Abstract
Introduction
For several years, many arthrometers have been developed to assess anterior knee laxity. The aim of our study was to evaluate the validity of a new practical and handy testing device with the hypothesis that the new arthrometer had good validity in terms of reliability and accuracy.
Methods
Lachman test was performed on five fresh frozen cadaveric knees by five examiners. Anterior tibial translation (ATT) was measured with a new arthrometer (BLU-DAT) and on lateral stress radiographs. Data on ATT were obtained under 7 kg (69 N), 9 kg (88 N), and maximum manual traction (MMT). Tests were performed on the same specimens before and after arthroscopic ACL excision. Inter-rater reliability of the BLU-DAT measures was assessed with the intraclass correlation coefficient (ICC) for single and average measurements. The Bland–Altman method was used to estimate agreement between the BLU-DAT and stress radiographs.
Results
ICC values for single measurements were 0.62, 0.54 and 0.58 for 7-kg, 9-kg and MMT assessment, respectively. Overall reliability was good (ICC = 0.63). ICC values for average measurements were 0.89, 0.85 and 0.88 for 7-kg, 9-kg and MMT assessment, respectively. Overall reliability was very good (ICC = 0.90) SEM ranged from 1.4 mm to 1.6 mm for single measurements and was below 1 mm at each testing condition for average measurements. Analysis of agreement between BLU-DAT and radiographic measurements showed a mean difference equal to 0.83 mm ± 2.1 mm (95% CI: 0.55–1.11). Upper LOA was equal to 4.9 mm (95% CI: 5.39–4.41). Lower LOA was equal to − 3.2 mm (95% CI: − 2.71 to − 3.69).
Conclusion
Measurement of anterior knee laxity with the BLU-DAT testing device has a good to very good inter-rater reliability and good agreement with a gold standard such as stress radiographs.
Cadaveric Diagnostic Study, Level of Evidence IV.
Keywords: Knee, Laxity, Anterior cruciate ligament, Anterior tibial translation, Arthrometer
Introduction
The diagnosis of anterior cruciate ligament (ACL) injury is mainly based on clinical examination and confirmed by imaging studies such as magnetic resonance imaging (MRI), which provides valid information on pathoanatomy and has a high correlation with gross pathological findings [1]. However, MRI cannot appraise the functional competence of the ACL.
The Lachman test and the pivot shift test represent the most accurate clinical tests to diagnose an insufficiency of ACL, both in acute and chronic conditions [2–5], albeit its reliability is affected by examiner’s experience and by patient’s compliance as well [4, 6–8].
Quantification of anterior knee laxity has a diagnostic value in case of ACL injury and might help to assess objective outcome of ACL surgery [9–11].
Since the 1980s, several devices named “arthrometers” have been developed to make the knee laxity testing reliable and accurate [12]. However, reliability and diagnostic accuracy of knee arthrometers can be undermined by several factors. Setting-related factors are the knee starting flexion and rotation position [13]. Examiner’s experience, strength, and hand dominance represent the main examiner-related factors [14–16]. Also, patient’s compliance can affect accuracy and reliability of a testing device. Some tools like stress radiographs or radiosterometric analysis (RSA), despite their excellent diagnostic accuracy, are unsuitable for the outpatient setting because of their size or costs [17, 18]. An instrumented laxity testing device should handle all these issues in order to be as accurate and reliable as possible and suitable for every condition of use. Unfortunately, an arthrometer that meet all those features is yet to come. Recently, a new portable testing device (BLU-DAT; FGP srl, Dossobuono, VR, Italy) has been realized for measurement of anterior knee laxity in the clinical setting. The purpose of the present study was to assess validity of this new arthrometer. The hypothesis of the study was that the new arthrometer BLU-DAT has a good validity in terms of reliability and accuracy.
Methods
The study was designed as a reliability study according to guidelines established by the QAREL checklist [19] approved by our university's institutional review board.
Study population
Five fresh-frozen lower limbs (femur cut under trochanteric region) from cadavers were used for the present study. Mean donor age was 52.6 ± 13.8 years (range: 31–66 years).
Presence of degenerative changes of the knee joint was assessed on plain radiographs. Diagnostic arthroscopy was performed at the beginning of the procedure to confirm integrity of the ACL. Specimens with evident signs of knee osteoarthritis (joint space narrowing and presence of marginal osteophytes), ACL injuries and radiographic and/or macroscopic signs of previous surgery (hardware, surgical scars) were excluded from the study.
Description of testing device
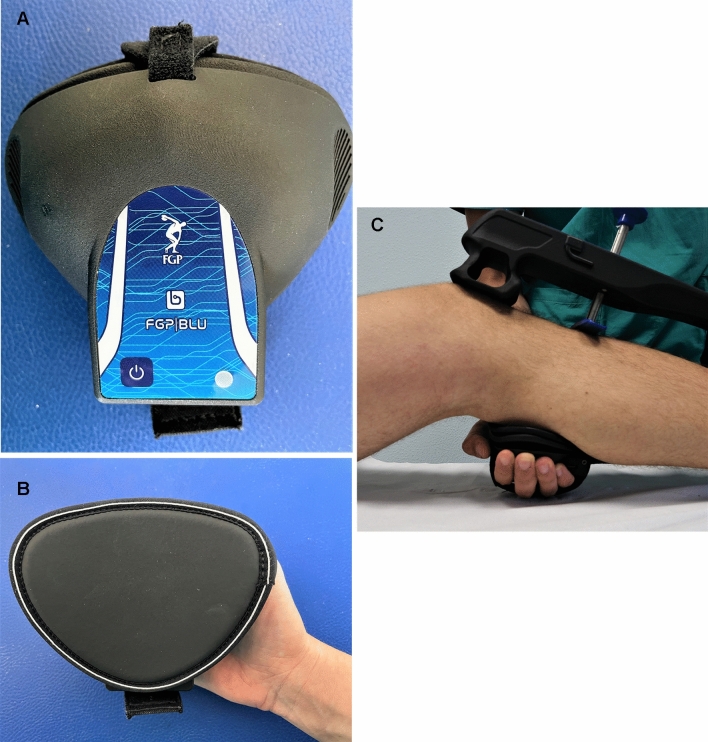
The BLU-DAT testing device is designed to measure anterior (or posterior) translation of the tibia respect to the femur. Displacement on the sagittal plane is measured by mean of a magnetic linear encoder whose mobile part is applied to a sliding rod enveloped in a guide (the probe), whereas the feeler is fixed to the arthrometer body (Fig. 1). Measurement of anterior tibia translation relative to the femur is showed on the device display. The device is also equipped by sensors which evaluate the degree of knee flexion during the test, thus allowing to check the proper knee flexion angle according to the clinical testing (i.e., Lachman test and anterior drawer test) (Fig. 2).
Fig. 1.

The BLU-DAT laxity testing device (A). Displacement on the sagittal plane is measured by a magnetic linear encoder whose mobile part is applied to a sliding rod enveloped in a guiding probe (arrow), which is attached to the body of the arthrometer (B)
Fig. 2.
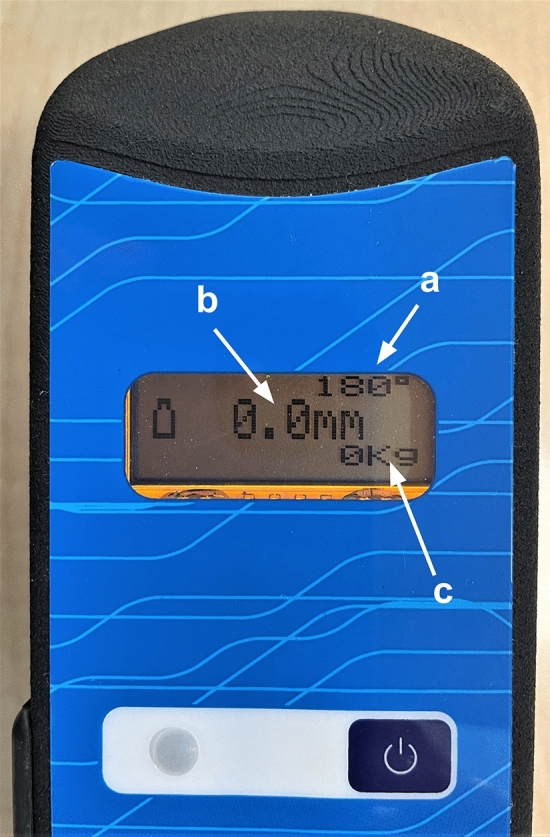
Digital display of the BLU-DAT device. On the display is possible to visualize knee flexion angle (a), where 180° corresponds to the plane parallel to the ground; anterior tibial translation expressed in mm (b); and the force applied expressed in kilograms (c)
The arthrometer has two supports: the proximal one should be placed at the level of the patella, whereas the distal one on the distal tibia. The right location of the device is achieved by making the probe falling approximately on the tibial tubercle (Fig. 3). The system can be connected by Bluetooth to an accessory dynamometer that allows to quantify the applied force (Fig. 4). This extension allows to combine displacement data to the force applied while performing the test. The possibility to track the force applied, as well as the knee flexion angle, help to control two important setting conditions that may influence reliability of the test.
Fig. 3.

The device in position with the upper support (a) positioned on the patella, the probe (b) on the tibial tuberosity, and the lower support (c) at the level of the distal tibia
Fig. 4.
An accessory dynamometer is connected via Bluetooth to the system and allows to quantify the applied force (A, B). The dynamometer is placed on the examiner’s hand that applies anterior traction to the tibia (C)
Intervention
Specimens were thawed overnight at room temperature; then lower limbs were mounted over an operating table. A clamp was used to fix the femur, while the foot was fixed to the table with a belt to avoid leg elevation by anterior traction during testing. Knee flexion was set at 30° and in neutral rotation. Three 1-mm titanium beads were positioned into the meta-epiphysis of both femur and tibia from different entry points with the use of a purposed injector through stab incisions. No soft tissues were removed before testing.
Lachman instrumented tests were conducted by five examiners with different skill level (one expert sports medicine surgeon, one sports medicine fellow and three residents with different progress of their residency program—PGY-1, -3 and -5, respectively). Measures of anterior tibial translation (ATT) were acquired under three different loading conditions: 7 kg (69 N), 9 kg (89 N) and maximum manual traction (MMT). An x-ray image intensifier was used while testing. The c-arm of the mobile x-ray unit was placed across the operating table to obtain a lateral view. Preliminary x-ray was obtained to confirm superimposition of the medial and lateral condyles of the distal femur and correct knee flexion angle. Then lateral x-rays were recorded for each test at resting position (no loading) and at the load peak.
Tests were numbered according to the examiner and loading condition and test sequence was randomized by using a random sequence generator (www. random.org). After testing, each specimen underwent an arthroscopic ACL excision, then tests were repeated according to a new random sequence.
Each examiner performed 30 evaluations by testing every specimen 6 times (with and without ACL under three loading conditions). Examiners were blind to test results of other examiners. Overall, 150 tests were carried out.
Outcome measurements
The primary outcome of the study was the inter-rater reliability of the measures acquired by the five examiners with the BLU-DAT testing device according to different loading conditions. Secondary outcome was the agreement between ATT data obtained with the testing device and those from radiographic images.
Data obtained from manual tests were transmitted via Bluetooth protocol to a PC and acquired by the dedicated BLU-DAT software (FGP). Anterior tibial translation at the force peak under 7 kg, 9 kg and MMT loading conditions were considered. Data were expressed in millimeters (mm).
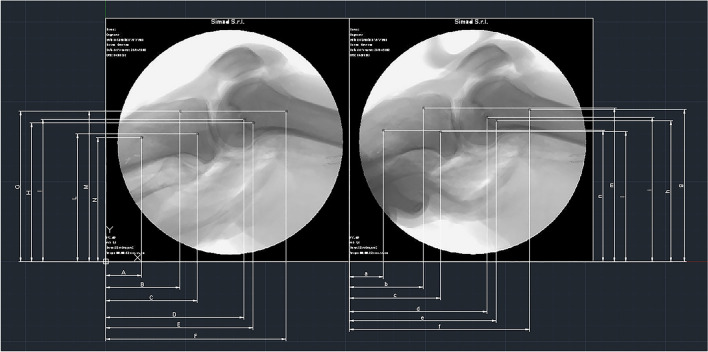
The output radiographs captured using the “HiRes2-XR” X-Ray machine (Kappa Optronics GmbH, Gleichen, Germany) have been exported with the dcm extension. All the collected images were renamed and sorted to match the collection sequence of the BLU-DAT data. Subsequently, the visualization MDICOM software (Kappa Optronics) has been used to convert the renamed files from the dcm to jpg format to allow resizing of the image when needed. All the images were then imported in the Autocad LT 2020 (Autodesk, San Rafael, CA, USA) CAD software to verify that each set had the correct scale; when correct scale was not confirmed, sets were resized using the Faststone photo resizer software (Faststone Soft) based on the known measure of the diameter of the titanium beads used as reference point.
The approach used to obtain the ATT data consisted of tracking the differences between the initial position of the tibia (resting phase, RP) and its final position during the test (loading phase, LP). The procedure was carried out with Autocad LT 2020 software. For each of the 6 titanium beads identified within the radiograph an X and Y coordinate has been identified and the mean of the X and Y components of the three titanium beads cluster of the tibia and femur was calculated in order to obtain the exact difference (delta, Δ) of the tibial and femoral position between the RP and the LP (Fig. 5).
Fig. 5.
Example of the method used to obtain objective ATT data by stress radiographs, by tracking the differences between the initial position of the tibia (resting phase, RP) and its final position during testing (loading phase, LP). For each of the 6 titanium spheres identified within the radiograph, an X- and Y-coordinate was identified and the X- and Y-components of the cluster of 3 titanium spheres of the tibia and femur were averaged to obtain the exact difference (delta, Δ) of tibial and femoral position between the RP and LP
Then the relative final displacement (RFD) of the tibia respect to the femur was calculated to eliminate any possible error due to femoral movement during the test as follows:
The RFD module was obtained by calculating the resultant of the X and Y components of displacement previously obtained:
The differences between the RP and the LP was expressed in mm.
Data analysis
Data were analyzed with statistical software (IBM SPSS Statistics 25; IBM, Armonk, NY, USA). Normal data distribution was assessed by Kolmogorov–Smirnov test. Descriptive statistics for continuous variables were reported as means and standard deviations. Comparison between raters for ATT measurement at different loading conditions was accomplished by one-way ANOVA. Student’s t test was used to compare normal and ACL-deficient knees for ATT measurement at different loading conditions. We analyzed the inter-rater reliability by calculating intraclass correlation coefficient (ICC) using a two-way random effect model and evaluation of absolute agreement. Inter-rater reliability was assessed with the ICC forms for single (2,1) and average (2,k) measurements. Confidence intervals were calculated at 95% confidence level for reliability coefficients. Additionally, from the ICC obtained and the standard deviation of the scores from all subjects, we established the precision by calculating the standard error of measurement (SEM) between observations [20]. ICC values ranged from 0 to 1, with 1 indicating perfect reliability, and they were interpreted as follows: < 0 as absent (complete discordance between observations), 0–0.20 as poor, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as good and 0.81–1 as very good [21].
Data obtained from all measurements were pooled and used for analysis of agreement between the two modalities for measurement of anterior tibial translation (testing device and radiographic images). The Bland–Altman method was used to assess agreement between the two measurements for the quantification of ATT [22]. According to this method, difference and mean of the measures obtained from the two measurements were calculated for every laxity test performed [23]. Bland–Altman method was applied by calculating difference of BLU-DAT measure—stress x-ray measure. Agreement was expressed as mean (d) and standard deviation (s) of the differences. Data were reported in a scatter plot of differences (y-axis) against means (x-axis), where upper and lower limits of agreement (LOA) were considered as d ± 2 s. Ninety-five percent confidence intervals (95% CIs) were calculated for mean difference and estimated LOAs.
Sample size calculation
Sample size was based on the primary outcome of the study (inter-rater reliability) and established in accordance with estimates provided by Walter et al. [24] for reliability studies using ICCs. A reliability hypothesis at a 5% significance level and a power of 80% (β = 0.20) requires a minimum sample of 29 to test inter-rater reliability based on five observers for a criterion coefficient value of 0.5 and a true value of 0.7.
Results
Comparison between raters for ATT measurement revealed no significant differences between raters at every testing condition (Table 1). Difference in average ATT between normal knees and after ACL cut was significant for every loading condition and at overall evaluation (Table 2).
Table 1.
Comparison between raters for ATT measurement at different loading conditions
| Rater | ATT | |||||
|---|---|---|---|---|---|---|
| 7 kg | p | 9 kg | p | MMT | p | |
| 1 | 2.5 ± 1.2 | 0.295 | 3.5 ± 1.5 | 0.385 | 4.8 ± 2.5 | 0.131 |
| 2 | 3.3 ± 2.1 | 4.1 ± 1.8 | 5.6 ± 2.3 | |||
| 3 | 3.1 ± 1.6 | 4.3 ± 2 | 6.2 ± 2.8 | |||
| 4 | 3.6 ± 1.8 | 4.7 ± 2.3 | 6.2 ± 3.3 | |||
| 5 | 2.1 ± 1.6 | 3.1 ± 2 | 3.5 ± 1.9 | |||
| Overall | 2.9 ± 1.7 | 3.9 ± 2 | 5.2 ± 2.7 | |||
Table 2.
Comparison between normal and ACL-deficient knees for ATT measurement at different loading conditions
| ACL | ATT | |||||
|---|---|---|---|---|---|---|
| 7 kg | p | 9 kg | p | MMT | p | |
| Normal | 1.8 ± 0.9 | < .0001 | 2.7 ± 1.7 | < .0001 | 3.7 ± 2.3 | < .0001 |
| Cut | 4 ± 1.6 | 5.1 ± 1.4 | 6.8 ± 2.2 | |||
ICC for single measurements revealed good inter-rater reliability for 7-kg and moderate for 9-kg and MMT assessment. SEM ranged from 1.4 mm to 1.6 mm. Overall, reliability was good. Inter-rater reliability for average measurements was very good for every loading condition and for overall estimate. SEM was below 1 mm for each testing condition (Table 3).
Table 3.
Reliability analysis for ATT measurement at different loading conditions
| Load | Single measurement | Average measurement | ||||||
|---|---|---|---|---|---|---|---|---|
| ICC | 95% CI | SEM | ICC | 95% CI | SEM | |||
| Lower | Upper | Lower | Upper | |||||
| 7 kg | 0.62 | 0.35 | 0.86 | 1.4 | 0.89 | 0.73 | 0.97 | 0.7 |
| 9 kg | 0.54 | 0.27 | 0.82 | 1.6 | 0.85 | 0.65 | 0.96 | 0.8 |
| MMT | 0.58 | 0.30 | 0.84 | 1.5 | 0.88 | 0.68 | 0.96 | 0.9 |
| Overall | 0.63 | 0.45 | 0.78 | 1.4 | 0.90 | 0.81 | 0.95 | 0.8 |
Analysis of agreement between BLU-DAT and radiographic measurements showed a mean difference equal to 0.83 mm ± 2.1 mm (95% CI: 0.55–1.11). Upper LOA was equal to 4.9 mm (95% CI: 5.39–4.41). Lower LOA was equal to − 3.2 mm (95% CI: − 2.71 to − 3.69) (Fig. 6).
Fig. 6.
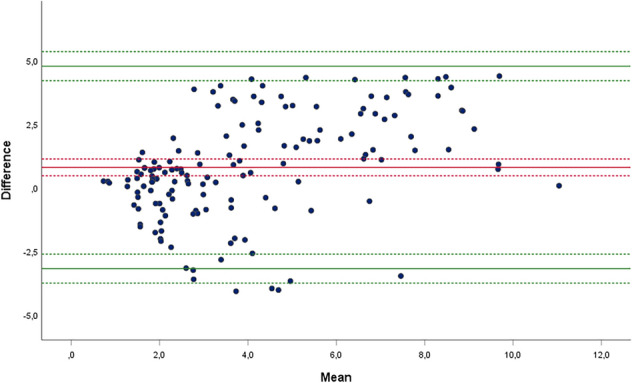
Bland–Altman scatter plot of differences against mean measures of anterior tibial translation (ATT) obtained with BLU-DAT and those obtained on stress radiographs. Difference was calculated as BLU-DAT measure—stress x-ray measure. Measures of ATT are expressed in millimeters. The middle (red) line represents the mean difference, and the top and bottom (green) lines represent the limits of agreement (LOA) between the two methods of measurements. Dotted lines represent 95% Cis around mean difference (red dotted line) and around upper and lower LOA (green dotted lines), respectively
Discussion
The most relevant finding of the present study is that reliability of the BLU-DAT testing device in measuring ATT was moderate to good and very good for single and average measurement, respectively. Precision of measurement (SEM) was within 1 mm for average measurements.
In recent decades, several instruments have been developed to quantify ATT. The KT-1000 arthrometer (Medmetric, San Diego, CA, USA) is the hallmark of these tools [12], and most of the new arthrometers have been validated by comparison with the KT-1000 [25–30]. However, reliability of KT-1000 is inconsistently reported in the literature, starting from good and excellent results in older studies [31], to more recent studies that showed lower ICCs, thus definitely downgrading the inter-rater reliability of the KT-1000 [32, 33]. We recall that the KT-1000 has been validated as a diagnostic tool for ACL injuries, hence the output of KT-1000 has been handled as binary or ordinal variable [34]. Conversely, in the present study, reliability of the BLU-DAT testing device was assessed by measuring ATT as continuous variable. Loading conditions were chosen to approximate standard experimental settings (15 lbs, 20 lbs and MMT) to test KT-1000, as reported in previous studies [34–38]. As variability was supposed to be related more to raters than to samples, we attempted to create the worst scenario for assessing reliability by increasing the number of raters (five) with different skills rather than by increasing the number of specimens. What is more, tests could not affect integrity of the specimens, and therefore they were tested several times with no risk of assessment bias due to changes in their mechanical properties. Different raters provided similar mean values for ATT regardless of their skill level and of loading conditions, and this was confirmed at reliability analysis. According to difference in ICC values for single and average measurements observed in the present study, in order to optimize reliability of the instrument, we suggest repeating measurement of ATT three times and calculating average measurement, as recommended for other knee arthrometers [39].
The second aim of this study was to evaluate accuracy of BLU-DAT in measuring ATT by comparison with a gold standard. In the present study, no direct comparison to another established arthrometer (eg. KT1000 or Rolimeter) was accomplished. However, as validity and reliability of other devices are still debated [39], no gold standard has been established to be used for comparison, hence fluoroscopic assessment was considered as the most valid reference standard to estimate real ATT.
Most of previous studies attempted to validate knee laxity testing devices using the correlation coefficient (r) as measurement of accuracy. However, correlation studies investigate the relationship between one variable and another, not the differences, and therefore this approach is not recommended as a method for assessing the comparability between methods [40]. The Bland–Altman method used in the present study allows to estimate how much two methods evaluating the same measure differ from each other by calculating the mean difference and the limits of agreement between them [22].
Results of our study confirmed that BLU-DAT has a good agreement with stress radiographs in measuring ATT, with a mean difference between the two measurements being less than one millimeter and LOAs, which represent extreme clinical scenarios, ranging from 4.9 mm to − 3.2 mm.
Bland–Altman method was applied by calculating difference of BLU-DAT measure—stress x-ray measure. As mean difference and 95%CI showed positive results and upper LOA was greater than lower one, we can argue that BLU-DAT has tendency toward overestimation of ATT, albeit within acceptable values. Moreover, by looking at the scatter plot (Fig. 6) we can observe that most of the values of mean difference approximating LOAs are for average ATT exceeding 3 mm, which is considered a threshold for diagnosing an ACL injury [41]. This means that overestimation of anterior knee laxity can occur for greater values of ATT, where diagnosis of ACL injury is already established.
Indeed, some authors evaluated the agreement between knee laxity testing devices and radiological measures [35]. Jorn et al. [42] measured anterior knee laxity in 12 patients after ACL reconstruction using the Stryker laxity tester (Stryker, (Kalamazoo, MI, USA) and RSA simultaneously, with loads of 90 N and 180 N. The mean difference between the two methods was 4.4 mm at 90 N and 8.0 mm at 180 N. The LOA between the two devices were − 1 to + 10 mm at 90 N, and 0 to 16 mm at 180 N, demonstrating a low level of agreement. Shino et al. [41]hypothesized that the lack of agreement between arthrometers and radiological techniques could be due to deformation of the surrounding soft tissues, which affects external device measurements and not the radiological ones.
Although mean difference in ATT between instrumented laxity tests and stress radiographs observed in the present study (less than 1 mm) was much smaller than previously reported [41, 42], some concerns exist about accuracy of BLU-DAT as LOA exceed acceptable values (3 mm-difference). Surely, measurement of ATT by side-to-side difference, as recommended for other arthrometers, might minimize the risk of assessment bias [41]. Unfortunately, due to nature of the present study, performed on single legs, no side-to-side difference could be assessed. Nevertheless, two different laxity conditions were tested for each specimen (intact and torn ACL), which approximated an experimental setting suitable for comparison between injured and contralateral healthy knee. Analysis of ATT before and after ACL cut showed significant difference for every loading condition and at overall evaluation. This means that the device is responsive to change in ATT due to ACL tear, thus confirming its diagnostic accuracy. In support of data obtained in the present study, and for a definitive validation of the instrument, further in vivo studies will certainly be needed to evaluate its reliability and diagnostic accuracy in the clinical setting by side-to-side comparison, as reported in validation studies of other external ATT measurement devices [39].
Finally, we want to focus on manageability of BLU-DAT, given its small size, which makes it an excellent tool for the outpatient setting, overcoming one of the major limitations of other instruments like GNRB, PKTD, and KT-1000 itself. In addition, the optional ability of the instrument to accurately measure force and flexion angle during the examination is crucial to control two of the major setting-related and examiner-related potential confounders.
The present study has some limitations. First, the experiment was conducted on cadaver specimens, making it impossible to test some factors that could have affected the reliability of the new arthrometer in vivo, such as patient compliance and hamstring contraction. Second, accuracy of knee flexion angle was not assessed, nor the exact initial tibial rotation was measured. Finally, no intra-rater reliability was tested.
Conclusions
Measurement of anterior knee laxity with the BLU-DAT testing device has a good to very good inter-rater reliability and good agreement with a gold standard such as stress radiographs.
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement. FGP srl has donated 2 arthrometers to the University of Brescia for research. The authors declare that no funds were received during the preparation of this manuscript.
Declarations
Conflict of interest
Giuseppe Milano has a potential conflict of interest in that he received, as scientific referent, the materials for the research from FGP srl. Andrea Raggi and Fabio Zanoni have a potential conflict of interest as FGP srl employees. The other authors have no potential conflict of interest.
Ethical approval
The study was approved by the institutional review board at the University of Brescia, Italy.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Giuseppe Milano, Email: giuseppe.milano@unibs.it.
Alessandro Colosio, Email: alessandro.colosio09813@gmail.com.
Alessandra Scaini, Email: alescaini@yahoo.it.
Marcello Motta, Email: marcello.motta1991@gmail.com.
Andrea Raggi, Email: andrea@fgpsrl.it.
Fabio Zanoni, Email: fabio@fgpsrl.it.
Stefano Galli, Email: elaste@libero.it.
Maristella F. Saccomanno, Email: maristellasaccomanno@hotmail.it
References
- 1.Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 2.Cooperman JM, Riddle DL, Rothstein JM. Reliability and validity of judgments of the integrity of the anterior cruciate ligament of the knee using the Lachman’s Test. Phys Ther. 1990;70:225–233. doi: 10.1093/ptj/70.4.225. [DOI] [PubMed] [Google Scholar]
- 3.Torg JS, Conrad W, Kalen V. Clinical I diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 4.Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36:267–288. doi: 10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 5.Hoshino Y, Kuroda R, Nagamune K, et al. In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med. 2007;35:1098–1104. doi: 10.1177/0363546507299447. [DOI] [PubMed] [Google Scholar]
- 6.Noyes FR, Cummings JF, Grood ES, et al. The diagnosis of knee motion limits, subluxations, and ligament injury. Am J Sports Med. 1991;19:163–171. doi: 10.1177/036354659101900212. [DOI] [PubMed] [Google Scholar]
- 7.Kuroda R, Hoshino Y, Kubo S, et al. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency: a global survey and kinematics assessment. Am J Sports Med. 2012;40:91–99. doi: 10.1177/0363546511423634. [DOI] [PubMed] [Google Scholar]
- 8.Musahl V, Hoshino Y, Ahlden M, et al. The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc. 2012;20:724–731. doi: 10.1007/s00167-011-1859-4. [DOI] [PubMed] [Google Scholar]
- 9.Chiang E-R, Chen K-H, Chih-Chang Lin A, et al. Comparison of tunnel enlargement and clinical outcome between bioabsorbable interference screws and cortical button-post fixation in arthroscopic double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study with a minimum follow. Arthrosc J Arthrosc Relat Surg. 2019;35:544–551. doi: 10.1016/j.arthro.2018.08.039. [DOI] [PubMed] [Google Scholar]
- 10.Wang H-D, Gao S-J, Zhang Y-Z. Comparison of clinical outcomes after anterior cruciate ligament reconstruction using a hybrid graft versus a hamstring autograft. Arthrosc J Arthrosc Relat Surg. 2018;34:1508–1516. doi: 10.1016/j.arthro.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 11.Svantesson E, Hamrin Senorski E, Webster KE, et al. Clinical outcomes after anterior cruciate ligament injury: panther symposium ACL injury clinical outcomes consensus group. Knee Surg Sports Traumatol Arthrosc. 2020;28:2415–2434. doi: 10.1007/s00167-020-06061-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniel DM, Lou SM, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13:401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 13.Fiebert I, Gresley J, Hoffman S, Kunkel K. Comparative measurements of anterior tibial translation using the KT-1000 knee arthrometer with the leg in neutral, internal rotation, and external rotation. J Orthop Sports Phys Ther. 1994;19:331–334. doi: 10.2519/jospt.1994.19.6.331. [DOI] [PubMed] [Google Scholar]
- 14.Ballantyne BT, French AK, Heimsoth SL, et al. Influence of examiner experience and gender on interrater reliability of KT-1000 arthrometer measurements. Phys Ther. 1995;75:898–906. doi: 10.1093/ptj/75.10.898. [DOI] [PubMed] [Google Scholar]
- 15.Berry J, Kramer K, Binkley J, et al. Error estimates in novice and expert raters for the KT-1000 arthrometer. J Orthop Sports Phys Ther. 1999;29:49–55. doi: 10.2519/jospt.1999.29.1.49. [DOI] [PubMed] [Google Scholar]
- 16.Sernert N, Helmers J, Kartus C, et al. Knee-laxity measurements examined by a left-hand- and a right-hand-dominant physiotherapist, in patients with anterior cruciate ligament injuries and healthy controls. Knee Surg Sports Traumatol Arthrosc. 2007;15:1181–1186. doi: 10.1007/s00167-007-0347-3. [DOI] [PubMed] [Google Scholar]
- 17.Isberg J, Faxèn E, Brandsson S, et al. KT-1000 records smaller side-to-side differences than radiostereometric analysis before and after an ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:529–535. doi: 10.1007/s00167-006-0061-6. [DOI] [PubMed] [Google Scholar]
- 18.Khan R, Konyves A, Rama KRBS, et al. RSA can measure ACL graft stretching and migration. Clin Orthop. 2006;448:139–145. doi: 10.1097/01.blo.0000224016.42669.17. [DOI] [PubMed] [Google Scholar]
- 19.Lucas NP, Macaskill P, Irwig L, Bogduk N. The development of a quality appraisal tool for studies of diagnostic reliability (QAREL) J Clin Epidemiol. 2010;63:854–861. doi: 10.1016/j.jclinepi.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. doi: 10.1519/15184.1. [DOI] [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 22.Martin Bland J, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. The Lancet. 1986;327:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 23.Hamilton C, Stamey J. Using Bland−Altman to assess agreement between two medical devices – don’t forget the confidence intervals! J Clin Monit Comput. 2007;21:331–333. doi: 10.1007/s10877-007-9092-x. [DOI] [PubMed] [Google Scholar]
- 24.Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17:101–110. doi: 10.1002/(sici)1097-0258(19980115)17:1<101::aid-sim727>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 25.Balasch H, Schiller M, Friebel H, Hoffmann F. Evaluation of anterior knee joint instability with the Rolimeter. Knee Surg Sports Traumatol Arthrosc. 1999;7:204–208. doi: 10.1007/s001670050149. [DOI] [PubMed] [Google Scholar]
- 26.Ganko A, Engebretsen L, Ozer H. The Rolimeter: a new arthrometer compared with the KT-1000. Knee Surg Sports Traumatol Arthrosc. 2000;8:36–39. doi: 10.1007/s001670050008. [DOI] [PubMed] [Google Scholar]
- 27.Ferretti A, Andrea F, Valeo L, et al. Smartphone versus knee ligament arthrometer when size does not matter. Int Orthop. 2014;38:2197–2199. doi: 10.1007/s00264-014-2432-9. [DOI] [PubMed] [Google Scholar]
- 28.Robert H, Nouveau S, Gageot S, Gagnière B. A new knee arthrometer, the GNRB®: experience in ACL complete and partial tears. Orthop Traumatol Surg Res. 2009;95:171–176. doi: 10.1016/j.otsr.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Collette M, Courville J, Forton M, Gagnière B. Objective evaluation of anterior knee laxity; comparison of the KT-1000 and GNRB® arthrometers. Knee Surg Sports Traumatol Arthrosc. 2012;20:2233–2238. doi: 10.1007/s00167-011-1869-2. [DOI] [PubMed] [Google Scholar]
- 30.Espregueira-Mendes J, Pereira H, Sevivas N, et al. Assessment of rotatory laxity in anterior cruciate ligament-deficient knees using magnetic resonance imaging with Porto-knee testing device. Knee Surg Sports Traumatol Arthrosc. 2012;20:671–678. doi: 10.1007/s00167-012-1914-9. [DOI] [PubMed] [Google Scholar]
- 31.Hanten WP, Pace MB. Reliability of measuring anterior laxity of the knee joint using a knee ligament arthrometer. Phys Ther. 1987;67:357–359. doi: 10.1093/ptj/67.3.357. [DOI] [PubMed] [Google Scholar]
- 32.Wiertsema SH, van Hooff HJA, Migchelsen LAA, Steultjens MPM. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008;15:107–110. doi: 10.1016/j.knee.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Sernert N, Kartus J, Köhler K, et al. Evaluation of the reproducibility of the KT-1000 arthrometer. Scand J Med Sci Sports. 2001;11:120–125. doi: 10.1034/j.1600-0838.2001.011002120.x. [DOI] [PubMed] [Google Scholar]
- 34.Arneja S, Leith J. Review article: validity of the KT-1000 knee ligament arthrometer. J Orthop Surg. 2009;17:77–79. doi: 10.1177/230949900901700117. [DOI] [PubMed] [Google Scholar]
- 35.Lerat JL, Moyen B, Jenny JY, Perrier JP. A comparison of pre-operative evaluation of anterior knee laxity by dynamic X-rays and by the arthrometer KT 1000. Knee Surg Sports Traumatol Arthrosc. 1993;1:54–59. doi: 10.1007/bf01552160. [DOI] [PubMed] [Google Scholar]
- 36.Anderson AF, Snyder RB, Federspiel CF, Lipscomb AB. Instrumented evaluation of knee laxity: a comparison of five arthrometers. Am J Sports Med. 1992;20:135–140. doi: 10.1177/036354659202000207. [DOI] [PubMed] [Google Scholar]
- 37.Kilinc BE, Kara A, Celik H, et al. Evaluation of the accuracy of Lachman and Anterior Drawer Tests with KT1000 ın the follow-up of anterior cruciate ligament surgery. J Exerc Rehabil. 2016;12:363–367. doi: 10.12965//jer.1632622.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paine R, Lowe W. Comparison of Kneelax and KT-1000 knee ligament arthrometers. J Knee Surg. 2012;25:151–154. doi: 10.1055/s-0032-1313916. [DOI] [PubMed] [Google Scholar]
- 39.Runer A, di Sarsina TR, Starke V, et al. The evaluation of Rolimeter, KLT, KiRA and KT-1000 arthrometer in healthy individuals shows acceptable intra-rater but poor inter-rater reliability in the measurement of anterior tibial knee translation. Knee Surg Sports Traumatol Arthrosc. 2021 doi: 10.1007/s00167-021-06540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giavarina D. Understanding Bland Altman analysis. Biochem Medica. 2015;25:141–151. doi: 10.11613/BM.2015.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shino K, Inoue M, Horibe S, et al. Measurement of anterior instability of the knee. A new apparatus for clinical testing. J Bone Joint Surg Br. 1987;69-B:608–613. doi: 10.1302/0301-620x.69b4.3611167. [DOI] [PubMed] [Google Scholar]
- 42.Jorn LP, Fridén T, Ryd L, Lindstrand A. Simultaneous measurements of sagittal knee laxity with an external device and radiostereometric analysis. J Bone Joint Surg Br. 1998;80-B:169–172. doi: 10.1302/0301-620x.80b1.0800169. [DOI] [PubMed] [Google Scholar]