Abstract
Breathing is silent in health but audible at a distance in chronic bronchitis and asthma. This clinical observation was tested by measurements of the intensity of the inspiratory breath sounds at the mouth at flow rates up to 60 1./min. There was a higher rate of increase in the intensity of the sound for equal increments in flow rate in these two diseases than in healthy subjects. Bronchodilator drugs reduced the intensity of abnormally loud inspiratory sounds.
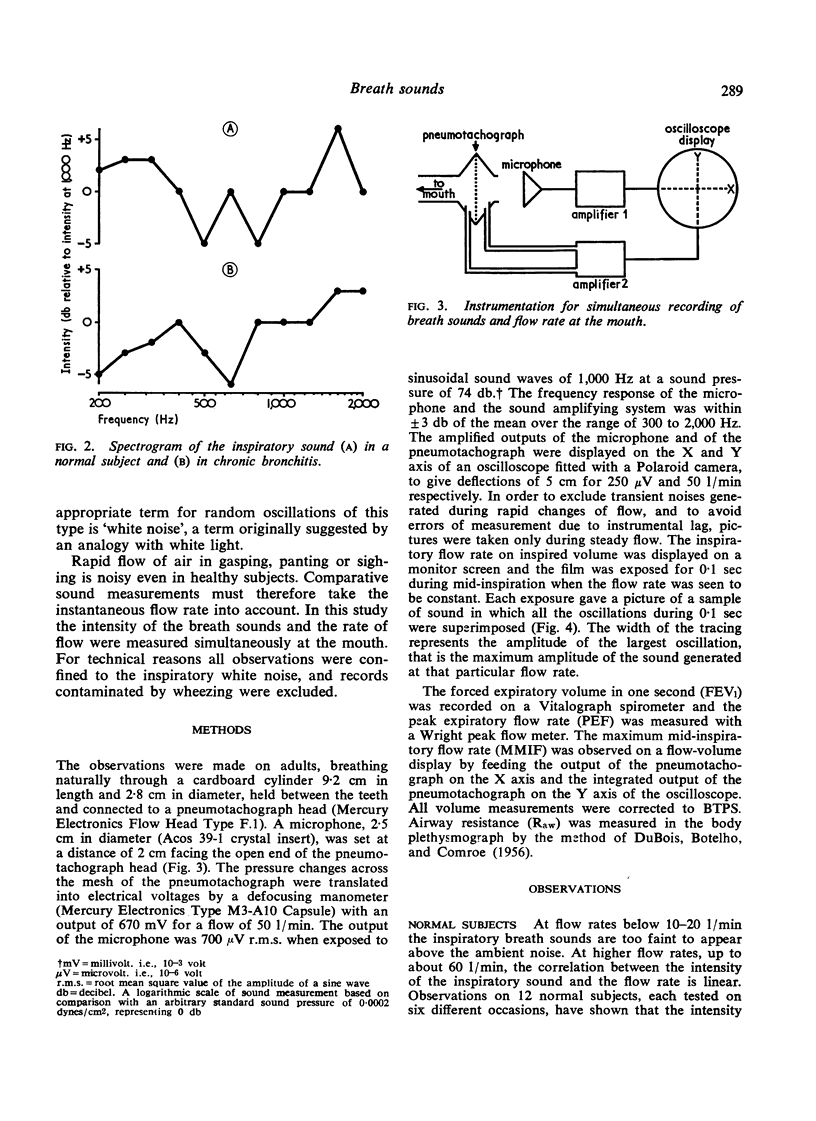
The noise is generated by turbulent flow of air in the upper respiratory tract, the trachea, and the central bronchi. Reduction of bronchial calibre increases flow velocity and intensifies turbulence. The intensity of the inspiratory sound in chronic bronchitis and asthma reflects calibre changes in the trachea, the principal bronchi, and their lobar and segmental branches.
An inverse correlation exists between the intensity of the inspiratory sound, the forced expiratory volume in one second, and the peak expiratory flow rate in chronic bronchitis and asthma, but not in primary emphysema. Discrepancies between sound, airway resistance, and forced expiratory measurements may indicate the site and mechanism of airway obstruction in individual patients.
The sound of inspiration heard with the unaided ear close to the patient's mouth is an important clinical sign. Noisy inspiration is common in chronic bronchitis and asthma, and the degree of narrowing of the central bronchi can be inferred from the loudness of the noise. Silent inspiration in the presence of severe expiratory obstruction is a sign of primary emphysema.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BENTIVOGLIO L. G., BEEREL F., BRYAN A. C., STEWART P. B., ROSE B., BATES D. V. REGIONAL PULMONARY FUNCTION STUDIED WITH XENON IN PATIENTS WITH BRONCHIAL ASTHMA. J Clin Invest. 1963 Aug;42:1193–1200. doi: 10.1172/JCI104805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUBOIS A. B., BOTELHO S. Y., COMROE J. H., Jr A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956 Mar;35(3):327–335. doi: 10.1172/JCI103282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leblanc P., Macklem P. T., Ross W. R. Breath sounds and distribution of pulmonary ventilation. Am Rev Respir Dis. 1970 Jul;102(1):10–16. doi: 10.1164/arrd.1970.102.1.10. [DOI] [PubMed] [Google Scholar]
- Nairn J. R., Turner-Warwick M. Breath sounds in emphysema. Br J Dis Chest. 1969 Jan;63(1):29–37. doi: 10.1016/s0007-0971(69)80041-0. [DOI] [PubMed] [Google Scholar]
- Pedley T. J., Schroter R. C., Sudlow M. F. The prediction of pressure drop and variation of resistance within the human bronchial airways. Respir Physiol. 1970 Jun;9(3):387–405. doi: 10.1016/0034-5687(70)90094-0. [DOI] [PubMed] [Google Scholar]