Abstract
Background:
Guidelines recommend inhaled corticosteroids (ICS) upon Emergency Department (ED) discharge after acute asthma exacerbations.
Objectives:
We sought to identify rates and predictors of ICS prescription at ED discharge. Secondary outcomes include ICS prescription rates in a high-risk subgroup; outpatient follow-up rates within 30 days; and variation in ICS prescriptions among attending emergency physicians.
Methods:
This was a retrospective cohort study of adult asthma ED discharges for acute asthma exacerbation across 5 urban, academic hospitals. We used multivariable logistic regression to evaluate predictors of ICS prescription after adjusting for patient characteristics and hospital-level clustering.
Results:
Among 3,948 adult ED visits, ICS was prescribed in 6% (n=238) of visits. Only 14% (n=552) completed an outpatient visit within 30 days. Among patients with 2 or more ED visits in 12-months, the ICS prescription rate was 6.7%. ICS administration in the ED (OR 9.91; 95% CI 7.99-12.28) and prescribing beta-agonists on discharge (OR 2.67; 95% CI 2.08-3.44) were associated with higher odds of ICS prescription. Decreased odds of ICS prescription was associated with Hispanic ethnicity (OR 0.71; 95% CI 0.51-0.99) relative to Black race, and private (OR 0.75; 95% CI 0.62-0.91) or no insurance (OR 0.54; 95% CI 0.35-0.84) relative to Medicaid. One-third (36%, n=66) of ED attendings prescribed zero ICS prescriptions during the study period.
Conclusions:
ICS are infrequently prescribed on ED asthma discharge, and most patients do not have outpatient follow-up within 30 days. Future studies should examine the extent to which ED ICS prescriptions improve outcomes for patients with barriers to accessing primary care.
Keywords: asthma, inhaled corticosteroids, emergency department, prescription
Introduction
Asthma affects 1 in every 12 persons in the United States and is associated with 1.9 million emergency department (ED) visits every year.1 The cumulative cost of this care to the health system is significant, with recent estimates as high as $50 billion anually.2 Patients of lower socioeconomic status, as well as members of historically minoritized racial and ethnic groups–in particular those living in urban areas–are not only disproportionately more likely to suffer from asthma, but are also more likely to experience more asthma-related ED visits and poor outcomes.3 Therefore, interventions to improve asthma care and reduce ED visits for asthma are critical to improving overall health, health expenditures, and health equity.
For nearly three decades, U.S. and international guidelines have recommended inhaled corticosteroids (ICS) as an essential component of long-term maintenance therapy for patients with persistent asthma given their ability to reduce asthma-related deaths and exacerbations.4,5 Since 2007, both the Global Initiative for Asthma (GINA) and the National Institutes of Health (NIH) have recommended prescription of ICS on discharge for patients presenting to the ED with acute asthma exacerbations.6,7 However, while the effectiveness of ICS to prevent asthma exacerbations and ED visits is well established in the outpatient setting, research suggests that ICS prescription rates from the ED remain low.8-17 Prior evidence suggests that reluctance to prescribe ICS at ED discharge is due to a perception among ED clinicians that patients should receive these prescriptions from their primary care providers.18,19 However, patients who seek care in the ED often experience disproportionate barriers to accessing primary care.20-22 In order to clarify the role ED clinicians should play in ICS prescribing, more research is needed regarding ICS prescribing patterns from the ED.
Therefore, we sought to describe ICS prescription rates among adult ED asthma discharge and identify predictors of new ICS prescription on ED discharge. Our secondary outcomes include ICS prescription rates in a high-risk subgroup; rates of outpatient follow-up within 30 days of an ED visit for asthma; and variation in ICS prescriptions among attending emergency physicians.
Methods
Study Design and Patient Data
We conducted a descriptive study of patients with an Emergency Department visit to an academic health system consisting of five hospitals for a diagnosis of asthma between January 1, 2018 and January 31, 2020. Utilizing an electronic health records (EHR) pull with manual chart review validation of key data variables for 3% (n=150) of the sample, we identified patients aged 18 years or older with an encounter diagnosis of asthma – as defined by ICD-10-CM codes (International Classification of Diseases, Tenth Revision, Clinical Modification) who were discharged home after evaluation. Patients placed in observation were included if discharged without undergoing a full inpatient admission. Patients who were admitted, transferred, or who expired during their ED visit were excluded from the study. Patient demographics and encounter data, past and current prescriptions, medication administered in the ED, prescriptions provided at ED discharge, and subsequent outpatient and ED visits were extracted from the medical record.
The primary outcome was prescription of ICS on ED discharge from their index visit. A patient’s index visit was defined as their first visit to a Mount Sinai ED that met the study criteria within the study window. To avoid classifying ED revisits as index ED visits, we excluded ED visits with prior asthma-related ED visits or hospitalizations within the 30 preceding days. An ICS prescription was defined as an order for any of the following on discharge from the ED: Budesonide-Formoterol Fumarate, Fluticasone Propionate-Salmeterol, Fluticasone Propionate, Beclomethasone, Ciclesonide, Flunisolide, Mometasone, or Mometasone-Formoterol inhaled medications. In order to focus on new prescriptions for ICS, patients with a history of ICS prescriptions listed in their electronic medical record were also excluded.
Secondary outcomes included prescription rates among a high-risk subpopulation of patients with one or more prior ED visits for asthma within the 12 month period preceding their index ED visit, as two or more exacerbations requiring ED treatment within 12 months is defined as “persistent asthma” by GINA guidelines.4,7 We conducted a secondary analysis of this high-risk subpopulation to determine if prescribing patterns were different for that cohort most likely to benefit from ED ICS prescription. We also evaluated outpatient follow-up within 30 days of ED discharge in both the overall sample and among the subset of patients with a primary care provider listed in the electronic heath record. Finally, to determine the extent to which ICS prescription rates were driven by differences in clinician practice patterns, we calculated for each ED attending physician the proportion of visits for which ICS were prescribed among adult ED asthma visits by patients with no prior ICS prescription.
The study protocol was reviewed and received a determination of exemption from the institutional IRB.
Patient Characteristics:
Patient characteristics included sex, age, race/ethnicity, insurance status, language preference (English vs. non-English), smoking history (ever smoker vs never smoker), presence or absence of established Primary Care Physician (PCP), Charlson Comorbidity Index score, past ED utilization, past prescriptions, and hospital site of index ED visit.
Statistical Analysis:
Ordinal and binary variables were compared using chi-square tests. Continuous variables were expressed as means and compared using t-tests. We used multivariable logistic regression to adjust for sex, race, insurance, smoking history, Charlson score, medications given and prescribed, presence of established PCP, and follow-up visits, after accounting for hospital-level clustering. We calculated descriptive statistics for rates of outpatient primary care follow-up. We repeated the logistic model after restricting to the subset of high-risk patients with 2 or more total ED visits in 12 months.
Results:
Primary analysis:
The cohort consisted of 3,948 unique ED visits among 2,999 patients with no prior prescription for ICS (Table 1), the majority of whom were female (60%). Nearly half (44%) of the cohort identified as Black, 34% as Hispanic, and 8% as White. With respect to insurance, 41% had Medicaid, 18% had Medicare, 27% had private insurance, and 10% were uninsured. Approximately half (49%) of patients had an established PCP documented in their chart at the time of their index visit. Only 3 patients (0.001%) were discharged from Observation. Overall, ICS was prescribed in 6.02% (n=238) of all visits.
Table 1:
Overall Cohort Demographics for Emergency Department Asthma Visits
| Variable | Overall cohort (n=3948 visits*) (%) |
Received ICS+ prescription (n=238, 6%) (%) |
Did not receive ICS+ prescription (n=3710, 94%) (%) |
|---|---|---|---|
| Female sex | 60.0 | 63.0 | 59.8 |
| Age Category | |||
| 18-39 years | 44.4 | 36.6 | 44.9 |
| 40-64 years | 39.6 | 46.6 | 39.2 |
| 65 years and older | 16.0 | 16.8 | 15.9 |
| Race/Ethnicity | |||
| Black or African American | 44.9 | 49.6 | 44.6 |
| White | 8.3 | 8.0 | 8.4 |
| Hispanic | 34.4 | 30.3 | 35.6 |
| Asian | 2.0 | 2.1 | 2.0 |
| Other | 10.5 | 10.1 | 10.5 |
| Primary Language | |||
| English | 91.8 | 92.9 | 91.8 |
| Insurance Type | |||
| Medicaid | 40.9 | 45.8 | 40.8 |
| Medicare | 17.9 | 19.3 | 17.8 |
| Private | 26.8 | 22.7 | 27.0 |
| None/Uninsured | 10.2 | 6.7 | 10.5 |
| Other | 4.2 | 5.5 | 4.2 |
| Smoking status | |||
| Current or former smoker | 19.9 | 22.3 | 19.7 |
| Charlson Comorbidity Score | |||
| 2 or more | 10.3 | 12.2 | 10.2 |
| Primary Care Provider | |||
| Documented in Electronic Health Record | 48.7 | 48.3 | 48.7 |
| Medications received in ED | |||
| Received SABA& in ED | 92.6 | 91.2 | 92.6 |
| Received oral steroid in ED | 72.6 | 71.0 | 72.8 |
| Received ICS+ in ED | 2.5 | 13.0 | 1.8 |
| Discharge prescription for oral steroid | 66.8 | 76.1 | 66.2 |
| Discharge prescription for SABA & | 64.6 | 81.1 | 63.6 |
| Outpatient visit within 30 days | 14.0 | 16.0 | 13.9 |
| ED revisit within 30 days | 3.8 | 4.6 | 3.7 |
There were 3,948 visits among 2,999 unique patients.
ICS = Inhaled Corticosteroid
SABA = Short Acting Beta Agonist
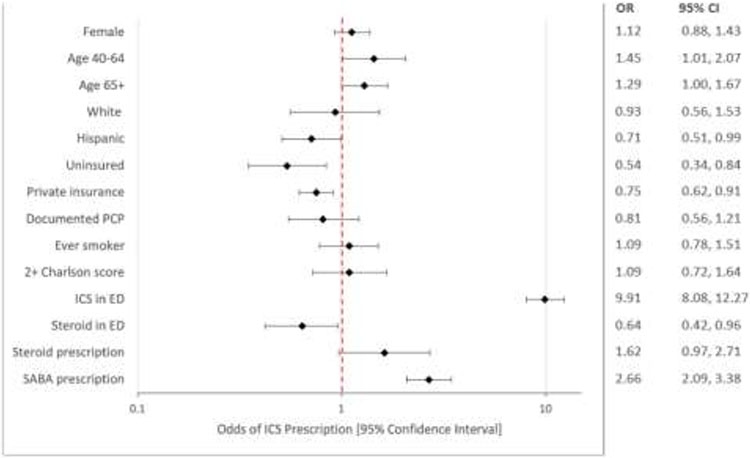
In multivariable logistic regression with the primary outcome of ICS prescription, patients age 40-64 years (OR 1.44; 95% CI 1.01-2.07) had increased odds of ICS prescription relative to age 18-39 (Figure 1). Patients who received an ICS in the ED during the course of treatment OR 9.96; 95% CI 8.08-12.27) and those who received prescription for a beta-agonist on discharge (OR 2.66; 95% CI 2.09-3.38) were more likely to receive an ICS prescription on discharge. Factors associated with decreased odds of ICS prescription included Hispanic ethnicity (OR 0.71; 95% CI 0.51-0.99) relative to Black race, and private insurance (OR 0.75; 95% CI 0.62-0.91) and no insurance (OR 0.54; 95% CI 0.35-0.84) relative to Medicaid. Patients who received a systemic steroid in the ED also had lower odds of ICS prescription on discharge (OR 0.64; 95% CI 0.42-0.96).
Figure 1: Multivariable logistic regression with primary outcome of ICS prescription (select variables*).
* Please see Appendix A for the complete model. Reference category for sex = male, age = 18-39 years, race = Black, insurance = Medicaid, PCP = no established PCP, Smoking status = never smoker, Charlson score = 0-1, ICS in ED = no ICS in ED, steroid in ED = no steroid in ED, steroid prescription = no steroid prescription, SABA prescription = no SABA prescription.
Subgroup Analysis for Persistent Asthma:
There were 1,815 unique visits among 870 patients with at least one ED visit within the 12 months prior to their index ED visit and no prior history of ICS prescription (Table 2). Within this cohort, ICS was prescribed in 6.67% (n=121) of visits, 17.96% of visits were followed by an outpatient visit within 30 days, and 7.44% were followed by an ED revisit within 30 days (Table 2).
Table 2:
Cohort Demographics for Patients with No ICS History and ≥1 Prior ED Visit
| Variable | Overall cohort (n=1815 visits*) (%) |
Received ICS+ prescription (n=121, 7%) (%) |
Did not receive ICS+ prescription (n=1694, 93%) (%) |
|---|---|---|---|
| Female sex | 53.9 | 56.2 | 53.8 |
| Age Category | |||
| 18-39 years | 41.0 | 38.8 | 41.2 |
| 40-64 years | 44.0 | 45.5 | 43.9 |
| 65 years and older | 15.0 | 15.7 | 15.0 |
| Race/Ethnicity | |||
| Black or African American | 50.5 | 57.9 | 49.9 |
| White | 5.8 | 4.1 | 6.0 |
| Hispanic | 35.4 | 32.2 | 35.7 |
| Asian | 1.5 | 0.8 | 1.5 |
| Other | 6.8 | 5.0 | 6.9 |
| Primary Language | |||
| English | 93.9 | 95.0 | 93.8 |
| Insurance Type | |||
| Medicaid | 47.8 | 52.9 | 47.4 |
| Medicare | 17.9 | 16.5 | 18.0 |
| Private | 21.5 | 18.2 | 21.8 |
| None/Uninsured | 9.0 | 5.8 | 9.3 |
| Other | 3.8 | 6.6 | 3.5 |
| Smoking status | |||
| Current or former smoker | 26.9 | 27.3 | 26.9 |
| Charlson Comorbidity Score | |||
| 2 or more | 15.5 | 16.5 | 15.5 |
| Primary Care Provider | |||
| Documented in Electronic Health Record | 57.2 | 59.5 | 57.0 |
| Medications received in ED | |||
| Received SABA& in ED | 93.6 | 91.7 | 93.7 |
| Received oral steroid in ED | 75.7 | 76.0 | 75.7 |
| Received ICS+ in ED | 3.6 | 16.5 | 2.7 |
| Discharge prescription for oral steroid | 69.3 | 80.2 | 68.5 |
| Discharge prescription for SABA & | 61.3 | 79.3 | 60.0 |
| Ambulatory visit within 30 days | 18.0 | 24.0 | 17.5 |
| ED revisit within 30 days | 7.4 | 9.1 | 7.3 |
There were 1815 visits among 870 unique patients.
ICS = Inhaled Corticosteroid
SABA = Short Acting Beta Agonist
In contrast to the primary analysis, there was no association between ICS prescription and race/ethnicity or insurance status within this cohort. The only variables associated with ICS prescription were receiving an ICS in the ED (OR 9.30; 95% CI 6.4-13.51) and receiving a prescription for a beta-agonist on discharge (OR 2.79; 95% CI 1.79-4.33). Evaluating the impact of baseline ED visits did not change the primary results.
Outpatient follow-up:
Only 13.98% (n=552) of visits were followed by an outpatient visit within 30 days, and 3.77% (n=149) of index visits were followed by an ED revisit within 30 days (Table 1). Among patients with a PCP documented in their chart, the 30-day outpatient follow-up rate was 21.3% (n=313).
Prescribing rates:
The median ED attending physician ICS prescription rate for patients with no prior history of ICS prescription was 5% and ranged from 0-40% (IQR 0-8). For those patients with no prior history of ICS prescription and at least one ED visit within the past 12 months, the median ED attending physician ICS prescription rate was 3% and ranged from 0-33% (IQR 0-4). One-third (36%, n=66) of ED attendings prescribed zero new ICS prescriptions for adult ED asthma patients during the study period.
Discussion:
In this observational study of adult asthma patients within a large, urban, academic health system, overall ICS prescription rates were extremely low and varied by demographic and non-clinical factors such as age, race, and insurance status. Even among a high-risk cohort of patients with 2 or more ED visits in a year, we observed very low rates of ICS prescribing as well as low rates of outpatient follow-up, with over 80% of patients having no outpatient follow-up within a month after their visit.
The lower likelihood of ICS prescription among Hispanic patients is concerning given that patients of Hispanic origin have twice the rate of ED visits relative to non-Hispanic white patients, and Puerto Ricans–who make up the single largest Hispanic subpopulation in New York City where our study was performed–have the highest rate of asthma mortality of any racial or ethnic subgroup in the United States.1,3,23 Hispanic patients are also significantly less likely to have access to a usual source of care as compared to non-Hispanic white patients, and are therefore also less likely to receive an ICS prescription in the outpatient setting.24 Underprescribing and underutilization of ICS among Hispanic populations is already well-documented in the outpatient setting, with non-Hispanic white patients with asthma nearly twice as likely to have an ICS prescription as compared to Hispanic patients.25,26 Our data suggests that this disparity is further perpetuated in the ED setting and offers an opportunity for interventions to improve access to this important medication.
Prescription rates that differ by insurance status suggest that factors related to socioeconomic status and access to care may contribute to low ED ICS prescription rates. While both patients with private insurance and uninsured patients were less likely to receive prescriptions for ICS on discharge as compared to patients with Medicaid, the mechanisms at play in both cases are likely different, especially given that private insurance is associated with lower odds of ED visits and admissions for patients with asthma.27-29 Cost is often cited as a prohibitive factor in the prescription of ICS, which may serve to explain why patients without insurance (most often those of low socioeconomic status) were less likely to receive a prescription.4,7,30,31 In contrast, patients with private insurance, a cohort synonymous with better access to care, may be perceived to be more likely to receive this prescription from an outpatient provider and thus less likely to require a prescription from the ED.
We found substantial variation in ICS prescription rates at the ED attending level, suggesting that dissemination of and adherence to asthma guidelines varies widely between ED clinicians. In our sample, nearly one-third of ED attending clinicians never prescribe ICS prescriptions for adult ED asthma patients, despite the low likelihood that patients will have an outpatient follow-up visit after ED discharge. When we limited our analysis to a high-risk cohort with at least 2 ED visits in a 12-month period, the major drivers of ED ICS prescription were ICS administration in the ED and receiving a prescription for a beta-agonist on discharge. This pattern suggests that among the patients with the highest need, the deciding factors regarding ICS prescription are not related to their demographics but rather to the standard practices of the providing physicians. The variation in ED attending prescription rates suggests both an opportunity to target ED clinicians in future quality improvement efforts and a need for further research examining the root of these prescribing differences.
A substantial body of evidence has established the effectiveness of ICS in improving asthma symptoms and quality of life and limiting exacerbations, ED visits, and hospitalizations.5,8,9,32 In 2019, the Global Initiative for Asthma (GINA) published sweeping new guidelines expanding their recommendation for ICS therapy to include not only patients with persistent asthma, but all those with any asthma diagnosis, stating: “For safety, GINA no longer recommends treatment of asthma in adolescents and adults with [short-acting beta-agonist (SABA)] alone. GINA recommends that all adults and adolescents with asthma should receive ICS controller-medication either as-needed (in mild asthma) or daily, to reduce their risk of serious exacerbations.”.30 Evidence suggests 70-84% of outpatient primary care providers prescribe inhaled corticosteroids when indicated; however, our analysis revealed that over 80% of patients discharged from the ED after an asthma exacerbation do not complete an outpatient visit within one month, implying many patients do not have opportunities outside of their ED visits to receive an ICS prescription.33,34 These findings suggest not only the need to develop and test interventions to improve care coordination and follow-up care after ED discharge, but also that there may be a role for ED physicians to play in initiating controller medications such as ICS for populations experiencing disproportionately poor access to care.
Previous surveys of emergency physician attitudes towards ICS prescribing indicate that two of the primary reasons cited for failure to prescribe are lack of clarity regarding guidelines and the belief that controller medications are not within the purview of emergency medicine.18,19 Given the updated guidelines regarding ICS therapy, the known benefits of ICS maintenance therapy, and the extremely low rates of outpatient follow-up after an ED visit for asthma, it may be time to reconsider this perspective. In fact, while emergency physicians may not have the same opportunities for longitudinal monitoring and medication titration available in the outpatient setting, recent evidence published in the New England Journal of Medicine (NEJM) suggests that even a single one-time intervention can have significant benefit for patients. In this pragmatic, open-label trial of 1201 adult Black and Latinx patients with moderate-to-severe asthma, provision of an ICS and one-time instruction on its use led to a lower annual rate of severe asthma exacerbations compared to usual care in the outpatient setting.35 Future research can further evaluate the feasibility and effectiveness of such interventions in the ED setting, but these findings suggest that there may well be a role to play for emergency physicians in initiating this important controller medication.
It is also unknown to what extent emergency physicians' input was incorporated into most recently updated guidelines recommending ICS prescription at ED discharge and whether these guidelines have been endorsed by emergency physician societies. Updated guidelines and policies written and/ or endorsed by emergency physician societies may be warranted in light in more recent evidence. Our study also underscores the need to critically re-examine the scope of ED care with respect to population health. While it is neither desirable nor sustainable for the ED to serve as the primary source of long-term care, the field of Emergency Medicine is, in many cases, already being asked to perform this function in its role as the health care system’s safety net.36 Updated practice guidelines that take this new reality into account would therefore be useful for emergency physicians to navigate the issue of ICS prescription both for patients with and without access to primary care.
Limitations:
Our findings should be interpreted within the context of several limitations. Patients with incomplete medication history, for example, those receiving primary care outside of the electronic health record, may have been inadvertently included in our cohort. Patients who returned to an ED or sought outpatient care outside of the health system would not have been captured in our EHR; however, prior research suggests that single center studies of asthma ED visit rates are comparable to statewide analyses.37 We focused on attending ED physicians because they have ultimate accountability for care. However, four of the five ED sites in the analysis are staffed by resident physicians and non-physician providers, so differences in the ED attending ICS prescription rate may be driven to a limited extent by the participation of other ED clinicians in patient care. Finally, our cohort was derived from within a large, diverse, urban, multi-center academic institution and the results of our analysis may not be applicable to other populations, including less diverse, suburban and/ or rural settings. Despite these limitations, however, we believe that our analysis utilizes a unique cohort and comparator group and provides valuable insights into a particularly vulnerable population.
Conclusions:
Our findings demonstrate extremely low rates of ICS prescription on ED asthma discharge, even among high-risk patients. Furthermore, over 80% of patients had no outpatient follow-up within 30 days of ED discharge, indicating that patients are not receiving ICS prescriptions at subsequent follow-up. Further research is needed to understand the extent to which ED ICS prescriptions improve outcomes for patients with barriers to accessing primary care. Interventions to improve ED prescribing and post-ED care coordination have the potential to improve access to ICS, improve health equity, and reduce overall asthma-related burden.
Supplementary Material
Article Summary:
1. Why is this topic important?
Asthma is a disease that disproportionately impacts communities of color and those of low socioeconomic status and interventions to improve asthma care and reduce ED visits for asthma are therefore critical to improving overall health and health equity. Inhaled corticosteroids (ICS) have been shown to be effective at preventing asthma exacerbations and Emergency Department (ED) visits in the outpatient setting, but research suggests that ICS prescription rates from the ED remain low.
2. What does this study attempt to show?
This study evaluates rates and predictors of ICS prescription from the ED after visits for asthma exacerbations, as well as rates of outpatient follow-up within 30 days of discharge. In this analysis we attempt to understand current practices regarding ICS prescription from the ED in order to determine whether patients seen in the ED for asthma exacerbations are receiving this important medication in a timely manner.
3. What are the key findings?
ICS are prescribed at only 6% of ED asthma discharges and 80% of ED asthma patients do not have any outpatient follow-up within 30 days. One-third of attending emergency physicians never prescribe ICS at ED discharge, and Hispanic, uninsured, or privately insured patients have the lowest odds of receiving an ICS prescription at discharge.
4. How is patient care impacted?
Given the known benefits of long-term ICS therapy and the extremely low rates of outpatient follow-up after an ED visit for asthma, further research is necessary to determine whether emergency physicians should consider prescribing ICS to patients on discharge after an ED visit for asthma. Clinical policies and interventions to improve ED prescribing and post-ED care coordination have the potential to improve access to ICS, improve health equity, and reduce overall asthma-related burden.
Financial Support:
Dr Lin was supported by NIH-NHLBI K23 HL143042. Dr. Abbott was supported by NIH-NHLBI 5T32HL129974-04 (PI: Lynne Richardson MD).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Works Cited
- 1.Moorman JE, Akinbami LJ, Bailey CM, et al. National surveillance of asthma: United States, 2001-2010. Vital Health Stat 3. 2012;(35):1–58. https://www.ncbi.nlm.nih.gov/pubmed/24252609 [PubMed] [Google Scholar]
- 2.Barnett SBL, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011;127(1):145–152. doi: 10.1016/j.jaci.2010.10.020 [DOI] [PubMed] [Google Scholar]
- 3.The Asthma and Allergy Foundation of America and the National Pharmaceutical Council. Ethnic Disparities in the Burden and Treatment of Asthma. Published online January 2005. https://www.aafa.org/media/1633/ethnic-disparities-burden-treatment-asthma-report.pdf
- 4.Self TH, Twilla JD, Rogers ML, Rumbak MJ. Inhaled corticosteroids should be initiated before discharge from the emergency department in patients with persistent asthma. J Asthma. 2009;46(10):974–979. doi: 10.3109/02770900903274483 [DOI] [PubMed] [Google Scholar]
- 5.Leung DYM, Nelson HS, Szefler SJ, Busse WW. Underprescribing of inhaled corticosteroids continues. J Allergy Clin Immunol. 2003;112(3):468. doi: 10.1016/S0091-6749(03)01947-X [DOI] [Google Scholar]
- 6.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Published online 2007. Available from: www.ginasthma.org
- 7.National Asthma Education, Prevention Program (National Heart, Lung, Blood Institute). Third Expert Panel on the Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health, National Heart, Lung, and Blood Institute; 2007. https://play.google.com/store/books/details?id=PEF8KMERKrcC [Google Scholar]
- 8.Boushey HA. Effects of inhaled corticosteroids on the consequences of asthma. J Allergy Clin Immunol. 1998;102(4 Pt 2):S5–16. doi: 10.1016/s0091-6749(98)70001-6 [DOI] [PubMed] [Google Scholar]
- 9.Rust G, Zhang S, Holloway K, Tyler-Hill Y. Timing of emergency department visits for childhood asthma after initial inhaled corticosteroid use. Popul Health Manag. 2015;18(1):54–60. doi: 10.1089/pop.2013.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blais L, Beauchesne MF. Use of inhaled corticosteroids following discharge from an emergency department for an acute exacerbation of asthma. Thorax. 2004;59(11):943–947. doi: 10.1136/thx.2004.022475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edmonds ML, Camargo CA, Saunders LD, Brenner BE, Rowe BH. Inhaled steroids in acute asthma following emergency department discharge. Cochrane Database Syst Rev. 2000;(3):CD002316. doi: 10.1002/14651858.CD002316 [DOI] [PubMed] [Google Scholar]
- 12.Rowe BH, Bota GW, Fabris L, Therrien SA, Milner RA, Jacono J. Inhaled budesonide in addition to oral corticosteroids to prevent asthma relapse following discharge from the emergency department: a randomized controlled trial. JAMA. 1999;281(22):2119–2126. doi: 10.1001/jama.281.22.2119 [DOI] [PubMed] [Google Scholar]
- 13.Sandifer JP, Jones AE. Are inhaled steroids beneficial on discharge from the emergency department for acute asthma? Ann Emerg Med. 2014;64(6):662–663. doi: 10.1016/j.annemergmed.2014.06.022 [DOI] [PubMed] [Google Scholar]
- 14.Andrews AL, Teufel RJ 2nd, Basco WT Jr, Simpson KN. A cost-effectiveness analysis of inhaled corticosteroid delivery for children with asthma in the emergency department. J Pediatr. 2012;161(5):903–907. doi: 10.1016/j.jpeds.2012.05.015 [DOI] [PubMed] [Google Scholar]
- 15.Brenner BE, Chavda KK, Camargo CA Jr. Randomized trial of inhaled flunisolide versus placebo among asthmatic patients discharged from the emergency department. Ann Emerg Med. 2000;36(5):417–426. doi: 10.1067/mem.2000.110824 [DOI] [PubMed] [Google Scholar]
- 16.Sin DD, Paul Man SF. Low-Dose Inhaled Corticosteroid Therapy and Risk of Emergency Department Visits for Asthma. Archives of Internal Medicine. 2002;162(14):1591. doi: 10.1001/archinte.162.14.1591 [DOI] [PubMed] [Google Scholar]
- 17.Rowe BH, Bota GW, Clark S, Camargo CA, Multicenter Airway Research Collaboration Investigators. Comparison of Canadian versus American emergency department visits for acute asthma. Can Respir J. 2007;14(6):331–337. doi: 10.1155/2007/450489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andrews AL, Teufel RJ 2nd, Basco WT Jr. Initiating inhaled steroid treatment for children with asthma in the emergency room: current reported prescribing rates and frequently cited barriers. Pediatr Emerg Care. 2013;29(9):957–962. doi: 10.1097/PEC.0b013e3182a219d0 [DOI] [PubMed] [Google Scholar]
- 19.Scarfone RJ, Zorc JJ, Angsuco CJ. Emergency physicians’ prescribing of asthma controller medications. Pediatrics. 2006;117(3):821–827. doi: 10.1542/peds.2005-0962 [DOI] [PubMed] [Google Scholar]
- 20.Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users. Acad Emerg Med. 2003;10(4):320–328. doi: 10.1111/j.1553-2712.2003.tbo1344.x [DOI] [PubMed] [Google Scholar]
- 21.Palmer E, Leblanc-Duchin D, Murray J, Atkinson P. Emergency department use: is frequent use associated with a lack of primary care provider? Can Fam Physician. 2014;60(4):e223–9. https://www.ncbi.nlm.nih.gov/pubmed/24733342 [PMC free article] [PubMed] [Google Scholar]
- 22.Rust G, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access: impact on adult use of emergency department services. Arch Intern Med. 2008;168(15):1705–1710. doi: 10.1001/archinte.168.15.1705 [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau. American FactFinder - Results. Published February 12, 2020. Accessed May 16, 2022. factfinder.census.gov.
- 24.Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Health Insurance Coverage and Access to Care Among Latinos: Recent Trends and Key Challenges.; 2021. https://aspe.hhs.gov/sites/default/files/documents/68c78e2fb15209dd191cf9b0b1380fb8/ASPE_Latino_Health_Coverage_IB.pdf
- 25.Kharat AA, Borrego ME, Raisch DW, Roberts MH, Blanchette CM, Petersen H. Assessing disparities in the receipt of inhaled corticosteroid prescriptions for asthma by Hispanic and non-Hispanic white patients. Ann Am Thorac Soc. 2015;12(2):174–183. doi: 10.1513/AnnalsATS.201405-186OC [DOI] [PubMed] [Google Scholar]
- 26.Crocker D, Brown C, Moolenaar R, et al. Racial and ethnic disparities in asthma medication usage and health-care utilization: data from the National Asthma Survey. Chest. 2009;136(4):1063–1071. doi: 10.1378/chest.09-0013 [DOI] [PubMed] [Google Scholar]
- 27.Qin X, Zahran HS, Malilay J. Asthma-related emergency department (ED) visits and post-ED visit hospital and critical care admissions, National Hospital Ambulatory Medical Care Survey, 2010-2015. J Asthma. 2021;58(5):565–572. doi: 10.1080/02770903.2020.1713149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinto JM, Wagle S, Navallo LJ, Petrova A. Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma. Children. 2020;7(9). doi: 10.3390/children7090107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu SY, Pearlman DN. Hospital readmissions for childhood asthma: the role of individual and neighborhood factors. Public Health Rep. 2009;124(1):65–78. doi: 10.1177/003335490912400110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2019. Inhaled corticosteroids should be initiated before discharge from the emergency department in patients with persistent asthma [DOI] [PubMed]
- 31.Institute of Medicine (US) Committee on the Consequences of Uninsurance. Who Goes Without Health Insurance? Who Is Most Likely to Be Uninsured? National Academies Press (US); 2001. Accessed June 3, 2022. https://www.ncbi.nlm.nih.gov/books/NBK223657/ [Google Scholar]
- 32.Bidwal M, Lor K, Yu J, Ip E. Evaluation of asthma medication adherence rates and strategies to improve adherence in the underserved population at a Federally Qualified Health Center. Res Social Adm Pharm. 2017;13(4):759–766. doi: 10.1016/j.sapharm.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 33.Akinbami LJ, Salo PM, Cloutier MM, et al. Primary care clinician adherence with asthma guidelines: the National Asthma Survey of Physicians. J Asthma. 2020;57(5):543–555. doi: 10.1080/02770903.2019.1579831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to asthma guidelines in children, tweens, and adults in primary care settings: A practice-based network assessment. Mayo Clin Proc. 2016;91(4):411–421. doi: 10.1016/j.mayocp.2016.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Israel E, Cardet JC, Carroll JK, et al. Reliever-Triggered Inhaled Glucocorticoid in Black and Latinx Adults with Asthma. N Engl J Med. 2022;386(16):1505–1518. doi: 10.1056/NEJMoa2118813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood). 2013;32(7):1196–1203. doi: 10.1377/hlthaff.2012.0825 [DOI] [PubMed] [Google Scholar]
- 37.Samuels-Kalow ME, Faridi MK, Espinola JA, Klig JE, Camargo CA Jr. Comparing Statewide and Single-center Data to Predict High-frequency Emergency Department Utilization Among Patients With Asthma Exacerbation. Acad Emerg Med. 2018;25(6):657–667. doi: 10.1111/acem.13342 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.