Abstract
In a US national cohort study of cisgender sexual minority adolescents (SMAs), we prospectively (1) assessed whether within-person changes in homonegative school climate (i.e., school contextual factors that lead SMAs to feel unsafe or threatened) were associated with risk of probable body dysmorphic disorder (BDD) and (2) tested whether internalized homonegativity and negative expectancies mediated this association. Data came from consecutive time points (18-month, 24-month, 30-month) of the Adolescent Stress Experiences over Time Study (ASETS; N = 758). The Body Dysmorphic Disorder Questionnaire measured probable BDD. Sexual Minority Adolescent Stress Inventory subscales measured past 30-day minority stress experiences. Multilevel models were specified with person mean-centered predictor variables to capture within-person effects. Across one year of follow-up, 26.86% screened positive for probable BDD at least once. Model results indicated significant total (risk ratio [RR]=1.43, 95% credible interval [CI]=1.35–1.52) and direct effects (RR=1.18, 95% CI=1.05–1.34) of homonegative school climate. Internalized homonegativity was independently associated with probable BDD (RR=1.28, 95% CI=1.12–1.46) and mediated 49.7% (95% CI=12.4–82.0) of the total effect. There was limited evidence of mediation via negative expectancies. Implementing SMA-protective school policies and targeting internalized homonegativity in clinical practice may reduce the prevalence and incidence of probable BDD among cisgender SMAs.
Keywords (MeSH): Sexual and gender minorities, Adolescent, Minority stress, Body dysmorphic disorder, Schools, Bullying
1. Introduction
Body dysmorphic disorder (BDD) is characterized by severe distress and impairments in psychosocial, academic, and occupational functioning arising from preoccupations with perceived flaws in physical appearance (American Psychiatric Association, 2013). Evidence from both adult and adolescent community samples indicates that BDD affects approximately 2% of the general population at a given time (Schneider et al., 2017; Veale et al., 2016). Of note, prior studies have documented substantial comorbidity of BDD with other mental and behavioral health concerns, including eating disorders (Dingemans et al., 2012), major depression (Nierenberg et al., 2002), social anxiety disorder (Barahmand & Shahbazi, 2015), substance use disorders (Grant et al., 2005), and suicidal ideation and attempts (Angelakis et al., 2016).
A growing body of evidence suggests that, relative to their cisgender heterosexual counterparts, cisgender sexual minority adolescents (i.e., those with a gender identity congruent with sex assigned at birth and non-heterosexual identity, attraction, or behavior) are at elevated risk of body image concerns (Parker & Harriger, 2020). Adolescent-specific sexual orientation disparities in BDD are currently unknown, though recent research from a non-probability sample suggests that upward of 50% of sexual minority adults may screen positive for probable BDD (Convertino, Brady, et al., 2021). Given an average age of onset of 16–17 years old (Bjornsson et al., 2013), identifying mechanisms that may influence the development of probable BDD among cisgender sexual minority adolescents is essential for efforts to reduce overall BDD-related morbidity and mortality.
1.1. Sexual minority stress and BDD
Explanations for sexual orientation disparities in BDD and related body image concerns have often been grounded in minority stress theory (Brooks, 1981; Meyer, 2003). This theory posits that social, economic, and political conditions place sexual minority people at increased risk of exposure to distal stressors (e.g., sexual orientation-based discrimination and harassment) that, in turn, disproportionately expose them to proximal stressors (e.g., internalized homonegativity, fear of rejection due to sexual orientation) and lead to adverse health outcomes. Further refining minority stress theory (Brooks, 1981; Meyer, 2003), the psychological mediation framework has been proposed to explain how distal minority stressors “get under the skin” by acting through proximal stressors to influence adverse mental health outcomes (Hatzenbuehler, 2009).
The role of sexual minority stress has rarely been tested in the context of BDD, and the extant literature on BDD among sexual minority people has largely relied on samples of college-aged students (Boroughs et al., 2010), adults (Convertino, Brady, et al., 2021), or combined samples of youth and adults (Oshana et al., 2020), with two studies including measures of sexual minority stress. Among sexual minority adult men and women (ages 18–30), Convertino, Brady and colleagues (2021) found that internalized homophobia, sexual orientation concealment, and heterosexist discrimination were independently and positively associated with increased odds of a positive screen for BDD. Relatedly, among sexual minority boys and men (ages 14–35), Oshana et al. (2020) document the independent associations of sexual orientation concealment and gay-related rejection sensitivity with greater odds of a positive screen for BDD. To date, no prior BDD study has tested psychological mediation hypotheses concerning sexual minority stress. In the broader literature, a recent analysis among sexual minority young adults found support for pathways from distal minority stressors, through proximal minority stressors, to disordered eating behaviors (Convertino, Helm, et al., 2021). However, our current understanding of potential relationships and causal pathways remains limited concerning clinical and public health intervention targets to prevent and treat probable BDD.
While adding substantially to the literature, the above studies on sexual minority stress and BDD are limited in critical ways. Both studies were cross-sectional, thus precluding a clear understanding of temporal ordering and measurement of changes over time. For Convertino, Brady and colleagues (2021), the sample only included adults. For Oshana et al. (2020), results were aggregated across adolescents and adults (ages 14–35) and limited to sexual minority boys and men. Thus, results from these studies may not necessarily apply to sexual minority adolescents or, in the case of Oshana et al. (2020), generalize to sexual minority girls and women. This distinction is important given that adolescence is a critical developmental period consisting of social, physical, and psychological transitions affecting body image development. These include physical pubertal changes and heightened social pressures to achieve body ideals relative to those experienced in pre-adolescent years (Forney et al., 2019; Mulgrew, 2020; O’Dea & Abraham, 1999). Given evidence that BDD most often develops during teenage years (Bjornsson et al., 2013), a central goal of the current study was to identify specific social and contextual factors experienced by sexual minority people during adolescence and how these factors may impact probable BDD development across time.
1.2. School climates and BDD
Given the amount of time young people spend in school settings, schools may serve as a critical intervention point to prevent BDD development. As such, childhood bullying has been prospectively linked with the development of eating pathology and body image concerns during later adolescence and young adulthood (Copeland et al., 2015; Gattario et al., 2020). For sexual minority adolescents, this mechanism is of particular salience because they are more likely to report being victims of school bullying relative to their heterosexual counterparts (Birkett et al., 2009). Moreover, school climates (i.e., social or contextual factors in schools) that promote acceptance of sexual minority students and implement anti-bullying measures have been associated with improved academic performance, reduced victimization experiences, and lower levels of mental health concerns among sexual minority adolescents (Birkett et al., 2009; Goodenow et al., 2006; Kosciw et al., 2020). However, the association between homonegative school climate (i.e., those that may lead sexual minority students to feel unsafe due to their sexual orientation) and probable BDD remains unstudied.
1.3. The current study
We used a longitudinal multilevel modeling approach to (1) assess the degree to which within-person changes in homonegative school climate are associated with risk of probable BDD and (2) investigate the potential mediational roles of internalized homonegativity and negative expectancies. We define internalized homonegativity as the degree to which a sexual minority individual feels negatively about or desires to change their sexual orientation, and negative expectancies refer to pessimistic thoughts of negative life events anticipated to occur due to one’s sexual minority status. Given prior evidence of positive associations between sexual minority stress constructs with probable BDD and BDD symptoms (Convertino, Brady, et al., 2021; Oshana et al., 2020), we hypothesized that a positive association would exist between homonegative school climate and screening positive for probable BDD. Based on minority stress theory and the psychological mediation framework (Brooks, 1981; Hatzenbuehler, 2009; Meyer, 2003), we additionally hypothesized that internalized homonegativity and negative expectancies would have mediational effects such that greater levels of homonegative school climate would be indirectly associated with probable BDD through greater internalized homonegativity and negative expectancies.
2. Methods
2.1. Sample and study design
Data came from three consecutive time points (18-month follow-up, 24-month follow-up, and 30-month follow-up) of the Adolescent Stress Experiences over Time Study, a US national, longitudinal cohort study of sexual minority adolescent stress and health patterns. We limited the analysis to these time points as they were the only ones to administer the Body Dysmorphic Disorder Questionnaire. Hereafter, we refer to these time points as baseline, 6-month, and 12-month. Data collection periods were November 2019 to November 2020 (baseline), May 2020 to May 2021 (6-month), and November 2020 to November 2021 (12-month).
Participants were initially recruited online through advertisements on Facebook, Instagram, and YouTube. Advertisements were targeted to 20 cohorts stratified by gender (girls, boys), geographic region (West, Southwest, Midwest, Southeast, Northeast), and urbanicity (rural and urban defined using Rural-Urban Commuting Area Codes). Additional participants were recruited through respondent-driven sampling such that enrolled participants could refer friends who may be eligible for the study. All participants provided assent. Parental consent was waived to protect participants from the risk of sensitive information disclosure (e.g., sexual orientation) to parents/guardians that could occur during the consent process. A designated Institutional Review Board approved study procedures. From the parent cohort study, we identified participants who responded to at least one time point included in the current study (n = 969).
Due to the complex nature of body image concerns experienced by transgender and gender expansive adolescents, we further limited analyses to cisgender sexual minority adolescents. Participants affirmed their current gender identity at each time point, and these records were compared against their sex assigned at birth. Participants were coded as cisgender if their gender identity at each time point aligned with their sex assigned at birth (e.g., male sex assigned at birth and current gender identity of boy/man). Otherwise, they were coded as transgender and gender expansive. In cases where a participant had missing gender identity data while their complete data at other time points indicated they were cisgender, we assumed they were cisgender during the study period. After removing transgender and gender expansive adolescents (n = 211), our final analytic sample was 758 (total observations = 2274).
2.2. Measures
A complete list of questionnaire items from the current study is available in the Supplementary Materials.
2.2.1. Probable BDD
We used the Body Dysmorphic Disorder Questionnaire (BDDQ) to derive a binary indicator of probable BDD (Phillips, 2005). Participants had probable BDD if they met all the following criteria: (1) responded “Yes” to the questions “Are you worried about how you look?” and “Do you think about your appearance problems a lot and wish you could think about them less?”; (2) responded “Yes” to at least one of four items assessing whether these concerns had negatively affected their psychological, academic, social, or occupational functioning; (3) indicated that, on an average day, they spent one or more hours thinking about these concerns; and (4) responded “No” to the question “Is your main concern with how you look that you aren’t thin enough or that you might get too fat?” All other participants were classified as not having probable BDD (reference group).
To our knowledge, the psychometric properties of the BDDQ have not been tested in a community sample of sexual minority adolescents. However, the BDDQ has demonstrated excellent sensitivity and specificity to detect cases in a variety of settings and populations, including an inpatient psychiatric sample of adults and adolescents (sensitivity=100%; specificity=92.5%) (Grant et al., 2001), a community sample of Swedish adult women (sensitivity=94%; specificity=90%) (Brohede et al., 2013), and a clinical sample of adult dermatology patients (sensitivity=100%; specificity=93%) (Dufresne et al., 2001).
2.2.2. Sexual Minority Adolescent Stress Inventory (SMASI)
The SMASI is a 64-item measure composed of 11 subscales to assess a broad range of sexual minority adolescent stress experiences (Schrager et al., 2018). Items were binary (1 = yes, 0 = no). Respondents are first asked whether they had ever experienced the stressor in their lifetime. Those who endorsed a lifetime experience were subsequently asked whether this experience occurred in the past 30 days. The current study used three SMASI subscales (all measured in the past 30-day timeframe): homonegative school climate, internalized homonegativity, and negative expectancies. For all subscales, higher scores indicated greater experiences of the sexual minority stressor. To aid regression model interpretation given each subscale has a different number of items, we created percentage scores by dividing the sum of each SMASI subscale by the number of items and multiplying by 10. Subscales scores were then person mean-centered to capture within-person effects, such that slope parameters can be interpreted for every 10% increase in the subscale score relative to person-specific mean values.
The psychometric properties of the SMASI have been previously validated among sexual minority adolescents, including criterion and divergent validity (Goldbach et al., 2017). Prior analyses additionally confirm the factor structure of the SMASI with 11 subscales and demonstrate measurement invariance by gender, age, sexual identity, and race/ethnicity (Goldbach et al., 2021).
2.2.2.1. Homonegative school climate.
This 4-item subscale captured experiences of victimization and discrimination in school settings attributable to the participant’s sexual minority status (e.g., “I felt unsafe or threatened in school because I am LGBTQ”).
2.2.2.2. Internalized homonegativity.
This 7-item subscale captured the degree to which participants felt negatively about their sexual orientation or expressed desires to change their sexual orientation (e.g., “If I could, I would become straight”).
2.2.2.3. Negative expectancies.
This 3-item subscale captured pessimistic thoughts of negative life events (i.e., fear of rejection, expecting a worse life) that they expected to occur due to their sexual minority status (e.g., “I expect people will reject me when they find out I am LGBTQ”).
2.2.3. Demographics
We report the following participant demographic characteristics: age in years, gender identity (cisgender boy/man, cisgender girl/woman), race/ethnicity (Asian or Pacific Islander, Black or African American, Hispanic or Latine, Multiracial, Native American or Alaska Native, White). We additionally report US geographic region (West, Southwest, Midwest, Southeast, Northeast) and urbanicity (urban, rural) collected at baseline.
2.3. Model specification
Prior to building regression models, we reviewed prior literature and theory to guide the selection of an appropriate model specification. Using the “dagitty” (Textor et al., 2016) and “rethinking” (McElreath, 2021) packages, we created a directed acyclic graph to visually represent causal inference assumptions and to identify the necessary set of measured covariates to adjust for potential confounding of the primary causal effect of interest (i.e., homonegative school climate to probable BDD) (Fig. 1). Guided by minority stress theory (Brooks, 1981; Meyer, 2003) and the psychological mediation framework (Hatzenbuehler, 2009), we posited that the total causal effect of homonegative school climate on probable BDD could be separated into a direct effect and parallel indirect effects through internalized homonegativity and negative expectancies. From a developmental perspective and based on prior literature documenting how body image concerns (Bucchianeri et al., 2013; Schneider et al., 2017) and exposure to sexual minority stressors (Goldbach & Gibbs, 2017) vary from adolescence to young adulthood, we included age as a covariate to adjust for potential confounding of the total, direct, and indirect effects.
Fig. 1.
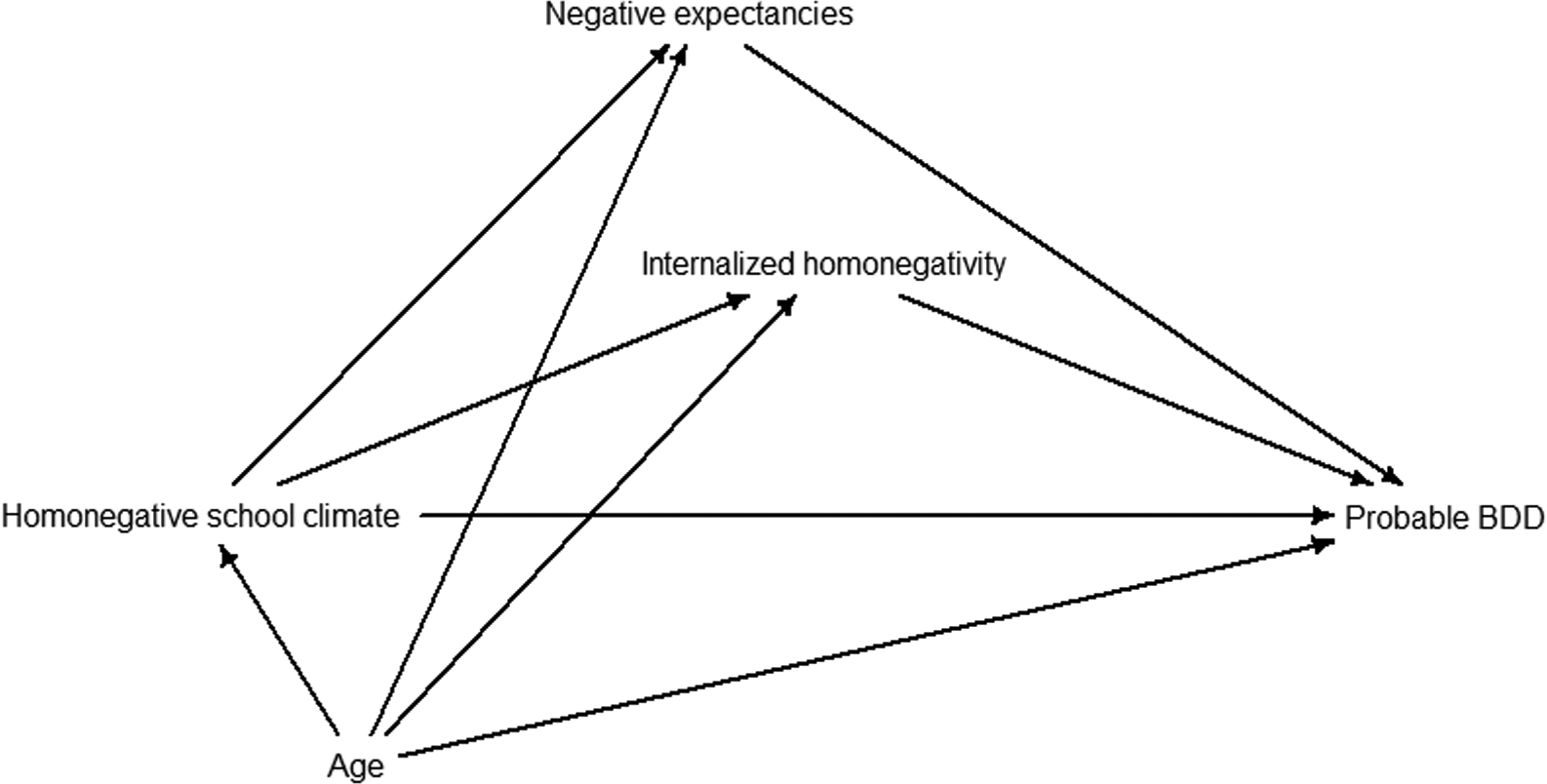
Directed acyclic graph. Note: Homonegative school climate (HSC) represents the primary exposure and probable body dysmorphic disorder (BDD) is the primary outcome. In the specified model, internalized homonegativity and negative expectancies are mediators along the causal pathway from HSC to probable BDD. Age is assumed to be associated with the exposure, mediators, and outcome, so it is included as a covariate to adjust for confounding of the total, direct, and indirect effects.
To estimate mediation effects with multiple mediators using the difference method (VanderWeele, 2016; VanderWeele & Vansteelandt, 2014), we sequentially fit four multilevel models with responses at each time point (level 1) nested within persons (level 2). To distinguish within-person and between-person effects of the minority stress variables, we included person mean-centered values as level 1 predictors and person-specific mean scores as level 2 predictors. With grand mean-centered age and time point as covariates, each model specified random intercepts and random slopes to allow participant-specific variation around fixed effects estimates. Model 1 estimated the total effect of homonegative school climate on probable BDD. Model 2 estimated the indirect effect through internalized homonegativity. Model 3 estimated the indirect effect through negative expectancies. Model 4 estimated the overall indirect effect through both mediator variables and the direct effect of homonegative school climate. Model equations are provided in the Supplemental Materials.
2.4. Missing data imputation
Multiple imputation with chained equations from the “mice” package was used to handle missing data by generating ten imputed datasets with ten iterations per imputation (van Buuren & Groothuis-Oudshoorn, 2011). We first specified an imputation method for each variable based on its distribution (e.g., logistic regression used for binary variables). For SMASI subscales, we imputed individual item responses and derived subscale scores for each dataset following imputation. The percentage of missing data on model variables at each time point were as follows: probable BDD (range=6.9–11.3%), homonegative school climate items (range=6.3–12.5%), internalized homonegativity items (range=6.5–12.1%) and negative expectancies items (range=6.4–11.3%).
2.5. Model estimation
All analyses were conducted in R version 4.2.2 (R Core Team, 2022), and model results were considered statistically significant at a two-sided 95% credible interval (CI) cutoff. Under a Bayesian estimation framework and in contrast to frequentist confidence intervals, this is interpreted as a 95% probability that the interval contains the population parameter value given the model, priors, and data (Hespanhol et al., 2019). For sample summary statistics presented in Table 1, we used frequentist confidence intervals.
Table 1.
Sample characteristics (N = 758).
| Characteristic | Mean (95% CI) | ||
|---|---|---|---|
| Probable BDD (%), screened positive at least once during study period | 26.86 (24.26, 29.46) | ||
| Baseline | 6-month | 12-month | |
| Probable BDD (%) | 12.22 (9.61, 14.82) | 11.16 (8.64, 13.69) | 16.36 (13.45, 19.27) |
| Homonegative school climate (%) | 15.81 (13.29, 18.33) | 12.80 (10.64, 14.97) | 15.09 (12.72, 17.46) |
| Internalized homonegativity (%) | 17.05 (14.92, 19.18) | 18.72 (16.51, 20.94) | 19.40 (17.07, 21.74) |
| Negative expectancies (%) | 30.95 (28.35, 33.56) | 31.27 (28.54, 33.99) | 29.56 (26.89, 32.23) |
| Age (years), range= 14–22 | 17.36 (17.28, 17.43) | 17.87 (17.80, 17.94) | 18.35 (18.28, 18.43) |
| N (%) | |||
| Gender | |||
| Cisgender boy/man | 259 (34.17) | ||
| Cisgender girl/woman | 499 (65.83) | ||
| Race and ethnicity | |||
| Asian or Pacific Islander | 59 (7.78) | ||
| Black or African American | 68 (8.97) | ||
| Hispanic or Latine | 104 (13.72) | ||
| Multiracial | 75 (9.89) | ||
| Native American or Alaska Native | 16 (2.11) | ||
| White | 436 (57.52) | ||
| U.S. geographic region | |||
| West | 197 (25.99) | ||
| Southwest | 103 (13.59) | ||
| Midwest | 134 (17.68) | ||
| Southeast | 175 (23.09) | ||
| Northeast | 149 (19.66) | ||
| Urbanicity | |||
| Urban | 613 (80.87) | ||
| Rural | 145 (19.13) |
Note: CI = confidence interval; BDD = body dysmorphic disorder. Estimates for probable BDD, homonegative school climate, internalized homonegativity, and negative expectancies were produced following multiple imputation procedures and pooled across ten imputed datasets. Due to raw count variability arising from differences across imputed datasets, probable BDD data overall and at each time point are presented as the pooled mean percentage with 95% CIs.
We used the “brms” package to fit models using Markov chain Monte Carlo (MCMC) methods (Bürkner, 2017), specifying four Markov chains, 2000 warmup iterations per chain, 4000 total iterations per chain, and uninformative priors. Models were estimated separately for each imputed dataset and pooled with the “brm_multiple” function (Bürkner, 2022). We used a Poisson outcome distribution and a log link function, and we report risk ratios from exponentiated coefficients. Poisson regression is commonly used in epidemiology to directly estimate risk ratios with binary outcome data (Chen et al., 2018; Naimi & Whitcomb, 2020), and it has advantageous qualities in the current study context. In contrast to odds ratios produced from logistic regression, the risk ratio is collapsible (Greenland et al., 1999), thus ensuring that marginal estimates are directly comparable to calculate the total, direct, and indirect effects accurately with the difference method (VanderWeele, 2016). Additionally, when the prevalence of the outcome is higher than the generally accepted threshold of 10% (as in the current study), odds ratios overestimate the risk of the outcome (Davies et al., 1998).
Model fit and convergence were evaluated using Gelman-Rubin convergence diagnostics, trace plots, and posterior predictive checks. All indicated model convergence and good fit for the observed data (Supplementary Materials). Skewness and kurtosis values and visual inspection of quantile-quantile plots indicated all posterior distributions of the primary model parameters approximated a normal distribution; thus, we present mean estimates with 95% CIs.
To calculate indirect effects, we extracted parameter-specific posterior distribution samples directly from the model fits (Yuan & MacKinnon, 2009). Using the difference method (VanderWeele, 2016; VanderWeele & Vansteelandt, 2014), we separately subtracted person mean-centered homonegative school climate parameter samples derived from Models 2–4 (indirect effect models) from the person mean-centered homonegative school climate parameter samples derived from Model 1 (total effect model). We then used the 2.5 and 97.5 percentiles of the difference estimate distribution to summarize 95% CIs around each mean. We present the percentage of the total effect mediated (i.e., the indirect effect) as the difference estimate distribution divided by the total effect distribution and then multiplied by 100.
2.6. Sensitivity analysis
To evaluate the robustness of results to different model and variable specifications, we performed the following sensitivity analyses: (1) include additional demographic variables (gender identity, race/ethnicity) as model covariates and (2) dichotomize the minority stress variables into “no past 30-day experience of the stressor” versus “any past 30-day experience of the stressor.” Overall, the results and takeaway messages obtained from the main model were robust to these sensitivity tests. One difference is that, for the dichotomous variable models, each person mean-centered minority stress variable was a significant, independent predictor of probable BDD risk. Thus, any experience (versus no experience) of the minority stressors in the current study may increase risk of probable BDD. Additional details can be found in the Supplementary Materials.
In the Supplementary Materials, we additionally report the prevalence of probable BDD inclusive of those who reported that their main body image concern was that they “aren’t thin enough” or “might get too fat.” This BDDQ item is used to screen-out individuals whose body image concerns may be better explained by an eating disorder (Phillips, 2005). Reanalyzing the data with this specification produced substantially higher prevalence of probable BDD at each time point (range=53.59–54.05%) and across the study period (73.03%).
3. Results
3.1. Sample characteristics
Descriptive statistics for the analytic sample are presented in Table 1. Participants had an average age of 17.36 years at baseline, and most participants were cisgender girls/women, White, and resided in urban areas. Overall, 26.86% screened positive for probable BDD at least once during the study period. The proportion at each time point with probable BDD was 12.22% (baseline), 11.16% (6-month), and 16.36% (12-month). Zero-order correlations comparing model variables within and across time points are presented in Table 2.
Table 2.
Zero-order correlations by time point (N = 758).
| Baseline | 6-month | 12-month | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BDD | HSC | IH | NE | Age | BDD | HSC | IH | NE | Age | BDD | HSC | IH | NE | Age | ||
| Baseline | BDD | — | 0.09 | 0.10 | 0.00 | −0.03 | 0.35 | 0.03 | 0.01 | 0.04 | −0.02 | 0.26 | −0.05 | −0.01 | 0.00 | −0.02 |
| HSC | — | 0.33 | 0.30 | −0.13 | −0.01 | −0.35 | −0.05 | −0.03 | −0.10 | 0.02 | −0.32 | −0.05 | −0.12 | −0.10 | ||
| IH | — | 0.33 | −0.03 | 0.00 | −0.06 | −0.21 | −0.03 | 0.00 | −0.08 | −0.09 | −0.29 | −0.14 | 0.02 | |||
| NE | — | −0.01 | −0.03 | −0.04 | −0.08 | −0.37 | −0.01 | −0.05 | −0.11 | −0.07 | −0.38 | 0.02 | ||||
| Age | — | −0.01 | 0.08 | −0.01 | 0.03 | 0.88 | −0.07 | −0.05 | −0.06 | −0.07 | 0.98 | |||||
| 6-month | BDD | — | 0.19 | 0.18 | 0.11 | 0.02 | 0.36 | 0.01 | 0.01 | 0.04 | −0.01 | |||||
| HSC | — | 0.65 | 0.38 | 0.18 | −0.05 | −0.05 | 0.00 | 0.02 | 0.09 | |||||||
| IH | — | 0.47 | 0.11 | 0.02 | 0.01 | −0.07 | 0.00 | 0.00 | ||||||||
| NE | — | 0.11 | −0.04 | −0.01 | −0.05 | −0.31 | 0.03 | |||||||||
| Age | — | −0.04 | −0.01 | −0.02 | −0.04 | 0.88 | ||||||||||
| 12-month | BDD | — | 0.53 | 0.56 | 0.44 | −0.06 | ||||||||||
| HSC | — | 0.74 | 0.60 | −0.05 | ||||||||||||
| IH | — | 0.63 | −0.06 | |||||||||||||
| NE | — | −0.08 | ||||||||||||||
| Age | — | |||||||||||||||
Note. BDD = probable body dysmorphic disorder. HSC = person mean-centered homonegative school climate. IH = person mean-centered internalized homonegativity. NE = person mean-centered negative expectancies. Correlations coefficients were calculated using Pearson (continuous and continuous) and point-biserial (categorical and continuous) methods.
3.2. Model results
Model results are summarized in Table 3. Overall, the total effect of person mean-centered homonegative school climate on probable BDD was significant (Model 1 risk ratio [RR =1.43, 95% CI=1.35–1.52), such that every 10% increase in homonegative school climate scores relative to an individual’s person-specific mean score was associated with 43% greater risk of probable BDD. After adjusting for both mediator variables, the direct effect of person mean-centered homonegative school climate on probable BDD remained significant (Model 4 RR=1.18, 95% CI=1.05–1.35). Person mean-centered internalized homonegativity was independently associated with an increased risk of probable BDD (Model 2 RR=1.30, 95% CI=1.14–1.48; Model 4 RR=1.28, 95% CI=1.12–1.46). In Model 3, person mean-centered negative expectancies had a positive association with probable BDD (RR=1.10, 95% CI=1.01–1.21); however, this association was not significant in the fully adjusted model (Model 4 RR=1.03, 95% CI=0.95–1.13).
Table 3.
Relative risk of probable BDD: Multilevel regression model results (N = 758).
| Parameters | Estimates |
|---|---|
| Model 1 | |
| PMC Homonegative school climate, RR (95% CI) | 1.43 (1.35, 1.52) |
| Random slopes variance | 0.0301 |
| Model 2 | |
| PMC Homonegative school climate, RR (95% CI) | 1.20 (1.07, 1.36) |
| Random slopes variance | 0.0118 |
| PMC Internalized homonegativity, RR (95% CI) | 1.30 (1.14, 1.48) |
| Random slopes variance | 0.0172 |
| Percentage of total effect mediated (95% CI) | 49.7% (12.4, 82.0) |
| Model 3 | |
| PMC Homonegative school climate, RR (95% CI) | 1.39 (1.26, 1.52) |
| Random slopes variance | 0.0277 |
| PMC Negative expectancies, RR (95% CI) | 1.10 (1.01, 1.21) |
| Random slopes variance | 0.0040 |
| Percentage of total effect mediated (95% CI) | 8.1% (−22.2, 36.3) |
| Model 4 | |
| PMC Homonegative school climate, RR (95% CI) | 1.18 (1.05, 1.34) |
| Random slopes variance | 0.0108 |
| PMC Internalized homonegativity, RR (95% CI) | 1.28 (1.12, 1.46) |
| Random slopes variance | 0.0159 |
| PMC Negative expectancies, RR (95% CI) | 1.03 (0.95, 1.13) |
| Random slopes variance | 0.0031 |
| Percentage of total effect mediated (95% CI) | 53.1% (16.3, 85.2) |
Note: RR = risk ratio. CI = credible interval. PMC = person mean-centered. Results were considered statistically significant (bold) if the 95% CI did not include the scale-specific null value. Models were structured with responses at each time point (level 1) nested within persons (level 2). Time point and grand mean-centered age were included as covariates. Minority stress variables (homonegative school climate, internalized homonegativity, negative expectancies) are person mean-centered to assess how within-person changes are associated with relative risk of probable BDD. Relative to person-specific mean values, RR estimates are interpreted as the relative risk of probable BDD associated with each 10% increase in minority stress percentage scores.
We found evidence of a significant indirect effect wherein internalized homonegativity mediated 49.7% (95% CI=12.4–82.0) of the total effect. Negative expectancies mediated 8.1% of the total effect, but this estimate was not significant (95% CI=−22.2 to 36.3). Additionally, the indirect effect estimate in fully adjusted model was significant (53.1%, 95% CI=16.3–85.2). In reference to the magnitude and significance of mediator variable parameter estimates in Model 4, this is primarily attributable to the effect internalized homonegativity rather than negative expectancies.
4. Discussion
Using data from a US national cohort study of cisgender sexual minority adolescents, the current study assessed how within-person changes in homonegative school climate were associated with risk of probable BDD across one year of follow-up. We additionally sought to identify whether within-person changes in proximal minority stressors (i.e., internalized homonegativity and negative expectancies) mediated this association. We found that, relative to their average level of homonegative school climate in the study period, participants who reported greater levels of homonegative school climate were at increased risk of having probable BDD. These findings suggest that implementing school policies that protect students from sexual orientation-based bullying and harassment may be a useful intervention to reduce the prevalence and incidence of probable BDD in this population. Independent of homonegative school climate and negative expectancies, we also found that greater within-person levels of internalized homonegativity (i.e., the degree to which one feels negatively about their sexual orientation) were prospectively associated with probable BDD, while there was no significant association between negative expectancies and probable BDD in the final model. Of note, internalized homonegativity partially mediated approximately half (49.7%) of the total effect of homonegative school climate on prospective risk of probable BDD.
While lower than prior prevalence estimates (approximately 50%) of probable BDD among sexual minority people (Gonzales & Blashill, 2021), a substantial proportion in the current study screened positive for probable BDD at each time point (range=11.16%−16.36%), with about one quarter (26.86%) screening positive at least once during the study period. Lower prevalence estimates in the current study may be due to sampling variation, particularly as both the current and prior study used non-probability sampling designs. Variation may also derive from measurement differences as Gonzales and Blashill (2021) used the Dysmorphic Concerns Questionnaire (DCQ) (Oosthuizen et al., 1998). In contrast with the BDDQ (Phillips, 2005), the DCQ does not differentiate between dysmorphic concerns attributable to fears of being too fat or not thin enough. The BDDQ scoring guidelines argue that these concerns may be better explained by an eating disorder (Phillips, 2005). Notably, when the current study data were reanalyzed to include those with concerns related to thinness/fatness, prevalence estimates of probable BDD at each time point were similar to those found by Gonzales and Blashill (2021). Regardless, estimates from both studies are substantially higher than a prior point prevalence estimate (1.7%) derived from a general community sample of adolescents (Schneider et al., 2017) and highlight a need for prevention and treatment efforts in this population.
We build on prior research linking sexual minority stressors and mental health symptoms among sexual minority adolescents. To our knowledge, this is the first study to document the prospective association of sexual minority stressors with probable BDD. Concerning homonegative school climate, our results are supported in the broader literature by findings of a prospective association between bullying and disordered eating behaviors among sexual minority youth (Katz-Wise et al., 2015). In this prior study, internalizing symptoms had a partial mediational effect, and gender and sexual orientation groups varied such that mediation was strongest among bisexual girls (Katz-Wise et al., 2015). In the current study, sensitivity analyses indicated that gender and race/ethnicity did not substantively alter associations among the main model variables. Concomitantly, prior research suggests certain subgroups of sexual minority people, such as Hispanic people and cisgender men, may have increased prevalence of probable BDD (Gonzales & Blashill, 2021). As both the current and prior study used convenience samples, future research with probability samples are needed to establish whether results apply equally across subgroups of sexual minority adolescents at the intersection of multiple dimensions of social identity and structural position.
Our finding of a positive association between internalized homonegativity and probable BDD aligns with prior research (Convertino, Brady, et al., 2021). We extend prior work by identifying internalized homonegativity as a longitudinal predictor of probable BDD and as a mediational mechanism that may link sexual orientation-based victimization experiences with probable BDD. Internalized homonegativity involves negative attitudes or beliefs towards one’s sexual orientation and may be conceptually related to BDD through general processes of negative self-appraisal, shame, and low self-esteem. There may also be certain shared characteristics of individuals who experience greater internalized homonegativity and those with probable BDD. For instance, those with increased levels of internalized homonegativity may also be predisposed to internalize other negative beliefs, including those concerning their body image. A potential causal pathway from exposure to homonegative school climates, through internalized homonegativity, to increased risk of probable BDD broadly aligns with the antecedents, beliefs, and consequences (ABC) Model (Ellis, 1991). Here, sexual orientation-based bullying serves as an antecedent event that gives rise to certain beliefs (i.e., internalized homonegativity), which then bring about emotional and behavioral consequences (i.e., probable BDD). Together, preventing sexual orientation-based school bullying and targeting internalized homonegativity in clinical practice may reduce the proportion of those with probable BDD in this population.
Caution of interpretation is warranted in light of certain limitations. Given that BDDQ scoring guidelines produce a binary screening result, we could not assess BDD symptom severity in this sample. Moreover, the BDDQ’s psychometric properties among sexual minority adolescents are not currently known, so measurement error may bias our results. Due to sample size restrictions, we also did not have sufficient statistical power to investigate the degree to which associations between sexual minority stressors and probable BDD may be moderated by intersectional position (e.g., those by mutually exclusive combinations of race and ethnicity, sex, gender, and sexual identity). Notably, data collection occurred partially during the COVID-19 pandemic. Participants who were engaged in remote learning due to school closures at the time of data collection may have reported reduced exposure to homonegative school climates, which may have impacted effect estimates. As in all observational research, our results may be biased due to unmeasured confounding. Finally, participants were recruited using a non-probability sampling method, so results may not be generalizable to all sexual minority adolescents in the United States. However, a strength of this study is that participants came from diverse localities across the United States with roughly equal breakdown across geographic regions.
4.1. Conclusions
Using a longitudinal modeling approach following participants over 12 months, the current study provides robust results that prospectively link within-person fluctuations in homonegative school climate with increased risk of probable BDD among cisgender sexual minority adolescents. Namely, as sexual minority adolescents experience more hostile or less affirming school environments than they are typically accustomed, they are more likely to screen positive for probable BDD. Independent of homonegative school climate, higher within-person levels of internalized homonegativity were also associated with a greater risk of probable BDD and mediated approximately half of the total effect of homonegative school climate. Future longitudinal studies utilizing probability samples and dimensional measures of BDD are needed to confirm and refine estimates obtained in the current study. This study has important implications for clinical practice and public health prevention efforts. Relative to general population estimates, a large proportion of sexual minority adolescents screened positive for probable BDD. Therefore, providers should screen for BDD among sexual minority adolescents to better ensure that this at-risk population is connected to treatment services. Sexual minority adolescents with probable BDD may also benefit from clinical interventions designed to reduce internalized homonegativity. From a public health perspective, practitioners and policymakers should focus on eliminating sexual orientation-based bullying and harassment in school settings. This could take the form of anti-bullying policies and non-discrimination protections for sexual minority students. Overall, sustained action on these multilevel determinants may prove effective for preventing and treating probable BDD among cisgender sexual minority adolescents.
Supplementary Material
Acknowledgements
This research was supported with funding from the National Institute on Minority Health and Health Disparities [grant number 1R01MD012252] and the National Institute of Mental Health [grant number T32MH019960].
Abbreviations:
- BDD
body dysmorphic disorder
Footnotes
CRediT authorship contribution statement
F. Hunter McGuire: Conceptualization, Methodology, Software, Formal analysis, Writing – original draft. Jeremy T. Goldbach: Conceptualization, Writing – review & editing, Supervision, Funding acquisition. John G. Senese IV: Data curation, Writing – review & editing. Juan R. Cabrera, Jr.: Data curation, Writing – review & editing. Sheree M. Schrager: Conceptualization, Methodology, Writing – review & editing, Supervision, Funding acquisition. Alexis E. Duncan: Writing – review & editing, Supervision.
Conflicts of interest
The authors have no conflicts of interest to report.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.bodyim.2023.02.007.
Data Availability
Data will be made available on request.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Angelakis I, Gooding PA, & Panagioti M (2016). Suicidality in body dysmorphic disorder (BDD): A systematic review with meta-analysis. Clinical Psychology Review, 49, 55–66. 10.1016/j.cpr.2016.08.002 [DOI] [PubMed] [Google Scholar]
- Barahmand U, & Shahbazi Z (2015). Prevalence of and associations between body dysmorphic concerns, obsessive beliefs and social anxiety. Asia-Pacific Psychiatry, 7(1), 54–63. 10.1111/appy.12085 [DOI] [PubMed] [Google Scholar]
- Birkett M, Espelage DL, & Koenig B (2009). LGB and questioning students in schools: The moderating effects of homophobic bullying and school climate on negative outcomes. Journal of Youth and Adolescence, 38(7), 989–1000. 10.1007/s10964-008-9389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornsson AS, Didie ER, Grant JE, Menard W, Stalker E, & Phillips KA (2013). Age at onset and clinical correlates in body dysmorphic disorder. Comprehensive Psychiatry, 54(7), 893–903. 10.1016/j.comppsych.2013.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boroughs MS, Krawczyk R, & Thompson JK (2010). Body dysmorphic disorder among diverse racial/ethnic and sexual orientation groups: Prevalence estimates and associated factors. Sex Roles, 63(9), 725–737. 10.1007/s11199-010-9831-1 [DOI] [Google Scholar]
- Brohede S, Wingren G, Wijma B, & Wijma K (2013). Validation of the body dysmorphic disorder questionnaire in a community sample of Swedish women. Psychiatry Research, 210(2), 647–652. 10.1016/j.psychres.2013.07.019 [DOI] [PubMed] [Google Scholar]
- Brooks VR (1981). Minority Stress and Lesbian Women. Lexington Books. [Google Scholar]
- Bucchianeri MM, Arikian AJ, Hannan PJ, Eisenberg ME, & Neumark-Sztainer D (2013). Body dissatisfaction from adolescence to young adulthood: Findings from a 10-year longitudinal study. Body Image, 10(1), 1–7. 10.1016/j.bodyim.2012.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bürkner P (2017). brms: An R package for bayesian multilevel models using stan. Journal of Statistical Software, 80(1), 1–28. [Google Scholar]
- Bürkner P Handle Missing Values with brms The Comprehensive R Archive Network. 〈https://cran.r-project.org/web/packages/brms/vignettes/brms_missings.html〉 2022. [Google Scholar]
- Chen W, Qian L, Shi J, & Franklin M (2018). Comparing performance between logbinomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Medical Research Methodology, 18(1), 63. 10.1186/s12874-018-0519-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convertino AD, Brady JP, Albright CA, Gonzales M, & Blashill AJ (2021). The role of sexual minority stress and community involvement on disordered eating, dysmorphic concerns and appearance- and performance-enhancing drug misuse. Body Image, 36, 53–63. 10.1016/j.bodyim.2020.10.006 [DOI] [PubMed] [Google Scholar]
- Convertino AD, Helm JL, Pennesi J-L, Gonzales M, & Blashill AJ (2021). Integrating minority stress theory and the tripartite influence model: A model of eating disordered behavior in sexual minority young adults. Appetite, 163, Article 105204. 10.1016/j.appet.2021.105204 [DOI] [PubMed] [Google Scholar]
- Copeland WE, Bulik CM, Zucker N, Wolke D, Lereya ST, & Costello EJ (2015). Does childhood bullying predict eating disorder symptoms? A prospective, longitudinal analysis. International Journal of Eating Disorders, 48(8), 1141–1149. 10.1002/eat.22459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies HTO, Crombie IK, & Tavakoli M (1998). When can odds ratios mislead? BMJ: British Medical Journal, 316(7136), 989–991. 10.1136/bmj.316.7136.989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingemans AE, van Rood YR, de Groot I, & van Furth EF (2012). Body dysmorphic disorder in patients with an eating disorder: Prevalence and characteristics. The International Journal of Eating Disorders, 45(4), 562–569. 10.1002/eat.20972 [DOI] [PubMed] [Google Scholar]
- Dufresne RG, Phillips KA, Vittorio CC, & Wilkel CS (2001). A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatologic Surgery: Official Publication for American Society for Dermatologic Surgery [et Al], 27(5), 457–462. 10.1046/j.1524-4725.2001.00190.x [DOI] [PubMed] [Google Scholar]
- Ellis A (1991). The revised ABC’s of rational-emotive therapy (RET). Journal of Rational-Emotive and Cognitive-Behavior Therapy, 9(3), 139–172. 10.1007/BF01061227 [DOI] [Google Scholar]
- Forney KJ, Keel PK, O’Connor S, Sisk C, Burt SA, & Klump KL (2019). Interaction of hormonal and social environments in understanding body image concerns in adolescent girls. Journal of Psychiatric Research, 109, 178–184. 10.1016/j.jpsychires.2018.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gattario KH, Lindwall M, & Frisén A (2020). Life after childhood bullying: Body image development and disordered eating in adulthood. International Journal of Behavioral Development, 44(3), 246–255. 10.1177/0165025419877971 [DOI] [Google Scholar]
- Goldbach JT, & Gibbs JJ (2017). A developmentally informed adaptation of minority stress for sexual minority adolescents. Journal of Adolescence, 55, 36–50. 10.1016/j.adolescence.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach JT, Schrager SM, & Mamey MR (2017). Criterion and divergent validity of the sexual minority adolescent stress inventory. Frontiers in Psychology, 8, 2057. 10.3389/fpsyg.2017.02057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach JT, Schrager SM, Mamey MR, & Rhoades H (2021). Confirming the reliability and validity of the sexual minority adolescent stress inventory in a national sample of sexual minority adolescents. Frontiers in Psychology, 12, 3457. 10.3389/fpsyg.2021.720199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales M, & Blashill AJ (2021). Ethnic/racial and gender differences in body image disorders among a diverse sample of sexual minority U.S. adults. Body Image, 36, 64–73. 10.1016/j.bodyim.2020.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodenow C, Szalacha L, & Westheimer K (2006). School support groups, other school factors, and the safety of sexual minority adolescents. Psychology in the Schools, 43(5), 573–589. 10.1002/pits.20173 [DOI] [Google Scholar]
- Grant JE, Kim SW, & Crow SJ (2001). Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. The Journal of Clinical Psychiatry, 62(7), 517–522. 10.4088/jcp.v62n07a03 [DOI] [PubMed] [Google Scholar]
- Grant JE, Menard W, Pagano ME, Fay C, & Phillips KA (2005). Substance use disorders in individuals with body dysmorphic disorder. quiz 404–405 The Journal of Clinical Psychiatry, 66(3), 309–316. 10.4088/jcp.v66n0306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Pearl J, & Robins JM (1999). Confounding and collapsibility in causal inference. Statistical Science, 14(1), 29–46. 10.1214/ss/1009211805 [DOI] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hespanhol L, Vallio CS, Costa LM, & Saragiotto BT (2019). Understanding and interpreting confidence and credible intervals around effect estimates. Brazilian Journal of Physical Therapy, 23(4), 290–301. 10.1016/j.bjpt.2018.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz-Wise SL, Scherer EA, Calzo JP, Sarda V, Jackson B, Haines J, & Austin SB (2015). Sexual minority stressors, internalizing symptoms, and unhealthy eating behaviors in sexual minority youth. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 49(6), 839–852. 10.1007/s12160-015-9718-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosciw JG, Clark CM, Truong NL, & Zongrone AD (2020). The 2019 National School Climate Survey: The Experiences of Lesbian, Gay, Bisexual, Transgender, and Queer Youth in Our Nation’s Schools. Gay, Lesbian, & Straight Education Network. [Google Scholar]
- McElreath R (2021). rethinking: Statistical Rethinking book package (R package version 2.21).
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulgrew K (2020). Puberty and Body Image. The Encyclopedia of Child and Adolescent Development. John Wiley & Sons Ltd.,1–9. 10.1002/9781119171492.wecad355 [DOI] [Google Scholar]
- Naimi AI, & Whitcomb BW (2020). Estimating risk ratios and risk differences using regression. American Journal of Epidemiology, 189(6), 508–510. 10.1093/aje/kwaa044 [DOI] [PubMed] [Google Scholar]
- Nierenberg AA, Phillips KA, Petersen TJ, Kelly KE, Alpert JE, Worthington JJ, Tedlow JR, Rosenbaum JF, & Fava M (2002). Body dysmorphic disorder in outpatients with major depression. Journal of Affective Disorders, 69(1–3), 141–148. 10.1016/s0165-0327(01)00304-4 [DOI] [PubMed] [Google Scholar]
- O’Dea JA, & Abraham S (1999). Onset of disordered eating attitudes and behaviors in early adolescence: Interplay of pubertal status, gender, weight, and age. Adolescence, 34(136), 671–679. [PubMed] [Google Scholar]
- Oosthuizen P, Lambert T, & Castle DJ (1998). Dysmorphic concern: Prevalence and associations with clinical variables. Australian and New Zealand Journal of Psychiatry, 32(1), 129–132. 10.3109/00048679809062719 [DOI] [PubMed] [Google Scholar]
- Oshana A, Klimek P, & Blashill AJ (2020). Minority stress and body dysmorphic disorder symptoms among sexual minority adolescents and adult men. Body Image, 34, 167–174. 10.1016/j.bodyim.2020.06.001 [DOI] [PubMed] [Google Scholar]
- Parker LL, & Harriger JA (2020). Eating disorders and disordered eating behaviors in the LGBT population: A review of the literature. Journal of Eating Disorders, 8. 10.1186/s40337-020-00327-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA (2005). The broken mirror: Understanding and treating body dysmorphic disorder. Oxford University Press. [Google Scholar]
- R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing. 〈https://www.R-project.org/〉. [Google Scholar]
- Schneider SC, Turner CM, Mond J, & Hudson JL (2017). Prevalence and correlates of body dysmorphic disorder in a community sample of adolescents. Australian & New Zealand Journal of Psychiatry, 51(6), 595–603. 10.1177/0004867416665483 [DOI] [PubMed] [Google Scholar]
- Schrager SM, Goldbach JT, & Mamey MR (2018). Development of the sexual minority adolescent stress inventory. Frontiers in Psychology, 9, 319. 10.3389/fpsyg.2018.00319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, & Ellison GT (2016). Robust causal inference using directed acyclic graphs: The R package “dagitty.”. International Journal of Epidemiology, 45(6), 1887–1894. 10.1093/ije/dyw341 [DOI] [PubMed] [Google Scholar]
- van Buuren S, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- VanderWeele TJ (2016). Mediation analysis: A practitioner’s guide. Annual Review of Public Health, 37, 17–32. 10.1146/annurev-publhealth-032315-021402 [DOI] [PubMed] [Google Scholar]
- VanderWeele TJ, & Vansteelandt S (2014). Mediation analysis with multiple mediators. Epidemiologic Methods, 2(1), 95–115. 10.1515/em-2012-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale D, Gledhill LJ, Christodoulou P, & Hodsoll J (2016). Body dysmorphic disorder in different settings: A systematic review and estimated weighted prevalence. Body Image, 18, 168–186. 10.1016/j.bodyim.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Yuan Y, & MacKinnon DP (2009). Bayesian mediation analysis. Psychological Methods, 14(4), 301–322. 10.1037/a0016972 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.


