Abstract
Objective:
Proper use of inhaled medications is essential for management of asthma, as inhaled therapies are recommended as first-line for both prevention and treatment of asthma symptoms. Optimizing adherence requires identifying and understanding multiple layers of systemic complexity to obtaining and using these therapies and offering specific solutions to address these barriers. Bronfenbrenner’s socio-ecological model provides a framework for examining multilevel systems – both internal and external – that contribute to the management of childhood asthma. The four levels in this model consist of factors related to the individual, interpersonal relationships, organizational entities, and societal structures and rules. This narrative review identifies influences and factors related to asthma inhaler adherence by each level and offers evidence-based solutions to each obstacle.
Data Sources:
We conducted PubMed searches to identify relevant articles for barriers and solutions impacting asthma control at each level of the socio-ecological model.
Study Selection:
Common barriers to asthma control at each model level were identified. Pertinent studies for each barrier were identified and reviewed by the writing group for inclusion into the narrative review.
Results:
For each level of the socio-ecological model, three primary issues were identified based on the literature review. Approaches for addressing each issue in an evidence-based, systematic fashion are presented.
Conclusion:
Understanding the obstacles and potential interventions to achieve proper use of inhaled medications is a critical step necessary to develop and implement systematic solutions aimed at improving asthma control and morbidity for the more than 6 million affected children in the United States.
Keywords: Children, asthma, inhalers, insurance, pediatric
Introduction
Despite decades of medical research and established national guidelines (1), asthma remains a leading cause of pediatric healthcare utilization and poor quality of life (2). Uncontrolled asthma negatively impacts school performance (3), cognitive and physical development (4), and mental health (5). The foundation of asthma treatment includes quick-relief medication, and, for those who require it, daily preventive therapy. In most cases, both rescue and preventive therapies are inhaled. While most children with persistent asthma can prevent exacerbations, symptoms, and mortality with daily use of inhaled corticosteroids (ICS) (6), real-world adherence with asthma treatment plans as well as inhaler technique are suboptimal, resulting in reduced asthma control (7). Optimizing use of inhaled medication requires understanding and addressing multiple layers of systemic complexity combined with numerous artificial barriers.
Inhaled medications can be delivered by nebulization or hand-held inhalers. Each device type has different attributes as well as pros and cons for their use (Table 1). Selection of inhaled medication and device types should be tailored to the patient’s specific needs with consideration given to age, asthma severity and control, ease of inhaler use, and pharmacologic properties of a particular agent. Payor factors, including formulary coverage and out-of-pocket cost, are often non-medical reasons that drive inhaler selection and may be at odds with medical considerations, especially in pediatric patients (8).
Table 1.
Common device types for inhaled medications.
| Device type | Description | Examples | Pros | Cons |
|---|---|---|---|---|
| Nebulizer | Medical device requiring a power source to generate fine mist from a liquid for inhalation | Albuterol, ipratropium, budesonide respules | Does not require effort on the part of the patient; can be used at any age | Requires a machine and electricity; medication administration is more time consuming than inhaler devices |
| Pressured metered dose inhaler (pMDI) | Small, pressurized canister in an inhaler that dispenses a preset dose of medication for inhalation with actuation of the device | Albuterol HFA, Flovent HFA, Dulera HFA | Quick and convenient medication administration; Can be used at any age | In most cases requires the use of a valved holding chamber for optimal deposition |
| Dry powder inhaler (DPI) | Handheld, breath actuated inhaler device with medication contained in a premeasured dose of inhaled powder | Proair Respiclick, Advair Diskus, Asmanex Twisthaler, Pulmicort Turbuhaler | Quick and convenient medication administration; does not require any attachments for use | Requires attainment of a minimum inhaled flow rate; not appropriate for younger children; multiple different styles and designs which can be confusing for users |
| Soft mist inhaler (SMI) | Handheld inhaler which releases a soft mist slower than a pMDI | Spiriva Respimat | Quick and convenient medication administration; does not require any attachments for use | Devices can be complex and requires assembly by end-user; requires cooperation and coordination for use, not appropriate for younger children |
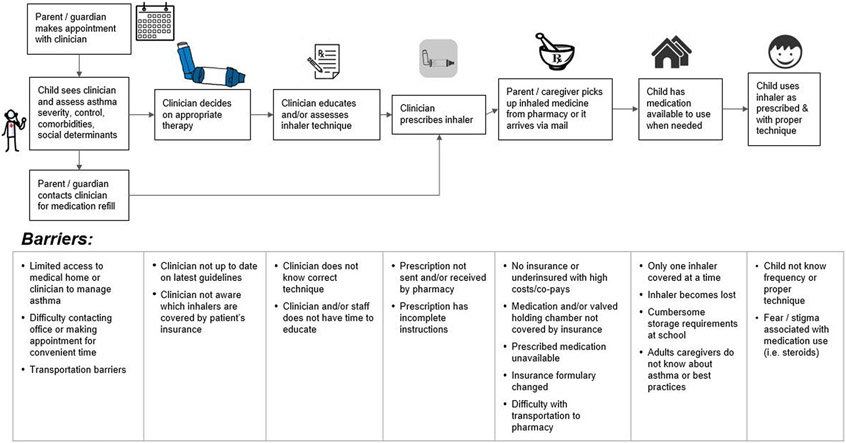
The pathway from needing asthma treatment to obtaining and using inhaler therapies has several steps with multiple potential barriers at each step (Figure 1). Historically, most children with persistent asthma have been prescribed two inhalers, an ICS-containing inhaler for maintenance and a short-acting bronchodilator for acute symptoms. With the 2020 National Heart, Lung, and Blood Institute (NHLBI) asthma guideline focused updates (1) and the 2022 Global Initiative for Asthma (GINA) guidelines (9), some children with asthma may only require a single combination inhaler containing ICS-formoterol for both maintenance and quick-relief purposes. Regardless of the specific medicines, education for patients and families on device use and written instructions (e.g. asthma action plan) are of paramount importance to promote real-world use and achieve asthma control. Once prescribed, families must be able to easily obtain the prescribed medications and accessories (e.g. valved holding chambers, “VHC”) before using the devices.
Figure 1.
Pathway to achieve proper inhaler use in children with asthma, with examples of barriers at each step.
All aspects of children’s lives are influenced by multiple interacting levels in society. These influences play critical roles in almost all areas of childhood development and health, including asthma management. Many of these influences are outside of the control of the individual and their immediate family, and competing interests often exist within these levels of influence. All influences at every level must be considered when working to optimize asthma care, including appropriate inhaler use.
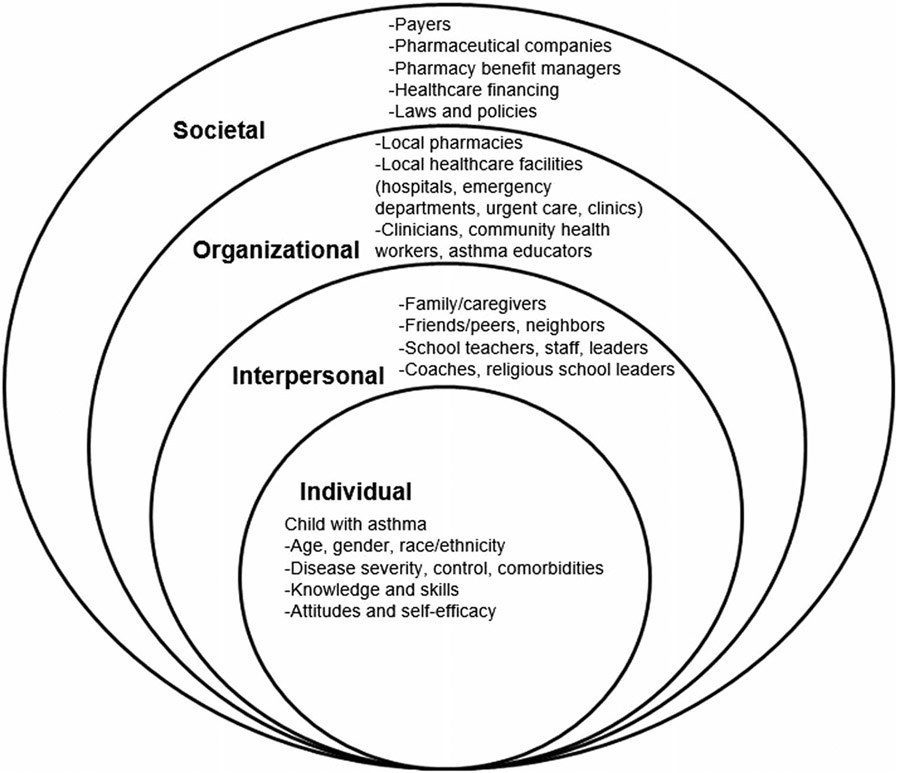
Bronfenbrenner’s socio-ecological model (10) provides a framework for examining multilevel systems – both internal and external – that contribute to childhood asthma management (Figure 2). The first level consists of factors directly related to the individual. The second level (or concentric layer) looks at the complex web of interpersonal relationships, including family, friends, peers, teachers, coaches, and religious leaders, who often directly influence children’s perceptions and behaviors. Expanding outward, there are organizational influences, including school systems, pharmacies, and healthcare systems, which may have different levels of integration and cohesion that can affect care and outcomes. Finally, at a societal level, there are influences and factors at the societal level, including payors, pharmaceutical companies, pharmacy benefit managers, as well as state and national healthcare laws and policies.
Figure 2.
Socio-ecological model for childhood asthma.
Methods
To conduct this review and frame it within the context of Bronfenbrenner’s socio-ecological model, common barriers to proper inhaler use were identified and then organized by each level of Bronfenbrenner’s socio-ecological model as outlined in Table 2. A literature search was conducted on PubMed using multiple keywords pertinent to the impact of each barrier along with potential solutions. Results were reviewed by all authors and synthesized into this focused review.
Table 2.
Barriers and possible solutions to obtaining and using inhalers organized by socio-ecological model levels.
| Socio-ecological model levels |
Examples of barriers to inhaler prescribing, accessibility, and proper use |
Potential solutions for improving inhaler prescribing and accessibility |
|---|---|---|
| 1. Individual | Perception of disease Child’s knowledge about asthma, proper inhaler use Expectations of disease control / self-efficacy |
|
| 2. Interpersonal | Family perceptions/knowledge about asthma and inhalers; barriers to medication administration, transportation Peer perceptions (e.g. bullying) School nurse availability, presence, knowledge, perceptions; teacher knowledge |
|
| 3. Organizational | Pharmacy access Navigation of complex health systems to obtain care and medication (53) Clinicians, community health workers, asthma educator limitations |
|
| 4. Societal | Lack of standardization of inhaler attributes (color, device style/instructions, etc.) by pharmaceutical companies Differences in coverage, co-pays, and formularies between payors Major disparities in healthcare access/outcomes caused by systemic/structural racism |
|
Results and discussion by socio-ecological level
Individual (child with asthma)
Disease severity, control, comorbidities
Barriers:
The individual child’s perception of their day-to-day symptoms and overall control are important factors in ongoing asthma management. A person who does not perceive their symptoms may be less inclined to use prescribed maintenance therapies and as a result experience worse outcomes (11). Conversely, one who over-perceives symptoms or misattributes symptoms of comorbidities (e.g. allergies, vocal cord dysfunction, anxiety) may inappropriately use quick-relief medications, placing them at risk for serious side effects.
Opportunities:
Routine assessments of asthma control both in clinic and at home, including in-person and mobile symptom scales and spirometry, may help children and their families to better understand asthma overall, recognize symptoms and trends in asthma control, and improve adherence with inhaled therapies (12,13). Multidisciplinary clinics for management of severe or difficult-to-treat asthma can create a unified treatment plan that balances patient and family-centered goals with treatment burden (14).
Knowledge and skills
Barriers:
Children at different developmental stages may have varied understanding of their condition. Key skills include developing an understanding of when and how to use their inhalers and other asthma medications, including self-carry and self-administration of quick-relief medications. Adolescents should progressively acquire self-management skills to facilitate independence, yet this time period often presents many challenges with maintaining asthma control due to competing social and academic pressures (15).
Opportunities:
Clinicians can assess knowledge and provide appropriate education, preferably within a broad socioecological framework encompassing multiple domains which affect knowledge and action (16). Important topics include rationale for daily use of controllers, when to use quick-relief medications, inhaler technique, and how and why to use VHCs. Older children and teenagers should be able to identify their controller and quick-relief medications. Patient and parent confidence in inhaler technique do not correlate well with actual technique, so objective assessment is crucial at every opportunity (17). Tailored educational opportunities with teach-back (18), pictorial asthma action plans (19), and mobile technology (13) can improve knowledge and management skills of children and their parents.
Attitudes and self-efficacy
Barriers:
Self-efficacy is a person’s belief in their own capacity to engage in actions that have a meaningful impact on their lives. Recurrent asthma exacerbations or frequent symptom impairment may leave children feeling like they do not have power over their asthma management. These beliefs may be reinforced or challenged by interpersonal relationships with parents, peers, healthcare professionals, and other influential people in the child’s life.
Opportunities:
Clinicians can help children with goal setting and understanding how treatments, including inhalers, improve their condition while providing positive feedback as patients meet goals of care. For older children and teens that resist using VHCs, alternative devices (i.e. DPIs) may be more appropriate. Interviewing teenagers without parents during visits may also identify unique concerns, delineate barriers to care, and help teenagers progress toward independent self-management.
Interpersonal
Family/caregivers
Barriers:
Many of the same barriers that can affect the individual child with asthma impact family and caregivers. Family members may lack knowledge and skills surrounding asthma and self-efficacy regarding their ability to improve their child’s condition. Families may have concerns about chronic medication use, especially steroids. Some families may use alternative or complimentary therapies at the exclusion of guideline-based care (20). Others may delegate responsibility for medication administration to young children before they are old enough to assume this responsibility. Conversely, families may fail to appropriately empower children as they mature. Competing priorities, such as housing instability, food insecurity, and multiple jobs, may impede medication pick-up from the pharmacy, daily/twice daily medication administration and/or ability to attend appointments (21). Lack of resources, such as transportation or comprehensive health insurance, may prevent families from attending routine visits for asthma management. Given the similarity in the appearance of multiple different inhaler products coupled with the fact that albuterol inhalers are available in 5+ colors, inhaler confusion and misuse is common (22), particularly for families with low health literacy or language barriers (23). Family dynamics, such as multiple primary households and caregivers, may add layers of complexity to optimal medical care and medication use.
Opportunities:
Clinicians must have the time to assess caregiver knowledge, expectations, and goals while assessing potential barriers to asthma management. These discussions are fundamental to improving parental self-efficacy, which is critical as parent confidence in medication use is associated with improved parental quality of life (24). Caregivers should be encouraged to monitor adherence in their older children and adolescents as they progress toward independence. In addition to assessing beliefs and expectations about inhaler use, clinical teams should address potential solutions to logistical barriers that may inhibit a family’s ability to administer asthma medications. Solutions may include facilitating medication home delivery, ensuring up-to-date prescriptions for inhalers and VHCs, strategizing approaches to transfer daily medications between different caregivers, and providing multiple copies of asthma action plans for all caregivers (e.g. parents, guardians, grandparents, school personnel).
Friends/peers
Barriers:
Acceptance within one’s peer group is typically considered essential by children and teenagers and is a major driver of behavior and choices, including for asthma management. Adolescents may not want to use inhalers around peers for fear of negative reactions or bullying, contributing to suboptimal adherence (25). Supportive peers, on the other hand, may improve acceptance of the child’s condition, adherence, and quality of life.
Opportunities:
Discussing peer influences at routine asthma visits can help clinicians better understand a child’s peer group and their values. Clinicians can meet one-on-one with adolescents to facilitate honest discussions. Inhaler strategies, such as using once-daily ICS dosing and using DPIs so VHCs are not required, may enhance adherence. Mobile applications may enable education and positive reinforcement while providing adolescents with accurate information, medication reminders, support, and means to securely and privately interact with healthcare professionals (13).
School/day care teachers, staff, nurses, leaders
Barriers:
Poorly controlled asthma negatively impacts school attendance and performance. Schools are integral in asthma management, yet direct communication between asthma healthcare professionals and schools is limited beyond providing paperwork to identify students with the condition and allow inhaler use. All school personnel, not just nurses, must be able to recognize when a child is experiencing an acute asthma exacerbation and poor asthma control as well as have knowledge, skills, and rescue inhalers available to take the necessary next steps, especially in schools without a full-time nurse. Many children with asthma do not have their own quick-relief medication accessible at school (26) and those that do often lack a second VHC for in-school use due to insurance coverage often only for one VHC annually.
Opportunities:
School-centered programs focused on improving coordination of asthma management, such as Building Bridges for Asthma Care Program, have significantly improved multiple domains of asthma care, including the proportion of students with completed school asthma action plans, quick-relief inhalers at school, and effective inhaler technique (27). Strong interest across stakeholders also exists for asthma management integration in Head Start programs (28). School nurse asthma programs that incorporate controller therapy administration in the school day to ensure adherence have reduced asthma-related hospital admissions and quick-relief medication refill rates (29,30). Given not every school has a full-time nurse, non-medical school staff should be trained on the indications and correct use of inhaled asthma medication during the school day, and inhalers should be accessible even if the nurse is not present. Fostering a supportive environment for inhaler self-carry amongst both peers and teachers may improve self-carry rates and asthma self-efficacy (26). Children who self-carry should know to alert teachers or parents when they are requiring albuterol more than once a day. Further, given the large percentage of children with asthma who do not keep a rescue inhaler at school, a small supply of undesignated quick-relief medications is critical in schools, as outlined by a recent policy statement by multiple professional medical organizations and key stakeholders, which also provides guidance for implementation (31).
Organizational
Pharmacies
Barriers:
Patients and families encounter multiple barriers to receiving chronic medications at pharmacies, including unavailability of medications, inconsistent processing of secondary insurance coverage of co-pays, no streamlined communication processes between pharmacies and prescribers, and lack of knowledge about updated asthma guidelines, for example Single Maintenance and Reliever Therapy (SMART) (1). Thus, patients and families may leave their local pharmacy without medications in-hand, often not knowing why.
Opportunities:
Partnerships and integration allowing direct receipt of medications by the patient in the clinic or hospital eliminates a major point of failure in obtaining medications (32). Educational partnerships can also assist pharmacists with understanding newer NHLBI guidelines which diverge from current FDA labeling, such as SMART. Pharmacists have the important opportunity with patients and families to review inhaler types, reinforce proper use and technique, and monitor refill rates. Improved integration between pharmacies and EMRs should provide clinicians with dispensing data to guide discussions and asthma management decisions during clinical encounters.
Healthcare facilities and systems
Barriers:
Patients receive asthma care in various settings – primary care, specialists, emergency departments/hospitals, free-standing urgent care sites. Without easy access to notes or prescription information across different electronic medical record (EMR) systems, clinicians do not have the most up-to-date information about acute exacerbations or revised asthma treatment plans (33). While mechanisms (including antiquated methods such as faxing) exist for communication amongst clinicians regardless of EMR, systemic barriers prevent fully integrated communication. Families seeking care through different healthcare systems may experience conflicting management recommendations if clinicians and stakeholders are not aware of all phases of care.
Opportunities:
National mandates should facilitate secure exchange of up-to-date clinical data and communications between health care professionals across various settings, including clinics, emergency departments, hospitals, and pharmacies. EMRs should be integrated with accurate insurance formulary and direct patient cost information to support decision-making. EMRs should provide appropriate prompts and flags for at-risk patients (e.g. recent ED visits or hospitalizations, not on appropriate controller therapy) while minimizing prompts with little clinical impact.
Clinicians, community health workers, asthma educators
Barriers:
Healthcare professionals face considerable challenges in delivering comprehensive guideline-based asthma care to children, including limited time and personnel resources. Asthma is one of many items that need to be addressed in a brief primary care encounter. Furthermore, disparities exist regarding the extent to which asthma guidelines are followed by prescribing physicians. Children with persistent asthma who are Black or Latinx, have public insurance, and/or receive care in hospital-based clinics and community health centers are less likely to be prescribed inhaled steroids than children who are White, have private insurance, and/or receive primary care in private practice settings (34). Frequent changes in asthma formularies and multitudes of new inhaler devices with different instructions can contribute to clinician confusion, suboptimal prescribing patterns, and inadequate patient and family education.
Opportunities:
Quality improvement projects, driven by key stakeholders and organizations, can help improve adherence to national guidelines in primary care. Easy Breathing©, a program that includes systematic symptom assessment, provider education on correct prescribing, and guidance on insurance formulary preferences, resulted in a three-fold increase in inhaled corticosteroid prescriptions and significant improvements in guideline adherence in urban primary care clinics in Hartford, CT (35). Development of an asthma specialty clinic within a primary care medical home can improve access to high-quality guideline-based asthma care, including correct identification of children who need to be prescribed ICS (36). Team members besides physicians and nurses, such as parent telephone coaches and trained health profession student educators can provide asthma education to patients and families to optimize correct use of inhaled medications (37,38). Other strategies for improving guideline adherence include appropriate electronic decision support tools (39), practice and community-level registries to promote guideline-based chronic disease management (40), and expanded funding for complementary resources outside the clinic walls such as community health workers (CHW) (41).
Societal
Disparities in access to care and outcomes
Barriers:
Disparities in access to care and outcomes continue to be significant problems. Asthma disproportionately affects minority and low-income youth with greater disparities among children under 5 years (33). Inequitable social determinants of health are associated with lower rates of guideline-based asthma care, including lower rates of maintenance inhaler prescriptions, and lower rates of specialist referral (42).
Opportunities:
Programs aimed at addressing asthma disparities have shown efficacy. CHWs and patient navigators can help ensure at-risk families have access to transportation and other resources to minimize the negative effects of social determinants of health. In addition, they can deliver culturally tailored education about asthma and its management, including medications. While CHW programs have proven beneficial (41), opportunities exist to move beyond grant-funded, short-term models to those that are reimbursed by insurers and integrated with clinical care and community settings. Telehealth, home spirometry, and other mobile health innovations are tools that can expand access in underserved and/or rural areas, though these may require technology and high-speed internet which remains challenging in some locations. Stakeholders at local, regional, and national levels must be involved in coordinated efforts to reduce air pollution and work toward equity in housing and living standards.
Payers
Barriers:
Public and private insurers play a critical role in ensuring children have access to necessary asthma medications. Restrictive formularies limit clinicians’ ability to prescribe guideline-based asthma medication, especially in children where consideration of device characteristics is essential to ensure proper use. Formulary changes for controller medication (sometimes called non-medical switching) leads to confusion and frustration for families and clinicians (43), resulting in reduction in lung function in pediatric asthma (44). Products preferred by insurance formularies may be inappropriate for younger children with asthma who are unable to use breath-actuated devices.
Out-of-pocket costs, even for covered medications, may be too expensive for families, leading to lower fill rates and increased healthcare utilization (45). Prescription drug costs in the United States are markedly higher than in other industrialized nations with no evidence of an association between research and development costs and prices; instead, prices are based almost solely on market conditions (46). Furthermore, complicated drug procurement, authorization, and distribution systems using pharmacy benefit managers as middlemen induce extra layers of complexity and lead to increased costs for patients (47). Prior authorization requirements contribute to administrative burden for clinic staff and lead to delays in obtaining therapy. Certain insurance plans may limit which specific pharmacies may be used, further limiting access. Barriers to obtaining prescription medications may lead to inappropriate, unregulated, and potentially dangerous use of over-the-counter alternative quick-reliever medications (e.g. Primatene Mist [epinephrine aerosol]) (48) or use of medications prescribed for another person (e.g. friend, relative).
Opportunities:
Formulary development should specifically consider children’s needs and allow flexibility for clinicians to select age and size appropriate products for a given class of asthma therapy. Uniform formularies across payers in a geographic area, such as the Massachusetts Medicaid Unified Formulary (49), may also help reduce clinician confusion. Policies should be implemented to limit non-medical switching and specifically to allow patients who are stable on a given therapy to remain on that therapy regardless of future formulary changes. Out-of-pocket costs for critical medications such as asthma inhalers should be minimized. Payors need to cover the cost of a sufficient number of VHCs along with pMDIs to ensure cost is not a barrier to a child using inhaled medication correctly at home and school.
Pharmaceutical companies
Barriers:
The design and availability of inhalers affect patient access and proper use. Pharmaceutical companies have a financial incentive to extend patents on their products to maintain trademark exclusivity and derive further profits. This incentive, in part, has led to the development of an array of unique asthma inhaler devices, sometimes altering traditional pMDIs and inhibiting their use by younger children. For example, in 2018, Teva’s pMDI version of QVAR®, readily usable in any age group with an appropriate VHC device, was replaced by the RediHaler® device, which is breath-actuated and therefore not practical for younger children. DPIs have assumed a dizzying array of proprietary formats, including Diskus®, Ellipta®, Flexhaler®, Handihaler®, Turbuhaler®, and Twisthaler®, each with unique idiosyncrasies and required sequence of steps for proper use.
Simple design choices may lead to confusion as well. Many patients differentiate their inhalers by color, such as blue for quick-relief inhalers and red for controller/maintenance inhalers. The lack of standardization of color schemes for different classes of inhalers makes it easy to confuse inhalers, especially when restrictive formularies and non-medical switching may lead to different products being prescribed than intended by the clinician. These issues may also contribute to families accumulating old inhalers, leading to confusion. In addition, canisters in pMDIs are interchangeable which, if done accidently, can inadvertently lead to children using the wrong product.
Beyond device design, other factors related to pharmaceutical companies can affect access. Supply chain disruptions, which have worsened during the COVID-19 pandemic, may cause shortages of products, requiring patients to be transitioned to other products. These changes may then create coverage issues with insurance formularies. Pharmaceutical companies may also incentivize payers with discounts to give preference to newer products on their formularies, leading to non-medical switching.
Opportunities:
Inhalers should be color coded by class across manufacturers to improve inhaler identification by patients, caregivers, and clinicians. Inhalers should be tamperproof to prevent inadvertent product switching, and device designs within product categories (e.g. pMDIs, DPIs) should be uniform for ease of use. In addition, stronger patent rules to minimize extensions could lead to more robust generics and lower costs. Pharmaceutical companies and payors should work to ensure that product shortages do not affect patient access to equivalent medications. Pharmaceutical companies and the FDA should consider studying safer alternatives for over-the-counter asthma medications, including reliever therapies that combine a bronchodilator and inhaled steroid for anti-inflammatory benefit, as these are likely to be safer and more effective than over-the-counter inhaled epinephrine.
Future directions and conclusions
The process for getting critical asthma medications to children and ensuring their proper use remains unnecessarily complex. Clinicians should be aware of how these barriers impact their patient population. Awareness is not sufficient; systematic changes are needed at various levels to remove barriers and ensure resources are available to address these barriers equitably. A comprehensive approach must be taken by national stakeholders and organizations across multiple domains to develop and implement strategies to ease this complexity and thereby improve pediatric asthma morbidity.
Funding
Anna Volerman was supported by the National Heart, Lung, and Blood Institute (K23HL143128).
Footnotes
Declaration of interest
S. Bickel, R. Cohen, J.P. Needleman, A. Volerman all declare they have no conflicts of interest, financial or otherwise to disclose.
References
- 1.Cloutier MM, Baptist AP, Blake KV, Brooks EG, Bryant-Stephens T, DiMango E, Dixon AE, Elward KS, Hartert T, Krishnan JA, et al. 2020 focused updates to the asthma management guidelines: report from the national asthma education and prevention program coordinating committee expert panel working group. J Allergy Clin Immunol. 2020;146(6):1217–1270. doi: 10.1016/j.jaci.2020.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kosse RC, Koster ES, Kaptein AA, de Vries TW, Bouvy ML. Asthma control and quality of life in adolescents: the role of illness perceptions, medication beliefs, and adherence. J Asthma. 2020;57(10):1145–1154. doi: 10.1080/02770903.2019.1635153 [DOI] [PubMed] [Google Scholar]
- 3.Koinis-Mitchell D, Kopel SJ, Farrow ML, McQuaid EL, Nassau JH. Asthma and academic performance in urban children. Ann Allergy Asthma Immunol. 2019;122(5):471–477. doi: 10.1016/j.anai.2019.02.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Byrne PM, Pedersen S, Schatz M, Thoren A, Ekholm E, Carlsson L-G, Busse WW. The poorly explored impact of uncontrolled asthma. Chest. 2013;143(2):511–523. doi: 10.1378/chest.12-0412 [DOI] [PubMed] [Google Scholar]
- 5.Selby L, Beresford F, Saglani S, Bush A, Jamalzadeh A, Moore Crouch R, Hall P, Fleming L. Emotional distress in children with problematic severe asthma is associated with parental anxiety and depression. Eur Respir J. 2018;52(suppl 62):PA1280. doi: 10.1183/13993003.congress-2018.PA1280 [DOI] [Google Scholar]
- 6.O'Byrne P, Fabbri LM, Pavord ID, Papi A, Petruzzelli S, Lange P. Asthma progression and mortality: the role of inhaled corticosteroids. Eur Respir J. 2019;54(1):1900491. doi: 10.1183/13993003.00491-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morton RW, Everard ML, Elphick HE. Adherence in childhood asthma: the elephant in the room. Arch Dis Child. 2014;99(10):949–953. doi: 10.1136/archdischild-2014-306243 [DOI] [PubMed] [Google Scholar]
- 8.Lab CsHoPP. When Medication Switching Threatens Care of Children with Asthma. 2018. Available from: https://policylab.chop.edu/sites/default/files/pdf/publications/When_Medication_Switching_Threatens_Care_Of_Children_With_Asthma.pdf.
- 9.Asthma GIf. Global Strategy for Asthma Management and Prevention. 2022. [Google Scholar]
- 10.Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. 2012;39(3):364–372. doi: 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- 11.Rhee H, Belyea MJ, Halterman JS. Adolescents’ perception of asthma symptoms and health care utilization. J Pediatr Health Care. 2011;25(2):105–113. doi: 10.1016/j.pedhc.2009.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kupczyk M, Hofman A, Kołtowski Ł, Kuna P, Łukaszyk M, Buczyłko K, Bodzenta-Łukaszyk A, Nastałek P, Soliński M, Dąbrowiecki P, et al. Home self-monitoring in patients with asthma using a mobile spirometry system. J Asthma. 2021;58(4):505–511. doi: 10.1080/02770903.2019.1709864 [DOI] [PubMed] [Google Scholar]
- 13.Roberts C, Sage A, Geryk L, Sleath B, Carpenter D. Adolescent preferences and design recommendations for an asthma self-management app: mixed-methods study. JMIR Form Res. 2018;2(2):e10055. doi: 10.2196/10055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leibel S, Geng B, Phipatanakul W, Lee E, Hartigan P. Screening social determinants of health in a multidisciplinary severe asthma clinical program. Pediatr Qual Saf. 2020;5(5):e360. doi: 10.1097/pq9.0000000000000360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson PD, Jayasuriya G, Haggie S, Uluer AZ, Gaffin JM, Fleming L. Issues affecting young people with asthma through the transition period to adult care. Paediatr Respir Rev. 2022;41:30–39. doi: 10.1016/j.prrv.2021.09.005 [DOI] [PubMed] [Google Scholar]
- 16.Rangachari P, May KR, Stepleman LM, Tingen MS, Looney S, Liang Y, et al. Measurement of key constructs in a holistic framework for assessing self-management effectiveness of pediatric asthma. Int J Environ Res Public Health. 2019; 16(17):3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volerman A, Toups MM, Hull A, Press VG. Does inhaler technique align with confidence among African–American children and their parents? Ann Allergy Asthma Immunol. 2019;123(1):100–101. doi: 10.1016/j.anai.2019.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, Brancati FL, Krishnan JA. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172(8):980–986. doi: 10.1164/rccm.200409-1291OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duncan CL, Walker HA, Brabson L, Williford DN, Hynes L, Hogan MB. Developing pictorial asthma action plans to promote self-management and health in rural youth with asthma: a qualitative study. J Asthma. 2018;55(8):915–923. doi: 10.1080/02770903.2017.1371743 [DOI] [PubMed] [Google Scholar]
- 20.Adams SK, Murdock KK, McQuaid EL. Complementary and alternative medication (CAM) use and asthma outcomes in children: an urban perspective. J Asthma. 2007;44(9):775–782. doi: 10.1080/02770900701645835 [DOI] [PubMed] [Google Scholar]
- 21.Smith LA, Bokhour B, Hohman KH, Miroshnik I, Kleinman KP, Cohn E, Cortés DE, Galbraith A, Rand C, Lieu TA, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122(4):760–769. doi: 10.1542/peds.2007-2750 [DOI] [PubMed] [Google Scholar]
- 22.Wu AC, Li L, Fung V, Kharbanda EO, Larkin EK, Butler MG, Galbraith A, Miroshnik I, Davis RL, Horan K, et al. Mismatching among guidelines, providers, and parents on controller medication use in children with asthma. J Allergy Clin Immunol Pract. 2016;4(5):910–916. doi: 10.1016/j.jaip.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inkelas M, Garro N, McQuaid EL, Ortega AN. Race/ethnicity, language, and asthma care: findings from a 4-state survey. Ann Allergy Asthma Immunol. 2008;100(2):120–127. doi: 10.1016/S1081-1206(10)60420-6 [DOI] [PubMed] [Google Scholar]
- 24.Kan K, Fierstein J, Boon K, Zavos P, Volerman A, Vojta D, Gupta RS, Madeleine Kanaley. Parental quality of life and self-efficacy in pediatric asthma. J Asthma. 2021;58(6):742–749. doi: 10.1080/02770903.2020.1731825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen R, Franco K, Motlow F, Reznik M, Ozuah PO. Perceptions and attitudes of adolescents with asthma. J Asthma. 2003;40(2):207–211. doi: 10.1081/jas-120017992 [DOI] [PubMed] [Google Scholar]
- 26.Volerman A, Kim TY, Sridharan G, Toups M, Hull A, Ignoffo S, Sharp LK, Press VG. A Mixed-methods study examining inhaler carry and use among children at school. J Asthma. 2020;57(10):1071–1082. doi: 10.1080/02770903.2019.1640729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cicutto L, Gleason M, Haas-Howard C, White M, Hollenbach JP, Williams S, McGinn M, Villarreal M, Mitchell H, Cloutier MM, et al. Building bridges for asthma care program: a school-centered program connecting schools, families, and community health-care providers. J Sch Nurs. 2020;36(3):168–180. doi: 10.1177/1059840518805824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruvalcaba E, Callaghan-Koru J, Rand CS, Eakin MN. Integrating asthma management and care in Maryland head start programs: a qualitative assessment of opportunities and needs. Eval Program Plann. 2019;77:101684. doi: 10.1016/j.evalprogplan.2019.101684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trivedi M, Patel J, Lessard D, Kremer T, Byatt N, Phipatanakul W, Pbert L, Goldberg R. School nurse asthma program reduces healthcare utilization in children with persistent asthma. J Asthma. 2018; 55(10):1131–1137. doi: 10.1080/02770903.2017.1396473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trivedi M, Patel J, Hoque S, Mizrahi R, Biebel K, Phipatanakul W, Lemon SC, Byatt N, Gerald LB, Rosal M, et al. Alignment of stakeholder agendas to facilitate the adoption of school-supervised asthma therapy. Pediatr Pulmonol. 2020;55(3):580–590. doi: 10.1002/ppul.24611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Volerman A, Lowe AA, Pappalardo AA, Anderson CMC, Blake KV, Bryant-Stephens T, Carr T, Carter H, Cicutto L, Gerald JK, et al. Ensuring access to albuterol in schools: from policy to implementation. An Official ATS/AANMA/ALA/NASN Policy Statement. Am J Respir Crit Care Med. 2021;204(5):508–522. doi: 10.1164/rccm.202106-1550ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sauers-Ford HS, Moore JL, Guiot AB, Simpson BE, Clohessy CR, Yost D, Mayhaus DC, Simmons JM, Gosdin CH. Local pharmacy partnership to prevent pediatric asthma reutilization in a satellite hospital. Pediatrics. 2016;137(4):e20150039. doi: 10.1542/peds.2015-0039 [DOI] [PubMed] [Google Scholar]
- 33.Childs E, Laws MA, Drainoni M-L, Nath A, Reid MJ, Sandel M, Cohen RT. Caring for young children with asthma: perspectives from urban community health centers. J Urban Health. 2017;94(6):824–834. doi: 10.1007/s11524-017-0186-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galbraith AA, Smith LA, Bokhour B, Miroshnik IL, Sawicki GS, Glauber JH, Hohman KH, Gay C, Lieu TA. Asthma care quality for children with minority-serving providers. Arch Pediatr Adolesc Med. 2010;164(1):38–45. doi: 10.1001/archpediatrics.2009.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cloutier MM, Wakefield DB, Carlisle PS, Bailit HL, Hall CB. The effect of easy breathing on asthma management and knowledge. Arch Pediatr Adolesc Med. 2002;156(10):1045–1051. doi: 10.1001/archpedi.156.10.1045 [DOI] [PubMed] [Google Scholar]
- 36.Snyder DA, Thomas OW, Gleeson SP, Stukus DR, Jones LM, Regan C, Shamansky A, Allen ED. Reducing emergency department visits utilizing a primary care asthma specialty clinic in a high-risk patient population. J Asthma. 2018;55(7):785–794. doi: 10.1080/02770903.2017.1369989 [DOI] [PubMed] [Google Scholar]
- 37.Garbutt JM, Banister C, Highstein G, Sterkel R, Epstein J, Bruns J, Swerczek L, Wells S, Waterman B, Strunk RC, et al. Telephone coaching for parents of children with asthma: impact and lessons learned. Arch Pediatr Adolesc Med. 2010;164(7):625–630. doi: 10.1001/archpediatrics.2010.91 [DOI] [PubMed] [Google Scholar]
- 38.Rice JL, Matlack KM, Simmons MD, Steinfeld J, Laws MA, Dovey ME, Cohen RT. LEAP: A randomized-controlled trial of a lay-educator inpatient asthma education program. Patient Educ Couns. 2015;98(12):1585–1591. doi: 10.1016/j.pec.2015.06.020 [DOI] [PubMed] [Google Scholar]
- 39.Gupta S, Price C, Agarwal G, Chan D, Goel S, Boulet L-P, Kaplan AG, Lebovic G, Mamdani M, Straus SE, et al. The Electronic Asthma Management System (eAMS) improves primary care asthma management. Eur Respir J. 2019;53(4):1802241. doi: 10.1183/13993003.02241-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shelef DQ, Badolato GM, Badh R, Owotomo O, Kachroo N, Weissman M, Teach SJ, Shah AY. Creation and validation of a citywide pediatric asthma registry for the District of Columbia. J Asthma. 2022;59(5):901–909. doi: 10.1080/02770903.2021.1895213 [DOI] [PubMed] [Google Scholar]
- 41.Cloutier MM. Asthma management programs for primary care providers: increasing adherence to asthma guidelines. Curr Opin Allergy Clin Immunol. 2016;16(2):142–147. doi: 10.1097/ACI.0000000000000242 [DOI] [PubMed] [Google Scholar]
- 42.Federico MJ, McFarlane AE 2nd, Szefler SJ, Abrams EM. The impact of social determinants of health on children with asthma. J Allergy Clin Immunol Pract. 2020;8(6):1808–1814. doi: 10.1016/j.jaip.2020.03.028 [DOI] [PubMed] [Google Scholar]
- 43.Salam T, Duhig A, Patel AA, Cameron A, Voelker J, Bookhart B, Coleman CI. Physicians’ perspectives regarding non-medical switching of prescription medications: results of an internet e-survey. PLoS One. 2020;15(1):e0225867. doi: 10.1371/journal.pone.0225867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bickel S, Morton R, O'Hagan A, Canal C, Sayat J, Eid N. Impact of payor-initiated switching of inhaled corticosteroids on lung function. J Pediatr. 2021;234:128–133 e1. doi: 10.1016/j.jpeds.2021.03.008 [DOI] [PubMed] [Google Scholar]
- 45.Karaca-Mandic P, Jena AB, Joyce GF, Goldman DP. Out-of-pocket medication costs and use of medications and health care services among children with asthma. Jama. 2012;307(12):1284–1291. doi: 10.1001/jama.2012.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kesselheim AS, Avorn J, Sarpatwari A. The high cost of prescription drugs in the United States: origins and prospects for reform. Jama. 2016;316(8):858–871. doi: 10.1001/jama.2016.11237 [DOI] [PubMed] [Google Scholar]
- 47.Drettwan JJ, Kjos AL. An ethical analysis of Pharmacy Benefit Manager (PBM) practices. Pharmacy (Basel). 2019;7(2):65. doi: 10.3390/pharmacy7020065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sadreameli SC, Brigham EP, Patel A. The surprising reintroduction of primatene mist in the United States. Ann Am Thorac Soc. 2019;16(10):1234–1236. doi: 10.1513/AnnalsATS.201902-164HP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Unified Pharmacy Product List Overview. 2021. The prescriber e-letter. Available from: https://www.mass.gov/doc/issue-1-january-2021-0/download. [Google Scholar]
- 50.Myers L, Murray RK. Overcoming health literacy barriers to improve asthma inhaler therapy adherence. Ann Am Thorac Soc. 2019;16(2):182–186. doi: 10.1513/AnnalsATS.201805-338PS [DOI] [PubMed] [Google Scholar]
- 51.Kaplan A, Price D. Matching inhaler devices with patients: the role of the primary care physician. Can Respir J. 2018;2018:9473051. doi: 10.1155/2018/9473051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Welch M, Ludden T, Mottus K, Bray P, Hendrickson L, Rees J, Halladay J, Tapp H. Patient and provider perspectives on uptake of a shared decision making intervention for asthma in primary care practices. J Asthma. 2019;56(5):562–572. doi: 10.1080/02770903.2018.1471703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Perez L, Morales KH, Klusaritz H, Han X, Huang J, Rogers M, Bennett IM, Rand CS, Ndicu G, Apter AJ, et al. A health care navigation tool assesses asthma self-management and health literacy. J Allergy Clin Immunol. 2016;138(6):1593–1599.e3. doi: 10.1016/j.jaci.2016.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fernandez Urrusuno R, Montero Balosa MC, Perez Perez P, Pascual de la Pisa B. Compliance with quality prescribing indicators in terms of their relationship to financial incentives. Eur J Clin Pharmacol. 2013;69(10):1845–1853. doi: 10.1007/s00228-013-1542-4 [DOI] [PubMed] [Google Scholar]
- 55.Parikh K, Perry K, Pantor C, Gardner C. Multidisciplinary engagement increases medications in-hand for patients hospitalized with asthma. Pediatrics. 2019;144(6):e20190674. doi: 10.1542/peds.2019-0674 [DOI] [PubMed] [Google Scholar]
- 56.Patel MR, Coffman JM, Tseng CW, Clark NM, Cabana MD. Physician communication regarding cost when prescribing asthma medication to children. Clin Pediatr (Phila). 2009;48(5):493–498. doi: 10.1177/0009922808330110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Apter AJ, Perez L, Han X, Ndicu G, Localio A, Park H, Mullen AN, Klusaritz H, Rogers M, Cidav Z, et al. Patient advocates for low-income adults with moderate to severe asthma: a randomized clinical trial. J Allergy Clin Immunol Pract. 2020;8(10):3466–3473 e11. doi: 10.1016/j.jaip.2020.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jetty A, Jabbarpour Y, Pollack J, Huerto R, Woo S, Petterson S. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations. J Racial Ethnic Health Disparities. 2022;9(1):68–81. doi: 10.1007/s40615-020-00930-4 [DOI] [PubMed] [Google Scholar]
- 59.Chung EK, Siegel BS, Garg A, Conroy K, Gross RS, Long DA, Lewis G, Osman CJ, Jo Messito M, Wade R, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46(5):135–153. doi: 10.1016/j.cppeds.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]