Abstract
Many low-income Americans experience food insecurity, which may have been exacerbated by economic instability during the early stages of the coronavirus pandemic. We assess the impact of Healthy Helping, a short-term fruit and vegetable incentive program aimed at alleviating food insecurity and improving diet quality for Supplemental Nutrition Assistance Program participants, on grocery purchases, using transaction data from a large supermarket chain in North Carolina. We compare Healthy Helping participants’ purchases of key food groups before and during the program with purchases by control shoppers participating in federal food assistance programs during the same period. Healthy Helping enrollment was associated with a $26.95 increase in monthly spending on fruits, vegetables, nuts, and legumes—an increase of 2.5 grams of fiber per 1,000 kilocalories purchased—and other shifts in the composition of food purchases, relative to control shoppers. These findings suggest that the program increased healthy food purchases while also increasing dollar sales at participating retailers. On average, participants did not use the full benefit; future research should explore factors associated with non- or underuse of benefits to inform program design and outreach.
Keywords: Food Security, Nutrition Policy, Food Assistance, COVID-19
Food insecurity is a major public health problem in the United States1 and is associated with chronic disease risk, including obesity,2 cardiovascular disease,3 and mortality.4 Prior research has linked food insecurity and lower diet quality,5 including reduced consumption of fruits and vegetables.6,7 In 2020 an estimated 10.5 percent of US households were food insecure, with higher prevalence for households with children (14.8 percent), non-Hispanic Black households (21.7 percent), and Hispanic households (17.2 percent).8
Some evidence suggests that food insecurity increased during the COVID-19 pandemic,9–11 although other studies have found no change.8 The pandemic’s impact on diet quality is also unclear, with studies reporting positive and negative changes to food purchasing and consumption, with heterogeneity by subpopulation.12,13 During the pandemic, households reported decreasing the amount of food consumed away from home14 and purchasing more food for cooking and eating at home,15 which has been associated with higher diet quality.16 Nevertheless, some studies have found that lower diet quality among food-insecure households persisted17 and that food-insecure households were more likely to decrease purchases of produce during the pandemic compared with food-secure households.11,18 These findings merit attention, as food-insecure people already experienced an elevated risk for poor diet quality and nutrition-related chronic diseases before the onset of the COVID-19 pandemic.2,3,5
One increasingly popular intervention to alleviate food insecurity and improve diet quality is financially incentivizing the purchase of fruits and vegetables.19 Recent studies suggest that these efforts increase fruit and vegetable purchases and consumption and may reduce cardiometabolic risk factors.20,21 However, most prior studies evaluated produce incentive programs at farmers’ markets, which may be used less frequently by racially and ethnically diverse populations, highlighting the need for incentives usable in other settings.22,23 Previous research on the impact of fruit and vegetable incentives is also limited by reliance on pre-post study designs without a matched control group and use of self-reported purchasing or consumption data.19
This study sought to understand the impact of Healthy Helping, a large-scale short-term COVID-relief fruit and vegetable incentive program, on participants’ purchases, using supermarket transaction data. We aimed to answer the following questions: Was Healthy Helping associated with an increase in purchases of fruits, vegetables, nuts, and legumes among program enrollees and program users? Was Healthy Helping enrollment and use associated with changes in purchases of less-healthy food groups? To address the second objective, we assessed changes in spending on food groups that are overconsumed in the US24 and contribute substantially to total energy, saturated fat, sodium, and sugar intake in the US25 Furthermore, we conducted exploratory analyses assessing the association between Healthy Helping participation and nutrient density of purchases.
Study Data And Methods
This longitudinal cohort study used loyalty card transaction data from a large supermarket chain with approximately 500 stores in North Carolina (we are unable to name the retailer, following data agreements). The analytic data set comprised all purchases made by households participating in the Supplemental Nutrition Assistance Program (SNAP) at the chain between October 2019 and December 2020. We defined SNAP participation as payment with an Electronic Benefits Transfer card at least once in a rolling three-month period. The transaction data included the UPC (barcode), quantity, volume, dollars spent, and payment code for each item. Food items were linked to nutrition facts panel information, as described in prior work,26 and categorized into seven food groups of interest (online appendix exhibit A1).27 We were not able to link all products to nutrition facts panel data (percentage of missing products by category ranged from 4.4 percent to 25.3 percent). All transactions were aggregated to the shopper ID-month level, so that each observation represents all purchases by a given store loyalty card number in a month. Although we refer to an individual store loyalty card number as a “shopper ID” or “shopper,” multiple people or household members may use a particular store loyalty card—however, we are unable to determine this using the available data.
Funded by the North Carolina General Assembly’s disbursement of Coronavirus Aid, Relief, and Economic Security Act of 2020 funding, Healthy Helping provided $40 per month for the purchase of fresh, frozen, or canned fruits and vegetables with no added sugar, added sodium, or added fat for a rolling three-month period. Funds were linked to customer store loyalty cards and could be used at any of the supermarket chain’s locations in North Carolina. Eligible items were identified automatically at checkout by a unique offer code. The cost of the items was then deducted from the shopper’s available Healthy Helping funds and the remaining monthly balance was printed at the bottom of the receipt.
To be eligible for Healthy Helping, people had to be current SNAP participants, ages eighteen or older, reside in North Carolina, and self-report being negatively affected by the COVID-19 pandemic. Eligible people were enrolled in Healthy Helping after calling a COVID-19 relief hotline funded by the North Carolina Department of Health and Human Services, as well as through recruitment and enrollment at forty-seven Division of Social Services county agencies and federally qualified health clinics across North Carolina on a rolling basis from June to December 2020 (see appendix exhibit A2 for more detail).27 Participants completed a brief screener on enrollment, including the Department of Agriculture (USDA) Six-Item Food Security Scale.28 Participants were enrolled in the program for three months or until December 31, 2020 (when the funds expired), whichever occurred first. Post–Healthy Helping observations were dropped if the shopper ID had no further Healthy Helping spending. If participants did not spend the full benefit amount during their three-month intervention period, benefits rolled over for two additional months.
The primary outcome of interest was total spending (in US dollars) on fruits, vegetables, nuts, and legumes. We also examined volume (in ounces) of fruits, vegetables, nuts, and legumes purchased and the percentage of total food and beverage spending on these items. For our second objective of understanding Healthy Helping’s impact on the overall healthfulness of shoppers’ purchases, we examined spending on six categories of less-healthy products (candy, desserts and sweet snacks, processed meats and seafood, salty snacks, sugar-sweetened beverages, and sweeteners and toppings). We also assessed dollars spent on each product category as a percentage of total food and beverage spending to account for possible changes in overall spending at the chain during the program. Finally, we conducted exploratory analyses to understand changes in the nutrient density of purchases.
Statistical Analysis
We used a difference-in-differences approach to estimate changes in food purchases among Healthy Helping participants before and during the program, relative to control shoppers. Controls were selected from SNAP participants who were not enrolled in Healthy Helping or another concurrent fruit and vegetable incentive program delivered through this retailer. Because of Healthy Helping’s rolling enrollment, we randomly assigned control shoppers an enrollment date (“index month”) matching the distribution of Healthy Helping enrollment. We then generated propensity scores for each shopper, using logistic regression to predict the probability of Healthy Helping enrollment based on pre-index month shopping (see appendix exhibit A3 for a list of included variables.27 Each shopper was assigned an overlap weight based on their estimated probability of being in the opposite group. Overlap weights create exactly balanced means across groups for all variables included in the logistic regression.29,30 We restricted our analyses to shoppers that had at least one shopper-month observation before their index month to generate the overlap weights.
To assess changes in purchases associated with Healthy Helping participation, we ran separate linear mixed models with overlap weights for each outcome, adjusted for month and year; participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in the previous three months; urbanicity of most frequently visited store (rural, suburban, or urban); and number of months of post–index period observations. We included random intercepts for most frequently visited store and shopper ID to account for repeated measures. We controlled for WIC participation as the amount of the cash value benefit for fruits and vegetables increased during the pandemic. We measured urbanicity on the basis of the location of the shopper ID’s most frequented store. Models included month and year to account for seasonality and the number of post–index month observations to address potential imbalances in follow-up time between groups. The coefficient of interest was the interaction between treatment group and time (pre– or post–index date).
For the main analyses, the exposure of interest was Healthy Helping enrollment, which allowed us to estimate the average treatment effect across Healthy Helping enrollees, regardless of actual program use. Because we were also interested in the effect of the Healthy Helping program among program users specifically (that is, the average treatment effect on the treated), we reran the analyses with date of first use of Healthy Helping funds, rather than enrollment date, as the exposure, excluding enrollees who did not use any Healthy Helping funds and dropping months in which a shopper was enrolled but had not yet used Healthy Helping funds.
We also conducted exploratory analyses to assess differences in the nutrient density of purchases, using the same linear mixed modeling approach as in the main analyses, while additionally controlling for the proportion of purchases in each category with missing nutrition information. Changes in nutrient density are reported in terms of grams of each nutrient per 1,000 kilocalories purchased.
Finally, because a substantial number of Healthy Helping participants did not have preenrollment purchasing data and were thus not included in the main analyses, we conducted sensitivity analyses (available in the appendix),27 including all shoppers who used Healthy Helping, even if they had no pre-enrollment purchases. Because the weights were based on pre–index date purchases and could not be generated for shoppers with no pre–index date purchasing data, we ran the same analyses described above but did not use the overlap weights (that is, unweighted analyses; see appendix exhibit A6).27
Data analysis was performed using Stata, version 16. A two-sided p value of 0.05 was set to denote statistical significance. The study was deemed to be not human subjects research by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Limitations
This study has several limitations. First, we only had purchasing data from one supermarket chain, rather than all sources of food acquisition, so we could not determine how Healthy Helping may have affected the overall nutritional quality of household purchases or dietary intake. Second, the supermarket transaction data contain no information about customer sociodemographic characteristics. Thus, we were unable to match our control group on potentially relevant demographic factors and had to rely on prior purchasing history, preferred store location, and payment sources. As a consequence, we were not able to make inferences about subpopulations. Furthermore, there could be other unobservable characteristics that we were unable to match on that may have introduced bias. Finally, we relied on loyalty cards to identify Healthy Helping and control shoppers, and thus only included transactions for which customers used their loyalty cards. This may not be a large limitation, as loyalty cards provide discounts to customers, thereby incentivizing their use.
Study Results
The data set included purchases from 28,927 people enrolled in Healthy Helping who shopped at the retailer using their loyalty card at least once during the study period. Of these people, 19,722 (68 percent) had pre–index month data (that is, they used their loyalty card before Healthy Helping enrollment) and were included in the main analysis, contributing 208,601 shopper-month observations over the course of fifteen months. The control group included 86,034 shoppers with 804,481 shopper-month observations. Healthy Helping enrollment spanned June–December 2020, although most participants were enrolled in September and October (exhibit 1). The majority of Healthy Helping participants most frequently shopped at a participating store in an urban county (55.7 percent). Food insecurity at enrollment was high, with 85.4 percent of the analytic sample reporting low or very low food security.
Exhibit 1:
Sample characteristics, Healthy Helping study, program enrollment and transaction data from a supermarket chain in North Carolina, October 2019–December 2020
| Enrolled in Healthy Helping and ever shopped at supermarket chain (n = 28,927) | Enrolled in Healthy Helping and had pre- and postintervention data for intent-to-treat analyses (main analysis cohort) (n = 19,722) | Used Healthy Helping and had pre- and postintervention data for treatment-on-treated analyses (n = 18,970) | ||||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Food insecure | 21,490 | 85.37a | 14,716 | 85.42b | 14,156 | 85.5c |
| Urbanicity | ||||||
| Urban | 15,988 | 55.27 | 10,987 | 55.71 | 10,580 | 55.77 |
| Suburban | 8,677 | 30.00 | 5,860 | 29.71 | 5,634 | 29.70 |
| Rural | 4,262 | 14.73 | 2,875 | 14.57 | 2,756 | 14.53 |
| Enrollment month | ||||||
| June | 10 | 0.03 | 5 | 0.03 | 4 | 0.02 |
| July | 692 | 2.39 | 402 | 2.05 | 375 | 1.98 |
| August | 6,265 | 21.66 | 4,275 | 21.68 | 4,089 | 21.56 |
| September | 11,578 | 40.02 | 8,010 | 40.61 | 7,769 | 40.95 |
| October | 10,277 | 35.53 | 6,958 | 35.28 | 6,666 | 35.14 |
| November | 84 | 0.29 | 59 | 0.30 | 57 | 0.30 |
| December | 21 | 0.07 | 13 | 0.07 | 10 | 0.05 |
SOURCE Authors’ analysis of program enrollment data and transaction data from a supermarket chain in North Carolina, October 2019–December 2020. NOTES Food security was assessed using the 6-item Department of Agriculture screener (see US Department of Agriculture, Economic Research Service. US household food security survey module: Six-item short form. See note 28 in text.) during Healthy Helping enrollment. People with low or very low food insecurity were classified as food insecure. Urbanicity was determined according to the federal Office of Management and Budget and the North Carolina Rural Center designation for each county; counties classified as “urban” or “rural” by both definitions were categorized as such, whereas counties with discordant classifications were categorized as “suburban.”
Of those who completed the screener (n = 25,174).
Of those who completed the screener (n = 17,228).
Of those who completed the screener (n = 16,556).
In the pre–index month period, unweighted mean monthly spending on food and beverages was higher among control shoppers than Healthy Helping participants ($195.81 [standard deviation (SD): $167.58] versus $180.32 [SD: $160.85]; p < 0.001) (appendix exhibit A4).27 Mean unweighted monthly spending in the control group was higher for all food and beverage categories of interest, including fruits, vegetables, nuts, and legumes ($23.27 [SD: $24.47] versus $21.98 [SD: $23.10]; p < 0.001), although the difference between groups did not exceed $2.00 for any category and was not statistically significant for sweeteners and toppings. As intended, after applying overlap weighting, the weighted means were balanced in the two groups for all variables included in the propensity score–generating process. For example, the weighted mean total spending on foods and beverages in the pre–index month period was $182.36 [SD: 163.74] among Healthy Helping participants and $182.36 [SD: 155.56] in the control group.
Exhibit 2 shows the difference-in-differences estimates for the changes in spending (overall and by category) before and during the program among Healthy Helping participants, relative to control shoppers during the same period. Mean total monthly spending increased by $57.34 in the Healthy Helping group compared with the control group. The primary outcome of interest—change in spending on fruits, vegetables, nuts, and legumes—increased by $26.95 in the Healthy Helping group relative to the control group (complete regression output is available in appendix exhibit A5),27 largely driven by increases in fruits, vegetables, nuts, and legumes without any added sugar, added sodium, or added fats. This rise in spending resulted in an increase in the volume of fruit, vegetable, nut, and legume purchases of 237.8 ounces per month over the change in purchase volume among control shoppers. The relative share of all food and beverage spending used for fruits, vegetables, nuts, and legumes increased by 13 percent among Healthy Helping shoppers.
Exhibit 2:
Changes in supermarket spending among Healthy Helping enrollees relative to controls, North Carolina, October 2019–December 2020
| Variable | Estimate | 95% CI |
|---|---|---|
| Total spending ($ per month) | 57.34 | 55.37, 59.30 |
| Food and beverage spending | ||
| Dollars spent ($ per month) | 55.32 | 53.52, 57.13 |
| Fruits, vegetables, nuts, and legumes | ||
| Dollars spent ($ per month) | 26.95 | 26.53, 27.37 |
| Relative share of food and beverage spending (%) | 12.99 | 12.58, 13.40 |
| Volume (ounces) | 237.79 | 233.37, 242.21 |
| Fruits, vegetables, nuts, and legumes with no added sugar, salt, or fat | ||
| Dollars spent ($ per month) | 25.36 | 24.96, 25.76 |
| Relative share of food and beverage spending (%) | 12.94 | 12.52, 13.35 |
| Candy, chocolate, and gum | ||
| Dollars spent ($ per month) | 0.57 | 0.51, 0.63 |
| Relative share of FB spending (%) | −0.20 | −0.24, −0.15 |
| Dessert and sweet snacks | ||
| Dollars spent ($ per month) | 2.80 | 2.58, 3.03 |
| Relative share of food and beverage spending (%) | −1.51 | −1.64, −1.39 |
| Processed meats and seafood | ||
| Dollars spent ($ per month) | 2.84 | 2.60, 3.09 |
| Relative share of food and beverage spending (%) | −1.29 | −1.41, −1.18 |
| Salty snacks | ||
| Dollars spent ($ per month) | 1.68 | 1.52, 1.84 |
| Relative share of food and beverage spending (%) | −0.83 | −0.91, −0.75 |
| Sugar-sweetened beverages | ||
| Dollars spent ($ per month) | 2.84 | 2.56, 3.12 |
| Relative share of food and beverage spending (%) | −2.53 | −2.72, −2.34 |
| Sweeteners and toppings | ||
| Dollars spent ($ per month) | 0.33 | 0.29, 0.38 |
| Relative share of food and beverage spending (%) | −0.17 | −0.20, −0.14 |
SOURCE Authors’ analysis of data from a supermarket chain in North Carolina, October 2019–December 2020. NOTES Intent to treat models include data from 19,722 Healthy Helping enrollees (208,601 shopper-months) and 86,034 control shoppers (804,481 shopper-months). Estimates are from linear mixed models with terms for Healthy Helping participation, time (pre– and post–index month), and a Healthy Helping-by-time product term. All estimates were statistically significantly different from 0 at the p < 0.001 level. Models were also adjusted for month and year; Special Supplemental Nutrition Program for Women, Infants, and Children use; urbanicity of most frequent store; and number of months of follow-up, with the shopper-month as the unit of analysis. Models include random intercepts for most frequent store and shopper ID. CI is confidence interval.
Spending increased in all studied food categories in the Healthy Helping group relative to the control group. The largest increases were for processed meats and seafood ($2.84) and sugar-sweetened beverages ($2.84). However, because of the sizeable increase in total spending and spending on fruits, vegetables, nuts, and legumes, the relative share of food and beverage spending on all less-healthy product categories decreased, with the largest decline for sugar-sweetened beverages (−2.5 percent). Results from the unweighted models including all Healthy Helping shoppers were similar to the results of the main analyses (appendix exhibit A6).27
In the treatment-on-treated analyses, the effect sizes were slightly larger, but followed the same overall pattern (exhibit 3). The increase in total spending among Healthy Helping shoppers relative to controls was $65.61, whereas the increase in spending on fruits, vegetables, nuts, and legumes was $30.22. The rise in fruit, vegetable, nut, and legume spending represented a 14 percent increase in share of food and beverage spending on fruits, vegetables, nuts, and legumes compared with control shoppers.
Exhibit 3:
Changes in supermarket spending among Healthy Helping users relative to controls, North Carolina, October 2019–December 2020
| Variable | Estimate | 95% CI |
|---|---|---|
| Total spending ($ per month) | 65.61 | 63.57, 67.65 |
| Food and beverage spending | ||
| Dollars spent ($ per month) | 63.18 | 61.31, 65.05 |
| Fruits, vegetables, nuts, and legumes | ||
| Dollars spent ($ per month) | 30.22 | 29.80, 30.64 |
| Relative share of food and beverage spending (%) | 14.39 | 13.95, 14.84 |
| Volume (ounces) | 266.5 | 261.9, 271.1 |
| Fruits, vegetables, nuts, and legumes with no added sugar, salt, or fat | ||
| Dollars spent ($ per month) | 28.44 | 28.03, 28.84 |
| Relative share of food and beverage spending (%) | 14.34 | 13.89, 14.79 |
| Candy, chocolate, and gum | ||
| Dollars spent ($ per month) | 0.65 | 0.59, 0.71 |
| Relative share of food and beverage spending (%) | −0.26 | −0.30, −0.22 |
| Dessert and sweet snacks | ||
| Dollars spent ($ per month) | 3.23 | 3.00, 3.47 |
| Relative share of food and beverage spending (%) | −1.71 | −1.84, −1.58 |
| Processed meats and seafood | ||
| Dollars spent ($ per month) | 3.32 | 3.06, 3.58 |
| Relative share of food and beverage spending (%) | −1.42 | −1.54, −1.31 |
| Salty snacks | ||
| Dollars spent ($ per month) | 1.98 | 1.81, 2.14 |
| Relative share of food and beverage spending (%) | −0.93 | −1.01, −0.84 |
| Sugar-sweetened beverages | ||
| Dollars spent ($ per month) | 3.34 | 3.05, 3.63 |
| Relative share of food and beverage spending (%) | −2.82 | −3.02, −2.63 |
| Sweeteners and toppings | ||
| Dollars spent ($ per month) | 0.38 | 0.34, 0.43 |
| Relative share of food and beverage spending (%) | −0.19 | −0.22, −0.16 |
SOURCE Authors’ analysis of data from a supermarket chain in North Carolina, October 2019–December 2020. NOTES Treatment on treated models include data from 18,970 Healthy Helping users who used Healthy Helping benefits (197,510 shopper-months) and 86,034 control shoppers (804,481 shopper-months). Estimates are from linear mixed models with terms for Healthy Helping participation, time (before or after month of first use [Healthy Helping shoppers] or before or after index month [control shoppers]) and a Healthy Helping-by-time product term. All estimates were statistically significantly different from 0 at the p < 0.001 level. Models were also adjusted for month and year; Special Supplemental Nutrition Program for Women, Infants, and Children use; urbanicity of most frequent store; and number of months of follow-up, with the shopper-month as the unit of analysis. Models include random intercepts for most frequent store and shopper ID.
Exhibit 4 addresses differences in the overall nutrient density of purchases by Healthy Helping participation status from our exploratory analysis. Results of this analysis show changes in grams of key nutrients per 1,000 kilocalories purchased. Shoppers in the Healthy Helping group increased the amount of carbohydrates purchased by 6.9 grams (95% confidence interval [CI]: 6.32, 7.39) and the amount of sugar purchased by 2.7 grams (95% CI: 2.26, 3.23) per 1,000 kilocalories, relative to controls. Conversely, total fat and saturated fat per 1,000 kcal decreased by 2.3 grams (95% CI: −2.54, −2.08) and 1.0 grams (95% CI: −1.11, −0.95), respectively. The amount of fiber per 1,000 kilocalories in Healthy Helping shopper (versus control) purchases rose 2.5 grams (95% CI: 2.37, 2.61).
Exhibit 4.
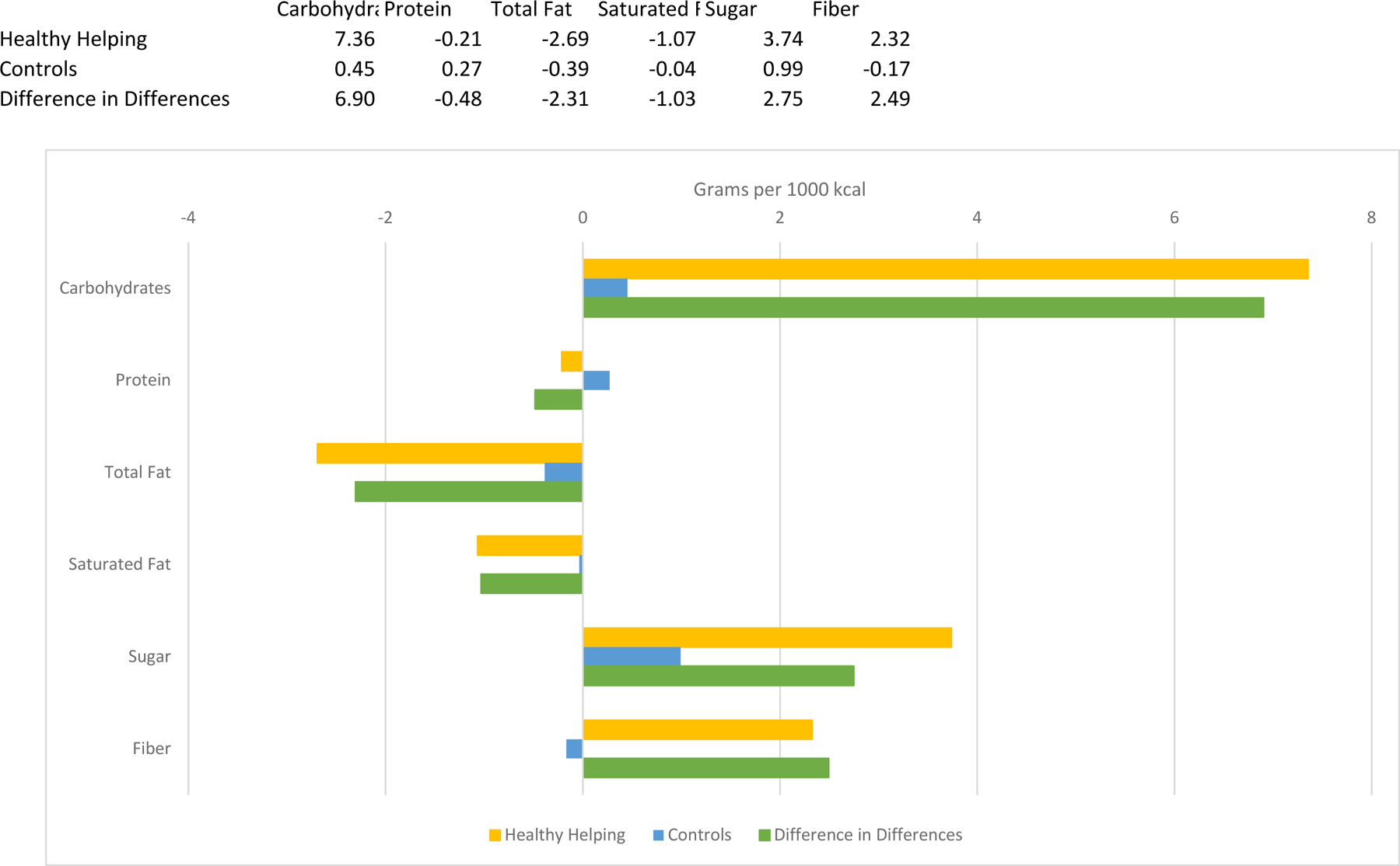
(figure)
Caption: Changes in nutrient density of Healthy Helping purchases compared with control purchases, North Carolina, October 2019–December 2020
Source/Notes: SOURCE Authors’ analysis of data from a supermarket chain in North Carolina, October 2019–December 2020. NOTES Models include data from 19,722 Healthy Helping enrollees (208,601 shopper-months) and 86,034 control shoppers (804,481 shopper-months). The bars show the change in the quantity of each nutrient per 1,000 kilocalories purchased for the Healthy Helping group and the control group and the difference between the changes in the Healthy Helping and control groups (difference-in-differences). Estimates are from linear mixed models with terms for Healthy Helping participation, time (pre– and post–index month), and a Healthy Helping-by-time product term. Models were also adjusted for month and year; Special Supplemental Nutrition Program for Women, Infants, and Children use; urbanicity of most frequent store; percentage of each food or beverage category missing nutrition information; and number of months of follow-up, with the shopper-month as the unit of analysis. Models include random intercepts for most frequent store and shopper ID. The p values for all difference-in-differences estimates are less than 0.001.
Discussion
Relative to SNAP shoppers not enrolled in Healthy Helping, we observed a $27 per month increase in fruit, vegetable, nut, and legume spending among Healthy Helping participants, which effectively doubled the spending on fruits, vegetables, nuts, and legumes in this group. Healthy Helping shoppers’ spending at the supermarket chain increased by $57, suggesting that they shifted more of their shopping to the chain during the intervention. As a consequence, Healthy Helping shoppers’ absolute dollar spending increased across food categories while the composition of spending shifted such that spending on less-healthy food groups declined as a percentage of overall food and beverage spending.
The increase in spending over and above the incentive amount provides evidence that early partnership in such incentive programs by retailers may be financially beneficial to the retailers and local economies. Indeed, prior research funded by the USDA indicates that programs providing funds for food purchases, such as SNAP and nutrition incentive programs, can generate multiplier effects, increasing the local economic impact of the program beyond the amount of food assistance or incentives redeemed.31 Relatively few supermarket chains have participated in fruit and vegetable incentive programs to date, although existing assessments of retailer perceptions have been largely favorable;32 these findings highlight additional positive impacts for retailers.
The exploratory analyses of nutrient density align with our food category findings, given the nutritional composition of most fruits and vegetables. Although we did not examine change in added sugar specifically, we expect that the increase in sugar is driven by naturally occurring sugars in fruit, as the majority of fruits, vegetables, nuts, and legumes purchased contained no added sugar.
Providing further context, a mixed methods study with a subsample of Healthy Helping participants found that participants’ diets during in the program were not significantly different than the typical American diet in 2009–10, despite the high prevalence of food insecurity in the sample.33 This suggests that Healthy Helping may have mitigated potential declines in diet quality associated with food insecurity during the pandemic. Although limited demographic information about Healthy Helping participants was available in the present study, the subsample of Healthy Helping participants (n = 200) in the mixed methods study were predominantly female, with a mean age of forty-nine, and most identified as non-Hispanic Black or African American.33 Respondents had relatively large household sizes (mean: 5.6); most did not have a college degree and had a household income less than $25,000 in 2019.33
This study’s findings align closely with results from an evaluation of a smaller produce prescription program with 667 participants at the same supermarket chain, which found that program enrollment was associated with a $24.34 per month increase in fruit, vegetable, nut, and legume spending.34 The study also noted a decline in sugar-sweetened beverage spending among program shoppers compared with controls,34 whereas we found a slight increase, although the share of total food and beverage spending on sugar-sweetened beverages and other less-healthy food groups declined in both studies.
Prior scoping19 and systematic20 reviews have consistently identified positive impacts of fruit and vegetable incentive programs on fruit and vegetable purchases and consumption, based primarily on studies in farmers’ markets, which generally permit use of incentives for fresh fruits and vegetables only. Although many benefits of fruit and vegetable incentive programs at farmers’ markets have been identified, it is important to consider community preferences, as well as access, availability, seasonality and reach of retail partners35; prior work has found that program participants at supermarkets were more likely to be Black and have lower levels of education compared with those who shopped at farmers’ markets.22
Fewer studies have evaluated fruit and vegetable incentive programs in supermarkets, which may be used for not only fresh fruits and vegetables but also less-perishable frozen and canned fruits and vegetables. Researchers have called for incentives delivered through supermarkets to expand program participation and increase fruit and vegetable purchases.35 Two randomized control trials in a Maine supermarket in which participants received a 50 percent discount on fresh and eligible frozen and canned fruits and vegetables purchased observed increases in fruit and vegetable spending of 15 percent36 and 27 percent.37 Two quasi-experimental studies evaluated the Double Up Food Bucks program in supermarkets in Michigan, which provided a 100 percent matching subsidy on purchases of qualifying fresh produce, and identified small increases in fruit and vegetable purchases.38,39 Differing incentive structures (for example, discount type, instant versus future benefit) may have contributed to the relatively small effect sizes in comparison to the present study.
This study makes several contributions to the literature. We used objective loyalty card transaction data from a large supermarket chain with nearly 500 outlets across 86 of North Carolina’s 100 counties. The transaction data span fifteen months and allowed us to follow shoppers longitudinally. Furthermore, the use of supermarket transaction data allows for the assessment of changes in non–fruit and vegetable food groups and the nutrient density and composition of the entire shopping cart. Our control group comprised SNAP households matched on the basis of prior shopping history to minimize differences between groups and enhance internal validity, as matching based on prior outcomes can reduce bias in difference-in-differences models when multiple observations per unit are available and the outcomes are serially correlated.40
Despite their potential, relatively few evaluations of fruit and vegetable incentive programs in the supermarket setting have been published. This is one of the largest analyses of a fruit and vegetable incentive program to date (regardless of retail setting). In addition to its scale, this program had several unique properties, including provision of the incentive through store loyalty cards; potentially reducing stigma; allowing customers to purchase fresh, frozen, or canned fruits and vegetables; and not requiring a “matching” purchase, which could serve as a model for future programs.
Importantly, although Healthy Helping shoppers increased their spending on fruits, vegetables, nuts, and legumes, most did not redeem the full benefit amount ($40 per month), which is consistent with findings from other social support programs,41,42 underscoring the need to understand barriers to and facilitators of program participation and redemption. For example, participants of a produce prescription program at a supermarket chain in Washington reported challenges using the program during checkout, including stigma and inability to redeem incentives.43 Addressing these barriers and improving participant experience will be critical for future nutrition-related incentive programs to achieve the objective of reducing food insecurity.
Conclusion
Participation in a fruit and vegetable incentive program for SNAP beneficiaries in North Carolina was associated with a $27 per month increase in purchases of fruits, vegetables, nuts, and legumes and a shift in the composition of food purchases at the participating retailer. Findings suggest that fruit and vegetable incentive programs can improve the nutritional profile of grocery purchases, particularly during a period of economic and health uncertainty. Future research to understand factors associated with nonuse and underuse of program funds is needed.
Supplementary Material
Acknowledgment
Preliminary study results were presented in a poster presentation at the Healthy Eating Research Annual Meeting (virtual), April 5, 2022. This work was supported by the North Carolina Department of Health and Human Services from their Coronavirus Aid, Relief, and Economic Security Act of 2020 allocation via a grant to Reinvestment Partners. Additional support came from the National Institutes of Health (NIH) in the form of a grant to the University of North Carolina’s Carolina Population Center (Grant No. P2C HD050924) and a grant to the North Carolina Translational and Clinical Sciences Institute’s National Center for Advancing Translational Sciences and Center for Health Equity Research (Grant No. UL1TR001111). Caitlin Lowery received support from a training grant from the NIH (Global Cardiometabolic Disease Training Grant No. T32 HL129969). Neal Curran and Sam Hoeffler report receiving grants from the Gus Schumacher Nutrition Incentive Program, Rockefeller Foundation, and Blue Cross Blue Shield of North Carolina Foundation outside the submitted work. Molly De Marco has received funding from the NIH, Robert Wood Johnson Foundation, Department of Agriculture, Share our Strength, and Department of Transportation. Shu Wen Ng has received funding from Bloomberg Philanthropies, Arnold Ventures, Robert Wood Johnson Foundation, Duke Endowment, and NIH and has worked as a paid consultant for the World Bank and New York City’s Department of Health and Mental Hygiene. The authors are very grateful to the participating supermarket chain for sharing their transaction data that allowed for this study. They also thank Amy E. Lo for research assistance and Sierra Mullen for data management assistance. The findings and conclusions are those of the authors alone and do not reflect the views of any other entities.
Notes
- 1.Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the United States. Annu Rev Public Health 2019;40:319–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myers CA, Mire EF, Katzmarzyk PT. Trends in adiposity and food insecurity among US adults. JAMA Netw Open 2020;3(8):e2012767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vercammen KA, Moran AJ, McClain AC, Thorndike AN, Fulay AP, Rimm EB. Food security and 10-year cardiovascular disease risk among U.S. adults. Am J Prev Med 2019;56(5):689–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun Y, Liu B, Rong S, Du Y, Xu G, Snetselaar LG, et al. Food insecurity is associated with cardiovascular and all-cause mortality among adults in the United States. J Am Heart Assoc 2020;9(19):e014629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rivera RL, Zhang Y, Wang Q, Maulding MK, Tooze JA, Wright BN, et al. Diet quality and associations with food security among women eligible for Indiana Supplemental Nutrition Assistance Program-Education. J Nutr 2020;150(8):2191–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright BN, Tooze JA, Bailey RL, Liu Y, Rivera RL, McCormack L, et al. Dietary quality and usual intake of underconsumed nutrients and related food groups differ by food security status for rural, Midwestern food pantry clients. J Acad Nutr Diet 2020;120(9):1457–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav 2013;45(2):159–64 [DOI] [PubMed] [Google Scholar]
- 8.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2020 [Internet] Washington (DC): US Department of Agriculture, Economic Research Service; 2021. Sep [cited 2022 Sep 16]. (Contract No. ERR-298). Available from: https://www.ers.usda.gov/webdocs/publications/102076/err-298.pdf [Google Scholar]
- 9.Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients 2020;12(7):2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siddiqi SM, Cantor J, Dastidar MG, Beckman R, Richardson AS, Baird MD, et al. SNAP participants and high levels of food insecurity in the early stages of the COVID-19 pandemic. Public Health Rep 2021;136(4):457–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Byker Shanks C, Houghtaling B, Shanks J, Grocke-Dewey M, Webber E, Andress L, et al. Disparities in dietary practices during the COVID-19 pandemic by food security status. Prev Med Rep 2022;28:101830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller S, Bruine de Bruin W, Livings M, Wilson J, Weber K, Frazzini A, et al. Self-reported dietary changes among Los Angeles County adults during the COVID-19 pandemic. Appetite 2021;166:105586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clay LA, Rogus S. Food access worries, food assistance use, purchasing behavior, and food insecurity among New Yorkers during COVID-19. Front Nutr 2021;8:647365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity (Silver Spring) 2020;28(11):2056–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cummings JR, Wolfson JA, Gearhardt AN. Health-promoting behaviors in the United States during the early stages of the COVID-19 pandemic. Appetite 2022;168:105659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolfson JA, Leung CW, Richardson CR. More frequent cooking at home is associated with higher Healthy Eating Index-2015 score. Public Health Nutr 2020;23(13):2384–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolfson JA, Posluszny H, Kronsteiner-Gicevic S, Willett W, Leung CW. Food insecurity and less frequent cooking dinner at home are associated with lower diet quality in a national sample of low-income adults in the US during the initial months of the COVID-19 pandemic. J Acad Nutr Diet 2022. May 13. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 18.Litton MM, Beavers AW. The relationship between food security status and fruit and vegetable intake during the COVID-19 pandemic. Nutrients 2021;13(3):712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Engel K, Ruder EH. Fruit and vegetable incentive programs for Supplemental Nutrition Assistance Program (SNAP) participants: a scoping review of program structure. Nutrients 2020;12(6):1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhat S, Coyle DH, Trieu K, Neal B, Mozaffarian D, Marklund M, et al. Healthy food prescription programs and their impact on dietary behavior and cardiometabolic risk factors: a systematic review and meta-analysis. Adv Nutr 2021;12(5):1944–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moran AJ, Gu Y, Clynes S, Goheer A, Roberto CA, Palmer A. Associations between governmental policies to improve the nutritional quality of supermarket purchases and individual, retailer, and community health outcomes: an integrative review. Int J Environ Res Public Health 2020;17(20):7493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vargo L, Ciesielski TH, Embaye M, Bird A, Freedman DA. Understanding SNAP recipient characteristics to guide equitable expansion of nutrition incentive programs in diverse food retail settings. Int J Environ Res Public Health 2022;19(9):4977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singleton CR, Kessee N, Chatman C, Spreen C. Racial/ethnic differences in the shopping behaviors and fruit and vegetable consumption of farmers’ market incentive program users in Illinois. Ethn Dis 2020;30(1):109–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGuire S Scientific report of the 2015 dietary guidelines advisory committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv Nutr 2016;7(1):202–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poti JM, Mendez MA, Ng SW, Popkin BM. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr 2015;101(6):1251–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Slining MM, Ng SW, Popkin BM. Food companies’ calorie-reduction pledges to improve U.S. diet. Am J Prev Med 2013;44(2):174–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. To access the appendix, click on the Details tab in the article online.
- 28.Department of Agriculture, Economic Research Service. US household food security survey module: six-item short form [Internet] Washington (DC): USDA, Economic Research Service; 2012. Sep [cited 2022 Sep 16]. Available from: https://www.ers.usda.gov/media/8282/short2012.pdf [Google Scholar]
- 29.Thomas LE, Li F, Pencina MJ. Overlap weighting: a propensity score method that mimics attributes of a randomized clinical trial. JAMA 2020;323(23):2417–8 [DOI] [PubMed] [Google Scholar]
- 30.Li F, Morgan KL, Zaslavsky AM. Balancing covariates via propensity score weighting. J Am Stat Assoc 2017;113(521):390–400 [Google Scholar]
- 31.Gretchen Swanson Center for Nutrition. Gus Schumacher Nutrition Incentive Program Training, Technical Assistance, Evaluation, and Information Center (GusNIP NTAE): impact findings. Year 2: September 1, 2020 to August 31, 2021 [Internet] Omaha (NE): Gretchen Swanson Center for Nutrition; 2022. [cited 2022 Sep 16]. Available from: https://www.nutritionincentivehub.org/media/fjohmr2n/gusnip-ntae-impact-findings-year-2.pdf [Google Scholar]
- 32.Franckle RL, Boulos RJ, Thorndike AN, Moran AJ, Khandpur N, Blue D, et al. Implementation of a 2-for-1 price incentive for fruits and vegetables in a grocery retail setting. Health Promot Pract 2022;15248399221086880; [Epub ahead of print] [DOI] [PubMed]
- 33.Lu I, Sheppard B, Ng SW, Burstein S, Charles E, Williams T, et al. Did a fruit and vegetable incentive program support low-income households in North Carolina during the COVID-19 pandemic? A mixed methods assessment of the Healthy Helping Program and other pandemic-related food assistance. J Hunger Environ Nutr 2022. Aug 7. [Epub ahead of print].
- 34.Berkowitz SA, Curran N, Hoeffler S, Henderson R, Price A, Ng SW. Association of a fruit and vegetable subsidy program with food purchases by individuals with low income in the US. JAMA Netw Open 2021;4(8):e2120377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.John S, Lyerly R, Wilde P, Cohen ED, Lawson E, Nunn A. The case for a national SNAP fruit and vegetable incentive program. Am J Public Health 2021;111(1):27–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polacsek M, Moran A, Thorndike AN, Boulos R, Franckle RL, Greene JC, et al. A supermarket double-dollar incentive program increases purchases of fresh fruits and vegetables among low-income families with children: the Healthy Double Study. J Nutr Educ Behav 2018;50(3):217–228.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moran A, Thorndike A, Franckle R, Boulos R, Doran H, Fulay A, et al. Financial incentives increase purchases of fruit and vegetables among lower-income households with children. Health Aff (Millwood) 2019;38(9):1557–66 [DOI] [PubMed] [Google Scholar]
- 38.Rummo PE, Noriega D, Parret A, Harding M, Hesterman O, Elbel BE. Evaluating a USDA program that gives SNAP participants financial incentives to buy fresh produce in supermarkets. Health Aff (Millwood) 2019;38(11):1816–23 [DOI] [PubMed] [Google Scholar]
- 39.Steele-Adjognon M, Weatherspoon D. Double Up Food Bucks program effects on SNAP recipients’ fruit and vegetable purchases. BMC Public Health 2017;17(1):946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ryan AM, Kontopantelis E, Linden A, Burgess JF Jr. Now trending: coping with non-parallel trends in difference-in-differences analysis. Stat Methods Med Res 2019;28(12):3697–711 [DOI] [PubMed] [Google Scholar]
- 41.Zhang Q, Zhang J, Park K, Tang C, McLaughlin PW, Stacy B. Women, infants, and children cash value benefit redemption choices in the electronic benefit transfer era. Am J Health Promot 2022;36(2):310–3 [DOI] [PubMed] [Google Scholar]
- 42.Singleton CR, Opoku-Agyeman W, Affuso E, Baskin ML, Levitan EB, Sen B, et al. WIC cash value voucher redemption behavior in Jefferson County, Alabama, and its association with fruit and vegetable consumption. Am J Health Promot 2018;32(2):325–33 [DOI] [PubMed] [Google Scholar]
- 43.Riemer S, Walkinshaw LP, Auvinen A, Marcinkevage J, Daniel M, Jones-Smith JC. Qualitative study on participant perceptions of a supermarket fruit and vegetable incentive program. J Acad Nutr Diet 2021;121(8):1497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


