child caregiving environment in a low-resource, rural context. Child Dev. 2021;92(5):e764–e80. doi: 10.1111/cdev.13651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehan J, Hiscock H, Massie J, Jaffe A, Hay M. Caregiver coping, mental health and child problem behaviours in cystic fibrosis: a cross-sectional study. Int J Behav Med. 2014;21(2):211–20. doi: 10.1007/s12529-013-9289-y. [DOI] [PubMed] [Google Scholar]
- 26.Javalkar K, Rak E, Phillips A, Haberman C, Ferris M, Van Tilburg M. Predictors of Caregiver Burden among Mothers of Children with Chronic Conditions.Children (Basel). 2017;4(5). [DOI] [PMC free article] [PubMed]
- 27.Hellerova L, Gonzalez AE, Dayan PS, George M. Caregiver perceptions of Mental Health and Barriers to and facilitators of their child’s treatment. Pediatr Emerg Care; 2021. [DOI] [PubMed]
- 28.Parikh K, Paul J, Foushee N, Waters D, Teach SJ, Hinds PS. Barriers and facilitators to Asthma Care after hospitalization as reported by caregivers, Health Providers, and School Nurses. Hosp Pediatr. 2018;8(11):706–17. doi: 10.1542/hpeds.2017-0182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its additional files.