Abstract
Background
: Psychosocial risk factors (PSRFs) have emerged as crucial non-traditional risk factors affecting outcomes in patients with heart failure (HF). There is a paucity of data studying these risk factors in HF nationally. Additionally, whether the COVID-19 pandemic impacted outcomes remains unexplored, given the increased psychosocial risk during these times.
Objectives
: To assess the impact of PSRFs on the outcomes of HF and their comparison across non-COVID and COVID eras.
Methods
: Patients with a diagnosis of HF were selected using the 2019-2020 Nationwide Readmissions Database. Two cohorts were created based on the presence or absence of PSRFs and compared across non-COVID (2019) and COVID (2020) eras. We examined the association using hierarchical multivariable logistic regression models.
Results
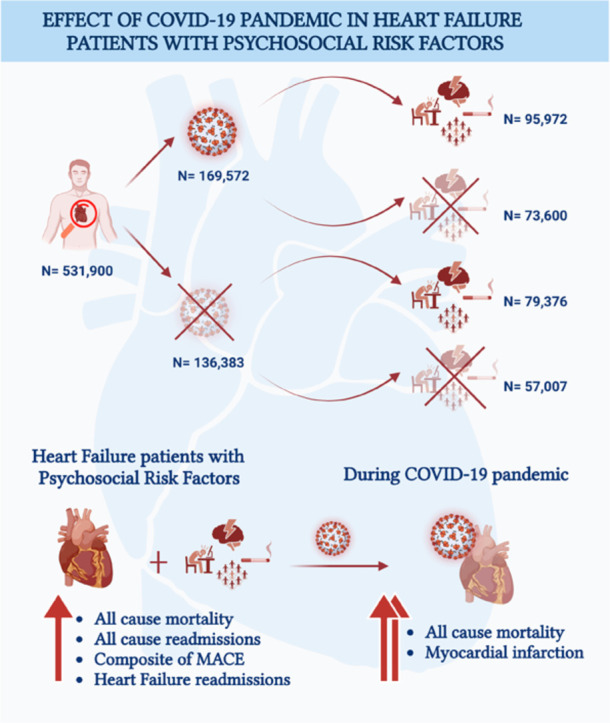
: A total of 305,955 patients were included, of which 175,348 (57%) had PSRFs. Patients with PSRFs were younger (P<0.001), less likely to be female (P<0.001), and had a higher prevalence of cardiovascular risk factors. All-cause readmissions were higher in patients with PSRFs in both eras. All-cause mortality [HR 1.15 (1.04-1.27), P=0.005] and a composite of MACE [HR 1.11 (1.06-1.16), P<0.001] were higher in patients in the non-COVID era. Compared to 2019, patients with PSRFs and HF in 2020 had significantly higher all-cause mortality [1.13 (1.03-1.24), P=0.009]; however, the composite of MACE was comparable [1.04 (1.00-1.09), P=0.03].
Conclusion
: The presence of PSRFs in patients with HF is associated with a significant increase in all-cause readmissions and all-cause mortality in COVID and non-COVID eras. The worse outcomes evident in the COVID era highlights the importance of multidisciplinary care in this vulnerable population.
Short Abstract
Psychosocial risk factors (PSRFs) are crucial non-traditional risk factors affecting outcomes in heart failure (HF) patients. We sought to investigate the impact of the COVID-19 pandemic on PSRFs and HF outcomes. Utilizing 2019-2020 Nationwide Readmissions Database, 305,955 patients with a diagnosis of HF were selected of which 175,348 (57%) had PSRFs. We further compared these subgroups across non-COVID (2019) and COVID (2020) eras. Multivariable logistic regression models were constructed for analysis. In patients with PSRFs, we noted higher 30-day all-cause readmissions, 30-day heart failure readmissions, 30-day all-cause mortality and composite of MACE. Readmissions were higher in both eras, while mortality was significantly higher during the COVID-19 era. This highlights the importance of multidisciplinary care in this vulnerable population.
Keywords: Psychosocial risk factors, Heart failure, COVID-19
Graphical abstract
Abbreviations
- PSRFs:
Psychosocial risk factors
- HF:
Heart failure
- COVID-19:
Coronavirus disease 2019
- MACE:
Major adverse cardiovascular event
Introduction
Heart failure (HF) is one of the common causes of hospital admissions and a significant contributor to morbidity and mortality. About 10% of the US population over 65 lives with HF1. Despite multiple effective treatment modalities and advancements, patients with heart failure continue to have worsening symptoms and frequent readmissions to the hospital. In addition to addressing all the medical risk factors, psychosocial determinants of health must be addressed to improve outcomes. Studies have shown that one of the important yet often missed risk factors is the impact of psychosocial health2, 3, 4, 5. Psychiatric conditions, including anxiety and depression, are more prevalent and can be debilitating comorbidities in patients with HF2 , 5. An estimated 20-30% of HF patients have co-existing depression6 , 7. These conditions are associated with adverse outcomes in HF, such as decreased adherence to medications and diet, increased hospitalizations or emergency department visits, and death6. In addition, complying with regular exercise, weight loss, and scheduled follow-up visits can be challenging. Other factors, including low socioeconomic status, marital status, and urban vs. rural location, are also associated with disparities in outcomes8. Of the various affected outcomes, quality of life is increasingly recognized as necessary3.
The SARS-CoV-2-associated Coronavirus-19 (COVID-19) global pandemic has exposed and exacerbated disparities in outcomes brought by PSRFs. Stringent lockdown, quarantine and isolation, and the fear of the pandemic worsened mental health among many patients. The first year of the COVID-19 pandemic (2020) increased the global prevalence of anxiety and depression by 25% per a WHO report9. This significant increase in the prevalence of mental health problems has also disrupted the availability of prompt care. Many hospitals cancelled elective procedures and a few outpatient services, including cardiac rehabilitation, as all the staff was redirected to the emergency and intensive care services, treating the severely ill. As a result, patients could not come for regular office visits/ follow-up appointments, affecting their baseline cardiovascular status10.
During the COVID-19 pandemic, loneliness and social isolation worsened cardiovascular outcomes11. However, there is a data paucity on its impact during the pandemic compared to pre-pandemic time on medical care.
Hence, we sought to study the impact of PSRFs in patients with known HF and compare outcomes in the pre-COVID-19 and COVID-19 eras.
Methods
Data Source
For this study, we analyzed the Nationwide Readmissions Database (NRD) from 2019-2020. It is a publicly available, all-payer, de-identified administrative dataset developed by the Agency for Healthcare Research and Quality (AHRQ) for the Healthcare Cost and Utilization Project (HCUP). It is constructed by combining discharges from 30 state inpatient databases, representing ∼60% of all United States hospitalizations. The patient can be traced across the hospitals within a state across one calendar year using linkage information provided in the NRD. Since the NRD contains a de-identified publicly available dataset for retrospective analysis, the study was deemed exempt by our Institutional Review Board and also precluded the need for informed consent.
Study Population
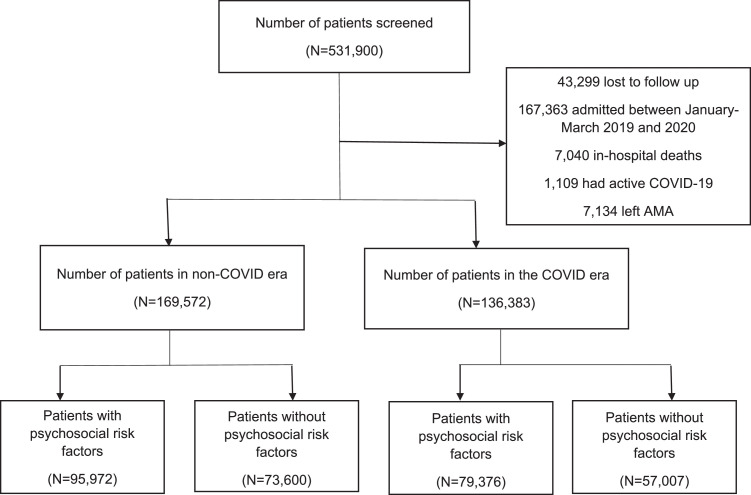
Hospitalizations for HF in adults aged ≥ 18 years in 2019 and 2020 were identified using the International Classification of Diseases, Tenth Revision, Procedure Coding System (ICD-10-CM) [Table S1]. ICD-10-CM (clinical modification) were used to identify comorbidities and outcomes [Table S1], and, HCUP Clinical Classification Software Refined (CCSR) was used to identify causes of readmissions [CIR001-CIR039 for cardiac causes; rest were designated non-cardiac, and CIR019 for heart failure]. Weighted samples were used for all analyses. The index admission was defined as the first hospitalization in the calendar year for HF. Patients were excluded if index HF hospitalization was in December of respective years owing to lack of 30-day follow-up data. We excluded patients with index HF admission in January-March of 2019 and 2020 (n=167,363) as we aimed to study the impact of the COVID-19 pandemic, which started in March 2020. Additional exclusion criteria included concomitant COVID-19 positive status in index HF admission (n= 1,109) and patients that left against medical advice (n=7,134) or were lost to follow up (n=43,299), or died (n=7,040) during index hospitalization due to lack of 30-day follow-up data. The final cohort included 305,955 index HF admissions across both years (Figure 1 ).
Figure 1.
. sssssssss
Psychosocial risk factors were classified into five domains based on previous work12: psychiatric disease, limited cognitive understanding, substance use disorder, uninsured status, and low socioeconomic status. The presence of ≥1 factor was used to define the cohort of patients with PSRFs.
Patient and Hospital Characteristics
We extracted baseline patient demographics (age, sex, median household income, primary expected payer), psychosocial risk factors, type of HF, comorbidities, hospital characteristics (bed size, hospital location, teaching status), and discharge disposition data [Table 1 ]. ICD-10-CM and HCUP CCSR codes were used to define these variables.
Table 1.
Baseline characteristics of patients with HF in non-COVID (2019) and COVID (2020) eras
| Characteristics | Patients with HF in 2019 (non-COVID era) | Patients with HF in 2020 (COVID era) | ||||
|---|---|---|---|---|---|---|
| With PSRFs N=79,376 | Without PSRFs N=57,007 | P value | With PSRFs N=95,972 | Without PSRFs N=73,600 | P value | |
| (58.2%) | (41.8%) | (56.6%) | (43.4%) | |||
| Age (mean, SD) | 67.1 (14.9) | 73.5 (3.3) | <0.001 | 68.5 (15.0) | 74.6 (13.2) | <0.001 |
| Female | 38,685 (48.7) | 28,607 (50.2) | <0.001 | 48,240 (50.3) | 38,024 (51.7) | <0.001 |
| Median household income, percentile | ||||||
| 0-25th | 41,733 (52.6) | - | <0.001 | 51,970 (54.2) | - | <0.001 |
| 26th-50th | 15,891 (20.0) | 22,534 (39.5) | 17,395 (18.1) | 27,138 (36.9) | ||
| 51st-75th | 12,308 (15.5) | 18,424 (32.3) | 15,064 (15.7) | 25,142 (34.2) | ||
| 76th-100th | 8,756 (11.0) | 15,024 (26.4) | 10,691 (11.1) | 19,975 (27.1) | ||
| Primary Payer | ||||||
| Medicare | 48,766 (61.4) | 43,225 (75.8) | <0.001 | 62,291 (64.9) | 57,401 (78.0) | <0.001 |
| Medicaid | 13,480 (17.0) | 4,228 (7.4) | 14,230 (14.8) | 4,893 (6.6) | ||
| Private insurance | 9,987 (12.6) | 8,113 (14.2) | 11,405 (11.9) | 9,794 (13.3) | ||
| Self-pay | 4,612 (5.8) | - | 5,421 (5.6) | - | ||
| No charge | 257 (0.3) | 94 (0.1) | 403 (0.4) | 133 (0.2) | ||
| Other | 2,130 (2.7) | 1,271 (2.2) | 2,119 (2.2) | 1,301 (1.8) | ||
| Psychosocial risk factors | ||||||
| Limited cognition | 10,053 (12.7) | - | <0.001 | 13,683 (14.3) | - | <0.001 |
| Substance abuse | 32,653 (41.1) | - | <0.001 | 35,541 (37.0) | - | <0.001 |
| Psychiatric disorders | 20,923 (26.4) | - | <0.001 | 23,939 (24.9) | - | <0.001 |
| Comorbidities | ||||||
| Smoking | 25,822 (32.5) | 341 (0.6) | <0.001 | 28,594 (29.8) | 566 (0.8) | <0.001 |
| Dyslipidemia | 39,249 (49.4) | 31,715 (55.6) | <0.001 | 46,830 (48.8) | 40,000 (54.3) | <0.001 |
| Hypertension | 68,197 (85.9) | 48,968 (85.9) | 0.92 | 82,805 (86.3) | 63,068 (85.7) | 0.001 |
| Diabetes | 30,468 (38.4) | 22,745 (39.9) | <0.001 | 36,658 (38.2) | 28,642 (38.9) | 0.003 |
| Obesity | 24,746 (31.2) | 16,827 (29.5) | <0.001 | 26,634 (27.8) | 19,195 (26.1) | <0.001 |
| Known CAD | 31,928 (40.2) | 24,696 (43.3) | <0.001 | 38,949 (40.6) | 32,191 (43.7) | <0.001 |
| Prior MI | 9,844 (12.4) | 7,074 (12.4) | 0.97 | 12,260 (12.8) | 9,254 (12.6) | 0.22 |
| Prior PCI | 8,659 (10.9) | 6,920 (12.1) | <0.001 | 10,867 (11.3) | 9,279 (12.6) | <0.001 |
| Prior CABG | 6,941 (8.7) | 6,486 (11.4) | <0.001 | 9,475 (9.9) | 9,284 (12.6) | <0.001 |
| Prior TIA/ stroke | 7,270 (9.2) | 5,322 (9.3) | 0.27 | 9,103 (9.5) | 7,430 (10.1) | <0.001 |
| Atrial fibrillation | 20,703 (26.1) | 18,651 (32.7) | <0.001 | 34,681 (36.1) | 35,036 (47.6) | <0.001 |
| Prior PPM | 4,816 (6.1) | 5,269 (9.2) | <0.001 | 6,809 (7.1) | 7,521 (10.2) | <0.001 |
| Prior ICD | 4,983 (6.3) | 3,897 (6.8) | <0.001 | 6,614 (6.9) | 5,549 (7.5) | <0.001 |
| Peripheral vascular disease | 11,300 (14.2) | 9,180 (16.1) | <0.001 | 14,239 (14.8) | 12,002 (16.3) | <0.001 |
| Anemia | 6,810 (8.6) | 4,911 (8.6) | 0.82 | 7,315 (7.6) | 5,654 (7.7) | 0.65 |
| Chronic kidney disease | 4,654 (5.9) | 4,663 (8.2) | <0.001 | 5,218 (5.4) | 5,429 (7.4) | <0.001 |
| Chronic lung disease | 34,704 (43.7) | 19,289 (33.8) | <0.001 | 42,463 (44.2) | 25,857 (35.1) | <0.001 |
| Chronic liver disease | 5,502 (6.9) | 2,739 (4.8) | <0.001 | 5,580 (5.8) | 2,835 (3.9) | <0.001 |
| Coagulopathy | 4,774 (6.0) | 3,922 (6.9) | <0.001 | 5,282 (5.5) | 4,569 (6.2) | <0.001 |
| Hypothyroidism | 12,076 (15.2) | 10,909 (19.1) | <0.001 | 15,201 (15.8) | 14,346 (19.5) | <0.001 |
| Pulmonary circulation disorders | 17,471 (22.0) | 14,005 (24.6) | <0.001 | 20,235 (21.1) | 17,418 (23.7) | <0.001 |
| Cancer | 3,057 (3.9) | 3,343 (5.9) | <0.001 | 3,680 (3.8) | 4,171 (5.7) | <0.001 |
| No. of Elixhauser comorbidities, median (IQR) | 5 (3) | 5 (3) | <0.001 | 5 (3) | 5 (2) | <0.001 |
| Hospital characteristics | ||||||
| Bed size | ||||||
| Small | 15,942 (20.1) | 13,163 (23.1) | <0.001 | 18,547 (19.3) | 16,962 (23.0) | <0.001 |
| Medium | 22,205 (28.0) | 15,826 (27.8) | 26,938 (28.1) | 20,943 (28.5) | ||
| Large | 41,229 (51.9) | 28,018 (49.1) | 50,487 (52.6) | 35,695 (48.5) | ||
| Location | ||||||
| Rural | 2,780 (3.5) | 1,296 (2.3) | <0.001 | 3,618 (3.8) | 1,445 (2.0) | <0.001 |
| Urban | 76,596 (96.5) | 55,711 (97.7) | 92,354 (96.2) | 72,155 (98.0) | ||
| Teaching Status | ||||||
| Non-teaching | 26,388 (33.2) | 16,776 (29.4) | <0.001 | 32,620 (34.0) | 21,847 (29.7) | <0.001 |
| Teaching | 52,988 (66.8) | 40,231 (70.6) | 63,352 (66.0) | 51,753 (70.3) | ||
| Heart failure type | ||||||
| HFrEF | 6,404 (8.1) | 4,073 (7.1) | <0.001 | 7,309 (7.6) | 5,294 (7.2) | 0.001 |
| HFpEF | 3,971 (5.0) | 3,725 (6.5) | <0.001 | 4,895 (5.1) | 4,812 (6.5) | <0.001 |
| Combined | 2,219 (2.8) | 1,566 (2.7) | 0.59 | 2,546 (2.7) | 2,032 (2.8) | 0.17 |
| Unspecified | 66,782 (84.1) | 47,643 (83.6) | 0.006 | 81,222 (84.6) | 61,462 (83.5) | <0.001 |
| Disposition | ||||||
| Routine | 47,507 (59.9) | 30,918 (54.2) | <0.001 | 56,876 (59.3) | 40,335 (54.8) | <0.001 |
| Short-term hospital | 849 (1.1) | 665 (1.2) | 1,088 (1.1) | 928 (1.3) | ||
| SNF | 9,788 (12.3) | 6,994 (12.3) | 15,885 (16.6) | 12,130 (16.5) | ||
| Home health care | 21,204 (26.7) | 18,409 (32.3) | 22,081 (23.0) | 20,183 (27.4) | ||
Data is represented as N (%)
AKI: acute kidney injury, AMI: acute myocardial infarction, CABG: coronary artery bypass graft, CAD: coronary artery disease, HFrEF: heart failure with reduced ejection fraction, HFpEF: heart failure with preserved ejection fraction, ICD: implantable cardioverter- defibrillator, IQR: inter-quartile range, MI: myocardial infarction, MV: mitral valve, PCI: percutaneous coronary intervention, PPM: permanent pacemaker, SD: standard deviation; SNF: skilled nursing facility, TIA: transient ischemic attack.
Outcomes
Primary outcomes of interest were 30-day all-cause readmissions, 30-day mortality, and 30-day major adverse cardiovascular event (defined as a composite of myocardial infarction, heart failure readmission, stroke and all-cause death). Only the first readmission was counted for patients with multiple readmissions within 30 days. Transfer to another hospital or inpatient rehabilitation center was not counted as readmission. Secondary outcomes included causes of 30-day readmissions (cardiac, non-cardiac, heart failure) using HCUP CCSR codes and individual outcomes of the 30-day MACE composite.
Statistical Analysis
Patient demographics, comorbidities, hospital characteristics, and discharge disposition were compared between patients with vs. without PSRF using the Pearson χ² test for categorical variables and the Kruskal-Wallis test for continuous variables and were further compared separately for 2019 and 2020. Weighted data were used for national-level estimates.
Multivariable hierarchical logistic regression models were constructed to evaluate differences in primary and secondary outcomes. Variables listed in Table 1 were used as covariates. Categorical variables were presented as frequency (percentage) and continuous variables as mean (SD) or median (IQR) as appropriate. Odds ratios and 95% confidence intervals (CIs) were used to report the results of regression analyses. Statistical analyses were performed using Stata, version 17 (Statistical Software: Release 17. College Station, TX: StataCorp LLC). Two-tailed p-values of <0.05 were considered significant for the analyses.
Results
Selection of cases
Using NRD, 531,900 index HF admissions were screened between 2019 and 2020. Of these, 305,955 patients met the inclusion criteria (Figure 1). 136,383 patients (45%) were admitted in 2019 (non-COVID era), while 169,572 (55%) were admitted in 2020 (COVID era). Psychosocial risk factors (PSRFs) were present in 56% of patients with HF in non-COVID era and in 58% of patients with HF in COVID era.
Baseline characteristics
There were significant differences in baseline characteristics in patients with PSRFs compared to those without, both in COVID and non-COVID eras [Table 1]. Patients with PSRFs were younger (P<0.001), less likely to be female (P<0.001), had a higher prevalence of cardiovascular risk factors, including pre-existing coronary artery disease (CAD), diabetes mellitus, dyslipidemia and smoking (P<0.001) [Table S2]. Additionally, baseline characteristics of patients with PSRFs in 2019 and 2020 are compared in Table S3.
Outcomes
As a group, all-cause readmissions were higher in patients with PSRFs when compared to those without [1.09 (1.06 - 1.11), P<0.001] (Table 2 ). This included both non-cardiac and cardiac (predominantly HF) readmissions. The adjusted outcomes for all-cause mortality [1.12 (1.04 - 1.20), P=0.003] and a composite of MACE [1.08 (1.04 - 1.12), P<0.001] were also higher in patients with PSRFs versus those without.
Table 2.
Comparison of outcomes in HF patients with and without PSRFs
| 30-day outcomes | Unadjusted outcomes | Adjusted outcomes | |||
|---|---|---|---|---|---|
| With PSRFs | Without PSRFs | P value | With PSRFs | P value | |
| N=175,348 | N=130,607 | N=175,348 | |||
| All-cause readmissions | 29,789 (16.9%) | 20,886 (15.9%) | <0.001 | 1.09 (1.06-1.11) | <0.001 |
| All-cause mortality | 2,160 (1.2%) | 1,695 (1.3%) | 0.106 | 1.12 (1.04-1.20) | 0.003 |
| MACE | 14,514 (8.2%) | 9,883 (7.5%) | <0.001 | 1.08 (1.04-1.12) | <0.001 |
| Myocardial infarction | 2,647 (1.5%) | 1,718 (1.3%) | <0.001 | 1.08 (1.00-1.16) | 0.036 |
| Stroke | 920 (0.5%) | 650 (0.5%) | 0.30 | 1.09 (0.97-1.23) | 0.155 |
| Cardiac readmissions | 15,862 (9.0%) | 11,195 (8.5%) | <0.001 | 1.03 (0.99-1.06) | 0.054 |
| Non-cardiac readmissions | 13,927 (7.9%) | 9,691 (7.4%) | <0.001 | 1.13 (1.10-1.17) | <0.001 |
| Heart failure readmissions | 10,589 (6.0%) | 7,023 (5.3%) | <0.001 | 1.08 (1.04-1.12) | <0.001 |
Data is represented as N (%), excepted adjusted outcomes. Adjusted outcomes are represented as odds ratio with confidence intervals.
Abbreviations: MACE, major adverse cardiovascular event; PSRF, psychosocial risk factor.
MACE includes composite of all-cause mortality, heart failure-readmissions, stroke and myocardial infarction.
Comparing patients with and without PSRFs in both COVID and non-COVID eras, all-cause readmissions were significantly higher in HF patients with PSRFs compared to those without (P<0.001) across both eras (Table 3 ). This was primarily driven by non-cardiac and HF readmissions (P<0.001). In addition, all-cause mortality was higher in patients with PSRFs when compared to those without, only in the non-COVID era [1.15 (1.04 - 1.27), P=0.005]. Similar results were seen with the composite of MACE and MI (P<0.01). These effects were, however, comparable in the COVID era (Table 3).
Table 3.
Comparison of outcomes in HF patients with and without PSRFs in non-COVID (2019) and COVID (2020) eras
| 30-day outcomes | Patients with HF in non-COVID era | ||||
|---|---|---|---|---|---|
| Unadjusted outcomes | Adjusted outcomes | ||||
| With PSRFs | Without PSRFs | P value | With PSRFs | P value | |
| N=95,972 | N=73,600 | N=95,972 | |||
| All-cause readmissions | 16,398 (17.1%) | 11,768 (15.9%) | <0.001 | 1.09 (1.06-1.13) | <0.001 |
| All-cause mortality | 1,126 (1.1%) | 908 (1.2%) | 0.257 | 1.15 (1.04-1.27) | 0.005 |
| MACE | 7,848 (8.1%) | 5,450 (7.4%) | <0.001 | 1.11 (1.06-1.16) | <0.001 |
| Myocardial infarction | 1,329 (1.3%) | 871 (1.1%) | <0.001 | 1.14 (1.03-1.27) | 0.012 |
| Stroke | 500 (0.5%) | 353 (0.4%) | 0.233 | 1.10 (0.93-1.29) | 0.26 |
| Cardiac readmissions | 8,739 (9.1%) | 6,262 (8.5%) | <0.001 | 1.05 (1.01-1.09) | 0.017 |
| Non-cardiac readmissions | 7,659 (7.9%) | 5,506 (7.4%) | <0.001 | 1.12 (1.08-1.17) | <0.001 |
| Heart failure readmissions | 5,793 (6.0%) | 3,926 (5.3%) | <0.001 | 1.10 (1.05-1.16) | <0.001 |
| Patients with HF in COVID era | |||||
| With PSRFs | Without PSRFs | P value | With PSRFs | P value | |
| N=79,376 | N=57,007 | N=79,376 | |||
| All-cause readmissions | 13,391 (16.8%) | 9,118 (15.9%) | <0.001 | 1.08 (1.04-1.12) | <0.001 |
| All-cause mortality | 1,034 (1.3%) | 787 (1.3%) | 0.22 | 1.08 (0.97-1.20) | 0.16 |
| MACE | 6,666 (8.3%) | 4,433 (7.7%) | <0.001 | 1.04 (0.99-1.10) | 0.063 |
| MI | 1,318 (1.6%) | 847 (1.4%) | 0.011 | 1.02 (0.92-1.14) | 0.69 |
| Stroke | 420 (0.5%) | 297 (0.5%) | 0.84 | 1.08 (0.91-1.29) | 0.38 |
| Cardiac readmissions | 7,123 (8.9%) | 4,933 (8.6%) | 0.04 | 1.01 (0.96-1.05) | 0.80 |
| Non-cardiac readmissions | 6,268 (7.8%) | 4,185 (7.3%) | <0.001 | 1.15 (1.10-1.20) | <0.001 |
| Heart failure readmissions | 4,796 (6.0%) | 3,097 (5.4%) | <0.001 | 1.05 (0.99-1.11) | 0.10 |
Data is represented as N (%), excepted adjusted outcomes. Adjusted outcomes are represented as odds ratio with confidence intervals.
Abbreviations: COVID, coronavirus disease 2019; HF, heart failure; MACE, major adverse cardiovascular event; PSRF, psychosocial risk factor.
MACE includes composite of all-cause mortality, heart failure-readmissions, stroke and myocardial infarction.
In contrast, among patients with PSRFs, there was no difference in all-cause readmissions [1.00 (0.97 - 1.03), P=0.78] and composite of MACE [1.04 (1.00-1.09), P=0.03] between COVID and non-COVID eras. However, there was a significant increase in all-cause mortality [1.13 (1.03-1.24), P=0.009] of HF patients hospitalized in the COVID era compared to the non-COVID era. Similarly, MI [1.19 (1.08-1.30), P<0.001] was higher in the COVID era versus the non-COVID era (Table 4 ).
Table 4.
Comparison of outcomes in HF patients with ≥1 psychosocial risk factor in non-COVID (2019) versus COVID (2020) eras
| Non-COVID era (2019) | COVID era (2020) | P value | Adjusted outcomes | P value | |
|---|---|---|---|---|---|
| N=95,972 (54.7%) | N=79,376 (45.3%) | ||||
| All-cause readmissions | 16,398 (17.1%) | 13,391 (16.8%) | 0.231 | 1.00 (0.97-1.03) | 0.78 |
| All-cause mortality | 1,126 (1.1%) | 1,034 (1.3%) | 0.014 | 1.13 (1.03-1.24) | 0.009 |
| MACE | 7,848 (8.1%) | 6,666 (8.3%) | 0.095 | 1.04 (1.00-1.09) | 0.03 |
| Myocardial infarction | 1,329 (1.3%) | 1,318 (1.6%) | <0.001 | 1.19 (1.08-1.30) | <0.001 |
| Stroke | 500 (0.5%) | 420 (0.5%) | 0.81 | 1.04 (0.90-1.19) | 0.59 |
| Cardiac readmissions | 8,739 (9.1%) | 7,123 (8.9%) | 0.34 | 1.00 (0.97-1.04) | 0.79 |
| Non-cardiac readmissions | 7,659 (7.9%) | 6,268 (7.8%) | 0.52 | 1.00 (0.96-1.04) | 0.91 |
| Heart failure readmissions | 5,793 (6.0%) | 4,796 (6.0%) | 0.96 | 1.02 (0.97-1.07) | 0.42 |
Data is represented as N (%), excepted adjusted outcomes. Adjusted outcomes are represented as odds ratio with confidence intervals.
Abbreviations: COVID, coronavirus disease 2019; HF, heart failure; MACE, major adverse cardiovascular event; PSRF, psychosocial risk factor.
MACE includes composite of all-cause mortality, heart failure-readmissions, stroke and myocardial infarction.
Discussion
The most important finding in our study is that among patients with PSRFs, the risk of MI and all-cause mortality increased during the COVID era. To our knowledge, ours is the first study showing the 30-day outcomes of HF admissions in patients with psychosocial risk factors in the COVID era. One possible causal mechanism is that the COVID-19 pandemic has highlighted pre-existing inequalities, particularly in terms of healthcare access and economic opportunities. The pandemic has disrupted the continuity of care for many services, disproportionately affecting vulnerable communities such as low-income individuals who may already experience numerous PSRFs13.
PSRFs are now increasingly recognized as crucial indicators for predicting outcomes in cardiovascular diseases. Studies have shown that the increasing prevalence of PSRFs is linked to a higher mortality risk and worse prognosis14, 15, 16, 17. In addition, patients with heart failure often experience a range of psychological risk factors, including depression and anxiety, leading to poor quality of life. Our study further supports this by demonstrating that PSRFs are prevalent in HF patients and predispose them to an increased risk of adverse outcomes. In our study, about 57% of HF patients had at least one PSRF, regardless of the impact of the COVID-19 pandemic. These risks may be related to the physical symptoms and limitations imposed by heart failure, as well as the emotional and social implications of the condition. Additionally, patients with heart failure may experience social isolation, financial stress, and caregiver burden, all of which can contribute to poor mental health. The added uncertainty, the fear of recurrent hospitalizations, and limited treatment options for the advanced disease may also lead to psychological distress18, 19, 20, 21, 22, 23.
Prior studies have reported that a significant proportion (15%) of hospitalized heart failure patients are diagnosed with substance use or tobacco use disorder24. We found an even higher rate of substance abuse and tobacco use in our study. Substance abuse disorder accounted for 37% in the non-COVID era and 41% in the COVID era among these patients, while smoking rates were 29.8% and 32.5% in the non-COVID and COVID eras, respectively. This is an important finding as it has been shown that substance abuse is a significant cause of morbidity in HF patients and is associated with increased emergency department visits and heart failure hospitalization25.
We report a 13% increase in mortality risk and a 19% increase in MI risk in patients with PSRFs during the COVID-19 pandemic compared to the previous year (Table 4). Although we cannot clearly explain why the mortality risk of patients with PSRFs increased during the COVID era, one of the possible reasons could be that the standard of care for HF treatment for hospitalized patients was not maintained enough in the beginning phase of the pandemic. Additionally, the conversion of cardiology wards and heart failure units to COVID-19 wards and the reallocation of healthcare professionals to care for COVID-19 patients affected the care of HF patients12 , 28. However, Shoaib et al. showed a significant rise in mortality from HF within 30 days of discharge during the COVID-19 pandemic despite the same practice of guideline-recommended medical therapy and interventions. They suggested that the mortality increase was likely due to post-discharge care, which caused suboptimal care after discharge25. Furthermore, the closure of outpatient clinics during the pandemic may have also contributed to inadequate post-discharge care and increased mortality26 , 27.
PSRFs increased the risk of 30-day all-cause readmissions by 9% in the non-COVID era and 8% in the COVID era (Table 3). Our study findings are more comprehensive regarding psychosocial risk factors as we analyzed the effect of limited cognition, substance abuse, and psychiatric disorders. Several randomized trials have reported follow-up interventions after discharge, such as medication counselling, medication reconciliation, formal education, detailed discharge planning, and phone follow-up to reduce readmissions28, 29, 30, 31; however, interventions focusing on PSRFs have been understudied. By demonstrating the effect of substance abuse, psychiatric disorders, and limited cognition on heart failure readmissions, we highlight the importance of different determinants of psychosocial risk factors on HF readmissions, which should be considered as prognostic factors, offering significant implications as a future strategy to reduce hospital readmissions and costs.
LIMITATIONS
Our study does have a few limitations. The NRD database relies solely on ICD coding and does not include parameters of hospital admission, including clinical, laboratory and echocardiography data. Similarly, it does not capture the involvement of multidisciplinary teams, if any, especially palliative care which can be of pivotal importance in advanced heart failure and affect the outcomes. We also could not divide the patients on the subtype of HF based on ICD coding, and, as such, could not associate outcomes based on subtypes of HF. Also, we do not have data on the severity of PSRF illness. Out-of-hospital mortality or emergency care visits are not captured. Finally, information on race/ethnicity is not available in NRD, which would have been beneficial, considering the disparities in PSRF across various ethnic groups.
Conclusion
The findings of our retrospective study using the pre-COVID and COVID Nationwide readmissions data in 2019 and 2020 underscores the effect of the COVID-19 pandemic on the association between PSRFs and HF outcomes. Although not considered a traditional risk factor for heart failure, PSRFs were associated with increased all-cause readmissions in both COVID and non-COVID eras, highlighting its magnitude. The 30-day all-cause mortality and MI in HF with PSRFs patients were higher in the COVID era. It is prudent to address the increased incidence and prevalence of PSRFs, such as substance use, psychiatric disease, and low socioeconomic status, along with the worsened quality of life during this pandemic which, when paired with substandard HF care in-hospital as well as post-discharge likely led to worse outcomes in the COVID era. Further studies are necessary, focusing on specific PSRF and their effect on reducing hospital readmissions in HF patients.
CLINICAL PERSPECTIVES
Competency in medical knowledge: In patients with heart failure, psychosocial risk factors lead to frequent readmissions and increased mortality. The additive effect of mental stress through the COVID-19 pandemic further worsened this association.
Competency in Patient Care: Patients with psychosocial risk factors should be provided a holistic approach with medication optimization, counselling, and measures to address cardiovascular risk factors and psychological and social health. A multidisciplinary team involving cardiology, psychiatry, and social services will be helpful.
Translational Outlook: Although psychosocial risk factors are a known risk factor for worse cardiovascular outcomes, future research is needed to see if regular behavioral interventions can help decrease the magnitude of these worse outcomes.
Declarations
Funding: No funds, grants, or other support was received.
Interests: The authors have no relevant financial or non-financial interests to disclose.
Acknowledgements
None.
Footnotes
The study was done utilizing the Nationwide Readmissions Database.
Funding: None.
Disclosures: None of the authors have any relevant disclosures.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.cpcardiol.2023.101795.
Appendix. Supplementary materials
References
- 1.Rod NH, Andersen I, Prescott E. Psychosocial risk factors and heart failure hospitalization: a prospective cohort study. American journal of epidemiology. 2011;174(6):672–680. doi: 10.1093/aje/kwr144. Sep 15. [DOI] [PubMed] [Google Scholar]
- 2.MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Archives of internal medicine. 2002;162(5):509–516. doi: 10.1001/archinte.162.5.509. Mar 11. [DOI] [PubMed] [Google Scholar]
- 3.Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY. Health-related quality of life in elderly patients with heart failure. Scandinavian Cardiovascular Journal. 1999;33(5):278–285. doi: 10.1080/14017439950141524. Jan 1. [DOI] [PubMed] [Google Scholar]
- 4.McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005;365(9474):1877–1889. doi: 10.1016/S0140-6736(05)66621-4. May 28-Jun 3. [DOI] [PubMed] [Google Scholar]
- 5.Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harvard review of psychiatry. 2018;26(4):175. doi: 10.1097/HRP.0000000000000162. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Journal of the American college of Cardiology. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. Oct 17. [DOI] [PubMed] [Google Scholar]
- 7.Sokoreli I, De Vries JJ, Pauws SC, Steyerberg EW. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart failure reviews. 2016;21:49–63. doi: 10.1007/s10741-015-9517-4. Jan. [DOI] [PubMed] [Google Scholar]
- 8.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. American journal of public health. 2004;94(10):1682–1686. doi: 10.2105/ajph.94.10.1682. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO - Covid 19 triggers 25% increase in prevalence of anxiety and depression worldwide. Available at: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide. Accessed April 6, 2023
- 10.DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for heart failure care during the COVID-19 pandemic. Heart failure. 2020;8(8):681–691. doi: 10.1016/j.jchf.2020.05.006. Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma T, Padala PR, Mehta JL. Loneliness and social isolation: determinants of cardiovascular outcomes. Current Cardiology Reviews. 2021 Nov 1;17(6):37–44. doi: 10.2174/1573403X17666210129101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newell P, Zogg C, Shirley H, et al. The effect of psychosocial risk factors on outcomes after aortic valve replacement. Cardiovascular Interventions. 2022 Nov 28;15(22):2326–2335. doi: 10.1016/j.jcin.2022.08.014. [DOI] [PubMed] [Google Scholar]
- 13.Patel JA, Nielsen FB, Badiani AA, Assi S, Unadkat VA, Patel B, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public health. 2020 Jun;183:110. [DOI] [PMC free article] [PubMed]
- 14.Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015 Sep 1;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 15.Bunker SJ, Colquhoun DM, Esler MD, et al. Stress” and coronary heart disease: psychosocial risk factors. Medical Journal of Australia. 2003;178(6):272–276. doi: 10.5694/j.1326-5377.2003.tb05193.x. Mar. [DOI] [PubMed] [Google Scholar]
- 16.Volz A, Schmid JP, Zwahlen M, Kohls S, Saner H, Barth J. Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. Journal of behavioral medicine. 2011;34:13–22. doi: 10.1007/s10865-010-9282-8. Feb. [DOI] [PubMed] [Google Scholar]
- 17.Sokoreli I, Pauws SC, Steyerberg EW, et al. Prognostic value of psychosocial factors for first and recurrent hospitalizations and mortality in heart failure patients: insights from the OPERA-HF study. European journal of heart failure. 2018;20(4):689–696. doi: 10.1002/ejhf.1112. Apr. [DOI] [PubMed] [Google Scholar]
- 18.Ishak WW, Edwards G, Herrera N, et al. Depression in heart failure: a systematic review. Innovations in clinical neuroscience. 2020 Apr 4;17(4-6):27. [PMC free article] [PubMed] [Google Scholar]
- 19.AbuRuz ME. Anxiety and depression predicted quality of life among patients with heart failure. Journal of multidisciplinary healthcare. 2018:367–373. doi: 10.2147/JMDH.S170327. Jul 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scherer M, Himmel W, Stanske B, et al. Psychological distress in primary care patients with heart failure: a longitudinal study. British Journal of General Practice. 2007 Oct 1;57(543):801–807. [PMC free article] [PubMed] [Google Scholar]
- 21.Shen BJ, Xu Y, Eisenberg S. Psychosocial and physiological predictors of mortality in patients of heart failure: Independent effects of marital status and C-reactive protein. International journal of behavioral medicine. 2017;24:83–91. doi: 10.1007/s12529-016-9579-2. Feb. [DOI] [PubMed] [Google Scholar]
- 22.Rodríguez-Artalejo F, Guallar-Castillón P, Herrera MC, et al. Social network as a predictor of hospital readmission and mortality among older patients with heart failure. Journal of cardiac failure. 2006 Oct 1;12(8):621–627. doi: 10.1016/j.cardfail.2006.06.471. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart & Lung. 2003 Mar 1;32(2):88–99. doi: 10.1067/mhl.2003.15. [DOI] [PubMed] [Google Scholar]
- 24.Snow SC, Fonarow GC, Ladapo JA, Washington DL, Hoggatt KJ, Ziaeian B. National rate of tobacco and substance use disorders among hospitalized heart failure patients. The American journal of medicine. 2019 Apr 1;132(4):478–488. doi: 10.1016/j.amjmed.2018.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nishimura M, Bhatia H, Ma J, et al. The impact of substance abuse on heart failure hospitalizations. The American journal of medicine. 2020 Feb 1;133(2):207–213. doi: 10.1016/j.amjmed.2019.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cowie MR, Mourilhe-Rocha R, Chang HY, et al. The impact of the COVID-19 pandemic on heart failure management: Global experience of the OPTIMIZE Heart Failure Care network. International Journal of Cardiology. 2022 Sep 15;363:240–246. doi: 10.1016/j.ijcard.2022.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shoaib A, Van Spall HG, Wu J, et al. Substantial decline in hospital admissions for heart failure accompanied by increased community mortality during COVID-19 pandemic. European Heart Journal-Quality of Care and Clinical Outcomes. 2021;7(4):378–387. doi: 10.1093/ehjqcco/qcab040. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Archives of internal medicine. 2001 Aug 13;161(15):1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 29.Song EK, Lennie TA, Moser DK. Depressive symptoms increase risk of rehospitalisation in heart failure patients with preserved systolic function. Journal of clinical nursing. 2009;18(13):1871–1877. doi: 10.1111/j.1365-2702.2008.02722.x. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. Journal of hospital medicine: an official publication of the Society of Hospital Medicine. 2009;4(4):211–218. doi: 10.1002/jhm.427. Apr. [DOI] [PubMed] [Google Scholar]
- 31.Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. Journal of the American College of Cardiology. 2002 Jan 2;39(1):83–89. doi: 10.1016/s0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.