Abstract
Objective
Placental pathology is a well-known cause of perinatal and neonatal mortality and morbidity, and may correlate with placental growth, which can be assessed indirectly by anthropometric placental measurements. The aim of this cross-sectional study was to investigate mean placental weight and its relationship with birthweight and maternal body mass index (BMI).
Methods
Fresh (not formalin fixed) consecutively delivered placentae of term newborns (37–42 weeks), collected between February 2022 and August 2022, and the mothers and newborns, were included. Mean placental weight, birthweight and maternal BMI were calculated. Pearson’s correlation coefficient, linear regression, and one-way analysis of variance were used to analyse continuous and categorical data.
Results
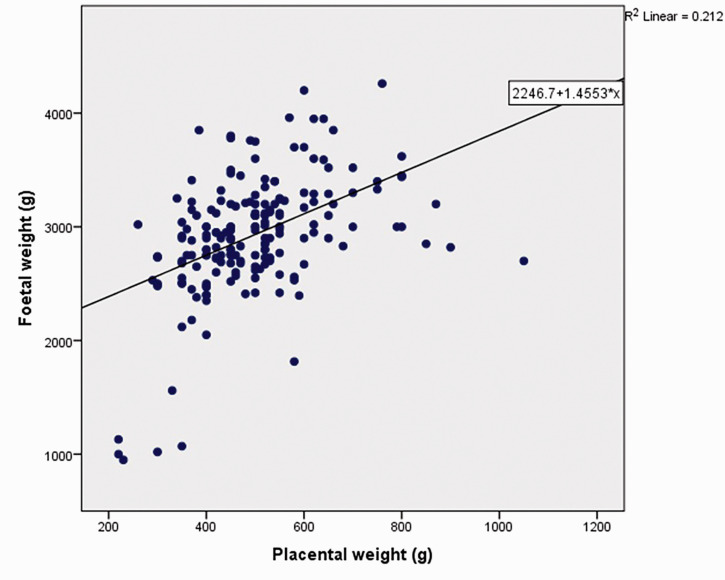
Out of 390 samples, 211 placentae (with 211 newborns and mothers) were included in this study after exclusion criteria were applied. Mean placental weight was 494.45 ± 110.39 g, and mean term birth weight/placental weight ratio was 6.21 ± 1.21 (range, 3.35–11.62 g). Placental weight was positively correlated with birthweight and maternal BMI, but not with newborn sex. Linear regression effect estimation of placental weight on birthweight revealed a medium correlation (R2 = 0.212; formula, 1.4553 × X + 2246.7, where X is placental weight [g]).
Conclusion
Placental weight was revealed to positively correlate with birthweight and maternal BMI.
Keywords: Placental, fetal, fetal weight to placental weight, maternal BMI, placental pathology, newborn weight
Introduction
Placental pathology is a well-known cause of perinatal and neonatal mortality and morbidity, with increased adverse maternal outcomes. 1 Complete and meticulous investigation of the placenta, including macroscopy, microscopy, immunohistochemistry, and genetic studies where relevant, is useful in revealing such pathology. Fetal growth and the ability to thrive in utero depends upon placental function. The average weight of a trimmed placenta at term is reported to be 510 g, with a diameter of 185 mm, 23 mm thickness, and an average volume of 500 ml. 2 Placental weight has also been reported to vary between 300 g and 890 g according to birthweight, with a mean of 590 ± 82 g. In general, the ratio between placental weight and newborn birthweight is 1:6. 3 Two standard references are endorsed by the College of American Pathologists regarding placental weight: absolute weight and fetal/placental weight ratio.4,5 Neonatal birthweight to placental weight ratio indicates the adequacy of fetal nutrition, while the placental weight to birthweight ratio is a proxy indicator of placental efficiency.6,7 Importantly, such morphometric measurements are heterogeneous throughout the world, varying from region to region, country to country, across regions within the same country, and according to the ethnicity/ancestry of the mother and fetus. The aim of the present study was to investigate the mean placental weight of the term newborn and its relationship with birthweight and maternal body mass index (BMI) in a single unit of a tertiary care hospital in Sri Lanka.
Participants and methods
Study population and data collection
This cross-sectional, descriptive-analytical survey (study) was conducted in the Professorial Unit, Teaching Hospital, Jaffna, which is the largest tertiary care hospital in the Northern Province of Sri Lanka, catering to obstetric and neonatal care for the entire Jaffna peninsula and to the majority of complicated patients from other districts of the Northern Province. The survey was conducted according to STROBE guidelines. 8 Ethical authorization was obtained from the Ethics review committee of the Teaching Hospital, Jaffna, Sri Lanka on 3 February 2022 (approval No. S-04/01/2022). Written informed consent was obtained from the mothers, according to the accepted method and ethics. Fresh (not formalin fixed) placentae of the term newborns (37–42 weeks) consecutively delivered by healthy pregnant mothers in the labour room, between February 2022 and August 2022, were included in this study. The placenta of term infants born to non-Sri Lankan mothers; twin placenta; placenta of term infants from mothers with chronic diseases, such as diabetes, hypertension, thyroid disorders, anaemia, or fetal growth restriction; placenta with disruption or damage during delivery; and/or pathological placenta; were excluded from the study. Pathological placentae were diagnosed by macroscopic and microscopic examination. Gestational age (GA) was recorded according to the first day of the last normal menstrual period (LMP). Ultrasound scan-dating was extracted from the antenatal reports. If the two were in agreement, i.e., did not differ by >10 days, the LMP-GA was used. If the difference was >10 days, then the booking scan GA was used. Ultrasound examinations for abnormal position of the placenta and accreta spectrum disorders of the placenta were routinely performed at 20 to 22 weeks of pregnancy. Maternal BMI (kg/m2) was extracted from the antenatal record obtained at the beginning of the booking visit during the first trimester after missing a menstrual period. The mothers were categorized into three groups according to their BMI: ≤24.99, 25-29.99, and ≥30. The weight of the fresh placenta (functional tissue) was measured (to the nearest g) after removal of the whole membranes, the whole length of the umbilical cord, and blood clots (trimmed weight), according to the Amsterdam protocol for placental examination. 9 The birthweight of the newborn (to the nearest g) was obtained within a few minutes of birth, before any significant postnatal weight loss.
Statistical analyses
Data are presented as mean ± SD or n (%) prevalence. All data were entered into an Excel spreadsheet (Microsoft Excel 2016, version 2211; Microsoft.com) by trained doctors after a pilot study. All patient details were de-identified and coding numbers were used to enter data. Data were then analysed with IBM SPSS Statistics for Windows, version 24.0 (IBM, Armonk, NY, USA). The relationship between newborn weight and placental weight, and between maternal BMI and placental weight, was assessed using Pearson’s correlation coefficient (for continuous data) and the square of the sample correlation coefficient (R2). The correlation between newborn weight and placental weight was also assessed by simple linear regression. One-way analysis of variance was applied to assess the associations of birthweight, placental weight and birthweight/placental weight ratio with the sex of the newborn. A P value <0.05 was considered statistically significant.
Results
A total of 211 placentae were included in this study, selected from 390 consecutive samples after exclusion criteria were applied (Table 1). The mean maternal age was 28.82 ± 5.09 years (range, 18–48 years), and mean maternal BMI was 23.42 ± 4.12 kg/m2 (range, 14.8–41.30 kg/m2). Out of 211 term newborns, 110 were male and 101 were female (Figure 1). The mean birthweight of the term newborns was 2966.66 ± 0.39 g (range, 2350–3960 g). The mean placental weight was 494.45 ± 110.39 g (range, 260–870 g), and mean birthweight: placental weight ratio was 6.21 ± 1.21 (range, 3.35–11.62). The 10th to 90th percentile range for the birthweight: placental weight ratio was 4.78–7.71 (Table 1). The BMI of the majority of mothers (72.5%) was <24.99 kg/m2, while 19.4% of the mothers had a BMI of between 25 and 29.99 kg/m2 and 8.1% of the mothers had a BMI ≥ 30 kg/m2 (Table 2). An underweight mother with a BMI of 14.8 kg/m2 delivered a baby with a weight of 3004 g and a placental weight of 520 g.
Table 1.
Distribution of 211 samples according to maternal age and body mass index (BMI), placental weight, term newborn birthweight and birthweight/placental weight ratio.
| Age, years | BMI, kg/m2 | Birthweight, g | Placental weight, g | Birthweight/placental weight ratio | |
|---|---|---|---|---|---|
| Mean | 28.82 | 23.42 | 2966.28 | 494.45 | 6.21 |
| Standard deviation | 5.09 | 4.12 | 353.535 | 110.39 | 1.21 |
| Minimum | 18 | 14.80 | 2350 | 260 | 3.35 |
| Maximum | 48 | 41.30 | 3960 | 870 | 11.62 |
| Percentiles | |||||
| 10th | 22.00 | 19.0800 | 2530.00 | 370.00 | 4.78 |
| 25th | 26.00 | 20.5000 | 2710.00 | 420.00 | 5.4717 |
| 50th | 28.00 | 23.0000 | 2920.00 | 480.00 | 6.1412 |
| 75th | 32.00 | 25.8000 | 3200.00 | 550.00 | 6.7143 |
| 90th | 36.00 | 29.0000 | 3448.00 | 648.00 | 7.71 |
Figure 1.
Distribution of 211 placentae according to the sex of the neonate.
Table 2.
Distribution of 211 placentae according to maternal body mass index (BMI).
| Maternal BMI, kg/m2 | Number of samples | Percentage |
|---|---|---|
| ≤24.99 | 153 | 72.5 |
| 25–29.99 | 41 | 19.4 |
| ≥30 | 17 | 8.1 |
| Total | 211 | 100.0 |
There was a statistically significant positive correlation between birthweight and placental weight (Pearson’s r = 0.454; P = 0.0001). Higher placental weight was found to be significantly associated with higher newborn birthweight (Figure 2 and Table 3), and linear regression analysis showed the following relationship between foetal weight in grams (Y) and placental weight in grams (X): Y = 1.4553X +2246.7 (Figure 2).
Figure 2.
Scatter plot and linear regression analysis showing the association between birthweight and placental weight in 211 singleton uncomplicated pregnancies.
Table 3.
Association of newborn birthweight and maternal body mass index (BMI) with placental weight.
| Birthweight and placental weight | BMI and placental weight | |
|---|---|---|
| Pearson’s correlation coefficient, r | 0.454 | 0.219 |
| Correlation coefficient, R2 | 0.206 | 0.048 |
| Statistical significance | P = 0.0001 | P = 0.001 |
There was also a statistically significant positive correlation between maternal BMI and placental weight (Pearson’s r = 0.219; P = 0.001; Table 3).
A statistically significant positive correlation was found between birthweight and sex of the term neonate (P = 0.017, male versus female birthweights), however, no statistically significant correlation was demonstrated between either placental weight or birthweight: placental weight ratio and the sex of the newborn (Table 4).
Table 4.
Association of newborn birthweight, placental weight, and birthweight: placental weight ratio with the sex of the neonate (n = 211; analysis of variance).
| Parameters | Statistical significance |
|---|---|
| Birthweight with neonate sex | P = 0.017 |
| Placental weight with neonate sex | P = 0.611 |
| Birthweight: placental weight ratio with neonate sex | P = 0.444 |
Discussion
Apparent inconsistencies in the weight of the placenta and fetal/placental weight ratio are directly associated with macrosomia, low birthweight, chromosomal disorders, preterm delivery, intrauterine growth retardation (IUGR), stillbirth, neonatal morbidity, and mortality. Indirectly, placental weight is associated with maternal ethnicity, maternal and fetal genetics, smoking, nutrition, environmental conditions, and drug misuse, including alcohol, maternal diseases, and acute placental injury due to trauma.2–4,10,11
Placental weight and its relationship with neonatal birthweight have been studied for over a century. Data on morphometric measurements of the placenta are ubiquitous in Western literature, but remain poorly addressed in Sri Lanka and other developing countries. There are no uniform national protocols in these countries for pathological examination of the placenta in clinical or autopsy investigations of perinatal morbidity and mortality, where most pathologists follow National Health Service (UK) or College of American Pathologists (USA) protocols for placental examination.5,12 Primarily, such morphometric measurements are heterogeneous worldwide, varying from region to region, country to country, across regions within the same country, and according to the ethnicity/ancestry of mother and fetus. Differences within the same country have been well-established in studies conducted in India, Nigeria, Malaysia, and China.2–4,10,11 Therefore, accurate reference values of placental weight and its relationship with neonatal birthweight and maternal BMI are important in the investigation of neonatal mortality, as well as in stillbirths.
In the present study, mean placental weight, neonate birthweight, and birthweight/placental weight ratio were respectively lower, identical, and higher compared with a selection of previously published studies (Table 5).13–19 The present findings support the evidence that placental weight and neonatal birthweight/placental weight ratio vary according to country, ancestry, and ethnicity. However, measurement methods vary widely between studies, particularly due to differences in placental preparations (fresh or fixed placenta), methodology, and purpose of the study. Fixation of the placenta will affect its weight, with an increase of 3–6%,9,20 according to the duration of the formalin fixation. Fresh unfixed placentae were included in the present study to minimize errors in weight. In contrast, formalin-fixed placentae were preferred in the context of macroscopic pathological examination for better visualization.
Table 5.
Evaluation of mean placental weight, neonate birthweight, and birthweight: placental weight ratio reported in previously published studies compared with the present study.
| Study | Country | Mean birthweight, g | Mean placental weight, g | Mean birthweight/ placental weight ratio |
|---|---|---|---|---|
| Asgharnia et al. 13 | Iran | 3214.3 | 529.7 | – |
| Kafle et al. 14 | Nepal | 2939.93 | 455.76 | 6.6:1 |
| Eskild et al. 15 | Norway | 3567.56 | 674.38 | 5.26:1 (0.190, placental weight/birthweight) |
| Soliman et al. 16 | Qatar | 3185 | 678 | 4.77 |
| Mehare et al. 17 | Ethiopia | 2900 | 524.36 | 5.52 |
| Jain et al. 18 | India (Bhopal) | 2633.5 | 486.78 | 5.78:1 |
| Salmani et al. 19 | India (Kerala) | 3140 | 435.92 | 5.72:1 |
| Present study | Sri Lanka | 2966.28 | 494.45 | 6.21 |
Excessive growth of the placenta (placentomegaly) is associated with multiple maternal and fetal conditions, including maternal diabetes, maternal anaemia, fetal anaemia, congenital syphilis, toxoplasmosis, congenital fetal nephrosis, idiopathic fetal hydrops, multiple placental chorioangiomas, large intervillous thrombi, and a large blood clot beneath the chorionic membrane (fetal surface-roof of the placenta). These are attributed to acute placental injury, poor perinatal outcome, a low Apgar score, respiratory distress syndrome, and perinatal death. Placental hypoplasia, indicated by low placental weight, has been associated with maternal cardiovascular disease, vasculitis, hypertension, diabetes mellitus, accelerated placental maturation, many of the major autosomal disorders, babies with trisomy, and major fetal malformations.10,11,18,21–24
Even though placental weight is an indicator of placental growth, it does not indicate the efficiency of the placental function. Most pathologists opine that the function and efficiency of the placenta are more important for fetal growth than measurements of weight alone: it indirectly depends on maternal well-being, including the nutritional state measured by maternal BMI. The neonatal birthweight to placental weight ratio indicates the adequacy of fetal nutrition by the functional tissue of the placenta.
In keeping with other studies, a linear relationship was found between neonate birthweight and placental weight (P < 0.0001) in the present study, with an estimated relationship between placental weight and the birthweight of the term fetus of y = 1.4553 x + 2246.7, where x is the weight of the placenta in grams and y is the neonate birthweight in grams. This formula may be used to calculate fetal weight in the Northern Province of Sri Lanka during perinatal death investigations of term fetuses, particularly in concealed pregnancies and infant homicides (infanticides). These reference values may also be used to help resolve medico-legal issues related to neonatal death due to trauma (infanticide/fresh neonatal homicide), medical misadventure, negligence, and in deaths where natural and traumatic causes co-exist. 25
Women with high pre-pregnancy BMI have been reported to deliver heavyweight placentae, 26 in keeping with the present study (P < 0.001), but BMI in the present study was calculated at the earliest antenatal visit in the first trimester followed the missed menstrual period. Women with a higher pre-pregnancy BMI are at risk of several obstetric complications (e.g., gestational diabetes mellitus, preeclampsia, and large-for-gestational-age babies) associated with higher morbidity for both mother and child. Surprisingly, an underweight mother in the present study (BMI, 14.8 kg/m2) delivered a baby with a fetal weight of 3004 g and a placental weight of 520 g. These findings highlight that other factors also contribute to fetal growth, in addition to maternal BMI. Data from various agencies show that pregnant mothers from Sri Lanka have been experiencing nutritional deficiencies due to the current economic crisis, in contrast to other western countries where obesity is widespread. In August 2022, an estimated 215 000 Sri Lankan women were pregnant, according to data from the Ministry of Health, Sri Lanka, including 11 000 adolescent girls, while 145 000 women were scheduled to deliver in the next 6 months. 27 Therefore, we recommend a large-scale community study on the relationship between maternal BMI, birthweight and placental weight in a population with an adequate sample size.
A relationship was demonstrated between the sex of the fetus and birthweight in the present study (P = 0.017), in adherence with other studies. 28 As stated by Brown et al., in 2014, 29 ‘fetal sex has long been known to have a consequence in placental weight, with known sex-specific placental gene expression, as well as sex-specific differences in biomarkers and placental gene–environment interactions’. However, no such significant correlation with placental weight (P = 0.611) was found in the present study, in contrast to other studies. 30 This may have been due to inadequate sampling or random representation of samples modified by survey criteria, or there may be no such true relationship between fetal sex and placental weight.
Although ultrasound assessments for dating GA and gestational position and accreta spectrum disorders of the placenta were performed in the present study, according to the Green-top guideline No. 27a, 31 a detailed morphological assessment of each placenta was not conducted. The present study did not assess the relationship between ultrasonography morphological assessment of the placenta and birthweight or maternal BMI, which may have been more informative.
A group of healthy and uncomplicated pregnancies with no specific placental pathology were studied in a single obstetric unit of a tertiary care hospital. Samples were collected in a consecutive manner for a period of 6 months (between February 2022 and August 2022). The study was conducted as a survey/pilot project to ascertain the study objectives. These limitations restrict the use of study findings in a nationwide manner. Similarly, correlation of ultrasound details of the placenta with maternal BMI and neonate birthweight will yield more data. The latter will be assessed in a separate prospective study by the authors. The authors recommend multi-centred studies with adequate sample sizes to overcome these limitations.
Conclusion
The mean placental weight of the Sri Lankan term fetus is most likely to be lower than in western studies, but consistent with South Asian studies according to the present analysis. A significant relationship was demonstrated between placental weight and birthweight or maternal BMI. These figures may be utilized to investigate the mortality and morbidity of term infants born in the Northern Province of Sri Lanka as well as to aid medico-legal investigation of term stillbirth and neonatal death. Further multicentred research is necessary to evaluate these parameters along with the health of infants born to nutritionally deprived mothers in the ongoing economic crisis.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605231172895 for Placental weight and its relationship with the birth weight of term infants and body mass index of the mothers by Raveendran Sathasivam, Pranavan Selliah, Raguraman Sivalingarajah, Uruthirapasupathi Mayorathan and Baththirange Malaka Munasinghe in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605231172895 for Placental weight and its relationship with the birth weight of term infants and body mass index of the mothers by Raveendran Sathasivam, Pranavan Selliah, Raguraman Sivalingarajah, Uruthirapasupathi Mayorathan and Baththirange Malaka Munasinghe in Journal of International Medical Research
Acknowledgement
The authors would like to thank the Director, consultants, doctors, staff, and midwives of the Professorial Obstetric Unit of the Teaching Hospital, Jaffna, Sri Lanka for the immense support extended during the study. Thanks also to Ms. Sathana Paramanathan, Research Assistant, University of Jaffna, for her valuable contribution during data analysis.
Author contributions: Raveendran Sathasivam – literature review, study design, writing the proposal, formulation of the questionnaire formulation, reading histology slides, data analysis, preparation of the manuscript.
Pranavan S – work on ethical clearance, data collection, reading histology of the placentae.
Raguraman S – data collection, data entry, manuscript preparation.
Mayorathan U – preparation of placenta for histology, reading histology slides, research supervisor.
Munasinghe BM – questionnaire preparation, data collection, manuscript editing, corresponding author.
The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data accessibility: Supplementary material for this paper is available upon request.
ORCID iD: Baththirange Malaka Munasinghe https://orcid.org/0000-0001-8373-4752
References
- 1.Roescher AM, Timmer A, Erwich JJ, et al. Placental pathology, perinatal death, neonatal outcome, and neurological development: a systematic review. PLoS One 2014; 9: e89419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janthanaphan M, Kor-Anantakul O, Geater A.Placental weight and its ratio to birth weight in normal pregnancy at Songkhlanagarind Hospital. J Med Assoc Thai 2006; 89: 130–137. [PubMed] [Google Scholar]
- 3.Panti AA, Ekele BA, Nwobodo EI, et al. The relationship between the weight of the placenta and birth weight of the neonate in a Nigerian Hospital. Niger Med J 2012; 53: 80–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Implantation, embryogenesis and placental development. In: Cunningham FG, Leveno KJ, Bloom SL, et al. (eds) Williams Obstetrics. 22nd ed. New York: McGraw-Hill, 2005, pp. 39–90.
- 5.Langston C, Kaplan C, Macpherson T, et al. Practice guideline for examination of the placenta: developed by the Placental Pathology Practice Guideline Development Task Force of the College of American pathologists. Arch Pathol Lab Med 1997; 121: 449–476. [PubMed] [Google Scholar]
- 6.Burkhardt T, Schäffer L, Schneider C, et al. Reference values for the weight of freshly delivered term placentas and for placental weight-birth weight ratios. Eur J Obstet Gynecol Reprod Biol 2006; 128: 248–252. [DOI] [PubMed] [Google Scholar]
- 7.Nascente LMP, Grandi C, Aragon DC, et al. Placental measurements and their association with birth weight in a Brazilian cohort. Rev Bras Epidemiol 2020; 23: e200004. [DOI] [PubMed] [Google Scholar]
- 8.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. [DOI] [PubMed] [Google Scholar]
- 9.Khong TY, Mooney EE, Ariel I, et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group consensus statement. Arch Pathol Lab Med 2016; 140: 698–713. [DOI] [PubMed] [Google Scholar]
- 10.Kowsalya V, Vijayakumar R, Valli G, et al. Morphometry examination of placenta in birth weight of full-term newborns in Puducherry, India. Pak J Biol Sci 2013; 16: 895–897. [DOI] [PubMed] [Google Scholar]
- 11.Sivarao S, Vidyadaran MK, Jammal AB, et al. Weight, volume and surface area of placenta of normal pregnant women and their relation to maternal and neonatal parameters in Malay, Chinese and Indian ethnic groups. Placenta 2002; 23: 691–696. [DOI] [PubMed] [Google Scholar]
- 12.Evans C, Cox P. Tissue pathway for histopathological examination of the placenta. 2nd ed. The Royal College of Pathologists, https://www.rcpath.org/profession/publications/cancer-datasets.html (2019, accessed 28 April 2022).
- 13.Asgharnia M, Esmailpour N, Poorghorban M, et al. Placental weight and its association with maternal and neonatal characteristics. Acta Med Iran 2008; 46: 467–472. [Google Scholar]
- 14.Kafle R, Nibedita K, Gupta BK.Mean birth weight and mean placental weight among deliveries in a tertiary care hospital. JNMA J Nepal Med Assoc 2019; 57: 364–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eskild A, Haavaldsen C, Vatten LJ.Placental weight and placental weight to birthweight ratio in relation to Apgar score at birth: a population study of 522 360 singleton pregnancies. Acta Obstet Gynecol Scand 2014; 93: 1302–1308. [DOI] [PubMed] [Google Scholar]
- 16.Soliman AT, Eldabbagh M, Saleem W, et al. Placental weight: relation to maternal weight and growth parameters of full-term babies at birth and during childhood. J Trop Pediatr 2013; 59: 358–364. [DOI] [PubMed] [Google Scholar]
- 17.Mehare T, Kebede D.Fetoplacental weight relationship in normal pregnancy and pregnancy complicated by pregnancy-induced hypertension and abruption of placenta among mothers who gave birth in Southern Ethiopia, 2018. Obstet Gynecol Int 2020; 2020: 6839416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jain A, Sharma D, Sharma V, et al. Study of placental weight in normal and pre-eclamptic pregnancies and its correlation with birth weight. Int J Med Res Rev 2016; 4: 2–8. [Google Scholar]
- 19.Salmani D, Purushothaman S, Somashekara SC, et al. Study of structural changes in placenta in pregnancy-induced hypertension. J Nat Sci Biol Med 2014; 5: 352–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox GE, Van Wesep R, Resau JH, et al. The effect of immersion formaldehyde fixation on human placental weight. Arch Pathol Lab Med 1991; 115: 726–728. [PubMed] [Google Scholar]
- 21.Weng EY, Moeschler JB, Graham JM., Jr.Longitudinal observations on 15 children with Wiedemann-Beckwith syndrome. Am J Med Genet 1995; 56: 366–373. [DOI] [PubMed] [Google Scholar]
- 22.Milani D, Pezzani L, Tabano S, et al. Beckwith-Wiedemann and IMAGe syndromes: two very different diseases caused by mutations on the same gene. Appl Clin Genet 2014; 7: 169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morales-Roselló J, Dias T, Khalil A, et al. Birth-weight differences at term are explained by placental dysfunction, but not by maternal ethnicity. Ultrasound Obstet Gynecol 2018; 52: 488–493. [DOI] [PubMed] [Google Scholar]
- 24.Weerakkody Y, Jones J. Placentomegaly. Reference article, Radiopaedia.org. 10.53347/rID-13573 (2011, accessed 25 December 2021). [DOI]
- 25.Cohen MC, Scheinberg I.Forensic aspects of perinatal deaths. Acad Forensic Pathol 2018; 8: 452–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brouwers L, Franx A, Vogelvang TE, et al. Maternal prepregnancy body mass index with placental histopathological characteristics in uncomplicated term pregnancies. Pediatr Dev Pathol 2019; 22: 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The United Nations Office at Geneva. Sri Lanka’s economic crisis pushes health system to brink of collapse, UN Geneva Working for Peace, Rights and Well-being. https://www.ungeneva.org/en/news-media/news/2022/08/sri-lankas-economic-crisis-pushes-health-system-brink-collapse (2022, accessed 5 October 2022).
- 28.Davis RO, Cutter GR, Goldenberg RL, et al. Fetal biparietal diameter, head circumference, abdominal circumference and femur length. A comparison by race and sex. J Reprod Med 1993; 38: 201–206. [PubMed] [Google Scholar]
- 29.Brown ZA, Schalekamp-Timmermans S, Tiemeier HW, et al. Fetal sex specific differences in human placentation: a prospective cohort study. Placenta 2014; 35: 359–364. [DOI] [PubMed] [Google Scholar]
- 30.Flatley C, Sole-Navais P, Vaudel M, et al. Placental weight centiles adjusted for age, parity and fetal sex. Placenta 2022; 117: 87–94. [DOI] [PubMed] [Google Scholar]
- 31.Jauniaux E, Alfirevic Z, Bhide AG, et al. ; Royal College of Obstetricians and Gynaecologists. Placenta praevia and placenta accreta: diagnosis and management: Green-top Guideline No. 27a. BJOG 2019; 126: e1–e48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605231172895 for Placental weight and its relationship with the birth weight of term infants and body mass index of the mothers by Raveendran Sathasivam, Pranavan Selliah, Raguraman Sivalingarajah, Uruthirapasupathi Mayorathan and Baththirange Malaka Munasinghe in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605231172895 for Placental weight and its relationship with the birth weight of term infants and body mass index of the mothers by Raveendran Sathasivam, Pranavan Selliah, Raguraman Sivalingarajah, Uruthirapasupathi Mayorathan and Baththirange Malaka Munasinghe in Journal of International Medical Research