Abstract
Pre-exposure prophylaxis (PrEP) is a highly effective daily pill that decreases the likelihood of HIV acquisition by up to 92% among individuals at risk for HIV. PrEP can be discretely used, autonomously controlled, and in place at the time of risk exposure, making it an especially promising method for HIV prevention for cisgender women (CGW). But, PrEP is underutilized by CGW relative to the demonstrable need. We apply the Integrative Model of Behavioral Prediction to identify the critical psychosocial factors that shape CGW’s intentions to use PrEP and their relevant underlying beliefs. We surveyed (N = 294) community- and clinic-recruited PrEP eligible CGW to understand the relative importance of attitudes, norms, and efficacy in shaping PrEP intentions. We utilized structural equation modeling to identify the relevant paths. We inspected the summary statistics in relation to three message three selection criteria. We identified beliefs that demonstrated (1) an association with intention, (2) substantial room to move the population, (3) practicality as a target for change through communication intervention. Results show that PrEP awareness was low. When women learned about PrEP, they voiced positive intentions to use it. There were significant and positive direct effects of SE (0.316***), attitudes (0.201**), and subjective norms (0.249***) on intention to initiate PrEP. We illustrate the strategic identification of beliefs within the relevant paths using the 3 belief selection criteria. We also discuss implications for social and structural communication interventions to support women’s HIV prevention.
Tenofovir disoproxil fumarate (TDF) plus emtricitabine (FTC) is a highly effective HIV pre-exposure prophylaxis (PrEP) medication (e.g., daily pill) that decreases the likelihood of HIV acquisition by up to 92% among individuals at risk for HIV through heterosexual sex, including cisgender women (CGW) (Baeten et al., 2012; Thigpen et al., 2012). As heterosexual contact is the leading route of HIV transmission among women (Centers for Disease Control and Prevention [CDC], 2018), gender-related factors such as relationship power imbalances and sexual scripts (Amaro & Raj, 2000; Amaro et al., 2001; Amaro, 1995; Pulerwitz et al., 2002) present significant challenges to condom use and therefore to HIV prevention for women (Adimora et al., 2013; Bowleg et al., 2004; Bowleg, 2004; Khan et al., 2011). PrEP can be discretely used, autonomously controlled, and in place at the time of risk exposure, making it an especially promising method for HIV prevention. PrEP is underutilized by CGW relative to the demonstrable need (Siegler et al., 2018), however. In 2015, the CDC estimated that 176,670 US CGW would benefit from PrEP for HIV prevention. Among them, only 3,400 had initiated PrEP use – translating to 98% unmet need for HIV prevention (Smith et al., 2018). Along the same lines, the PrEP to need ratio, or the number of PrEP users in a population divided by the number of new HIV infections in that group, was 2.1 for men, but only 0.4 for CGW in 2017 (Siegler et al., 2018).
Sex and gender disparities in PrEP uptake are exacerbated by racial disparities; PrEP uptake among Black women lags far behind other racial groups (Smith et al., 2018). Though Black women represent most HIV diagnoses among CGW (Centers for Disease Control and Prevention [CDC], 2016), White women are significantly more likely to uptake PrEP (Bush et al., 2016). Between 2014 to 2017, Black women comprised only 33% of CGW who initiated PrEP nationally; in contrast, they represented the majority (59%) of new HIV diagnoses among US women in 2017 (Huang et al., 2018). Black CGW are underserved by HIV prevention and PrEP services, evidenced by the disparity between diffusion of PrEP uptake and the distribution of HIV infection among CGW.
When Black women who are at risk for HIV learn about PrEP, they are excited about it and voice willingness to use it (Goparaju et al., 2015). However, awareness of PrEP among women remains low (Auerbach et al., 2015; Bogorodskaya et al., 2020; Calabrese et al., 2019; Elion & Coleman, 2016; Flash et al., 2014; Goparaju et al., 2017; Ojikutu et al., 2018; Wingood et al., 2013). There is a dire need to increase PrEP awareness, a critical antecedent to uptake, in communities disproportionately impacted by HIV and underserved with respect to PrEP, specifically. However, raising awareness is only an initial step (Aaron et al., 2018; Auerbach & Hoppe, 2015; Flash et al., 2017). Successful intervention activities to increase PrEP utilization will necessarily include communications components to raise awareness of and knowledge about PrEP, promote uptake, and support adherence and retention. These strategic communication efforts are more likely to be successful insofar as they are informed by formative research that identifies the relevant psychosocial factors at play and applies theory to articulate the ways those factors work in concert to shape behavior (Atkin & Rice, 2013; LaCroix et al., 2014; Noar et al., 2009; Noar, 2006, 2008; Snyder & Hamilton, 2002; Snyder, 2007).
Existing research, which identifies factors that are relevant to Black CGW’s PrEP use, provides important formative empirical knowledge regarding which factors are relevant. Existing research, however, does not offer a theoretically grounded understanding of their relative importance or how those factors relate to one another to shape uptake. While understanding which factors shape intentions is a critical initial step, it is also necessary to move beyond identifying the relevant psychosocial factors to understanding how these factors exert their impact.
The purpose of this study was to apply theory to understand the relative importance of relevant psychosocial factors that shape CGW’s decision to use PrEP. Specifically, we apply the Integrative Model of Behavioral Prediction (Fishbein, 2000) to identify the psychosocial factors that shape CGW’s intentions to use PrEP (Fishbein & Ajzen, 2010). In doing so, we aim to inform theoretically grounded communication efforts to increase PrEP awareness and uptake among CGW with elevated HIV risk.
Focus groups (Auerbach et al., 2015; Garfinkel et al., 2017; Goparaju et al., 2017; Smith et al., 2012) and survey research (Ojikutu et al., 2018; Scott et al., 2021; Wingood et al., 2013) demonstrate that attitudes, injunctive and descriptive norms, and self-efficacy (SE) are important factors shaping PrEP uptake intentions among Black women. For example, qualitative and quantitative research has consistently shown that beliefs about drug effectiveness, side-effects (i.e., attitudes), perceptions of peer, partner, provider support (i.e., norms), and self-efficacy to manage side effects are critical to CGW’s consideration of PrEP for HIV prevention.
Existing literature also suggests important differences among CGW in perceptions of norms and the importance of normative factors. For example, in a national survey of unmarried Black (N = 1,042) and White women (N = 411) aged 20–44 years by Wingood et al. (2013), willingness to use PrEP was high among Black women (69%) and White women (54%). Women would also be more likely to use PrEP if it was recommended by a healthcare provider (i.e., injunctive norms) and if they anticipated that their peers would use PrEP (i.e., descriptive norms). In that study, Black women voiced more willingness to use PrEP relative to their White counterparts, particularly if it was recommended by a healthcare provider and supported by peer norms. This evidence suggests that although uptake has been low, particularly among eligible Black women, CGW’s willingness to use PrEP may be relatively high and susceptible to normative influence. However, published literature currently fails to offer a theoretically grounded analysis of the relative weight of normative factors compared to other psychosocial influences.
Integrative model of behavioral prediction
The Integrative Model of Behavioral Prediction (Fishbein, 2000, 2009) asserts that for behaviors under individuals’ control, the most proximal determinant of behavior is the intention to enact the behavior; individuals who intend to enact a behavior are likely to do so, assuming that they are capable and environmental constraints are not excessive (Figure 1). Behavioral intentions are determined by global attitudinal assessments, normative perceptions, and perceptions of behavioral control. At the global level, attitudes are favorability toward the behavior. Normative perceptions are the general sense that the behavior is (or is not) acceptable to important social referents (i.e., injunctive norms) and that similar others engage in the behavior (i.e., descriptive norms). Also, at the global level, self-efficacy refers to perceptions of agency.
Figure 1.
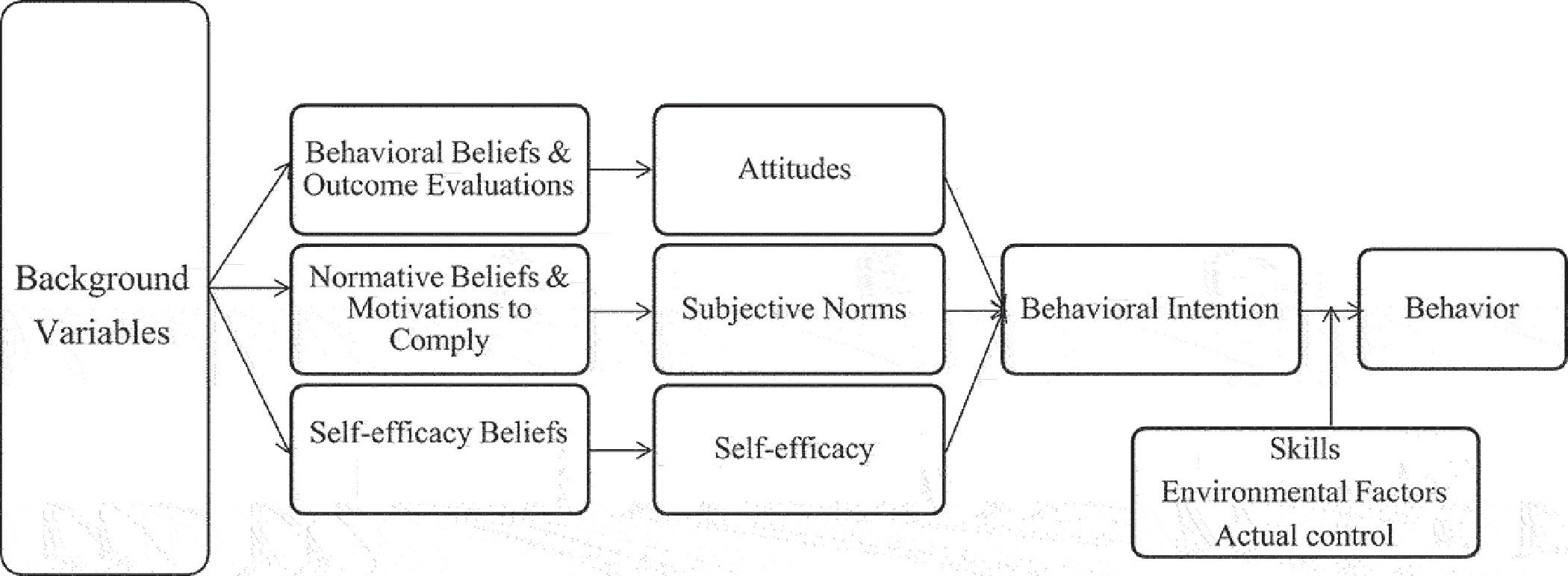
Integrative model of behavioral prediction.
Global assessments are determined by beliefs. Attitudes are determined by behavioral beliefs and their valence. For example, the behavioral belief “if I use PrEP, I will be protected from HIV” may positively influence behavioral intentions because protection from HIV is a positive outcome. Subjective norms are determined by beliefs about specific normative referents and the motivation to comply with them. People look to specific others with whom they are motivated to comply when determining what both is behaviorally acceptable and common. Perceptions of behavioral control are determined by underlying beliefs about ones’ ability to overcome specific barriers that are likely to be present (Fishbein & Ajzen, 2010). Other variables, such as age, education, and socio-economic status, are considered “background variables,” which are posited to affect behavior indirectly by shaping the beliefs people endorse. Background variables may also intervene in the relationship between intentions and behaviors to thwart or bolster acting on intentions. There are critical social and structural determinants that impact HIV prevention behavior (Adimora & Schoenbach, 2002; Amaro, 1995; Auerbach & Hoppe, 2015; Wingood & DiClemente, 2000). These factors are considered environmental constraints that may bolster or thwart action. Finally, behavioral accomplishment may depend on particular skills, and the extent to which enactment is actually under volitional control.
The IMBP provides prescription for identifying the relative importance of psychosocial paths that determine the behavior and identifying relevant underlying beliefs that determine behavioral intentions (Yzer, 2017). Application of the model in the formative stages of program of intervention development facilitates identification of the topics communication activities should cover (Cappella et al., 2001; Fishbein & Yzer, 2003). Thus, the IMBP provides a framework for identifying communication strategies that address the most pertinent beliefs within the most important paths to intention (i.e., attitudes, subjective norms, SE).
The IMBP and its theoretical predecessors have been widely supported and used in the development and evaluation of an expansive range of behavioral and public health communication interventions, including those focused on HIV prevention (Albarracin et al., 2001; Fishbein et al., 2001, 2001; Fishbein, 2000; Hull et al., 2011; Jemmott et al., 1998, 2005). Meta-analytic evidence has also shown support for the model across behaviors that include smoking cessation, driving, cancer screening, exercise, oral hygiene, and condom use (Armitage & Conner, 2001; Godin & Kok, 1996; McEachan et al., 2016). In this body of evidence, the IMBP accounts for a considerable amount of variance in behavioral outcomes (19% – 32%) and intentions (40% – 58%) (McEachan et al., 2011, 2016).
Given that PrEP initiation and persistence require considerable individual commitment, we utilize the IMBP to understand the psychosocial factors which shape decisions around PrEP. To this end, we designed a cross-sectional study of CGW in a high HIV prevalence community. We proposed two exploratory, theoretically grounded (Bleakley & Hennessy, 2012) research questions (RQ): RQ1) what is the relative importance of the psychosocial paths that shape PrEP intention? RQ2) given the significant paths, which specific beliefs shape the relevant determinants of intention?
Method
Study setting
The District of Columbia is an epicenter of the HIV epidemic in the US, with over 13,000 residents with HIV and an alarmingly high prevalence of 1.9% among African American CGW. In 2016, Black CGW comprised 49% of the CGW population in DC, but represented more than 90% of CGW living with HIV (HAHSTA, 2020). Washington, DC is one of the 48 US counties with the highest HIV incidence (United States Department of Health and Human Services, 2019). In DC, health insurance coverage is 94% (HAHSTA, 2017), and the DC Department of Health (DC Health) offers the PrEP Drug Assistance Program for insured and uninsured residents. Through DC Health and other community clinics, uninsured and underinsured individuals can also obtain a same-day10-day initial supply of PrEP and continued medication free of cost.
Participants and procedure
We collected data from a community-based sample (n = 190) and a tertiary care hospital clinic-based sample (n = 104) (N = 294). For the community-based sample, respondents who met eligibility criteria were referred for in-person screening from other community research efforts (Wejnert et al., 2017). We also posted flyers around the community. Eligibility criteria included: sexually active, HIV negative, Black CGW, age 20–49 and residence in DC, presence of any HIV risk factor (i.e., having an HIV-positive sex partner, sexually active in high prevalence area, a recent sexually transmitted infection, participation in sex work, inconsistent condom use). Participants received a $20 gift card incentive for their participation. We conducted the surveys in a private office rented from a local healthcare provider in the Anacostia neighborhood (8th Ward) of DC. Trained research assistants offered to administer the survey to all respondents verbally and survey data were entered on a tablet device using the Qualtrics platform either by the research assistant or the participant. The survey assessed HIV risk perceptions, awareness of PrEP, demographic characteristics, HIV risk behaviors, and prevention behaviors. Participants were then shown a six-minute informational video that included a description of PrEP, eligibility criteria, side-effects, side effect severity, cost, and efficacy, which has demonstrated effectiveness in pilot samples (Amico et al., 2014, 2014). Participants were then given the opportunity to ask any questions prior to completing the survey assessing the theoretical constructs.
We also surveyed a convenience sample of CGW presenting for family planning services at a tertiary care center in Washington DC (n = 104). We approached women in the waiting room of the obstetrics and gynecology clinic. After we obtained informed consent, women completed the survey on a tablet in the private exam room while waiting for their provider. The survey procedures and measures were identical to the community recruited sample. This study was approved by institutional review boards at the first and last authors’ institutional affiliations.
Measures
This research is based on formative research that was conceptualized, implemented, and analyzed in collaboration with a woman serving local HIV prevention community-based organization, The Women’s Collective. We developed the measures for this study based on ten elicitation focus groups that were theoretically grounded in the IMBP (N = 54). Measures adhere to the formulation of behavior from an IMBP perspective insofar as they refer to the target (i.e., you), action (i.e., using PrEP), context (i.e., for HIV prevention), and time (i.e., in the next 12 months). All variables were coded or recoded such that more positive responses were reflected by higher numbers.
We measured global constructs using 5-point Likert scales. We assessed intentions to use PrEP using a single item: “Do you plan to use PrEP to reduce your risk of getting HIV in the next 12 months?” We assessed attitudes using a single item: “Overall, would you say that using PrEP daily to prevent HIV risk is a good or a bad thing.” We assessed subjective norms using the mean of two variables, each measured using 5-point Likert scales: “Thinking about the people who are important to you – would they support or not support your using PrEP for HIV prevention in the next 12 months?” and “Thinking about people who are similar to you – how likely would they be to use PrEP for HIV prevention in the next 12 months?” Perceived behavioral control was assessed using a single item 5-point Likert scale of self-efficacy (Fishbein & Ajzen, 2010) “If I really wanted to, I could use PrEP daily for HIV prevention.”
We measured behavioral beliefs, normative referents, motivation to comply with each referent, and self-efficacy beliefs using 5-point Likert scales. We constructed normative belief measures by multiplying participants’ ratings of the motivation to comply with each referent by the respondents’ perception of the corresponding referents’ support for her PrEP uptake. As a result, the injunctive normative belief items range from 1 to 25. All items were coded such that higher scores represent more positive behavioral belief, more normative support, and higher SE. Table 1 provides the specific question wording for belief level variables.
Table 1.
Descriptive statistics for IMBP correlates of behavioral intention.
| Construct | N | Mean (SD) |
|---|---|---|
|
| ||
| Attitude: Overall, would you say that using PrEP daily to prevent HIV risk is a good or a bad thing | 237 | 4.47 (0.86) |
| Behavioral Beliefs | ||
| 1. PrEP is a safe way to prevent HIV infection | 218 | 4.24 (1.16) |
| 2. PrEP is an effective tool to prevent HIV infection | ||
| 3. If I take PrEP daily, I will feel protected from HIV | 210 | 4.03 (1.20) |
| Subjective norms: (mean of two items) | 236 | 3.947 (0.90) |
| Thinking about the people who are important to you – would they support or not support your using PrEP for HIV prevention in the next 12 months? Thinking about people who are similar to you – how likely would they be to use PrEP for HIV prevention in the next 12 months? | ||
| Normative Beliefs × Motivations to Comply | ||
| 1. Doctor | 213 | 20.98 (5.64) |
| 2. Main sex partner | 205 | 19.55 (6.97) |
| 3. Best friend | 122 | 15.23 (8.50) |
| 4. Mother | 189 | 17.08 (7.52) |
| 5. Sister | 180 | 12.92 (8.30) |
| Self-efficacy: If I really wanted to, I could use PrEP daily for HIV prevention | 235 | 4.17 (1.11) |
| Self-efficacy beliefs | ||
| 1. If I really wanted to, I could remember to take the pill every day. | 237 | 4.19 (1.14) |
| 2. I could take the pill every day, even if it gave me a stomach-ache. | 237 | 3.48 (1.43) |
| 3. I know where to start the process if I want to use PrEP for HIV prevention. | 237 | 4.07 (1.19) |
| 4. I could use PrEP for HIV prevention, even if my main partner didn’t want me to. | 236 | 4.23 (1.19) |
| 5. I just can’t take pills. (reverse coded) | 236 | 4.01 (1.30) |
| 6. Using daily PrEP to prevent HIV would make me feel in control of my health. | 235 | 3.98 (1.16) |
Analysis
We utilized structural equation modeling (SEM) as the main statistical technique to examine the relationships among targeted variables (Hennessy et al., 2012; Hull et al., 2011; Jordan et al., 2012). SEM analysis was carried out in two steps. First, we conducted a confirmatory factor analysis (CFA) to estimate the adequacy of the measurement models. Then, the structural model was analyzed to estimate relationships between latent and observed variables.
To evaluate model fit, we report the Chi-squared test, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the standardized root mean square residual (SRMR)(Kline, 2010). We used commonly used cutoff criteria to assess whether the goodness-of-fit indices are indicative of acceptable fit: (1) CFI and TLI values .90 or greater (Hu & Bentler, 1999); (2) RMSEA value close to .05 or below (MacCallum et al., 1992); 3) An SRMR value not large than .08 (Hu & Bentler, 1999); and (4) A nonsignificant χ2 value at a .05 threshold. However, the Chi-Square statistic was not used to judge model fit in this study because of its sensitivity to the current study’s sample size. When a large sample is employed in the study, the significance test of the Chi-Square often rejects the model (Bentler & Bonett, 1980; Jöreskog & Sörbom, 1993). We examined the validity and reliability of latent constructs using standardized factor loadings and Cronbach’s alpha (Hair et al., 2006). All descriptive statistics were conducted using SPSS version 26. Structural equation modeling was conducted using Mplus 8 (Muthén et al., 2017). We considered a p-value ≤ .05 to be statistically significant.
To understand which beliefs were important determinants of intentions to utilize PrEP, we examined the descriptive statistics for the beliefs underlying the relevant psychosocial constructs. We assessed (1) which beliefs were associated with intentions (i.e., correlations with intention and direct measures; significance of mean differences between intenders and non-intenders), and (2) the extent to which there was substantial “room to move” (i.e., the proportion who do not already fully endorse the belief) with respect to each belief (Brennan et al., 2017; Hornik & Woolf, 1999; Hornik et al., 2018; Jordan et al., 2012). The third criterion for identifying target beliefs is whether it is possible to change a particular belief through communication. Decisions about this criterion should be grounded in evidence-based and culturally-informed subjective judgment (Fishbein & Yzer, 2003), rather than statistical evidence.
Results
Sample characteristics
Among the 294 CGW who completed the survey, the average participant age was 33.4 years (±11.7SD). Respondents were predominantly Black (92.2%), single (78.9%), and 88% had health insurance coverage (70.1% Medicaid). Though 16.3% of respondents reported leaving school prior to graduation/GED, the majority of respondents had completed high school/GED (50.3%), some college (27.9%), or a college degree (4.9%); 22.1% described themselves as employed full time. The majority of the sample (53.1%) reported household incomes of less than $12,500; 11.3% reported < $25,000 and 19.4% reported annual household incomes > $25,000. There were 18.0% of participants who reported housing stability. One respondent reported ever having taken PrEP in the past 12 months to reduce risk of HIV infection.
Few respondents (11.9%) had ever heard of PrEP prior to their participation in the study. Though, when they learned about it, respondents indicated somewhat positive intentions to use it (mean 3.39, SD 1.29). Table 1 displays descriptive statistics for belief level measures while Table 2 reports correlations among the study variables.
Table 2.
Correlations for study variables.
| BI | AH | BB 1 | BB 2 | BB 3 | Subj. Norm | Doc | Main | BF | Mother | Sister | SE | SE 1 | SE 2 | SE 3 | SE 4 | SE 5 | SE 6 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Behavioral | ||||||||||||||||||
| Intention | — | |||||||||||||||||
| Attitude | .40*** | |||||||||||||||||
| Behavioral Belief | ||||||||||||||||||
| (BB) 1 | .39*** | .42*** | — | |||||||||||||||
| BB 2 | .32*** | .29*** | .79*** | — | ||||||||||||||
| BB 3 | .47*** | .45*** | .66*** | .59*** | — | |||||||||||||
| Subjective | ||||||||||||||||||
| Norm | .37*** | .35*** | .26*** | .27*** | .32*** | — | ||||||||||||
| Doc | .39*** | .31*** | .28*** | .39*** | .30*** | .24* | — | |||||||||||
| Main Sex Partner | .39*** | .25* | .22* | .26** | .26** | .37*** | .66*** | — | ||||||||||
| Best Friend | .41*** | .17 | .20** | .23* | .24** | .35*** | .60*** | .65*** | — | |||||||||
| Mother | .27*** | .06 | .20* | .17*** | .18 | .33*** | .49*** | .55*** | .62*** | — | ||||||||
| Sister | .34*** | .14 | .26* | .23* | .25* | .40*** | .52*** | .62*** | .59*** | .85*** | — | |||||||
| PBC | .43*** | .37*** | .45*** | .37*** | .48*** | .18** | .19* | .18* | .15 | .20* | .24* | — | ||||||
| Self-efficacy Belief | ||||||||||||||||||
| (SE) 1 | .39*** | .43*** | .40*** | .37*** | .43*** | .17* | .31*** | .27*** | .18* | .23** | .19* | .54*** | — | |||||
| SE 2 | .42*** | .32*** | .35*** | .39*** | .37*** | .37*** | .33*** | .27*** | .34*** | .31*** | .29*** | .31*** | .49*** | — | ||||
| SE 3 | .17* | .31*** | .38*** | .45*** | .40*** | .16* | .20** | .19** | .26** | .22** | .26** | .37*** | .32*** | .26*** | — | |||
| SE 4 | .26*** | .25*** | .37*** | .28*** | .33*** | .20** | .07 | .11 | .16* | .20** | .15 | .31*** | .37*** | .30*** | .30*** | — | ||
| SE 5 | .26*** | .21** | .27*** | .21** | .21*** | .24** | .09* | .09* | .08 | .12* | .12* | .26*** | .40*** | .34*** | .12 | 0.26*** | — | |
| SE 6 | 39*** | .42*** | .47*** | .52*** | .38*** | .22** | .25*** | .22** | .25*** | .18* | .22** | .40*** | .38*** | .42*** | .34*** | 0.40*** | 0.27*** | — |
p < 0.05
p < 0.01
p < 0.001
Measurement model
Results demonstrated that internal consistency was acceptable for attitudinal beliefs (α = .921), efficacy beliefs (α = 0.921), and normative referents (α = 0.939). Each of the observed belief items significantly loaded on the three respective latent factors for attitudinal beliefs (.380 to .419), normative beliefs (.377 to .501) and self-efficacy beliefs (.501 to .814), and all of the factor loadings were statistically significant.
Structural model
The SEM analysis demonstrated a good fit of the hypothesized model (χ2 = 207.601, df = 128, CFI=.924, TLI=.910, RMSEA=.057, SRMR=.070). The hypothesized structural model with standardized path coefficients is presented in Figure 2. Results showed that the relationships among the variables were significant and positive. There were significant and positive direct effects of SE (0.316, p < .01), subjective norms (0.249, p < .001) and attitudes (0.201, p < .001) on intention to initiate PrEP.
Figure 2.
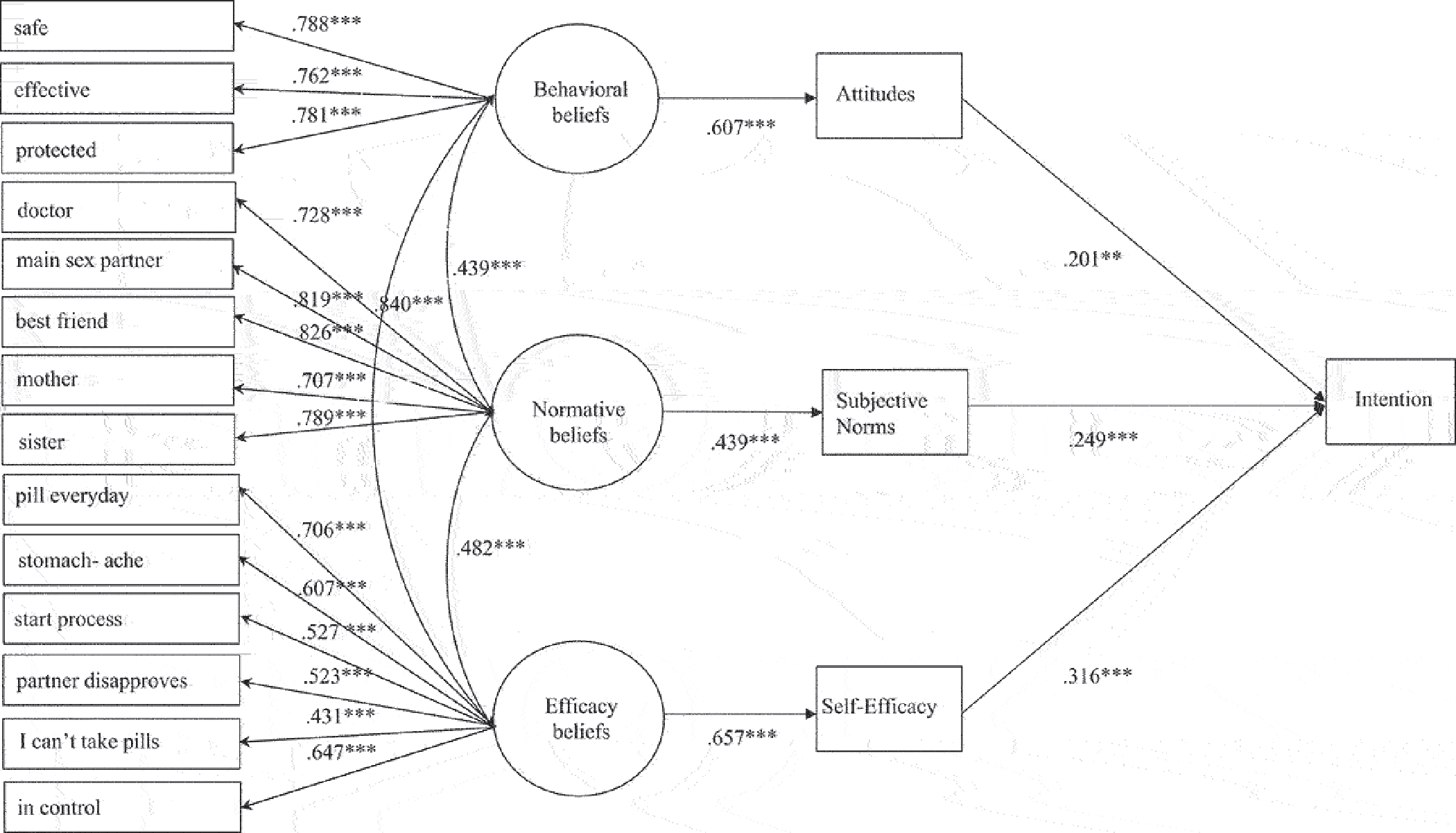
Structural equation model of the psychosocial determinants of PrEP uptake intention. Coefficients are standardized estimates; *p < .05; **p < .01; ***p < .001.
Underlying beliefs
The previous analysis demonstrated that SE, norms, and to a lesser extent, attitudes, are significant and substantial correlates of intentions to use PrEP. Table 3 details the relevant statistics for identifying important underlying beliefs, including correlations between specific beliefs and intentions. The table shows mean ratings for beliefs among those with high and low intentions, and the significance of the differences between group means, as well as the proportion of respondents who did not strongly endorse each belief (i.e., room to move).
Table 3.
Descriptive statistics for belief level variables by intender status and their correlations with behavioral intention.
| Construct | Non-intenders mean (SD) | Intenders mean (SD)# | Corr. (r) with intention | % to move+ |
|---|---|---|---|---|
|
| ||||
| Behavioral beliefs | ||||
| 1. PrEP is a safe way to prevent HIV infection | 3.94 (1.07) | 4.67 (0.74)*** | .39 | 43.2 |
| 2. PrEP is an effective tool to prevent HIV infection | 3.99 (1.03) | 4.53 (0.90)*** | .32 | 45.3 |
| 3. If I take PrEP daily, I will feel protected from HIV | 3.79 (1.04) | 4.60 (0.78)*** | .47 | 50.2 |
| Normative beliefs | ||||
| 1. Doctor | 19.14 (6.26) | 22.95 (4.09)*** | .39 | 44.1 |
| 2. Main sex partner | 17.74 (7.56) | 21.35 (5.84)*** | .39 | 48.8 |
| 3. Best friend | 13.500 (8.71) | 16.90 (8.00)* | .41 | 69.7 |
| 4. Mother | 14.73 (7.62) | 19.37 (6.71)*** | .27 | 64 |
| 5. Sister | 11.70 (8.06) | 14.22 (8.40)* | .34 | 78.9 |
| Self-efficacy beliefs | ||||
| 1. If I really wanted to, I could remember to take the pill every day. | 3.83 (1.25) | 4.57 (0.89)*** | .39 | 45.6 |
| 2. I could take the pill every day, even if it gave me a stomach-ache. | 2.88 (1.44) | 4.10 (1.12)*** | .42 | 67.9 |
| 3. I know where to start the process if I want to use PrEP for HIV prevention. | 3.90 (1.21) | 4.25 (1.16)* | .17 | 50.2 |
| 4. I could use PrEP for HIV prevention, even if my main partner didn’t want me to. | 3.93 (1.21) | 4.25 (1.16)*** | .26 | 38.1 |
| 5. I just can’t take pills. (reverse coded) | 2.28 (1.29) | 1.68 (1.24)*** | .26 | 44.9 |
| 6. Using daily PrEP to prevent HIV would make me feel in control of my health. | 3.53 (1.14) | 4.45 (0.99)*** | .39 | 56.2 |
p < .05
p < .01
p < .001 intenders = (4) probably and (5) definitely, n = 116; non-intenders = (1) definitely, (2) probably or (3) maybe not (n = 122).
p-values refer to mean comparisons between intenders and non-intenders; + proportion who did not give strongest positive response.
Correlations with intentions
Within the SE path, correlations between beliefs and intentions ranged from .17 to .42. The beliefs that using PrEP would “make me feel in control of my health,” that “I could take the pill every day, even if it gave me a stomach-ache” and that one could remember to take the pill each day most clearly distinguished intenders from non-intenders, with large mean differences. The belief that one could take PrEP daily, even if it causes stomach-ache demonstrated the largest mean differences, followed by beliefs about how PrEP would make one feel in control of her health. These beliefs were also were most strongly correlated with intentions. The normative path was also important in the formation of intentions. All normative beliefs demonstrated significant, positive correlations with intentions, which ranged from .27 to .41. This analysis demonstrated that beliefs about the support of best friends doctors, and main sex-partners were most strongly correlated with intentions. Among them, beliefs about doctors support of PrEP use demonstrated the largest mean differences between intenders and non-intenders. The attitudinal path was relatively less strongly associated with intentions, though still significant and substantial. All behavioral beliefs were moderately and positively associated with intentions. The belief that if I use PrEP, I will be protected from HIV is most strongly correlated with intention and useful in distinguishing intenders from non-intenders, because it demonstrates the largest mean difference.
Room to move
Table 3 also demonstrates “room to move” (Hornik & Woolf, 1999); the proportion of respondents who did not report the strongest positive response possible for each belief item. Within the SE path, the beliefs that demonstrated the most room to move were that one could take the pill each day, even with side-effects, that using PrEP would “make me feel in control of my health” and that “I know where to start the process . . . ” It is notable that two of the beliefs with the most room to move are also the beliefs that best distinguish intenders from non-intenders and exhibit the strongest correlations with intentions. Similarly, all of the injunctive normative beliefs also demonstrated substantial room to move, though sister, best friend and mother demonstrated the highest proportion. Among them, beliefs about ones’ best friend were also strongly correlated with intentions and demonstrated significant mean differences between intenders and non-intenders. It is also notable that beliefs about healthcare providers and partners also demonstrated substantial room to move. Similarly, there was substantial room to move for all behavioral beliefs. Notably, the belief that if I use PrEP, I will be protected from HIV” exhibited the most room to move as well as the highest correlation with intentions and the largest mean differences between intenders and non-intenders.
Discussion
In this study, we sought to understand the relative importance of psychosocial factors shaping women’s intentions to use PrEP from the perspective of The RAA. In our analysis, perceptions of behavioral control, subjective norms and attitudes are important psychosocial paths that shape intentions to use PrEP among CGW. In this study, we found that SE was weighted most heavily in the formulation of intention to uptake PrEP, followed by normative perceptions and to a lesser extent, attitudes.
Daily oral PrEP with TDF/FTC is both highly effective at reducing HIV transmission and well-tolerated, but has not been widely utilized by CGW at risk for HIV. Along with barrier contraception, PrEP is integral to HIV risk reduction for CGW and the elimination of disparities in HIV acquisition. Nationally, CGW represent only 2–3% of PrEP users, a disparately low number relative to the need for prevention. Further, Black women are dramatically underserved relative to patterns of infection and the distribution of PrEP uptake among women. Yet, there is inchoate literature on CGWs PrEP uptake, particularly in relation to modeling the relative importance of the many factors that may shape their decision to use PrEP.
Theoretically grounded insight into the relative importance of the determinants of PrEP uptake is critically important formative knowledge. This empirical evidence is necessary to develop and implement effective communication interventions that can work to mitigate the drastic inequities in PrEP utilization. This study represents a step forward in understanding the relative importance of psychosocial factors shaping PrEP intentions and identifying the relative weight of the specific underlying beliefs within each path, which should be the focus of strategic communication and behavioral interventions.
Descriptive results showed that, as in previous research, CGW were receptive to PrEP insofar as sample means indicate moderately positive intentions to use it, when they learn about it. Attitudes toward PrEP were primarily positive, as were perceptions of injunctive norms around PrEP use. Respondents also reported positive expectations about their ability to use it in light of various challenges that are likely to be present.
All of the beliefs demonstrated significant associations with intentions and substantial “room to move” within the sample. But, only some of these beliefs are strong contenders for fruitful intervention foci. Control beliefs demonstrated moderate to strong correlations with intentions, particularly beliefs about managing the daily regimen (i.e., taking the pill every day), managing side-effects (i.e., stomach-ache), and that PrEP would “make me feel in control of my health.” Among these beliefs, beliefs about the ability to manage side effects (i.e., stomach-ache) and that PrEP is empowering (i.e., “will make me feel in control of my health”) satisfied the first and second criteria. Based on our informed judgment, we anticipate that these beliefs are also well suited to be addressed through communication. Among the most important normative beliefs were beliefs about the support of main sex partners, best friends, and healthcare providers. These beliefs demonstrated substantial mean differences between intenders and non-intenders, significant and moderate to strong correlations with intention and substantial room to move. Whether they satisfy the third criterion is questionable, in our view. It may be difficult and inappropriate to focus on beliefs about provider, partner, and peer support without associated efforts to ensure that the expectation of support is met with actual support.
Within the attitudinal path, the belief that “if I take PrEP, I will be protected from HIV” is most strongly correlated with intention and useful in distinguishing intenders from non-intenders, because it demonstrates the largest mean difference. This belief also demonstrated the most room to move. This belief meets the first and second criteria. We also anticipate that this belief may be a fruitful focus of persuasive communication efforts.
This analysis suggests which beliefs could be fruitful targets in terms of their distribution in the sample and their correlation with intentions. However, this analysis does not reveal which beliefs could be reasonably expected to be changed through communication and behavioral intervention. This is a critically important aspect of belief selection which should be informed by knowledge of and collaboration with the communities involved. Collaborative and participatory research, which centers on the lived experiences and perspectives of the focal community, enhances the likelihood that communication and behavioral intervention activities focused on specific beliefs will be resonant, relevant, convincing, and effective. For example, the belief that one knows where to start the process if one wants to use PrEP may be a good contender for intervention based on the first and second criteria. This belief is significantly associated with intention and there is much room to move. However, this belief is likely rooted in experience, difficult and potentially inappropriate to attempt change through persuasive communication alone. Other kinds of communication and public health interventions may be better suited to address the complexities of navigating the healthcare system experienced by this population.
Among normative referents, CGW were most motivated to comply with healthcare providers, main sex partners, and best friends, and generally anticipated that these individuals would be supportive of their PrEP use. However, there were a substantial number of women who expressed perceptions of less than full support of these important normative referents. Strategies that cultivate and communicate the support of healthcare providers, partners, peers, and family are productive if not crucial avenues for intervention. We emphasize that, given low awareness in this population, the importance CGW placed on the support of providers and the large mean differences in mean differences between intenders and non-intenders, communication and behavioral intervention activities to increase CGW’s PrEP uptake should focus on increasing provider’s discussion of PrEP with women to increase awareness and supportive norms.
The RAA specifies, and extant communication and public health research and practice illustrate, that the relationship between intentions and behaviors is moderated by environmental (e.g., prohibitive policies)(Calabrese et al., 2019), social and individual (i.e., access to quality healthcare, skills) factors. Even the best intentions may be thwarted in unsupportive social-structural contexts (Bowleg et al., 2013; Bowleg, 2012; Flash et al., 2017). Interventions that focus on bolstering attitudes, perceptions of norms, and efficacy may fail without concomitant efforts to bolster access, support adherence, cultivate social support and facilitate navigation of resources. Psychosocial determinants are necessary but not sufficient to support behavioral enactment in this context. For example, the impact of subjective norms may be mediated by intentions, but norms may also serve as environmental barriers insofar as partners and providers create actual barriers to access (i.e., limiting autonomy), undermining intentions.
The setting for this research is a critically important contextual factor in understanding the factors that shape CGW’s consideration of PrEP. In DC, many environmental barriers to access have been mitigated (i.e., due to Medicaid expansion, public insurance coverage is high, PrEP is covered, and same-day, free PrEP is also available through multiple channels). Yet, even in a context in which PrEP use is facilitated by programs and policies that increase access, community prevalence is high, and CGW express willingness to use it, underutilization persists because women are unaware of this option, indicating structural communication gaps (Goulbourne & Yanovitzky, 2021). Thus, the results of this research identify apertures for communication interventions beyond those focused on individual belief change. In particular, strategies that focus on the structures that shape inequitable access to information (i.e., communication infrastructure, healthcare delivery practices, guidance for PrEP eligibility) are sorely needed.
Finally, the RAA approach provides prescription for strategic efforts (i.e., community discussions, patient-provider communication tools, advertising, op-eds, behavioral interventions) to raise awareness of PrEP and cultivate intentions to use it in this population through persuasion or changing the extremity with beliefs are held. Another strategy is to render the beliefs that people already strongly endorse more salient, or media priming (Fishbein & Yzer, 2003). Communication efforts to raise PrEP awareness and uptake could focus on highlighting the beliefs that women already endorse, which are favorable to PrEP to uptake but have weak correlations with intention. Strengthening the correlations between positively held beliefs and behavioral intentions has the potential to induce change in large proportions of the audience (Fishbein & Yzer, 2003). Extant research demonstrates the media priming phenomenon in political communication contexts (Ewoldsen & Rhodes, 2020). Future research should test this potentially powerful mechanism of effects in this context.
Limitations
This study is cross-sectional. Thus, we cannot determinant the extent to which intentions translate into behavior in this study. The persistent information gaps complicate this problem, as CGW who may benefit from PrEP, particularly women of color, report low awareness and uptake perpetually. Thus, the extent to which behavioral intention correlates with behavior is unclear in this context. Though, the intention-behavior relationship has been established in related contexts (Albarracin et al., 2001).
Relatedly, this study was prompted by evidence of pervasive low awareness in populations of eligible Black women (Flash et al., 2017; Goparaju et al., 2015; Ojikutu et al., 2018; Patel et al., 2019), which was corroborated in this sample. But, in order to understand women’s perspectives about PrEP, they must first be informed about it. We showed a 6-minute, informational video to explain PrEP and it’s indications. The professionally produced video was developed by HIV prevention research scientists in collaboration with clinicians and with financial support of the manufacturer. It has demonstrated effectiveness for conveying factual information about PrEP (Amico et al., 2014) and is highly circulated (Amico et al., 2014). It is likely that exposure to the video influenced awareness of what PrEP is, how it works and is used, eligibility criteria, and side-effects, which limits the generalizability of our findings to women who learn comprehensive and accurate information about PrEP.
Finally, the correspondence across measures is not perfect. Daily use of PrEP is implied in “use of PrEP for HIV prevention” for CGW and is emphasized in the informational video presented to CGW in this study. Thus, we did do not consider this a necessary aspect of the conceptualization of TACT. The global measures of attitudes and efficacy are limited by the absence of the specification of time (“next 12 months”), which may attenuate relationships.
Conclusion
Persistently low awareness and utilization of PrEP among CGW is a direct challenge to ending the epidemic and eliminating disparities in HIV infection. This research addresses an important gap in empirical knowledge by identifying the relative importance of psychosocial factors in PrEP uptake intentions among women who may benefit from PrEP use. Further, this research identifies the relevant beliefs within those paths, which may be fruitful targets of intervention activities. Addressing beliefs relevant to CGW to impact psychosocial path to PrEP uptake intentions is a necessary strategy in the effort to end the HIV epidemic.
Acknowledgements
Authors wish to acknowledge Dr. Lisa Bowleg, Dr. Irene Kuo and Dr. David Huebner, as well as the DC Center for Research Developmental and Scientific Cores for their thoughtful feedback on this project. We also wish to thank Mr. Anthony Rawls, Ms. Tori Rivera and Ms. Kelsey Vahid and for their contribution to data collection efforts.
Funding
Research reported in this publication was supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001409 and by the National Institute on Drug Abuse of the National Institutes of Health under award number 1K01DA050496-01A1. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health. This research was also facilitated by Pilot Award funding, services, and resources provided by the District of Columbia Center for AIDS Research, an NIH funded program (P30AI117970), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, NIDDK, NIMHD, NIDCR, NINR, FI, C, and OAR.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Aaron E, Blum C, Seidman D, Hoyt MJ, Simone J, Sullivan M, & Smith DK (2018). Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care and STDS, 32(1), 16–23. 10.1089/apc.2017.0201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adimora AA, Ramirez C, Auerbach JD, Aral SO, Hodder S, Wingood G, El-Sadr W, Bukusi EA, & HIV Prevention Trials Network Women at Risk Committee. (2013). Preventing HIV infection in women. Journal of Acquired Immune Deficiency Syndromes, 63 (Suppl. 2), S168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adimora A, & Schoenbach VJ (2002). Contextual factors and the black-white disparity in heterosexual HIV transmission. Epidemiology, 13(6), 707–712. 10.1097/00001648-200211000-00016 [DOI] [PubMed] [Google Scholar]
- Albarracin D, Johnson BT, Fishbein M, & Muellerleile PA (2001). Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin, 127(1), 142–161. 10.1037/0033-2909.127.1.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaro H (1995). Love, sex, and power: Considering women’s realities in HIV prevention. The American Psychologist, 50(6), 437–447. 10.1037/0003-066X.50.6.437 [DOI] [PubMed] [Google Scholar]
- Amaro H, & Raj A (2000). On the margin: Power and women’s HIV risk reduction strategies. Sex Roles, 42(7–8), 723–749. 10.1023/A:1007059708789 [DOI] [Google Scholar]
- Amaro H, Raj A, & Reed E (2001). Women’s sexual health: The need for feminist analyses in public health in the decade of behavior. Psychology of Women Quarterly, 25(4), 324–334. 10.1111/1471-6402.00032 [DOI] [Google Scholar]
- Amico KR, Balthazar C, Coggia T, & Hosek S (2014, June 8–10). PrEP audio visual representation (PrEP REP): Development and pilot of a PrEP education video [Conference presentation]. 9th International Conference on HIV Treatment and Prevention Adherence, IAPAC, Miami, FL, United States. [Google Scholar]
- Amico KR, Balthazar C, Coggia T, & Hosek S (2014). What is PrEP?. http://www.whatisprep.org/
- Armitage CJ, & Conner M (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology, 40(4), 471–499. 10.1348/014466601164939 [DOI] [PubMed] [Google Scholar]
- Atkin CK, & Rice RE (2013). Theory and principles of public communication campaigns. In Rice RE & Atkin CK (Eds.), Public communication campaigns (4th ed., pp. 3–20). Sage Publications, Inc. [Google Scholar]
- Auerbach JD, & Hoppe TA (2015). Beyond “getting drugs into bodies”: Social science perspectives on pre-exposure prophylaxis for HIV. Journal of the International AIDS Society, 18(Suppl. 3), S19983–19988. 10.7448/IAS.18.4.19983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach JD, Kinsky S, Brown G, & Charles V (2015). Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care and STDs, 29(2), 102–110. 10.1089/apc.2014.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten J, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Tappero JW, Bukusi EA, Cohen CR, Katabira E, Ronald A, Tumwesigye E, Were E, Fife KH, Kiarie J, Farquhar C, John-Stewart G, Kakia A, Odoyo J . . . Celum C (2012). Antiretroviral pre-exposure prophylaxis for HIV prevention in men and women. The New England Journal of Medicine, 367(5), 399–410. 10.1056/NEJMoa1108524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM, & Bonett DG (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88(3), 588–606. 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- Bleakley A, & Hennessy M (2012). The quantitative analysis of reasoned action theory. The Annals of the American Academy of Political and Social Science, 640(1), 28–41. 10.1177/0002716211424265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogorodskaya M, Lewis SA, Krakower DS, & Avery A (2020). Low awareness of and access to pre-exposure prophylaxis but high interest among heterosexual women in Cleveland, Ohio. Sexually Transmitted Diseases, 47(2), 96–99. 10.1097/OLQ.0000000000001082 [DOI] [PubMed] [Google Scholar]
- Bowleg L (2004). Love, sex, and masculinity in sociocultural context HIV concerns and condom use among African American men in heterosexual relationships. Men and Masculinities, 7(2), 166–186. 10.1177/1097184X03257523 [DOI] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality—An important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Burkholder GJ, Massie JS, Wahome R, Teti M, Malebranche DJ, & Tschann JM (2013). Racial discrimination, social support, and sexual HIV risk among Black heterosexual men. AIDS and Behavior, 17(1), 407–418. 10.1007/s10461-012-0179-0 [DOI] [PubMed] [Google Scholar]
- Bowleg L, Lucas KJ, & Tschann JM (2004). The ball was always in his court: An exploratory analysis of sexual relationship scripts, sexual scripts and condom use among African American women. Psychology of Women Quarterly, 28(1), 70–82. 10.1111/j.1471-6402.2004.00124.x [DOI] [Google Scholar]
- Brennan E, Gibson LA, Kybert-Momjian A, Liu J, & Hornik RC (2017). Promising themes for antismoking campaigns targeting youth and young adults. Tobacco Regulatory Science, 3(1), 29–46. 10.18001/TRS.3.1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush S, Magnuson D, Rawlings MK, Hawkins T, McCallister S, & Mera Giler R (2016). Racial characteristics of FTC/TDF for pre-exposure prophylaxis (PrEP) users in the US. ASM Microbe/ICAAC. https://www.natap.org/2016/HIV/062216_02.htm
- Calabrese SK, Tekeste M, Mayer KH, Magnus M, Krakower DS, Kershaw TS, Eldahan AI, Gaston Hawkins LA, Underhill K, Hansen NB, Betancourt JR, & Dovidio JF (2019). Considering stigma in the provision of HIV pre-exposure prophylaxis: Reflections from current prescribers. AIDS Patient Care and STDs, 33(2), 79–88. 10.1089/apc.2018.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese SK, Willie TC, Galvao RW, Tekeste M, Dovidio JF, Safon CB, Blackstock O, Taggart T, Kaplan C, Caldwell A, & Kershaw TS (2019). Current US guidelines for prescribing HIV pre-exposure prophylaxis (PrEP) disqualify many women who are at risk and motivated to use PrEP. Journal of Acquired Immune Deficiency Syndromes, 81(4), 395–405. 10.1097/qai.0000000000002042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappella JN, Fishbein M, Hornik R, Ahern RK, & Sayeed S (2001). Using theory to select messages in antidrug media campaigns. In Rice RE & Atkin CK (Eds.), Public communication campaigns (3rd ed., pp. 214–230). Sage Publications, Inc. [Google Scholar]
- Centers for Disease Control and Prevention. (2016). HIV Surveillance Report, 2015. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf
- Centers for Disease Control and Prevention. (2018). HIV in the United States: At a glance. https://www.natap.org/2018/HIV/081018_02.htm
- Elion R, & Coleman M (2016). The preexposure prophylaxis revolution: From clinical trials to routine practice: Implementation view from the USA. Current Opinion in HIV and AIDS, 11(1), 67–73. 10.1097/COH.0000000000000222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewoldsen DR, & Rhodes N (2020). Media priming and accessibility. In Oliver MB, Raney AA & Bryant J (Eds.), Media effects: Advances in theory and research (4th ed., pp. 83–99). Routledge. [Google Scholar]
- Fishbein M (2000). The role of theory in HIV prevention. AIDS Care, 12 (3), 273–278. 10.1080/09540120050042918 [DOI] [PubMed] [Google Scholar]
- Fishbein M (2009). An integrative model for behavioral prediction and its application to health promotion. In DiClemente RJ, Crosby RA & Kegler MC (Eds.), Emerging theories in health promotion practice and research (pp. 215–234). Jossey-Bass. [Google Scholar]
- Fishbein, & Ajzen I. (2010). Predicting and changing behavior: The reasoned action approach ((1st ed.). Psychology Press. 10.4324/9780203838020 [DOI] [Google Scholar]
- Fishbein M, Hennessy M, Kamb M, Bolan GA, Hoxworth T, Iatesta M, Rhodes F, Zenilman JM, & Project Respect Study Group. (2001). Using intervention theory to model factors influencing behavior change. Project RESPECT. Evaluation & the Health Professions, 24(4), 363–384. 10.1177/01632780122034966 [DOI] [PubMed] [Google Scholar]
- Fishbein M, Von Haeften I, & Appleyard J (2001). The role of theory in developing effective interventions: Implications from Project SAFER. Psychology, Health & Medicine, 6(2), 223–238. 10.1080/13548500123176 [DOI] [Google Scholar]
- Fishbein M, & Yzer MC (2003). Using theory to design effective health behavior interventions. Communication Theory, 13(2), 164–183. 10.1111/j.1468-2885.2003.tb00287.x [DOI] [Google Scholar]
- Flash CA, Dale SK, & Krakower DS (2017). Pre-exposure prophylaxis for HIV prevention in women: Current perspectives. International Journal of Women’s Health, 2017(9), 391–401. 10.2147/IJWH.S113675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flash CA, Stone VE, Mitty JA, Mimiaga MJ, Hall KT, Krakower D, & Mayer KH (2014). Perspectives on HIV prevention among urban black women: A potential role for HIV pre-exposure prophylaxis. AIDS Patient Care & STDs, 28(12), 635–642. 10.1089/apc.2014.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, & Decker MR (2017). Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care, 29(6), 751–758. 10.1080/09540121.2016.1234679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G, & Kok G (1996). The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion, 11(2), 87–98. 10.4278/0890-1171-11.2.87 [DOI] [PubMed] [Google Scholar]
- Goparaju L, Experton LS, Praschan NC, Warren-Jeanpiere L, Young MA, & Kassaye S (2015). Women want pre-exposure prophylaxis but are advised against it by their HIV-positive counterparts. Journal of AIDS & Clinical Research, 6(11), 1–10. 10.4172/2155-6113.1000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goparaju L, Praschan N, Warren-Jeanpiere L, Experton L, Young M, & Kassaye S (2017). Stigma, partners, providers and costs: Potential barriers to PrEP uptake among US women. Journal of AIDS & Clinical Research, 8(9), 730–748. 10.4172/2155-6113.1000730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulbourne T, & Yanovitzky I (2021). The communication infrastructure as a social determinant of health: Implications for health policy-making and practice. The Milbank Quarterly, 99(1), 24–40. 10.1111/1468-0009.12496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAHSTA. (2017). Annual epidemiology & surveillance report: Data Through December 2016. https://doh.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/HAHSTA%20Annual%20Report%202017%20-%20Final%20%282%29%20%282%29pdf
- HAHSTA. (2020). Annual epidemiology & surveillance report: Data Through December 2019. https://doh.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/HAHSTA%20Annual%20Report%202017%20-%20Final%20%282%29%20%282%29.pdf
- Hair J, Black W, Babin B, Anderson R, & Tatham R (2006). Multivariate data analysis (6th ed.). Pearson Prentice Hall. [Google Scholar]
- Hennessy M, Bleakley A, & Fishbein M (2012). Measurement models for reasoned action theory. The Annals of the American Academy of Political and Social Science, 640(1), 42–57. 10.1177/0002716211424709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornik R, Volinsky A, Mannis S, Gibson L, Brennan E, Lee S, & Tan A (2018). Validating the Hornik & Woolf approach to choosing media campaign themes: Do promising beliefs predict behavior change in a longitudinal study? Communication Methods and Measures, 13(1), 60–68. 10.1080/19312458.2018.1515902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornik R, & Woolf KD (1999). Using cross-sectional surveys to plan message strategies. Social Marketing Quarterly, 5(2), 34–41. 10.1080/15245004.1999.9961044 [DOI] [Google Scholar]
- Huang YA, Zhu W, Smith DK, Harris N, & Hoover KW (2018). HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. Morbidity and Mortality Weekly Report, 67(41), 1147–1150. 10.15585/mmwr.mm6741a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hull SJ, Hennessy M, Bleakley A, Fishbein M, & Jordan A (2011). Identifying the causal pathways from religiosity to delayed adolescent sexual behavior. Journal of Sex Research, 48(6), 543–553. 10.1080/00224499.2010.521868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, Jemmott LS, Braverman PK, & Fong GT (2005). HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine, 159(5), 440–449. 10.1001/archpedi.159.5.440 [DOI] [PubMed] [Google Scholar]
- Jemmott JB, Jemmott LS, & Fong GT (1998). Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: A randomized controlled trial. Journal of the American Medical Association, 279(19), 1529–1536. 10.1001/jama.279.19.1529 [DOI] [PubMed] [Google Scholar]
- Jordan A, Piotrowski JT, Bleakley A, & Mallya G (2012). Developing media interventions to reduce household sugar-sweetened beverage consumption. The Annals of the American Academy of Political and Social Science, 640(1), 118–135. 10.1177/0002716211425656 [DOI] [Google Scholar]
- Jöreskog KG, & Sörbom D (1993). LISREL 8: Structural equation modeling with the SIMPLIS command language. Scientific Software International. [Google Scholar]
- Khan MR, Behrend L, Adimora AA, Weir SS, Tisdale C, & Wohl DA (2011). Dissolution of primary intimate relationships during incarceration and associations with post-release STI/HIV risk behavior in a Southeastern city. Sexually Transmitted Diseases, 38(1), 43–47. 10.1097/OLQ.0b013e3181e969d0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2010). Promise and pitfalls of structural equation modeling in gifted research. In Thompson B & Subotnik RF (Eds.), Methodologies for conducting research on giftedness (pp. 147–169). American Psychological Association. 10.1037/12079-007 [DOI] [Google Scholar]
- LaCroix JM, Snyder LB, Huedo-Medina TB, & Johnson BT (2014). Effectiveness of mass media interventions for HIV prevention, 1986–2013: A meta-analysis. Journal of Acquired Immune Deficiency Syndromes, 66(Suppl. 3), S329–340. 10.1097/QAI.0000000000000230 [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Roznowski M, & Necowitz LB (1992). Model modifications in covariance structure analysis: The problem of capitalization on chance. Psychological Bulletin, 111(3), 490–504. 10.1037/0033-2909.111.3.490 [DOI] [PubMed] [Google Scholar]
- McEachan RR, Conner M, Taylor NJ, & Lawton RJ (2011). Prospective prediction of health-related behaviours with the theory of planned behaviour: A meta-analysis. Health Psychology Review, 5(2), 97–144. 10.1080/17437199.2010.521684 [DOI] [Google Scholar]
- McEachan RR, Taylor N, Harrison R, Lawton R, Gardner P, & Conner M (2016). Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine, 50(4), 592–612. 10.1007/s12160-016-9798-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK, & Asparouhov T (2017). Regression and mediation analysis using Mplus. Muthén & Muthén. [Google Scholar]
- Noar SM (2006). A 10-year retrospective of research in health mass media campaigns: Where do we go from here? Journal of Health Communication, 11(1), 21–42. 10.1080/10810730500461059 [DOI] [PubMed] [Google Scholar]
- Noar SM (2008). Behavioral interventions to reduce HIV-related sexual risk behavior: Review and synthesis of meta-analytic evidence. AIDS and Behavior, 12(3), 335–353. 10.1007/s10461-007-9313-9 [DOI] [PubMed] [Google Scholar]
- Noar SM, Black HG, & Pierce LB (2009). Efficacy of computer technology-based HIV prevention interventions: A meta-analysis. AIDS, 23(1), 107–115. 10.1097/QAD.0b013e32831c5500 [DOI] [PubMed] [Google Scholar]
- Ojikutu BO, Bogart LM, Higgins-Biddle M, Dale SK, Allen W, Dominique T, & Mayer KH (2018). Facilitators and barriers to pre-exposure prophylaxis (PrEP) use among black individuals in the United States: Results from the national survey on HIV in the black community (NSHBC). AIDS and Behavior, 22(11), 1–12. 10.1007/s10461-018-2067-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AS, Goparaju L, Sales JM, Mehta CC, Blackstock OJ, Seidman D, Ofotokun I, Kempf MC, Fischl MA, Golub ET, Adimora AA, French AL, DeHovitz J, Wingood G, Kassaye S, & Sheth AN (2019). PrEP eligibility among at-risk women in the Southern United States: Associated factors, awareness, and acceptability. Journal of Acquired Immune Deficiency Syndromes, 80 (5), 527–532. 10.1097/QAI.0000000000001950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulerwitz J, Amaro H, Jong WD, Gortmaker SL, & Rudd R (2002). Relationship power, condom use and HIV risk among women in the USA. AIDS Care, 14(6), 789–800. 10.1080/0954012021000031868 [DOI] [PubMed] [Google Scholar]
- Scott RK, Hull SJ, Richards RC, Klemmer K, Salmoran F, & Huang JC (2021). Awareness, acceptability, and intention to initiate HIV pre-exposure prophylaxis among pregnant women. AIDS Care, 34 (2), 1–13. 10.1080/09540121.2021.1916870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler AJ, Mouhanna F, Giler RM, Weiss K, Pembleton E, Guest J, Jones J, Castel A, Yeung H, Kramer M, McCallister S, & Sullivan PS (2018). The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis–to-need ratio in the fourth quarter of 2017, United States. Annals of Epidemiology, 28(12), 841–849. 10.1016/j.annepidem.2018.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Toledo L, Smith DJ, Adams MA, & Rothenberg R (2012). Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Education and Prevention, 24(5), 408–421. 10.1521/aeap.2012.24.5.408 [DOI] [PubMed] [Google Scholar]
- Smith DK, Van Handel M, & Grey J (2018). Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Annals of Epidemiology, 28(12), 850–857. 10.1016/j.annepidem.2018.05.003 [DOI] [PubMed] [Google Scholar]
- Snyder LB (2007). Health communication campaigns and their impact on behavior. Journal of Nutrition Education and Behavior, 39(2), S32–40. 10.1016/j.jneb.2006.09.004 [DOI] [PubMed] [Google Scholar]
- Snyder LB, & Hamilton MA (2002). A meta-analysis of US health campaign effects on behavior: Emphasize enforcement, exposure, and new information, and beware the secular trend. In Hornik RC (Ed.), Public health communication (pp. 373–400). Lawrence Erlbaum Associates. [Google Scholar]
- Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, Henderson FL, Pathak SR, Soud FA, Chillag KL, Mutanhaurwa R, Chirwa LI, Kasonde M, Abebe D, Buliva E, Gvetadze RJ, Johnson S, Sukalac T, Thomas VT . . . Brooks JT (2012). Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. The New England Journal of Medicine, 367(5), 423–434. 10.1056/NEJMoa1110711 [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. (2019). Ending the HIV epidemic in the United States. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview
- Wejnert C, Raymond HF, Robbins T, Prejean J, Hall HI, McCray E, Paz-Bailey G, & NHBS study group. (2017). Achieving greater HIV prevention impact through CDC’s national HIV behavioral surveillance system. Journal of Acquired Immune Deficiency Syndromes, 75(Suppl. 3), S249–252. [DOI] [PubMed] [Google Scholar]
- Wingood GM, & DiClemente RJ (2000). Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior, 27(5), 539–565. 10.1177/109019810002700502 [DOI] [PubMed] [Google Scholar]
- Wingood GM, Dunkle K, Camp C, Patel S, Painter JE, Rubtsova A, & DiClemente RJ (2013). Racial differences and correlates of potential adoption of preexposure prophylaxis: Results of a national survey. Journal of Acquired Immune Deficiency Syndromes, 63(Suppl. 1), S95–101. 10.1097/QAI.0b013e3182920126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yzer M (2017). Reasoned action as an approach to understanding and predicting health message outcomes. In Parrot R (Ed.), Oxford Research Encyclopedia of Communication (pp. 21). Oxford University Press. 10.1093/acrefore/9780190228613.013.255 [DOI] [Google Scholar]


