Abstract
Purpose:
The purposes of this study were to: 1) Describe the incidence of disordered eating, weight bias, body dissatisfaction, and psychological distress, 2) Examine the relationship between sociodemographic variables (gender, ethnicity, and income) and disordered eating, weight bias, body dissatisfaction, and psychological distress in a sample of low-income adolescents.
Design and Methods:
A cross-sectional study was conducted with 105 adolescents from low-income neighborhoods. Participants completed self-report questionnaires to assess eating behaviors, weight bias, body dissatisfaction, and psychological functioning. Height and weight were measured, and information on household income was collected.
Results:
The participant’s mean age was 16.31 (SD = 2.8) years, 66% female, 47% Hispanic, and 46% African American. The mean annual income was $17,018 (SD = 11,355). Twenty-eight percent self-reported having some form of disordered eating, and 15% reported an eating disorder. The group with eating disorder reported the highest levels of weight bias (M = 93.4, SD = 109.6), body dissatisfaction (M = 94.6, SD = 47.6), and psychological distress (M = 1.4, SD = 0.97).
Conclusion:
This study found a high prevalence of eating disorders with eating disorder participants experiencing the highest levels of weight bias and psychological distress. Future studies are needed to identify and evaluate community and school-based interventions to minimize weight bias and disordered eating.
Practice Implications:
Nurses are at the forefront of healthcare and should collaborate with educators, school counselors, administrators, coaches, parents, and students, to address weight bias and disordered eating in schools by implementing school-based curriculum and policies.
Pediatric obesity is a major health threat in the U.S. The current rate of obesity in children ages 2 to 19 years is 17% with the highest prevalence among Black and Hispanic ethnic groups (Ogden, Carroll, Kit, & Flegal, 2014). Research has shown that unhealthy weight control behaviors are predictors for obesity (Neumark-Sztainer, Wall, Story, & Standish, 2012).
Unhealthy weight control behaviors, disordered eating, and body dissatisfaction are highly prevalent among adolescents (Ackard, Fulkerson, & Neumark-Sztainer, 2007; Eisenberg, Berge, Fulkerson, & Neumark-Sztainer, 2012; Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011) placing them at a higher risk for psychological distress including depression, anxiety, and suicidal behavior (Ackard, Fulkerson, & Neumark-Sztainer, 2011; Crow, Eisenberg, Story, & Neumark-Sztainer, 2008; Stice, Hayward, Cameron, Killen, & Taylor, 2000). The high prevalence of disordered eating among adolescents has been shown to be predictive of obesity (Neumark-Sztainer et al., 2012) potentiating the progression towards a clinical eating disorder (Pearson et al., 2017; Stice, Marti, Shaw, & Jaconis, 2009; The McKnight Investigators, 2003). In fact, Stice et al. (2009) followed adolescents for an 8-year period and found that 12% of participants met the criteria for one or more eating disorders during adolescence.
Disordered eating or unhealthy weight control behaviors including dietary restraint, binge eating and purging behaviors, and misuse of laxatives and diuretics all fall under the DSM V category of “Other Specified Feeding or Eating Disorder”(DSM V, 2013). In some research studies disordered eating is referred to as subthreshold eating disorder (Ackard et al., 2011; Stice et al., 2009) and is often a pre-clinical symptom for full threshold eating disorder (Le Grange et al., 2014; Stice et al., 2009).
Another factor that may impact obesity and disordered eating is weight bias (WB). Despite increasing rates of obesity, obese individuals are experiencing increasing levels of stigma (Andreyeva, Puhl, & Brownell, 2008; Latner & Stunkard, 2003). Higher levels of WB are associated with unhealthy coping strategies, such as eating more food (Puhl et al., 2017; Puhl & Brownell, 2006), higher body mass index (BMI; Myers & Rosen, 1999; Mamun, O’Callaghan, Williams, & Najman, 2013; Neumark-Sztainer et al., 2007; Takizawa, Danese, Maughan, & Arseneault, 2015), body dissatisfaction, and lower psychosocial functioning (Annis, Cash, & Hrabosky, 2004; Bucchianeri, Eisenberg, Wall, Piran, & Neumark-Sztainer, 2014). Additionally, obese individuals experiencing WB are at increased risk for depression and other mental health disorders (Bucchianeri et al., 2014; Friedman et al., 2005).
Although research regarding the relationship of WB, disordered eating, and psychological distress exists, very few data comes from ethnically and culturally diverse populations and virtually none from low-income adolescents, who are at the highest risk for being obese. The overrepresentation of Caucasian youth from middle and upper socioeconomic strata in most weight-based studies makes it difficult to draw conclusions about ethnic and socioeconomic differences. The few studies conducted with ethnically diverse populations have shown conflicting results with disordered eating, eating disorders, and WB. One study found that binge eating disorder was more common in African American than Caucasian women (Striegel-Moore, Wilfley, Pike, Dohm, & Fairburn, 2000). Another study found a higher prevalence of WB among minorities, particularly African Americans (Puhl, Andreyeva, & Brownell, 2008). Conversely, Almeida, Savoy, and Boxer (2011) found lower rates of WB and binge eating risk factors among African Americans compared to their Caucasian and Latino counterparts. When examining eating disorders in a diverse low-income sample of college students, another research group found lower rates of eating disorders in African Americans and Caucasians compared to Latinos (Gentile, Raghavan, Rajah, & Gates, 2007). Rodgers, Watts, Austin, Haines, and Neumark-Sztainer (2017) evaluated ethnic/racial differences with disordered eating in a diverse overweight sample and found limited differences between Asian, White, Black, and Hispanic adolescents. Only one group of researchers examined WB in an ethnically diverse and disadvantaged youth population; however, they explored BMI and weight gain related to WB and not eating behaviors and psychological distress. Also, the analysis from the study focused on gender and not ethnic differences with data from only one school, limiting the generalizability of the findings (Feeg, Candelaria, Krenitsky-Korn, & Vessey, 2014). To our knowledge, no studies have been conducted explicitly focusing on multi-ethnic low-income adolescents examining eating behaviors, weight bias, and psychological functioning with both a non-overweight and overweight sample. With obesity rates highest for multi-ethnic and low-income adolescents (Babey, Hastert, Wolstein, & Diamant, 2010; Barlow, 2007; Hastert, Babey, Diamant, & Brown, 2008; Singh, Siahpush, & Kogan, 2010), efforts to improve our understanding of eating behaviors, WB, and psychological distress in this population are warranted. Only by elucidating the correlations of these variables can effective multidisciplinary and multi-ethnic interventions be designed.
Purpose
The purposes of this study were to
Describe the incidence of disordered eating, WB, body dissatisfaction, and psychological distress in a sample of multi-ethnic low-income adolescents.
Examine the relationship between sociodemographic variables (gender, ethnicity, and income) and disordered eating, WB, body dissatisfaction, and psychological distress in a sample of low-income adolescents.
We predict that participants reporting more disordered eating will have higher levels of WB and psychological distress. We also hypothesize that girls and African Americans in our sample will experience more disordered eating and WB.
Design and Methods
A cross-sectional study design was utilized, and study participants were enrolled from low-income neighborhoods in a major metropolitan city in the Western U.S. Participants were eligible if they were between 13 and 19 years of age and able to read, write, and speak English. The study was approved by the appropriate Institutional Review Board. Sampling bias was minimized by recruiting participants from the community instead of participants who were seeking treatment.
The sample was recruited outside libraries and community centers frequented by adolescents in low-income neighborhoods. The study was explained to each parent and adolescent individually who approached the investigator indicating interest in participating in the study. After informed consent was obtained from the parent and assent from adolescents <18 (adolescents ≥18 years consented without their parents), the participants were screened for eligibility. Of the 109 that consented to participate, 2 were excluded because they were pregnant, and 2 changed their minds. Large tables with chairs and corrugated dividers were set up for privacy where participants filled out the questionnaires. Participants completed self-report questionnaires to assess eating behaviors, WB, body dissatisfaction and psychological functioning; average time for questionnaire completion was 25–30 min. Four participants had challenges understanding how to proceed through the eating behavior questionnaire and needed guidance from the researcher. Demographic information collected included age, gender, grade, ethnic background, and employment. Household income was collected from the parent or participant at the time consent was obtained. The researcher or trained data collectors measured height to the nearest centimeter and weight to the nearest tenth of a kilogram. Participants were asked to remove their jackets, shoes, hats, and removable hair accessories before being weighed and measured. Height was obtained using a portable stadiometer, and weight was measured with a digital scale (Model BG17; Beurer body analysis scale, Hallandale Beach, FL) which was zero balanced before each participant was weighed. To provide privacy participants were weighed behind a 4 panel folding screen room divider.
Measures
Disordered Eating
Eating behaviors were measured using the adolescent version of the Questionnaire of Eating and Weight Patterns (QWEP-A). The QWEP-A was adapted from the adult Questionnaire on Eating and Weight Patterns-Revised (QWEP; Spitzer et al., 1993) by using simpler words to ensure adequate understanding in the adolescent population. Psychometric properties of the QWEP-A have shown moderate stability, adequate predictive proficiency, and concurrent validity (W.G. Johnson, Grieve, Adams, & Sandy, 1999; Johnson, Kirk, & Reed, 2001). In addition, test-retest results revealed significant levels of stability (Johnson et al., 2001).
The 12-item self-report measure classifies participants into several categories including no diagnosis, episodic overeating, binge eating, binge eating syndrome, binge eating disorder, and possible bulimia. Differentiation between these categories depended on whether the participant reported loss of control, distress, and frequency of binges per week. As with previous studies, participants were categorized into one of three eating behavior groups. The first group was no diagnosis; the second was nonclinical binging which included episodic overeating, binge eating, and binge eating syndrome; the third group was eating disorders which included binge eating disorder and possible bulimia. The symptoms of the nonclinical binging category were similar to subthreshold eating disorder or disordered eating.
Stigmatizing Experiences
Weight bias was assessed using the Stigmatizing Situations Inventory-Adolescents (SSI-A) which is a revised version of the Stigmatizing Situations Inventory (SSI) adapted for adolescents. Myers and Rosen (1999) developed the original 50 item SSI, rated on a 10-point scale with a Cronbach alpha of .94 (Friedman et al., 2005). This scale included items such as “People telling you that you will never find a boy/girlfriend if you don’t lose weight,” “Not being able to find clothes that fit,” “Parents nagging you to lose weight.” Each item is rated according to how often an individual has experienced WB (0 = never, 1 = once in your life, 2 = several times in your life, 3 = about once a year, 4 = several times a year, 5 = about once a month, 6 = several times a month, 7 = about once a week, 8 = several times a day, 9 = daily). The higher the score, the higher the frequency of bias the adolescent was experiencing. A mean of ‘0’ indicates no stigmatizing experiences, a mean of ‘5’ is experiencing various types of stigma about once a month, a mean of ‘9’ is experiencing stigma on all items of the scale at least once every day.
There is no evidence found that the original SSI has ever been utilized in an adolescent population. In addition, the SSI contains questions geared towards adults (e.g., losing your job because of your size and not being hired because of your weight, shape or size). Therefore, the tool was modified based on input from an expert panel of nutritionists, physicians, counselors, and nurses specializing in adolescent care. Revisions were made by the researcher based on the evaluation of the expert panel. Items such as “Strangers asking intrusive, personal questions about your weight” were modified to “Strangers asking nosy or personal questions about your weight” and “As an adult, having a child make fun of you” was changed to “As a teen, having another teen, adult, or younger child make fun of you.” Items related to work, such as “Losing a job because of your size” or “Not being hired because of your weight, shape, or size” were eliminated. Following revisions, the 42-item SSI-A had a Cronbach alpha of .98 and Pearson r of .89 at p < .01 in our sample.
Body Dissatisfaction
Body dissatisfaction was assessed using the Body Shape Questionnaire (BSQ), a 34-item scale that measures the desire to lose weight, body satisfaction and feelings of low self-worth. Each item was scored from 1 to 6 (never, rarely, sometimes, often, very often and always). A score of <80 shows no concern with shape. Eighty to 110 is mild concern, 111 to 140 is moderate concern, and over 140 is severe concern with shape. The BSQ has high internal consistency and reliability at .97 and .88, respectively (Rosen, Jones, Ramirez, & Waxman, 1996) and has been used in the adolescent population (Gleason, Alexander, & Somers, 2000; Rodríguez-Cano, Beato-Fernández, & Llario, 2006).
Psychological Functioning
Psychological distress was determined using the Symptom Checklist 90-R (SCL-90-R), a 90-item measure of psychological functioning that addresses nine dimensions (somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) of psychological distress on a 5-point Likert scale. The SCL-90-R has been normed for adolescents’ ages 13 to 18 years and has demonstrated high internal consistency, reliability, and validity (Sadowski & Friedrich, 2000). The Global Severity Index (GSI) is a subscale that measures overall level of psychological symptoms. More severe symptoms of distress are evidenced by higher GSI scores.
Data Analysis
All analyses were performed using SPSS version 22. Descriptive statistics were used to evaluate the frequencies and distributions of all variables and participant background characteristics. Differences in sociodemographic characteristics were tested using Chi-square or independent t-tests, depending on the level of measurement.
Pearson’s correlations were used to determine the relations among all continuous variables (income, BMI, WB, body dissatisfaction and psychological functioning). Comparisons between eating behavior groups (no diagnosis, nonclinical binging, and eating disorders) and WB, body dissatisfaction, and psychological functioning were performed using one-way analysis of variance (ANOVA) with a Bonferroni-Hochberg correction, a conservative test accounting for multiple comparisons applied to each family of posthoc tests.
Results
Demographic Data and Incidence of Disordered Eating, Weight Bias, and Psychological Distress
The 105 participants’ in the sample had a mean age of 16.3 (SD = 2.3) years and mean annual income of $17,018 (SD = 11,355). A majority were female (66%), and they were primarily Hispanic (47%) or African American (46%). We classified the participants as Hispanic or non-Hispanic (African American, Caucasian, and other). We recognize that the non-Hispanic group may have little in common, this strategy was employed to permit analyses without losing data. This sample was representative of the population where the data were collected. The sociodemographic characteristics (gender and ethnicity) of participants were comparable among participants in the eating behavior groups: no diagnosis (n = 60), nonclinical binging (n = 29), and eating disorders (n = 16; Table 1).
Table 1.
Demographic characteristics of participants in the no diagnosis, nonclinical binging, and eating disorder groups (N = 105).
| No diagnosis (n = 60) | Nonclinical binginga (n = 29) | Eating disorderb (n = 16) | |
|---|---|---|---|
| Gender, % | |||
| Male | 20 (19.0%) | 12 (11.4%) | 4 (3.8%) |
| Female | 40 (38.1%) | 17 (16.2%) | 12 (11.4%) |
| Ethnicity, % | |||
| Hispanic | 30 (28.6%) | 14 (13.2%) | 5 (4.8%) |
| Non-Hispanic | 30 (28.6%) | 15 (14.3%) | 11 (10.5%) |
Note. BMI categories: underweight <18.5; non-overweight 18.5–24.9; overweight 25–29.9; obese >30.
Nonclinical binging includes episodic overeating, binge eating, and binge eating syndrome.
Eating disorder includes binge eating disorder and bulimia.
The most common stigmatizing situations reported were “having another teen or a younger child make fun of you” (M = 1.67, SD = 2.60), “being called names, laughed at or teased by other teens or younger children” (M = 1.63, SD = 2.44), “children loudly making comments about your weight to others” (M = 1.50, SD = 2.37) and “a parent nagging you to lose weight” (M = 1.47, SD = 2.71). Overall, 58% (n = 61) of the sample reported having at least one stigmatizing experience, 31.5% (n = 33) reported severe concern with body shape (BSQ score >140), and 21% (n = 22) had high levels of psychological distress (GSI raw score above 0.63). Weight bias means were highest in the obese (Fig. 1) and eating disorder groups (Fig. 2).
Fig. 1.
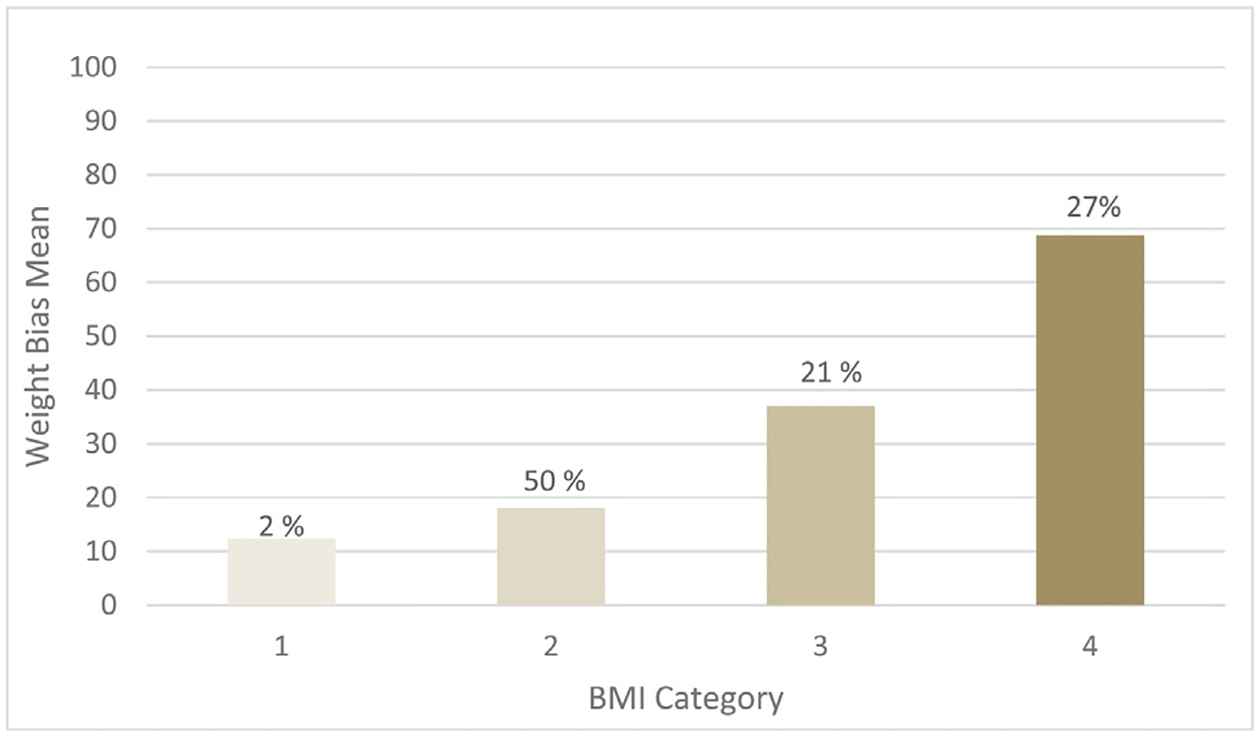
Weight bias means, represented by percentages, within BMI categories. BMI categories: 1 = underweight <18.5; 2 = non-overweight 18.5–24.9; 3 = overweight 25–29.9; 4 = obese >30.
Fig. 2.
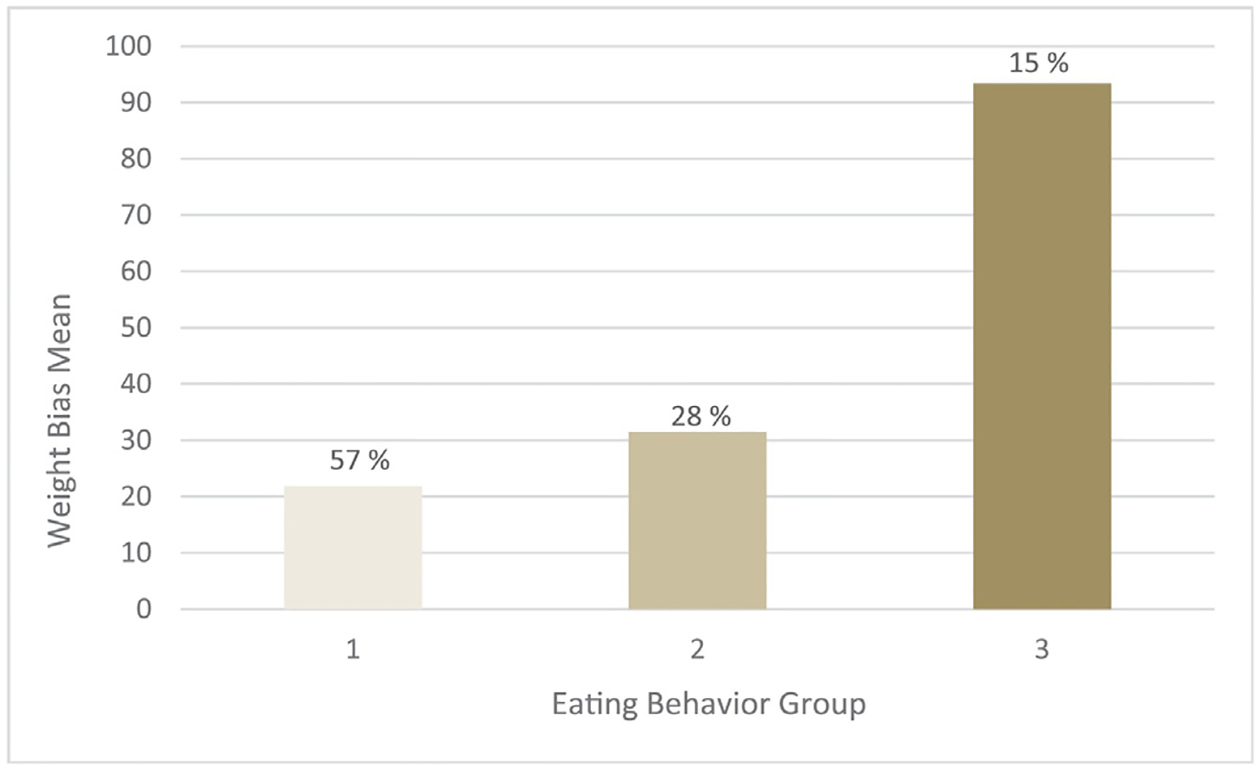
Weight bias means, represented by percentages, within eating behavior groups. Eating behavior groups: 1 = no diagnosis; 2 = nonclinical binging includes episodic overeating, binge eating, and binge eating syndrome; 3 = eating disorder includes binge eating disorder and bulimia.
Relationship Between Demographic Characteristics and Key Variables
Females (M = 72.41, SD = 37.52) reported higher body dissatisfaction than males (M = 51.83, SD = 19.79), t (103) = 3.07, p = .001. There was also a significant difference in psychological distress between males (M = 0.47, SD = 0.49) and females (M = 0.88, SD = 0.84), t (103) = 2.69, p = .002. However, no significant difference was found when comparing males and females on WB (p = .18). Females experienced higher levels of nonclinical binging and higher levels of eating disorders compared to males (Table 1), although these differences did not reach statistical significance, p = .53. Non-Hispanics had higher scores for WB (M = 39.88, SD = 71.01) and psychological distress (M = 0.85, SD = 0.87) than the Hispanics (M = 30.29, SD = 38.08; M = 0.61, SD = 0.60), however only psychological distress reached statistical difference, t (103) = 1.63, p = .005. There was no statistical difference between ethnic groups with respect to eating behavior, p = .40.
Correlations between income, BMI, WB, body dissatisfaction and psychological distress are presented in Table 2. The analyses revealed correlations between BMI, WB, body dissatisfaction and psychological distress. Participants with higher BMIs experienced more WB and reported higher levels of body dissatisfaction and psychological distress. Income was not significantly correlated with any other variable.
Table 2.
Correlational matric for income, BMI, weight bias, body dissatisfaction (BSQ), and psychological functioning (GSI) (N = 105).
| Measure | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Income | – | −.123 | −.060 | −.171 | .058 |
| 2. BMI | −.123 | – | .424* | .436* | .190 |
| 3. Weight bias | −.171 | .436* | – | .539* | .506* |
| 4. BSQ | −.060 | .424* | .539* | – | .609* |
| 5. GSI | .058 | .190 | .506* | .609* | – |
p <.01.
One-way ANOVA analyses indicated significant differences between the eating behavior groups on body dissatisfaction, WB, and psychological distress (Table 3). The eating disorder group reported much higher body dissatisfaction than the other two eating behavior groups. When comparing the eating behavior groups to weight bias, results indicated a significant difference between the no diagnosis and eating disorder group and between the nonclinical binging and the eating disorder group but not between the no diagnosis and the nonclinical binging group (p > .95). Similar results were noted when analyzing the eating behavior and psychological distress. Group differences were noted between the no diagnosis and eating disorder group and between the nonclinical binging and the eating disorder group but not between the no diagnosis and the nonclinical binging group (p > .95) on psychological distress. Mean scores indicated the highest levels of psychological distress among the eating disorder group, followed by the no diagnosis and the nonclinical groups. Post-hoc Bonferroni-Hochberg tests revealed statistically significant differences between the eating behavior groups on body dissatisfaction F (2,102) = 8.2, p = .000, η2 = .139, WB F (2,102) = 11.7, p = .000, η2 = .186, and psychological distress F (2,102) = 9.1, p = .000, η2 = .152.
Table 3.
Comparison of mean differences of body dissatisfaction (BSQ), weight bias and psychological distress (GSI) by eating behavior groups.
| Variable | Eating disorder | Nonclinical binging | No diagnosis | ED vs NCB (95% CI) | ED vs ND (95% CI) |
|---|---|---|---|---|---|
| BSQ | 94.6 (47.6) | 63.1 (30.2) | 58.7 (27.1) | 7.4, 55.6 | 14.2, 57.7 |
| Weight bias | 93.3 (109.6) | 31.4 (35.5) | 21.8 (34.1) | 21.9,102 | 35.3, 107.6 |
| GSI | 1.40 (0.97) | 0.59 (0.54) | 0.63 (0.71) | 0.31,1.40 | 0.32, 1.30 |
Note: Cells contain mean (SD). 95% CIs are Bonferroni adjusted. CIs that do not include 0 are statistically significant. ED = eating disorder, NCB = nonclinical binging, ND = no diagnosis.
Discussion
We examined the relationship between eating behaviors, WB, and psychological distress in a sample of multi-ethnic low-income adolescents. We found a high prevalence of both disordered eating and WB in our sample. Similar to other studies, high rates (28%) of nonclinical binging were reported (Ackard et al., 2007; Decaluwé, Braet, & Fairburn, 2003). This is concerning because not only can disordered eating worsen over time and eventually meet the criteria for an eating disorder (Neumark-Sztainer et al., 2011), but disordered eating can also cause weight gain and obesity (Field et al., 2007; Neumark-Sztainer et al., 2011; Tanofsky-Kraff et al., 2006). Our sample suggested high rates of eating disorders, 15% of our sample compared to 3% of the national average (Swanson, Crow, LeGrange, Swendson, & Merikangas, 2011). The reasons for the high prevalence of eating disorders in our study are not known. One possibility could be that adolescents in low-income areas are experiencing more eating disorders for such reasons as food insecurities, trauma, ethnicity, educational status and obesity. Researchers have found a higher prevalence of eating disorder and binge eating among low-income adolescents (de Souza Ferreira & da Veiga, 2008; J. G. Johnson, Cohen, Kasen, & Brook, 2002) as well as in ethnically diverse low-income college students (Gentile et al., 2007). Other possible explanations could be an overestimation of binge eating in self-report questionnaires and the small sample size. A larger multi-ethnic low-income adolescent sample is warranted in future research. Further investigations are also needed to evaluate whether food insecurities, trauma, and educational status increase the risk for development of eating disorders in low-income diverse youth.
More than half (58%) of our sample reported having at least one stigmatizing experience in their lives. Participants who were not overweight or obese also experienced discrimination, which is concerning because research has shown trends towards weight gain with perceived WB across all BMI groups (Jackson, Beeken, & Wardle, 2014; Sutin & Terracciano, 2013). The majority of the stigma reported came from peers, other children and their parents. This is an important finding because a longitudinal study examining WB and adverse eating and weight related outcomes found WB from both family and peers predicted unhealthy weight control behaviors and higher body dissatisfaction in females and higher BMI in males (Puhl et al., 2017). Our results also indicate WB was positively correlated with BMI which is consistent with previous reports (Bucchianeri et al., 2014; Feeg et al., 2014; Friedman et al., 2005; Puhl, Peterson, & Luedicke, 2013). It is evident from these results that low-income overweight and obese adolescents are dealing with stigmatizing experiences related to weight. Also, our findings indicate that WB correlated highly with psychological distress. In other words, those encountering WB exhibited clear signs of body image disturbance and altered psychological functioning. However, we were not able to determine whether other factors were associated with psychological distress considering these adolescents came from low-income neighborhoods with potential exposure to other adverse events.
The highest levels of WB were reported by the eating disordered and obese group in our sample. This finding is similar to other studies demonstrating the highest amount of WB occurred in youth with higher BMIs (Hayden-Wade et al., 2005; Puhl et al., 2017), which can increase the risk of body dissatisfaction, depressive symptoms and suicidal ideation (Russell-Mayhew, McVey, Bardick, & Ireland, 2012; Taylor, 2011). This finding is supportive of the data that shows that eating can be used as a coping mechanism to counter the effects of distress experienced from WB (Hübner et al., 2016; Puhl et al., 2017; Puhl & Brownell, 2006). WB is not the only pathway to disordered eating and obesity, but it is a risk factor that has been identified in previous studies (Kirsch, Shapiro, Conley, & Heinrichs, 2016; Neumark-Sztainer et al., 2007; Puhl et al., 2017). A recent longitudinal study found WB during childhood may lead to emotional eating negatively affecting long-term weight loss maintenance in adulthood (Hübner et al., 2016). Therefore, WB interventions should be considered in the prevention of both eating disorders and obesity.
Gender differences in this study were similar to previous research indicating females had higher levels of body dissatisfaction and psychological distress (Eisenberg, Neumark-Sztainer, & Paxton, 2006; Lawler & Nixon, 2011; Santos, Richards, & Bleckley, 2007; von Soest & Wichstrøm, 2008) than males. Previous studies have indicated that body dissatisfaction and psychological functioning may contribute to obesity and negative health outcomes (Durso, Latner, & Ciao, 2016; Muennig, Jia, Lee, & Lubetkin, 2008; Wilson, Latner, & Hayashi, 2013). Our data showed no gender differences in WB contrary to other studies, where girls reported more WB than boys (Eisenberg, Neumark-Sztainer, Haines, & Wall, 2006; Neumark-Sztainer et al., 2002). In addition to elucidating gender differences with WB, future researchers should focus on exploring the types of bias and the perceptions and internationalization of bias which may be more crucial than the amount of bias experienced in this population (Lewis et al., 2011).
Examining ethnic differences in our study revealed higher levels of eating disorders and WB in African Americans than in Latinos, but these differences did not reach statistical significance. With conflicting data on ethnic differences in the adult population and limited data in low income ethnically diverse adolescent population, further research is needed on WB and eating behaviors with a larger sample size and broader geographical locations.
We found associations between BMI, body dissatisfaction, weight bias, and psychological distress which are supported in the literature (Durso & Latner, 2008; Durso et al., 2016; Eisenberg et al., 2006; Stice et al., 2000). It is difficult to determine causation from this study, and whether weight change precipitated WB or WB leads to increases in BMI. Sutin and Terracciano (2013) found a correlation between WB, weight gain, and obesity with non-obese participants who reported WB at baseline being 2.5 times more likely to be obese at follow up 4 years later. This research and other studies reveal the difficulty with weight loss (Wott & Carels, 2010) and weight loss maintenance (Hübner et al., 2016) secondary to WB, adding the negative consequences of stigma and highlighting the importance of prevention of WB in adolescents.
Finally, the relationship of eating behavior to body dissatisfaction, psychological distress, and weight bias was investigated. Supported by previous studies, our findings suggest the eating disorder group had the highest level of reported WB (Ackard et al., 2011; Almeida et al., 2011; Durso & Latner, 2008). It is interesting to note that those who did not report any disordered eating had higher levels of psychological distress than those reporting disordered eating. There may be other factors that may explain psychological distress in low-income adolescents that warrant further investigation.
Certain limitations must be considered when interpreting the results from this study. First, the study utilized a descriptive cross-sectional study design; causation and directionality between disordered eating, WB, and psychological distress cannot be determined. Second, Hispanic participants accounted for 48% of our study sample and were assessed as a monolithic group. The small sample size might not be representative of the overall Hispanic population. This methodological concern will be noted for future studies as it limits data specificity unique to each group. Third, the QWEP-A may not be the best tool to assess eating behaviors in this population. A number of participants, especially the younger adolescents, found it challenging to use this tool and asked clarifying questions during the study. It is difficult to determine whether language factored into this considering 48% of our sample was Latino from predominately Spanish speaking neighborhoods. The tool was also difficult to analyze due to the categorical nature of the responses. Also, the tool was designed to measure and quantify binging and disordered eating/eating disorders, which may be more accurately assessed in face to face structured interviews of both adolescents and their parents rather than in a self-report questionnaire. Fourth, the SSI-A was revised but requires factor analysis, which was beyond the scope of this study. Fifth, body dissatisfaction and disordered eating are influenced by many other factors such as media, culture, family and social support, all of which were not explored in this study. The study was limited in a geographical area with a small sample size. Further exploration of WB and disordered eating in low-income multi-ethnic adolescents over a longer period of time is needed.
Despite these limitations, this study provides key information concerning the incidence and relationship of eating behaviors and WB in multi-ethnic and low-income. Our results have clinical implications that underscore the need to develop interventions addressing both disordered eating and WB in order to arrest the rates of childhood obesity.
Nursing Implications
Nurses can be change agents and are the advocates and health educators for families, patients, and communities. They can serve as role models to other healthcare providers, educators, school counselors, administrators, coaches and increase awareness of disordered eating and WB. Nurses and Nurse Practitioners, especially those in schools and primary care settings, can take a few steps in addressing WB. The first step is to provide information to others on all contributors of obesity including genetic, environmental, biological, psychological, and social factors. This will help address the common and simplistic assumption among healthcare providers and the public that weight gain and weight loss is about calories and exercise alone. The next step is to strive towards ensuring a welcoming and safe environment for obese individuals in schools, clinics and other healthcare facilities. This involves adjusting the physical environment and interaction with obese patients. Nurses are trained in therapeutic communication and can teach others to use patient-centered communication strategies. Finally, nurses should be involved in researching and evaluating interventions to reduce weight bias and disordered eating.
Conclusion
This study is the first to examine disordered eating and WB in exclusively multi-ethnic and low-income adolescent population. We found a high prevalence of eating disorders in both ethnic groups with eating disordered participants experiencing the highest levels of WB, body dissatisfaction, and psychological distress. This study supports findings from previous studies and adds to the literature that overweight and obese adolescents report increasing levels of disordered eating, WB, body dissatisfaction, and psychological distress. Additionally, non-overweight participants experienced WB, which should be considered when designing interventional studies to reduce WB. Future studies are needed to identify and evaluate community and school-based interventions to minimize WB and disordered eating. Research strongly supports the inclusion of content on prevention of eating disorders and WB in school-based curriculum (Aimé, LeBlanc, & Maïano, 2017; Puhl, Neumark-Sztainer, Austin, Suh, & Wakefield, 2016) and implementing school-based policies, with educators, school counselors, administrators, coaches, school nurses, parents, and students, to address weight bias (Puhl et al., 2016; Puhl, Neumark-Sztainer, Austin, Luedicke, & King, 2014) and disordered eating in schools (Neumark-Sztainer, Story, & Coller, 1999; Puhl et al., 2016; Yager & O’Dea, 2005).
Acknowledgements
This study was supported by Sigma Theta Tau International Gamma Tau-at-Large Chapter. The authors express their appreciation to Dr. Peggy Compton for providing support and encouragement during the final stages of this research. We are immensely grateful to Dr. Bernard Weiner for his insight on an earlier version of this manuscript. Special thanks to Dr. Judith Baggs, Dr. Angie Docherty, and Patti Warkentin for editorial feedback and Dr. Nathan Dieckmann for statistical expertise.
Funding
This research was funded by Sigma Theta Tau International Gamma Tau-at-Large Chapter.
Footnotes
Declaration of Interest
The authors report no declarations of interest.
Conflict of Interest
None of the authors has any actual or potential conflict of interest including any financial, personal, or other relationships with people or organizations that could inappropriately influence or be perceived to influence this work.
References
- Ackard DM, Fulkerson JA, & Neumark-Sztainer D (2007). Prevalence and utility of DSM-IV eating disorder diagnostic criteria among youth. International Journal of Eating Disorders, 40, 409–417. 10.1002/eat.20389. [DOI] [PubMed] [Google Scholar]
- Ackard DM, Fulkerson JA, & Neumark-Sztainer D (2011). Psychological and behavioral risk profiles as they relate to eating disorder diagnoses and symptomatology among a school-based sample of youth. International Journal of Eating Disorders, 44, 440–446. 10.1002/eat.20846. [DOI] [PubMed] [Google Scholar]
- Aimé A, LeBlanc L, & Maïano C (2017). Is weight-related bullying addressed in school-based anti-bullying programs? Revue Européenne de Psychologie Appliquée/European Review of Applied Psychology, 67, 163–169. 10.1016/j.erap.2017.02.001. [DOI] [Google Scholar]
- Almeida L, Savoy S, & Boxer P (2011). The role of weight stigmatization in cumulative risk for binge eating. Journal of Clinical Psychology, 67, 278–292. 10.1002/jclp.20749. [DOI] [PubMed] [Google Scholar]
- Andreyeva T, Puhl RM, & Brownell KD (2008). Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity, 16, 1129–1134. 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- Annis NM, Cash TF, & Hrabosky JI (2004). Body image and psychosocial differences among stable average weight, currently overweight, and formerly overweight women: The role of stigmatizing experiences. Body Image, 1, 155–167. 10.1016/j.bodyim.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Babey SH, Hastert TA, Wolstein J, & Diamant AL (2010). Income disparities in obesity trends among California adolescents. American Journal of Public Health, 100, 2149–2155. 10.2105/AJPH.2010.192641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow SE (2007). Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics, 120(Supplement), S164–S192. 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Bucchianeri MM, Eisenberg ME, Wall MM, Piran N, & Neumark-Sztainer D (2014). Multiple types of harassment: Associations with emotional well-being and unhealthy behaviors in adolescents. Journal of Adolescent Health, 54, 724–729. 10.1016/j.jadohealth.2013.10.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, & Neumark-Sztainer D (2008). Are body dissatisfaction, eating disturbance, and body mass index predictors of suicidal behavior in adolescents? A longitudinal study. Journal of Consulting and Clinical Psychology, 76, 887–892. 10.1037/a0012783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decaluwé V, Braet C, & Fairburn CG (2003). Binge eating in obese children and adolescents. The International Journal of Eating Disorders, 33, 78–84. 10.1002/eat.10110. [DOI] [PubMed] [Google Scholar]
- Durso LE, & Latner JD (2008). Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity, 16(Suppl. 2), S80–S86. 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, & Ciao AC (2016). Weight bias internalization in treatment-seeking overweight adults: Psychometric validation and associations with self-esteem, body image, and mood symptoms. Eating Behaviors, 21, 104–108. 10.1016/j.eatbeh.2016.01.011. [DOI] [PubMed] [Google Scholar]
- Eisenberg M, Neumark-Sztainer D, Haines J, & Wall M (2006). Weight-teasing and emotional well-being in adolescents: Longitudinal findings from project EAT. Journal of Adolescent Health, 38, 675–683. 10.1016/j.jadohealth.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Berge JM, Fulkerson JA, & Neumark-Sztainer D (2012). Associations between hurtful weight-related comments by family and significant other and the development of disordered eating behaviors in young adults. Journal of Behavioral Medicine, 35, 500–508. 10.1007/s10865-011-9378-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, & Paxton SJ (2006). Five-year change in body satisfaction among adolescents. Journal of Psychosomatic Research, 61, 521–527. 10.1016/j.jpsychores.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Feeg VD, Candelaria LM, Krenitsky-Korn S, & Vessey JA (2014). The relationship of obesity and weight gain to childhood teasing. Journal of Pediatric Nursing, 29, 511–520. 10.1016/j.pedn.2014.08.011. [DOI] [PubMed] [Google Scholar]
- Field AE, Aneja P, Austin SB, Shrier LA, de Moor C, & Gordon-Larsen P (2007). Race and gender differences in the association of dieting and gains in BMI among young adults. Obesity, 15, 456–464. 10.1038/oby.2007.560. [DOI] [PubMed] [Google Scholar]
- Friedman KE, Reichmann SK, Costanzo PR, Zelli A, Ashmore JA, & Musante GJ (2005). Weight stigmatization and ideological beliefs: Relation to psychological functioning in obese adults. Obesity Research, 13, 907–916. 10.1038/oby.2005.105. [DOI] [PubMed] [Google Scholar]
- Gentile K, Raghavan C, Rajah V, & Gates K (2007). It doesn’t happen here: Eating disorders in an ethnically diverse sample of economically teasing experiences among students. Eating Disorders, 15, 405–425. 10.1080/10640260701667904. [DOI] [PubMed] [Google Scholar]
- Gleason JH, Alexander AM, & Somers C (2000). Later adolescents’ reactions to three types of childhood teasing: Relations with self-esteem and body image. Social Behavior and Personality, 28, 471–480. 10.2444/sbp.2000.28.5.471. [DOI] [Google Scholar]
- Hastert TA, Babey SH, Diamant AL, & Brown ER (2008). Low-income adolescents face more barriers to healthy weight. Policy Brief (UCLA Center for Health Policy Research)(PB2008–4), 1–8. [PubMed] [Google Scholar]
- Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, & Wilfley DE (2005). Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research, 13, 1381–1392. 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- Hübner C, Schmidt R, Selle J, Köhler H, Müller A, de Zwaan M, & Hilbert A (2016). Comparing self-report measures of internalized weight stigma: The Weight Self-Stigma Questionnaire versus the Weight Bias Internalization Scale. PLoS ONE, 11(10), e0165566. 10.1371/journal.pone.0165566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SE, Beeken RJ, & Wardle J (2014). Perceived weight discrimination and changes in weight, waist circumference, and weight status: Weight discrimination and changes in weight. Obesity, 22, 2485–2488. 10.1002/oby.20891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, & Brook JS (2002). Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. The American Journal of Psychiatry, 159, 394–400. 10.1176/appi.ajp.159.3.394. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Grieve FG, Adams CD, & Sandy J (1999). Measuring binge eating in adolescents: Adolescent and parent versions of the questionnaire of eating and weight patterns. The International Journal of Eating Disorders, 26, 301–314. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Kirk AA, & Reed AE (2001). Adolescent version of the questionnaire of eating and weight patterns: Reliability and gender differences. The International Journal of Eating Disorders, 29, 94–96. [DOI] [PubMed] [Google Scholar]
- Kirsch AC, Shapiro JB, Conley CS, & Heinrichs G (2016). Explaining the pathway from familial and peer social support to disordered eating: Is body dissatisfaction the link for male and female adolescents? Eating Behaviors, 22, 175–181. 10.1016/j.eatbeh.2016.06.018. [DOI] [PubMed] [Google Scholar]
- Latner JD, & Stunkard AJ (2003). Getting worse: The stigmatization of obese children. Obesity Research, 11, 452–456. 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- Lawler M, & Nixon E (2011). Body dissatisfaction among adolescent boys and girls: The effects of body mass, peer appearance culture and internalization of appearance ideals. Journal of Youth and Adolescence, 40, 59–71. 10.1007/s10964-009-9500-2. [DOI] [PubMed] [Google Scholar]
- Le Grange D, O’Connor M, Hughes EK, Macdonald J, Little K, & Olsson CA (2014). Developmental antecedents of abnormal eating attitudes and behaviors in adolescence. International Journal of Eating Disorders, 47, 813–824. 10.1002/eat.22331. [DOI] [PubMed] [Google Scholar]
- Lewis S, Thomas SL, Blood RW, Castle DJ, Hyde J, & Komesaroff PA (2011). How do obese individuals perceive and respond to the different types of obesity stigma that they encounter in their daily lives? A qualitative study. Social Science & Medicine, 73, 1349–1356. 10.1016/j.socscimed.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Mamun AA, O’Callaghan MJ, Williams GM, & Najman JM (2013). Adolescents bullying and young adults body mass index and obesity: A longitudinal study. International Journal of Obesity, 37, 1140–1146. 10.1038/ijo.2012.182. [DOI] [PubMed] [Google Scholar]
- Muennig P, Jia H, Lee R, & Lubetkin E (2008). I think therefore I am: Perceived ideal weight as a determinant of health. American Journal of Public Health, 98, 501–506. 10.2105/AJPH.2007.114769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers A, & Rosen JC (1999). Obesity stigmatization and coping: Relation to mental health symptoms, body image, and self-esteem. International Journal of Obesity and Related Metabolic Disorders, 23,221–230. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, & Mulert S (2002). Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity, 26, 123–131. 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Story M, & Coller T (1999). Perceptions of secondary school staff toward the implementation of school-based activities to prevent weight-related disorders: A needs assessment. American Journal of Health Promotion, 13, 153–156. 10.4278/0890-1171-13.3.153. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, & Loth K (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association, 111, 1004–1011. 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & Standish AR (2012). Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. Journal of Adolescent Health, 50, 80–86. 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, & van den Berg PA (2007). Shared risk and protective factors for overweight and disordered eating in adolescents. American Journal of Preventive Medicine, 33, 359–369. 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2014). Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA, 311, 806. 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Miller J, Ackard DM, Loth KA, Wall MM, Haynos AF, & Neumark-Sztainer D (2017). Stability and change in patterns of eating disorder symptoms from adolescence to young adulthood. International Journal of Eating Disorders, 50, 748–757. 10.1002/eat.22692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R, Peterson JL, & Luedicke J (2013). Fighting obesity or obese persons? Public perceptions of obesity-related health messages. International Journal of Obesity, 37, 774–782. 10.1038/ijo.2012.156. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Andreyeva T, & Brownell KD (2008). Perceptions of weight discrimination: Prevalence and comparison to race and gender discrimination in America. International Journal of Obesity, 32, 992–1000. 10.1038/ijo.2008.22. [DOI] [PubMed] [Google Scholar]
- Puhl RM, & Brownell KD (2006). Confronting and coping with weight stigma: An investigation of overweight and obese adults. Obesity, 14, 1802–1815. 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Neumark-Sztainer D, Austin SB, Luedicke J, & King KM (2014). Setting policy priorities to address eating disorders and weight stigma: Views from the field of eating disorders and the US general public. BMC Public Health, 14, 524. 10.1186/1471-2458-14-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Neumark-Sztainer D, Austin SB, Suh Y, & Wakefield DB (2016). Policy actions to address weight-based bullying and eating disorders in schools: Views of teachers and school administrators. The Journal of School Health, 86, 507–515. 10.1111/josh.12401. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Wall MM, Chen C, Bryn Austin S, Eisenberg ME, & Neumark-Sztainer D (2017). Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: A 15-year longitudinal study. Preventive Medicine, 100, 173–179. 10.1016/j.ypmed.2017.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers RF, Watts AW, Austin SB, Haines J, & Neumark-Sztainer D (2017). Disordered eating in ethnic minority adolescents with overweight: Ethnic minority with overweight. International Journal of Eating Disorders, 50, 665–671. 10.1002/eat.22652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Cano T, Beato-Fernández L, & Llario AB (2006). Body dissatisfaction as a predictor of self-reported suicide attempts in adolescents: A Spanish community prospective study. The Journal of Adolescent Health, 38, 684–688. 10.1016/j.jadohealth.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Rosen JC, Jones A, Ramirez E, & Waxman S (1996). Body Shape Questionnaire: Studies of validity and reliability. The International Journal of Eating Disorders, 20, 315–319. . [DOI] [PubMed] [Google Scholar]
- Russell-Mayhew S, McVey G, Bardick A, & Ireland A (2012). Mental health, wellness, and childhood overweight/obesity. Journal of Obesity, 2012, 1–9. 10.1155/2012/281801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadowski CM, & Friedrich WN (2000). Psychometric properties of the Trauma Symptom Checklist for Children (TSCC) with psychiatrically hospitalized adolescents. Child Maltreatment, 5, 364–372. 10.1177/1077559500005004008. [DOI] [PubMed] [Google Scholar]
- Santos M, Richards CS, & Bleckley KM (2007). Comorbidity between depression and disordered eating in adolescents. Eating Behaviors, 8, 440–449. 10.1016/j.eatbeh.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, & Kogan MD (2010). Rising social inequalities in US childhood obesity, 2003–2007. Annals of Epidemiology, 20, 40–52. 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- von Soest T, & Wichstrøm L (2008). The impact of becoming a mother on eating problems. International Journal of Eating Disorders, 41, 215–223. 10.1002/eat.20493. [DOI] [PubMed] [Google Scholar]
- de Souza Ferreira JE, & da Veiga GV (2008). Eating disorder risk behavior in Brazilian adolescents from low socio-economic level. Appetite, 51, 249–255. 10.1016/j.appet.2008.02.015. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Yanovski S, Wadden T, Wing R, Marcus MD, Stunkard A, … Horne RL (1993). Binge eating disorder: Its further validation in a multisite study. The International Journal of Eating Disorders, 13, 137–153. [PubMed] [Google Scholar]
- Stice E, Hayward C, Cameron RP, Killen JD, & Taylor CB (2000). Body-image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology, 109, 438–444. 10.1037/0021-843X.109.3.438. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, & Jaconis M (2009). An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology, 118, 587–597. 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, & Fairburn CG (2000). Recurrent binge eating in black American women. Archives of Family Medicine, 9, 83–87. [DOI] [PubMed] [Google Scholar]
- Sutin AR, & Terracciano A (2013). Perceived weight discrimination and obesity. PLoS ONE, 8(7), e70048. 10.1371/journal.pone.0070048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, LeGrange D, Swendson J, & Merikangas KR (2011). Prevalence and correlates of eating disorders in adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 68, 714. 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takizawa R, Danese A, Maughan B, & Arseneault L (2015). Bullying victimization in childhood predicts inflammation and obesity at mid-life: A five-decade birth cohort study. Psychological Medicine, 45, 2705–2715. 10.1017/S0033291715000653. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, … Yanovski JA (2006). A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics, 117, 1203–1209. 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor NL (2011). “Guys, she’s humongous!”: Gender and weight-based teasing in adolescence. Journal of Adolescent Research, 26, 178–199. 10.1177/0743558410371128. [DOI] [Google Scholar]
- The McKnight Investigators (2003). Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight Longitudinal Risk Factor Study. American Journal of Psychiatry, 160, 248–254. 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- Wilson RE, Latner JD, & Hayashi K (2013). More than just body weight: The role of body image in psychological and physical functioning. Body Image, 10, 644–647. 10.1016/j.bodyim.2013.04.007. [DOI] [PubMed] [Google Scholar]
- Wott CB, & Carels RA (2010). Overt weight stigma, psychological distress and weight loss treatment outcomes. Journal of Health Psychology, 15, 608–614. 10.1177/1359105309355339. [DOI] [PubMed] [Google Scholar]
- Yager Z, & O’Dea JA (2005). The role of teachers and other educators in the prevention of eating disorders and child obesity: What are the issues? Eating Disorders, 13, 261–278. 10.1080/10640260590932878. [DOI] [PubMed] [Google Scholar]


